Abstract
The unique ability to adapt and thrive in inhospitable, stressful tumor microenvironments (TME) also renders cancer cells resistant to traditional chemotherapeutic treatments and/or novel pharmaceuticals. Cancer cells exhibit extensive metabolic alterations involving hypoxia, accelerated glycolysis, oxidative stress, and increased extracellular ATP that may activate ancient, conserved prion adaptive response strategies that exacerbate multidrug resistance (MDR) by exploiting cellular stress to increase cancer metastatic potential and stemness, balance proliferation and differentiation, and amplify resistance to apoptosis. The regulation of prions in MDR is further complicated by important, putative physiological functions of ligand-binding and signal transduction. Melatonin is capable of both enhancing physiological functions and inhibiting oncogenic properties of prion proteins. Through regulation of phase separation of the prion N-terminal domain which targets and interacts with lipid rafts, melatonin may prevent conformational changes that can result in aggregation and/or conversion to pathological, infectious isoforms. As a cancer therapy adjuvant, melatonin could modulate TME oxidative stress levels and hypoxia, reverse pH gradient changes, reduce lipid peroxidation, and protect lipid raft compositions to suppress prion-mediated, non-Mendelian, heritable, but often reversible epigenetic adaptations that facilitate cancer heterogeneity, stemness, metastasis, and drug resistance. This review examines some of the mechanisms that may balance physiological and pathological effects of prions and prion-like proteins achieved through the synergistic use of melatonin to ameliorate MDR, which remains a challenge in cancer treatment.
Keywords: melatonin, prions, cancer multidrug resistance, tumor microenvironment, liquid–liquid phase separation, hypoxia, pH, heme iron, band 3, copper
1. Introduction
The symptom of prion protein infection was first described in 1732 when Merino sheep scraped pathologically against fences [1], but the term prion (PRoteinaceous Infective ONly particle) was not coined until 1982 by Prusiner who defined prions in 1998 as heritable, infectious, proteinaceous particles that are converted from the normal, cellular form (PrPC) into the pathogenic form (PrPSc) that associates with amyloid plaques [2,3]. The full-length prion protein (PrP) [4] exists as a native, soluble cellular PrPC isoform with important physiological functions [5] including cellular differentiation [6,7,8], proliferation [9], and adhesion [10]; myelin maintenance [11]; circadian rhythm regulation [12,13]; signal transduction [14]; glucose homeostasis [15,16]; immune regulation [17,18]; as well as copper homeostasis, utilization [19,20]; iron uptake, transport, and metabolism [21,22,23]; and even facilitating the persistence and storage of memory [24,25]. In humans, quantitative transcriptomics analysis (RNA-Seq) of 27 different tissues obtained from 95 human individuals [26] found the prion gene PRNP to be ubiquitously expressed in all 27 human tissues examined in addition to mitochondria, with the highest expressions found in the brain, followed by the ovary, prostate, heart, gallbladder, endometrium, adrenal, urinary bladder, thyroid, testis, skin, esophagus, and lung [27]. Cellular PrPC has since been identified in brain mitochondria of wild-type and transgenic mice in the absence of disease [28]. After Masison and Wickner discovered the prion protein in Saccharomyces cerevisiae [29], increased understanding of prion physiological and pathological functions began to converge on the “prion hypothesis”, where non-Mendelian, protein-based, epigenetic inheritance in prions is proposed to be the essential driving force behind prion propagation [30,31,32,33,34,35,36,37,38,39].
Prion-based inheritance of conformationally-encoded phenotype information may allow genetically identical cells to express diverse, adaptive phenotypes with distinct evolutionary advantages [39,40,41,42]. The study of prions in yeast reveals a unique “bet-hedging” feature [43,44] where cells form reversible prion colonies that can readily adapt to changing stress conditions in the environment. Cells with phenotypes created by prions may survive with a fitness advantage that is lost in cells without prions. Prion proteins allow yeast cells to adapt instantaneously to changing environments where frequency of phenotype gain/loss is dictated by the level of stress in the environment [45]. The fact that prions are often overexpressed in invasive, drug-resistant cancers highlights the important connection between the “prion hypothesis” and cancer MDR [46].
Tumor cells adapt to stressful environmental pressure including anti-cancer therapies by remodeling signaling pathways involving transcription, translation, and posttranslational modifications [47]. Tumor heterogeneity and plasticity are formidable challenges to overcome in drug resistance [48]. Reversibility of phenotypes in both cancer cells and prions allows the speedy addition or removal of genetic traits as adaptations to environmental stress [49]. It is perhaps not a coincidence that the spontaneous phenotype shifts in a highly metastatic murine fibrosarcoma cell line (KHT), observed to be approximately 10−5 per cell per generation [50], matches the 10−5 per cell per generation frequency of phenotype alterations from de novo prion formation reported in haploid S. cerevisiae strains [51]. Even though phenotype alterations may be reversible in both metastatic melanoma cells [52] and yeast prions [44,53], the reversible “curability” of [URE3]—the prion form of Ure2 protein in haploid yeast first observed by Wickner in 1994—was actually a reflection of the temporary inactivation by guanidinium (a curing agent) of the conversion of Ure2 into the altered [URE3] prion form, which then promptly repopulated itself under selective conditions [30]. Mutations or overexpression of Ure2 can increase the conversion into prion [URE3] by 1000-fold [30,51].
Prions are often overexpressed in many forms of cancer [54,55,56], and the prion protein gene (PRNP) was detected by means of in silico analysis to be mutated in some cancer patients [57]. The ability of prions to enhance cancer proliferation, invasion, metastasis, increase stemness, and promote resistance to cytotoxic therapeutics has been extensively reviewed [55,58,59,60,61,62,63,64,65,66,67,68,69,70,71]. Since prion expression and conversion from the normal, soluble state to the pathogenic, aggregate form can be induced by stress [72], it is not surprising that prions are associated with MDR in many types of cancer [73,74,75] including gastric cancer [76], breast cancer [77], glioblastoma multiforme [78], and colorectal cancer [79], whereas silencing prion protein expression re-sensitizes breast cancer cells to adriamycin [80] and colorectal cancer cells to fucoidan [81]. Results from two randomized trials that evaluated the expression of PrPC protein in normal breast and breast cancer tissues from 756 ER-negative breast cancer patients revealed a significant correlation with resistance to adjuvant chemotherapy in ER-negative disease [82]. The overexpression of PrPC in cancer may be an innate, adaptive response conferring survival advantage reflecting evolutionary selection pressure [46,83].
Many anticancer drugs including cisplatin [84,85], doxorubicin [86], and temozolomide [87] exert their oncostatic efficacy by elevating production of reactive oxygen species (ROS) to enhance oxidative damage. The fact that PrPC enhances clinical resistance to cisplatin in colorectal cancer cell [88] and increases invasiveness and resistance to doxorubicin-induced apoptosis in LS 174T colon cancer cells [89] supports the theory that PrPC serves important physiological functions [5] including antioxidant protection [90]. PrPC was observed to defend against ROS-induced DNA damage in human neuroblastoma SH-SY5Y cells [91] while 1C11 cells from PrPnull C57BL/6J mice displayed a 50% increase in ROS combined with a reduction in major antioxidant systems, including reduced glutathione (GSH) [92]. Some of the antioxidant effects associated with PrPC depend on its ability to bind metal ions such as copper. The octarepeat peptide region in the unstructured N-terminal domain of PrPC contains histidine residues that possess high binding affinity to copper and can form complexes with doxorubicin to significantly lower drug efficacy [93,94]. PrPC interaction with temozolomide in glioma resulting in drug resistance may also be related to copper-binding effects [95,96].
The study of melatonin as an anti-cancer adjuvant [97,98,99] and oncostatic agent capable of inhibiting cancer metastasis while enhancing drug efficacy has been extensively documented and reviewed [100,101,102,103,104,105,106,107,108,109,110,111,112]. However, the interactions between melatonin and prions in cancer are not straightforward. For example, melatonin upregulates PrPC expression to protect mesenchymal stem cells (MSCs) against ischaemic injury [113] but inhibits PrPC expression to cause apoptosis in colorectal cancer cells [114]. When used in combination with anti-cancer drugs such as oxaliplatin and 5-fluorouracil (5-FU), melatonin becomes even more effective in inducing apoptosis and senescence in 5-FU-resistant colon stem cells and oxaliplatin-resistant colorectal cancer cells by suppressing PrPC expression [115,116]. Yet melatonin was also reported to protect MSCs harvested from chronic kidney disease (CKD) mouse models against H2O2-induced senescence by upregulating PrPC expression [113].
The seemingly contradictory, pleiotropic interactions between melatonin and prions actually reflect a delicate balance pivoted upon their intrinsic, natural response to stress. PrPC has recently been demonstrated to protect animals from acute, inflammatory lipopolysaccharide (LPS, Escherichia coli O26:B6) challenge by modulating the expression of immune response genes [117]. Similarly, in MSCs treated with LPS-stimulated macrophages, the addition of 1 μM (but not 0.1, 10, or 100 μM) melatonin upregulated PrPC expression and produced a maximal effect in conferring resistance against oxidative stress by enhancing MSC proliferation [118]. Conversely, using 2 mM melatonin (2000-fold increase) in LPS-stimulated prostate cancer cells inhibited migration and invasion [119]; the addition of 1 mM melatonin also inhibited cellular prion protein expression to promote apoptosis via superoxide-mediated oxidative stress in colorectal cancer cells [114]. It is plausible that at appropriately high concentrations, melatonin modulates the inhospitable, highly stressful tumor microenvironment (TME) to attenuate elevated PrPC stress responses that may activate the conversion into pathological, self-templating aggregates, whereas lower levels support the natural, physiological protective reactions of prions under duress. The conversion of PrPC into self-templating aggregates is now believed to be associated with liquid–liquid phase separation (LLPS), which is an energy-efficient thermodynamic process that results in the rapid formation and dissolution of biomolecular condensates used by living organisms as adaptation to changing environments [120,121,122,123,124]. Living organisms may have always relied upon melatonin to effectively modulate prion propagation using unique features including the regulation of liquid–liquid phase separation [125].
2. Liquid–Liquid Phase Separation May Regulate Prion Conversion and Propagation
Melatonin (N-acetyl-5-methoxytryptamine) is extensively studied for its potent antioxidant cascading reactions which continue to generate effective free radical scavenging metabolites while interacting with different ROS [126,127,128,129,130,131,132,133,134,135]. Since its discovery in the bovine pineal gland in 1958 [136], melatonin is now understood to be mainly produced in mitochondria in all present-day vertebrates [137,138,139]. The early, successful distribution of melatonin via horizontal gene transfers may accentuate the preponderant reliance on this ancient molecule for protection against endogenous and exogenous stress in all eukaryotes and bacteria tested [140,141,142,143,144]. Similar to the induction of prions in yeast as a response to stress, unfavorable exogenous or endogenous conditions such as oxidative stress, nutrient deprivation, and fluctuations in temperature and pH also induce increased production of melatonin in plants [145,146,147,148] and animals [149,150,151,152,153]. It has been proposed that a high reserve/maximum capacity of melatonin synthesis in humans provides a higher level of survival fitness as effective adaptation to unpredicted internal and external environmental stressors while enhancing recovery rates from injury and external pathogenic attacks [154,155]. Since S. cerevisiae can produce varying levels of melatonin under different nutritional and environmental conditions [156,157,158] and absorb exogenous melatonin in an oxidative stress-dependent manner [159,160], it is possible that living organisms may have evolved the ability to adjust appropriate levels of melatonin during stress exposure to support PrPC physiological functions while restraining pathological conformational changes as part of stress adaptation including exposure to lethal doses of ultraviolet (UV) irradiation.
2.1. Melatonin May Modulate Stress-Induced Prion Conversion
The pathological prion PrPSc isoform is extremely resistant to inactivation by UV radiation at 254 nm with doses up to 120,000 J/m2 [161,162]. Cellular PrPC expression is often increased in neuroblastoma, breast, and colorectal cancer cell lines after ionizing radiation treatment, and suppressing PrPC can reduce radioresistance in tumor cells [163]. S. cerevisiae pretreated with melatonin were enriched in a dose-dependent manner and were protected from H2O2-induced oxidative stress as well as exposure to 254 nm UV irradiation with increased cell viability via dynamic modulation of antioxidant genes [160]. Even though melatonin is radio-protective [164], it can also increase radiosensitivity when used as adjuvant with radiotherapy to substantially improved tumor remission, 1-year survival, and alleviation of radiochemotherapy-related cytotoxic effects [61,165,166] such as the increased expression of heat shock protein 70 (Hsp70) [167,168]. Exposure to UV irradiation has been reported to elevate Hsp70 in yeast, human skin cells, murine fibroblasts and keratinocytes, as well as transgenic mouse models. Increased expression of Hsp70 is generally considered as protective [169,170,171,172], but the induction of Hsp70 also leads to increased expression of PrPC as part of the adaptive antioxidant responses.
Melatonin is a potent antioxidant that is produced in human skin, and UVB irradiation of human keratinocytes resulted in intensely elevated local melatonin metabolism that was dependent and directly proportional to UVR dose applied [173]. The use of 1 mM melatonin prevented DNA damage and suppression of antioxidant enzymes and proteins in UVR-treated ex vivo human skin [174]. More importantly, melatonin suppressed the upregulation of Hsp70 in human full-thickness skin and human epidermal keratinocytes exposed to UV radiation but complemented the suppression of Hsp70 by reversing all effects induced by Hsp70 inhibition such as enhanced gene expression of proinflammatory cytokines and proapoptotic proteins [175]. The suppression of Hsp70 by melatonin provides a glimpse into the complex interplay between melatonin and prions where living organisms may use melatonin as a “broad-based metabolic buffer” to tune prion propagation in response to stress.
Experimental studies on S. cerevisiae showed that excess Ssa1 of the Hsp70 family was responsible for the de novo formation of [PSI+] which is the pathological prion isoform of yeast release factor Sup35 [169]. Even though contradictory results were reported in a study where the use of 0.5 and 1.5 µM 17-(dimethylaminoethylamino)-17-demethoxygeldanamycin (17-DMAG) [176]—a semi-synthetic derivative of the antibiotic geldanamycin—strongly induced Hsp70 expression in a rabbit kidney epithelial (RK13) cell line but significantly decreased PrPSc accumulation, the authors also acknowledged the completely unanticipated in vivo results that showed an increase in PrPSc from interactions with normal brain homogenates (NBH) obtained from WT Hsp70+/+ control mice, whereas NBH substrates from Hsp-null (Hsp−/−) mice did not support the generation of any PrPSc [177]. The confounding observation may be explained by the fact that 17-DMAG is unable to induce Hsp70 at concentrations below 20 nM, but the half-maximal inhibitory concentration (IC50) at only 8 nM 17-DMAG could inhibit the formation of misfolded proteins and toxic aggregates in polyglutamine disorders such as Huntington’s disease [178]. Therefore, a 62.5 or 187.5-fold increase in the use of 17-DMAG may have suppressed PrPSc accumulation regardless of Hsp70 activation status. However, it is also possible that in vitro and in vivo results for 17-DMAG are totally different as 17-DMAG administered to sepsis-LPS animal models at 5 mg/kg increased expression of Hsp70, conferring antioxidant protection to increase survival rates [179] which may imply activation of PrPC by Hsp70.
The exposure of human NT-2 cells to heat (42 °C) simultaneously increased mRNA levels for both Hsp70 and PrP protein [180]. Most importantly, irradiation of human prion proteins at 302 nm caused complete structural unfolding with rapid precipitation and specific structural conversion into soluble β-sheeted oligomers with characteristics similar to structurally destabilized species that often precede pathological isoform aggregation [181]. However, the precipitation formed during UV irradiation entirely blocked UV transmission, implying that the original intention of aggregate formation is instinctively protective in nature [181]. It is now widely accepted that all living organisms depend upon the formation of dynamic, membraneless compartments in response to environmental changes. The balance between reversible and irreversible aggregation of these condensates during the process of liquid–liquid phase separation (LLPS) may be the linchpin that defines the fine line that separates health from disease [182].
2.2. The Intrinsically Disordered Region in Prions Is Requisite for Liquid–Liquid Phase Separation, Cytoplasmic Inheritance, and Modulation of Pathological Conversion
Biomolecular condensates are intracellular membraneless organelles (MLOs) that compartmentalize and organize proteins, ribonucleic acids (RNAs), and other nucleic acids [183]. In response to continuously changing endogenous or exogenous conditions, all living organisms including eukaryotes [184,185], prokaryotes [186,187], and archaea [188,189] depend on LLPS as the primary driver to fuel the condensation or dissolution of MLOs in rapid, energy-efficient reactions such as stress response [190], signal transduction [191,192], redox balance [193], as well as genome expression, organization and repair [194]. The canonical yeast translation termination factor Sup35, responsible for catalyzing translation termination during growth, contains an evolutionarily conserved, intrinsically disordered prion N-terminal domain that can phase separate under stress to form protective, reversible biomolecular condensates [124,195,196] which can restore cell growth functions upon termination of stress. However, the intrinsically disordered N-terminal region of Sup35 can also phase separate to form irreversible heritable aggregates that are the prion isoforms [PSI+] responsible for generating heritable phenotypic variations as part of stress adaptation [124,197,198].
Proteins with intrinsically-disordered prion or prion-like domains, which are often highly enriched in nucleic acid binding proteins but may be prone to the formation of fibrillar assemblies, are widely conserved across evolution and are accepted to be the source for protein-based cytoplasmic inheritance essential in the formation of new, opportunistic, adaptive traits that ensure survival in hostile environments [39,196,199,200]. Within the Saccharomyces proteome, intrinsically disordered proteins capable of LLPS are often located in the nucleus and are involved in the regulation of transcription and cell signaling [201]. Thus, the formation of reversible condensates rather than irreversible aggregates in response to stress may have been a primary function of prions and prion-like domains that serve as stress sensors and adaptors. Sup35 in many yeast species actually do not have the ability to form [PSI+] prions [202,203]. By contrast, intrinsically disordered regions (IDRs) in prion-like domains, which easily phase separate and form dynamic condensates, are highly conserved across all three domains of life—eukaryotes, prokaryotes, and archaea—as well as viruses [204,205,206,207,208,209]. LLPS of IDRs in proteins enables the rapid formation of membraneless organelles without mechanical barriers but are distinctly segregated by chemical boundaries [210,211]. However, phase separation at its core is an entropically unfavorable thermodynamic process requiring a reduction or a negative change in global free energy enabled by energetically favorable multivalent protein–protein interactions that can offset energetic costs [183,212,213].
2.2.1. The Role of ATP and RNA in Prion Phase Separation
Thermodynamic nonequilibrium processes, such as posttranslational modification (PTM) involving the hydrolysis of adenosine triphosphate, which can induce free energy changes of −7.3 kcal/mol, can facilitate the exchange of substrates and information between condensates in their native and droplet states during LLPS [214,215,216,217]. Adenosine triphosphate (ATP) at micromolar concentration provides free energy to fuel phase separation by generating supersaturation gradients inducing droplet segregation [212,218,219]. However, ATP can also function as a biological hydrotrope at physiological concentrations from ~2 to 8 mM, solubilizing abnormal, pathological aggregates often associated with neurodegenerative disorders [220,221,222,223,224]. ATP is a universal and specific biphasic modulator of LLPS in IDRs, altering physicochemical properties, conformation dynamics, assembly, and aggregation [225]. More recently, ATP has been proposed to be a kosmotropic anion behaving like a “biological aggregation inhibitor” that can increase protein stability and reduce thermal aggregation [223,226,227].
Experimental studies revealed that LLPS can promote the spontaneous conversion of human and mouse recombinant prion protein (rPrP) into the pathological PK-resistant PrPres isoform without involving kinetic energy or seeding from PrPSc. However, the conversion process was dependent upon interactions between the intrinsically disordered N-terminal domain and kosmotropic anions [121]. Incubating kosmotropic anions with recombinant PrP elevates protein stability, inducing misfolding into PrPSc amyloid-like aggregates [228]. Yet the efficiency of droplet formation via LLPS did not exactly match with the Hofmeister series [121,229]. It is possible that interactions between ATP, which has recently been proposed to be a kosmotropic anion [226], and RNA can vitally influence the outcome of LLPS of prions and prion-like domains. Recent experimental results reported the ratio between the negatively-charged ATP and RNA can affect aggregation and dissolution where ATP competitively binds to condensate-forming proteins in IDRs to inhibit RNA-driven phase separation of the proteins [230].
Ribonucleic acid (RNA)—a single-stranded molecule with alternating ribose and phosphate groups attached to adenine, uracil, cytosine or guanine bases—is an essential architectural component that can influence the composition and morphological outcome of condensate phases in LLPS [231], as well as regulate spatiotemporal distribution of MLOs by fine-tuning biophysical properties such as viscosity and internal molecular dynamics [232]. RNA modulates condensate formation during LLPS due to the high negative charge densities buried in the phosphate backbones. As a result, phase separation can be promoted by a low level of negatively charged RNA molecules interacting with positively charged proteins, whereas high levels of RNA may repel the same proteins to dissolve condensates [233,234]. In essence, the IDRs of prions and prion-like domains drive phase separation and the assembly of condensates while RNA can regulate the dynamics of those condensates [235], potentially stimulating conversion of PrPC into PrPSc [236,237,238]. ATP is one of the four nucleotide monomers required for RNA synthesis [239,240]. The intricate relationship between ATP and RNA may extend as far back as the highly-debated “RNA world” [241,242,243] when ATP was an integral energy-providing component of a metabolic system composed of nucleic acid enzymes, which is believed to precede the evolution of ribosomal protein synthesis [244,245].
Prions and prion-like molecules have likely assumed central roles in early chemical evolutionary processes preceding the Last Universal Common Ancestor (LUCA), which eventually resulted in present-day living systems [246,247]. The ability of prions to efficiently replace their non-aggregate native state by assembling short peptides into β-sheet amyloid aggregates with high structural stability and resistance to hostile, extreme environments may have facilitated self-replication, catalytic activities, and analogical information transfer in protein-based, self-propagating, information-processing biomolecules in early life forms ~3.9 billion years ago [248,249,250]. The phase behavior of the prion-forming protein Sup35 PrD in yeast is critically modulated by stress. Exposing Sup35 PrD to 10 mM arsenite promoted droplet formation in 93% of treated cells, whereas only 30% of untreated cells formed droplets [251]. Although the formation of non-infectious, self-assembled macromolecular complexes represents a vital physiological function, these assemblies are highly susceptible to the formation of pathological aggregates that are now associated with cancer [252,253,254] and neurodegenerative disorders. Cancer is now recognized as a disease that may result from aberrant LLPS and aggregation of MLOs [252,255,256,257,258,259,260,261,262]. Wild-type human tumor suppressor protein p53 expressed in yeast undergoes LLPS induced by multivalent interactions between its intrinsically disordered N- and C-termini to form unstable droplets that dissolve quickly when stress is removed. However, when overexpressed, the p53 protein lost tumor-suppressing transcription ability, forming aggregates that behaved in a comparable manner to stable, heritable prions [263,264,265].
2.2.2. RNA- and Copper-Binding Modulate the Conversion of PrPC to PrPSc
The regulation of prion functionality and conversion into toxic aggregates may be fundamentally propelled by LLPS [120,121,122,123], and the intrinsically disordered N-terminal region of the physiological PrPC has been shown to be necessary and sufficient for LLPS of PrP [266,267]. Large nucleation barriers enable deep supersaturation that favors the formation of toxic aggregates in Sup PrD while kinetic barriers for the formation of dynamic intracellular condensates are easily breached by PTMs and changes in salt, pH, and temperature during LLPS [251,268,269]. Nevertheless, fluctuations in RNA concentrations can modulate prion aggregation in a bimodal, concentration-dependent manner where high protein to RNA ratios stimulate aggregation and low ratios suppress condensate formation. RNAs of different sources and lengths were reported to markedly alter rPrP aggregation in a concentration-dependent manner [270]. Even though prions are understood to reside in lipid rafts on plasma membranes [271,272], prions found in cytosol of neuronal and non-neuronal cells form ribonucleoprotein (RNP) complexes similar to membraneless RNA granules or chromatoid bodies containing mRNAs, and RNA proteins including the DEAD-box RNA helicase DDX6 and other non-coding RNA, small nuclear RNA, and microRNAs. The domain located between residues 30 and 49 in the intrinsically disordered N-terminal is necessary for the assembly of these PrP-RNP granules, which is believed to have important functions in RNA processing and posttranscriptional gene regulation, and are different from other cytosolic prion-containing aggresomes previously observed [273,274,275,276]. However, when overexpressed, cytosolic PrP in neurons can exhibit toxicity in certain cell populations [277].
PrPC replication environment depleted of RNA gave rise to a completely new strain of PrPSc without changing PrP primary structure [278]. Mutations in residues can increase binding of RNA to specific sites in PrPC, facilitating the formation of a pincer motif that leads to the decay of the N-terminal α-helix, which is a requisite step in the hastened conversion of PrPC to the toxic, infectious PrPSc isoform [279,280]. Experimental studies showed that mutant peptides may exhibit greater resistance to cancer drugs such as cisplatin as a result of weakened adduct binding affinity. Although increasing the cisplatin ratio to 2:1 facilitated adduct binding, it was still ineffective in preventing aggregation [281], whereas truncated variants of rPrP lacking octarepeat peptides in the N-terminal domain were less susceptible to aggregation [270]. In fact, neutralizing mutations can considerably reduce cytotoxicity from amyloid fibril formation in the prion-prone peptide PrP 106–126 belonging to the intrinsically disordered N-terminal domain [282]. Perhaps not coincidentally, MDR in gastric cancer is associated with four of the five copper-binding octarepeat peptides located within the N-terminal domain. Mutant gastric cancer cells constructed from gene splicing lacking octarepeat peptides (residues ~51–91) exhibited highly decreased anti-apoptotic capacity and lowered antioxidant responses to stress [283,284].
