Version Changes
Revised. Amendments from Version 1
The abstract was rewritten to make it concise and increase readability. The introduction section was amended to make the aim more specific and precise. Changes were made in the p-values for better understanding. The conclusion section was amended to specify the implication of the study.
Abstract
Background: Coronavirus disease 2019 (COVID-19) requires mass immunization to control the severity of symptoms and global spread. Data from developed countries have shown a high prevalence of parental COVID-19 vaccine hesitancy. However, parental vaccine hesitancy data in low- and middle-income countries are scarce. This study aimed to assess the prevalence of parental vaccine hesitancy and identify subgroups with higher odds of vaccine hesitancy in parents in Bangladesh.
Methods: A cross-sectional study was conducted on the parents of children aged <18 years from October 10, 2021 to October 31, 2021. Parents participated in face-to-face interviews in randomly selected locations in Bangladesh using a vaccine hesitancy questionnaire. Factors associated with COVID-19 vaccine hesitancy were identified using binary logistic regression analysis.
Results: Data from 2,633 eligible parents were analyzed. Overall, 42.8% reported COVID-19 vaccine hesitancy for their youngest child. The final model suggested the following factors were associated with hesitancy: children's age; parent's age, religion, occupation, monthly household income, permanent address, living location, status of tobacco use, adherence with regular government vaccination programs (other than COVID-19), perceptions of COVID-19 vaccine efficacy among Bangladeshi children, self-vaccination intentions, reported family members' illness or death from COVID-19, and perceived threat of COVID-19 were the independent predictors of parental COVID-19 vaccine hesitancy. Conversely, participants who were not tobacco users, parents who were very likely to believe that their children or family members could be infected with COVID-19 in the following year and who were very concerned about their children or a family member contracting COVID-19 in the next year had significantly lower odds of COVID-19 vaccine hesitancy.
Conclusions: Our study suggested that vaccine hesitation varied based on sociodemographic characteristics, religion, behavior, and perceived COVID-19 threat. Therefore, interventions focused on addressing vaccine hesitancy among specific subgroups are warranted.
Keywords: Bangladesh, COVID-19, developing countries, parents, pediatrics, vaccine hesitancy.
Introduction
Mass immunization against coronavirus disease 2019 (COVID-19) is one of the heaviest relied upon measures to control the spread of symptomatic severe acute respiratory syndrome coronavirus 2 (SARS-CoV2) and end the global pandemic. 1 Many countries have targeted vaccinating at least 80% of their total population, including individuals aged 18 years and below, to achieve herd immunity. 2 , 3 However, vaccine hesitancy, defined as a delay in acceptance or refusal of vaccines despite the availability of vaccination services, 4 is a significant threat to the smooth uptake of vaccinations worldwide. 5
Since December 2019, more than 433 million COVID-19 cases have been identified globally, and more than 5.8 million people have died of the disease, with a significantly high prevalence in older adults. 6 However, the infection rate among children and adolescents is not negligible, and they can carry and spread the virus. 7 Furthermore, unvaccinated populations are supposedly suitable hosts for new variants. 8
Recent data indicate that a small number of countries, such as the USA, are unlikely to reach the 80% target for herd immunity; however, vaccinating 22% of the American population, which is the size of the pediatric population, would effectively boost community protection against COVID-19. 3 Nonetheless, more than one in three parents in the USA were vaccine-hesitant for their children. 3 In China, this rate was 52.5%. 9 Along with sociodemographic variables such as age, sex, educational qualification, occupation, and religious beliefs, overall vaccine hesitancy also varies by political theology, perceived pandemic threat, or the socioeconomic status of the target population. 10 – 12 Additionally, the reporting of adverse events, the vaccine's effectiveness in children, and availability of research on the specific age groups of their children may play a crucial role when parents decide to vaccinate their children. Furthermore, one survey revealed that along with potential immediate adverse effects of the vaccines, the possible long-term harmful effects were a growing concern for parents. 13
The triumph of immunization, among other programs, relies on the vaccination of a wide proportion of pediatric and adult populations in low- and middle-income countries where variants of concern, such as SARS-CoV-2 B.1.617.2 Delta, have been detected. 14 , 15 In Bangladesh, by November 2021, only 18% of the entire population had been fully vaccinated against this disease. 16 However, approximately 35% of the Bangladeshi population are aged 18 years and younger. 17 Thus, to achieve herd immunity, this young cohort should be included in the mass vaccination program. Therefore, the government of Bangladesh has planned to vaccinate students aged between 12 and 17 years. Vaccination among the young student cohort began, to a limited extent, in cities including Dhaka from November 1, 2021. 18
There is a lack of information regarding vaccine hesitancy among parents of children aged 18 years and below worldwide. In Bangladesh, a previous study revealed that 32% of the adult study population refused to be vaccinated against COVID-19. 10 We hypothesized that the parental vaccine hesitancy rate would not match that in the general adult population. Therefore, this study sought to (1) conduct a nationally representative assessment of parental vaccine hesitancy and (2) identify subgroups of parents with higher odds of vaccine hesitancy.
Methods
Ethics statements
The Institutional Review Board of Uttara Adhunik Medical College and Hospital approved this study (Approval number: UAMC-IRB-2021/09). Written informed consent for both participation and publication of data was obtained from all participants.
