Abstract
CD44, a cell-adhesion molecule has a dual role in tumor growth and progression; it acts as a tumor suppressor as well as a tumor promoter. In our previous work, we developed a tetracycline-off regulated expression of CD44’s gene in the breast cancer (BC) cell line MCF-7 (B5 clone). Using cDNA oligo gene expression microarray, we identified SOD2 (superoxide dismutase 2) as a potential CD44-downstream transcriptional target involved in BC metastasis. SOD2 gene belongs to the family of iron/manganese superoxide dismutase family and encodes a mitochondrial protein. SOD2 plays a role in cell proliferation and cell invasion via activation of different signaling pathways regulating angiogenic abilities of breast tumor cells. This review will focus on the findings supporting the underlying mechanisms associated with the oncogenic potential of SOD2 in the onset and progression of cancer, especially in BC and the potential clinical relevance of its various inhibitors.
Keywords: SOD2, CD44, hyaluronan, breast cancer, invasion
1. Introduction
Tumor cell invasion is the most defining and recurring event during the multistage process of metastasis. It involves the activation of a complex molecular network involving, involving, in particular, cell adhesion molecules (CAMs) [1,2] which facilitate the adhesion of invading cells to their surrounding extracellular matrix (ECM) [3]. Among numerous CAM protein families, CD44 is the principal cell surface receptor for hyaluronic acid (HA), a major component of the ECM produced by embryonic stem cells, connective tissue cells, bone marrow cells [4,5], and cancer cells [6,7]. We have previously reported that the interaction of CD44 with HA activates various oncogenic signaling pathways, leading to tumor cell survival, proliferation, and invasion [8,9,10,11,12,13].
In order to better understand the exact function of the standard form of CD44 (CD44s) in BC and further elucidate the signaling mechanisms that underpin CD44-promoted BC invasion/metastasis, we have previously developed a tetracycline (Tet)-Off-regulated expression system of CD44s both in vitro [11] and in vivo [12]. Moreover, we applied microarray gene expression profiling, using total RNA samples isolated from “CD44-On versus CD44-Off cells”. Bioinformatics analyses revealed more than 200 CD44-downstream transcriptional target genes that were upregulated or downregulated. Four genes have already been validated, and their signaling pathways linking their transcriptional activation to CD44 upstream regulation, have already been published [14].
Among the remaining genes, SOD2 was significantly upregulated upon interaction of CD44 with its major ligand hyaluronan (HA), suggesting that SOD2 might be an additional novel transcriptional target of CD44-downstream signaling that underpins its role in promoting BC tumor cell invasion and metastasis.
SOD2 encodes the manganese superoxide dismutase (Mn-SOD), which is involved in regulating oxidative stress in the cell through the dismutation of superoxide radicals (O2−) to H2O2 and molecular oxygen [15,16,17]. Reactive oxygen species (ROS) cause DNA damage, resulting in genetic aberrations and genomic instability, thus promoting mutagenesis and carcinogenesis [18,19]. Damage by ROS is usually mitigated by antioxidant actions of non-enzymatic antioxidants or antioxidant enzymes, thereby reducing the likelihood of mutations and possibly oncogenic transformation [20]. Alteration in the expression of antioxidant enzymes, like catalase (CAT), glutathione peroxidases (GPx), and superoxide dismutases (SOD), can impair regulation of enzymatic activity and modify ROS detoxification [21].
The SOD family encompasses three members, SOD1, SOD2, and SOD3. While SOD1 is localized in the cytoplasm and the mitochondrial intermembrane space, SOD2 is exclusively present in the mitochondrial matrix, and SOD3 is extracellularly present [22]. Genetic variations in SOD2 have been found to be associated with many diseases, including neurodegeneration, mitochondrial dysfunction, premature aging, angiogenesis, and cancer [23,24,25,26,27].
This review presents data from the literature supporting our hypothesis that SOD2 might be a novel transcriptional target of CD44-downstream signaling, which promotes BC cell invasion. We have discussed these lines of evidence and proposed a model of the signaling pathways linking CD44 activation by HA to the transactivation of SOD2 to promote breast tumor cell invasion.
2. Structure of SOD2
The human SOD2 gene, located on the long arm of chromosome 6 (6q25.3; from base pair 159,669,069 to base-pair 159,762,281), consists of 5 exons and 4 introns [16,17] encoding 222 amino acids [22,28,29]. The genetic sequence reveals that the SOD2 promoter lacks the typical TATA and CAAT boxes; it is, however, rich in GC sequences as well as binding sites for specificity protein (SP) and activator protein 2 (AP2) transcription factors [29]. Sp1 and NF-kB are two transcription factors that have been well-studied in the regulation of SOD2 expression. Sp1 maintains SOD2’s basal promoter activity, whereas Nf-kB increases SOD2 transcription mostly through a cis-element inside the second intronic enhancer region [30]. Additionally, the 3′-untranslated region of SOD2 mRNA shows a conserved 41 bp translational enhancer region [30].
The SOD2 protein is a homo-tetramer (86–88 kDa in total), with each of the four subunits having a molecular mass of around 23 kDa, and each including a manganese (Mn+3) cofactor [28]. The precursor monomer of SOD2 starts with a 26 amino acid mitochondrial targeting sequence (MTS), which is vital for mitochondrial localization [31]. For example, SOD2 gene polymorphisms, which result in a substitution of Ala-9 to Val (Val9Ala) [28], or Ala-16 to Val (Val16Ala) alter the structure of SOD2 MTS, and have been linked with susceptibility to various pathologies [32,33].
Each mature SOD2 monomer consists of two unique domains, an N-terminal helical hairpin domain and a C-terminal a/b domain. The C-terminal a/b domain contains five-alpha helices and three-stranded antiparallel beta-sheets. Together, these domains encompass key residues (D159, H163, H26, and H74), allowing the active site to interact with the Mn³+ cofactor and a water molecule [34], which are critical to the enzyme’s dismutase activity.
3. Functions of SOD2
Physiologically, SOD2 is expressed in both normal and malignant cells, thus, the following sections will discuss the role of SOD2 in both contexts.
3.1. Physiological Function of SOD2 in Normal Cells
While aerobic respiration produces low amounts of ROS, cells utilize SODs to prevent these molecules from causing damage. SODs provide such a mechanism, since most of the ROS is produced by the electron transport chain in the mitochondrial matrix of human cells, where SOD2 is ideally localized [35]. Integration of the Mn cofactor into the SOD2 catalytic site triggers the enzyme to carry out its dismutase activity [15,16], and thus enables it to maintain mitochondrial integrity [36,37] and protect mitochondrial DNA (mtDNA) and mtDNA Polymerase C from oxidative damage or inactivation [38].
3.2. Physiological Functions of SOD2 in Cancer
Various lines of evidence lead to the conclusion that SOD2 can act either as a tumor suppressor gene (TSG) or as an oncogene [39].
Variations in SOD2 activity are found during different cell cycle stages [40,41,42]; and an argument for a TSG role can be made based on studies showing reduced SOD2 expression in pancreatic cancer cells, as well as glioma cells, and SOD2 results showing significantly delayed tumor cell growth in nude mice xenograft studies [43,44]. Such loss of SOD2 expression enhances cell cycle progression (mitosis) by increasing O2•− levels [45], thus stimulating ROS-mediated DNA damage and inducing cell transformation and tumorigenesis [46,47].
Different mechanisms have been proposed for the loss of SOD2 in cancer. Mutations in the SOD2 gene promoter have been reported to impact the AP2 binding pattern in colorectal cancer cells, resulting in loss of SOD2 expression [48]. Some evidence also points to epigenetic modifications as a reason for the downregulation of SOD2 expression [39,41,42]. SOD2 promoter methylation was reported in both transformed and cancer cells [49,50], and in another study, cytosine methylation of the second intron of SOD2 was found to result in reduced SOD2 expression [47]. Such methylation patterns have been reported in breast and pancreatic cancers as well as multiple myeloma [49,50,51,52].
While reduced SOD2 expression is commonly reported in the early stages of tumor growth, some studies report elevated levels of SOD2 during metastatic progression [36,53,54]. SOD2 was overexpressed in metastatic tumor lesions and aggressive tumor cell lines. Upregulated SOD2 levels enhance the oxidation of PTEN and PTP-N12, further activating Akt and p130 cas/Rac1 signaling pathways, respectively [37]; these pathways regulate the hallmarks of cancer during tumor progression [37,55,56,57,58]. Thus, these data put together point to an oncogenic role of SOD2 in the onset and progression of cancer.
Table 1 summarizes the mechanisms underlying the dual role of SOD2 in different cancers.
Table 1.
Mechanisms underlying the expression of SOD2 in different cancers.
| Type of Cancer | SOD2 Expression | Underlying Mechanism | References |
|---|---|---|---|
| Bladder | Downregulated | Not determined | [59] |
| Brain | Downregulated | SOD2 hyperacetylation | [60] |
| Upregulated | Not determined | [61,62,63] | |
| Breast | Downregulated | p53 transcriptional inhibition Presence of DDB2 Epigenetics SOD2 hyperacetylation |
[51,64,65,66] |
| Upregulated | Loss of p53 NF-kB Nrf2 activation |
[64,67,68] | |
| Colorectal | Downregulated | Elevated AP1 at SNP promoter | [48] |
| Upregulated | Not determined | [69,70] | |
| Esophageal | Downregulated | Not determined | [71] |
| Upregulated | [59] | ||
| Leukemia | Downregulated | Not determined | [59] |
| Upregulated | ARNT activation | [44] | |
| Liver | Downregulated | Calcium blocking of SIRT3 | [72,73] |
| Upregulated | Not determined | [59] | |
| Lung | Downregulated | Ala16Val substitution | [74] |
| Upregulated | Not determined | [59] | |
| Lymphoma | Upregulated | Not determined | [75] |
| Melanoma | Downregulated | Loss of heterozygosity | [76] |
| Multiple Myeloma | Downregulated | Epigenetic silencing | [49,50] |
| Ovarian | Upregulated | Keap1 mutation Nrf2 activation |
[52,57,77] |
| Pancreatic | Downregulated | Epigenetic silencing miR-301a activation Ala16Val substitution |
[78,79,80] |
| Upregulated | Not determined | [81] | |
| Prostate | Upregulated | Low miR-17 expression | [70,82] |
| Renal Clear Cell | Downregulated | HIF-1α activation Oxidation |
[83,84] |
| Sarcoma | Downregulated | Nitration | [59] |
| Upregulated | Not determined | [59] | |
| Tongue Squamous Cell | Downregulated | miR-222 activation | [85] |
| Upregulated | c-myc activation | [86] |
Ala: alanine; AP1: activated promoter 1; ARNT: aryl hydrocarbon receptor nuclear translocator; c-myc: cellular myelocytomatosis; DDB2: damaged DNA binding 2; HIF-1α: hypoxia-inducible factor 1-alpha; Keap1: kelch-like ECH-associated protein 1; miR: micro-RNA; NF-kB: nuclear factor-kappa B; Nrf2: nuclear factor erythroid 2–related factor 2; SIRT3: sirtuin 3; SNP: single nucleotide polymorphism; Val: Valine.