Prion protein antioxidant defense is specifically mediated by ROS cleavage and copper-binding in the octarepeat peptide region in the N-terminal domain [285,286,287]. Copper is an essential trace element used in all domains of life as a structural component for proteins and as cofactor in catalytic oxidation-reduction (redox) reactions that can result in the production of ROS [288]. Binding of copper (Cu(II), Cu2+) to PrPC facilitates redox balance and copper homeostasis [289] both of which are often disturbed in the TME where cancer drug resistance is associated with higher serum copper levels in patients compared to healthy controls or patients who responded to chemotherapy [290,291]. Copper also changes the conformation of the N-terminal domain [292,293,294,295], which may impede LLPS [121,296] or even prevent the formation of straight β-strands backbone structures in the infectious PrPSc form when bound to the non-octarepeat peptides (residues 92–96) [297,298]. However, the Cu2+ inhibition of amyloid formation is dependent upon binding capacity that becomes less effective at a lower pH [93,299], which is characteristic of most TMEs. In addition, under physiological conditions, Cu2+ bound to full-length, uncleaved PrP can induce misfolding that increases seeding, which serves as templates for aggregation [300,301]. Melatonin is not only a potent antioxidant capable of chelating copper and modulating ROS-dependent prion cleavage, but is also proposed to be an important regulator of phase separation [125].
2.3. The Role of Melatonin in the Regulation of Liquid–Liquid Phase Separation and ROS-Induced Cleavage in Prions
Phase separation is an evolutionarily conserved response used by living organisms to assemble biomolecular condensates as efficient adaptation to rapidly changing endogenous or exogenous stressors [190,196]. The formation of condensates during LLPS is a process of nucleation and growth constrained by an energy barrier that can usually be breached by thermodynamic nonequilibrium PTMs [269,302]. Many well-known targets of melatonin including NLRP3 inflammasome [303,304,305] and tumor suppressor protein p53 [306,307,308] contain prion-like IDRs that facilitate LLPS [265,309,310,311] and are regulated by ATP-dependent PTMs such as phosphorylation, ubiquitination, and SUMOylation [312,313,314,315,316,317], while DEAD-box RNA helicases such as DDX3X, which are tuned by RNA and ATP [318], can critically determine the outcome of prionoid LLPS in NLRP3 [310]. Posttranslational modification of PrPC initiates and/or propagates PrPSc aggregates [319,320], profoundly altering prion assembly pathways [321] to produce new strains with different protein conformations in vivo [322]. The addition of a single, fully-charge phosphate group at pH 7.5 to various locations in human peptide sequence corresponding to residues 59–71 from the intrinsically disordered N-terminal domain inhibited fibril formation, whereas phosphorylation of the same peptides at pH 1.1, when the phosphate is fully protonated, caused rapid fibril formation [323].
Melatonin may efficiently mediate important PTMs that regulate proteins which can form physiological condensates or pathological prion-like aggregates due to its ability to protect mitochondrial and cytoplasmic ATP levels and maintain requisite RNA concentration, which not only ensure proper formation and dissolution of condensates [125] but possibly also modulate reentrant phase transitions that are important biochemical timekeeping RNA-dependent transformations where increased RNA dissolves condensates to return to an identical or macroscopically similar state before the phase transition [324]. Since prion targeting of lipid rafts [272,325,326] can affect membrane signaling [327,328] and lipid composition [329], the role of melatonin in the prevention of lipid peroxidation, modification of lipid hydrocarbon chain to promote phase separation in ternary membrane models [330,331], stabilizing lipid liquid ordered (Lo) to liquid disordered (Ld) phase separation over a range of temperatures [332], and displacing cholesterol in competitive binding to lipid molecules [330] provides additional insight into the complex relationship between melatonin and prion physiological and potential pathological conversion mediated by phase separation and associated processes.
2.3.1. The Role of Melatonin in PrPC LLPS and Amyloid Beta Binding
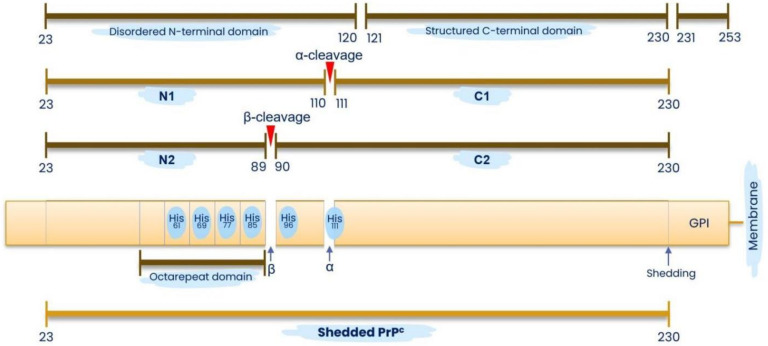
Cellular PrP contains 253 residues and is often bound to lipid rafts on membranes via glycosylphosphatidylinositol (GPI) anchors [272,333]. Residues 1 to 23 comprise the N-terminal signal peptide that is cleaved upon maturation; residues 23 to 120 comprise the positively charged, unstructured N-terminal domain; residues 121 to 230 comprise the structured C-terminal domain; and residues 231 to 253 comprise the GPI anchor signal [272,333,334,335] (Figure 1). PrPC is rich in α-helical content and can be converted into insoluble, non-infections proteinase K (PK)-resistant (PrPres) isoforms [121,336,337] or infectious, stable, PK-resistant PrPSc isoforms, rich in aggregation-prone β-sheet structures that are associated with detrimental, cytotoxic effects [2,335,337,338,339,340]. Early workers postulated that the misfolding of PrPC is the central mechanism governing the conversion to the toxic PrPSc isoform, and that the earliest event in prion misfolding involves metastable intermediates with aggregation-prone, β-sheet enriched structures [341,342,343,344].
Figure 1.
Schematic representation of the prion protein structure. Residues 1–23 comprise the N-terminal signal peptide that is cleaved upon maturation; residues 23–120 comprise the unstructured N-terminal domain; residues 121–230 comprise the structured C-terminal domain; and residues 231–253 comprise the GPI anchor signal tethered to lipid rafts on plasma membranes. α-cleavage of residues 110/111 yields N1 (residues 23–110) and C1 (residues 111–230) fragments while ROS-induced β-cleavage at residues 89/90 produces N2 (residues 23–89) and C2 (residues 90–230) fragments. Four histidine residues in the octarepeat domain and two histidine residues in the fifth nonoctarepeat binding site exhibit high-affinity to copper ions. Shedding by proteolysis of the GPI anchor at residues 230–231 releases a full-length, soluble PrPC (23–230).
Experimental studies in 2018 reported that PrPC undergoes LLPS at physiological pH and salinity, and can exist in multiple phases with extensive secondary structure rearrangement. LLPS of PrPC and N-terminal residues 23–110 (N1) could be triggered by excess amyloid-β oligomers (Aβo), resulting in the formation of reversible hydrogels with up to 300-fold Aβo enrichment. These Aβo/PrP hydrogels engaged signal-transducing metabotropic glutamate receptor mGluR5 and altered its cell surface mobility [345]. It was proposed that Aβo binding by soluble (anchor-free) prion protein and N-terminal fragments is a protective response [346] due to reports showing N1 strongly suppressed Aβo toxicity in vitro and attenuated Aβ-induced memory function in a mouse model in vivo, in addition to inhibiting the aggregation and assembly of Aβ(1–42) into amyloid fibrils, reducing neurotoxicity [347].
Aβo is a pathological ligand [348] often found to cluster at excitatory synapses with mGluR5 and PrPC, acting as a scaffold for mGluR5 to disrupt synaptic function and glutamate signaling [349,350,351]. The interactions between Aβo–PrPC and mGluR5 at the neuronal surface also activate the cytoplasmic Fyn tyrosine kinase to undermine neuronal functions and plasticity via increased intracellular calcium [352,353,354,355]. Fyn is associated with cancer pathogenesis and drug resistance and is often found to be upregulated in prostate cancer [356] and tamoxifen-resistant breast cancer cell lines [357]. In gastric cancer, Fyn is frequently overexpressed and is positively correlated with metastasis [358]. Not surprisingly, PrPC accelerates colon cancer metastasis via the Fyn-SP1-SATB1 axis [62]. The fact that melatonin can downregulate mGluR5 expression by diminishing Tet1 expression, which uncouples Tet1 from the mGluR5 promoter [359], modulating the PrPC/mGlur5/Fyn/Pyk2 pathway to alleviate Aβo neurotoxicity [360], casts a more favorable light upon PrPC LLPS-induced Aβo binding and cascading signaling effects, further highlighting the important role of melatonin in supporting PrPC physiological activities while ameliorating pathological consequences. In 2021, König et al. reported solid-state MAS NMR spectroscopy investigations of Aβ(1–42) oligomers complexed with huPrP represented a heterogeneous mixture of β-strand-rich assemblies where binding with PrPC effectively trapped Aβ oligomers and prevented further development into various fibril types, prompting the authors to speculate whether this feature was coincidental or is the original intended physiological function of PrPC [361]. Additional discoveries from recent experimental studies continue to deepen understanding of the complex relationship between prion LLPS, copper, the TME, and melatonin.
2.3.2. Is the N-1 Fragment from the Intrinsically Disordered N-1 Domain Necessary and Sufficient for LLPS?
The mature PrPC comprise two well-differentiated domains—a structured C-terminal (residues 121–231) and the unstructured N-terminal domain (residues 23–120) [333,362,363]. Within the N-terminal domain at residues 51–90, there are four octarepeats [364,365], which contain copper-binding histidines and a “pseudorepeat” lacking a histidine [333,363]. A fifth consensus copper-binding site can be found between residues 91 and 111 [363], which is an area known for amyloidogenic β-sheet formation coordinated by copper binding to His96 and His111 which results in structural plasticity changes involving “closed” or “open” conformations that are prion-resistant or prion-susceptible, respectively [366,367] (Figure 1). In addition to binding copper and other divalent metals such as nickel(II), zinc(II), and manganese(II), albeit with much lowered affinity [368], histidines in PrP and especially within the octarepeat peptides bind hemin where affinity increased with the number of histidines and length of the peptide [369]. The binding of copper to the four octarepeat peptides induces conformational changes that rapidly dissociate PrPC from lipid-rafts, laterally translocating the protein from detergent-resistant lipid rafts into detergent-soluble regions of plasma membranes before endocytosis through clathrin-coated pits or caveolae [326,370,371,372,373,374]. The region containing octarepeat peptides can also be dissociated from the membrane-bound prion protein via proteolytic or ROS-induced cleavage [375,376].
The constitutive, irreversible, posttranslational proteolytic α-cleavage of residues 110/111 in PrPC yields N1 (residues 23–110) and C1 (residues 111–230) fragments while ROS-induced β-cleavage at residues 89/90 produces N2 (residues 23–89) and C2 (residues 90–230) fragments [120,377,378,379,380] (Figure 1). The soluble N-terminal cleavage fragments become untethered while the C-terminal cleavage fragments remain bound to lipid rafts on membranes via GPI anchors [272,380,381]. Shedding by proteolysis releases a full-length, soluble PrPC (23–230) that is cleaved from the membrane GPI anchor around reside 230–231 and reduces the cytotoxicity of amyloid-β oligomers [379,382,383] (Figure 1). The nature and function of proteolytic cleavage of PrPC and perhaps even PrPSc [384,385] are yet to be fully elucidated, although it is postulated that proteolytic processing generates bioactive soluble prion protein fragments and induces conformational and functional changes to cell-bound prions [375,379,386].
Substantial evidence from experimental studies have shown that β-cleavage can also be induced by exposure to ROS (H2O2) but is dependent upon pH and Cu2+. Binding to copper facilitated β-cleavage by H2O2 in the octapeptide repeat region but the rate of cleavage was reduced when pH was lowered [376,387]. A higher level of α-cleavage in full-length PrPC producing more C1 fragments was correlated with better resistance to the propagation of PrPres [388], whereas deleting α-cleavage sites while retaining residues 23–31 produced toxic, lethal phenotypes [389]. However, biologically active N2 fragments (residues 23–89) from β-cleavage modulates cellular stress response [285], and deleting the octarepeat regions not only abolished ROS-mediated β-cleavage but also greatly reduced cell viability and increased intracellular free radicals from impaired glutathione peroxidase activity [390]. Both N1 and N2 cleavage fragments can also maintain neuronal stem cell quiescence by modulating ROS levels [391]. Cancer cell stemness contributes to MDR, and the ability to maintain stem cell pools in a quiescent, slow-growing state facilitates protection from antiproliferative drugs and evasion from immune surveillance to promote tumor development [392,393,394].
In February 2021, Tange et al. reported that at neutral pH 7.0, interactions between kosmotropic anions and N2 residues 23–89 in the N-terminal region of rPrP were most optimal in driving rPrP LLPS, forming gels that acquired conformational conversion into PK-resistant β-sheet–rich, non-seeding structures without the use of kinetic energy or PrPSc [121]. These findings support results from early experimental studies where kosmotropic anions promoted the conversion of rPrP into PrPSc-like aggregates [228]. However, Kamps et al. published their report later in 2021 showing that at physiological pH 7.4, N1, but not N2, underwent LLPS driven primarily by the polybasic motif in the postoctarepeat region containing an amyloid β-binding domain [266]. Interestingly, during their experiments, Tange et al. found the presence of copper inhibited LLPS [121], whereas Kamps et al. did not test the effect of copper on LLPS [266]. Even though copper binding to histidines in PrPC can induce conformational changes that could reduce potential toxicity effected by N-terminal with octarepeat sequences [294,300,377,395] but also impede LLPS, it is not inconceivable that the difference in pH of mediums used in the two studies in addition to the absence of copper and kosmotropic anions may offer a plausible explanation for LLPS observed in N2 [121,266].
2.3.3. Changing pH and/or Crossing Isoelectric Points Can Drive Phase Separation of Prion N2 Fragments
Under normal physiological conditions, the pH of the human body is maintained in a tight range between 7.35 and 7.45, with 7.40 accepted as the average physiological pH [396]. Changes in pH in an organism is a critical stress factor that can induce the formation of MLOs through LLPS [124,397,398]. Results from in vitro experimental studies demonstrate that changes in pH can trigger phase separation of stress sensing poly(A)-binding proteins in yeast to form hydrogels [190]. Under nutrient depletion, yeast cells are unable to regulate pH using proton pumps; the ensuing acidification triggers phase separation, reversibly transitioning the yeast cytoplasm from a fluid- to a solid-like, dormant state with reduced mobility [399]. Prions can undergo huge conformational changes below pH 7.2 when interacting with nucleic acids, forming large RNA–protein complexes in a pH-dependent manner [400,401], whereas increasing concentrations of chaotropic salts such as sodium chloride (NaCl) at pH 7.5 prevented the formation of RNA prion complexes [400,402]. Reducing pH can cause thermodynamic instability propelling the conversion of PrPC into PK-resistant isoforms by destabilization of salt bridges in nucleic acids and protonation of histidine residues in PrPC [403,404]. Conversely, increasing pH can cause histidine residues that serve as molecular switches in histidine-rich squid beak proteins (HBPs) to deprotonate and trigger phase separation [405]. pH jumps from pH 11.0 to pH 7.5 caused proteins kept in solution to quickly undergo LLPS to form droplets upon protonation at native pH. Decreasing pH is often used as an effective technique to induce LLPS in proteins without having to cross the isoelectric point of the proteins [406].
Phase separation can often be triggered as the pH moves close to a protein’s isoelectric point (pI), which is the pH value at which a molecule carries no net electrical charge where the negative and positive charges are equal or cancelled. Therefore, proteins will carry a net positive charge if the pH of the surrounding liquid medium is below their pI and a net negative charge if the surrounding pH is above their pI [407]. Experimental results indicate that phase separation frequently occurs at pH values corresponding to the protein’s isoelectric point at thermodynamic equilibrium, whereas cells are almost always under nonequilibrium conditions that may also affect phase separation [408]. Nonetheless, proteins were shown to be the least soluble near their pIs where solubility is affected by the increase in net charge, which may be proportional to increases or reductions in the surrounding pH [409], with the implication that a net charge of zero may induce protein aggregation. Testing of several disease-associated transmissible spongiform encephalopathies (TSEs) human prion proteins (PrPTSE) found their isoelectric points to be more acidic than pH 7 [410], which may explain why Tange et al. observed LLPS of N2 fragments at neutral pH in the presence of kosmotropic anions, and Kamps et al. were unable to induce LLPS of N2, which lacked the postoctarepeat region with the amyloid β-binding domain, at physiological pH 7.4 [121,266]. Copper-binding, which can interfere with LLPS, is also pH dependent.
2.3.4. Copper Chelation by Melatonin in Prion Phase Separation May Ameliorate Prion-Induced Multidrug Resistance
At neutral or physiological pH copper (Cu2+) is fully bound to histidine residues in the octarepeat and other regions of PrPC at a 1:1 ratio [411,412]. Reducing pH to 6.7 results in loss of binding by 50%, and further reductions to pH 6.0 completely inhibited binding [93], or led to dissociation of the Cu(II)-amide− bonds [411]. Although normally found bound to proteins, Cu(II) may be released and become free to catalyze the formation of highly reactive hydroxyl radicals inducing cellular toxicity [413,414]. Exchangeable copper (CuEXC) represents the labile fraction of copper complexed to albumin and other peptides but not within ceruloplasmin [415,416]. In the healthy individuals tested, CuEXC was found to be 0.57 to 1.12 μM, or 3.24% to 8.58% of total copper concentration in plasma [417], which is normally ~16.7 μM on average [418], whereas human and murine prions are almost fully saturated at 5 μM copper [419]. Copper is increasingly associated with the growth and proliferation of cancer cells and the promotion of breast cancer metastasis [420,421]. Thus, in environments below neutral pH—the hallmark of cancer TME—prions may not bind to copper completely, which then becomes a challenging situation in the context of cancer MDR.
Prions are copper-sensitive stress sensors that are activated upon copper-binding to initiate signal transduction processes that increase antioxidant enzyme activities and glutathione levels [19,422]. Exposure to Cu(II) was shown to increase the expression of PrPC in primary hippocampal and cortical neurons [423], and increased oxidative stress induced by intracellular Cu(II) quickly upregulated PrPC transcription mediated by ataxia-telangiectasia mutated (ATM) in murine neuro-2a and human HeLa cells [424]. In addition, ROS-mediated β-cleavage at residues 89/90, which produces N2 (residues 23–89) [379,425], is also copper- and pH-dependent, with the rate of cleavage at neutral pH diminishing with decreasing pH [376]. PrP mutants lacking the copper-binding octarepeat peptides could not undergo β-cleavage by ROS and displayed increased sensitivity to oxidative stress [390]. Hence, in an acidic extracellular environment favored by cancer cells, prion expression may be elevated due to increased oxidative stress from incomplete Cu(II) binding, which also results in suppressed antioxidant protection from copper-dependent ROS-mediated β-cleavage [390]. Increased oxidative stress and a lower pH will also trigger PrPC phase separation, which may lead to the aggregation of the pathological PK-resistant isoforms. Oxidative stress causes prion protein misfolding and a 900-fold increase in binding affinity, resulting in oligomerization that seeds aggregation [300]. In the aggregated, PK-resistant pathological state, the prion isoform can potentially facilitate non-Mendelian, epigenetic inheritance, which confers stress and drug-resistant survival features to cancer cells [40,426].
Melatonin is not only a highly efficient antioxidant that continues to generate effective free radical scavenging metabolites while interacting with different ROS [126,127,128,129,130,131,132,133,134,135], but also binds with copper in situ [427] and may exert protective effects against copper-induced toxicity in animals and plants potentially via chelation [428,429]. Under physiological conditions, in vitro and in vivo animal experiments found melatonin treatment at 1 mM and 50 mg/kg (intraperitoneal injection), respectively, decreased hydroxyl radical formation by high concentration of copper and pro-oxidant polyphenols, preventing DNA damage via copper chelation [430]. A theoretical study employing physicochemical analysis in 2015 proposed that under physiological pH 7.4, melatonin can chelate Cu(II) via the coupled-deprotonation-chelation mechanism (CDCM), with 3-hydroxymelatonin (3OHM) being the most effective metabolite for such purpose [431]. In 2019, computational studies simulating physiological mediums reported results that supported these findings. However, when comparing Gibbs free energies between melatonin complexes formed with various metals examined using the well-known metal-chelating agent ethylenediaminetetraacetic acid (EDTA) [432] as control, copper complexed with melatonin and principal metabolites showed the lowest Gibbs free energy values in the order of EDTA, AMK, 3OHM, melatonin, and AFMK, where EDTA- and AMK-Cu complexes exhibited the highest stabilities with the lowest Gibbs free energy at approximately −161 and −149, respectively [433].
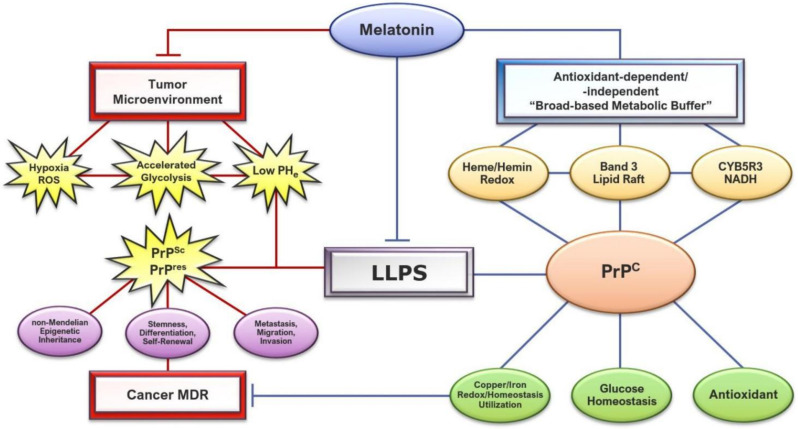
Considering the fact that deprotonation increases the chelation viability for Cu(II), reduced pH can, therefore, negatively impact melatonin’s ability to chelate copper [431]. However, it is perhaps not a coincidence that melatonin increases pH, restoring pH homeostasis to regulate prion phase separation, facilitate copper-binding, and modulate ROS-mediated cleavage via a reduction in oxidative stress through its potent antioxidant cascades [434]. Treating irradiated healthy and tumor-control Balb/c mice with melatonin (20 mg/kg) ameliorated oxidative stress in heart and lung tissues. However, melatonin administration increased superoxide dismutase (SOD) and glutathione peroxidase (GPx) antioxidant responses only in normal but not tumor cells [435]. It is plausible that by reducing ROS levels in oxidative TMEs, melatonin decreased PrPC expression, which in turn lowered antioxidant activities. Results from an in silico analysis demonstrated that the overexpression of PrPC under optimal culture conditions did not alter proliferation, resistance to cell death, and metabolism in colorectal cancer cell lines [436], and consequently, supported the hypothesis that the correlation between overexpression of PrPC, cancer malignancy, and MDR are actually results of a highly-stressed TME rather than outcomes being driven by PrPC overexpression. The ability of melatonin to act as a “broad-based metabolic buffer” which can tune prion propagation in response to stress signals becomes particularly significant in the context of TME and drug resistance (Figure 2).
Figure 2.
Schematic illustrating the regulation of prion protein phase separation by melatonin, attenuating conversions into infections, pathological PrPSc and non-infectious, insoluble PrPres isoforms, which may promote cancer multidrug resistance (MDR) via different mechanisms, including non-Mendelian epigenetic inheritance, stemness, metastasis, and resistance to apoptosis. By acting as a “broad-based metabolic buffer”, melatonin modulates the tumor microenvironment to control hypoxia and oxidative stress, ameliorating the effects of accelerated glycolysis and low extracellular pH (pHe) that can trigger the liquid–liquid phase separation (LLPS) of physiological prion (PrPC). Melatonin employs antioxidant-dependent and -independent features to protect heme redox and NADH levels; band 3, lipid raft, and CYB5R3 functionality; and, provides an optimal environment for prions to assume essential physiological functions including reduction in oxidative stress, maintenance of cellular energy homeostasis, and ensuring proper iron/copper redox/homeostasis and utilization, which may further enhance cancer drug sensitivity.
3. Melatonin May Promote PrP Physiological Functions and Inhibit Pathological Effects via Global Modulation of the Tumor Microenvironment to Enhance Cancer Drug Efficacy
One of the major metabolic adaptations employed by cancer cells is the “Warburg effect” where mitochondrial oxidative phosphorylation (OXPHOS) is suppressed in favor of accelerated aerobic glycolysis [437], producing a toxic tumor microenvironment (TME) characterized by high alkalinity in the cytosol and high acidity in the extracellular environment resulting in an elevated alkaline intracellular pH (pHi) but an acidic, reduced extracellular pH (pHe) that can promote oncogenic properties [438,439]. This reversed pH gradient is widely accepted as the hallmark of cancers [440,441]. Cancer cells have been associated with higher values of pHi between 7.12 and 7.65 and a lower pHe of ~6.2–6.9, whereas pHi in normal cells is stringently maintained at a narrow range between 7.0 and 7.2, and pHe at ~7.4 [442,443,444,445,446,447,448,449]. In normal cells, metabolic and developmental transitions are highly dependent upon changes in pHi [450,451,452] and in silico studies showed that alkaline pHi, which is coupled to accelerated glycolysis and adaptation to hypoxia, maximized cancer cell proliferation, whereas reversing the pHi to normal acidic values prevented adaptations, halting tumor cell growth [453]. An acidic pHe in the TME is directly correlated to deficient oxygen supply from rapid cancer cell division and growth.
Tumor hypoxia causes the metabolic shift towards acidity where proton (H+) accumulation is proportional to O2 levels [454]. Excess intracellular protons are often extruded into extracellular space via different mechanisms [455] including membrane transporters [456], carbonic anhydrase enzymes [457], and lysosomes [458], or sequestered in proton sinks [459]. The ensuing acidic pHe may directly interfere with the efficacy of weakly basic chemotherapeutic drugs by impeding their intracellular distribution through “ion trapping” [460]. While the combination of proton disequilibrium and reversed pH gradient act as positive feedback promoting metastasis that exacerbate cancer MDR [441,447,461,462,463], it is the fall in intracellular proton that is mainly responsible for accelerated glycolysis in cancer cells [464]. Since mitochondria ATP synthases are rapidly translocated to cell surface lipid rafts under tumor-like hypoxic and acidic environments [465,466,467], cancer cells can also rely on the internalization of extracellular ATP (eATP) to significantly elevate intracellular ATP (iATP) to enhance drug resistance by maintaining the energy requirement of drug efflux by ATP-binding cassette (ABC) transporters [468,469,470]. eATP has been associated with cancer cell migration and invasion [471,472], induction of epithelial-mesenchymal transition (EMT) to promote metastasis in lung cancer [473], and activation of cancer stem cell-like changes to promote metastasis in non-small-cell lung cancer [474].