Study design and participants
This cross-sectional study was conducted in Bangladesh from October 10, 2021 to October 31, 2021. A margin of 2% error, confidence level of 95%, and response distribution of 50% were used to calculate the sample size to target fathers/mothers of 80 million children and obtain a minimum sample size of 2,401 participants. 19 , 20 Approximately 3,000 parents aged ≥18 years with children aged under 18 years who permanently live in Bangladesh were conveniently invited to participate in individualized interview sessions using a previously employed vaccine hesitancy questionnaire. 10 , 21 , 35 We received data from 2,703 parents, as a result of a 10% refusal rate. However, 36 parents who did not answer all questions were excluded. We also excluded 34 data points for contradicting answers. Considering these exclusions, 2,633 respondents were ultimately included in the final analysis. 35
Study questionnaire
In the first portion of the questionnaire, participants were queried regarding vaccine hesitancy and perceived COVID-19 threat. First, parents were asked about the likelihood of vaccinating their youngest children. Parental vaccine hesitancy was measured using the question, “If a vaccine that would be effective against coronavirus disease among children was available, how likely would you be to have your children vaccinated?” (response options: very likely, somewhat likely, not likely, or definitely not). Second, participants were asked two questions regarding the perceived COVID-19 threat: (1) “How likely is it that your children or a family member could get infected with coronavirus in the next year?” (response options: very likely, somewhat likely, not likely, or definitely not). (2) “How concerned are you that your children or a family member could get infected with coronavirus in the next year?” (response options: very concerned, concerned, slightly concerned, or not concerned at all).
The second part of the questionnaire included a wide array of sociodemographic questions for both children and parents. A set of structured questions assessed the child's health (healthy/disabled), age, and sex. Information on parents' sex, age, religion, current marital status, education, employment status, monthly household income (Bangladeshi taka), permanent address, region of residence (north, south, and central zones in Bangladesh, including Dhaka), current residence type (own/rented/others), family type (nuclear or extended, number of children, current tobacco use status, religious practice habits, and political affiliation was collected. Additionally, parents were asked several other COVID-19 vaccine-related questions: “Do you think the COVID-19 vaccine will be effective among Bangladeshi children?” (response options: no, yes, or skeptical), “Have you received or plan to receive the COVID-19 vaccine,” “Did you or your family member(s) test positive for COVID-19,” and “Have you lost any of your family member(s) to COVID-19?” The last three questions received dichotomous (yes or no) answers.
Sampling technique and data collection
Data were collected from all eight geographic divisions of Bangladesh, and a dual-stage cluster sampling technique was used to include potential samples. We randomly chose marketplaces, shopping malls, waiting rooms of large hospitals, diagnostic centers, bus and railway stations, and residences and processed them as clusters in the first stage. To obtain data from the parents of children with disabilities, we also visited randomly selected centers for disabled children. The list of given data collection sites was collected from division websites. In the second stage, we chose participants conveniently. Data from exclusively the father or mother of a child were taken to avoid repeating data.
Eight teams of two persons each were created. A team member read the questions aloud to the interviewees individually, and read response options from which participants’ choices were recorded. Subsequently, the answers were checked and confirmed by the second team member. The coinvestigator reviewed the data collection sheets for completeness, accuracy, and internal consistency and secured them with the principal investigator. Individual face-to-face interviews were conducted to ensure participant privacy. All participants were informed of the voluntary nature of their participation, and the interviews were conducted in Bangla.
Statistical analyses
The crucial outcome of this study was vaccine hesitancy. We dichotomized the four responses to the vaccine hesitancy question as either a positive (very likely and somewhat likely) or a negative (not likely and definitely not) attitude toward the COVID-19 vaccine. 10 Fisher’s exact test was used for two nominal variables, and the chi-square test was used for more than two nominal variables to assess vaccine hesitancy rates and draw comparisons between the groups. Binary logistic regression analyses were performed to identify the predictors of parental COVID-19 vaccine hesitancy and compute adjusted odds ratios (AORs) with a 95% confidence interval (CI). Factors significantly associated with vaccine hesitancy in the descriptive analysis were included in the regression model. A goodness-of-fit test for the adjusted logistic regression model was performed using the Hosmer-Lemeshow test. The significance level was set at p<0.05, and SPSS (version 22.0; IBM Corp; RRID: SCR_002865) was used to perform all data analyses.
Results
Parents and children's characteristics
Overall, 2,633 parents aged 34.97±7.87 years (mean±standard deviation) were included in the analysis, with 52.8% (1,390) being women. In total, 396 (15%) parents of children with a physical disability were included. Among the children, 1,372 (52.1%) were boys, and 1,206 (45.8%) were in the 0–4-year-old group. Most parents (653, 24.8%) were in the 31–35-year-old group. Overall, 2,358 (89.4%) parents were Muslim, 1,791 (68%) were a nuclear family member, 1,075 (40.8%) had two children, 1,022 (38.8%) had a low education level, 756 (28.7%) were homemakers, and 833 (31.6%) had a low-middle household income. Among all participants, 1,528 (58%) were from a village, 1,323 (50%) were living in the central zone including Dhaka, 1,695 (64.4%) were tobacco non-users, 1,797 (68.2%) were regular religious practitioners, and 1,032 (39.2%) were politically neutral respondents. A total of 177 (6.3%) parents did not adhere to the regular government vaccination programs other than COVID-19, and 1,458 (55.4%) remained skeptical about the effectiveness of the COVID-19 vaccine for Bangladeshi children. Furthermore, 722 (27.4%) parents were either not vaccinated or did not receive the COVID-19 vaccine; however, 752 (28.6%) parents reported that they or their family members tested positive for COVID-19, and 151 (5.7%) had lost a family member to COVID-19. Details of the responses to the questions regarding the likelihood of children or family members' infection by COVID-19 and the level of concern about children or family members contracting the disease in the next year are shown in Table 1.
Table 1.
