Abstract
Introduction: Photobiomodulation or low-level laser therapy (LLLT;<0.5 W) has been used as a non-invasive treatment for various medical indications. Short (visible; 635-650 nm) and longer (invisible; 810-850 nm and 915-980 nm) near-infrared wavelengths have been commonly used, but power setting deficiencies or incorrect wavelength settings can cause negative outcomes. The 1064 nm wavelength as the longest wavelength is a relative newcomer in high-powered (>0.5 W) laser photobiomodulation therapy (HPL-PBMT) with unique biophysical characteristics.
Methods: A comprehensive search of 2016-2021 PubMed, Google Scholar, and Cochrane databases for "photobiomodulation" restricted to clinical trials for patients with a medical diagnosis was done. "1064 nm" content was identified and restricted to high-powered lasers (>0.5 watt). Cohen’s d was calculated for the effect size and the difference was determined as a measure of relative 1064 nm HPL-PBMT efficacy.
Results: The 22 independent studies meeting inclusion criteria focused on knee arthropathies, spine, shoulder/elbow, wound, gynecological, or osteoporosis with evaluation of pain, function, quality of life, range of motion (ROM), and anatomy. Pain was reduced with statistical significance (P<0.05) in 90% of study assessments (n=20) and 100% of studies focused on the knee (n=6). Of 18 studies assessing functional outcome measures, 100% demonstrated statistically significant improvements. Follow-up assessments up to 6 months in 5 knee arthritis studies revealed long-term pain reduction after cessation of treatment. Improvements in wound healing, bone mineral density, and knee cartilage thickness were demonstrated. The largest effect sizes observed were pain reduction in knee arthritis (average Cohen’s d effect size=2.46).
Conclusion: These studies have established that 1064 nm HPL-PBMT can effectively reduce pain, increase ROM, increase functional scores, and increase the quality of life for knee osteoarthritis and spinal disorders, with limitations. More studies are needed for clinical validation of single-trial data detecting changes in musculoskeletal conditions, cartilage thickness and bone density.
Keywords: Photobiomodulation, Musculoskeletal, Pain, Knee, Arthritis, Transcranial
Introduction
Clinical trial studies evaluating the effectiveness of low-level (LLLT) laser photobiomodulation therapy (PBMT) have yielded inconsistent outcomes due to differences in laser parameter settings involving variable power levels, wavelength selection, light coherence, operation modes (pulsed versus continuous), beam sizes, and dosage depending on indications and specific patient populations.1 However, over the past 5 years, significant advances have been made, clarifying our understanding of which factors are most important for achieving reproducibly effective therapeutic outcomes.2-6
Positive therapeutic outcomes can be dependent on the ability of laser light to penetrate and ultimately reach pathological tissues.7-10 As light transmits through tissue, it is lost by three processes: reflection, scattering, and absorption of light by water, melanin, or other chromophores. The depth of laser light penetration is dependent on the adjustable laser setting parameters of power density and wavelength.5 Multiple randomized controlled trials that directly compare low-power (< 0.5 W) and high-power (> 0.5 W)laser therapy have proven that high power can be required for efficacy.7-10 The highest power settings that can generate heat may need to be modified, depending on the condition being treated and the response of the patient. The upper limit of high-power laser settings to the patient can be modified in a number of ways, including faster movement of the treatment headpiece, administering therapy in pulsed light modes, using appropriate wavelength selection, and administration of specific cold or cryotherapy prior to laser therapy treatment.
Heat can be generated when light is absorbed by water or chromophores such as melanin - the predominant chromophore in skin. At the extreme, the high relative absorption by water, as with a carbon dioxide laser, which uses a light wavelength of 10 600 nm, results in flash boiling with tissue ablation, which is useful for surgical purposes. For photobiomodulation purposes, it is more desirable to consider wavelengths with characteristic minimal absorption of water and/or melanin, so there are both a reduction in heat generation and a greater depth of penetration at the high-power settings needed to reach deep tissue pathologies.5,11-13 The 810-830 nm wavelength has the lowest absorption of water of commonly used PBMT wavelengths14 (Figure S1,15,16Supplementary file 1).
Depth of Penetration
Along the path of light from the source to the target pathologic tissue, there is at first higher absorption by melanin pigments in the skin, which is subtracted from deep tissue photobiomodulation delivery. Melanin represents a group of pigments in the skin that absorbs and reflects light and may be the most significant initial barrier to consider with respect to the depth of tissue photobiomodulation. Depending on the wavelength used, the upfront heat generated from absorption by melanin may be a dominant factor limiting the upper maximal limit of tolerable power intensity, particularly in darker pigmented individuals. The 1064 nm wavelength is distinguished as the longest wavelength that is routinely used.17 Eumelanin is the predominant melanin, and most significantly, 830 nm light is absorbed by eumelanin, but 1064 nm light is not.5 Accordingly, the initial melanin-generated heat produced with typical PBMT is no longer a concern with 1064 nm.
Sharma et al performed a comparative wavelength study of utility in photoacoustic imaging analysis, a rapidly emerging field of expanding utility that relies on the conversion of light energy to sound energy as first discovered by Alexander Graham Bell.18 The depth of penetration studies determined that the greatest depths of penetration were achieved by the 1064 nm laser with maximum permissible power settings as compared to 532 nm or 800 nm.3
Basic research by Marshall and Vlkova compared the depth of penetration for commonly used PBMT wavelengths.5 First, they performed a literature-based analysis of reflection, refractive indices (scattering), absorption by water, and absorption by melanin with respect to commonly used wavelengths in PBMT. The researchers pointed out that the refraction index is 3x less for 1064 nm (1.5 cm -1) light than for 810 nm (4.6 cm -1) light and that general reflection, scattering, and absorption by melanin for wavelengths above 1000 nm are uniformly lower, while the 810 nm wavelength is the least absorbed by water. In subsequent experiments, investigators measured the depth of penetration through agarose-based tissue-mimicking media.19 Significantly, at high powers, the investigators determined that the relative energy detectable at 6.2 mm depths was the highest for 1064 nm (47%), followed by simultaneous 810 nm with 970 nm irradiation (37%), and lastly 810 nm (26%).5 The investigators concluded that wavelengths above 1000 nm have negligible absorption and reflection by melanin and that the 1064 nm wavelength has deeper penetration than 810 nm and 970 nm.