3.1. Melatonin May Attenuate Prion Propagation and Cancer Multidrug Resistance by Increasing Extracellular pH
Extracellular acidification and hypoxia in melanoma cells can reprogram metabolism to enhance survival, invasiveness, and promote immunosuppressive environments that exacerbate drug resistance [475]. Hypoxia induces increased expression of cellular prion protein to enhance the viability of mesenchymal stem cells [476], and PrPC mRNA and protein levels were significantly upregulated (4.3-fold increase in luciferase activity) in gastric cancer cell lines exposed to hypoxia [59]. In fact, increased expression of PrPC in multicellular prostate tumor spheroids is regulated by redox to counterbalance increased oxidative stress through upregulated antioxidant defense [477]. Prion phase separation can be activated by cellular stress such as changes in pH and fluctuations in levels of kosmotropic anions including ATP [121,226,406,455] (see Section 2.2.1.). Biopsies from metastatic melanoma revealed elevated levels of amyloid-like aggregations [478], and amyloidogenic peptides were shown to incorporate ATP when aggregating into amyloid fibrils [479]. Increased eATP in addition to increased oxidative stress and reduced pHe in TME may exacerbate prion β-sheet conversions upon triggering of phase separation. Even though LLPS converted rPrP into the PK-resistant PrPres isoform, it is still unclear whether phase separation of PrPC is the primary cause for the conversion of PrPC into PrPSc. However, oxidative stress is increasingly associated with the conformational change in the α-helix structure of PrPC to the β-sheet structure of PrPSc [480,481,482,483]. It is not surprising that the migration of metastatic melanoma, which is dependent on acidic pHe, is promoted by the prion protein [67,484,485]. Experimental studies on skin reconstructed with melanoma cell lines found treatment with 1 mM melatonin controlled growth and impaired invasion and metastasis by disrupting cytoskeleton formation [486] while high-dose melatonin (5 mg/m2/day to 700 mg/m2/day) showed stable, favorable responses in human subjects diagnosed with advanced malignant melanoma [487]. Melatonin also prevented the aggressive phenotype shifts in breast cancer cell lines maintained under acidosis conditions by modulating proliferation and apoptosis [488]. Melatonin can exert inhibitory oncostatic effects due to its ability to regulate acid-base balance fluctuations, which are consequences of a hypoxic TME [454].
In vitro experimental studies showed that exposure of two human pancreatic cancer cell lines (MIA PaCa-2 and PANC-1) to 1 μM melatonin with continuous presence (including measurement) for 24 h stimulated the secretion of bicarbonate, rebalancing ion transport via modulating mRNA expression of pancreatic solute transporters SLC26A6, SLC4A4b, SLC9A1, and other non-genomic effects on acid-base transport that were not identified [489]. Expressed in all cells, carbonic anhydrases (CAs) are catalytic enzymes responsible for the reversible conversion of carbon dioxide (CO2) and water (H2O) into bicarbonate (HCO3−) and protons (H+) [490,491]. The CA isoforms CA-IX and CA-XII contribute to extracellular acidification and intracellular alkalinization in response to increased CO2 load under hypoxic conditions. The reversed pH gradient of increased pHi and reduced pHe is a major pro-survival mechanism used by cancer cells [492,493]. In vivo experiments showed that silencing of CA-IX led to a 40% reduction in xenograft tumor volume with up-regulation of CA-XII levels, whereas invalidation of both isoforms produced an impressive 85% reduction [494].
Melatonin treatment of triple negative human breast cancer cell line (MDA-MB-231) and female Balb/c xenograft mice at 1 mM and 40 mg/kg, respectively, showed slightly different results between gene expression and protein levels of CAs. Tumor samples from xenograft mice treated with high-dose melatonin exhibited significant downregulation of mRNA gene expression of CA-XII and markedly reduced protein levels of both CA-IX and CA-XII when compared to untreated controls, whereas in vitro results from cultured MDA-MB-231 cancer cells treated with 1 mM melatonin only showed a significant reduction in CA-XII gene expression, with an insignificant difference in protein levels of CA-IX and CA-XII between the melatonin-treated and control groups [495]. Since CA-IX and CA-XII are inducible by hypoxia, in the same study, melatonin also reduced gene expression and protein levels of hypoxia-inducible factor 1α (HIF-1α) in vitro and in vivo [495,496]. Reversed pH gradients with dysregulated acid-base balance in TME may be consequences of hypoxia where arterial hemoglobin desaturation and reduced O2 saturation can lower pHe to below 6.8 [497,498]. Low partial pressure of oxygen (pO2) can directly affect resistance to radiotherapy by limiting the ability of O2 to general free radicals to exert oxidative damage to macromolecules and membranes [447,499]. Reducing the affinity of hemoglobin for oxygen represented by a right-shift in the hemoglobin-oxygen dissociation curve [500,501] can drastically increase tumor radiosensitivity [502], whereas tumor hypoxia, by lowering pO2 which shifts the dissociation curve to the left, thereby increasing hemoglobin affinity to O2, is often associated with less effective radiation-mediated apoptosis and increased metastatic potential with poorer prognosis [503,504]. The fact that melatonin exerted higher efficacy in modulating pH in vivo may reflect the powerful, dynamic relationship with prions in the regulation of iron homeostasis and hemoglobin O2 saturation, which control hypoxia and the resulting pH imbalances that exacerbate cancer proliferation and MDR.
3.2. PrPC Protective Physiological Responses and Ligand-Binding May Become Pathological Liabilities in the Tumor Microenvironment
The tumor environment is uniquely adapted to promote cancer cell survival and proliferation. Elevated hypoxia from low oxygen tension produces low pH with increasing accumulation of protons (H+) resulting in the formation of excess ROS [454,505] and deficient energy supply are all high-stress conditions that may trigger phase separation survival responses [258,261,506] with potential to activate PrPC conversion to pathological templates that may promote cytoplasmic inheritance to increase survival rates [39,196,199,200]. PrPC was identified in the nucleus of NB4 human promyelocytic leukemia cell line [507], and also in the form of ‘granules’ in nuclei of uninfected bovine neuronal cells [508]. The fact that PrPC is abundantly localized in the nuclear lamina and interacts with structural chromatin components [509] supports the hypothesis of PrP epigenetic regulation where prions can facilitate inheritance of activated chromatin states to provide adaptive advantages [40,41]. PrPC identified in the nucleus of actively dividing normal epithelial cells was associated with the proliferation, differentiation, and subcellular distribution of architectural proteins [510]. In S. cerevisiae, prion-forming protein Sup35 PrD phase behavior is modulated by stress and energy depletion where droplet formation under arsenite stress and energy depletion was observed in 93% of cells examined [251]. The identification of LLPS in the nucleus further emphasizes the important role of PrPC conversion from stress-induced phase separation resulting in tumor cell genomic instability [511] and dysregulation of gene expressions [259].
Most of the physiological functions of PrP are dependent on complex interactions with its binding partners. The unstructured N-terminal domain between residues 23 and 120 contains an octapeptide repeat region (residues 51–90) and an amyloidogenic region between residues 90 and 120 involving histidines 96 and 111, which bind metals with a special high affinity for copper [272,294,367,412,512], while residues 23–90 of the unstructured N-terminal constitute a region that specifically targets to lipid rafts, and PrP with deleted N-terminal is unable to bind to lipid rafts [325]. The constitutive, tight association between PrPC and lipid rafts [326,513] and its wide expression in stem cells [8,514,515,516,517] offer additional insight as to how prions interact with membrane supramolecular complexes [518] to participate in an extensive range of physiological functions including transcription, scaffolding, and signaling [267], and modulate cancer stemness, differentiation, self-renewal, and proliferation to augment cancer MDR [65,71,77,516,519,520]. Although PrPC does not bind iron directly, the binding of Cu2+ in the N-terminal domain modulates iron metabolism through copper homeostasis [289]. Wild-type (WT) PrPC over-expression or deletion in specific mouse brain regions is associated with striking variations in levels of copper, iron, and even zinc [521]. PrPnull mice showed reduced iron mobilization, diminished serum iron content, and excess accumulation in liver and spleen as a result of impaired copper-dependent ceruloplasmin (ferroxidase) activity, which is responsible for the regulation of iron mobilization [522,523].
3.3. Interactions between PrPC, Iron, and Heme May Enhance Aggressive Drug Resistance in Tumors
Iron is required in essential metabolic processes [524], and PrP may perform important roles in iron uptake and transport [22]. Absence of PrP induces systemic iron deficiency in PrPKO mice caused by less efficient uptake by red blood cells (RBCs), liver, and brain as the result of impaired transport of iron from the duodenal enterocytes—a condition that can be easily reversed by expressing WT PrP [23]. Similarly, over-expression of PrPC increased intracellular iron, cellular labile iron pool, and iron content of ferritin leading to a decrease in total cellular content of transferrin (Tf) and transferrin receptor (TfR) proteins responsible for iron uptake, but an increase in ferritin responsible for iron storage [525]. Iron dyshomeostasis in brain neurons may be caused by sequestration of iron by the insoluble, aggregation-prone, infectious PrPSc isoform, which can form complexes with ferritin to induce bio-insufficiency [526]. Dysregulated iron homeostasis in cancer energy metabolism may be an important contributing factor in cancer drug resistance.
Aerobic glycolysis, commonly referred to as the “Warburg effect” [527], is undoubtedly the hallmark of cancer cells [437,528]. Enhanced, accelerated aerobic glycolysis has been shown to be responsible for resistance against various cancer drugs including sorafenib [529], palbociclib [530], oxaliplatin [531], doxorubicin [532], lapatinib [533] paclitaxel [534], bevacizumab [535], and cetuximab [536]. However, recent studies also revealed that many cancers such as myeloid leukemia [537], non-Hodgkin’s lymphoma [538], pancreatic ductal adenocarcinoma [539], melanoma [540], and high-grade prostate cancers [541] do not have impaired mitochondrial OXPHOS [542] while aggressive and drug-resistant cancers may actually upregulate mitochondrial oxidative phosphorylation (OXPHOS) as part of their defense mechanisms [543,544,545] to enhance autophagy [546], increase stemness [547], or remodel OXPHOS metabolism to promote survival [541,548].
Under physiological conditions, ATP hydrolysis is tightly regulated and the standard energy (ΔG′ATP) is maintained between 53 and 60 kJ/mol, where 56 kJ/mole, in principle, is regarded as the endpoint of both genetic and metabolic processes required for sustaining life [549,550]. Chemical energy of ATP is primarily used to power ionic membrane pumps that support cell and organ viability [551]. Uncontrolled proliferation, heightened dedifferentiation, and resistance to apoptosis in cancer cells may be the result of survival mechanisms activated in response to chemical energy deficiencies [549,552]. The exploitation of iron-containing heme is a preferred and highly effective counter-strategy employed by cancer cells to modulate energy metabolism and reprogram their environment [553,554,555]. Iron metabolism is vital for normal and cancerous cells [524,556]. The regulation of iron homeostasis in carcinogenic mechanisms has been extensively discussed and reviewed [554,556,557], where targeting iron metabolism via iron depletion or iron overload is considered a formidable anti-cancer strategy [558,559]. In addition, large cohort studies have also discovered a positive correlation between dietary heme iron intake and colon carcinogenesis [560,561].
3.3.1. Iron and Heme Facilitate Increased Energy Production in Cancer Cells
Iron is a transition metal with essential physiological functions including oxygen transport and production of cellular energy [524]. However, the two primary biological redox states of Fe2+ and Fe3+ can also catalyze the generation of hydroxyl radicals (•OH) through the Fenton reaction [562]. The pleiotropic relationship between iron and oxygen began ~3.5 billion years ago when cyanobacteria first introduced oxygen (O2) to earth’s water and atmosphere via water oxidation in the production of ATP [563,564,565,566]. During mitochondrial OXPHOS, oxygen consumption by cytochrome c oxidase (COX or complex IV) may reach 90% of total cellular oxygen [567] as part of the O2 reduction process that maintains the proton-motive gradient via proton pumping across the inner mitochondrial membrane. Proton pumping is mainly powered by the creation of a net positive charge via the oxidation of low-spin heme iron in COX [568,569]. In the human body, most of the iron is contained in heme proteins such as hemoglobin, myoglobin, and cytochromes [570,571]. The important, terminal step that completes the biosynthesis of heme occurs on the inner surface of the inner mitochondrial membrane (IMM) where ferrous iron (Fe2+) is inserted into the tetrapyrrole macrocycle of protoporphyrin IX (PPIX) by ferrochelatase [571,572,573].
Mitochondrial respiration is dependent upon homeostasis of the heme synthesis-export system, which regulates the tricarboxylic acid cycle (TCA) and controls the rate of OXPHOS where reduced heme synthesis or hypoxia induces heme export to shut down OXPHOS and activates glycolysis. However, the feedback effect of heme-export in turn increases heme synthesis, which can fuel increased TCA-cycle flux and OXPHOS rates [574]. Breast and lung cancer cells exhibit abnormal upregulation of the feline leukemia virus subgroup C receptor 1 (FLVCR1) heme-exporter [575]. Inhibition of FLVCR1 in breast and lung cancer cells resulted in dramatic reductions in proliferation, migration, invasion but acceleration in apoptosis [576,577,578]. Vascular disrupting agents (VDAs) such as combretastatin A-4 phosphate (CA4P) that are used to treat solid tumors often result in increased tumor recurrence and post-VDA treatment resistance because even though VDAs reduce tumor oxygenation, they also trigger upregulated heme flux, biosynthesis, uptake, and degradation [579] as defense mechanisms. Enhanced heme function leading to increased mitochondrial energy production fueling proliferation and progression is a classic feature of aggressive, high-mortality non-small-cell lung cancers (NSCLCs) [580] and other chemoresistant cancers [581]. PrP binds to both heme and hemin in human RBCs.
3.3.2. PrPC Regulates Heme Synthesis and Export to Modulate Glucose and Antioxidant Homeostasis in Cancer
PrPC is widely expressed in human blood where the number of prion molecules bound per blood cell was detected to be 290 ± 140 on red blood cells [582], 619 ± 167 on platelets, and 11,363 ± 2320 on lymphocytes [583]. Since the normal number of RBCs in man is ~5 × 109/mL, it is reasonable to assume that RBCs may be the main source of cell-associated PrPC in human blood [582]. Each of the four iron PPIX–heme complexes within hemoglobin of RBC contains an iron ion existing in either the reduced ferrous (Fe2+) state in heme, or the oxidized ferric (Fe3+) state in hemin [584,585,586,587]. PrP is a physiological ligand of both heme and hemin, and may be responsible for regulating heme homeostasis and heme redox activities. The in vitro direct interaction between heme (Fe2+) and PrPC not only enhanced peroxidase activity, but also inhibited the conversion of PrPC to PrPSc while preventing fibril formation in the heme-amyloid-β complexes [588]. By contrast, hemin is the PPIX–heme complex with iron in the oxidized ferric (Fe3+) state and can generate ROS through the Fenton reaction [562]. The prion protein exhibits great affinity for hemin, and binding to hemin causes PrP to form insoluble aggregates in vitro; yet hemin (Fe3+) bound to PrPC also exhibited enhanced peroxidase activities with the implication that PrPC possesses inherent protective, antioxidant functions [369,589]. In fact, brain lysates from PrP knockout mice had higher levels of oxidative damage to proteins and lipids compared to WT mice of the same genetic background [590]. In addition, cultures of primary cerebellar granule neurons derived from PrP knockout mice were highly susceptible to H2O2-induced toxicity as a result of significantly decreased glutathione reductase activities measured in vitro and in vivo [591].
Drug resistant cancers often display increased antioxidant defense via upregulation of reduced glutathione (GSH) production through metabolic modulation favoring a glycolytic shift that activates the pentose phosphate pathway (PPP) [592]. Recent evidence showed that both the glucose-6-phosphate dehydrogenase (G6PD) pathway and a less characterized hexose-6-phosphate dehydrogenase (H6PD) pathway contribute to accelerated cancer cell growth [593]. In breast cancer, hyperglycemia is an important factor that can reduce chemotherapy efficacy by promoting proliferation, invasion, migration, and anti-apoptotic defenses via accelerated glucose metabolism [594]. Breast cancer MCF-7 cell lines resistant to adriamycin showed increased glucose metabolism with heightened expression of glucose transporter GLUT1 [595,596]. An important physiological function of PrPC is the maintenance of glucose homeostasis through regulation of intracellular iron levels that control glucose metabolism through heme synthesis [597]. Pancreatic iron stores in PrP knockout mice were significantly lower than WT controls and silencing expression of PrPC in human pancreatic β-cells (1.1B4) significantly lowered intracellular iron and dramatically upregulated GLUT1 and GLUT2. By contrast, iron overloading downregulated glucose transporters GLUT1 and GLUT2 in a PrPC-dependent manner [15]. Experimental results showed that PrPC may act as an ancillary protein that is required for the function and expression of GLUT1 where PrPC depletion inhibited glucose utilization in human colorectal carcinoma cell lines and a human colorectal xenograft model in nude mice, with significant reductions in proliferation and survival of cancer cells both in vitro and in vivo [598]. In addition, prion-like aggregates of the islet amyloid polypeptide (IAPP) in the islets of Langerhans were proposed to play important roles in causing β-cell dysfunction and loss resulting in insulin resistance and hyperglycemia [599]. IAPP binds to heme-forming complexes, which facilitates the production of partially reduced oxygen species (PROS) that can damage β-cells [600,601,602,603].
Heme controls glucose regulation via direct interactions with insulin at two high-affinity insulin heme-binding sites, and heme-insulin complexes exhibit enhanced peroxidase activity and increased insulin cross-linking that lead to permanent loss of insulin functionality [604]. Increased heme levels and export from elevated FLVCR1 mRNA expression in adipose tissues of T2D patients were positively correlated with fasting glucose, triglycerides, and serum ferritin; but negatively correlated with insulin sensitivity [605]. The binding of hemin to prion may be a protective, physiological response that defends heme homeostasis since hemin with oxidized, ferric iron is unable to bind oxygen [606]. Hemin is potentially cytotoxic [607,608,609] due to its ability to inhibit glutathione S-transferase activity through competitive binding in human erythrocytes [610] and cause degradation and covalent cross-linking of glutathione reductase in yeast models [611]. Hemin bound to PrPC exhibits increased peroxidase activity compared to free hemin as a result of the coordination of PrPC octarepeat peptide region residues 34–94 to ferric iron in hemin [284,589]. However, this initial increase in peroxidase activity over a longer time frame may eventually elevate oxidative stress causing aggregation of insoluble PrPC isoforms [369,483] which can potentially change the conformation and physiological functions of PrPC. In cancer cells, heme serves important functions in the regulation of cell cycle and cell growth. Inhibition of heme synthesis caused cell cycle arrest, senescence, and apoptosis [612]. Therefore, increased oxidative stress in the TME [613] may elevate prion-hemin binding, resulting in increased tumor MDR.
3.3.3. Upregulation of Hemoglobin Synthesis by Hemin-Bound PrPC May Increase Cancer Multidrug Resistance
The binding of hemin to PrPC in diverse cell lines results in aggregation or degradation of PrPC in a cell-type specific manner. However, the binding interaction also significantly upregulates hemoglobin synthesis in hematopoietic cells, where brain organotype cultures exposed to hemin showed increased α-globin in PrP WT compared to PrP knockout samples. Additionally, RBCs from PrP knockout mice had markedly lower α-globin levels compared to PrP WT controls [614]. Since heme regulates gene expression transcriptionally and post-transcriptionally [615,616], heme can initiate changes in key factors that control extensive processes from cell cycle and Ras signaling to chromatin structure, splicing, and protein folding [617,618]. Heme controls chromatin and genome function previously not associated with heme regulation [619]. Thus, the upregulation of heme synthesis as a result of PrPC binding to hemin may be a significant factor contributing to cancer drug resistance [553]. Even though PrPC bound to hemin (ferric PPIX) showed rapid precipitation with increased aggregation and decreased solubility [369,589], in vitro heme (ferrous PPIX) interaction with PrPC inhibited the seeded conversion of PrPC to PrPSc in protein misfolding cycling amplification assays where conversion could be inhibited at heme concentrations from 10 to 1000 μM but not at 1 μM [588]. Porphyrin tetrapyrroles (IC50 ~0.5–1 mM) inhibited the formation of PK-resistant PrP without affecting the biosynthesis of normal PK-sensitive PrP in scrapie-infected mouse neuroblastoma (ScNB) cell cultures [620]. If the redox cycling between heme and hemin is intended as a natural feedback control for prion conversions, then the elevated ROS in TME together with increased oxidative stress from prolonged peroxidase activity from PrPC-hemin complexes [369,588] may terminate the feedback cycle to favor increased hemin-PrPC binding that heightens cancer drug resistance as a result of elevated hemoglobin synthesis. Using melatonin to restore heme–hemin redox balance may prevent conversion of PrPC to PrPSc and preserve PrPC physiological functions while enhancing cancer drug efficacy.
3.4. Melatonin Maintains Hemoglobin Redox Balance by Protecting CYB5R3 and Band 3 Protein in an Antioxidant-Independent Manner
Due to the natural redox state of ferrous and ferric iron in heme, hemoglobin can become “biologic Fenton reagents” which readily promote hydroxyl radical formation [621]. Therefore, erythrocytes (red blood cells) must depend on robust antioxidant systems to maintain heme redox balance [622,623,624]. The physiological autoxidation of hemoglobin (0.5–3%/day) creates the reversible hemin (ferric PPIX) derivative, commonly known as methemoglobin (MetHb) [625,626], where the sixth coordination position of the heme iron is occupied by either hydroxide (OH−) or water (H2O) [627]. The water molecule coordinated to the iron atom in ferric MetHb results in increased instability compared to ferrous heme, and can also cause significant loss of heme at rates substantially higher than even ferrylHb (Fe4+) [628]. In addition, MetHb cannot bind oxygen and must be effectively reduced back to the ferrous state by NADH-cytochrome b5 reductase 3 (CYB5R3). CYB5R3, also known as NADH–cytochrome b5–metHb reductase, is a flavoprotein responsible for the transfer of electrons from NADH via cytochrome b5 (CYB5) to reduce MetHb, producing NAD+ [629,630]. CYB5R3 exists in two isoforms, where the soluble isoform is found exclusively in RBCs [631,632], and the membrane-bound isoform is ubiquitously expressed in mammalian cells including erythrocytes, mitochondria, and lipid rafts [630,633,634,635,636].
Elevated oxidative stress in the TME [613,637] may challenge antioxidant systems in RBCs leading to increased formation of MetHb and the release of free heme that can be complexed with PrPC. Rapid depletion of NADH in erythrocytes exposed to oxidants such as T-butylhydroperoxide resulted in elevated MetHb due to increased consumption to support recovery of reduced glutathione [638]. However, in 1999 when Tesoriere et al. exposed human erythrocytes to cumene hydroperoxide (cumOOH) to induce the oxidation of a 1% suspension of RBCs, which led to 100% hemolysis of samples in 180 min, the addition of 50 µM melatonin effectively delayed denaturing of hemoglobin and release of hemin in an antioxidant-independent manner. Melatonin treatment inhibited hemin precipitation in oxidized RBCs compared to controls where increased hemin swiftly partitioned into RBC membranes. Even though MetHb may be responsible for the generation of additional •OH, and melatonin is a potent scavenger of hydroxyl radical [126] with its relatively low oxidation potential of approximately +570 mV [639] compared to •OH [640], the protective effects observed by Tesoriere et al. were not related to antioxidant functions. Nevertheless, 35% of melatonin was consumed by RBCs under cumOOH challenge, while no melatonin was consumed by reactions with •OH in the experiment [641]. Six years later, Tan et al. demonstrated that melatonin may have been utilized to recycle NADH to regenerate CYB5R3 in the reduction of MetHb [642].
Tan and colleagues reported for the first time in 2005 that melatonin is able to recycle NAD+ to NADH, forming the N1-acetyl-N2-formyl-5-methoxykynuramin (AFMK) metabolite in the process through the cleavage of the pyrrole ring [642,643]. Melatonin is an ideal electron donor due to its electron-rich aromatic indole ring [644]. The use of 1 millimolar (mM) melatonin prevented the loss of NADH in PC12 cells subjected to 150 µM paraquat incubation while 2000 µM MEL provided greatest protection to NADH loss from 500 µM orthovanadate (Va5+) incubation [642] (Table 1). In the absence of NADH, melatonin reduced autoxidation of human oxyhemoglobin (HbO2). Autoxidation was increased when HbO2 was incubated with NADH and the effect was profoundly augmented by the addition of melatonin (each at 500 µM). However, addition of melatonin did not change the level of NADH consumption even though HbO2 autoxidation was markedly elevated. Since NADH levels remained constant, it was concluded that the presence of melatonin recycled NADH through electron donation to form AFMK as metabolite [642]. Melatonin can also protect band-3 protein at the membrane level in an antioxidant-independent manner. Addition of 300 μM H2O2 to erythrocytes decreased expression of band 3 and altered cell shapes without causing lipid peroxidation or formation of MetHb. In the absence of catalase, the addition of 100 μM melatonin reversed RBC cell-shape changes and restored band 3 protein conformation and expression levels. Interestingly, treatment with 1 μM melatonin was ineffective and even caused cell-shape changes and increased lipid peroxidation in RBCs challenged with H2O2 [645,646]. The fact that melatonin at pharmacological doses exerted opposite effects on RBCs is reminiscent of various observations where low and high doses achieved opposite effects in stimulating or inhibiting prion activities, respectively [114,118] (Table 1). Regardless, the protection of band 3 by melatonin may be a significant contributing factor in the attenuation of TME-associated hypoxia and accelerated glycolysis, which directly modulate PrPC phase separation and related functions.