Descriptive analysis: Sociodemographic characteristics, COVID-19 threat, and parental vaccine hesitancy.
| Variables | Total sample n (%) | Likelihood of vaccinating children | P-value | ||
|---|---|---|---|---|---|
| Not likely/definitely not n (%) | Very likely/somewhat likely n (%) | ||||
| All participants | 2633 (100) | 1126 (42.8) | 1507 (57.2) | N/A | |
| Children's health | 0.507 | ||||
| Healthy | 2237 (85) | 957 (42.8) | 1280 (57.2) | ||
| Disabled | 396 (15) | 169 (42.7) | 227 (57.3) | ||
| Children's age group | <0.001 | ||||
| 0–4 | 1206 (45.8) | 649 (53.8) | 557 (46.2) | ||
| 5–9 | 870 (33) | 344 (39.5) | 526 (60.5) | ||
| 10–14 | 354 (13.4) | 98 (27.7) | 256 (72.3) | ||
| 15–<18 | 203 (7.7) | 35 (17.2) | 168 (82.8) | ||
| Children's sex | <0.001 | ||||
| Male | 1372 (52.1) | 537 (39.1) | 835 (60.9) | ||
| Female | 1261 (47.9) | 589 (46.7) | 672 (53.3) | ||
| Parents' age group | <0.001 | ||||
| 18–25 | 268 (10.2) | 146 (54.5) | 122 (45.5) | ||
| 26–30 | 604 (22.9) | 329 (54.5) | 275 (45.5) | ||
| 31–35 | 653 (24.8) | 288 (43.8) | 367 (56.2) | ||
| 36–40 | 563 (21.4) | 223 (39.6) | 340 (60.4) | ||
| 41–45 | 285 (10.8) | 86 (30.2) | 199 (69.8) | ||
| 46–50 | 162 (6.2) | 37 (22.8) | 125 (77.2) | ||
| ≥51 | 98 (3.7) | 19 (19.4) | 79 (80.6) | ||
| Parents' sex | 0.237 | ||||
| Female | 1390 (52.8) | 604 (43.5) | 786 (52.2) | ||
| Male | 1243 (47.2) | 522 (42) | 721 (58) | ||
| Marital status | 0.438 | ||||
| Married | 2527 (96) | 1082 (42.8) | 1445 (57.2) | ||
| Divorced or widowed | 106 (4) | 44 (41.5) | 62 (58.5) | ||
| Religion | <0.001 | ||||
| Muslim | 2358 (89.4) | 1069 (45.4) | 1285 (54.6) | ||
| Hindu | 258 (9.8) | 56 (21.7) | 202 (78.3) | ||
| Buddhist | 6 (0.2) | 0 (0) | 6 (100) | ||
| Christian | 15 (0.6) | 1 (6.7) | 14 (93.3) | ||
| Type of family | 0.167 | ||||
| Extended family | 842 (32) | 372 (44.2) | 470 (55.8) | ||
| Nuclear family | 1791 (68) | 754 (42.1) | 1037 (57.9) | ||
| Number of children | 0.993 | ||||
| One | 924 (35.1) | 395 (42.7) | 529 (57.3) | ||
| Two | 1075 (40.8) | 461 (42.9) | 614 (57.1) | ||
| Three or more | 634 (24.1) | 270 (42.6) | 364 (57.4) | ||
| Educational qualification | <0.001 | ||||
| ≤ High school | 1022 (38.8) | 473 (46.3) | 549 (53.7) | ||
| Higher secondary education | 594 (22.6) | 316 (53.2) | 278 (46.8) | ||
| Graduate | 608 (23.1) | 236 (38.8) | 372 (61.2) | ||
| Postgraduate | 409 (15.5) | 101 (24.7) | 308 (75.3) | ||
| Occupation | <0.001 | ||||
| Service | 677 (25.7) | 248 (36.6) | 429 (63.4) | ||
| Business | 472 (17.9) | 198 (41.9) | 274 (58.1) | ||
| Unemployed | 179 (6.8) | 132 (73.7) | 47 (26.3) | ||
| Student | 56 (2.1) | 34 (30.7) | 22 (39.3) | ||
| Home maker | 756 (28.7) | 364 (48.1) | 392 (51.9) | ||
| Healthcare | 216 (8.2) | 64 (29.6) | 152 (70.4) | ||
| Daily labor | 277 (10.5) | 86 (31) | 191 (69) | ||
| Monthly household income (৳) | <0.001 | ||||
| <৳ 15 000 | 799 (30.3) | 401 (50.2) | 398 (49.8) | ||
| ৳ 15000–30000 | 833 (31.6) | 409 (49.1) | 424 (50.9) | ||
| ৳ 31000–45000 | 433 (16.4) | 150 (34.6) | 283 (65.4) | ||
| >৳ 45000 | 568 (21.6) | 166 (29.2) | 402 (70.8) | ||
| Current residence type | 0.030 | ||||
| Own | 1436 (54.5) | 646 (45) | 790 (55) | ||
| Rented | 1075 (40.8) | 427 (39.7) | 648 (60.3) | ||
| Others | 122 (4.6) | 53 (43.4) | 69 (56.6) | ||
| Permanent address | <0.001 | ||||
| Village | 1528 (58) | 687 (45) | 814 (55) | ||
| Semi-urban | 535 (20.3) | 247 (45.2) | 288 (53.8) | ||
| City | 570 (21.6) | 192 (33.7) | 378 (66.3) | ||
| Current living location | <0.001 | ||||
| Central zone | 1323 (50.2) | 542 (41.0) | 781 (59.0) | ||
| North zone | 921 (35) | 472 (51.2) | 449 (48.8) | ||
| South zone | 389 (14.8) | 112 (28.8) | 277 (71.2) | ||
| Present tobacco user | <0.001 | ||||
| No | 1695 (64.4) | 679 (40.1) | 1016 (59.9) | ||
| Yes | 938 (35.6) | 447 (47.7) | 491 (52.3) | ||
| Regular religious practice | 0.099 | ||||
| No | 836 (31.8) | 377 (45.1) | 459 (54.9) | ||
| Yes | 1797 (68.2) | 749 (41.7) | 1048 (58.3) | ||
| Political affiliation | <0.001 | ||||
| Ruling party | 779 (30.3) | 283 (35.8) | 516 (64.6) | ||
| Opposition | 296 (11.2) | 175 (59.1) | 121 (40.9) | ||
| Neutral | 1032 (39.2) | 488 (47.3) | 544 (52.7) | ||
| Prefer not to say | 506 (19.2) | 180 (35.6) | 326 (64.4) | ||
| Vaccinated/plan to vaccinate children under regular (other than COVID-19) govt. vaccination programs | <0.001 | ||||