3.3. Physiological Functions of SOD2 in Invasion, Metastasis, and Angiogenesis
Accumulation of free radicals is associated with mitochondrial function and metastatic disease progression. Although, ROS play a role in tumor initiation and progression, the underlying mechanisms and causes of enhanced ROS accumulation during tumorigenesis still lie nascent.
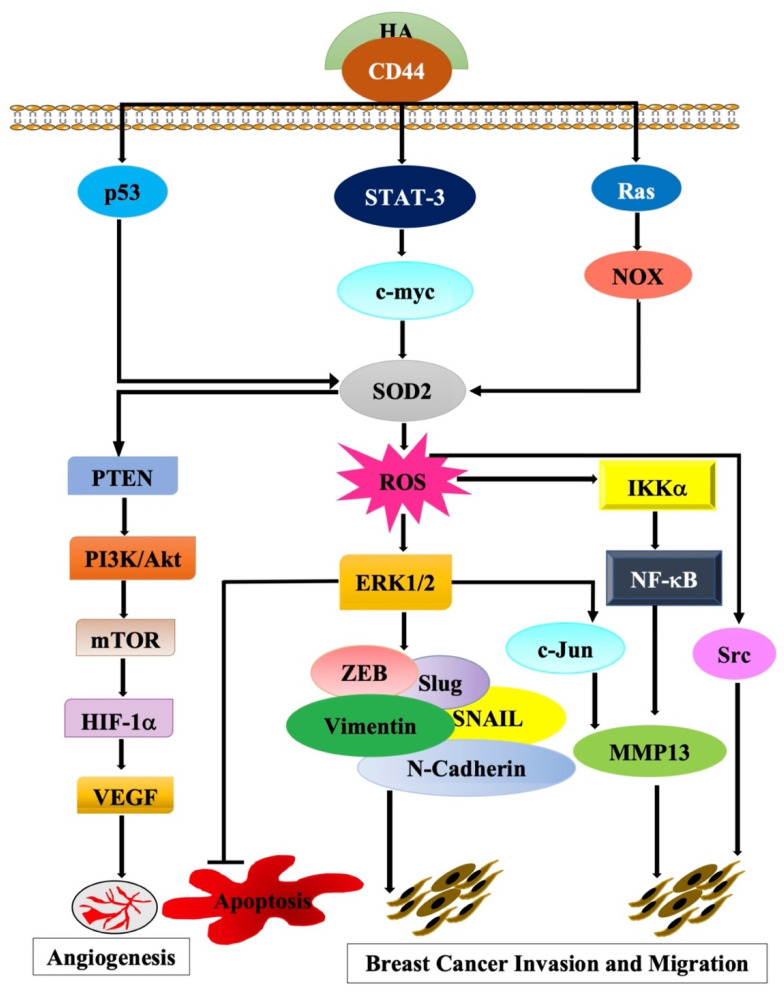
Findings from various studies strongly support our hypothesis that the activation of CD44 by its major ligand hyaluronan (HA) activates the transcription of SOD2 to promote tumor cell invasion/metastasis (Figure 1).
Figure 1.
A proposed novel model of the molecular signaling pathways that link the activation of CD44 by its ligand hyaluronan (HA) to the transactivation of its potential target gene SOD2.
SOD2 expression increases cellular oxidant/antioxidant ratios, which are directly associated with tumor progression, angiogenesis and migration, and invasion [53,87]. In several cancers, SOD2 expression is elevated during metastasis [61,62,88,89,90,91,92,93]. Increased SOD2 expression in metastatic cancer cell lines as well as in tumor tissues is associated with increased SOD2 activity, thus, indicating a functional role for SOD2 during metastatic progression and poor outcome, particularly in BC [54,81,94,95,96], where elevated SOD2 expression is associated with metastatic progression in estrogen receptor (ER) negative BCs [93].
The transcriptional repressor DDB2 plays an important role in the dual nature of SOD2 in BC [65]. While in ER-positive BC cells (MCF7), DDB2 reduced acetylated H3 histones and decreased binding of Sp1 to SOD2 promoter, in ER-negative BC cells (MDA-MB-231), the lack of DDB2 induced high levels of SOD2 [65]. In the BC cell line, T47D, SOD2 expression was regulated by progestin [97].
Additionally, oxygen-free radicals and ionizing radiation have been shown to stimulate SOD2 expression in a TNFα-dependent manner [98,99], as altered TNFα levels correlate with enhanced metastatic disease [100]. Briefly, TNFα ligands bind to TNFRs to stimulate upstream IKKs and phosphorylate IκB that is bound to the inactive NF-κB dimer (RelA + p50) in the cytoplasm. IκB underwent proteasome degradation and activated NF-κB translocates into the nucleus, where it triggers the expression of genes encoding proteins. NFκB triggers the activity of the SOD2 promoter, thus inducing SOD2 expression [101,102]. NF-κB has also been found to cooperate with ZEB2 to increase SOD2 gene expression in cells containing high levels of CD44 (CD44H), which leads to the induction of epithelial-mesenchymal transition mechanism [103].
Overexpression of SOD2 in tumor cells correlates with enhanced expression and activity of MMPs, leading to enhanced matrix degradation and a release of cytokines and growth factors, thereby promoting metastasis [104]. For example, in the ER positive BC cell line, MCF7 increased ROS, enhanced SOD2 expression, and activated MMP2 in parallel [105]. Similarly, overexpression of SOD2 in HT-1080 fibrosarcoma, as well as 253J bladder carcinoma cells, significantly promoted migration and invasion both in vitro and in vivo [56,92,106]. One of the effects of increased SOD2 expression is a significant reduction in catalase activity, resulting in increased H2O2 production [53,56], which has been shown to upregulate the expression of MMP-1 [107], and might increase the levels of VEGF and MMP-9, known contributors of cell invasion and angiogenesis [108,109].
Further, binding of Ets-1 to the MMP-1 promoter and sustained JNK signaling requires the enzyme activity of SOD2 [108,110]. Thus, it appears that SOD2 is essential for the stimulation of MMP-1 as well as other MMP family members via the H2O2-dependent activation of MAPK signaling [108,110,111], resulting in the remodeling and degradation of the ECM and the basement membranes, thereby promoting tumor cell invasion and metastasis [112].
The above, along with our findings that SOD2 was significantly upregulated upon the interaction of CD44 with its major ligand HA [14]; prompted us to hypothesize that SOD2 might be a novel transcriptional target of CD44-downstream signaling, and thus, have a critical role in promoting BC tumor cell invasion and metastasis.
As a matter of fact, elevated content of SOD2 is correlated with increased tumor cell invasion, metastasis, proliferation, and resistance to apoptosis [53]. Thus, there is an association between CD44 and SOD2 as they are involved in common signaling pathways promoting metastasis, cell migration, cell invasion, and angiogenesis [113]. Our initial experiments revealed that HA treatment of MDA-MB-231 BC cells significantly increased CD44 expression at 24 h, which was accompanied by a parallel pattern of expression of its transcriptional target SOD2 at RNA levels. More interestingly, inhibition of CD44 using specific siRNA significantly decreased RNA expression levels of SOD2. Ongoing functional, molecular, and pharmacological experiments aim to validate the physiological relevance of the CD44/SOD2 signaling pathway in BC cell invasion and further identify its intermediate molecular players.
3.4. Potential Inhibitors Targeting SOD2
There is a dire need to develop anticancer therapeutics targeting ROS signaling, and hence, use of SOD mimetics that simulate endogenous SOD enzyme activity or inhibit oxidative injury—biomarkers of cell proliferation are being explored.
The epigenetic drug zebularine was found to effectively reverse SOD2 promoter methylation in the KAS6/1 human multiple myeloma cells [49]. In addition, tirchostatin A and sodium butyrate were also found to alter SOD2 expression by regulating histone methylation and acetylation in breast cancer cells [51,114]. Synthetic SOD mimetics were also reported to cross the blood–brain barrier and exert a protective effect against neurodegenerative diseases [115,116,117,118].
Adenoviral vectors, in combination with chemotherapeutic agents have also been used to induce SOD expression. In breast tumor xenograft models, injection of Cu-ZnSOD or SOD2 adenoviral vectors in combination with BCNU significantly reduced breast cancer cell growth and increased nude mice survival [119]. Moreover, dual gene virotherapy utilizing adenovirus consisting of SOD2 and TRAIL-induced apoptosis inhibited colorectal tumor growth in xenograft models [120].
As mentioned above, elevated ROS stress in cancer cells is an unfavorable event associated with increased cancer progression and carcinogenesis. Recently, research has identified drugs capable of increasing cellular ROS accumulation to eliminate cancer cells [121,122]. Since oxidative stress linked with carcinogenesis makes cancer cells highly dependable on their antioxidant systems [123,124,125], inhibition of the antioxidant system could result in a substitutional accumulation of ROS and provoke apoptosis. Thus pharmacological drugs could be used to eradicate cancer cells by applying significant ROS stress.