Table 1.
Pleiotropic effects of low and high melatonin doses on in vitro and in vivo models involving prion propagation and/or associated processes.
| Model/Description | Melatonin Doses | Melatonin’s Effects | Reference |
|---|---|---|---|
| MSCs/Model of ER stress–induced ischaemic injury. | 1 μM MEL pretreatment 30 min at 37 °C. | Increased expression of PrPC and antioxidant enzymes to reduce oxidative stress. | [113] |
| MSCs/Model of indoxyl sulfate-induced senescence. |
1 µM MEL + 5 µM pioglitazone. | Treatment promoted highest MSC growth rates and inhibited senescence via enhanced PrPC expression. |
[647] |
| TH1/Model of high glucose-mediated fibrosis. | 1 µM MEL as pretreatment. | Prevented high glucose-induced fibrosis by recovering PrPC expression to augment antioxidant protection. |
[648] |
| SNU-C5/WT cells/Model of colorectal cancer cell apoptosis. |
1 mM MEL treatment 24 h. | Reduced PrPC and PINK1 expression to increase mitochondrial superoxide. | [114] |
| Human colon CSCs (S707)/Model of PRNP overexpression. |
500 μM MEL + 1 μM 5-FU treatment for 72 h. |
Treatment suppressed proliferation and increased apoptosis by inhibiting PrPC-OCT4 axis. |
[115] |
| Murine/Model of human CSCs (S707) xenograft tumorigenesis. |
500 μM MEL + 1 μM 5-FU treatment for 72 h. |
Treatment decreased PrPC expression to reduce tumor volume and suppress cell proliferation. |
[115] |
| SNU-C5/Oxal-R/Model of PrPC expression in oxaliplatin-resistant colon cancer cells. |
500 μM MEL + 1 μM oxaliplatin for 24 h. |
MEL induced oxaliplatin-mediated apoptosis via blockade of PrPC-mediated antioxidant activities. |
[116] |
| PC12/Model of paraquat-induced NADH depletion. |
1 mM MEL incubation at 35 °C for 1 h. |
Prevented the loss of NADH/NAD+ caused by paraquat treatment. | [642] |
| Oxyhemoglobin/Model of vanadate-induced NADH oxidation. |
2 mM MEL. | Treatment conferred the highest level of protection against NADH oxidation compared to lower doses. |
[642] |
| Murine/Model of B16-F10 melanoma cell proliferation. |
1 mM MEL 24 h I incubation. |
Significantly reduced growth rate and migration. |
[649] |
| C57BL/6J mice/Model of lung metastasis via B16-F10 cell injection. |
20 mg/kg in drinking water or IP injection for 15 days. |
Melatonin did not alter cell migration or proliferation. |
[649] |
| Kunming mice/Model of copper-induced liver injury. | 50 mg/kg IP injection once daily, 3 times. | Inhibited copper-induced hepatotoxicity and DNA damage via copper chelation, preventing formation of hydroxyl radical. | [430] |
MSC: mesenchymal stem cell; ER: endoplasmic reticulum; TH1: human renal proximal tubule epithelial cell line; SNU-C5/WT: wild-type colon cancer cell line; PINK1: PTEN-induced kinase 1; CSCs: cancer stem cells; 5-FU: 5-fluorouracil; OCT-4: octamer-binding transcription factor 4; SNU-C5/Oxal-R: oxaliplatin-resistant colon cancer cell line; PC12: adrenal phaeochromocytoma cell line; C57BL/6J mice: inbred strain with complete melatonin “knockdown”; IP: intraperitoneal; Kunming mice: outbred stock with no known report of melatonin “knockdown” (see Abbreviations for additional acronyms).
3.5. Melatonin Increases O2 Saturation to Reduce TME Hypoxic Stress by Protecting Band 3 Protein
Hypoxia is an environmental selection pressure that can significantly exacerbate cancer drug resistance. As adaptation to hypoxia, changes in gene expression affecting cellular and physiological functions often result in increased cancer aggressiveness and treatment resistance [650,651,652]. A recent study using in silico modeling and the simulation of in vivo cancer cell growth found that increasing oxygen concentration and pH value in the TME could result in significant shrinkage of tumor growth size [653]. Melatonin is an effective oncostatic agent capable of modulating important elements in TME that drive immunosuppression, cell proliferation, metastasis, and resistance to apoptosis [654]. Using melatonin to maintain RBC heme redox balance and band 3 functionality directly targeting the hypoxia feedback cycle in TME could be an important linchpin in dismantling the TME to enhance drug sensitivity [655,656,657,658,659].
Hypoxic stress promotes phase separation of glycolytic enzymes into cytoplasmic G-bodies that increased glycolytic output in S. cerevisiae and human hepatocarcinoma cells [660,661]. Hypoxia can induce increased expression of PrPC [476] to facilitate persistence and storage of memory in animals and plants [24,25,662]. In vivo and ex vivo models showed post-hypoxic cells reoxygenated in the bloodstream retained a hypoxia-induced cancer stem cell-like phenotype where exposure to intratumoral hypoxia promoted chemotherapy resistance, increased recurrence, and capacity to metastasize in post-hypoxic cells compared to cells never exposed to hypoxia [663]. The fact that pathological prion isoforms can remain dormant for an extended period of time may be another significant consideration in targeting dormancy in cancer. Cancer cells become dormant when they switch from an active to a quiescent state and cancer dormancy remains a major challenge in clinical oncology where tumor recurrence can resurface years after initial diagnosis [664]. Not surprisingly, stress has been identified as one of the triggers that can awaken cancer cells from dormancy [47,665], and hypoxic stress that reduces pH is able to activate prion aggregation [666] and phase separation (Section 2.3.3).
3.5.1. Hypoxia in TME Is Modulated by Fluctuations in Red Blood Cell Flux
Band 3, or anion exchanger 1 (AE1), is probably the world’s quickest bicarbonate/chloride transporter with a turnover of ~105 chloride ions per second per molecule [667,668,669]. The C-terminal domain of this large polytopic membrane protein is embedded in the lipid bilayer, tethered to the cytoskeleton comprising the RBC membrane [670,671,672]. Band 3 is not only a critical anion transporter supporting oxygen delivery by RBCs [673], but also a primary scaffolding structure for large macromolecular complexes that modulate RBC membrane flexibility and integrity [670,674]. Disruption of band 3 and its association with proteins such as ankyrin-1 and spectrin tetramers in the RBC skeletal network [670] can induce a four-fold reduction in membrane stiffness that negatively impacts RBC membrane deformability and elasticity [675,676]. RBCs must maintain a high degree of deformability and elasticity in order to travel through capillaries and small vessels with diameters under 5 µM to fulfill their primary objective of oxygen delivery [677,678,679]. The loss of band 3 functionality can directly impact hypoxia in cancer TME, activating a positive feedback cycle where hypoxia increases band 3 disruptions to reduce RBC deformability, which in turn augments the reduction in red cell flux and O2 delivery.
The deformability of RBCs, which is regulated by membrane flexibility, supports the normal transit of RBCs through capillaries with lumens narrower than the cell diameter of RBCs [680,681]. Capillary RBC flux is possibly the most important determining factor for oxygen delivery to cells [682] where changes in red cell flux (RCF) can lead to changes in vascular pO2 resulting in transient hypoxia. Experimental studies revealed that even in well-vascularized regions of tumors, a two-fold variation in RCF can produce intermittent hypoxia (IH) in 30% of the tissues, whereas in poorly vascularized regions, the same degree of fluctuation produced significantly higher levels of transient hypoxia [683]. In addition, oxygen delivery by RBCs can be decreased by excess oxidative stress [684]. High O2 tension in arterial blood and hemoglobin’s natural inclination to become “biologic Fenton reagents” result in the continuous production of ROS within RBCs [621,685]. Oxidative stress, often elevated in patients with sickle cell disease (SCD), was found to be associated with increased hemoglobin degradation, which correlated negatively with decreased RBC deformability [686,687]. SCD is caused by a substitution of valine for glutamic acid at the β-6 position in the hemoglobin β-chain [688,689]. This polymorphism constrains band 3 mobility impacting RBC membrane properties [690] which not only decreases RBC deformability but also affects the ability of RBC to lower oxidative stress. Since erythrocytes lack the TCA cycle, the only source for the reducing equivalent NADPH that recycles oxidized glutathione (GSSG) to GSH is the pentose phosphate pathway (PPP) [691,692]. In erythrocytes, PPP facilitates the continuous reduction of NADP+ to NADPH via the conversion of glucose 6-phosphate (G6P) to 6-phosphogluconolactone catalyzed by glucose-6-phosphate-dehydrogenase (G6PD) [693]. Under steady-state conditions, the main G6P flux is maintained via glycolysis. However, the flux to PPP under oxidative stress can be enhanced more than 20 times [694], and band 3 plays a critical role in the maintenance of glycolytic flux to PPP in RBCs.
3.5.2. Hypoxia Prolongs Deoxygenation and Elevates Hemin Release to Damage RBC Membrane Integrity and Band 3 Proteins
Glycolysis in RBC is responsible for the production of NADH [695], which is used by CYB5R3 to reduce MetHb [629], and the deoxygenation of erythrocytes (deoxyHb) can increase glycolysis by 26% in RBCs [696]. During deoxygenation, the temporary dissociation of ankyrin from band 3 that releases the spectrin/actin cytoskeleton from RBC membranes can improve blood flow by enhancing RBC deformability without a loss in elasticity [677,697]. However, hypoxia can increase deoxyHb [698] to prolong deoxygenation, rupturing band 3-ankyrin bridges to decrease membrane mechanical stability, deformability, increase abnormal morphology, and induce spontaneous vesiculation of RBCs [697,699]. Under normal oxygenation and deoxygenation conditions, band 3 suppresses glycolytic flux to maintain pentose phosphate pathway activities by forming complexes with glycolytic enzymes (GEs), inhibiting glycolysis. However, when oxygenated RBCs were treated with pervanadate, a reagent that inhibits band 3 protein binding by inducing phosphorylation of tyrosines [700], glycolytic fluxes were increased by 45% while PPP shunt fluxes became 66% lower than controls as a result of GE-band 3 complex inhibition [701]. Regardless of oxygenation status, GEs in band 3 knockout mice are unable to bind to RBC membranes but are distributed throughout the cytoplasm [702]. Interestingly band 3 regulates its own phosphorylation according to stress sensed in the environment.
Band 3 has been proposed to be a “redox stress sensor” that regulates its own phosphorylation as an adaptation to stress via dissociation from ankyrin and the spectrin-actin skeleton, which alters membrane structures [703,704]. Even though band 3 can selectively phosphorylate and remove oxidized regions from RBC membranes [705], increased hemin release as a result of oxidative stress [706] may still impact RBC deformability, decreasing O2 delivery [693]. Hemin has been shown to cause rapid destruction of RBC membrane integrity by destabilizing spectrin–protein 4.1–actin interactions [706]. Protein 4.1, a principal constituent of RBC membranes, can be mobilized in a dose-dependent manner to cause complete loss of ankyrin-band 3 binding at high hemin levels [707,708]. In addition, hemin aggregates bound to RBC membranes can reorganize membrane lipid composition to induce membrane disorder and permeabilization [709].
3.5.3. Oxygen Saturation and Transport Are Directly Modulated by Heme Redox Balance
The oxidative state of MetHb (Fe3+) also shifts the oxygen dissociation curve to the left, where the conversion of a ferrous atom to the ferric state results in increased affinity of the remaining ferrous atoms for O2, thus negatively impacting O2 transport and release [501,710,711]. On the other hand, band 3 may act as a “molecular switch” that mediates O2 transport by modulating O2 saturation and erythrocyte properties [712,713]. The preferential binding of band 3 to deoxyHb shifts the O2 dissociation curve to the right in a concentration-dependent manner [714]. Kidney band 3 proteins lacking residues that bind deoxyHb were unable to alter Hb-O2 affinity [715]. Therefore, maintaining heme–hemin redox homeostasis is a critical consideration in controlling hypoxia in TME. Early experimental results showed the PPP shunt only accounted for a small part of the reduction of total MetHb [716] and excess hemin reduction may require NADH-dependent CYB5R3 ferrous-ferric iron recycling. Melatonin has been demonstrated to enhance NADH recycling to regenerate CYB5R3 in the reduction of MetHb [641,642], protect RBC morphology, and maintain expression of band 3 [645] all in an antioxidant-independent manner. In addition, melatonin was able to shift the O2 dissociation curve to the right, increasing O2 release, in rats exposed to hypothermia [717]. Melatonin may also protect band 3 through modulation of lipid composition. It is perhaps not a coincidence that one of the important physiological functions of PrPC is heme/hemin-binding, and that both band 3 and PrPC reside in lipid rafts.
3.5.4. The Role of Membrane Lipids and Lipid Rafts in Prion Physiological Function and Pathological Propagation
Membrane surfaces offer distinct advantages in the formation of MLOs [718,719,720]. Lipid rafts, which are phase-separated regions in membrane lipid bilayers, enable thermodynamic interactions between membrane-anchored proteins and condensate components, facilitating phase separation [721]. The unstructured N-terminal domain of PrPC is intrinsically disordered and is prone to phase separation under hypoxia or other stressful conditions such as changes in pH in TMEs. The PrPC GPI anchor signal comprising residues 231–253 is usually found tethered to lipid rafts [272,333,722] (Figure 1). Upon cleavage, the soluble N-terminal cleavage fragments (N1, N2) are released while the C-terminal cleavage fragments remain bound to lipid rafts on membranes via GPI anchors [272,380,381]. The shedding of PrPC by proteolysis cleaves residues 23–230 from the membrane GPI anchor around residue 231, releasing a full-length, soluble PrPC, which was shown to reduce the cytotoxicity of amyloid-β oligomers [382]. The N-terminal domain of PrPC also contains a lipid raft-targeting region that allows interactions with membrane lipids in a GPI-independent manner [272,325,326,722]. However, tethering of the N-terminal domain to lipid rafts can compromise prion protein cellular response to oxidative stress from increased aggregation of PK-resistant N-terminal fragments [723,724]. The composition of lipids in membranes and lipid rafts can influence lipid–protein interactions, which induce either the formation of α-helix structures or β-sheet-rich amyloids [383,725]. In vitro studies reported that under physiological conditions, interactions between anionic lipids and rPrP can overcome energy barriers to increase β-sheet aggregation, converting a significant portion of α-helix in soluble, full-length rPrP to a PK-resistant conformation similar to PrPSc [726]. Nevertheless, it is possible that the structured C-terminal domain contained in full-length WT PrP may be protective against formation of β-rich amyloid-like aggregates.
3.6. Melatonin May Prevent PrPC Pathological Conversion from Phase Separation Caused by Mutations
The C-terminal domain (residues 121–230) of human prion (huPrP) was shown to undergo large conformational changes induced by reductions in pH and increases in temperature [727]. Copper bound to the fifth, nonoctarepeat binding site in the segment containing histidine residues 96 and 111 changes the structural plasticity of the N-terminal to a more compacted conformation that may facilitate prion conversion [366,728,729] (Figure 1). Simulation of the conformational transition from PrPC to PrPSc using ratchet-and-pawl molecular dynamics (rMD)-based methodology revealed that the C-terminal domain acts as a primary conversion surface for the unstructured N-terminal domain, initiating a cascade of conformational transitions that provide further templating leading to the complete conversion into the pathological PrPSc isoform [730]. Even though copper-binding can affect conformational changes in the C-terminal domains to alter aggregation behavior, mutations in C-terminal domains in both yeast and human PrP can greatly influence prion propagation also [120,731].
The pathological mutation at residue 145 (Y145Stop), located within the highly structured globular C-terminal domain (121–230), produces a highly disordered region that spontaneously phase separates under physiological conditions resulting in a truncated N-terminal that lacks C-terminal fragments [120,732]. Even though mutant Prp145 is normally degraded rapidly by the ubiquitin-protease system (UPS), PrP145 is prone to aggregation and intracellular accumulation under stress or aging-related reduced proteasomal functions [120,732]. Transgenic (Tg) mice with PrP but lack C1 fragments showed accelerated accumulation of pathogenic PrPSc after scrapie inoculation, whereas Tg(C1) mice expressing N-terminally deleted forms (PrP(Δ23–111)) in the absence of endogenous PrP remained completely healthy and did not accumulate PK-resistant PrP after scrapie inoculation [733]. Even though prion proteins are believed to be the cause for neurodegenerative diseases, under physiological conditions, PrPC often act as important stress-induced signaling molecules to activate neuroprotective features to counter hypoxic brain damage (rodent in vivo, human brain tissue in vitro) [734] and ischemic injury (rat model) [735], whereas the deletion of PrPC in brains of transgenic PrPC-knockout mice increased infarct size by 200% [736] and aggravated neuronal cerebral ischemia through reduced post-ischemic phospho-Akt expression that impaired the antiapoptotic PI3K/Akt signaling pathway [737]. Since melatonin regulates the UPS and promotes ubiquitination [308,738,739,740], the presence of adequate melatonin may ensure the proper, timely degradation of mutated PrP145 by ubiquitin [732] to prevent phase-separated condensate formation of self-templating amyloid-like aggregates and pathological truncation of PrPC. Without adequate melatonin, even in the absence of mutations, the physiological association of the N-terminal lipid raft-targeting region may cause lipid and membrane disruptions that alter membrane functions, signaling, and band 3 protein functionality, which can all exacerbate the detrimental effects of TMEs to enhance MDR.
4. The Effects of Melatonin on Lipid Phase Transition, Lipid Composition, and Prion Propagation in Cancer Multidrug Resistance
Lipid rafts are dynamic, transient, mobile, nanoscopic (10–200 nm) liquid-ordered (Lo) domains that are rich in sphingolipids and cholesterol formed as a result of thermodynamic LLPS [741,742]. The location of lipid rafts on plasma membranes, intracellular membranes, and extracellular vesicles enable relevant biological functions, effectively serving as hotspots for signal transduction [743], trafficking, and sorting of proteins and lipids [744,745]. However, lipid rafts are increasingly associated with cancer MDR as quite a few cancer-related proteins involved in migration, invasion, and metastasis are found in lipid rafts, which serve as signaling hubs for these proteins [328,746,747,748]. Multidrug resistance protein 1 (MDR1), one of the ATP-binding cassette transporters responsible for drug efflux, resides in lipid rafts in prostate cancer cell lines [749], and the inhibition of flotillins—scaffolding proteins that are key components in lipid rafts—was shown to reverse MDR in colon cancer cell lines [750].
Lipid rafts have been extensively studied for the localization, trafficking, cellular signaling, cell-to-cell transmission, and conversion of PrPC to PrPSc [272,326,751]. Lipid rafts are also involved in the metal/copper-mediated endocytosis of prions via clathrin-coated pits or caveolae [370,371,372]. In proliferating neuronal CAD 5 cell lines, PrPC is predominantly associated with lipid rafts on cytoplasmic membranes [752] while in human dental pulp mesenchymal stem cells, the integrity of lipid rafts is essential for the preservation of recombinant prion protein (23–231) physiological activities affecting neuronal differentiation and signaling. The critical localization of PrP in lipid raft microdomains allows prions to recruit and interact with important biochemical signaling partners [753,754]. Even though lipid rafts may influence the conversion of PrPC into PK-resistant isoforms [723,724], interactions between PrP N-terminal residues and membranes can also lead to membrane dysfunctions [755].
The amyloidogenic prion residues 106–126 [756,757] in the N-terminal domain are characterized by hydrophilic and hydrophobic regions that can increase lipid density and membrane viscosity upon embedding into lipid bilayers [758]. The prion peptide fragment 106–126 can form heterogenous single cation channels with different conductance and kinetic properties in lipid bilayers, modifying electrolyte homeostasis and affecting cellular functions [759,760,761] while the conversion of PrPC to PrPSc is often associated with membrane abnormalities including decreased membrane fluidity [762]. The conversion process of PrPC to PrPSc involves the conformational change of α-helical structures to PK-resistant β-sheets rather than chemical modifications. These conformational changes dysregulated membrane receptors causing a 5-to 13-fold reduction in bradykinin (Bk) binding affinity despite a 3-to 4-fold increase in Bk receptors on neuro N2a cells resulting in decreased Ca2+ and Bk second-messenger IP3 responses [763]. Due to the amphipathic nature of the prion fragment 106–126, it has been proposed that the toxic effects resembling many membrane-active antimicrobial peptides (AMPs) are initiated by the direct association of monomeric peptides with membrane matrix. Experimental studies employing atomic force microscopy, Raman and electron paramagnetic resonance spectroscopy, revealed that PrP 106–126 membrane interactions can impair bilayer mechanical integrity via the modulation of both line tension, which can produce porous defects, and lipid vibrational dynamics. PrP 106–126 membrane interactions can enhance intra-chain conformational disorder without altering inter-chain interactions in cylindrical-shaped phosphatidylcholine lipid molecules but increase inter-chain interactions without changing the intra-chain conformational order in cone-shaped phosphatidylethanolamine lipid molecules [764].
The physiological relationship between prions and lipid membranes may be dependent upon the presence of a sufficient level of melatonin in order to prevent or ameliorate potential pathological outcomes. Infecting transgenic mice that expressed PrP without GPI anchors with a stable form of PrPSc produced a completely new prion strain with 25–50-times higher levels of PK-resistant PrPSc compared to WT mice. However, C57BL/6 mice were selected for the breeding of GPI-knockout mutants used in these experiments [765]. Most inbred mice including C57BL/6 exhibit reduced melatonin production where the serotonin N-acetyltransferase (arylalkylamine N-acetyltransferase, AANAT) mRNA encodes a severely truncated AANAT protein due to a stop codon being spliced into a pseudo-exon, with the C57BL/6J strain exhibiting complete melatonin “knockdown” [766], whereas two very short peaks in the middle of darkness and at light onset were observed in C57BL/6 mice [767]. It is, therefore, not unreasonable to hypothesize that the lack of continuous presence of melatonin in plasma lipid bilayers contributed to the pathogenic conversion of PrP fragments interacting with lipids in membranes.
4.1. Melatonin Maintains Lipid Raft Integrity and Prion Physiological Functions by Modulating Cholesterol and Lipid Phase Transitions
The amyloidogenic PrP106–126 residues exhibit fusogenic properties, promoting lipid mixing [768] which can be exacerbated by low pH or high cholesterol levels [769,770,771]. In fact, cholesterol suppression has been shown to mediate prion propagation where PrPC degradation and PrPSc conversion were substantially reduced in cholesterol-rich neuronal N2a cells treated with lovastatin, an inhibitor of the rate-limiting enzyme in the 3-hydroxy-3-methyl-glutaryl-CoA (HMG-CoA) reductase cholesterol biosynthetic pathway [772,773]. In addition, PrP106–126 membrane interactions can impair bilayer mechanical integrity to form pores via modulating line tension [764]. Line tension maintains the energetic boundaries between lipid raft domains and surrounding membranes, and can, therefore, affect the physiological size, form, and shapes of lipid rafts [774]. Increasing cholesterol content in membrane lipids can reduce line tension to produce nanoscopic lipid rafts [775], which, theoretically, is a desirable physiological state as opposed to enlarged, micron-sized lipid rafts that are produced under inflammatory conditions and carry pro-inflammatory, oncogenic signaling molecules [328,776,777]. However, in a highly oxidative, low pH TME, the effect of cholesterol on lipid rafts and prion propagation in the absence of adequate melatonin as a “broad-based metabolic buffer” to regulate lipid peroxidation, line tension, and cholesterol homeostasis becomes highly questionable (Figure 2).
Breast cancer and prostate cancer are associated with high serum cholesterol [778,779] while their respective cell lines have been shown to contain more lipid rafts that were sensitive to cholesterol depletion-induced apoptosis compared to healthy cells [780]. Cholesterol metabolism is increasingly associated with cancer MDR from increased gene transcription of drug efflux transporters or reprogramming of metabolic pathways that enable MDR phenotypes [781,782,783]. Depletion of cholesterol in lipid rafts in drug-resistant cancer cells was demonstrated to facilitate the accumulation of doxorubicin or rhodamine 123 via suppressing MDR-1 activity and increasing drug sensitivity to overcome drug resistance [784]. Increased cholesterol, on the contrary, can facilitate prion propagation due to its inherent electrostatic properties. Under physiological conditions, interactions between anionic lipids and rPrP can overcome energy barriers to increase β-sheet aggregation, converting a significant portion of α-helix in soluble, full-length rPrP to a PK-resistant conformation similar to PrPSc [726]. Increasing cholesterol content can lower surface charge of lipid membranes in saline solutions from positive to negative [785]. Therefore, excess cholesterol may alter prion interactions with negatively charged anionic lipids to intensify the aggregation of PK-resistance β-sheet amyloids [786,787].
Melatonin not only directly interacts with cholesterol to counteract and alleviate the effects of cholesterol on lipid membranes [788], but also regulates lipid dynamics and composition, inducing lipid phase separation by modifying lipid hydrocarbon chain order [330,331]. By increasing disorder in the Ld phase, melatonin displaces cholesterol, driving cholesterol into the ordered Lo phase via competitive binding to lipid molecules [330]. The preferential location of melatonin at hydrophilic/hydrophobic membrane interface due to its ability to form strong H-bonds with hydrophilic lipid headgroups allows nonpolar melatonin to reverse cholesterol- and prion-induced membrane rigidity [762,789,790,791,792,793]. In the POPC/bovine brain sphingomyelin-supported lipid bilayer and POPC/bovine brain sphingomyelin/cholesterol-supported lipid bilayer membrane models, the PrP106–126 fragment was demonstrated to cause membrane thinning in the Lo phase and membrane disintegration in the Ld phase [329]. More importantly, the results obtained suggest that PrP106–126 fragment membrane interactions mainly occurred in the Ld phase where the peptides bound to the headgroup region of lipids in the Ld phase of the membrane increased membrane strain [329]. Since melatonin can stabilize lipid Lo/Ld phase-coexistence over an extended range of temperatures (up to 45 °C), effectively preventing the formation of the Ld phase at high temperatures [332], it is quite possible that local variations in melatonin concentration can affect prion interactions with membrane lipids via the reordering of membrane lipids, which impacts the lipid phase transition, line tension, membrane fluidity, and functionality of lipid rafts.