| No | 177 (6.7) | 103 (58.2) | 74 (41.8) | ||
| Yes | 2456 (93.3) | 1023 (41.7) | 1433 (58.3) | ||
| Do you think the COVID-19 vaccine will be effective in Bangladeshi children? | <0.001 | ||||
| No | 167 (6.3) | 151 (90.4) | 16 (9.6) | ||
| Yes | 1008 (38.3) | 54 (5.4) | 954 (94.6) | ||
| Skeptical | 1458 (55.4) | 921 (63.2) | 537 (36.8) | ||
| Have you taken or plan to take the COVID-19 vaccine? | <0.001 | ||||
| No | 722 (27.4) | 653 (88) | 87 (12) | ||
| Yes | 1911 (72.6) | 491 (25.7) | 1420 (74.3) | ||
| Have you or your family member(s) tested positive for COVID-19? | <0.001 | ||||
| No | 1881 (71.4) | 947 (50.3) | 934 (49.7) | ||
| Yes | 752 (28.6) | 179 (23.8) | 573 (76.2) | ||
| Have you lost any of your family member(s) to COVID-19? | <0.001 | ||||
| No | 2482 (94.3) | 1105 (44.5) | 1377 (55.5) | ||
| Yes | 151 (5.7) | 21 (13.9) | 130 (86.1) | ||
| Perceived likelihood of children or family members' infection in the next year | <0.001 | ||||
| Very likely | 345 (13.1) | 51 (14.8) | 294 (85.2) | ||
| Somewhat likely | 1678 (63.7) | 665 (39.6) | 1013 (60.4) | ||
| Not likely | 451 (17.1) | 296 (65.6) | 155 (34.4) | ||
| Definitely not | 159 (6) | 114 (71.7) | 45 (28.3) | ||
| Level of concern about children or family members' infection in the next year | <0.001 | ||||
| Very concerned | 386 (14.7) | 72 (18.7) | 314 (81.3) | ||
| Concerned | 1020 (38.7) | 384 (37.6) | 636 (62.4) | ||
| Slightly concerned | 673 (25.6) | 303 (45) | 370 (55) | ||
| Not concerned at all | 554 (21) | 367 (66.2) | 187 (33.8) | ||
Results of the descriptive analysis
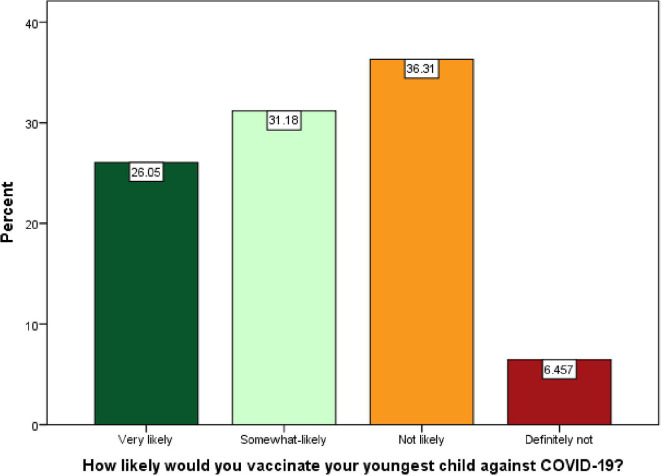
Overall, 42.8% of parents reported hesitancy toward the COVID-19 vaccine for their youngest child. Closer analysis revealed that 26.05% of parents were very likely, 31.18% were somewhat likely, and 36.31% were not likely to vaccinate their child. While only 6.46% were definitely not vaccinating their child against COVID-19 ( Figure 1). The incidence of vaccine hesitancy was significantly high among the parents of 0–4-year-old children (53.8%; p<0.001), parents of girls (46.7%; p<0.001), young parents (54.5%; p<0.001), Muslims (45.4%; p<0.001), parents who received college education (53.2%; p<0.001), unemployed parents (73.7%; p<0.001), parents with a household income of <৳15 000 (50.2%; p<0.001), those who lived in their own house (45%; p=0.030), came from a village (45%; p<0.001), lived in the north zone (51.2%; p<0.001), tobacco users (47.7%; p<0.001), and parents politically affiliated with opposition parties (59.1%; p<0.001). Similarly, participants who did/will not vaccinate their child with regular vaccines (other than COVID-19) available under government programs (58.2%; p<0.001), those who did not believe in the effectiveness of the COVID-19 vaccine for Bangladeshi children (90%; p<0.001), and those who did not/will not receive the COVID-19 vaccine for themselves (88%; p<0.001) showed high vaccine hesitancy. Parents who were not likely to believe that their children or a family member could be infected with COVID-19 in the next year (71.7%; p<0.001) and those not concerned about their children or a family member getting COVID-19 in the next year (66.2%; p<0.001) showed high levels of vaccine hesitancy ( Table 1).
Figure 1.
Likelihood of COVID-19 vaccine acceptance/refusal by Bangladeshi parents for children aged <18.
Results of the regression analysis
Subgroups with significant higher odds of vaccine hesitancy were found to be parents of children aged 0–4 years (AOR=5.87, 95% CI=2.91–11.85; p<0.001), parents aged 26–30 years (AOR=2.73, 95% CI=1.04–7.16; p=0.035), Muslims (AOR=24.27, 95% CI=2.36–248.74; p=0.007), unemployed parents (AOR=2.94, 95% CI=1.35–6.41; p=0.007), parents with a household income of <৳15 000 (AOR=1.49, 95% CI=0.962–1.84; p=0.009), those from a semi-urban area (AOR=1.61, 95% CI=1.09–2.38; p=0.016), those residing in the north zone (AOR=3.71, 95% CI=2.37–5.82; p<0.001), those who did not vaccinate or will not vaccinate their child with regular vaccines (other than COVID-19) available under government programs (AOR=1.93, 95% CI=1.19–3.14; p=0.007), those who did not believe in the effectiveness of the COVID-19 vaccine for Bangladeshi children (AOR=5.80, 95% CI=3.12–10.78; p<0.001), and those who did/will not receive the COVID-19 vaccine for themselves (AOR=10.15, 95% CI=7.16–14.39; p<0.001).