Promoting ROS accumulation in cancer cells to a toxic level is the focus of some emerging cancer therapies, which makes SOD2 a good potential target. Various drugs are known to trigger ROS generation and accumulation; these include mitochondrial electron transport chain modulators (doxorubicin, topotecan), redox-cycling compounds (motexafin gadolinium), glutathione (GSH) depleting agents (buthionine sulphoximine, β-phenylethyl isothiocyanates (PEITC)), and inhibitors of SOD (2-methoxyestradiol) and catalase (e.g., 3-amino-1,2,4-triazole) [126,127,128].
Rapamycin and its analogs are being used in clinical trials for certain types of cancer as rapamycin alone can inhibit cell proliferation and induce apoptosis [129,130]. Moreover, rapamycin promotes chemosensitivity by blocking mTORC1 and activating Akt, thus resulting in ROS-induced cell death [131,132,133,134].
FOXM1 is a transcription factor that is over-expressed in the majority of human tumors. It can induce SOD2 expression, resulting in a decrease of ROS-levels in cancer cells, thereby promoting angiogenesis and metastasis [135,136]. Targeting FOXM1 in combination with oxidative stress is considered as an essential therapeutic strategy against cancer. Proteasome inhibitors (MG132) as well as thiazole antibiotics (siomycin-A) reduce FOXM1 expression and activity and induce apoptosis through DNA damaging agents, including doxorubicin and γ-irradiation [137,138,139].
In contrast to the above, the use of antioxidants has also shown some positive results. These often take the form of traditional therapeutics—natural occurring antioxidants. Natural products including curcumin [140,141,142], lycopene [143], ginger [144,145], and hesperetin [146] are redox-active and induce a pro-oxidative mechanism of action indicating their role as anti-tumorigenic, anti-inflammatory, and anti-angiogenic.
In one study, curcumin oil was found to maintain SOD2 expression and delayed bile acid-enhanced esophageal injury and cancer progression [147]. It has also been shown to decrease breast cancer-induced lung metastasis by approximately 40% and, in combination with paclitaxel, further inhibited breast cancer growth [148].
Astaxanthin, a xanthophyll, possesses anti-inflammatory properties and exerts its effect via ROS/reactive nitrogen species scavenging by inhibiting the expression of inflammatory cytokines (NF-κB, TNF-α, and IL-8) [149].
The natural dietary element, ginger has both antioxidant and anti-carcinogenic properties: ginger supplementation enhanced SOD, CAT, GPx, glutathione-S-transferase, and glutathione reductase activities, thus reducing oxidative stress as well as cancer cell growth [150].
Oroxylin A, a flavonoid extracted from a Chinese medicinal plant, can induce SOD2 gene expression, glycolysis inhibition, and reduced tumor growth of transplanted human breast tumors in vivo [151].
One of the dietary combination supplements, protandim, was shown to be effective in inhibiting tumor progression as well lipid peroxidation [152]. Protandim enhanced activities of both SOD and CAT, thus reducing tumor growth [153].
This indicates the use of antioxidants to target ROS generation.
Table 2 summarizes anti-SOD2-based therapeutic approaches.
Table 2.
Therapeutic Strategies for targeting SOD2.
| Therapy | Treatment | Mode of Action | References |
|---|---|---|---|
| Epigenetic Drugs | Zebularine | Reverses SOD2 promoter methylation | [49] |
| Tirchostatin A | Regulates histone methylation and acetylation | [51,114] | |
| Sodium butyrate | |||
| Adenoviral Vectors | Cu-Zn SOD/SOD2 adenoviral vectors combined with BCNU | Induces SOD expression to reduce cancer cell growth and increases survival | [119] |
| SOD2 and TRAIL combination | Enhances SOD expression to stimulate cell apoptosis and reduce tumor growth | [120] | |
| Topoisomerase inhibitors | Doxorubucin | Reduces cancer growth by binding to the topoisomerase enzymes and block topoisomerases 1 and 2 | [154] |
| Topotecan | |||
| Redox Cyclin Compounds | Motexafin gadolinium | Induces apoptosis by alteration in mitochondrial membrane potential, depletion of intracellular GSH and increased ROS production. | [155] |
| GSH Depleting Agents | Buthionine sulphoximine | Eliminates GSH from the cells by blocking GPx and accumulates ROS production Oxidative inactivation of H-Ras and NF-kB Oxidative damage of mitochondria Induces apoptosis |
[126,127,128,133] |
| β-phenylethyl isothiocyanates (PEITC) | |||
| SOD2 inhibitors | 2-methoxyestradiol | Blocks both manganese and copper, zinc superoxide dismutases and reduces cancer growth | [156] |
| Catalase | 3-amino-1,2,4, triazole | Reduces CAT activity Enhances intracellular H2O2 levels Decreases GPx activity |
[157] |
| Anti-fungal Antibiotic | Rapamycin | Inhibits cell proliferation Stimulates apoptosis Blocks mTORC1 and activates Akt to promote chemoresistance |
[129,130,131,132,133,134] |
| Proteosome inhibitor | MG132 | Reduces FOXM1 expression to induce apoptosis | [137,138,139] |
| Thiazole Antibiotic | siomycin-A | ||
| Natural Products | Curcumin | Conserves SOD2 expression Delays bile acid-induced esophageal injury and cancer progression |
[147,148] |
| Astaxanthin | Inhibits expression of NF-κB, TNF-α, and IL-8 to induce ROS/reactive nitrogen species scavenging | [149] | |
| Ginger | Inhibits oxidative stress and cancer growth by stimulating SOD, CAT, GPx, glutathione-S-transferase, and glutathione reductase activities | [150] | |
| Oroxylin A | Induces SOD2 gene expression Inhibits glycolysis Suppresses tumor growth |
[151] | |
| Protandim | Stimulates SOD and CAT activities Reduces tumor growth |
[153] |
2-ME: 2-methoxyestradiol; Akt: protein kinase B; BCNU: 1,3-bis(2-chloroenthyl)-1-nitrosurea; CAT: catalase; Cu-Zn: copper–zinc; FOXM1: forkhead box M1; GPx: glutathione peroxidases; GSH: glutathione; IL: interleukin; mTORC1: mammalian target of rapamycin complex 1; NF-kB: nuclear factor-kappa B; PEITC: phenylethyl isothiocyanates; ROS: reactive oxygen species; TNF: tumor necrosis factor; TRAIL: TNF-related apoptosis-inducing ligand.
4. Conclusions
Several studies have suggested the complicity of antioxidant enzymes in cancer development and identified high expression of SOD2 as a factor in cancer progression. The ability to use SOD2 to modify the cellular redox environment can help with the identification of redox-responsive signaling events that stimulate malignancy, such as invasion, migration, and prolonged tumor cell survival. Additional studies of these redox-driven events will help in the development of targeted therapeutic strategies to efficiently restrict redox-signaling essential for malignant progression. In particular, results from our own work and others support our hypothesis that CD44-HA interaction can transactivate SOD2, ultimately leading to BC progression.
Abbreviations
2-ME: 2-methoxyestradiol; Akt: protein kinase B; Ala: alanine; AP: activated protein; ARNT: aryl hydrocarbon receptor nuclear translocator; BC: breast cancer; BCNU: 1,3-bis(2-chloroenthyl)-1-nitrosurea; c-myc: cellular myelocytomatosis; CAMs: cell adhesion molecules; CAT: catalase; Cu-Zn: copper–zinc; DDB2: damaged DNA binding 2; ECM: extracellular matrix; ER: estrogen receptor; FOXM1: forkhead box M1; GPx: glutathione peroxidases; GSH: glutathione; HA: hyaluronan; HIF-1α: hypoxia-inducible factor 1-alpha; IL: interleukin; JNK: jun N-terminal kinase; Keap1: kelch-like ECH-associated protein 1; MAPK: mitogen-activated protein kinase; miR: micro-RNA; Mn: manganese; mTORC1: mammalian target of rapamycin complex 1;MTS: mitochondrial targeting sequence; MMP: matrix metalloproteinase; NF-kB: nuclear factor-kappa B; Nrf2: nuclear factor erythroid 2–related factor 2; PEITC: phenylethyl isothiocyanates; PTEN: phosphatase and tensin homolog; PTP-N12: protein tyrosine phosphatase non-receptor type 12; Rac1: Ras-related C3 botulinum toxin substrate 1; ROS: reactive oxygen species; SIRT3: sirtuin 3; SNP: single nucleotide polymorphism; SOD: superoxide dismutase; SP: specificity protein; TNF: tumor necrosis factor; TNFR: tumor necrosis factor receptor; TRAIL: TNF-related apoptosis-inducing ligand; TSG: tumor suppressor gene; Val: valine.
Author Contributions
Conceptualization, A.O.; writing—original draft preparation, N.A.; writing—review and editing, I.G., R.S.R. and A.O.; funding acquisition, A.O. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Qatar University Internal grant number: QUST-1-CAS2019-22, QUST-2-CAS-2021-137 and QUST-2-CAS-2021-138 and, the Qatar Foundation grant number: UREP24-117-1-027. Open Access funding was provided by the Qatar National Library.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data sharing is not applicable to this article as no new data or datasets were created, generated, or analyzed in this study.