At 0.5 mol% concentration, melatonin can penetrate lipid bilayers to form fluid domains where melatonin molecules are aligned parallel to phospholipid tails, but at 30 mol% concentration, melatonin molecules become aligned parallel to the lipid bilayer close to the headgroup regions where one melatonin molecule associates with up to 2 lipid molecules, forming an ordered, uniform, lateral, crystal-like structure evenly distributed throughout membrane models tested [794]. The fact that exogenous melatonin supplementation injected at doses between 10 and 200 mg/kg showed dramatically different dose-dependent subcellular distribution in male Wistar rat cerebral cortex, where membranes were able to reach 10-times higher concentration levels than in the cytosol [795], may imply that high melatonin concentration produced under duress may act as a “broad-based metabolic buffer”, disrupting prion interactions with membrane lipids to prevent aberrant phase separation resulting in pathological aggregations [721,726] while defending band 3 proteins from membrane disruptions caused by prion-hemin binding effects (Figure 2).
4.2. Melatonin May Preserve Band 3 Interactions with Membrane Lipids in Antioxidant-Dependent and -Independent Manners
Results from more recent atomistic molecular dynamics (MD) simulations investigating interactions between band 3 and nanoscopic lipid raft domains support early experimental observations that band 3 prefers to localize in Lo lipid raft domains albeit the concentration of cholesterol, comprising ~45 mol% of erythrocyte membranes, greatly affects membrane and band 3 interactions [796,797,798,799,800]. Cholesterol enrichment resulting in an elevated cholesterol-to-phospholipids mole ratio exceeding the normal 0.9–1.0 amount resulted in decreased membrane fluidity and strikingly abnormal changes in red cell contours characterized by deranged folding and scalloping of cell margins [800]. These changes may be explained by band 3 interactions with lipid phases as a result of cholesterol enrichment. All-atom MD simulations revealed that in ternary lipid bilayers composed of saturated lipids, unsaturated lipids, and cholesterol, the band 3 C-terminal domain, which is associated with the erythrocyte cytoskeleton, interacted with high electrostatic attraction with anionic lipids in the Lo domains of phase-separated lipid bilayers, whereas in lipid bilayers with increased cholesterol concentration (50 mol%), band 3 was observed to preferentially target the Ld phase and avoided contacts with cholesterol-enriched Lo domains [796]. The association of band 3 with lipid nanodomains in erythrocytes greatly influences physiological functions [667,801] where band 3 fragments can move into lipid bilayers, seeking each other out to form functional fragments [802,803]. Thus, disturbances in lipid composition as a result of hypoxia or increased ROS in TMEs can potentially disrupt band 3 and associated proteins, including ankyrin-1 and spectrin tetramers in erythrocyte skeletal networks [670,697,699], reducing RBC membrane deformability and elasticity [675,676] and lowering O2 saturation [498] to reinforce the negative feedback, which enhances TME-induced MDR.
Lipid peroxidation is a cascading event initiated by ROS attacking anionic headgroups at membrane interfaces [804] where oxidized moieties residing close to lipid headgroups perturb membrane bilayer structures, modifying membrane properties including increasing membrane permeability [805], decreasing membrane fluidity [806,807], and increasing line tension, which can transform nanometer-scale lipid rafts into larger, micron-sized domains [776,808,809] that carry pro-inflammatory molecules often associated with cancer cell signaling pathways [328,777,780]. Experimental results using giant membrane vesicle model systems showed that lipid peroxidation induced significant changes in membrane phase behavior, causing a dramatic escalation of phase separation at room temperature, which increased the non-raft phase while decreasing affinity of tested raft proteins for raft domains [810]. Melatonin, with its free radical scavenging metabolites [131,133,134] and preferential location in membrane bilayer headgroups, enables dynamic interactions that can attenuate peroxidation effects via a reduction in bilayer thickness and increasing fluidity [790,794,811] while the presence of both hydrophilic and lipophilic moieties facilitates the neutralization of both aqueous and lipophilic free radicals including hydroxyl radical (•OH) and hydroperoxyl radical (•OOH) [126,812,813]. The fact that melatonin prevents lipid peroxidation cascades and stabilizes lipid Lo-Ld phase separation over a range of temperatures to prevent the formation of non-raft Ld phase become especially meaningful when reports from correlative studies identified lipid peroxidation as the primary pathogenic event associated with the propagation of PK-resistant PrPres converted from physiological PrPC [814]. Hence, without viable prions to contain damages of free hemin caused by excess oxidative stress, hemin aggregates bound to RBC membranes can reorganize membrane lipid composition to induce membrane disorder and permeabilization [709].
It is apparent that the role of melatonin in attenuating lipid peroxidation, preserving lipid raft and band 3 integrity, and supporting prion physiological functions can effectively terminate negative feedback influences that exacerbate MDR in TMEs. Even though melatonin has been demonstrated to both increase and inhibit prion expression, the seemingly controversial pleiotropic features of melatonin only accentuate its ultimate functions acting as a “broad-based metabolic buffer” that can support prion physiological stress-response functions but suppress pathological, self-templating aggregates activated by hypoxic, stress-laden TMEs (Figure 2).
4.3. The Pleiotropic Effects of Melatonin in the Regulation of Prions in Cancer Multidrug Resistance
Various experimental studies demonstrated that low levels of melatonin upregulate the expression of PrPC, stimulating antioxidant, protective, survival responses. Both in vitro and in vivo studies reported that melatonin upregulated the expression of PrPC to rescue mesenchymal stem cells (MSCs) from oxidative stress-induced apoptosis at only 1 μM concentration [113], whereas silencing of PrPC inhibited all melatonin-mediated therapeutic effects on MSC proliferation and functionality at the same 1 μM dose [118]. A quantity of 1 μM melatonin co-administered with 5 μM pioglitazone not only prevented indoxyl sulfate-induced senescence but also promoted high growth rates in MSCs [647]. Treatment of human renal proximal tubule epithelial (TH1) cells with 1 μM melatonin increased expression of PrPC to augment antioxidant effects against high glucose-mediated fibrosis, successfully preventing fibrotic phenotype changes [648] (Table 1). Alternatively, in order to inhibit or reverse prion-mediated oncogenic effects and drug resistance, a much higher dosage is often used instead.
In a high oxidative TME, adequate NADH may be necessary to serve as essential substrates for CYB5R3 to reduce MetHb from ferric to ferrous heme [629,630]. Experimental studies showed that at 2 mM concentration, melatonin provided the greatest protection against loss of NADH from exposure to 500 µM orthovanadate (Va5+) incubation [642], whereas to reverse acid pHe, a lower but continuous presence of melatonin was demonstrated to be requisite [489]. Hence, even though 1 mM melatonin was able to significantly reduce in vitro proliferation and migration in murine melanoma B16-F10 cells, in vivo B16-F10 murine models using C57BL/6J mice treated with melatonin at 20 mg/kg (intraperitoneal injection or drinking water) matching in vitro dosage were unable to prevent metastasis or curb proliferation [649] (Table 1). C57BL/6J are inbred mice expressing severely truncated AANAT that results in complete melatonin “knockdown” [766]. It is possible that 20 mg/kg melatonin supplementation via intraperitoneal injection or drinking water in murine models incapable of producing melatonin did not provide a continuous presence of melatonin required to reverse acidic pHe conditions that promote melanoma metastasis and proliferation [649,815]. However, 1 mM melatonin did promote colorectal cancer cell apoptosis by decreasing expression of PrPC and PINK1 to increase superoxide accumulation resulting in mitochondria-mediated cell death. The effects of melatonin were amplified when PrPC was completely knocked down [114]. By contrast, in a non-cancerous environment, melatonin upregulated PrPC and PINK1 where MSC harvested from chronic kidney disease mouse models treated with 100 μM melatonin exhibited reduced H2O-induced senescence compared to normal mouse MSC [113] (Table 1).
The interactions between prions and lipid rafts may also affect cancer stem cell regulation. Lipid rafts and caveolae play important roles in maintaining the self-renewal of embryonic stem (ES) cells by facilitating receptor-mediated signal transductions [816,817]. Cancer cells and ES cells share common gene transcription regulators such as Oct4 which contributes to pluripotency [818,819,820]. PrPC is able to regulate cancer stem cell properties via interactions with stem cell marker proteins [66]. By interacting with human mesenchymal-epithelial transition factor (c-MET), PrPC upregulated Oct4 to enhance cancer stem cell characteristics in colorectal cancer [821]. In various specimens from colorectal cancer patients, PrPC was found to directly regulate Oct4, and the expression of PrPC and Oct4 were both upregulated and correlated significantly with metastasis and tumor stages [115]. Melatonin, not surprisingly, can enhance drug sensitivity, inhibiting colon cancer progression by regulating PrPC interactions with Oct4. Treating human colon cancer stem cells (CSCs) with 500 μM melatonin and 1 μM 5-fluorouracil (5-FU) caused apoptosis and inhibited expression of the stem cell marker Oct4 by inhibition of PrPC expression [115]. When used in combination with 1 μM oxaliplatin, 500 μM MEL melatonin promoted apoptosis of oxaliplatin-resistant colorectal cancer cells, again, by inhibition of PrPC [116]. Overexpression of PrPC plays a vital role in colorectal cancer oxaliplatin-resistance via enhanced superoxide dismutase (SOD) and catalase antioxidant activities, and oxaliplatin-resistance cancer cells often exhibit reduced intracellular superoxide anion generation. In addition, by inhibiting PrPC expression, melatonin can induce endoplasmic reticulum (ER) stress and apoptosis in oxaliplatin-resistant cells, effectively blocking oxaliplatin-associated elevation of SOD and catalase antioxidant activities [116] (Table 1).
The use of melatonin at appropriate levels relevant to context may be a principal consideration when targeting prion and associated biological functions such as stem cell regulation. In non-cancerous settings, melatonin has been demonstrated to enhance pluripotency and stem cell proliferation at 500 ng/L (2.15 nmol/L) by inducing the expression of stem cell markers including Oct4 [822]. At 10 nmol/L concentration in human non-cancer cells, melatonin selectively upregulated transcription of pluripotency and differentiation markers such as NANOG [823], completely contrary to findings in ovarian cancer stem cell experiments where melatonin inhibited the invasion and migration of cancer stem cells by inhibiting NANOG expression, albeit at exceptionally high concentrations between 3.4 and 6.3 mM [824]. It is tempting to hypothesize that at higher concentrations, melatonin can modulate inhospitable environment to attenuate PrPC stress responses, whereas lower levels stimulate and support the natural, physiological protective activities of prions.
5. Conclusions
Liquid–liquid phase separation is postulated as the fundamental process driving the formation and dissolution of biomolecular condensates as rapid, energy-efficient, adaptive survival responses to exogenous and endogenous stress. Melatonin and prions are both ancient, evolutionarily conserved molecules exhibiting synergistic relationships that are integral to the stress response pathways employed ubiquitously by living organisms to counter exogenous and endogenous stress. Aberrant phase separation resulting in the aggregation of condensates may be implicated in the conversion of prions from physiological soluble isoforms to pathological, self-templating isoforms intended to enhance survival via non-Mendelian, epigenetic inheritance, which, ironically, may enhance cancer drug resistance in less-than-optimal tumor microenvironments. As a “broad-based metabolic buffer” in a highly-stressed TME, melatonin can not only temper pH and oxygen imbalances to support PrPC physiological functions and prevent phase separation-induced pathological aggregation and conversion, but may also modulate epigenetic adaptations promoting metastasis, invasion, and stemness by intervening heme-and membrane-PrPC interactions via redox activities and lipid homeostasis and lipid phase transition stabilization, respectively. If the in silico observation of increased expression of PrPC in cancer cells under optimal conditions does not modulate proliferation, resistance to cell death, and metabolism can be independently confirmed by in vitro/in vivo studies, then the concept of melatonin as a “broad-based metabolic buffer” characterized by exceptional antioxidant-dependent and -independent features that can fine-tune the tumor microenvironment at appropriate or even continuous applications may be an additional, but perhaps essential, consideration as a viable therapeutic solution to counter cancer MDR.
Acknowledgments
Special thanks to Allan Lenon Cura for the preparation and design of the graphic illustration.
Abbreviations
| 3OHM | 3-hydroxymelatonin |
| Aβ | β-amyloid peptide |
| Aβo | amyloid-β oligomers |
| Akt | protein kinase B |
| ATP | adenosine triphosphate |
| COX | cytochrome c oxidase |
| CYB5R3 | NADH-cytochrome b5 reductase 3 |
| DNA | deoxyribonucleic acid |
| ER | endoplasmic reticulum |
| ES | embryonic stem |
| G6P | glucose 6-phosphate |
| G6PD | glucose-6-phosphate-dehydrogenase |
| Ga | giga annum (billion years) |
| GLUT1 | glucose transporter 1 |
| GOE | great oxidation event |
| H+ | hydrogen proton |
| H2O2 | hydrogen peroxide |
| IDR | intrinsically disordered region |
| Ld | liquid disordered |
| Lo | liquid ordered |
| LLPS | liquid–liquid phase separation |
| mM | millimolar |
| μM | micromolar |
| MD | molecular dynamics |
| MetHb | methemoglobin |
| MLO | membraneless organelle |
| MSC | mesenchymal stem cell |
| NAD+ | nicotinamide adenine dinucleotide |
| NADH | nicotinamide adenine dinucleotide hydrogen |
| NLRP3 | NLR pyrin domain containing 3 (inflammasome) |
| nM | nanomolar |
| •OH | hydroxyl radical |
| •OOH | hydroperoxyl radical |
| OXPHOS | oxidative phosphorylation |
| pHe | extracellular pH |
| pHi | intracellular pH |
| PI3K | phosphoinositide 3-kinase |
| POPE | 1-palmitoyl-2-oleoyl-sn-glycero-3-phosphatidylethanolamine |
| POPC | 1-palmitoyl-2-oleoyl-sn-glycero-3-phosphatidylcholine |
| PTM | post-translational modification |
| RBC | red blood cell |
| RCF | red cell flux |
| Redox | oxidation-reduction |
| RNA | ribonucleic acid |
| RNP | ribonucleoprotein |
| ROS | reactive oxygen species |
| UPS | ubiquitin-protease system |
| UVR | ultraviolet radiation |
| VDA | vascular disrupting agent |
| WT | wild-type |
Author Contributions
Conceptualization and writing, D.L.; review and editing, R.J.R. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Zabel M.D., Reid C. A Brief History of Prions. Pathog. Dis. 2015;73:ftv087. doi: 10.1093/femspd/ftv087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Prusiner S.B. Novel Proteinaceous Infectious Particles Cause Scrapie. Science. 1982;216:136–144. doi: 10.1126/science.6801762. [DOI] [PubMed] [Google Scholar]
- 3.Prusiner S.B. Prions. Proc. Natl. Acad. Sci. USA. 1998;95:13363–13383. doi: 10.1073/pnas.95.23.13363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Riek R., Hornemann S., Wider G., Glockshuber R., Wüthrich K. NMR Characterization of the Full-Length Recombinant Murine Prion Protein, mPrP(23-231) FEBS Lett. 1997;413:282–288. doi: 10.1016/S0014-5793(97)00920-4. [DOI] [PubMed] [Google Scholar]
- 5.Castle A.R., Gill A.C. Physiological Functions of the Cellular Prion Protein. Front. Mol. Biosci. 2017;4:19. doi: 10.3389/fmolb.2017.00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Peralta O.A., Huckle W.R., Eyestone W.H. Expression and Knockdown of Cellular Prion Protein (PrPC) in Differentiating Mouse Embryonic Stem Cells. Differentiation. 2011;81:68–77. doi: 10.1016/j.diff.2010.09.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Miranda A., Ramos-Ibeas P., Pericuesta E., Ramirez M.A., Gutierrez-Adan A. The Role of Prion Protein in Stem Cell Regulation. Reproduction. 2013;146:R91–R99. doi: 10.1530/REP-13-0100. [DOI] [PubMed] [Google Scholar]
- 8.Lee Y.J., Baskakov I.V. The Cellular Form of the Prion Protein Guides the Differentiation of Human Embryonic Stem Cells into Neuron-, Oligodendrocyte-, and Astrocyte-Committed Lineages. Prion. 2014;8:266–275. doi: 10.4161/pri.32079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Garcia D.M., Campbell E.A., Jakobson C.M., Tsuchiya M., Shaw E.A., DiNardo A.L., Kaeberlein M., Jarosz D.F. A Prion Accelerates Proliferation at the Expense of Lifespan. Elife. 2021;10:e60917. doi: 10.7554/eLife.60917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Málaga-Trillo E., Solis G.P., Schrock Y., Geiss C., Luncz L., Thomanetz V., Stuermer C.A.O. Regulation of Embryonic Cell Adhesion by the Prion Protein. PLoS Biol. 2009;7:e55. doi: 10.1371/journal.pbio.1000055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bremer J., Baumann F., Tiberi C., Wessig C., Fischer H., Schwarz P., Steele A.D., Toyka K.V., Nave K.-A., Weis J., et al. Axonal Prion Protein Is Required for Peripheral Myelin Maintenance. Nat. Neurosci. 2010;13:310–318. doi: 10.1038/nn.2483. [DOI] [PubMed] [Google Scholar]
- 12.Tobler I., Gaus S.E., Deboer T., Achermann P., Fischer M., Rülicke T., Moser M., Oesch B., McBride P.A., Manson J.C. Altered Circadian Activity Rhythms and Sleep in Mice Devoid of Prion Protein. Nature. 1996;380:639–642. doi: 10.1038/380639a0. [DOI] [PubMed] [Google Scholar]
- 13.Cagampang F.R., Whatley S.A., Mitchell A.L., Powell J.F., Campbell I.C., Coen C.W. Circadian Regulation of Prion Protein Messenger RNA in the Rat Forebrain: A Widespread and Synchronous Rhythm. Neuroscience. 1999;91:1201–1204. doi: 10.1016/S0306-4522(99)00092-5. [DOI] [PubMed] [Google Scholar]
- 14.Liebert A., Bicknell B., Adams R. Prion Protein Signaling in the Nervous System—A Review and Perspective. Sign. Transduct. Insights. 2014;3:STI.S12319. doi: 10.4137/STI.S12319. [DOI] [Google Scholar]
- 15.Ashok A., Singh N. Prion Protein Modulates Glucose Homeostasis by Altering Intracellular Iron. Sci. Rep. 2018;8:6556. doi: 10.1038/s41598-018-24786-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Strom A., Wang G.-S., Scott F.W. Impaired Glucose Tolerance in Mice Lacking Cellular Prion Protein. Pancreas. 2011;40:229–232. doi: 10.1097/MPA.0b013e3181f7e547. [DOI] [PubMed] [Google Scholar]
- 17.Isaacs J.D., Jackson G.S., Altmann D.M. The Role of the Cellular Prion Protein in the Immune System. Clin. Exp. Immunol. 2006;146:1–8. doi: 10.1111/j.1365-2249.2006.03194.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Aucouturier P., Carp R.I., Carnaud C., Wisniewski T. Prion Diseases and the Immune System. Clin. Immunol. 2000;96:79–85. doi: 10.1006/clim.2000.4875. [DOI] [PubMed] [Google Scholar]
- 19.Rachidi W., Vilette D., Guiraud P., Arlotto M., Riondel J., Laude H., Lehmann S., Favier A. Expression of Prion Protein Increases Cellular Copper Binding and Antioxidant Enzyme Activities but Not Copper Delivery. J. Biol. Chem. 2003;278:9064–9072. doi: 10.1074/jbc.M211830200. [DOI] [PubMed] [Google Scholar]
- 20.Alfaidy N., Chauvet S., Donadio-Andrei S., Salomon A., Saoudi Y., Richaud P., Aude-Garcia C., Hoffmann P., Andrieux A., Moulis J.-M., et al. Prion Protein Expression and Functional Importance in Developmental Angiogenesis: Role in Oxidative Stress and Copper Homeostasis. Antioxid. Redox Signal. 2013;18:400–411. doi: 10.1089/ars.2012.4637. [DOI] [PubMed] [Google Scholar]
- 21.Haldar S., Tripathi A., Qian J., Beserra A., Suda S., McElwee M., Turner J., Hopfer U., Singh N. Prion Protein Promotes Kidney Iron Uptake via Its Ferrireductase Activity. J. Biol. Chem. 2015;290:5512–5522. doi: 10.1074/jbc.M114.607507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Singh A., Haldar S., Horback K., Tom C., Zhou L., Meyerson H., Singh N. Prion Protein Regulates Iron Transport by Functioning as a Ferrireductase. J. Alzheimers Dis. 2013;35:541–552. doi: 10.3233/JAD-130218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Singh A., Kong Q., Luo X., Petersen R.B., Meyerson H., Singh N. Prion Protein (PrP) Knock-out Mice Show Altered Iron Metabolism: A Functional Role for PrP in Iron Uptake and Transport. PLoS ONE. 2009;4:e6115. doi: 10.1371/journal.pone.0006115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Si K., Kandel E.R. The Role of Functional Prion-Like Proteins in the Persistence of Memory. Cold Spring Harb. Perspect. Biol. 2016;8:a021774. doi: 10.1101/cshperspect.a021774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pearson H. Prion Proteins May Store Memories. Nature. 2003 doi: 10.1038/news031229-2. [DOI] [Google Scholar]
- 26.Fagerberg L., Hallström B.M., Oksvold P., Kampf C., Djureinovic D., Odeberg J., Habuka M., Tahmasebpoor S., Danielsson A., Edlund K., et al. Analysis of the Human Tissue-Specific Expression by Genome-Wide Integration of Transcriptomics and Antibody-Based Proteomics. Mol. Cell. Proteom. 2014;13:397–406. doi: 10.1074/mcp.M113.035600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.PRNP Prion Protein [Homo Sapiens (Human)]-Gene—NCBI. [(accessed on 12 December 2021)]; Available online: https://www.ncbi.nlm.nih.gov/gene/5621.