Contrarily, participants who were non-tobacco users (AOR=0.71, 95% CI=0.53–0.96; p=0.025), who appeared to be very likely to believe that their children or a family member could be infected with COVID-19 in the next year (AOR=0.21, 95% CI=0.97–0.44; p<0.001), and who were very concerned about their children or a family member contracting COVID-19 in the next year (AOR=0.34, 95% CI=0.21–0.58; p<0.001) had significantly lower odds of COVID-19 vaccine hesitancy ( Table 2).
Table 2.
Binary logistic regression: predictors of parental vaccine hesitancy in study participants.
| Variables | Adjusted OR | Standard error | 95% CI | P-value | |
|---|---|---|---|---|---|
| Children's age group (year) | |||||
| 0–4 | 5.876 | 0.358 | 2.914 | 11.850 | <0.001 |
| 5–10 | 2.845 | 0.348 | 1.438 | 5.631 | 0.003 |
| 11–14 | 1.101 | 0.359 | 0.545 | 2.225 | 0.789 |
| 15–<18 | References | ||||
| Children's sex | |||||
| Male | 0.918 | 0.127 | 0.716 | 1.176 | 0.498 |
| Female | Reference | ||||
| Parents' age group | |||||
| 18–25 | 1.513 | 0.522 | 0.544 | 4.205 | 0.427 |
| 26–30 | 2.732 | 0.492 | 1.042 | 7.165 | 0.041 |
| 31–35 | 2.755 | 0.481 | 1.073 | 7.075 | 0.035 |
| 36–40 | 2.737 | 0.476 | 1.077 | 6.958 | 0.034 |
| 41–45 | 2.524 | 0.487 | 0.972 | 6.552 | 0.057 |
| 46–50 | 1.101 | 0.522 | 0.396 | 3.064 | 0.853 |
| ≥51 | Reference | ||||
| Religion | |||||
| Muslim | 24.277 | 1.187 | 2.369 | 248.740 | 0.007 |
| Hindu | 18.704 | 1.206 | 1.758 | 198.977 | 0.015 |
| Others | Reference | ||||
| Educational qualification | |||||
| ≤High school | 1.002 | 0.279 | 0.579 | 1.731 | 0.995 |
| Higher secondary education | 1.292 | 0.246 | 0.798 | 2.093 | 0.297 |
| Graduate | 1.007 | 0.223 | 0.651 | 1.560 | 0.974 |
| Postgraduate | Reference | ||||
| Occupation | |||||
| Service | 2.327 | 0.303 | 1.285 | 4.213 | 0.005 |
| Business | 1.463 | 0.310 | 0.797 | 2.686 | 0.219 |
| Unemployed | 2.943 | 0.398 | 1.350 | 6.415 | 0.007 |
| Student | 4.389 | 0.480 | 1.714 | 11.242 | 0.002 |
| Home maker | 2.105 | 0.281 | 1.214 | 3.650 | 0.008 |
| Healthcare | 2.775 | 0.370 | 1.344 | 5.728 | 0.006 |
| Daily labor | Reference | ||||
| Monthly household income (৳) | |||||
| <৳ 15 000 | 1.499 | 0.266 | 0.962 | 1.840 | 0.009 |
| ৳ 15000–30000 | 0.826 | 0.210 | 0.547 | 1.248 | 0.364 |
| ৳ 31000–45000 | 0.559 | 0.216 | 0.366 | 0.854 | 0.007 |
| >৳ 45000 | Reference | ||||
| Current residence type | |||||
| Own | 1.202 | 0.310 | 0.655 | 2.205 | 0.552 |
| Rented | 0.984 | 0.311 | 0.535 | 1.810 | 0.959 |
| Others | Reference | ||||
| Permanent address | |||||
| Village | 1.259 | 0.177 | 0.891 | 1.780 | 0.192 |
| Semi-urban | 1.614 | 0.198 | 1.095 | 2.381 | 0.016 |
| City | Reference | ||||
| Current living location | |||||
| Central zone including Dhaka | 3.112 | 0.213 | 2.049 | 4.727 | <0.001 |
| North zone | 3.716 | 0.230 | 2.370 | 5.827 | <0.001 |
| South zone | Reference | ||||
| Present tobacco user | |||||
| No | 0.716 | 0.149 | 0.535 | 0.959 | 0.025 |
| Yes | Reference | ||||
| Political affiliation | |||||
| Ruling party | 1.001 | 0.188 | 0.692 | 1.448 | 0.997 |
| Opposition | 1.310 | 0.261 | 0.785 | 2.188 | 0.301 |
| Neutral | 0.971 | 0.176 | 0.687 | 1.371 | 0.865 |
| I prefer not to say | Reference | ||||
| Vaccinated/plan to vaccinate children under regular (other than COVID-19) govt. vaccination programs | |||||
| No | 1.937 | 0.247 | 1.193 | 3.144 | 0.007 |
| Yes | Reference | ||||
| Do you think the COVID-19 vaccine will be effective for Bangladeshi children | |||||
| No | 5.805 | 0.316 | 3.124 | 10.786 | <0.001 |
| Yes | 0.052 | 0.171 | 0.037 | 0.073 | <0.001 |
| Skeptical | Reference | ||||
| Have you taken or plan to take the COVID-19 vaccine | |||||
| No | 10.152 | 0.178 | 7.161 | 14.392 | <0.001 |
| Yes | Reference | ||||
| Have you or your family member(s) tested positive for COVID-19 | |||||
| No | 1.320 | 0.164 | 0.956 | 1.822 | 0.091 |
| Yes | Reference | ||||
| Have you lost any of your family member(s) to COVID-19 | |||||
| No | 2.502 | 0.337 | 1.293 | 4.839 | 0.006 |
| Yes | Reference | ||||
| Perceived likelihood of children or family members' infection in the next year | |||||
| Very likely | 0.206 | 0.383 | 0.097 | 0.437 | <0.001 |
| Somewhat likely | 0.413 | 0.330 | 0.216 | 0.788 | 0.007 |
| Not likely | 0.687 | 0.329 | 0.360 | 1.309 | 0.253 |
| Definitely not | Reference | ||||
| Level of concern about children or family members' infection in the next year | |||||
| Very concerned | 0.345 | 0.267 | 0.205 | 0.583 | <0.001 |
| Concerned | 0.502 | 0.207 | 0.334 | 0.754 | 0.001 |
| Slightly concerned | 0.593 | 0.202 | 0.399 | 0.881 | 0.010 |
| Not concerned at all | Reference | ||||
Discussion
This nationally representative comprehensive study found a significantly high prevalence of COVID-19 vaccine hesitancy among parents in Bangladesh for their children. The prevalence of parental vaccine hesitancy was much higher than the prevalence previously found in adults (42.8 vs 32.5), which supported our hypothesis. There were substantial differences in COVID-19 vaccine hesitancy according to sociodemographic factors and perceived COVID-19 threat among parents. The logistic regression model revealed that the children's age and parents' age, religion, occupation, monthly household income, permanent address, current living location, tobacco use, adherence to the regular government pediatric vaccination programs (other than COVID-19), perception about COVID-19 vaccine effectiveness for children in Bangladesh, self-vaccine hesitancy, loss of a family member due to COVID-19, and perceived COVID-19 threat could all be used independently to predict parental vaccine hesitancy for children aged <18 years.