Meta-analysis
Understanding the clinical biophysics of 1064 nm HPL-PBMT is complicated, but ultimately what matters the most is to determine the optimal laser settings that provide the best clinical outcomes for specific indications. Towards this end, we performed a meta-analysis of all published clinical trials using high-powered 1064 nm wavelength-emitting lasers that was limited to published studies reported within the past 5 years of clinical trials.
Methods
Search for Evidence and Article Selection
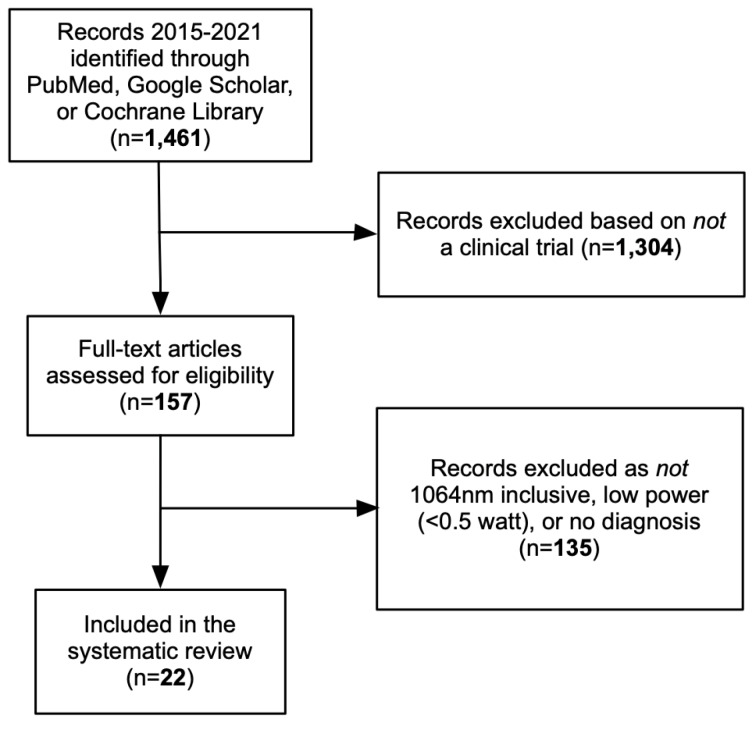
This study conforms to all PRISMA guidelines and reports the required information accordingly. We performed a systematic review of the best evidence using Cochrane guidelines. Our structured question for this review was as follows in Figure 1. We searched the most important and appropriate electronic medical databases including PubMed, Cochrane library, and Google Scholar. We searched for the word “photobiomodulation” restricted to the years 2016-2021. The articles that were deemed to be irrelevant to the research objectives were excluded. After collecting the full texts of articles which were related to the objectives of this study, the references of these articles were reviewed. The related references were identified, and their full texts were reviewed.
Figure 1.
Search Results and Article Selection.
Inclusion and Exclusion Criteria
The inclusion criteria were (1) clinical trials, (2) use of high-powered lasers with power settings > 0.5 W, (3) patients with a medical diagnosis, (4) comparison of high-powered lasers versus LLLT or placebo lasers or common backgrounds, and (5) use of outcome measures such as pain, range of motion (ROM), quality of life, cartilage thickness, disability indices, bone density, or gait. The exclusion criteria included (1) fundamental research or studies on animals, (2) controlled trials involving patients without a medical diagnosis, (3) review articles, (4) articles which did not have related statistical and clinical data.
Statistical Analysis
The significance level was set at P < 0.05. A statistical method was designed to measure the effect size specifically attributable to 1064 nm HPL-PBMT as compared to a common background. Cohen’s d formula was used for the calculation of the effect size (ES).20,21 The standardized mean of group assessments made before and after treatment was divided by the pooled standard deviation.
The difference of effect sizes between two separate groups (± 1064 nm HPL-PBMT) was calculated via the subtraction of the ES for each group as a metric for determining the relative efficacy specifically attributable to 1064 nm HPL-PBMT.9
Difference in effect size = ES 1 – ES 2
Interpretation was based on the values established by Cohen: small effect ≤ 0.2, medium effect 0.2-0.8, and large effect > 0.8.20
Results
The 22 studies meeting the criteria to be included in this meta-analysis have evaluated a variety of outcome measures including changes in pain, function, quality of life, ROM, and strength as well as anatomical structures (Table 1; see online Supplementary file 2, Table S1). Seven of the studies were double-blinded controlled trials.22-28 Thirteen of the studies were single-blinded controlled trials involving blinding either the practitioner or the assessor.8,29-40 No adverse events were reported in any studies except for one study involving patients diagnosed with hemophilic arthropathy, in which one patient experienced paresthesia at the application site and three others had nondescript adverse events, none of which were serious.
Table 1. Clinical Trial Studies Selected for Meta-analysis of 1064 nm Wavelength PBMT .