Conflicts of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Martin T., Ye L., Sanders A.J., Lane J., Jiang W.G. Cancer Invasion and Metastasis: Molecular and Cellular Perspective. In: Jandial R., editor. Madame Curie Bioscience Database [Internet] Landes Bioscience; Austin, TX, USA: 2013. pp. 2000–2013. [Google Scholar]
- 2.Martin T.A., Jiang W.G. Loss of tight junction barrier function and its role in cancer metastasis. Biochim. Biophys. Acta. 2009;1788:872–891. doi: 10.1016/j.bbamem.2008.11.005. [DOI] [PubMed] [Google Scholar]
- 3.Bendas G., Borsig L. Cancer cell adhesion and metastasis: Selectins, integrins, and the inhibitory potential of heparins. Int. J. Cell Biol. 2012;2012:676731. doi: 10.1155/2012/676731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Domev H., Amit M., Laevsky I., Dar A., Itskovitz-Eldor J. Efficient engineering of vascularized ectopic bone from human embryonic stem cell-derived mesenchymal stem cells. Tissue Eng. Part. A. 2012;18:2290–2302. doi: 10.1089/ten.tea.2011.0371. [DOI] [PubMed] [Google Scholar]
- 5.Gronthos S., Franklin D.M., Leddy H.A., Robey P.G., Storms R.W., Gimble J.M. Surface protein characterization of human adipose tissue-derived stromal cells. J. Cell Physiol. 2001;189:54–63. doi: 10.1002/jcp.1138. [DOI] [PubMed] [Google Scholar]
- 6.Isacke C.M., Yarwood H. The hyaluronan receptor, CD44. Int. J. Biochem. Cell Biol. 2002;34:718–721. doi: 10.1016/S1357-2725(01)00166-2. [DOI] [PubMed] [Google Scholar]
- 7.Lee J.Y., Spicer A.P. Hyaluronan: A multifunctional, megaDalton, stealth molecule. Curr. Opin. Cell Biol. 2000;12:581–586. doi: 10.1016/S0955-0674(00)00135-6. [DOI] [PubMed] [Google Scholar]
- 8.Abdraboh M.E., Gaur R.L., Hollenbach A.D., Sandquist D., Raj M.H., Ouhtit A. Survivin is a novel target of CD44-promoted breast tumor invasion. Am. J. Pathol. 2011;179:555–563. doi: 10.1016/j.ajpath.2011.04.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hill A., McFarlane S., Mulligan K., Gillespie H., Draffin J.E., Trimble A., Ouhtit A., Johnston P.G., Harkin D.P., McCormick D., et al. Cortactin underpins CD44-promoted invasion and adhesion of breast cancer cells to bone marrow endothelial cells. Oncogene. 2006;25:6079–6091. doi: 10.1038/sj.onc.1209628. [DOI] [PubMed] [Google Scholar]
- 10.Ouhtit A., Abd Elmageed Z.Y., Abdraboh M.E., Lioe T.F., Raj M.H.G. In vivo evidence for the role of CD44s in promoting breast cancer metastasis to the liver. Am. J. Pathol. 2007;171:2033–2039. doi: 10.2353/ajpath.2007.070535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ouhtit A., Madani S., Gupta I., Shanmuganathan S., Abdraboh M.E., Al-Riyami H., Al-Farsi Y.M., Raj M.H.G. TGF-beta2: A Novel Target of CD44-Promoted Breast Cancer Invasion. J. Cancer. 2013;4:566–572. doi: 10.7150/jca.6638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ouhtit A., Rizeq B., Saleh H.A., Rahman M.M., Zayed H. Novel CD44-downstream signaling pathways mediating breast tumor invasion. Int J. Biol. Sci. 2018;14:1782–1790. doi: 10.7150/ijbs.23586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ouhtit A., Abdraboh M.E., Hollenbach A.D., Zayed H., Raj M.H.G. CD146, a novel target of CD44-signaling, suppresses breast tumor cell invasion. Cell Commun. Signal. 2017;15:1–10. doi: 10.1186/s12964-017-0200-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Naor D., Nedvetzki S., Golan I., Melnik L., Faitelson Y. CD44 in cancer. Crit. Rev. Clin. Lab. Sci. 2002;39:527–579. doi: 10.1080/10408360290795574. [DOI] [PubMed] [Google Scholar]
- 15.Aguirre J.D., Culotta V.C. Battles with iron: Manganese in oxidative stress protection. J. Biol. Chem. 2012;287:13541–13548. doi: 10.1074/jbc.R111.312181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yamakura F., Kawasaki H. Post-translational modifications of superoxide dismutase. Biochim. Biophys. Acta. 2010;1804:318–325. doi: 10.1016/j.bbapap.2009.10.010. [DOI] [PubMed] [Google Scholar]
- 17.Becuwe P., Ennen M., Klotz R., Barbieux C., Grandemange S. Manganese superoxide dismutase in breast cancer: From molecular mechanisms of gene regulation to biological and clinical significance. Free Radic. Biol. Med. 2014;77:139–151. doi: 10.1016/j.freeradbiomed.2014.08.026. [DOI] [PubMed] [Google Scholar]
- 18.Storz P. Reactive oxygen species in tumor progression. Front. Biosci. 2005;10:1881–1896. doi: 10.2741/1667. [DOI] [PubMed] [Google Scholar]
- 19.Jackson A.L., Loeb L.A. The contribution of endogenous sources of DNA damage to the multiple mutations in cancer. Mutat. Res. 2001;477:7–21. doi: 10.1016/S0027-5107(01)00091-4. [DOI] [PubMed] [Google Scholar]
- 20.Janicka A., Szymańska-Pasternak J., Bober J. Polymorphisms in the oxidative stress-related genes and cancer risk. Ann. Acad Med. Stetin. 2013;59:18–28. [PubMed] [Google Scholar]
- 21.Forsberg L., de Faire U., Morgenstern R. Oxidative stress, human genetic variation, and disease. Arch. Biochem. Biophys. 2001;389:84–93. doi: 10.1006/abbi.2001.2295. [DOI] [PubMed] [Google Scholar]
- 22.Zelko I.N., Mariani T.J., Folz R.J. Superoxide dismutase multigene family: A comparison of the CuZn-SOD (SOD1), Mn-SOD (SOD2), and EC-SOD (SOD3) gene structures, evolution, and expression. Free Radic. Biol. Med. 2002;33:337–349. doi: 10.1016/S0891-5849(02)00905-X. [DOI] [PubMed] [Google Scholar]
- 23.Flynn J.M., Melov S. SOD2 in mitochondrial dysfunction and neurodegeneration. Free Radic. Biol. Med. 2013;62:4–12. doi: 10.1016/j.freeradbiomed.2013.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Treiber N., Maity P., Singh K., Ferchiu F., Wlaschek M., Scharffetter-Kochanek K. The role of manganese superoxide dismutase in skin aging. Dermato-Endocrinology. 2012;4:232–235. doi: 10.4161/derm.21819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fukai T., Ushio-Fukai M. Superoxide dismutases: Role in redox signaling, vascular function, and diseases. Antioxid. Redox Signal. 2011;15:1583–1606. doi: 10.1089/ars.2011.3999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Connor K.M., Subbaram S., Regan K.J., Nelson K.K., Mazurkiewicz J.E., Bartholomew P.J., Aplin A.E., Tai Y.T., Aguirre-Ghiso J., Flores S.C., et al. Mitochondrial H2O2 regulates the angiogenic phenotype via PTEN oxidation. J. Biol. Chem. 2005;280:16916–16924. doi: 10.1074/jbc.M410690200. [DOI] [PubMed] [Google Scholar]
- 27.Juan C.M., Rosa M.S., Isabel Q.-G. MnSOD/SOD2 in Cancer: The Story of a Double Agent. React. Oxyg. Species. 2018;5:86–106. [Google Scholar]
- 28.Wilcox C.S. Effects of tempol and redox-cycling nitroxides in models of oxidative stress. Pharmacol. Ther. 2010;126:119–145. doi: 10.1016/j.pharmthera.2010.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wan X.S., Devalaraja M.N., St Clair D.K. Molecular structure and organization of the human manganese superoxide dismutase gene. DNA Cell Biol. 1994;13:1127–1136. doi: 10.1089/dna.1994.13.1127. [DOI] [PubMed] [Google Scholar]
- 30.Chung D.J., Wright A.E., Clerch L.B. The 3′ untranslated region of manganese superoxide dismutase RNA contains a translational enhancer element. Biochemistry. 1998;37:16298–16306. doi: 10.1021/bi980935g. [DOI] [PubMed] [Google Scholar]
- 31.Wispé J.R., Clark J.C., Burhans M.S., Kropp K.E., Korfhagen T.R., Whitsett J.A. Synthesis and processing of the precursor for human mangano-superoxide dismutase. Biochim. Biophys. Acta. 1989;994:30–36. doi: 10.1016/0167-4838(89)90058-7. [DOI] [PubMed] [Google Scholar]
- 32.Brown A.L., Lupo P.J., Okcu M.F., Lau C.C., Rednam S., Scheurer M.E. SOD2 genetic variant associated with treatment-related ototoxicity in cisplatin-treated pediatric medulloblastoma. Cancer Med. 2015;4:1679–1686. doi: 10.1002/cam4.516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sutton A., Khoury H., Prip-Buus C., Cepanec C., Pessayre D., Degoul F. The Ala16Val genetic dimorphism modulates the import of human manganese superoxide dismutase into rat liver mitochondria. Pharm. Genom. 2003;13:145–157. doi: 10.1097/01.fpc.0000054067.64000.8f. [DOI] [PubMed] [Google Scholar]
- 34.Borgstahl G.E., Parge H.E., Hickey M.J., Beyer W.F., Jr., Hallewell R.A., Tainer J.A. The structure of human mitochondrial manganese superoxide dismutase reveals a novel tetrameric interface of two 4-helix bundles. Cell. 1992;71:107–118. doi: 10.1016/0092-8674(92)90270-M. [DOI] [PubMed] [Google Scholar]
- 35.Slot J.W., Geuze H.J., Freeman B.A., Crapo J.D. Intracellular localization of the copper-zinc and manganese superoxide dismutases in rat liver parenchymal cells. Lab. Investig. 1986;55:363–371. [PubMed] [Google Scholar]