To the best of our knowledge, this is the first study to examine parental COVID-19 vaccine hesitancy in Bangladesh. Furthermore, very limited data are available for parental vaccine hesitancy in Indian subcontinental countries. Thus, there is limited information about the previous hesitancy rate in this region. However, the rate observed in this study (42.8%) is similar to that found in the USA (42%) 21 and slightly lower than that found in China (52%). 9 Contrarily, the observed rate was significantly higher than that in Brazil, Malaysia, and Saudi Arabia. 8 , 22 , 23 The high parental vaccine hesitancy rate in Bangladesh poses a threat to the global public health goal of vaccinating an optimal percentage of the subcontinental population and achieving herd immunity; this is a concern not only in Bangladesh but also in other countries in the Indian subcontinent.
Health behavior theory is centrally influenced by disease risk perception. Herein, a strong association was found between perceived COVID-19 threat and parental vaccine hesitancy. Parents who thought their children or family members were not likely to be at risk of contracting COVID-19 were highly hesitant toward vaccinating their children. Similarly, parents who were not concerned about children or family members’ infections were hesitant. Furthermore, vaccine hesitancy was significantly higher among those who did not believe or remained skeptical about COVID-19 vaccine efficacy among Bangladeshi children than among those who did. These findings were consistent with the results of previous studies that measured COVID-19 vaccine hesitancy among the adult population. 10 , 24 , 25 Ignorance, belief in conspiracy theories, and even denial of the existence of COVID-19 may influence one's perceptions of self-vaccination or vaccinating a child. 26 Therefore, further studies are warranted to improve understanding the in-depth association between COVID-19 threat and vaccine hesitancy among different population groups.
Parents who reported unemployment, an education level lower than or equal to high school, a household income of <৳ 15 000-৳ 30 000, along with those from the village or semi-urban area were significantly more vaccine-hesitant. Similarly, a previous study found high vaccine hesitancy among parents who were unemployed, had a low education level, and those belonging to lower-income in several high- and middle-income countries. 3 , 8 , 22 , 27 Furthermore, our previous study on the adult Bangladeshi population found a similar trend. 10 Global research and studies conducted in the USA and Saudi Arabia among the general population reported identical results. 28 – 30
A previous study found a higher prevalence of vaccine hesitancy among younger parents and parents of children aged between 0 and 4 years, 21 and our analysis yielded similar results. However, unlike a previous study in Malaysia (a multi-ethnic country), 23 in Bangladesh, we found high vaccine hesitancy among Muslim parents than among non-Muslim parents in Bangladesh. Hence, more studies are warranted to understand the influence of religion on the decisions regarding vaccine acceptance and rejection.
Our study found a significantly high prevalence of parental vaccine hesitancy among tobacco users. A previous study also found a similar result, citing the association between unhealthy life practices and vaccine hesitancy among tobacco users. 10 Interestingly, vaccine hesitancy among parents living in the north zone of Bangladesh has also been shown to be high. This is likely because the north zone of Bangladesh is a tobacco-producing area with a high poverty level. Therefore, this information may explain the high prevalence of vaccine hesitancy among parents who are tobacco users and reside in the north zone of Bangladesh.
Additionally, this study found a strong association between self-vaccination intention and vaccination decision for children. The incidence of parental vaccine hesitancy was 10 times higher among parents who did not receive or will not receive the COVID-19 vaccine for themselves than among those who did and will receive the COVID-19 vaccine. Furthermore, parents who did not get their children vaccinated with regular vaccines other than COVID-19 were also highly hesitant toward the COVID-19 vaccine for their children, indicating stubborn vaccine hesitancy among groups of people. Therefore, special advocacy targeting these groups is recommended when including them in the vaccination program to eradicate vaccine-preventable diseases. Conversely, we found high vaccination willingness among parents who reported that their family member(s) had either tested positive for or died of COVID-19. The harmful effect of COVID-19 may encourage patients to make a favorable decision about vaccinating their children when the vaccine becomes available.
Strengths and limitations
This is the first study to reveal the rate of parental vaccine hesitancy for children in Bangladesh. This study included parental data from all eight divisions of Bangladesh by randomly selected data collection sites; of the participating parents, 52% were women, 10% Hindu parents, and 1% Buddhist and Christian, providing a good representation of the population. Additionally, we conducted anonymous face-to-face interviews to reduce social desirability bias, minimize non-response, and maximize the quality of collected data. Data from parents of children with disabilities have also increased the generalizability of our findings.
Nevertheless, this study has several limitations. Previous studies have found that vaccine hesitancy is complicated; time and location vary, and adherence-specific matter depends on the perceived behavioral nature of the community. 31 – 33 We conducted this study when the COVID-19 detection rate in the community was significantly lower than the average rate in the country, which may have influenced the perceived threat of the disease and the vaccine hesitancy rate. This study did not measure social and traditional media influences, which may have confounded the results. 34 Lastly, our questionnaire did not include questions specific to attitudes, beliefs, or mistrust about the vaccine.