| Categorical |
Diagnosis
Reference |
Groups | 1064 nm Laser Session | Treatment & Follow-up | PEDroScore a | Outcome |
|---|---|---|---|---|---|---|
| Knee | Knee osteoarthritis 3307439326; 2020 |
laser + ET n = 20 sham laser + ET n = 20 (double-blinded) |
Analgesic: 12 W, 12 J/cm2 25 Hz for 300 J Biomodulatory: 12 W, 120 J/cm2for 3000 J |
Treatment: 5 x/wk 2 wk Follow-up: EOT, 6 wk |
7* | Pain reduced (VAS & WOMAC) ROM increased Femoral cartilage thickness increased |
| Knee osteoarthritis 3017843237; 2019 |
laser n = 30 ET n = 30 CPT n = 30 (single-blinded) |
5W, 30Hz, 70% duty, 60 J/cm2, 2400 J | Treatment: 3x/wk 12 wk Follow-up: EOT, 12 wk |
6* | Pain reduced Stiffness in knee reduced (WOMAC stiffness) ROM increased |
|
| Juvenile rheumatoid arthritis 3001619328; 2018 |
laser + ET n = 15 sham laser + ET n = 15 (double-blinded) |
3 kW peak power, 10.5 W average, 120-150 µs, 20-30Hz, 10 J/cm2, 60 cm2 spot size, 15J per point to 10 points, 1500 J total 8 m/session |
Treatment: 3x/wk 4wk Follow-up: EOT, 12wk |
5* | Pain reduced Gate improved (GAITrite) |
|
| Hemophilic arthropathy 2797659135; 2018 |
laser + PT n = 15 sham laser + PT n = 15 (single-blinded) |
Power level not described, 610 mJ/cm2, 750 J/knee total to both knees 8m/session |
Treatment: 3/wk 12 wk Follow-up: EOT |
6* | Pain reduced Gait improved |
|
| Knee Osteoarthritis 2807850336; 2017 |
laser + GCS + ET n = 23 GCS + ET n = 22 ET n = 22 (single-blinded) |
3 kW peak power, 10.5 W average, 510–1780 mJ/cm2, < 120 μs, 10-30 Hz, 0.2cm2 spot size, 3000 J total 7 m/session |
Treatment: 2x/wk 6wk Follow-up: EOT, 3 mon |
6* | Pain reduced (WOMAC) Synovial thickness reduced |
|
| Knee osteoarthritis 2809671134; 2016 |
laser n = 37 sham laser n = 35 (single-blinded) |
3x analgesic sessions: 12 W, 12 J/cm2, 300 J, 25 cm2 treatment area 2 m, 25 Hz 4x bio stimulatory sessions: 12 W, 120 J/cm2, 3000 J, 25 cm2 treatment area, 10 m |
Treatment: 7d Follow-up: EOT, 1mo, 3mos |
5 | Pain reduced (& dolorimetry) | |
| Spine | Non-specific lower back pain 3117830644; 2020 |
laser n = 20 LLLT n = 20 control n = 20 (single-blinded) |
Laser: 12 W, 150 J/cm2, 1 cm2 diameter, 1200 J total, 15 m/session LLLT: 850 nm, 800 mW, 1cm spot, 1 kHz, 80% duty, average of 50 J/cm2, 1200 J total 30 m/session |
Treatments: Laser: 2x/wk 12wk LLLT: 2x/wk 12wk Follow-up: EOT |
6* | Pain reduced Disability reduced Lumbar mobility improved ROM increased QoL improved |
| Cervical disc herniation 3214703732; 2019 |
laser + ET n = 20 ultrasound + TENS + ET n = 20 (single-blinded) |
3 kW peak power, 10-40 Hz, 360-1780 mJ/cm2, 120-150 μs, 5 mm diameter analgesic phase at 8 W, 5 J/cm2, 25 Hz, 1850 J total 15 m/session |
Treatment: 5x/wk 4 wk Follow-up: EOT |
5* | Pain reduced QoL improved ROM increased |
|
| Cervical spondylosis 344388332; 2019 |
laser + ET n = 42 ultrasound + TENS + ET n = 42 (single-blinded) |
3 kW peak power, 120-150 μs, 10-40 Hz, 510-1780 mJ/cm2, 5 mm spot, 2050 J total 30 m/session |
Treatment: 2x/wk 12 wk Follow-up: 4 wk |
4* | Pain reduced ROM increased Disability reduced (laser the most effective) |
|
| Lower lumbar disc degeneration 3017441840; 2018 |
laser n = 18 sham laser n = 17 LLLT n = 16 sham LLLT n = 17 (single-blinded) |
Laser: 10 W, 60 J/cm2, 1200 J total, 10 m/session LLLT: 65 mW, 785 nm, 8 J/cm2, 8 m/session |
Treatment: 5x/wk 3wks Follow-up: EOT, 1 mon, 3 mon |
8 | No benefits by VAS scores, disability indices, or questionnaires | |
| Lumbar disc protrusion 2885450045; 2018 |
laser + spinal decompression n = 32 spinal decompression n = 31 |
12 W, 150 J/cm2, 1 cm spot, 7500 J total: fast manual scanning 3000 J, then 15000 J, then slow manual scanning 3000 J 10 m/session |
Treatment: 5x/wk 2 wk Follow-up: EOT, 4 wk |
6 | Pain reduced ROM increased |
|
| Chronic neck pain 2691468429; 2016 |
laser + ET n = 30 placebo + ET n = 30 (double-blinded) |
3 kW peak power, 510-1780 mJ/cm, 120-150 μs, 10-40 Hz, 0.5 cm diameter, and 0.2 cm2 spot size, 2250 J total over 3 phases (see manuscript), 75 cm2 treated area 15 m/session |
Treatment: 2x/wk 6wk Follow-up: EOT |
4* | Disability reduced ROM increased |
|
| Shoulder Arm |
Subacromial Impingement Syndrome 33400001224; 2021 |
laser + exercise n = 32 sham laser + exercise n = 31 (double-blinded) |
3 kW peak power, 360-1780 mJ/cm2, 40 Hz, 2781 J total 25 m/session |
Treatment: 5x/wk 3wk Follow-up: EOT, 12 wk |
8 | Pain reduced ROM increased Strength increased Daily activity increased |
| Subacromial impingement Syndrome 2722057739; 2016 |
laser + MT + KT + EX n = 19 ET n = 15 KT +EX n = 20 MT + KT + EX n = 16 (single-blinded) |
3 kW peak power; 5 mm spot diameter; 3 s phases: fast manual scanning 100cm2/30s of the zones of muscular contracture, particularly trapezius, supraspinatus, and deltoid during shoulder abduction, for 1000 J/cm2, 2nd phase 50 J to each of 4 trigger points; final phase with slow manual scanning 100 cm2/60 s to same first phase areas for 1000 J total - 510, 610, and 710 mJ/cm2 for a total of 2050 J. 30 m/session. |
Treatment: 3x/15d Follow-up: EOT |
6* | Pain reduced (SPALDI) Disability reduced ROM increased |
|
| Lateral epicondylitis 2990093838; 2016 |
laser n = 31 bandage n = 34 (single-blinded) |
75 s at 4 W for 6 J/cm2 Analgesic: targeting painful areas 4 sessions. Biostimulatory: 6x sessions 6 W 100-150 J/cm2 12 m/session |
Treatment: 5x/wk 2wk Follow-up: 6 wk |
5* | Pain reduced, disability reduced, hand strength increased, and QoL improved | |
| Foot | Calcaneal spur 3147809525; 2020 |
laser + ET n = 21 sham laser + ET n = 21 (double-blinded) |
3 kW peak power, 360–1780 mJ/cm2, 150 μs, 10.5 W average power, 10-40 Hz, 0.2 cm2 spot size, 1281 J total, 10 m/session | Treatment: 5x/wk 3 wk Follow-up: 4 wk, 12 wk |
7* | Improved pedographic measures |
| Plantar fasciitis 3251301843; 2020 |
laser n = 51 LLLT n = 51 (single-blinded) |
laser: 12 W, 120 J/cm2, 3000 J total, 25 cm2 spot, 7m/session LLLT; 785 nm, 50 mW, 50-60 Hz, 4 J/cm2, 140 J total, 35 cm2 spot, 7 m/session |
Treatment: 3x/wk 8x 3wk Follow-up: EOT, 4 wk |
8* | No statistical difference in pain Laser more effective than LLLT in the opinion of participants |
|