- 36.Dhar S.K., St Clair D.K. Manganese superoxide dismutase regulation and cancer. Free Radic. Biol. Med. 2012;52:2209–2222. doi: 10.1016/j.freeradbiomed.2012.03.009. [DOI] [PubMed] [Google Scholar]
- 37.Hempel N., Melendez J.A. Intracellular redox status controls membrane localization of pro- and anti-migratory signaling molecules. Redox. Biol. 2014;2:245–250. doi: 10.1016/j.redox.2014.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kienhöfer J., Häussler D.J., Ruckelshausen F., Muessig E., Weber K., Pimentel D., Ullrich V., Bürkle A., Bachschmid M.M. Association of mitochondrial antioxidant enzymes with mitochondrial DNA as integral nucleoid constituents. FASEB J. 2009;23:2034–2044. doi: 10.1096/fj.08-113571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kim Y.S., Gupta Vallur P., Phaëton R., Mythreye K., Hempel N. Insights into the Dichotomous Regulation of SOD2 in Cancer. Antioxidants. 2017;6:86. doi: 10.3390/antiox6040086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sarsour E.H., Kalen A.L., Goswami P.C. Manganese superoxide dismutase regulates a redox cycle within the cell cycle. Antioxid. Redox Signal. 2014;20:1618–1627. doi: 10.1089/ars.2013.5303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Oberley L.W., Oberley T.D., Buettner G.R. Cell differentiation, aging and cancer: The possible roles of superoxide and superoxide dismutases. Med. Hypotheses. 1980;6:249–268. doi: 10.1016/0306-9877(80)90123-1. [DOI] [PubMed] [Google Scholar]
- 42.Oberley L.W., Oberley T.D., Buettner G.R. Cell division in normal and transformed cells: The possible role of superoxide and hydrogen peroxide. Med. Hypotheses. 1981;7:21–42. doi: 10.1016/0306-9877(81)90018-9. [DOI] [PubMed] [Google Scholar]
- 43.Zhong W., Oberley L.W., Oberley T.D., St Clair D.K. Suppression of the malignant phenotype of human glioma cells by overexpression of manganese superoxide dismutase. Oncogene. 1997;14:481–490. doi: 10.1038/sj.onc.1200852. [DOI] [PubMed] [Google Scholar]
- 44.Weydert C., Roling B., Liu J., Hinkhouse M.M., Ritchie J.M., Oberley L.W., Cullen J.J. Suppression of the malignant phenotype in human pancreatic cancer cells by the overexpression of manganese superoxide dismutase. Mol. Cancer Ther. 2003;2:361–369. [PubMed] [Google Scholar]
- 45.Sarsour E.H., Kumar M.G., Chaudhuri L., Kalen A.L., Goswami P.C. Redox control of the cell cycle in health and disease. Antioxid. Redox Signal. 2009;11:2985–3011. doi: 10.1089/ars.2009.2513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bravard A., Sabatier L., Hoffschir F., Ricoul M., Luccioni C., Dutrillaux B. SOD2: A new type of tumor-suppressor gene? Int. J. Cancer. 1992;51:476–480. doi: 10.1002/ijc.2910510323. [DOI] [PubMed] [Google Scholar]
- 47.Huang Y., He T., Domann F.E. Decreased expression of manganese superoxide dismutase in transformed cells is associated with increased cytosine methylation of the SOD2 gene. DNA Cell Biol. 1999;18:643–652. doi: 10.1089/104454999315051. [DOI] [PubMed] [Google Scholar]
- 48.Xu Y., Krishnan A., Wan X.S., Majima H., Yeh C.C., Ludewig G., Kasarskis E.J., St Clair D.K. Mutations in the promoter reveal a cause for the reduced expression of the human manganese superoxide dismutase gene in cancer cells. Oncogene. 1999;18:93–102. doi: 10.1038/sj.onc.1202265. [DOI] [PubMed] [Google Scholar]
- 49.Hodge D.R., Peng B., Pompeia C., Thomas S., Cho E., Clausen P.A., Marquez V.E., Farrar W.L. Epigenetic silencing of manganese superoxide dismutase (SOD-2) in KAS 6/1 human multiple myeloma cells increases cell proliferation. Cancer Biol. Ther. 2005;4:585–592. doi: 10.4161/cbt.4.5.1704. [DOI] [PubMed] [Google Scholar]
- 50.Hurt E.M., Thomas S.B., Peng B., Farrar W.L. Integrated molecular profiling of SOD2 expression in multiple myeloma. Blood. 2007;109:3953–3962. doi: 10.1182/blood-2006-07-035162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hitchler M.J., Wikainapakul K., Yu L., Powers K., Attatippaholkun W., Domann F.E. Epigenetic regulation of manganese superoxide dismutase expression in human breast cancer cells. Epigenetics. 2006;1:163–171. doi: 10.4161/epi.1.4.3401. [DOI] [PubMed] [Google Scholar]
- 52.Hu Y., Rosen D.G., Zhou Y., Feng L., Yang G., Liu J., Huang P. Mitochondrial manganese-superoxide dismutase expression in ovarian cancer: Role in cell proliferation and response to oxidative stress. J. Biol. Chem. 2005;280:39485–39492. doi: 10.1074/jbc.M503296200. [DOI] [PubMed] [Google Scholar]
- 53.Hempel N., Carrico P.M., Melendez J.A. Manganese superoxide dismutase (SOD2) and redox-control of signaling events that drive metastasis. Anticancer Agents Med. Chem. 2011;11:191–201. doi: 10.2174/187152011795255911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hempel N., Ye H., Abessi B., Mian B., Melendez J.A. Altered redox status accompanies progression to metastatic human bladder cancer. Free Radic. Biol. Med. 2009;46:42–50. doi: 10.1016/j.freeradbiomed.2008.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hanahan D., Weinberg R.A. Hallmarks of Cancer: The Next Generation. Cell. 2011;144:646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 56.Connor K.M., Hempel N., Nelson K.K., Dabiri G., Gamarra A., Belarmino J., Van De Water L., Mian B.M., Melendez J.A. Manganese superoxide dismutase enhances the invasive and migratory activity of tumor cells. Cancer Res. 2007;67:10260–10267. doi: 10.1158/0008-5472.CAN-07-1204. [DOI] [PubMed] [Google Scholar]
- 57.Hemachandra L.P., Shin D.H., Dier U., Iuliano J.N., Engelberth S.A., Uusitalo L.M., Murphy S.K., Hempel N. Mitochondrial Superoxide Dismutase Has a Protumorigenic Role in Ovarian Clear Cell Carcinoma. Cancer Res. 2015;75:4973–4984. doi: 10.1158/0008-5472.CAN-14-3799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hempel N., Bartling T.R., Mian B., Melendez J.A. Acquisition of the metastatic phenotype is accompanied by H2O2-dependent activation of the p130Cas signaling complex. Mol. Cancer Res. 2013;11:303–312. doi: 10.1158/1541-7786.MCR-12-0478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Rhodes D.R., Yu J., Shanker K., Deshpande N., Varambally R., Ghosh D., Barrette T., Pandey A., Chinnaiyan A.M. ONCOMINE: A cancer microarray database and integrated data-mining platform. Neoplasia. 2004;6:1–6. doi: 10.1016/S1476-5586(04)80047-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Cheng Y., Dai C., Zhang J. SIRT3-SOD2-ROS pathway is involved in linalool-induced glioma cell apoptotic death. Acta Biochim. Pol. 2017;64:343–350. doi: 10.18388/abp.2016_1438. [DOI] [PubMed] [Google Scholar]
- 61.Cobbs C.S., Levi D.S., Aldape K., Israel M.A. Manganese superoxide dismutase expression in human central nervous system tumors. Cancer Res. 1996;56:3192–3195. [PubMed] [Google Scholar]
- 62.Park C.K., Jung J.H., Moon M.J., Kim Y.Y., Kim J.H., Park S.H., Kim C.Y., Paek S.H., Kim D.G., Jung H.W., et al. Tissue expression of manganese superoxide dismutase is a candidate prognostic marker for glioblastoma. Oncology. 2009;77:178–181. doi: 10.1159/000231888. [DOI] [PubMed] [Google Scholar]
- 63.Zhong W., Yan T., Lim R., Oberley L.W. Expression of superoxide dismutases, catalase, and glutathione peroxidase in glioma cells. Free Radic. Biol. Med. 1999;27:1334–1345. doi: 10.1016/S0891-5849(99)00181-1. [DOI] [PubMed] [Google Scholar]
- 64.Dhar S.K., Tangpong J., Chaiswing L., Oberley T.D., St Clair D.K. Manganese superoxide dismutase is a p53-regulated gene that switches cancers between early and advanced stages. Cancer Res. 2011;71:6684–6695. doi: 10.1158/0008-5472.CAN-11-1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Minig V., Kattan Z., van Beeumen J., Brunner E., Becuwe P. Identification of DDB2 protein as a transcriptional regulator of constitutive SOD2 gene expression in human breast cancer cells. J. Biol. Chem. 2009;284:14165–14176. doi: 10.1074/jbc.M808208200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zou X., Santa-Maria C.A., O’Brien J., Gius D., Zhu Y. Manganese Superoxide Dismutase Acetylation and Dysregulation, Due to Loss of SIRT3 Activity, Promote a Luminal B-Like Breast Carcinogenic-Permissive Phenotype. Antioxid. Redox Signal. 2016;25:326–336. doi: 10.1089/ars.2016.6641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hart P.C., Ratti B.A., Mao M., Ansenberger-Fricano K., Shajahan-Haq A.N., Tyner A.L., Minshall R.D., Bonini M.G. Caveolin-1 regulates cancer cell metabolism via scavenging Nrf2 and suppressing MnSOD-driven glycolysis. Oncotarget. 2016;7:308–322. doi: 10.18632/oncotarget.5687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ennen M., Minig V., Grandemange S., Touche N., Merlin J.L., Besancenot V., Brunner E., Domenjoud L., Becuwe P. Regulation of the high basal expression of the manganese superoxide dismutase gene in aggressive breast cancer cells. Free Radic. Biol. Med. 2011;50:1771–1779. doi: 10.1016/j.freeradbiomed.2011.03.013. [DOI] [PubMed] [Google Scholar]