- 28.Faris R., Moore R.A., Ward A., Race B., Dorward D.W., Hollister J.R., Fischer E.R., Priola S.A. Cellular Prion Protein Is Present in Mitochondria of Healthy Mice. Sci. Rep. 2017;7:41556. doi: 10.1038/srep41556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Masison D.C., Wickner R.B. Prion-Inducing Domain of Yeast Ure2p and Protease Resistance of Ure2p in Prion-Containing Cells. Science. 1995;270:93–95. doi: 10.1126/science.270.5233.93. [DOI] [PubMed] [Google Scholar]
- 30.Wickner R.B. [URE3] as an Altered URE2 Protein: Evidence for a Prion Analog in Saccharomyces Cerevisiae. Science. 1994;264:566–569. doi: 10.1126/science.7909170. [DOI] [PubMed] [Google Scholar]
- 31.Patino M.M., Liu J.J., Glover J.R., Lindquist S. Support for the Prion Hypothesis for Inheritance of a Phenotypic Trait in Yeast. Science. 1996;273:622–626. doi: 10.1126/science.273.5275.622. [DOI] [PubMed] [Google Scholar]
- 32.True H.L., Lindquist S.L. A Yeast Prion Provides a Mechanism for Genetic Variation and Phenotypic Diversity. Nature. 2000;407:477–483. doi: 10.1038/35035005. [DOI] [PubMed] [Google Scholar]
- 33.True H.L., Berlin I., Lindquist S.L. Epigenetic Regulation of Translation Reveals Hidden Genetic Variation to Produce Complex Traits. Nature. 2004;431:184–187. doi: 10.1038/nature02885. [DOI] [PubMed] [Google Scholar]
- 34.Shorter J., Lindquist S. Prions as Adaptive Conduits of Memory and Inheritance. Nat. Rev. Genet. 2005;6:435–450. doi: 10.1038/nrg1616. [DOI] [PubMed] [Google Scholar]
- 35.Wiltzius J.J.W., Landau M., Nelson R., Sawaya M.R., Apostol M.I., Goldschmidt L., Soriaga A.B., Cascio D., Rajashankar K., Eisenberg D. Molecular Mechanisms for Protein-Encoded Inheritance. Nat. Struct. Mol. Biol. 2009;16:973–978. doi: 10.1038/nsmb.1643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tuite M.F., Serio T.R. The Prion Hypothesis: From Biological Anomaly to Basic Regulatory Mechanism. Nat. Rev. Mol. Cell Biol. 2010;11:823–833. doi: 10.1038/nrm3007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Halfmann R., Jarosz D.F., Jones S.K., Chang A., Lancaster A.K., Lindquist S. Prions Are a Common Mechanism for Phenotypic Inheritance in Wild Yeasts. Nature. 2012;482:363–368. doi: 10.1038/nature10875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wickner R.B., Edskes H.K., Bateman D.A., Kelly A.C., Gorkovskiy A., Dayani Y., Zhou A. Amyloids and Yeast Prion Biology. Biochemistry. 2013;52:1514–1527. doi: 10.1021/bi301686a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Harvey Z.H., Chen Y., Jarosz D.F. Protein-Based Inheritance: Epigenetics beyond the Chromosome. Mol. Cell. 2018;69:195–202. doi: 10.1016/j.molcel.2017.10.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Harvey Z.H., Chakravarty A.K., Futia R.A., Jarosz D.F. A Prion Epigenetic Switch Establishes an Active Chromatin State. Cell. 2020;180:928–940.e14. doi: 10.1016/j.cell.2020.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Manjrekar J. Epigenetic Inheritance, Prions and Evolution. J. Genet. 2017;96:445–456. doi: 10.1007/s12041-017-0798-3. [DOI] [PubMed] [Google Scholar]
- 42.Sanders D.W., Kaufman S.K., Holmes B.B., Diamond M.I. Prions and Protein Assemblies That Convey Biological Information in Health and Disease. Neuron. 2016;89:433–448. doi: 10.1016/j.neuron.2016.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Newby G.A., Lindquist S. Blessings in Disguise: Biological Benefits of Prion-like Mechanisms. Trends Cell Biol. 2013;23:251–259. doi: 10.1016/j.tcb.2013.01.007. [DOI] [PubMed] [Google Scholar]
- 44.Halfmann R., Alberti S., Lindquist S. Prions, Protein Homeostasis, and Phenotypic Diversity. Trends Cell Biol. 2010;20:125–133. doi: 10.1016/j.tcb.2009.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Garcia D.M., Jarosz D.F. Rebels with a Cause: Molecular Features and Physiological Consequences of Yeast Prions. FEMS Yeast Res. 2014;14:136–147. doi: 10.1111/1567-1364.12116. [DOI] [PubMed] [Google Scholar]
- 46.Antony H., Wiegmans A.P., Wei M.Q., Chernoff Y.O., Khanna K.K., Munn A.L. Potential Roles for Prions and Protein-Only Inheritance in Cancer. Cancer Metastasis Rev. 2012;31:1–19. doi: 10.1007/s10555-011-9325-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Senft D., Ronai Z.E.A. Adaptive Stress Responses during Tumor Metastasis and Dormancy. Trends Cancer Res. 2016;2:429–442. doi: 10.1016/j.trecan.2016.06.004. [DOI] [PubMed] [Google Scholar]
- 48.Easwaran H., Tsai H.-C., Baylin S.B. Cancer Epigenetics: Tumor Heterogeneity, Plasticity of Stem-like States, and Drug Resistance. Mol. Cell. 2014;54:716–727. doi: 10.1016/j.molcel.2014.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Oamen H.P., Lau Y., Caudron F. Prion-like Proteins as Epigenetic Devices of Stress Adaptation. Exp. Cell Res. 2020;396:112262. doi: 10.1016/j.yexcr.2020.112262. [DOI] [PubMed] [Google Scholar]
- 50.Harris J.F., Chambers A.F., Hill R.P., Ling V. Metastatic Variants Are Generated Spontaneously at a High Rate in Mouse KHT Tumor. Proc. Natl. Acad. Sci. USA. 1982;79:5547–5551. doi: 10.1073/pnas.79.18.5547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fernandez-Bellot E., Guillemet E., Cullin C. The Yeast Prion [URE3] Can Be Greatly Induced by a Functional Mutated URE2 Allele. EMBO J. 2000;19:3215–3222. doi: 10.1093/emboj/19.13.3215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Quintana E., Shackleton M., Foster H.R., Fullen D.R., Sabel M.S., Johnson T.M., Morrison S.J. Phenotypic Heterogeneity among Tumorigenic Melanoma Cells from Patients That Is Reversible and Not Hierarchically Organized. Cancer Cell. 2010;18:510–523. doi: 10.1016/j.ccr.2010.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Derkatch I.L., Bradley M.E., Zhou P., Chernoff Y.O., Liebman S.W. Genetic and Environmental Factors Affecting the de Novo Appearance of the [PSI+] Prion in Saccharomyces Cerevisiae. Genetics. 1997;147:507–519. doi: 10.1093/genetics/147.2.507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Liang J., Pan Y.L., Ning X.X., Sun L.J., Lan M., Hong L., Du J.P., Liu N., Liu C.J., Qiao T.D., et al. Overexpression of PrPC and Its Antiapoptosis Function in Gastric Cancer. Tumour Biol. 2006;27:84–91. doi: 10.1159/000092488. [DOI] [PubMed] [Google Scholar]
- 55.Mehrpour M., Codogno P. Prion Protein: From Physiology to Cancer Biology. Cancer Lett. 2010;290:1–23. doi: 10.1016/j.canlet.2009.07.009. [DOI] [PubMed] [Google Scholar]
- 56.Dalai W., Matsuo E., Takeyama N., Kawano J., Saeki K. Increased Expression of Prion Protein Gene Is Accompanied by Demethylation of CpG Sites in a Mouse Embryonal Carcinoma Cell Line, P19C6. J. Vet. Med. Sci. 2017;79:644–648. doi: 10.1292/jvms.16-0554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kim Y.-C., Won S.-Y., Jeong B.-H. Identification of Prion Disease-Related Somatic Mutations in the Prion Protein Gene (PRNP) in Cancer Patients. Cells. 2020;9:1480. doi: 10.3390/cells9061480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Liang J., Pan Y., Zhang D., Guo C., Shi Y., Wang J., Chen Y., Wang X., Liu J., Guo X., et al. Cellular Prion Protein Promotes Proliferation and G1/S Transition of Human Gastric Cancer Cells SGC7901 and AGS. FASEB J. 2007;21:2247–2256. doi: 10.1096/fj.06-7799com. [DOI] [PubMed] [Google Scholar]
- 59.Liang J., Bai F., Luo G., Wang J., Liu J., Ge F., Pan Y., Yao L., Du R., Li X., et al. Hypoxia Induced Overexpression of PrP(C) in Gastric Cancer Cell Lines. Cancer Biol. Ther. 2007;6:769–774. doi: 10.4161/cbt.6.5.4001. [DOI] [PubMed] [Google Scholar]
- 60.Yap Y.H.-Y., Say Y.-H. Resistance against Apoptosis by the Cellular Prion Protein Is Dependent on Its Glycosylation Status in Oral HSC-2 and Colon LS 174T Cancer Cells. Cancer Lett. 2011;306:111–119. doi: 10.1016/j.canlet.2011.02.040. [DOI] [PubMed] [Google Scholar]
- 61.Wang Y.-M., Jin B.-Z., Ai F., Duan C.-H., Lu Y.-Z., Dong T.-F., Fu Q.-L. The Efficacy and Safety of Melatonin in Concurrent Chemotherapy or Radiotherapy for Solid Tumors: A Meta-Analysis of Randomized Controlled Trials. Cancer Chemother. Pharmacol. 2012;69:1213–1220. doi: 10.1007/s00280-012-1828-8. [DOI] [PubMed] [Google Scholar]
- 62.Wang Q., Qian J., Wang F., Ma Z. Cellular Prion Protein Accelerates Colorectal Cancer Metastasis via the Fyn-SP1-SATB1 Axis. Oncol. Rep. 2012;28:2029–2034. doi: 10.3892/or.2012.2025. [DOI] [PubMed] [Google Scholar]
- 63.Du L., Rao G., Wang H., Li B., Tian W., Cui J., He L., Laffin B., Tian X., Hao C., et al. CD44-Positive Cancer Stem Cells Expressing Cellular Prion Protein Contribute to Metastatic Capacity in Colorectal Cancer. Cancer Res. 2013;73:2682–2694. doi: 10.1158/0008-5472.CAN-12-3759. [DOI] [PubMed] [Google Scholar]
- 64.Martin-Lannerée S., Hirsch T.Z., Hernandez-Rapp J., Halliez S., Vilotte J.-L., Launay J.-M., Mouillet-Richard S. PrP(C) from Stem Cells to Cancer. Front. Cell Dev. Biol. 2014;2:55. doi: 10.3389/fcell.2014.00055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Corsaro A., Bajetto A., Thellung S., Begani G., Villa V., Nizzari M., Pattarozzi A., Solari A., Gatti M., Pagano A., et al. Cellular Prion Protein Controls Stem Cell-like Properties of Human Glioblastoma Tumor-Initiating Cells. Oncotarget. 2016;7:38638–38657. doi: 10.18632/oncotarget.9575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Go G., Lee S.H. The Cellular Prion Protein: A Promising Therapeutic Target for Cancer. Int. J. Mol. Sci. 2020;21:9208. doi: 10.3390/ijms21239208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ke J., Wu G., Zhang J., Li H., Gao S., Shao M., Gao Z., Sy M.-S., Cao Y., Yang X., et al. Melanoma Migration Is Promoted by Prion Protein via Akt-hsp27 Signaling Axis. Biochem. Biophys. Res. Commun. 2020;523:375–381. doi: 10.1016/j.bbrc.2019.12.042. [DOI] [PubMed] [Google Scholar]
- 68.Bing T., Wang J., Shen L., Liu X., Shangguan D. Prion Protein Targeted by a Prostate Cancer Cell Binding Aptamer, a Potential Tumor Marker? ACS Appl. Bio Mater. 2020;3:2658–2665. doi: 10.1021/acsabm.0c00024. [DOI] [PubMed] [Google Scholar]
- 69.Cha S., Sin M.J., Kim M.J., Kim H.J., Kim Y.S., Choi E.K., Kim M.Y. Involvement of Cellular Prion Protein in Invasion and Metastasis of Lung Cancer by Inducing Treg Cell Development. Biomolecules. 2021;11:285. doi: 10.3390/biom11020285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mouillet-Richard S., Ghazi A., Laurent-Puig P. The Cellular Prion Protein and the Hallmarks of Cancer. Cancers. 2021;13:5032. doi: 10.3390/cancers13195032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ryskalin L., Biagioni F., Busceti C.L., Giambelluca M.A., Morelli L., Frati A., Fornai F. The Role of Cellular Prion Protein in Promoting Stemness and Differentiation in Cancer. Cancers. 2021;13:170. doi: 10.3390/cancers13020170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Chernoff Y.O. Stress and Prions: Lessons from the Yeast Model. FEBS Lett. 2007;581:3695–3701. doi: 10.1016/j.febslet.2007.04.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Suzuki G., Shimazu N., Tanaka M. A Yeast Prion, Mod5, Promotes Acquired Drug Resistance and Cell Survival under Environmental Stress. Science. 2012;336:355–359. doi: 10.1126/science.1219491. [DOI] [PubMed] [Google Scholar]
- 74.Déry M.-A., Jodoin J., Ursini-Siegel J., Aleynikova O., Ferrario C., Hassan S., Basik M., LeBlanc A.C. Endoplasmic Reticulum Stress Induces PRNP Prion Protein Gene Expression in Breast Cancer. Breast Cancer Res. 2013;15:R22. doi: 10.1186/bcr3398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hinton C., Antony H., Hashimi S.M., Munn A., Wei M.Q. Significance of Prion and Prion-like Proteins in Cancer Development, Progression and Multi-Drug Resistance. Curr. Cancer Drug Targets. 2013;13:895–904. doi: 10.2174/156800961131300092. [DOI] [PubMed] [Google Scholar]
- 76.Du J., Pan Y., Shi Y., Guo C., Jin X., Sun L., Liu N., Qiao T., Fan D. Overexpression and Significance of Prion Protein in Gastric Cancer and Multidrug-Resistant Gastric Carcinoma Cell Line SGC7901/ADR. Int. J. Cancer. 2005;113:213–220. doi: 10.1002/ijc.20570. [DOI] [PubMed] [Google Scholar]
- 77.Li Q.-Q., Cao X.-X., Xu J.-D., Chen Q., Wang W.-J., Tang F., Chen Z.-Q., Liu X.-P., Xu Z.-D. The Role of P-Glycoprotein/cellular Prion Protein Interaction in Multidrug-Resistant Breast Cancer Cells Treated with Paclitaxel. Cell. Mol. Life Sci. 2009;66:504–515. doi: 10.1007/s00018-008-8548-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ryskalin L., Busceti C.L., Biagioni F., Limanaqi F., Familiari P., Frati A., Fornai F. Prion Protein in Glioblastoma Multiforme. Int. J. Mol. Sci. 2019;20:5107. doi: 10.3390/ijms20205107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Lee J.H., Yun C.W., Lee S.H. Cellular Prion Protein Enhances Drug Resistance of Colorectal Cancer Cells via Regulation of a Survival Signal Pathway. Biomol. Ther. 2018;26:313–321. doi: 10.4062/biomolther.2017.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Meslin F., Hamaï A., Gao P., Jalil A., Cahuzac N., Chouaib S., Mehrpour M. Silencing of Prion Protein Sensitizes Breast Adriamycin-Resistant Carcinoma Cells to TRAIL-Mediated Cell Death. Cancer Res. 2007;67:10910–10919. doi: 10.1158/0008-5472.CAN-07-0512. [DOI] [PubMed] [Google Scholar]
- 81.Yun C.W., Yun S., Lee J.H., Han Y.-S., Yoon Y.M., An D., Lee S.H. Silencing Prion Protein in HT29 Human Colorectal Cancer Cells Enhances Anticancer Response to Fucoidan. Anticancer Res. 2016;36:4449–4458. doi: 10.21873/anticanres.10989. [DOI] [PubMed] [Google Scholar]
- 82.Meslin F., Conforti R., Mazouni C., Morel N., Tomasic G., Drusch F., Yacoub M., Sabourin J.C., Grassi J., Delaloge S., et al. Efficacy of Adjuvant Chemotherapy according to Prion Protein Expression in Patients with Estrogen Receptor-Negative Breast Cancer. Ann. Oncol. 2007;18:1793–1798. doi: 10.1093/annonc/mdm406. [DOI] [PubMed] [Google Scholar]
- 83.Wickner R.B., Kelly A.C. Prions Are Affected by Evolution at Two Levels. Cell. Mol. Life Sci. 2016;73:1131–1144. doi: 10.1007/s00018-015-2109-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Yu W., Chen Y., Dubrulle J., Stossi F., Putluri V., Sreekumar A., Putluri N., Baluya D., Lai S.Y., Sandulache V.C. Cisplatin Generates Oxidative Stress Which Is Accompanied by Rapid Shifts in Central Carbon Metabolism. Sci. Rep. 2018;8:4306. doi: 10.1038/s41598-018-22640-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Cepeda V., Fuertes M.A., Castilla J., Alonso C., Quevedo C., Pérez J.M. Biochemical Mechanisms of Cisplatin Cytotoxicity. Anticancer Agents Med. Chem. 2007;7:3–18. doi: 10.2174/187152007779314044. [DOI] [PubMed] [Google Scholar]
- 86.Pilco-Ferreto N., Calaf G.M. Influence of Doxorubicin on Apoptosis and Oxidative Stress in Breast Cancer Cell Lines. Int. J. Oncol. 2016;49:753–762. doi: 10.3892/ijo.2016.3558. [DOI] [PubMed] [Google Scholar]
- 87.Barciszewska A.-M., Gurda D., Głodowicz P., Nowak S., Naskręt-Barciszewska M.Z. A New Epigenetic Mechanism of Temozolomide Action in Glioma Cells. PLoS ONE. 2015;10:e0136669. doi: 10.1371/journal.pone.0136669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Atkinson C.J., Kawamata F., Liu C., Ham S., Győrffy B., Munn A.L., Wei M.Q., Möller A., Whitehall V., Wiegmans A.P. EGFR and Prion Protein Promote Signaling via FOXO3a-KLF5 Resulting in Clinical Resistance to Platinum Agents in Colorectal Cancer. Mol. Oncol. 2019;13:725–737. doi: 10.1002/1878-0261.12411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Chieng C.K.-L., Say Y.-H. Cellular Prion Protein Contributes to LS 174T Colon Cancer Cell Carcinogenesis by Increasing Invasiveness and Resistance against Doxorubicin-Induced Apoptosis. Tumour Biol. 2015;36:8107–8120. doi: 10.1007/s13277-015-3530-z. [DOI] [PubMed] [Google Scholar]
- 90.Klamt F., Dal-Pizzol F., Conte da Frota M.L., Jr., Walz R., Andrades M.E., da Silva E.G., Brentani R.R., Izquierdo I., Fonseca Moreira J.C. Imbalance of Antioxidant Defense in Mice Lacking Cellular Prion Protein. Free Radic. Biol. Med. 2001;30:1137–1144. doi: 10.1016/S0891-5849(01)00512-3. [DOI] [PubMed] [Google Scholar]
- 91.Watt N.T., Routledge M.N., Wild C.P., Hooper N.M. Cellular Prion Protein Protects against Reactive-Oxygen-Species-Induced DNA Damage. Free Radic. Biol. Med. 2007;43:959–967. doi: 10.1016/j.freeradbiomed.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 92.Arnould H., Baudouin V., Baudry A., Ribeiro L.W., Ardila-Osorio H., Pietri M., Caradeuc C., Soultawi C., Williams D., Alvarez M., et al. Loss of Prion Protein Control of Glucose Metabolism Promotes Neurodegeneration in Model of Prion Diseases. PLoS Pathog. 2021;17:e1009991. doi: 10.1371/journal.ppat.1009991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Viles J.H., Cohen F.E., Prusiner S.B., Goodin D.B., Wright P.E., Dyson H.J. Copper Binding to the Prion Protein: Structural Implications of Four Identical Cooperative Binding Sites. Proc. Natl. Acad. Sci. USA. 1999;96:2042–2047. doi: 10.1073/pnas.96.5.2042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Wiegmans A.P., Saunus J.M., Ham S., Lobb R., Kutasovic J.R., Dalley A.J., Miranda M., Atkinson C., Foliaki S.T., Ferguson K., et al. Secreted Cellular Prion Protein Binds Doxorubicin and Correlates with Anthracycline Resistance in Breast Cancer. JCI Insight. 2019;5:e124092. doi: 10.1172/jci.insight.124092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Zhuang D., Liu Y., Mao Y., Gao L., Zhang H., Luan S., Huang F., Li Q. TMZ-Induced PrPc/par-4 Interaction Promotes the Survival of Human Glioma Cells. Int. J. Cancer. 2012;130:309–318. doi: 10.1002/ijc.25985. [DOI] [PubMed] [Google Scholar]
- 96.Li X., Shao F., Sun J., Du K., Sun Y., Feng F. Enhanced Copper-Temozolomide Interactions by Protein for Chemotherapy against Glioblastoma Multiforme. ACS Appl. Mater. Interfaces. 2019;11:41935–41945. doi: 10.1021/acsami.9b14849. [DOI] [PubMed] [Google Scholar]
- 97.Odeh L.H., Talib W.H., Basheti I.A. Synergistic Effect of Thymoquinone and Melatonin against Breast Cancer Implanted in Mice. J. Cancer Res. Ther. 2018;14:324–330. doi: 10.4103/0973-1482.235349. [DOI] [PubMed] [Google Scholar]
- 98.Zhelev Z., Ivanova D., Bakalova R., Aoki I., Higashi T. Synergistic Cytotoxicity of Melatonin and New-Generation Anticancer Drugs Against Leukemia Lymphocytes But Not Normal Lymphocytes. Anticancer Res. 2017;37:149–159. doi: 10.21873/anticanres.11300. [DOI] [PubMed] [Google Scholar]
- 99.Lin S., Hoffmann K., Gao C., Petrulionis M., Herr I., Schemmer P. Melatonin Promotes Sorafenib-Induced Apoptosis through Synergistic Activation of JNK/c-Jun Pathway in Human Hepatocellular Carcinoma. J. Pineal Res. 2017;62:e12398. doi: 10.1111/jpi.12398. [DOI] [PubMed] [Google Scholar]
- 100.Gurunathan S., Qasim M., Kang M.-H., Kim J.-H. Role and Therapeutic Potential of Melatonin in Various Type of Cancers. Onco. Targets. Ther. 2021;14:2019–2052. doi: 10.2147/OTT.S298512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Talib W.H., Alsayed A.R., Abuawad A., Daoud S., Mahmod A.I. Melatonin in Cancer Treatment: Current Knowledge and Future Opportunities. Molecules. 2021;26:2506. doi: 10.3390/molecules26092506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Schettig R., Sears T., Klein M., Tan-Lim R., Matthias R., Aussems C., Hummel M., Sears R., Poteet Z., Warren D., et al. Melatonin: A Powerful Integrative Adjunctive Agent for Oncology. J. Cancer Ther. 2020;11:571–596. doi: 10.4236/jct.2020.119049. [DOI] [Google Scholar]
- 103.Reiter R.J., Rosales-Corral S.A., Tan D.-X., Acuna-Castroviejo D., Qin L., Yang S.-F., Xu K. Melatonin, a Full Service Anti-Cancer Agent: Inhibition of Initiation, Progression and Metastasis. Int. J. Mol. Sci. 2017;18:843. doi: 10.3390/ijms18040843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Su S.-C., Hsieh M.-J., Yang W.-E., Chung W.-H., Reiter R.J., Yang S.-F. Cancer Metastasis: Mechanisms of Inhibition by Melatonin. J. Pineal Res. 2017;62:e12370. doi: 10.1111/jpi.12370. [DOI] [PubMed] [Google Scholar]
- 105.Di Bella G., Mascia F., Gualano L., Di Bella L. Melatonin Anticancer Effects: Review. Int. J. Mol. Sci. 2013;14:2410–2430. doi: 10.3390/ijms14022410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Mediavilla M.D., Sanchez-Barcelo E.J., Tan D.X., Manchester L., Reiter R.J. Basic Mechanisms Involved in the Anti-Cancer Effects of Melatonin. Curr. Med. Chem. 2010;17:4462–4481. doi: 10.2174/092986710794183015. [DOI] [PubMed] [Google Scholar]
- 107.Sánchez-Barceló E.J., Mediavilla M.D., Tan D.X., Reiter R.J. Clinical Uses of Melatonin: Evaluation of Human Trials. Curr. Med. Chem. 2010;17:2070–2095. doi: 10.2174/092986710791233689. [DOI] [PubMed] [Google Scholar]
- 108.Sainz R.M., Mayo J.C., Rodriguez C., Tan D.X., Lopez-Burillo S., Reiter R.J. Melatonin and Cell Death: Differential Actions on Apoptosis in Normal and Cancer Cells. Cell. Mol. Life Sci. 2003;60:1407–1426. doi: 10.1007/s00018-003-2319-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Reiter R.J., Tan D.-X., Sainz R.M., Mayo J.C., Lopez-Burillo S. Melatonin: Reducing the Toxicity and Increasing the Efficacy of Drugs. J. Pharm. Pharmacol. 2002;54:1299–1321. doi: 10.1211/002235702760345374. [DOI] [PubMed] [Google Scholar]
- 110.Vijayalaxmi, Thomas C.R., Jr., Reiter R.J., Herman T.S. Melatonin: From Basic Research to Cancer Treatment Clinics. J. Clin. Oncol. 2002;20:2575–2601. doi: 10.1200/JCO.2002.11.004. [DOI] [PubMed] [Google Scholar]
- 111.Panzer A., Viljoen M. The Validity of Melatonin as an Oncostatic Agent. J. Pineal Res. 1997;22:184–202. doi: 10.1111/j.1600-079X.1997.tb00322.x. [DOI] [PubMed] [Google Scholar]
- 112.Reiter R.J. Melatonin Suppression by Static and Extremely Low Frequency Electromagnetic Fields: Relationship to the Reported Increased Incidence of Cancer. Rev. Environ. Health. 1994;10:171–186. doi: 10.1515/REVEH.1994.10.3-4.171. [DOI] [PubMed] [Google Scholar]
- 113.Lee J.H., Yoon Y.M., Han Y.-S., Jung S.K., Lee S.H. Melatonin Protects Mesenchymal Stem Cells from Autophagy-Mediated Death under Ischaemic ER-Stress Conditions by Increasing Prion Protein Expression. Cell Prolif. 2019;52:e12545. doi: 10.1111/cpr.12545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Yun C.W., Kim S., Lee J.H., Lee S.H. Melatonin Promotes Apoptosis of Colorectal Cancer Cells via Superoxide-Mediated ER Stress by Inhibiting Cellular Prion Protein Expression. Anticancer Res. 2018;38:3951–3960. doi: 10.21873/anticanres.12681. [DOI] [PubMed] [Google Scholar]
- 115.Lee J.H., Yun C.W., Han Y.-S., Kim S., Jeong D., Kwon H.Y., Kim H., Baek M.-J., Lee S.H. Melatonin and 5-Fluorouracil Co-Suppress Colon Cancer Stem Cells by Regulating Cellular Prion Protein-Oct4 Axis. J. Pineal Res. 2018;65:e12519. doi: 10.1111/jpi.12519. [DOI] [PubMed] [Google Scholar]
- 116.Lee J.H., Yoon Y.M., Han Y.-S., Yun C.W., Lee S.H. Melatonin Promotes Apoptosis of Oxaliplatin-Resistant Colorectal Cancer Cells Through Inhibition of Cellular Prion Protein. Anticancer Res. 2018;38:1993–2000. doi: 10.21873/anticanres.12437. [DOI] [PubMed] [Google Scholar]