| Plantar fasciitis 2962788831; 2018 |
laser n = 35 LLLT n = 35 (single-blinded) |
laser: 3x analgesic: 8 W, 75s, 6J/cm2, 150 J total; 6x bio-stimulation: 30s, 6 W, 150 J/cm2 dose LLLT: 904 nm, 240 mW, 5000 Hz, 0.16 W/cm2, 160 s per session, 680 J total |
Treatment: 3x/wk 3 wk Follow-up: EOT |
8* | Pain reduced (VAS) Function improved QoL improved (laser all more than LLLT) |
|
| Wound | Caesarian healing in diabetic women 2970670846; 2018 |
laser n = 20 sham laser n = 20 |
10.5 W, 0.5-1.8 J/cm2, 10-40 Hz, 150 μs pulses 10–40 Hz, 150 J first phase, then 1 cm away from wound 20 J per each of 12 points, last phase, same as first, but slow scanning | Treatment: 3x/wk 6 wk Follow-up: EOT |
5* | Wound appearance improved |
| Post-burn pruritus 2823307130; 2017 |
laser n = 25 sham laser n = 24 (double-blinded) |
3k W peak power, 0.5-1.8 J/cm2, 150 μs pulses 10–40 Hz, 0.2 cm2spot size, 3000 J | Treatment: 3/wk 6 wk Follow-up: EOT, 12 wk |
10 | Itch severity reduced QoL improved Pain reduced (VAS) |
|
| Gynecological | Primary dysmenorrhea 2918428127; 2017 |
laser n = 26 PEMF n = 26 (double-blinded) |
3 kW peak power, 810-1780 mJ/cm2, 150 μs, 10–40 Hz, 880 J total 15m/session |
3 treatments per cycle for 3 cycles (3 mon) Follow-up: EOT |
4* | Pain reduced Prostaglandins reduced |
| Bone | Osteoporosis & osteopenia by DEXA scan 2906875642; 2018 |
laser + ET n = 25 sham laser + exercise n = 25 laser only n = 25 placebo n = 25 (single-blinded) |
10.5 W, 510-1780 mJ/cm2, 150µs pulses 10-30 Hz, spot size 0.2 cm2, 3,000J delivered 2x phases: fast scanning at 510, 610, and 710 mJ/cm2 for 1500 J, then slow scanning 18 m/session |
Treatment: 3x/wk 24 wk Follow-up: EOT, 1 y |
Z* | Lumbar bone mineral density improved |
aDatabase retrieved and confirmed PEDro scores based on 10-point scale. ROM-range of motion.
In all of these studies except one, statistically significant improvements were observed in one or more of these areas when comparing baseline measures to data collected at the end of treatment, with the probability value set at the standard P < 0.05. Twenty of the studies used pain as one of the outcome measures, with 19 studies using the visual analog scale (VAS) and one using the Present Pain Intensity Scale. 18 studies showed a statistically significant decrease in pain when comparing the baseline and after-treatment measures within the 1064 nm HPL-PBMT groups. Fourteen of those twenty studies also showed a statistically significant difference when they were compared (1064 nm HPL-PBMT vs control).
From those 20 studies, 13 examined long-term effects, lasting from 4 to 12 weeks after treatment. In 9 of those 13 studies, data showed that the statistically significant decreases in pain measures were still present in the 1064 nm HPL-PBMT groups. Similar data are found in a majority of the studies when considering other outcome measures. A considerable number of studies focused on the knee and spinal cord (6 each, 12 total), while 3 studies focused on the foot and 3 on the shoulder/arm for 18 controlled trial studies. The four remaining studies did not focus on musculoskeletal disorders: two wounds, one bone, and one primary dysmenorrhea. The greatest categorically favorable pain reduction responses were observed with the treatment of knee pathologies (see online Supplementary file 2, Table S1). One 2020 knee osteoarthritis study included measures of changes in knee cartilage from 3 different ultrasound aspects at 6 weeks after the cessation of treatment.24 High-powered 1064 nm PBMT caused a medium-to-large effect size when looking at changes in cartilage thickness from all three aspects, given that Cohen’s |d| < 0.2 = small effect, 0.2 < |d| < 0.8 = medium effect, and |d| > 0.8 = large effect.20
ROM consistently increased in all 9 studies after treatment with 1064 nm HPL-PBMT. These included two studies focused on knee arthritis,24,34 five on various spinal diagnoses (lower back pain,38 herniation,30 cervical spondylosis,29 neck pain,27 lumbar disc protrusion41), and two on shoulder/arm-related subacromial impingement syndrome.22,36
Additional promising results showed significant improvement in various functional measures. The studies that did employ one or more measures of function used such scales as the European Quality of Life Survey (EuroQoL), the Oswestry Disability Index (ODI), the Neck Disability Index (NDI), the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), the Quality of Life - Short Form 36 (SF-36) and the GAITRite System, among others. The various scales and indices were found to be valid and reliable in all studies. Some of the scales take into account various aspects of general functioning such as mobility, self-care skills, common daily activities, pain, anxiety, and social functioning. The ODI and NDI look at functional disability levels related to pain, whereas the WOMAC looks at not only functional activities, such as using stairs, rising from sitting, standing, bending, walking, getting into and out of a car, and putting on and taking off socks, but also pain and stiffness. The GAITRite looks at functional gait parameters in an objective, quantifiable way. Of the 22 studies in this meta-analysis, 18 used some sort of functional outcome measure at baseline, at the end of treatment, and at long-term follow-up, which included 12 of the studies. All 18 studies showed statistically significant improvement in the various functional measures utilized when comparing baseline values to values at the end of treatment within HPL-PBMT groups, and the 12 studies with long-term follow-up continued to exhibit statistically significant improvement in function within the 1064 nm HPL-PBMT groups. When comparing results between 1064 nm HPL-PBMT and control groups, the positive trends continued for the most part. Of the 18 studies using a functional outcome measure, the 1064 nm HPL-PBMT groups showed statistically significant improvement in function when compared to the control groups in 15 of those studies. Ten out of the 12 studies that looked at long-term follow-up found those differences continued with the 1064 nm HPL-PBMT groups outperforming the control groups.