- 69.Govatati S., Malempati S., Saradamma B., Divyamaanasa D., Naidu B.P., Bramhachari P.V., Narayana N., Shivaji S., Bhanoori M., Tamanam R.R., et al. Manganese-superoxide dismutase (Mn-SOD) overexpression is a common event in colorectal cancers with mitochondrial microsatellite instability. Tumour. Biol. 2016;37:10357–10364. doi: 10.1007/s13277-016-4918-0. [DOI] [PubMed] [Google Scholar]
- 70.Miar A., Hevia D., Muñoz-Cimadevilla H., Astudillo A., Velasco J., Sainz R.M., Mayo J.C. Manganese superoxide dismutase (SOD2/MnSOD)/catalase and SOD2/GPx1 ratios as biomarkers for tumor progression and metastasis in prostate, colon, and lung cancer. Free Radic. Biol. Med. 2015;85:45–55. doi: 10.1016/j.freeradbiomed.2015.04.001. [DOI] [PubMed] [Google Scholar]
- 71.Sun G.G., Wang Y.D., Chen L.Q., Wang S.J., Liu G.L., Yu X.R., Cheng Y.J., Liu Q. Novel cancer suppressor gene for esophageal cancer: Manganese superoxide dismutase. Dis. Esophagus. 2011;24:346–353. doi: 10.1111/j.1442-2050.2010.01149.x. [DOI] [PubMed] [Google Scholar]
- 72.Oberley L.W., Bize I.B., Sahu S.K., Leuthauser S.W., Gruber H.E. Superoxide dismutase activity of normal murine liver, regenerating liver, and H6 hepatoma. J. Natl. Cancer Inst. 1978;61:375–379. [PubMed] [Google Scholar]
- 73.Ren T., Zhang H., Wang J., Zhu J., Jin M., Wu Y., Guo X., Ji L., Huang Q., Zhang H., et al. MCU-dependent mitochondrial Ca(2+) inhibits NAD(+)/SIRT3/SOD2 pathway to promote ROS production and metastasis of HCC cells. Oncogene. 2017;36:5897–5909. doi: 10.1038/onc.2017.167. [DOI] [PubMed] [Google Scholar]
- 74.Liu G., Zhou W., Park S., Wang L.I., Miller D.P., Wain J.C., Lynch T.J., Su L., Christiani D.C. The SOD2 Val/Val genotype enhances the risk of nonsmall cell lung carcinoma by p53 and XRCC1 polymorphisms. Cancer. 2004;101:2802–2808. doi: 10.1002/cncr.20716. [DOI] [PubMed] [Google Scholar]
- 75.Yu W., Denu R.A., Krautkramer K.A., Grindle K.M., Yang D.T., Asimakopoulos F., Hematti P., Denu J.M. Loss of SIRT3 Provides Growth Advantage for B Cell Malignancies. J. Biol. Chem. 2016;291:3268–3279. doi: 10.1074/jbc.M115.702076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Walker G.J., Palmer J.M., Walters M.K., Nancarrow D.J., Parsons P.G., Hayward N.K. Simple tandem repeat allelic deletions confirm the preferential loss of distal chromosome 6q in melanoma. Int J. Cancer. 1994;58:203–206. doi: 10.1002/ijc.2910580210. [DOI] [PubMed] [Google Scholar]
- 77.Konstantinopoulos P.A., Spentzos D., Fountzilas E., Francoeur N., Sanisetty S., Grammatikos A.P., Hecht J.L., Cannistra S.A. Keap1 mutations and Nrf2 pathway activation in epithelial ovarian cancer. Cancer Res. 2011;71:5081–5089. doi: 10.1158/0008-5472.CAN-10-4668. [DOI] [PubMed] [Google Scholar]
- 78.Hurt E.M., Thomas S.B., Peng B., Farrar W.L. Molecular consequences of SOD2 expression in epigenetically silenced pancreatic carcinoma cell lines. Br. J. Cancer. 2007;97:1116–1123. doi: 10.1038/sj.bjc.6604000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Pandit H., Zhang W., Li Y., Agle S., Li X., Li S.P., Cui G., Martin R.C. Manganese superoxide dismutase expression is negatively associated with microRNA-301a in human pancreatic ductal adenocarcinoma. Cancer Gene Ther. 2015;22:481–486. doi: 10.1038/cgt.2015.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Wheatley-Price P., Asomaning K., Reid A., Zhai R., Su L., Zhou W., Zhu A., Ryan D.P., Christiani D.C., Liu G. Myeloperoxidase and superoxide dismutase polymorphisms are associated with an increased risk of developing pancreatic adenocarcinoma. Cancer. 2008;112:1037–1042. doi: 10.1002/cncr.23267. [DOI] [PubMed] [Google Scholar]
- 81.Lewis A., Du J., Liu J., Ritchie J.M., Oberley L.W., Cullen J.J. Metastatic progression of pancreatic cancer: Changes in antioxidant enzymes and cell growth. Clin. Exp. Metastasis. 2005;22:523–532. doi: 10.1007/s10585-005-4919-7. [DOI] [PubMed] [Google Scholar]
- 82.Xu Y., Fang F., Zhang J., Josson S., St Clair W.H., St Clair D.K. miR-17* suppresses tumorigenicity of prostate cancer by inhibiting mitochondrial antioxidant enzymes. PLoS ONE. 2010;5:e14356. doi: 10.1371/journal.pone.0014356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Gao Y.H., Li C.X., Shen S.M., Li H., Chen G.Q., Wei Q., Wang L.S. Hypoxia-inducible factor 1α mediates the down-regulation of superoxide dismutase 2 in von Hippel-Lindau deficient renal clear cell carcinoma. Biochem. Biophys. Res. Commun. 2013;435:46–51. doi: 10.1016/j.bbrc.2013.04.034. [DOI] [PubMed] [Google Scholar]
- 84.Zhao Z., Azadzoi K.M., Choi H.P., Jing R., Lu X., Li C., Wang F., Lu J., Yang J.H. LC-MS/MS Analysis Unravels Deep Oxidation of Manganese Superoxide Dismutase in Kidney Cancer. Int. J. Mol. Sci. 2017;18:319. doi: 10.3390/ijms18020319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Liu X., Yu J., Jiang L., Wang A., Shi F., Ye H., Zhou X. MicroRNA-222 regulates cell invasion by targeting matrix metalloproteinase 1 (MMP1) and manganese superoxide dismutase 2 (SOD2) in tongue squamous cell carcinoma cell lines. Cancer Genom. Proteom. 2009;6:131–139. [PMC free article] [PubMed] [Google Scholar]
- 86.Liu Z., He Q., Ding X., Zhao T., Zhao L., Wang A. SOD2 is a C-myc target gene that promotes the migration and invasion of tongue squamous cell carcinoma involving cancer stem-like cells. Int. J. Biochem. Cell Biol. 2015;60:139–146. doi: 10.1016/j.biocel.2014.12.022. [DOI] [PubMed] [Google Scholar]
- 87.Kamarajugadda S., Cai Q., Chen H., Nayak S., Zhu J., He M., Jin Y., Zhang Y., Ai L., Martin S.S., et al. Manganese superoxide dismutase promotes anoikis resistance and tumor metastasis. Cell Death Dis. 2013;4:e504. doi: 10.1038/cddis.2013.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Izutani R., Asano S., Imano M., Kuroda D., Kato M., Ohyanagi H. Expression of manganese superoxide dismutase in esophageal and gastric cancers. J. Gastroenterol. 1998;33:816–822. doi: 10.1007/s005350050181. [DOI] [PubMed] [Google Scholar]
- 89.Ye H., Wang A., Lee B.S., Yu T., Sheng S., Peng T., Hu S., Crowe D.L., Zhou X. Proteomic based identification of manganese superoxide dismutase 2 (SOD2) as a metastasis marker for oral squamous cell carcinoma. Cancer Genom. Proteom. 2008;5:85–94. [PMC free article] [PubMed] [Google Scholar]
- 90.Malafa M., Margenthaler J., Webb B., Neitzel L., Christophersen M. MnSOD expression is increased in metastatic gastric cancer. J. Surg. Res. 2000;88:130–134. doi: 10.1006/jsre.1999.5773. [DOI] [PubMed] [Google Scholar]
- 91.Gulubova M., Vlaykova T. Expression of the xenobiotic- and reactive oxygen species-detoxifying enzymes, GST-pi, Cu/Zn-SOD, and Mn-SOD in the endocrine cells of colorectal cancer. Int. J. Colorectal. Dis. 2010;25:1397–1405. doi: 10.1007/s00384-010-1041-3. [DOI] [PubMed] [Google Scholar]
- 92.Quirós I., Sáinz R.M., Hevia D., García-Suárez O., Astudillo A., Rivas M., Mayo J.C. Upregulation of manganese superoxide dismutase (SOD2) is a common pathway for neuroendocrine differentiation in prostate cancer cells. Int. J. Cancer. 2009;125:1497–1504. doi: 10.1002/ijc.24501. [DOI] [PubMed] [Google Scholar]
- 93.Tsanou E., Ioachim E., Briasoulis E., Damala K., Charchanti A., Karavasilis V., Pavlidis N., Agnantis N.J. Immunohistochemical expression of superoxide dismutase (MnSOD) anti-oxidant enzyme in invasive breast carcinoma. Histol. Histopathol. 2004;19:807–813. doi: 10.14670/hh-19.807. [DOI] [PubMed] [Google Scholar]
- 94.Salzman R., Kanková K., Pácal L., Tomandl J., Horáková Z., Kostrica R. Increased activity of superoxide dismutase in advanced stages of head and neck squamous cell carcinoma with locoregional metastases. Neoplasma. 2007;54:321–325. [PubMed] [Google Scholar]
- 95.Kahlos K., Anttila S., Asikainen T., Kinnula K., Raivio K.O., Mattson K., Linnainmaa K., Kinnula V.L. Manganese superoxide dismutase in healthy human pleural mesothelium and in malignant pleural mesothelioma. Am. J. Respir Cell Mol. Biol. 1998;18:570–580. doi: 10.1165/ajrcmb.18.4.2943. [DOI] [PubMed] [Google Scholar]
- 96.Skrzycki M., Scibior D., Podsiad M., Czeczot H. Activity and protein level of CuZnSOD and MnSOD in benign and malignant liver tumors. Clin. Biochem. 2008;41:91–96. doi: 10.1016/j.clinbiochem.2007.09.014. [DOI] [PubMed] [Google Scholar]