Conclusions
Our study identified several subgroups of parents who show significantly COVID-19 vaccine hesitancy for their children. To ensure the optimum coverage of vaccines, the government, public health officials, and advocates should be prepared to address parental vaccine hesitancy to reach their target and establish programs to improve childhood COVID-19 vaccine literacy among parents. The rates of willingness are subject to change with the suitability of vaccines; however, the ambivalent effects of vaccines may further reduce those rates. Special strategies should be taken targeting the subgroups of parents with higher vaccine hesitancy in this study. Furthermore, availability of safety and efficacy data for COVID-19 vaccines for children in social and traditional media, community and healthcare centers, and mosques/temples would likely positively impact community members’ attitudes toward childhood COVID-19 vaccination and, thus, may increase vaccination rates in general. Engaging community and religious leaders, family physicians, and trustworthy relatives should accelerate advocacy programs to reduce parental vaccine hesitancy for their children in the community.
Data availability
Underlying data
Open Science Framework: Parental coronavirus disease vaccine hesitancy for children in Bangladesh: a cross-sectional study. https://doi.org/10.17605/OSF.IO/43G5M 35
The project contains the following underlying data:
-
•
Parental Vac Hesitancy F1000.sav (raw data from questionnaires)
Extended data
Open Science Framework: Parental coronavirus disease vaccine hesitancy for children in Bangladesh: a cross-sectional study. https://doi.org/10.17605/OSF.IO/43G5M 35
The project contains the following extended data:
-
•
Parental Vac Questionnaire.docx
Reporting guidelines
Open Science Framework: Parental coronavirus disease vaccine hesitancy for children in Bangladesh: a cross-sectional study. https://doi.org/10.17605/OSF.IO/43G5M 35
This project contains the following reporting guidelines checklist:
-
•
STROBE_checklist_Par_Vac_Hesi.docx
Data are available under the terms of the Creative Commons Attribution 4.0 International license (CC-BY 4.0).
Acknowledgements
The authors would like to thank the participants for providing the information used to conduct the study. Also, the authors would like to thank Zarin Tasnim and Umme Salma Khan for assisting with data collection.
Funding Statement
The author(s) declared that no grants were involved in supporting this work.
[version 2; peer review: 3 approved]
References
- 1. Hodgson SH, Mansatta K, Mallett G, et al. : What defines an efficacious COVID-19 vaccine? A review of the challenges assessing the clinical efficacy of vaccines against SARS-CoV-2. Lancet Infect. Dis. 2021 Feb 1 [cited 2022 Jan 13];21(2):e26–e35. 10.1016/S1473-3099(20)30773-8 Reference Source [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Randolph HE, Barreiro LB: Herd Immunity: Understanding COVID-19. Immunity. 2020 [cited 2021 Oct 28];52:737–741. Cell Press. 10.1016/j.immuni.2020.04.012 Reference Source [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Alfieri NL, Kusma JD, Heard-Garris N, et al. : Parental COVID-19 vaccine hesitancy for children: vulnerability in an urban hotspot. BMC Public Health. 2021 Dec 13 [cited 2021 Oct 28];21(1):1662. 10.1186/s12889-021-11725-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. MacDonald NE: Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015 Aug 14 [cited 2021 Jan 16];33(34):4161–4164. 10.1016/j.vaccine.2015.04.036 Reference Source [DOI] [PubMed] [Google Scholar]
- 5. Cascini F, Pantovic A, Al-Ajlouni Y, et al. : Attitudes, acceptance and hesitancy among the general population worldwide to receive the COVID-19 vaccines and their contributing factors: A systematic review. iScience. 2021 Oct [cited 2021 Oct 29];40:101113. 10.1016/j.eclinm.2021.101113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. World Health Organization: Weekly Operational Update on COVID-19. World Heal Organ;2021; (February):1–10. Reference Source [Google Scholar]
- 7. Kostoff RN, Calina D, Kanduc D, et al. : Why are we vaccinating children against COVID-19?. Toxicol. Rep. 2021 Jan 1;8:1665–1684. 10.1016/j.toxrep.2021.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 8. Bagateli LE, Saeki EY, Fadda M, et al. : COVID-19 Vaccine Hesitancy among Parents of Children and Adolescents Living in Brazil. Vaccine. 2021 Sep 30 [cited 2021 Oct 5];9(10):1115. 10.3390/vaccines9101115 Reference Source [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Zhang M-X, Lin X-Q, Chen Y, et al. : Determinants of parental hesitancy to vaccinate their children against COVID-19 in China. Expert Rev. Vaccines. 2021 Aug 23 [cited 2021 Oct 5];20:1339–1349. 10.1080/14760584.2021.1967147 [DOI] [PubMed] [Google Scholar]
- 10. Ali M, Hossain A: What is the extent of COVID-19 vaccine hesitancy in Bangladesh? A cross-sectional rapid national survey. BMJ Open. 2021 Aug 24 [cited 2021 Aug 24];11(8):e050303. 10.1136/bmjopen-2021-050303 Reference Source [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Jamison AM, Quinn SC, Freimuth VS: “You don’t trust a government vaccine”: Narratives of institutional trust and influenza vaccination among African American and white adults. Soc. Sci. Med. 2019 Jan [cited 2021 Nov 4];221:87–94. 10.1016/j.socscimed.2018.12.020 Reference Source [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kempe A, Saville AW, Albertin C, et al. : Parental Hesitancy About Routine Childhood and Influenza Vaccinations: A National Survey. Pediatrics. 2020 Jul 1 [cited 2021 Nov 4];146(1):e20193852. 10.1542/peds.2019-3852 Reference Source [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hamel L, Lopes L, Kearney A, et al. : KFF COVID-19 vaccine monitor: Parents and the pandemic. KFF. 2021 [cited 2021 Nov 4]. Reference Source [Google Scholar]