The three studies comparing high-powered 1064 nm to lower-powered PBMT indicated that PBMT of a higher power was required to achieve effectiveness. In one trial involving patients with plantar fasciitis (PF), those treated with 1064 nm high-powered PBMT exhibited better outcomes than those treated with low-powered PBMT.8,40 Another study involving PF patients did not result in any improvements after high- or low-powered PBMT.40 The PF studies may be limited by the ability to identify the target site to aim at the laser given that PF pain has the potential to be referred to as neuronal pain.42 The third study comparing high-powered 1064 nm PBMT to low-powered PBMT showed benefits for both approaches in the treatment of chronic lower back pain.38
Assessments performed after the cessation of treatment helped determine whether the benefits were sustaining and not merely transient effects. Fourteen studies performed follow-up assessments ranging from 1 to 12 months. All five studies focused on knee arthritis demonstrated a sustained reduction in pain with a large effect, and follow-ups were performed for 6 weeks to 3 mos.24,26,31,33,34 One knee arthritis study detected increased knee cartilage thickness with a large effect detectable 6 weeks after the cessation of treatment that was initially performed for 3 weeks.24 Three spine-related diagnoses had follow-up assessments.29,37,41 A large positive effect was observed for the treatment of cervical spondylosis or lumbar disc protrusion, both 1 month after the cessation of treatment, while no significant benefit was observed for the treatment of lower lumbar disc degeneration. No sustained benefit was observed with foot-related treatments, calcaneal spur or PF after follow-up.
Discussion
Our systematic meta-analysis method is largely based on, supported by, and confirmed by a previous meta-analysis that focused on the beneficial effects of high-powered laser photobiomodulation therapy on musculoskeletal pain.9 In the previous analysis, investigators concluded that HPL-PBMT can be an effective approach to pain management. We also reached this conclusion and extended these studies further by including newer publications and focusing primarily on the determination of the range and extent of any indications that responded favorably to treatments using specifically the 1064 nm wavelength of HPL-PBMT.
Of all anatomical musculoskeletal categories, the largest amount of data obtained in our study involved the knee (6 studies). Reductions in pain, increases in ROM, and increased functionality were consistently observed. The data conclusively support that HPL-PBMT with 1064 nm treatment can be highly efficacious in the reduction of pain in knee arthritis with the potential for increasing ROM, quality of life, and even cartilage growth.
The two trials which assessed cartilage thickness after 1064 nm HPL-PBMT were particularly impressive since there are few, if any, known treatments that have been able to demonstrably increase knee cartilage thickness.24,33 One trial did not detect significant changes in cartilage thickness after performing treatments twice per week for 6 weeks; however, another trial that involved more frequent daily treatments for just 2 weeks resulted in significantly detectable increases in cartilage thickness, which was detectable even 6 weeks after the cessation of treatment. More studies are needed to determine the extent to which high-powered PBMT is capable of increasing joint cartilage thickness.
The large effect size seen repeatedly when treating knee anatomies may be in part due to the shorter depth of light penetration that is required to reach pathologic tissues in the knee. By contrast, anatomies with greater potential for referred nerve pain, including PF and spinal diagnoses analyzed within this study, appear to be more challenging to treat based on our analysis of the effect size and under the particular 1064 nm HPL-PBMT treatment settings that were used. Lumbar discs are chronically weightbearing and no therapeutic benefit was seen after the treatment of lumbar disc degenerative disease.37
Importantly, the improved outcome results observed months after the cessation of treatment in multiple studies with large effect sizes indicate that 1064 nm HPL-PBMT can effectively stimulate healing beyond merely providing transient symptomatic relief. Treatment reduced pain in knee (5 studies), spine (2), and shoulder/arm (1) studies and also stimulated increases in knee cartilage thickness, improved quality of life, and improved functional outcomes in assessments performed for times ranging from 6 weeks to 3 months after the end of treatment.
This meta-analysis also confirms that 1064 nm HPL-PBMT is also highly effective in promoting wound healing.28,43 Significantly, wound healing is distinguished as one of the simplest and unequivocal measurable PBMT outcomes. Similar to wound healing, the effectiveness of treating oral mucositis with PBMT is indisputable, with easily measurable outcomes and unequivocally positive results. Oral mucositis routinely occurs in patients undergoing hematopoietic stem cell transplantation or radiotherapy ± chemotherapy and can cause extensive pain and suffering. Photobiomodulation has proven to be an effective drug-free treatment for cancer patients undergoing the standard of care treatments.44
Owing in part to the clearly positive and reproducible therapeutic results of PBMT, the prevention or treatment of oral mucositis with PBMT is now the most universally accepted, recognized, and established guideline-directed PBMT-utilizing approach in photomedicine and is commonly covered by insurers.45,46 Effective oral mucositis photobiomodulation is routinely performed with low-level light ≤ 100 mW because a negligible depth of tissue penetration is required to reach the targeted superficial highly-regenerating and circulating cells of the oral cavity.
By contrast, higher laser power settings are required to reach deeper tissue pathologies, and therefore, the outcome measures for the treatment of musculoskeletal disorders may not be as clear as those observed with overt oral mucositis outcomes. Studies examining low-powered PBMT have commonly led to inconsistent or negative outcomes when indications involve deeper tissue pathologies that absolutely require higher-powered lasers for the light to reach the target pathological tissues. This has an adverse effect on the field of medical PBMT and threatens to cause medical researchers to miss the identification of indications that are in fact highly responsive to the administration of high-powered photobiomodulation.