- 97.Holley A.K., Kiningham K.K., Spitz D.R., Edwards D.P., Jenkins J.T., Moore M.R. Progestin stimulation of manganese superoxide dismutase and invasive properties in T47D human breast cancer cells. J. Steroid Biochem. Mol. Biol. 2009;117:23–30. doi: 10.1016/j.jsbmb.2009.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Siemankowski L.M., Morreale J., Briehl M.M. Antioxidant defenses in the TNF-treated MCF-7 cells: Selective increase in MnSOD. Free Radic. Biol. Med. 1999;26:919–924. doi: 10.1016/S0891-5849(98)00273-1. [DOI] [PubMed] [Google Scholar]
- 99.Whitsett J.A., Clark J.C., Wispé J.R., Pryhuber G.S. Effects of TNF-alpha and phorbol ester on human surfactant protein and MnSOD gene transcription in vitro. Am. J. Physiol. 1992;262:L688–L693. doi: 10.1152/ajplung.1992.262.6.L688. [DOI] [PubMed] [Google Scholar]
- 100.Szlosarek P., Charles K.A., Balkwill F.R. Tumour necrosis factor-alpha as a tumour promoter. Eur. J. Cancer. 2006;42:745–750. doi: 10.1016/j.ejca.2006.01.012. [DOI] [PubMed] [Google Scholar]
- 101.Josson S., Xu Y., Fang F., Dhar S.K., St Clair D.K., St Clair W.H. RelB regulates manganese superoxide dismutase gene and resistance to ionizing radiation of prostate cancer cells. Oncogene. 2006;25:1554–1559. doi: 10.1038/sj.onc.1209186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Pani G., Colavitti R., Bedogni B., Fusco S., Ferraro D., Borrello S., Galeotti T. Mitochondrial superoxide dismutase: A promising target for new anticancer therapies. Curr Med. Chem. 2004;11:1299–1308. doi: 10.2174/0929867043365297. [DOI] [PubMed] [Google Scholar]
- 103.Kinugasa H., Whelan K.A., Tanaka K., Natsuizaka M., Long A., Guo A., Chang S., Kagawa S., Srinivasan S., Guha M., et al. Mitochondrial SOD2 regulates epithelial–mesenchymal transition and cell populations defined by differential CD44 expression. Oncogene. 2015;34:5229–5239. doi: 10.1038/onc.2014.449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Ranganathan A.C., Nelson K.K., Rodriguez A.M., Kim K.H., Tower G.B., Rutter J.L., Brinckerhoff C.E., Huang T.T., Epstein C.J., Jeffrey J.J., et al. Manganese superoxide dismutase signals matrix metalloproteinase expression via H2O2-dependent ERK1/2 activation. J. Biol. Chem. 2001;276:14264–14270. doi: 10.1074/jbc.M100199200. [DOI] [PubMed] [Google Scholar]
- 105.Zhang H.J., Zhao W., Venkataraman S., Robbins M.E., Buettner G.R., Kregel K.C., Oberley L.W. Activation of matrix metalloproteinase-2 by overexpression of manganese superoxide dismutase in human breast cancer MCF-7 cells involves reactive oxygen species. J. Biol. Chem. 2002;277:20919–20926. doi: 10.1074/jbc.M109801200. [DOI] [PubMed] [Google Scholar]
- 106.Dinney C.P., Fishbeck R., Singh R.K., Eve B., Patha.a.ak S., Brown N., Xie B., Fan D., Bucana C.D., Fidler I.J., et al. Isolation and characterization of metastatic variants from human transitional cell carcinoma passaged by orthotopic implantation in athymic nude mice. J. Urol. 1995;154:1532–1538. doi: 10.1016/S0022-5347(01)66923-4. [DOI] [PubMed] [Google Scholar]
- 107.Wenk J., Brenneisen P., Wlaschek M., Poswig A., Briviba K., Oberley T.D., Scharffetter-Kochanek K. Stable overexpression of manganese superoxide dismutase in mitochondria identifies hydrogen peroxide as a major oxidant in the AP-1-mediated induction of matrix-degrading metalloprotease-1. J. Biol. Chem. 1999;274:25869–25876. doi: 10.1074/jbc.274.36.25869. [DOI] [PubMed] [Google Scholar]
- 108.Nelson K.K., Ranganathan A.C., Mansouri J., Rodriguez A.M., Providence K.M., Rutter J.L., Pumiglia K., Bennett J.A., Melendez J.A. Elevated SOD2 activity augments matrix metalloproteinase expression: Evidence for the involvement of endogenous hydrogen peroxide in regulating metastasis. Clin. Cancer Res. 2003;9:424–432. [PubMed] [Google Scholar]
- 109.Guo D., Wang Q., Li C., Wang Y., Chen X. VEGF stimulated the angiogenesis by promoting the mitochondrial functions. Oncotarget. 2017;8:77020. doi: 10.18632/oncotarget.20331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Nelson K.K., Subbaram S., Connor K.M., Dasgupta J., Ha X.F., Meng T.C., Tonks N.K., Melendez J.A. Redox-dependent matrix metalloproteinase-1 expression is regulated by JNK through Ets and AP-1 promoter motifs. J. Biol. Chem. 2006;281:14100–14110. doi: 10.1074/jbc.M601820200. [DOI] [PubMed] [Google Scholar]
- 111.Nelson K.K., Melendez J.A. Mitochondrial redox control of matrix metalloproteinases. Free Radic. Biol. Med. 2004;37:768–784. doi: 10.1016/j.freeradbiomed.2004.06.008. [DOI] [PubMed] [Google Scholar]
- 112.Gialeli C., Theocharis A.D., Karamanos N.K. Roles of matrix metalloproteinases in cancer progression and their pharmacological targeting. FEBS J. 2011;278:16–27. doi: 10.1111/j.1742-4658.2010.07919.x. [DOI] [PubMed] [Google Scholar]
- 113.Toole B.P. Hyaluronan-CD44 Interactions in Cancer: Paradoxes and Possibilities. Clin. Cancer Res. 2009;15:7462–7468. doi: 10.1158/1078-0432.CCR-09-0479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Maehara K., Uekawa N., Isobe K. Effects of histone acetylation on transcriptional regulation of manganese superoxide dismutase gene. Biochem. Biophys. Res. Commun. 2002;295:187–192. doi: 10.1016/S0006-291X(02)00646-0. [DOI] [PubMed] [Google Scholar]
- 115.Jung C., Rong Y., Doctrow S., Baudry M., Malfroy B., Xu Z. Synthetic superoxide dismutase/catalase mimetics reduce oxidative stress and prolong survival in a mouse amyotrophic lateral sclerosis model. Neurosci. Lett. 2001;304:157–160. doi: 10.1016/S0304-3940(01)01784-0. [DOI] [PubMed] [Google Scholar]
- 116.Patel M., Day B.J. Metalloporphyrin class of therapeutic catalytic antioxidants. Trends Pharmacol. Sci. 1999;20:359–364. doi: 10.1016/S0165-6147(99)01336-X. [DOI] [PubMed] [Google Scholar]
- 117.Rong Y., Doctrow S.R., Tocco G., Baudry M. EUK-134, a synthetic superoxide dismutase and catalase mimetic, prevents oxidative stress and attenuates kainate-induced neuropathology. Proc. Natl. Acad. Sci. USA. 1999;96:9897–9902. doi: 10.1073/pnas.96.17.9897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Salvemini D., Riley D.P., Cuzzocrea S. SOD mimetics are coming of age. Nat. Rev. Drug Discov. 2002;1:367–374. doi: 10.1038/nrd796. [DOI] [PubMed] [Google Scholar]
- 119.Weydert C.J., Zhang Y., Sun W., Waugh T.A., Teoh M.L., Andringa K.K., Aykin-Burns N., Spitz D.R., Smith B.J., Oberley L.W. Increased oxidative stress created by adenoviral MnSOD or CuZnSOD plus BCNU (1,3-bis(2-chloroethyl)-1-nitrosourea) inhibits breast cancer cell growth. Free Radic. Biol.Med. 2008;44:856–867. doi: 10.1016/j.freeradbiomed.2007.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Zhang Y., Gu J., Zhao L., He L., Qian W., Wang J., Wang Y., Qian Q., Qian C., Wu J., et al. Complete elimination of colorectal tumor xenograft by combined manganese superoxide dismutase with tumor necrosis factor-related apoptosis-inducing ligand gene virotherapy. Cancer Res. 2006;66:4291–4298. doi: 10.1158/0008-5472.CAN-05-1834. [DOI] [PubMed] [Google Scholar]
- 121.Huang P., Feng L., Oldham E.A., Keating M.J., Plunkett W. Superoxide dismutase as a target for the selective killing of cancer cells. Nature. 2000;407:390–395. doi: 10.1038/35030140. [DOI] [PubMed] [Google Scholar]
- 122.Pelicano H., Feng L., Zhou Y., Carew J.S., Hileman E.O., Plunkett W., Keating M.J., Huang P. Inhibition of mitochondrial respiration: A novel strategy to enhance drug-induced apoptosis in human leukemia cells by a reactive oxygen species-mediated mechanism. J. Biol. Chem. 2003;278:37832–37839. doi: 10.1074/jbc.M301546200. [DOI] [PubMed] [Google Scholar]
- 123.Irani K., Xia Y., Zweier J.L., Sollott S.J., Der C.J., Fearon E.R., Sundaresan M., Finkel T., Goldschmidt-Clermont P.J. Mitogenic signaling mediated by oxidants in Ras-transformed fibroblasts. Science. 1997;275:1649–1652. doi: 10.1126/science.275.5306.1649. [DOI] [PubMed] [Google Scholar]
- 124.Vafa O., Wade M., Kern S., Beeche M., Pandita T.K., Hampton G.M., Wahl G.M. c-Myc can induce DNA damage, increase reactive oxygen species, and mitigate p53 function: A mechanism for oncogene-induced genetic instability. Mol. Cell. 2002;9:1031–1044. doi: 10.1016/S1097-2765(02)00520-8. [DOI] [PubMed] [Google Scholar]
- 125.Sattler M., Verma S., Shrikhande G., Byrne C.H., Pride Y.B., Winkler T., Greenfield E.A., Salgia R., Griffin J.D. The BCR/ABL Tyrosine Kinase Induces Production of Reactive Oxygen Species in Hematopoietic Cells *. J. Biol. Chem. 2000;275:24273–24278. doi: 10.1074/jbc.M002094200. [DOI] [PubMed] [Google Scholar]