- 14. Faria NR, Mellan TA, Whittaker C, et al. : Genomics and epidemiology of the P.1 SARS-CoV-2 lineage in Manaus, Brazil. Science (80-). 2021 May 21 [cited 2021 Nov 4];372(6544):815–821. 10.1126/science.abh2644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mlcochova P, Kemp SA, Dhar MS, et al. : SARS-CoV-2 B.1.617.2 Delta variant replication and immune evasion. Nature. 2021 Nov 4 [cited 2021 Nov 4];599(7883):114–119. 10.1038/s41586-021-03944-y Reference Source [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mathieu Edouard RH: Coronavirus (COVID-19) Vaccinations - Statistics and Research - Our World in Data. Nat. Hum. Behav. 2021 [cited 2021 Nov 4];5–7. Reference Source [Google Scholar]
- 17. United Nations Population Fund: Handbook of Disease Burdens and Quality of Life Measures. New York, NY: Springer New York;2010 [cited 2021 Nov 7];4344–4344. Reference Source [Google Scholar]
- 18. Children 12 and above to get jabs|The Daily Star:[cited 2021 Nov 7]. Reference Source
- 19. Taherdoost H: Determining sample size; How to calculate survey sample size. Int J Econ Manag Syst. 2017;2(2):237–239. Reference Source [Google Scholar]
- 20. James E, Joe W, Chadwick C: Organizational research: Determining appropriate sample size in survey research. Inf. Technol. Learn. Perform. J. 2001;19(1):43–50. [Google Scholar]
- 21. Szilagyi PG, Shah MD, Delgado JR, et al. : Parents’ Intentions and Perceptions About COVID-19 Vaccination for Their Children: Results From a National Survey. Pediatrics. 2021 Oct;148(4):e2021052335. 10.1542/peds.2021-052335 Reference Source [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Aldakhil H, Albedah N, Alturaiki N, et al. : Vaccine hesitancy towards childhood immunizations as a predictor of mothers’ intention to vaccinate their children against COVID-19 in Saudi Arabia. J. Infect. Public Health. 2021 Oct 1 [cited 2021 Nov 6];14(10):1497–1504. 10.1016/j.jiph.2021.08.028 Reference Source [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Mohd Azizi FS, Kew Y, Moy FM: Vaccine hesitancy among parents in a multi-ethnic country, Malaysia. Vaccine. 2017 May 19 [cited 2021 Oct 6];35(22):2955–2961. 10.1016/j.vaccine.2017.04.010 Reference Source [DOI] [PubMed] [Google Scholar]
- 24. Caserotti M, Girardi P, Rubaltelli E, et al. : Associations of COVID-19 risk perception with vaccine hesitancy over time for Italian residents. Soc. Sci. Med. 2021 Mar 1 [cited 2021 Jun 17];272:113688. 10.1016/j.socscimed.2021.113688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kucukkarapinar M, Karadag F, Budakoglu I, et al. : COVID-19 Vaccine Hesitancy and Its Relationship With Illness Risk Perceptions, Affect, Worry, and Public Trust: An Online Serial Cross-Sectional Survey From Turkey. Psychiatry Clin Psychopharmacol. 2021 Apr 12;31(1):98–109. 10.5152/pcp.2021.21017 Reference Source [DOI] [Google Scholar]
- 26. Bertin P, Nera K, Delouvée S: Conspiracy Beliefs, Rejection of Vaccination, and Support for hydroxychloroquine: A Conceptual Replication-Extension in the COVID-19 Pandemic Context. Front. Psychol. 2020 Sep 18; 0:2471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Teasdale CA, Borrell LN, Shen Y, et al. : Parental plans to vaccinate children for COVID-19 in New York city. Vaccine. 2021 Aug;39(36):5082–5086. 10.1016/j.vaccine.2021.07.058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Lazarus JV, Ratzan SC, Palayew A, et al. : A global survey of potential acceptance of a COVID-19 vaccine. Nat. Med. 2020 Oct 20 [cited 2021 Jan 16];27:225–228. 10.1038/s41591-020-1124-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Al-Mohaithef M, Padhi BK: Determinants of COVID-19 Vaccine Acceptance in Saudi Arabia: A Web-Based National Survey. J. Multidiscip. Healthc. 2020 Nov 20 [cited 2021 Feb 5];13:1657–1663. 10.2147/JMDH.S276771 Reference Source [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Malik AA, McFadden SM, Elharake J, et al. : Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine. 2020 Sep [cited 2021 Jan 14];26:100495. 10.1016/j.eclinm.2020.100495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Xiao X, Wong RM: Vaccine hesitancy and perceived behavioral control: A meta-analysis. Vaccine. 2020 Jul 14 [cited 2021 Feb 5];38(33):5131–5138. 10.1016/j.vaccine.2020.04.076 Reference Source [DOI] [PubMed] [Google Scholar]
- 32. Larson HJ, Jarrett C, Eckersberger E, et al. : Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: A systematic review of published literature, 2007-2012. Vaccine. 2014;32:2150–2159. Elsevier BV. 10.1016/j.vaccine.2014.01.081 [DOI] [PubMed] [Google Scholar]
- 33. Wilson K, Nguyen HH, Brehaut H: Acceptance of a pandemic influenza vaccine: a systematic review of surveys of the general public. Infect Drug Resist. 2011 Oct 20 [cited 2021 Feb 5];4(1):197. 10.2147/IDR.S23174 Reference Source [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Reno C, Maietti E, Di Valerio Z, et al. : Vaccine Hesitancy towards COVID-19 Vaccination: Investigating the Role of Information Sources through a Mediation Analysis. Infect Dis Rep. 2021 Aug 12 [cited 2021 Nov 7];13(3):712–723. 10.3390/idr13030066 Reference Source [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Ali M: Parental Coronavirus Disease Vaccine Hesitancy for Children in Bangladesh: A Cross-sectional Study. OSF. 2022 January 14. 10.17605/OSF.IO/43G5M [DOI] [PMC free article] [PubMed] [Google Scholar]