Safety Profile
In the twenty-two studies examined, 1064 nm HPL-PBMT caused no serious adverse events, and no significantly negative effects were observed across all outcome measures (Table S1). It is also impressive that there were no significantly negative effects observed after all of our measures, which is consistent with previous early analysis examining musculoskeletal pain.9 This demonstrates and supports the exceptional safety profile of high-powered photobiomodulation as a therapeutic approach.
Onychomycosis or tinea unguium – a fungal infection of the toenail
There was one 1064 nm HPL-PBMT study of note that did fulfill the criteria for inclusion in our meta-analysis, but that described the successful treatment of localized infectious disease. Onychomycosis is a common fungal toenail infection that can progress to an inability to walk or stand without disabling pain. Researchers reported that 1064 nm HPL-PBMT cured 11% of 56 patients with onychomycosis as compared to 21% cured when anti-fungal was used in combination with topical antifungal medication.47 The study did not meet the selection criteria for inclusion in our meta-analysis because it was an uncontrolled retrospective study. Nonetheless, the results support that more clinical trials are justified for consideration of the use of HPL-PBMT as a therapeutic approach, especially in the treatment of anatomically localized disease. Weber et al. pointed out that the approach is likely to be most useful for treating patients that are unable to tolerate systemic antifungals.
Treatment Sites
One possible limitation of deep tissue HPL-PBMT studies is the challenge of properly aiming the laser given the potential for nerve-referred pain that is actually caused by distal pathologies. Missing the target pathology may be less likely to happen for the contained anatomy of the knee or toe (onychomycosis), so this may be part of the reason that knee outcomes are so universally positive in this analysis. By contrast, the less reproducibly positive outcomes observed involving the spine or PF foot pain may be improved with an appropriate aiming laser by the hands of a skilled and knowledgeable practitioner.
Multiple Applications
Our meta-analysis concludes that all three diagnoses listed in Table 2 can be effectively treated with high-powered 1064 nm PBMT to provide therapeutic benefits: knee arthritis, wound healing, and spinal disorders. High-powered 1064 nm PBMT had a large positive effect on all three conditions after follow-up assessment (Table 2). Treatment of chronic neck pain and non-specific lower back pain also resulted in a large reduction in pain, but assessment in these studies was limited because the assessment was only done at the end of treatment. Based on the analysis, the data predict that all of these spinal disorders can benefit from high-powered 1064 nm HPL-PBMT, but more clinical validation is needed to achieve recognition and acceptance by third party payors.
Table 2. Most Responsive Indications Limited to Studies With a Follow-up (Not Just End of Trial Assessment) and Prioritized From Top to Bottom Based on the Largest to Smallest Cohen’s d Effect Size .
Conclusion
Our meta-analysis strongly supports that 1064 nm HPL-PBMT is a safe, tolerable, effective, and long-lasting therapeutic approach for the management of musculoskeletal pain. A specific application for the knee stood out with PBMT being extremely effective. Further clinical trials using high-power 1064 nm PBMT settings with continuous mode or pulse settings are needed to provide greater clinical validation of beneficially responsive non-superficial deeper tissue indications to achieve greater consensus and improved outcomes.
Ethical Considerations
Not applicable.
Conflict of Interests
CEV is the CEO of Aspen Laser with patent and pending patents.
Funding
WTP was supported by compensation from Aspen Laser, LLC.
Acknowledgements
We thank and gratefully acknowledge Thomas A. Hertel, MSPT, for critical reading and analysis of the manuscript. We would like to thank Mazlum Serdar Akaltun for sharing all mean and SD data measures of changes in pain, cartilage thickness, and functionality scores.24
Supplementary Materials
Supplementary file 1 contain Figure S1.
Supplementary file 2 contain Table S1.
Please cite this article as follows: Penberthy WT, Vorwaller CE. Utilization of the 1064 nm wavelength in photobiomodulation: a systematic review and meta-analysis. J Lasers Med Sci. 2021;12:e86. doi:10.34172/jlms.2021.86.
References
- 1.Dompe C, Moncrieff L, Matys J, Grzech-Les ´niak, K K, Kocherova I, Bryja A. et al. Photobiomodulation-Underlying Mechanism and Clinical Applications. J Clin Med. 2020;9(6):1724. doi: 10.3390/jcm9061724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Salehpour F, Majdi A, Pazhuhi M, Ghasemi F, Khademi M, Pashazadeh F. et al. Transcranial Photobiomodulation Improves Cognitive Performance in Young Healthy Adults: A Systematic Review and Meta-Analysis. Photobiomodul Photomed Laser Surg. 2019;37(10):635–643. doi: 10.1089/photob.2019.4673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sharma AS, Srishti Srishti, Periyasamy V, Pramanik M. Photoacoustic imaging depth comparison at 532-, 800-, and 1064- nm wavelengths: Monte Carlo simulation and experimental validation. J Biomed Optics. 2019;24(12):121904. doi: 10.1117/1.JBO.24.12.121904. [DOI] [Google Scholar]
- 4.Sommer AP, Schemmer P, Pavláth AE, Försterling H-D, Mester ÁR, Trelles MA. Quantum biology in low level light therapy: death of a dogma. Ann Transl Med. 2020;8(7):440. doi: 10.21037/atm.2020.03.159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marshal RP, Vlkova K. Spectral Dependence of Laser Light on Light tissue Interactions and its Influence on Laser Therapy: An Experimental Study. Insights Biomed. 2020;5(1):1–4. doi: 10.36648/2572-5610.4.4.66. [DOI] [Google Scholar]