- 126.Trachootham D., Zhou Y., Zhang H., Demizu Y., Chen Z., Pelicano H., Chiao P.J., Achanta G., Arlinghaus R.B., Liu J., et al. Selective killing of oncogenically transformed cells through a ROS-mediated mechanism by beta-phenylethyl isothiocyanate. Cancer Cell. 2006;10:241–252. doi: 10.1016/j.ccr.2006.08.009. [DOI] [PubMed] [Google Scholar]
- 127.Trachootham D., Alexandre J., Huang P. Targeting cancer cells by ROS-mediated mechanisms: A radical therapeutic approach? Nat. Rev. Drug Discov. 2009;8:579–591. doi: 10.1038/nrd2803. [DOI] [PubMed] [Google Scholar]
- 128.Xiao D., Lew K.L., Zeng Y., Xiao H., Marynowski S.W., Dhir R., Singh S.V. Phenethyl isothiocyanate-induced apoptosis in PC-3 human prostate cancer cells is mediated by reactive oxygen species-dependent disruption of the mitochondrial membrane potential. Carcinogenesis. 2006;27:2223–2234. doi: 10.1093/carcin/bgl087. [DOI] [PubMed] [Google Scholar]
- 129.Dancey J.E. Therapeutic targets: MTOR and related pathways. Cancer Biol. Ther. 2006;5:1065–1073. doi: 10.4161/cbt.5.9.3175. [DOI] [PubMed] [Google Scholar]
- 130.Pópulo H., Lopes J.M., Soares P. The mTOR signalling pathway in human cancer. Int. J. Mol. Sci. 2012;13:1886–1918. doi: 10.3390/ijms13021886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Bhaskar P.T., Hay N. The two TORCs and Akt. Dev. Cell. 2007;12:487–502. doi: 10.1016/j.devcel.2007.03.020. [DOI] [PubMed] [Google Scholar]
- 132.Hay N. The Akt-mTOR tango and its relevance to cancer. Cancer Cell. 2005;8:179–183. doi: 10.1016/j.ccr.2005.08.008. [DOI] [PubMed] [Google Scholar]
- 133.Nogueira V., Hay N. Molecular pathways: Reactive oxygen species homeostasis in cancer cells and implications for cancer therapy. Clin. Cancer Res. 2013;19:4309–4314. doi: 10.1158/1078-0432.CCR-12-1424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Harrington L.S., Findlay G.M., Lamb R.F. Restraining PI3K: mTOR signalling goes back to the membrane. Trends Biochem. Sci. 2005;30:35–42. doi: 10.1016/j.tibs.2004.11.003. [DOI] [PubMed] [Google Scholar]
- 135.Pilarsky C., Wenzig M., Specht T., Saeger H.D., Grützmann R. Identification and validation of commonly overexpressed genes in solid tumors by comparison of microarray d.data. Neoplasia. 2004;6:744–750. doi: 10.1593/neo.04277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Park H.J., Carr J.R., Wang Z., Nogueira V., Hay N., Tyner A.L., Lau L.F., Costa R.H., Raychaudhuri P. FoxM1, a critical regulator of oxidative stress during oncogenesis. EMBO J. 2009;28:2908–2918. doi: 10.1038/emboj.2009.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Halasi M., Gartel A.L. Suppression of FOXM1 sensitizes human cancer cells to cell death induced by DNA-damage. PLoS ONE. 2012;7:e31761. doi: 10.1371/journal.pone.0031761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Bhat U.G., Halasi M., Gartel A.L. FoxM1 is a general target for proteasome inhibitors. PLoS ONE. 2009;4:e6593. doi: 10.1371/journal.pone.0006593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Radhakrishnan S.K., Bhat U.G., Hughes D.E., Wang I.C., Costa R.H., Gartel A.L. Identification of a chemical inhibitor of the oncogenic transcription factor forkhead box M1. Cancer Res. 2006;66:9731–9735. doi: 10.1158/0008-5472.CAN-06-1576. [DOI] [PubMed] [Google Scholar]
- 140.Cai W., Zhang B., Duan D., Wu J., Fang J. Curcumin targeting the thioredoxin system elevates oxidative stress in HeLa cells. Toxicol. Appl. Pharm. 2012;262:341–348. doi: 10.1016/j.taap.2012.05.012. [DOI] [PubMed] [Google Scholar]
- 141.Leong P.K., Chiu P.Y., Ko K.M. Prooxidant-induced glutathione antioxidant response in vitro and in vivo: A comparative study between schisandrin B and curcumin. Biol. Pharm. Bull. 2012;35:464–472. doi: 10.1248/bpb.35.464. [DOI] [PubMed] [Google Scholar]
- 142.Ravindran J., Subbaraju G.V., Ramani M.V., Sung B., Aggarwal B.B. Bisdemethylcurcumin and structurally related hispolon analogues of curcumin exhibit enhanced prooxidant, anti-proliferative and anti-inflammatory activities in vitro. Biochem. Pharmacol. 2010;79:1658–1666. doi: 10.1016/j.bcp.2010.01.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Yeh S.L., Huang C.S., Hu M.L. Lycopene enhances UVA-induced DNA damage and expression of heme oxygenase-1 in cultured mouse embryo fibroblasts. Eur. J. Nutr. 2005;44:365–370. doi: 10.1007/s00394-004-0536-5. [DOI] [PubMed] [Google Scholar]
- 144.Oboh G., Ademiluyi A.O., Akinyemi A.J. Inhibition of acetylcholinesterase activities and some pro-oxidant induced lipid peroxidation in rat brain by two varieties of ginger (Zingiber officinale) Exp. Toxicol. Pathol. 2012;64:315–319. doi: 10.1016/j.etp.2010.09.004. [DOI] [PubMed] [Google Scholar]
- 145.Lee E., Surh Y.J. Induction of apoptosis in HL-60 cells by pungent vanilloids, [6]-gingerol and [6]-paradol. Cancer Lett. 1998;134:163–168. doi: 10.1016/S0304-3835(98)00253-5. [DOI] [PubMed] [Google Scholar]
- 146.Chan T., Galati G., O’Brien P.J. Oxygen activation during peroxidase catalysed metabolism of flavones or flavanones. Chem. Biol. Interact. 1999;122:15–25. doi: 10.1016/S0009-2797(99)00103-9. [DOI] [PubMed] [Google Scholar]
- 147.Schiffman S.C., Li Y., Martin R.C. The association of manganese superoxide dismutase expression in Barrett’s esophageal progression with MnTBAP and curcumin oil therapy. J. Surg. Res. 2012;176:535–541. doi: 10.1016/j.jss.2011.11.1013. [DOI] [PubMed] [Google Scholar]
- 148.Aggarwal B.B., Shishodia S., Takada Y., Banerjee S., Newman R.A., Bueso-Ramos C.E., Price J.E. Curcumin suppresses the paclitaxel-induced nuclear factor-kappaB pathway in breast cancer cells and inhibits lung metastasis of human breast cancer in nude mice. Clin. Cancer Res. 2005;11:7490–7498. doi: 10.1158/1078-0432.CCR-05-1192. [DOI] [PubMed] [Google Scholar]
- 149.Yasui Y., Hosokawa M., Mikami N., Miyashita K., Tanaka T. Dietary astaxanthin inhibits colitis and colitis-associated colon carcinogenesis in mice via modulation of the inflammatory cytokines. Chem. Biol. Interact. 2011;193:79–87. doi: 10.1016/j.cbi.2011.05.006. [DOI] [PubMed] [Google Scholar]
- 150.Manju V., Nalini N. Chemopreventive efficacy of ginger, a naturally occurring anticarcinogen during the initiation, post-initiation stages of 1,2 dimethylhydrazine-induced colon cancer. Clin. Chim. Acta. 2005;358:60–67. doi: 10.1016/j.cccn.2005.02.018. [DOI] [PubMed] [Google Scholar]
- 151.Wei L., Zhou Y., Qiao C., Ni T., Li Z., You Q., Guo Q., Lu N. Oroxylin A inhibits glycolysis-dependent proliferation of human breast cancer via promoting SIRT3-mediated SOD2 transcription and HIF1α destabilization. Cell Death Dis. 2015;6:e1714. doi: 10.1038/cddis.2015.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Nelson S.K., Bose S.K., Grunwald G.K., Myhill P., McCord J.M. The induction of human superoxide dismutase and catalase in vivo: A fundamentally new approach to antioxidant therapy. Free Radic. Biol. Med. 2006;40:341–347. doi: 10.1016/j.freeradbiomed.2005.08.043. [DOI] [PubMed] [Google Scholar]
- 153.Liu J., Gu X., Robbins D., Li G., Shi R., McCord J.M., Zhao Y. Protandim, a fundamentally new antioxidant approach in chemoprevention using mouse two-stage skin carcinogenesis as a model. PLoS ONE. 2009;4:e5284. doi: 10.1371/journal.pone.0005284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Shin H.J., Kwon H.K., Lee J.H., Anwar M.A., Choi.i S. Etoposide induced cytotoxicity mediated by ROS and ERK in human kidney proximal tubule cells. Sci. Rep. 2016;6:34064. doi: 10.1038/srep34064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Evens A.M., Lecane P., Magda D., Prachand S., Singhal S., Nelson J., Miller R.A., Gartenhaus R.B., Gordon L.I. Motexafin gadolinium generates reactive oxygen species and induces apoptosis in sensitive and highly resistant multiple myeloma cells. Blood. 2005;105:1265–1273. doi: 10.1182/blood-2004-03-0964. [DOI] [PubMed] [Google Scholar]
- 156.Zhang Q., Ma Y., Cheng Y.-F., Li W.-J., Zhang Z., Chen S.-Y. Involvement of reactive oxygen species in 2-methoxyestradiol-induced apoptosis in human neuroblastoma cells. Cancer Lett. 2011;313:201–210. doi: 10.1016/j.canlet.2011.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Ruiz-Ojeda F.J., Gomez-Llorente C., Aguilera C.M., Gil A., Rupérez A.I. Impact of 3-Amino-1,2,4-Triazole (3-AT)-Derived Increase in Hydrogen Peroxide Levels on Inflammation and Metabolism in Human Differentiated Adipocytes. PLoS ONE. 2016;11:e0152550. doi: 10.1371/journal.pone.0152550. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no new data or datasets were created, generated, or analyzed in this study.