- 117.Salvesen Ø., Reiten M.R., Espenes A., Bakkebø M.K., Tranulis M.A., Ersdal C. LPS-Induced Systemic Inflammation Reveals an Immunomodulatory Role for the Prion Protein at the Blood-Brain Interface. J. Neuroinflamm. 2017;14:106. doi: 10.1186/s12974-017-0879-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Lee J.H., Han Y.-S., Lee S.H. Potentiation of Biological Effects of Mesenchymal Stem Cells in Ischemic Conditions by Melatonin via Upregulation of Cellular Prion Protein Expression. J. Pineal Res. 2017;62:e12385. doi: 10.1111/jpi.12385. [DOI] [PubMed] [Google Scholar]
- 119.Tian Q.-X., Zhang Z.-H., Ye Q.-L., Xu S., Hong Q., Xing W.-Y., Chen L., Yu D.-X., Xu D.-X., Xie D.-D. Melatonin Inhibits Migration and Invasion in LPS-Stimulated and -Unstimulated Prostate Cancer Cells Through Blocking Multiple EMT-Relative Pathways. J. Inflamm. Res. 2021;14:2253–2265. doi: 10.2147/JIR.S305450. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 120.Agarwal A., Rai S.K., Avni A., Mukhopadhyay S. An Intrinsically Disordered Pathological Prion Variant Y145Stop Converts into Self-Seeding Amyloids via Liquid-Liquid Phase Separation. Proc. Natl. Acad. Sci. USA. 2021;118:e2100968118. doi: 10.1073/pnas.2100968118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Tange H., Ishibashi D., Nakagaki T., Taguchi Y., Kamatari Y.O., Ozawa H., Nishida N. Liquid-Liquid Phase Separation of Full-Length Prion Protein Initiates Conformational Conversion in Vitro. J. Biol. Chem. 2021;296:100367. doi: 10.1016/j.jbc.2021.100367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Lau Y., Oamen H.P., Caudron F. Protein Phase Separation during Stress Adaptation and Cellular Memory. Cells. 2020;9:1302. doi: 10.3390/cells9051302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Matos C.O., Passos Y.M., do Amaral M.J., Macedo B., Tempone M.H., Bezerra O.C.L., Moraes M.O., Almeida M.S., Weber G., Missailidis S., et al. Liquid-Liquid Phase Separation and Fibrillation of the Prion Protein Modulated by a High-Affinity DNA Aptamer. FASEB J. 2020;34:365–385. doi: 10.1096/fj.201901897R. [DOI] [PubMed] [Google Scholar]
- 124.Franzmann T.M., Jahnel M., Pozniakovsky A., Mahamid J., Holehouse A.S., Nüske E., Richter D., Baumeister W., Grill S.W., Pappu R.V., et al. Phase Separation of a Yeast Prion Protein Promotes Cellular Fitness. Science. 2018;359 doi: 10.1126/science.aao5654. [DOI] [PubMed] [Google Scholar]
- 125.Loh D., Reiter R.J. Melatonin: Regulation of Biomolecular Condensates in Neurodegenerative Disorders. Antioxidants. 2021;10:1483. doi: 10.3390/antiox10091483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Tan D.X., Manchester L.C., Reiter R.J., Plummer B.F. Cyclic 3-Hydroxymelatonin: A Melatonin Metabolite Generated as a Result of Hydroxyl Radical Scavenging. Biol. Signals Recept. 1999;8:70–74. doi: 10.1159/000014571. [DOI] [PubMed] [Google Scholar]
- 127.Reiter R.J. Melatonin: Lowering the High Price of Free Radicals. News Physiol. Sci. 2000;15:246–250. doi: 10.1152/physiologyonline.2000.15.5.246. [DOI] [PubMed] [Google Scholar]
- 128.Tan D.X., Manchester L.C., Reiter R.J., Plummer B.F., Limson J., Weintraub S.T., Qi W. Melatonin Directly Scavenges Hydrogen Peroxide: A Potentially New Metabolic Pathway of Melatonin Biotransformation. Free Radic. Biol. Med. 2000;29:1177–1185. doi: 10.1016/S0891-5849(00)00435-4. [DOI] [PubMed] [Google Scholar]
- 129.de Almeida E.A., Martinez G.R., Klitzke C.F., de Medeiros M.H.G., Di Mascio P. Oxidation of Melatonin by Singlet Molecular Oxygen (O2(1deltag)) Produces N1-Acetyl-N2-Formyl-5-Methoxykynurenine. J. Pineal Res. 2003;35:131–137. doi: 10.1034/j.1600-079X.2003.00066.x. [DOI] [PubMed] [Google Scholar]
- 130.Matuszak Z., Bilska M.A., Reszka K.J., Chignell C.F., Bilski P. Interaction of Singlet Molecular Oxygen with Melatonin and Related Indoles. Photochem. Photobiol. 2003;78:449–455. doi: 10.1562/0031-8655(2003)078<0449:IOSMOW>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 131.Reiter R.J., Tan D.-X., Terron M.P., Flores L.J., Czarnocki Z. Melatonin and Its Metabolites: New Findings Regarding Their Production and Their Radical Scavenging Actions. Acta Biochim. Pol. 2007;54:1–9. doi: 10.18388/abp.2007_3264. [DOI] [PubMed] [Google Scholar]
- 132.Noda Y., Mori A., Liburdy R., Packer L. Melatonin and Its Precursors Scavenge Nitric Oxide. J. Pineal Res. 1999;27:159–163. doi: 10.1111/j.1600-079X.1999.tb00611.x. [DOI] [PubMed] [Google Scholar]
- 133.Galano A., Reiter R.J. Melatonin and Its Metabolites vs Oxidative Stress: From Individual Actions to Collective Protection. J. Pineal Res. 2018;65:e12514. doi: 10.1111/jpi.12514. [DOI] [PubMed] [Google Scholar]
- 134.Purushothaman A., Sheeja A.A., Janardanan D. Hydroxyl Radical Scavenging Activity of Melatonin and Its Related Indolamines. Free Radic. Res. 2020;54:373–383. doi: 10.1080/10715762.2020.1774575. [DOI] [PubMed] [Google Scholar]
- 135.Hardeland R. Melatonin, Its Metabolites and Their Interference with Reactive Nitrogen Compounds. Molecules. 2021;26:4105. doi: 10.3390/molecules26134105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Lerner A.B., Case J.D., Takahashi Y., Lee T.H., Mori W. Isolation of melatonin, the pineal gland factor that lightens melanocytes. J. Am. Chem. Soc. 1958;80:2587. doi: 10.1021/ja01543a060. [DOI] [Google Scholar]
- 137.He C., Wang J., Zhang Z., Yang M., Li Y., Tian X., Ma T., Tao J., Zhu K., Song Y., et al. Mitochondria Synthesize Melatonin to Ameliorate Its Function and Improve Mice Oocyte’s Quality under in Vitro Conditions. Int. J. Mol. Sci. 2016;17:939. doi: 10.3390/ijms17060939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Tan D.-X., Manchester L.C., Qin L., Reiter R.J. Melatonin: A Mitochondrial Targeting Molecule Involving Mitochondrial Protection and Dynamics. Int. J. Mol. Sci. 2016;17:2124. doi: 10.3390/ijms17122124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Suofu Y., Li W., Jean-Alphonse F.G., Jia J., Khattar N.K., Li J., Baranov S.V., Leronni D., Mihalik A.C., He Y., et al. Dual Role of Mitochondria in Producing Melatonin and Driving GPCR Signaling to Block Cytochrome c Release. Proc. Natl. Acad. Sci. USA. 2017;114:E7997–E8006. doi: 10.1073/pnas.1705768114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Reiter R.J., Rosales-Corral S., Tan D.X., Jou M.J., Galano A., Xu B. Melatonin as a Mitochondria-Targeted Antioxidant: One of Evolution’s Best Ideas. Cell. Mol. Life Sci. 2017;74:3863–3881. doi: 10.1007/s00018-017-2609-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Zhao D., Yu Y., Shen Y., Liu Q., Zhao Z., Sharma R., Reiter R.J. Melatonin Synthesis and Function: Evolutionary History in Animals and Plants. Front. Endocrinol. 2019;10:249. doi: 10.3389/fendo.2019.00249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Tan D.-X., Hardeland R., Back K., Manchester L.C., Alatorre-Jimenez M.A., Reiter R.J. On the Significance of an Alternate Pathway of Melatonin Synthesis via 5-Methoxytryptamine: Comparisons across Species. J. Pineal Res. 2016;61:27–40. doi: 10.1111/jpi.12336. [DOI] [PubMed] [Google Scholar]
- 143.Tan D.-X., Manchester L.C., Liu X., Rosales-Corral S.A., Acuna-Castroviejo D., Reiter R.J. Mitochondria and Chloroplasts as the Original Sites of Melatonin Synthesis: A Hypothesis Related to Melatonin’s Primary Function and Evolution in Eukaryotes. J. Pineal Res. 2013;54:127–138. doi: 10.1111/jpi.12026. [DOI] [PubMed] [Google Scholar]
- 144.Coon S.L., Klein D.C. Evolution of Arylalkylamine N-Acetyltransferase: Emergence and Divergence. Mol. Cell. Endocrinol. 2006;252:2–10. doi: 10.1016/j.mce.2006.03.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Arnao M.B., Hernández-Ruiz J. Growth Conditions Determine Different Melatonin Levels in Lupinus albus, L. J. Pineal Res. 2013;55:149–155. doi: 10.1111/jpi.12055. [DOI] [PubMed] [Google Scholar]
- 146.Martinez V., Nieves-Cordones M., Lopez-Delacalle M., Rodenas R., Mestre T.C., Garcia-Sanchez F., Rubio F., Nortes P.A., Mittler R., Rivero R.M. Tolerance to Stress Combination in Tomato Plants: New Insights in the Protective Role of Melatonin. Molecules. 2018;23:535. doi: 10.3390/molecules23030535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Byeon Y., Back K. Melatonin Synthesis in Rice Seedlings in Vivo Is Enhanced at High Temperatures and under Dark Conditions due to Increased Serotonin N-Acetyltransferase and N-Acetylserotonin Methyltransferase Activities. J. Pineal Res. 2014;56:189–195. doi: 10.1111/jpi.12111. [DOI] [PubMed] [Google Scholar]
- 148.Sun C., Liu L., Wang L., Li B., Jin C., Lin X. Melatonin: A Master Regulator of Plant Development and Stress Responses. J. Integr. Plant Biol. 2021;63:126–145. doi: 10.1111/jipb.12993. [DOI] [PubMed] [Google Scholar]
- 149.Oxenkrug G.F., McIntyre I.M. Stress-Induced Synthesis of Melatonin: Possible Involvement of the Endogenous Monoamine Oxidase Inhibitor (tribulin) Life Sci. 1985;37:1743–1746. doi: 10.1016/0024-3205(85)90303-0. [DOI] [PubMed] [Google Scholar]
- 150.Stokkan K.A., Nonaka K.O., Lerchl A., Vaughan M.K., Reiter R.J. Low Temperature Stimulates Pineal Activity in Syrian Hamsters. J. Pineal Res. 1991;10:43–48. doi: 10.1111/j.1600-079X.1991.tb00008.x. [DOI] [PubMed] [Google Scholar]
- 151.Stokkan K.A., Reiter R.J., Nonaka K.O., Lerchl A., Yu B.P., Vaughan M.K. Food Restriction Retards Aging of the Pineal Gland. Brain Res. 1991;545:66–72. doi: 10.1016/0006-8993(91)91270-B. [DOI] [PubMed] [Google Scholar]
- 152.Uzun A., Baltaci A.K., Kilic M., Mogulkoc R. The Effect of Acute Swimming Exercise on Plasma Melatonin Levels in Rats. Bratisl. Lek. Listy. 2012;113:64–66. doi: 10.4149/BLL_2012_015. [DOI] [PubMed] [Google Scholar]
- 153.Tan D.-X., Manchester L.C., Esteban-Zubero E., Zhou Z., Reiter R.J. Melatonin as a Potent and Inducible Endogenous Antioxidant: Synthesis and Metabolism. Molecules. 2015;20:18886–18906. doi: 10.3390/molecules201018886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Tan D.-X., Hardeland R. The Reserve/Maximum Capacity of Melatonin’s Synthetic Function for the Potential Dimorphism of Melatonin Production and Its Biological Significance in Mammals. Molecules. 2021;26:7302. doi: 10.3390/molecules26237302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Carrillo-Vico A., Calvo J.R., Abreu P., Lardone P.J., García-Mauriño S., Reiter R.J., Guerrero J.M. Evidence of Melatonin Synthesis by Human Lymphocytes and Its Physiological Significance: Possible Role as Intracrine, Autocrine, And/or Paracrine Substance. FASEB J. 2004;18:537–539. doi: 10.1096/fj.03-0694fje. [DOI] [PubMed] [Google Scholar]
- 156.Morcillo-Parra M.Á., Beltran G., Mas A., Torija M.-J. Effect of Several Nutrients and Environmental Conditions on Intracellular Melatonin Synthesis in Saccharomyces Cerevisiae. Microorganisms. 2020;8:853. doi: 10.3390/microorganisms8060853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Morcillo-Parra M.Á., Valera M.J., Beltran G., Mas A., Torija M.-J. Glycolytic Proteins Interact With Intracellular Melatonin in Saccharomyces Cerevisiae. Front. Microbiol. 2019;10:2424. doi: 10.3389/fmicb.2019.02424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Germann S.M., Baallal Jacobsen S.A., Schneider K., Harrison S.J., Jensen N.B., Chen X., Stahlhut S.G., Borodina I., Luo H., Zhu J., et al. Glucose-Based Microbial Production of the Hormone Melatonin in Yeast Saccharomyces Cerevisiae. Biotechnol. J. 2016;11:717–724. doi: 10.1002/biot.201500143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Sunyer-Figueres M., Vázquez J., Mas A., Torija M.-J., Beltran G. Transcriptomic Insights into the Effect of Melatonin in Saccharomyces Cerevisiae in the Presence and Absence of Oxidative Stress. Antioxidants. 2020;9:947. doi: 10.3390/antiox9100947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Bisquert R., Muñiz-Calvo S., Guillamón J.M. Protective Role of Intracellular Melatonin Against Oxidative Stress and UV Radiation in Saccharomyces Cerevisiae. Front. Microbiol. 2018;9:318. doi: 10.3389/fmicb.2018.00318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Bellinger-Kawahara C., Cleaver J.E., Diener T.O., Prusiner S.B. Purified Scrapie Prions Resist Inactivation by UV Irradiation. J. Virol. 1987;61:159–166. doi: 10.1128/jvi.61.1.159-166.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Alper T., Cramp W.A., Haig D.A., Clarke M.C. Does the Agent of Scrapie Replicate without Nucleic Acid? Nature. 1967;214:764–766. doi: 10.1038/214764a0. [DOI] [PubMed] [Google Scholar]
- 163.Bernardino-Sgherri J., Siberchicot C., Auvré F., Busso D., Brocas C., El Masri G., Lioutsko A., Ferri F., Radicella J.P., Romeo P.-H., et al. Tumor Resistance to Radiotherapy Is Triggered by an ATM/TAK1-Dependent-Increased Expression of the Cellular Prion Protein. Oncogene. 2021;40:3460–3469. doi: 10.1038/s41388-021-01746-0. [DOI] [PubMed] [Google Scholar]
- 164.Vijayalaxmi, Reiter R.J., Tan D.-X., Herman R.S., Thomas C.R., Jr. Melatonin as a Radioprotective Agent: A Review. Int. J. Radiat. Oncol. Biol. Phys. 2004;59:639–653. doi: 10.1016/j.ijrobp.2004.02.006. [DOI] [PubMed] [Google Scholar]
- 165.Farhood B., Goradel N.H., Mortezaee K., Khanlarkhani N., Salehi E., Nashtaei M.S., Mirtavoos-Mahyari H., Motevaseli E., Shabeeb D., Musa A.E., et al. Melatonin as an Adjuvant in Radiotherapy for Radioprotection and Radiosensitization. Clin. Transl. Oncol. 2019;21:268–279. doi: 10.1007/s12094-018-1934-0. [DOI] [PubMed] [Google Scholar]
- 166.Alonso-González C., González A., Menéndez-Menéndez J., Martínez-Campa C., Cos S. Melatonin as a Radio-Sensitizer in Cancer. Biomedicines. 2020;8:247. doi: 10.3390/biomedicines8080247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Gehrmann M., Specht H.M., Bayer C., Brandstetter M., Chizzali B., Duma M., Breuninger S., Hube K., Lehnerer S., van Phi V., et al. Hsp70—A Biomarker for Tumor Detection and Monitoring of Outcome of Radiation Therapy in Patients with Squamous Cell Carcinoma of the Head and Neck. Radiat. Oncol. 2014;9:131. doi: 10.1186/1748-717X-9-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Rothammer A., Sage E.K., Werner C., Combs S.E., Multhoff G. Increased Heat Shock Protein 70 (Hsp70) Serum Levels and Low NK Cell Counts after Radiotherapy—Potential Markers for Predicting Breast Cancer Recurrence? Radiat. Oncol. 2019;14:78. doi: 10.1186/s13014-019-1286-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Allen K.D., Wegrzyn R.D., Chernova T.A., Müller S., Newnam G.P., Winslett P.A., Wittich K.B., Wilkinson K.D., Chernoff Y.O. Hsp70 Chaperones as Modulators of Prion Life Cycle: Novel Effects of Ssa and Ssb on the Saccharomyces Cerevisiae Prion [PSI+] Genetics. 2005;169:1227–1242. doi: 10.1534/genetics.104.037168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Roh B.H., Kim D.H., Cho M.K., Park Y.L., Whang K.U. Expression of Heat Shock Protein 70 in Human Skin Cells as a Photoprotective Function after UV Exposure. Ann. Dermatol. 2008;20:184–189. doi: 10.5021/ad.2008.20.4.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Simon M.M., Reikerstorfer A., Schwarz A., Krone C., Luger T.A., Jäättelä M., Schwarz T. Heat Shock Protein 70 Overexpression Affects the Response to Ultraviolet Light in Murine Fibroblasts. Evidence for Increased Cell Viability and Suppression of Cytokine Release. J. Clin. Investig. 1995;95:926–933. doi: 10.1172/JCI117800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Matsuda M., Hoshino T., Yamashita Y., Tanaka K.-I., Maji D., Sato K., Adachi H., Sobue G., Ihn H., Funasaka Y., et al. Prevention of UVB Radiation-Induced Epidermal Damage by Expression of Heat Shock Protein 70. J. Biol. Chem. 2010;285:5848–5858. doi: 10.1074/jbc.M109.063453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Fischer T.W., Sweatman T.W., Semak I., Sayre R.M., Wortsman J., Slominski A. Constitutive and UV-Induced Metabolism of Melatonin in Keratinocytes and Cell-Free Systems. FASEB J. 2006;20:1564–1566. doi: 10.1096/fj.05-5227fje. [DOI] [PubMed] [Google Scholar]
- 174.Fischer T.W., Kleszczyński K., Hardkop L.H., Kruse N., Zillikens D. Melatonin Enhances Antioxidative Enzyme Gene Expression (CAT, GPx, SOD), Prevents Their UVR-Induced Depletion, and Protects against the Formation of DNA Damage (8-Hydroxy-2′-Deoxyguanosine) in Ex Vivo Human Skin. J. Pineal Res. 2013;54:303–312. doi: 10.1111/jpi.12018. [DOI] [PubMed] [Google Scholar]
- 175.Kleszczyński K., Zwicker S., Tukaj S., Kasperkiewicz M., Zillikens D., Wolf R., Fischer T.W. Melatonin Compensates Silencing of Heat Shock Protein 70 and Suppresses Ultraviolet Radiation-Induced Inflammation in Human Skin Ex Vivo and Cultured Keratinocytes. J. Pineal Res. 2015;58:117–126. doi: 10.1111/jpi.12197. [DOI] [PubMed] [Google Scholar]
- 176.Mellatyar H., Talaei S., Pilehvar-Soltanahmadi Y., Barzegar A., Akbarzadeh A., Shahabi A., Barekati-Mowahed M., Zarghami N. Targeted Cancer Therapy through 17-DMAG as an Hsp90 Inhibitor: Overview and Current State of the Art. Biomed. Pharmacother. 2018;102:608–617. doi: 10.1016/j.biopha.2018.03.102. [DOI] [PubMed] [Google Scholar]
- 177.Mays C.E., Armijo E., Morales R., Kramm C., Flores A., Tiwari A., Bian J., Telling G.C., Pandita T.K., Hunt C.R., et al. Prion Disease Is Accelerated in Mice Lacking Stress-Induced Heat Shock Protein 70 (HSP70) J. Biol. Chem. 2019;294:13619–13628. doi: 10.1074/jbc.RA118.006186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Herbst M., Wanker E.E. Small Molecule Inducers of Heat-Shock Response Reduce polyQ-Mediated Huntingtin Aggregation. A Possible Therapeutic Strategy. Neurodegener. Dis. 2007;4:254–260. doi: 10.1159/000101849. [DOI] [PubMed] [Google Scholar]
- 179.Wang Y.-L., Shen H.-H., Cheng P.-Y., Chu Y.-J., Hwang H.-R., Lam K.-K., Lee Y.-M. 17-DMAG, an HSP90 Inhibitor, Ameliorates Multiple Organ Dysfunction Syndrome via Induction of HSP70 in Endotoxemic Rats. PLoS ONE. 2016;11:e0155583. doi: 10.1371/journal.pone.0155583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Shyu W.-C., Harn H.-J., Saeki K., Kubosaki A., Matsumoto Y., Onodera T., Chen C.-J., Hsu Y.-D., Chiang Y.-H. Molecular Modulation of Expression of Prion Protein by Heat Shock. Mol. Neurobiol. 2002;26:1–12. doi: 10.1385/MN:26:1:001. [DOI] [PubMed] [Google Scholar]
- 181.Redecke L., Binder S., Elmallah M.I.Y., Broadbent R., Tilkorn C., Schulz B., May P., Goos A., Eich A., Rübhausen M., et al. UV-Light-Induced Conversion and Aggregation of Prion Proteins. Free Radic. Biol. Med. 2009;46:1353–1361. doi: 10.1016/j.freeradbiomed.2009.02.013. [DOI] [PubMed] [Google Scholar]
- 182.Webber C.J., Lei S., Wolozin B. Chapter Five-The Pathophysiology of Neurodegenerative Disease: Disturbing the Balance between Phase Separation and Irreversible Aggregation. In: Uversky V.N., editor. Progress in Molecular Biology and Translational Science. Volume 174. Academic Press; Cambridge, MA, USA: 2020. pp. 187–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Feng Z., Chen X., Wu X., Zhang M. Formation of Biological Condensates via Phase Separation: Characteristics, Analytical Methods, and Physiological Implications. J. Biol. Chem. 2019;294:14823–14835. doi: 10.1074/jbc.REV119.007895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Ning W., Guo Y., Lin S., Mei B., Wu Y., Jiang P., Tan X., Zhang W., Chen G., Peng D., et al. DrLLPS: A Data Resource of Liquid–liquid Phase Separation in Eukaryotes. Nucleic Acids Res. 2019;48:D288–D295. doi: 10.1093/nar/gkz1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Gomes E., Shorter J. The Molecular Language of Membraneless Organelles. J. Biol. Chem. 2019;294:7115–7127. doi: 10.1074/jbc.TM118.001192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Azaldegui C.A., Vecchiarelli A.G., Biteen J.S. The Emergence of Phase Separation as an Organizing Principle in Bacteria. Biophys. J. 2021;120:1123–1138. doi: 10.1016/j.bpj.2020.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Ladouceur A.-M., Parmar B.S., Biedzinski S., Wall J., Tope S.G., Cohn D., Kim A., Soubry N., Reyes-Lamothe R., Weber S.C. Clusters of Bacterial RNA Polymerase Are Biomolecular Condensates That Assemble through Liquid-Liquid Phase Separation. Proc. Natl. Acad. Sci. USA. 2020;117:18540–18549. doi: 10.1073/pnas.2005019117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Salvador-Castell M., Demé B., Oger P., Peters J. Lipid Phase Separation Induced by the Apolar Polyisoprenoid Squalane Demonstrates Its Role in Membrane Domain Formation in Archaeal Membranes. Langmuir. 2020;36:7375–7382. doi: 10.1021/acs.langmuir.0c00901. [DOI] [PubMed] [Google Scholar]
- 189.Price R.E., Lesniewski R., Nitzsche K.S., Meyerdierks A., Saltikov C., Pichler T., Amend J.P. Archaeal and Bacterial Diversity in an Arsenic-Rich Shallow-Sea Hydrothermal System Undergoing Phase Separation. Front. Microbiol. 2013;4:158. doi: 10.3389/fmicb.2013.00158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Riback J.A., Katanski C.D., Kear-Scott J.L., Pilipenko E.V., Rojek A.E., Sosnick T.R., Drummond D.A. Stress-Triggered Phase Separation Is an Adaptive, Evolutionarily Tuned Response. Cell. 2017;168:1028–1040.e19. doi: 10.1016/j.cell.2017.02.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Li P., Banjade S., Cheng H.-C., Kim S., Chen B., Guo L., Llaguno M., Hollingsworth J.V., King D.S., Banani S.F., et al. Phase Transitions in the Assembly of Multivalent Signalling Proteins. Nature. 2012;483:336–340. doi: 10.1038/nature10879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Su X., Ditlev J.A., Hui E., Xing W., Banjade S., Okrut J., King D.S., Taunton J., Rosen M.K., Vale R.D. Phase Separation of Signaling Molecules Promotes T Cell Receptor Signal Transduction. Science. 2016;352:595–599. doi: 10.1126/science.aad9964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Saito Y., Kimura W. Roles of Phase Separation for Cellular Redox Maintenance. Front. Genet. 2021;12:691946. doi: 10.3389/fgene.2021.691946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Laflamme G., Mekhail K. Biomolecular Condensates as Arbiters of Biochemical Reactions inside the Nucleus. Commun. Biol. 2020;3:773. doi: 10.1038/s42003-020-01517-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Franzmann T.M., Alberti S. Prion-like Low-Complexity Sequences: Key Regulators of Protein Solubility and Phase Behavior. J. Biol. Chem. 2019;294:7128–7136. doi: 10.1074/jbc.TM118.001190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Franzmann T.M., Alberti S. Protein Phase Separation as a Stress Survival Strategy. Cold Spring Harb. Perspect. Biol. 2019;11:a034058. doi: 10.1101/cshperspect.a034058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Lawson V.A., Priola S.A., Meade-White K., Lawson M., Chesebro B. Flexible N-Terminal Region of Prion Protein Influences Conformation of Protease-Resistant Prion Protein Isoforms Associated with Cross-Species Scrapie Infection in Vivo and in Vitro. J. Biol. Chem. 2004;279:13689–13695. doi: 10.1074/jbc.M303697200. [DOI] [PubMed] [Google Scholar]