- 6. Pruitt T, Parvez H, Wang X, Liu H. Investigation of 1064- nm Laser Fluence Within Tissue Phantoms for Better Prediction of Transcranial Photobiomodulation Depth. 2020. Paper presented at: Optical Tomography and Spectroscopy; 2020 Apr 20. Optical Society of America, 10.1364/TRANSLATIONAL.2020.JW3A.29 [DOI]
- 7.Kaydok E, Ordahan B, Solum S, Karahan AY. Short-term Efficacy Comparison of High-intensity and Low-intensity Laser Therapy in the Treatment of Lateral Epicondylitis: A Randomized Double-blind Clinical Study. Arch Rheumatol. 2020;35(1):60–67. doi: 10.5606/ArchRheumatol.2020.7347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ordahan B, Karahan AY, Kaydok E. The effect of high-intensity versus low-level laser therapy in the management of plantar fasciitis: a randomized clinical trial. Lasers Med Sci. 2018;33(6):1363–1369. doi: 10.1007/s10103-018-2497-6. [DOI] [PubMed] [Google Scholar]
- 9.Ezzati K, Laakso E-L, Salari A, Hasannejad A, Fekrazad R, Aris A. The Beneficial Effects of High-Intensity Laser Therapy and Co-Interventions on Musculoskeletal Pain Management: A Systematic Review. J Lasers Med Sci. 2020;11(1):81–90. doi: 10.15171/jlms.2020.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ezzati K, Laakso E-L, Saberi A, Yousefzadeh Chabok S, Nasiri E, Bakhshayesh Eghbali B. A comparative study of the dose-dependent effects of low level and high intensity photobiomodulation (laser) therapy on pain and electrophysiological parameters in patients with carpal tunnel syndrome: a randomized controlled trial. Eur J Phys Rehabil Med. 2020;56(6):733–740. doi: 10.23736/S1973-9087.19.05835-0. [DOI] [PubMed] [Google Scholar]
- 11.Henderson TA, Morries LD. Near-infrared photonic energy penetration: can infrared phototherapy effectively reach the human brain? Neuropsychiatr Dis Treat. 2015;11:2191–2208. doi: 10.2147/NDT.S78182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Simpson CR, Kohl M, Essenpreis M, Cope M. Near-infrared optical properties of ex vivo human skin and subcutaneous tissues measured using the Monte Carlo inversion technique. Phys Med Biol. 1998;43(9):2465–2478. doi: 10.1088/0031-9155/43/9/003. [DOI] [PubMed] [Google Scholar]
- 13.Esnouf A, Wright PA, Moore JC, Ahmed S. Depth of penetration of an 850 nm wavelength low level laser in human skin. Acupunct Electrother Res. 2007;32(1-2):81–86. doi: 10.3727/036012907815844165. [DOI] [PubMed] [Google Scholar]
- 14. Calderhead RG. Photobiological Basics of Photosurgery and Phototherapy. HA NMI Medical Publishing; 2011.
- 15. Toselli F, Bodechtel J, eds. Imaging Spectroscopy: Fundamentals and Prospective Applications. Springer Netherlands; 1992.
- 16. Splinter R, Hooper BA, Hooper BA. An Introduction to Biomedical Optics. CRC Press; 2006. 10.1201/9781420011838 [DOI]
- 17.Wang P, Li T. Which wavelength is optimal for transcranial low-level laser stimulation? J Biophotonics. 2019;12(2):e201800173. doi: 10.1002/jbio.201800173. [DOI] [PubMed] [Google Scholar]
- 18.Steinberg I, Huland DM, Vermesh O, Frostig HE, Tummers WS, Gambhir SS. Photoacoustic clinical imaging. Photoacoustics. 2019;14:77–98. doi: 10.1016/j.pacs.2019.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mustari A, Nishidate I, Wares MdA. et al. Agarose-based Tissue Mimicking Optical Phantoms for Diffuse Reflectance Spectroscopy. J Vis Exp. 2018;(138):57578. doi: 10.3791/57578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd edition. Routledge; 1988.
- 21.Brand A, Bradley MT, Best LA, Stoica G. Multiple trials may yield exaggerated effect size estimates. J Gen Psychol. 2011;138(1):1–11. doi: 10.1080/00221309.2010.520360. [DOI] [PubMed] [Google Scholar]
- 22.Yılmaz M, Eroglu S, Dundar U, Toktas H. The effectiveness of high-intensity laser therapy on pain, range of motion, functional capacity, quality of life, and muscle strength in subacromial impingement syndrome: a 3-month follow-up, double-blinded, randomized, placebo-controlled trial. Lasers Med Sci. 2021 doi: 10.1007/s10103-020-03224-7. [DOI] [PubMed] [Google Scholar]
- 23.Yesil H, Dundar U, Toktas H, Eyvaz N, Yeşil M. The effect of high intensity laser therapy in the management of painful calcaneal spur: a double blind, placebo-controlled study. Lasers Med Sci. 2020;35(4):841–852. doi: 10.1007/s10103-019-02870-w. [DOI] [PubMed] [Google Scholar]
- 24.Akaltun MS, Altindag O, Turan N, Gursoy S, Gur A. Efficacy of high intensity laser therapy in knee osteoarthritis: a double-blind controlled randomized study. Clin Rheumatol. 2020;40(5):1989–1995. doi: 10.1007/s10067-020-05469-7. [DOI] [PubMed] [Google Scholar]
- 25.Thabet AAE-M, Elsodany AM, Battecha KH, Alshehri MA, Refaat B. High-intensity laser therapy versus pulsed electromagnetic field in the treatment of primary dysmenorrhea. J Phys Ther Sci. 2017;29(10):1742–1748. doi: 10.1589/jpts.29.1742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.El-Shamy SM, Alayat MSM, Abdelgalil AA, Alshehri MA. Long-Term Effect of Pulsed Nd:YAG Laser in the Treatment of Children with Juvenile Rheumatoid Arthritis: A Randomized Controlled Trial. Photomed Laser Surg. 2018;36(8):445–451. doi: 10.1089/pho.2018.4444. [DOI] [PubMed] [Google Scholar]
- 27.Alayat MS, Mohamed AA, Helal OF, Khaled OA. Efficacy of high-intensity laser therapy in the treatment of chronic neck pain: a randomized double-blind placebo-control trial. Lasers Med Sci. 2016;31(4):687–94. doi: 10.1007/s10103-016-1910-2. [DOI] [PubMed] [Google Scholar]
- 28.Ebid AA, Ibrahim AR, Omar MT, El Baky AMA. Long-term effects of pulsed high-intensity laser therapy in the treatment of post-burn pruritus: a double-blind, placebo-controlled, randomized study. Lasers Med Sci. 2017;32(3):693–701. doi: 10.1007/s10103-017-2172-3. [DOI] [PubMed] [Google Scholar]
- 29.Venosa M, Romanini E, Padua R, Cerciello S. Comparison of high-intensity laser therapy and combination of ultrasound treatment and transcutaneous nerve stimulation in patients with cervical spondylosis: a randomized controlled trial. Lasers Med Sci. 2019;34(5):947–953. doi: 10.1007/s10103-018-2682-7. [DOI] [PubMed] [Google Scholar]
- 30.Yilmaz M, Tarakci D, Tarakci E. Comparison of high-intensity laser therapy and combination of ultrasound treatment and transcutaneous nerve stimulation on cervical pain associated with cervical disc herniation: A randomized trial. Complement Ther Med. 2020;49:102295. doi: 10.1016/j.ctim.2019.102295. [DOI] [PubMed] [Google Scholar]
- 31.Angelova A, Ilieva EM. Effectiveness of High Intensity Laser Therapy for Reduction of Pain in Knee Osteoarthritis. Pain Res Manag. 2016;2016:9163618. doi: 10.1155/2016/9163618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.El-Shamy SM, Abdelaal AAM. Efficacy of pulsed high-intensity laser therapy on pain, functional capacity, and gait in children with haemophilic arthropathy. Disabil Rehabil. 2018;40(4):462–468. doi: 10.1080/09638288.2016.1261416. [DOI] [PubMed] [Google Scholar]
- 33.Alayat MSM, Aly THA, Elsayed AEM, Fadil ASM. Efficacy of pulsed Nd:YAG laser in the treatment of patients with knee osteoarthritis: a randomized controlled trial. Lasers Med Sci. 2017;32(3):503–511. doi: 10.1007/s10103-017-2141-x. [DOI] [PubMed] [Google Scholar]
- 34.A Nazari A, Moezy A, Nejati P, Mazaherinezhad A. Efficacy of high-intensity laser therapy in comparison with conventional physiotherapy and exercise therapy on pain and function of patients with knee osteoarthritis: a randomized controlled trial with 12-week follow up. Lasers Med Sci. 2019;34(3):505–516. doi: 10.1007/s10103-018-2624-4. [DOI] [PubMed] [Google Scholar]
- 35.Salli A, Akkurt E, Izki AA, Şen Z, Yilmaz H. Comparison of High Intensity Laser and Epicondylitis Bandage in the Treatment of Lateral Epicondylitis. Arch Rheumatol. 2016;31(3):234–238. doi: 10.5606/ArchRheumatol.2016.5793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pekyavas NO, Baltaci G. Short-term effects of high-intensity laser therapy, manual therapy, and Kinesio taping in patients with subacromial impingement syndrome. Lasers Med Sci. 2016;31(6):1133–1141. doi: 10.1007/s10103-016-1963-2. [DOI] [PubMed] [Google Scholar]
- 37.Taradaj J, Rajfur K, Shay B, Rajfur J, Ptaszkowski K, Walewicz K. et al. Photobiomodulation using high- or low-level laser irradiations in patients with lumbar disc degenerative changes: disappointing outcomes and remarks. Clin Interv Aging. 2018;13:1445–1455. doi: 10.2147/CIA.S168094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Abdelbasset WK, Nambi G, Alsubaie SF, Abodonya AM, Saleh AK, Ataalla NN. et al. A Randomized Comparative Study between High-Intensity and Low-Level Laser Therapy in the Treatment of Chronic Nonspecific Low Back Pain. Evid Based Complement Alternat Med. 2020;2020:1350281. doi: 10.1155/2020/1350281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Alayat MSM, Abdel-Kafy EM, Thabet AAM, Abdel-Malek AS, Ali TH, Header EA. Long-Term Effect of Pulsed Nd-YAG Laser Combined with Exercise on Bone Mineral Density in Men with Osteopenia or Osteoporosis: 1 Year of Follow-Up. Photomed Laser Surg. 2018;36(2):105–111. doi: 10.1089/pho.2017.4328. [DOI] [PubMed] [Google Scholar]
- 40.Naruseviciute D, Kubilius R. The effect of high-intensity versus low-level laser therapy in the management of plantar fasciitis: randomized participant blind controlled trial. Clin Rehabil. 2020;34(8):1072–108. doi: 10.1177/0269215520929073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chen L, Liu D, Zou L, Huang J, Chen J, Zou Y. et al. Efficacy of high intensity laser therapy in treatment of patients with lumbar disc protrusion: A randomized controlled trial. J Back Musculoskelet Rehabil. 2018;31(1):191–196. doi: 10.3233/BMR-170793. [DOI] [PubMed] [Google Scholar]
- 42.Alshami AM, Souvlis T, Coppieters MW. A review of plantar heel pain of neural origin: differential diagnosis and management. Man Ther. 2008;13(2):103–111. doi: 10.1016/j.math.2007.01.014. [DOI] [PubMed] [Google Scholar]
- 43.Thabet AAE-M, Mahran HG, Ebid AA, Alshehri MA. Effect of pulsed high intensity laser therapy on delayed caesarean section healing in diabetic women. J Phys Ther Sci. 2018;30(4):570–575. doi: 10.1589/jpts.30.570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. THOR Photomedicine Ltd. Annette Quinn - Oral Mucositis Academy of Laser Dentistry 2016. YouTube. Accessed April 16, 2021. https://www.youtube.com/watch?v = xU5_9169dbw.
- 45.Zadik Y, Arany PR, Fregnani ER, Bossi P, Antunes HS, Bensadoun RJ. et al. Systematic review of photobiomodulation for the management of oral mucositis in cancer patients and clinical practice guidelines. Support Care Cancer. 2019;27(10):3969–3983. doi: 10.1007/s00520-019-04890-2. [DOI] [PubMed] [Google Scholar]
- 46. Cold Laser and High-Power Laser Therapies - Medical Clinical Policy Bulletins | Aetna. Accessed October 14, 2020. http://www.aetna.com/cpb/medical/data/300_399/0363.html.
- 47.Weber GC, Firouzi P, Baran AM, Bölke E, Schrumpf H, Buhren BA. et al. Treatment of onychomycosis using a 1064- nm diode laser with or without topical antifungal therapy: a single-center, retrospective analysis in 56 patients. Eur J Med Res. 2018;23(1):53. doi: 10.1186/s40001-018-0340-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary file 1 contain Figure S1.
Supplementary file 2 contain Table S1.