- 198.Frankenfield K.N., Powers E.T., Kelly J.W. Influence of the N-Terminal Domain on the Aggregation Properties of the Prion Protein. Protein Sci. 2005;14:2154–2166. doi: 10.1110/ps.051434005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Chakravarty A.K., Jarosz D.F. More than Just a Phase: Prions at the Crossroads of Epigenetic Inheritance and Evolutionary Change. J. Mol. Biol. 2018;430:4607–4618. doi: 10.1016/j.jmb.2018.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Chakrabortee S., Byers J.S., Jones S., Garcia D.M., Bhullar B., Chang A., She R., Lee L., Fremin B., Lindquist S., et al. Intrinsically Disordered Proteins Drive Emergence and Inheritance of Biological Traits. Cell. 2016;167:369–381.e12. doi: 10.1016/j.cell.2016.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Ward J.J., Sodhi J.S., McGuffin L.J., Buxton B.F., Jones D.T. Prediction and Functional Analysis of Native Disorder in Proteins from the Three Kingdoms of Life. J. Mol. Biol. 2004;337:635–645. doi: 10.1016/j.jmb.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 202.Edskes H.K., Khamar H.J., Winchester C.-L., Greenler A.J., Zhou A., McGlinchey R.P., Gorkovskiy A., Wickner R.B. Sporadic Distribution of Prion-Forming Ability of Sup35p from Yeasts and Fungi. Genetics. 2014;198:605–616. doi: 10.1534/genetics.114.166538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Edskes H.K., Engel A., McCann L.M., Brachmann A., Tsai H.-F., Wickner R.B. Prion-Forming Ability of Ure2 of Yeasts Is Not Evolutionarily Conserved. Genetics. 2011;188:81–90. doi: 10.1534/genetics.111.127217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Basile W., Salvatore M., Bassot C., Elofsson A. Why Do Eukaryotic Proteins Contain More Intrinsically Disordered Regions? PLoS Comput. Biol. 2019;15:e1007186. doi: 10.1371/journal.pcbi.1007186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Wang C., Uversky V.N., Kurgan L. Disordered Nucleiome: Abundance of Intrinsic Disorder in the DNA- and RNA-Binding Proteins in 1121 Species from Eukaryota, Bacteria and Archaea. Proteomics. 2016;16:1486–1498. doi: 10.1002/pmic.201500177. [DOI] [PubMed] [Google Scholar]
- 206.Peng Z., Yan J., Fan X., Mizianty M.J., Xue B., Wang K., Hu G., Uversky V.N., Kurgan L. Exceptionally Abundant Exceptions: Comprehensive Characterization of Intrinsic Disorder in All Domains of Life. Cell. Mol. Life Sci. 2015;72:137–151. doi: 10.1007/s00018-014-1661-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Xue B., Dunker A.K., Uversky V.N. Orderly Order in Protein Intrinsic Disorder Distribution: Disorder in 3500 Proteomes from Viruses and the Three Domains of Life. J. Biomol. Struct. Dyn. 2012;30:137–149. doi: 10.1080/07391102.2012.675145. [DOI] [PubMed] [Google Scholar]
- 208.Ito Y., Mikawa T., Smith B.O. In-Cell NMR of Intrinsically Disordered Proteins in Prokaryotic Cells. In: Uversky V.N., Dunker A.K., editors. Intrinsically Disordered Protein Analysis: Volume 1, Methods and Experimental Tools. Humana Press; Totowa, NJ, USA: 2012. pp. 19–31. [DOI] [PubMed] [Google Scholar]
- 209.Xue B., Williams R.W., Oldfield C.J., Dunker A.K., Uversky V.N. Archaic Chaos: Intrinsically Disordered Proteins in Archaea. BMC Syst. Biol. 2010;4((Suppl S1)):S1. doi: 10.1186/1752-0509-4-S1-S1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Schuster B.S., Dignon G.L., Tang W.S., Kelley F.M., Ranganath A.K., Jahnke C.N., Simpkins A.G., Regy R.M., Hammer D.A., Good M.C., et al. Identifying Sequence Perturbations to an Intrinsically Disordered Protein That Determine Its Phase-Separation Behavior. Proc. Natl. Acad. Sci. USA. 2020;117:11421–11431. doi: 10.1073/pnas.2000223117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Kamimura Y.R., Kanai M. Chemical Insights into Liquid-Liquid Phase Separation in Molecular Biology. BCSJ. 2021;94:1045–1058. doi: 10.1246/bcsj.20200397. [DOI] [Google Scholar]
- 212.Hyman A.A., Weber C.A., Jülicher F. Liquid-Liquid Phase Separation in Biology. Annu. Rev. Cell Dev. Biol. 2014;30:39–58. doi: 10.1146/annurev-cellbio-100913-013325. [DOI] [PubMed] [Google Scholar]
- 213.Ahlers J., Adams E.M., Bader V., Pezzotti S., Winklhofer K.F., Tatzelt J., Havenith M. The Key Role of Solvent in Condensation: Mapping Water in Liquid-Liquid Phase-Separated FUS. Biophys. J. 2021;120:1266–1275. doi: 10.1016/j.bpj.2021.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Hondele M., Heinrich S., De Los Rios P., Weis K. Membraneless Organelles: Phasing out of Equilibrium. Emerg. Top. Life Sci. 2020;4:331–342. doi: 10.1042/ETLS20190190. [DOI] [PubMed] [Google Scholar]
- 215.Riback J.A., Zhu L., Ferrolino M.C., Tolbert M., Mitrea D.M., Sanders D.W., Wei M.-T., Kriwacki R.W., Brangwynne C.P. Composition-Dependent Thermodynamics of Intracellular Phase Separation. Nature. 2020;581:209–214. doi: 10.1038/s41586-020-2256-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Luo Y.-Y., Wu J.-J., Li Y.-M. Regulation of Liquid-Liquid Phase Separation with Focus on Post-Translational Modifications. Chem. Commun. 2021;57:13275–13287. doi: 10.1039/D1CC05266G. [DOI] [PubMed] [Google Scholar]
- 217.Lodish H., Berk A., Lawrence Zipursky S., Matsudaira P., Baltimore D., Darnell J. Biochemical Energetics. W. H. Freeman and Company; New York, NY, USA: 2000. [Google Scholar]
- 218.Brangwynne C.P., Mitchison T.J., Hyman A.A. Active Liquid-like Behavior of Nucleoli Determines Their Size and Shape in Xenopus Laevis Oocytes. Proc. Natl. Acad. Sci. USA. 2011;108:4334–4339. doi: 10.1073/pnas.1017150108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Wright R.H.G., Le Dily F., Beato M. ATP, Mg2+, Nuclear Phase Separation, and Genome Accessibility. Trends Biochem. Sci. 2019;44:565–574. doi: 10.1016/j.tibs.2019.03.001. [DOI] [PubMed] [Google Scholar]
- 220.Patel A., Malinovska L., Saha S., Wang J., Alberti S., Krishnan Y., Hyman A.A. ATP as a Biological Hydrotrope. Science. 2017;356:753–756. doi: 10.1126/science.aaf6846. [DOI] [PubMed] [Google Scholar]
- 221.Hayes M.H., Peuchen E.H., Dovichi N.J., Weeks D.L. Dual Roles for ATP in the Regulation of Phase Separated Protein Aggregates in Xenopus Oocyte Nucleoli. Elife. 2018;7:e35224. doi: 10.7554/eLife.35224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Kang J., Lim L., Song J. ATP Enhances at Low Concentrations but Dissolves at High Concentrations Liquid-Liquid Phase Separation (LLPS) of ALS/FTD-Causing FUS. Biochem. Biophys. Res. Commun. 2018;504:545–551. doi: 10.1016/j.bbrc.2018.09.014. [DOI] [PubMed] [Google Scholar]
- 223.Sridharan S., Kurzawa N., Werner T., Günthner I., Helm D., Huber W., Bantscheff M., Savitski M.M. Proteome-Wide Solubility and Thermal Stability Profiling Reveals Distinct Regulatory Roles for ATP. Nat. Commun. 2019;10:1155. doi: 10.1038/s41467-019-09107-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Pal S., Paul S. ATP Controls the Aggregation of Aβ16-22 Peptides. J. Phys. Chem. B. 2020;124:210–223. doi: 10.1021/acs.jpcb.9b10175. [DOI] [PubMed] [Google Scholar]
- 225.Song J. Adenosine Triphosphate Energy-Independently Controls Protein Homeostasis with Unique Structure and Diverse Mechanisms. Protein Sci. 2021;30:1277–1293. doi: 10.1002/pro.4079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Mehringer J., Do T.-M., Touraud D., Hohenschutz M., Khoshsima A., Horinek D., Kunz W. Hofmeister versus Neuberg: Is ATP Really a Biological Hydrotrope? Cell Rep. Phys. Sci. 2021;2:100343. doi: 10.1016/j.xcrp.2021.100343. [DOI] [Google Scholar]
- 227.Mandl I., Grauer A., Neuberg C. Solubilization of Insoluble Matter in Nature; I. The Part Played by Salts of Adenosinetriphosphate. Biochim. Biophys. Acta. 1952;8:654–663. doi: 10.1016/0006-3002(52)90103-0. [DOI] [PubMed] [Google Scholar]
- 228.Diaz-Espinoza R., Mukherjee A., Soto C. Kosmotropic Anions Promote Conversion of Recombinant Prion Protein into a PrPSc-like Misfolded Form. PLoS ONE. 2012;7:e31678. doi: 10.1371/journal.pone.0031678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Yeh V., Broering J.M., Romanyuk A., Chen B., Chernoff Y.O., Bommarius A.S. The Hofmeister Effect on Amyloid Formation Using Yeast Prion Protein. Protein Sci. 2010;19:47–56. doi: 10.1002/pro.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Zhou Q., Usluer S., Zhang F., Lenard A.J., Bourgeois B.M.R., Madl T. ATP Regulates RNA-Driven Cold Inducible RNA Binding Protein Phase Separation. Protein Sci. 2021;30:1438–1453. doi: 10.1002/pro.4123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Garcia-Jove Navarro M., Kashida S., Chouaib R., Souquere S., Pierron G., Weil D., Gueroui Z. RNA Is a Critical Element for the Sizing and the Composition of Phase-Separated RNA-Protein Condensates. Nat. Commun. 2019;10:3230. doi: 10.1038/s41467-019-11241-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Elbaum-Garfinkle S., Kim Y., Szczepaniak K., Chen C.C.-H., Eckmann C.R., Myong S., Brangwynne C.P. The Disordered P Granule Protein LAF-1 Drives Phase Separation into Droplets with Tunable Viscosity and Dynamics. Proc. Natl. Acad. Sci. USA. 2015;112:7189–7194. doi: 10.1073/pnas.1504822112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Conn G.L., Gittis A.G., Lattman E.E., Misra V.K., Draper D.E. A Compact RNA Tertiary Structure Contains a Buried Backbone-K+ Complex. J. Mol. Biol. 2002;318:963–973. doi: 10.1016/S0022-2836(02)00147-X. [DOI] [PubMed] [Google Scholar]
- 234.Henninger J.E., Oksuz O., Shrinivas K., Sagi I., LeRoy G., Zheng M.M., Andrews J.O., Zamudio A.V., Lazaris C., Hannett N.M., et al. RNA-Mediated Feedback Control of Transcriptional Condensates. Cell. 2021;184:207–225.e24. doi: 10.1016/j.cell.2020.11.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Gotor N.L., Armaos A., Calloni G., Torrent Burgas M., Vabulas R.M., De Groot N.S., Tartaglia G.G. RNA-Binding and Prion Domains: The Yin and Yang of Phase Separation. Nucleic Acids Res. 2020;48:9491–9504. doi: 10.1093/nar/gkaa681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Deleault N.R., Lucassen R.W., Supattapone S. RNA Molecules Stimulate Prion Protein Conversion. Nature. 2003;425:717–720. doi: 10.1038/nature01979. [DOI] [PubMed] [Google Scholar]
- 237.Saá P., Sferrazza G.F., Ottenberg G., Oelschlegel A.M., Dorsey K., Lasmézas C.I. Strain-Specific Role of RNAs in Prion Replication. J. Virol. 2012;86:10494–10504. doi: 10.1128/JVI.01286-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Gomes M.P.B., Millen T.A., Ferreira P.S., e Silva N.L.C., Vieira T.C.R.G., Almeida M.S., Silva J.L., Cordeiro Y. Prion Protein Complexed to N2a Cellular RNAs through Its N-Terminal Domain Forms Aggregates and Is Toxic to Murine Neuroblastoma Cells. J. Biol. Chem. 2008;283:19616–19625. doi: 10.1074/jbc.M802102200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Conaway R.C., Conaway J.W. ATP Activates Transcription Initiation from Promoters by RNA Polymerase II in a Reversible Step prior to RNA Synthesis. J. Biol. Chem. 1988;263:2962–2968. doi: 10.1016/S0021-9258(18)69162-8. [DOI] [PubMed] [Google Scholar]
- 240.Grummt I., Grummt F. Control of Nucleolar RNA Synthesis by the Intracellular Pool Sizes of ATP and GTP. Cell. 1976;7:447–453. doi: 10.1016/0092-8674(76)90175-6. [DOI] [PubMed] [Google Scholar]
- 241.Joyce G.F. RNA Evolution and the Origins of Life. Nature. 1989;338:217–224. doi: 10.1038/338217a0. [DOI] [PubMed] [Google Scholar]
- 242.Joyce G.F. The Antiquity of RNA-Based Evolution. Nature. 2002;418:214–221. doi: 10.1038/418214a. [DOI] [PubMed] [Google Scholar]
- 243.Robertson M.P., Joyce G.F. The Origins of the RNA World. Cold Spring Harb. Perspect. Biol. 2012;4:a003608. doi: 10.1101/cshperspect.a003608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.White H.B., 3rd Coenzymes as Fossils of an Earlier Metabolic State. J. Mol. Evol. 1976;7:101–104. doi: 10.1007/BF01732468. [DOI] [PubMed] [Google Scholar]
- 245.Goldman A.D., Kacar B. Cofactors Are Remnants of Life’s Origin and Early Evolution. J. Mol. Evol. 2021;89:127–133. doi: 10.1007/s00239-020-09988-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Jheeta S., Chatzitheodoridis E., Devine K., Block J. The Way Forward for the Origin of Life: Prions and Prion-Like Molecules First Hypothesis. Life. 2021;11:872. doi: 10.3390/life11090872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Zajkowski T., Lee M.D., Mondal S.S., Carbajal A., Dec R., Brennock P.D., Piast R.W., Snyder J.E., Bense N.B., Dzwolak W., et al. The Hunt for Ancient Prions: Archaeal Prion-Like Domains Form Amyloid-Based Epigenetic Elements. Mol. Biol. Evol. 2021;38:2088–2103. doi: 10.1093/molbev/msab010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Maury C.P.J. Amyloid and the Origin of Life: Self-Replicating Catalytic Amyloids as Prebiotic Informational and Protometabolic Entities. Cell. Mol. Life Sci. 2018;75:1499–1507. doi: 10.1007/s00018-018-2797-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Maury C.P.J. Self-Propagating Beta-Sheet Polypeptide Structures as Prebiotic Informational Molecular Entities: The Amyloid World. Orig. Life Evol. Biosph. 2009;39:141–150. doi: 10.1007/s11084-009-9165-6. [DOI] [PubMed] [Google Scholar]
- 250.Lupi O., Dadalti P., Cruz E., Sanberg P.R., Cryopraxis’ Task Force for Prion Research Are Prions Related to the Emergence of Early Life? Med. Hypotheses. 2006;67:1027–1033. doi: 10.1016/j.mehy.2006.04.056. [DOI] [PubMed] [Google Scholar]
- 251.Khan T., Kandola T.S., Wu J., Venkatesan S., Ketter E., Lange J.J., Rodríguez Gama A., Box A., Unruh J.R., Cook M., et al. Quantifying Nucleation In Vivo Reveals the Physical Basis of Prion-like Phase Behavior. Mol. Cell. 2018;71:155–168.e7. doi: 10.1016/j.molcel.2018.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Lu J., Qian J., Xu Z., Yin S., Zhou L., Zheng S., Zhang W. Emerging Roles of Liquid–Liquid Phase Separation in Cancer: From Protein Aggregation to Immune-Associated Signaling. Front. Cell Dev. Biol. 2021;9:1465. doi: 10.3389/fcell.2021.631486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Petronilho E.C., Pedrote M.M., Marques M.A., Passos Y.M., Mota M.F., Jakobus B., de Sousa G.D.S., Pereira da Costa F., Felix A.L., Ferretti G.D.S., et al. Phase Separation of p53 Precedes Aggregation and Is Affected by Oncogenic Mutations and Ligands. Chem. Sci. 2021;12:7334–7349. doi: 10.1039/D1SC01739J. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.de Oliveira G.A.P., Cordeiro Y., Silva J.L., Vieira T.C.R.G. Chapter Nine-Liquid-Liquid Phase Transitions and Amyloid Aggregation in Proteins Related to Cancer and Neurodegenerative Diseases. In: Donev R., editor. Advances in Protein Chemistry and Structural Biology. Volume 118. Academic Press; Cambridge, MA, USA: 2019. pp. 289–331. [DOI] [PubMed] [Google Scholar]
- 255.Ahn J.H., Davis E.S., Daugird T.A., Zhao S., Quiroga I.Y., Uryu H., Li J., Storey A.J., Tsai Y.-H., Keeley D.P., et al. Phase Separation Drives Aberrant Chromatin Looping and Cancer Development. Nature. 2021;595:591–595. doi: 10.1038/s41586-021-03662-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Zeigler T.M., Chung M.C., Narayan O.P., Guan J. Protein Phase Separation: Physical Models and Phase-Separation- Mediated Cancer Signaling. Adv. Phys. X. 2021;6:1936638. doi: 10.1080/23746149.2021.1936638. [DOI] [Google Scholar]
- 257.Taniue K., Akimitsu N. Aberrant Phase Separation and Cancer. FEBS J. 2021;289:17–39. doi: 10.1111/febs.15765. [DOI] [PubMed] [Google Scholar]
- 258.Boija A., Klein I.A., Young R.A. Biomolecular Condensates and Cancer. Cancer Cell. 2021;39:174–192. doi: 10.1016/j.ccell.2020.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Nozawa R.-S., Yamamoto T., Takahashi M., Tachiwana H., Maruyama R., Hirota T., Saitoh N. Nuclear Microenvironment in Cancer: Control through Liquid-Liquid Phase Separation. Cancer Sci. 2020;111:3155–3163. doi: 10.1111/cas.14551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Zhang H., Zhao R., Tones J., Liu M., Dilley R.L., Chenoweth D.M., Greenberg R.A., Lampson M.A. Nuclear Body Phase Separation Drives Telomere Clustering in ALT Cancer Cells. Mol. Biol. Cell. 2020;31:2048–2056. doi: 10.1091/mbc.E19-10-0589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Jiang S., Fagman J.B., Chen C., Alberti S., Liu B. Protein Phase Separation and Its Role in Tumorigenesis. Elife. 2020;9:e60264. doi: 10.7554/eLife.60264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Wang W., Chen Y., Xu A., Cai M., Cao J., Zhu H., Yang B., Shao X., Ying M., He Q. Protein Phase Separation: A Novel Therapy for Cancer? Br. J. Pharmacol. 2020;177:5008–5030. doi: 10.1111/bph.15242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Park S.-K., Park S., Pentek C., Liebman S.W. Tumor Suppressor Protein p53 Expressed in Yeast Can Remain Diffuse, Form a Prion, or Form Unstable Liquid-like Droplets. iScience. 2021;24:102000. doi: 10.1016/j.isci.2020.102000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Kamagata K., Kanbayashi S., Honda M., Itoh Y., Takahashi H., Kameda T., Nagatsugi F., Takahashi S. Liquid-like Droplet Formation by Tumor Suppressor p53 Induced by Multivalent Electrostatic Interactions between Two Disordered Domains. Sci. Rep. 2020;10:580. doi: 10.1038/s41598-020-57521-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Wells M., Tidow H., Rutherford T.J., Markwick P., Jensen M.R., Mylonas E., Svergun D.I., Blackledge M., Fersht A.R. Structure of Tumor Suppressor p53 and Its Intrinsically Disordered N-Terminal Transactivation Domain. Proc. Natl. Acad. Sci. USA. 2008;105:5762–5767. doi: 10.1073/pnas.0801353105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Kamps J., Lin Y.-H., Oliva R., Bader V., Winter R., Winklhofer K.F., Tatzelt J. The N-Terminal Domain of the Prion Protein Is Required and Sufficient for Liquid-Liquid Phase Separation: A Crucial Role of the Aβ-Binding Domain. J. Biol. Chem. 2021;297:100860. doi: 10.1016/j.jbc.2021.100860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Polido S.A., Kamps J., Tatzelt J. Biological Functions of the Intrinsically Disordered N-Terminal Domain of the Prion Protein: A Possible Role of Liquid–Liquid Phase Separation. Biomolecules. 2021;11:1201. doi: 10.3390/biom11081201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Posey A.E., Holehouse A.S., Pappu R.V. Phase Separation of Intrinsically Disordered Proteins. Methods Enzymol. 2018;611:1–30. doi: 10.1016/bs.mie.2018.09.035. [DOI] [PubMed] [Google Scholar]
- 269.Martin E.W., Harmon T.S., Hopkins J.B., Chakravarthy S., Incicco J.J., Schuck P., Soranno A., Mittag T. A Multi-Step Nucleation Process Determines the Kinetics of Prion-like Domain Phase Separation. Nat. Commun. 2021;12:4513. doi: 10.1038/s41467-021-24727-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Kovachev P.S., Gomes M.P.B., Cordeiro Y., Ferreira N.C., Valadão L.P.F., Ascari L.M., Rangel L.P., Silva J.L., Sanyal S. RNA Modulates Aggregation of the Recombinant Mammalian Prion Protein by Direct Interaction. Sci. Rep. 2019;9:12406. doi: 10.1038/s41598-019-48883-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Naslavsky N., Stein R., Yanai A., Friedlander G., Taraboulos A. Characterization of Detergent-Insoluble Complexes Containing the Cellular Prion Protein and Its Scrapie Isoform. J. Biol. Chem. 1997;272:6324–6331. doi: 10.1074/jbc.272.10.6324. [DOI] [PubMed] [Google Scholar]
- 272.Lewis V., Hooper N.M. The Role of Lipid Rafts in Prion Protein Biology. Front. Biosci. 2011;16:151–168. doi: 10.2741/3681. [DOI] [PubMed] [Google Scholar]
- 273.Beaudoin S., Vanderperre B., Grenier C., Tremblay I., Leduc F., Roucou X. A Large Ribonucleoprotein Particle Induced by Cytoplasmic PrP Shares Striking Similarities with the Chromatoid Body, an RNA Granule Predicted to Function in Posttranscriptional Gene Regulation. Biochim. Biophys. Acta. 2009;1793:335–345. doi: 10.1016/j.bbamcr.2008.10.009. [DOI] [PubMed] [Google Scholar]
- 274.Yokota S. Historical Survey on Chromatoid Body Research. Acta Histochem. Cytochem. 2008;41:65–82. doi: 10.1267/ahc.08010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Cohen E., Taraboulos A. Scrapie-like Prion Protein Accumulates in Aggresomes of Cyclosporin A-Treated Cells. EMBO J. 2003;22:404–417. doi: 10.1093/emboj/cdg045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Goggin K., Beaudoin S., Grenier C., Brown A.-A., Roucou X. Prion Protein Aggresomes Are poly(A)+ Ribonucleoprotein Complexes That Induce a PKR-Mediated Deficient Cell Stress Response. Biochim. Biophys. Acta. 2008;1783:479–491. doi: 10.1016/j.bbamcr.2007.10.008. [DOI] [PubMed] [Google Scholar]
- 277.Mironov A., Jr., Latawiec D., Wille H., Bouzamondo-Bernstein E., Legname G., Williamson R.A., Burton D., DeArmond S.J., Prusiner S.B., Peters P.J. Cytosolic Prion Protein in Neurons. J. Neurosci. 2003;23:7183–7193. doi: 10.1523/JNEUROSCI.23-18-07183.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Gonzalez-Montalban N., Lee Y.J., Makarava N., Savtchenko R., Baskakov I.V. Changes in Prion Replication Environment Cause Prion Strain Mutation. FASEB J. 2013;27:3702–3710. doi: 10.1096/fj.13-230466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Alred E.J., Lodangco I., Gallaher J., Hansmann U.H.E. Mutations Alter RNA-Mediated Conversion of Human Prions. ACS Omega. 2018;3:3936–3944. doi: 10.1021/acsomega.7b02007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Morillas M., Vanik D.L., Surewicz W.K. On the Mechanism of Alpha-Helix to Beta-Sheet Transition in the Recombinant Prion Protein. Biochemistry. 2001;40:6982–6987. doi: 10.1021/bi010232q. [DOI] [PubMed] [Google Scholar]
- 281.Wang X., Cui M., Zhao C., He L., Zhu D., Wang B., Du W. Regulation of Aggregation Behavior and Neurotoxicity of Prion Neuropeptides by Platinum Complexes. Inorg. Chem. 2014;53:5044–5054. doi: 10.1021/ic500092t. [DOI] [PubMed] [Google Scholar]
- 282.Huang J.-J., Li X.-N., Liu W.-L., Yuan H.-Y., Gao Y., Wang K., Tang B., Pang D.-W., Chen J., Liang Y. Neutralizing Mutations Significantly Inhibit Amyloid Formation by Human Prion Protein and Decrease Its Cytotoxicity. J. Mol. Biol. 2020;432:828–844. doi: 10.1016/j.jmb.2019.11.020. [DOI] [PubMed] [Google Scholar]
- 283.Wang J.H., Du J.P., Li S.J., Zhai L.P., Yang X.Y., Wang Z.H., Wu Z.T., Han Y. Octarepeat Peptides of Prion Are Essential for Multidrug Resistance in Gastric Cancer Cells. J. Dig. Dis. 2012;13:143–152. doi: 10.1111/j.1751-2980.2011.00563.x. [DOI] [PubMed] [Google Scholar]
- 284.Zahn R. The Octapeptide Repeats in Mammalian Prion Protein Constitute a pH-Dependent Folding and Aggregation Site. J. Mol. Biol. 2003;334:477–488. doi: 10.1016/j.jmb.2003.09.048. [DOI] [PubMed] [Google Scholar]
- 285.Haigh C.L., Drew S.C., Boland M.P., Masters C.L., Barnham K.J., Lawson V.A., Collins S.J. Dominant Roles of the Polybasic Proline Motif and Copper in the PrP23-89-Mediated Stress Protection Response. Pt 10J. Cell Sci. 2009;122:1518–1528. doi: 10.1242/jcs.043604. [DOI] [PubMed] [Google Scholar]
- 286.Chattopadhyay M., Walter E.D., Newell D.J., Jackson P.J., Aronoff-Spencer E., Peisach J., Gerfen G.J., Bennett B., Antholine W.E., Millhauser G.L. The Octarepeat Domain of the Prion Protein Binds Cu(II) with Three Distinct Coordination Modes at pH 7.4. J. Am. Chem. Soc. 2005;127:12647–12656. doi: 10.1021/ja053254z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Stöckel J., Safar J., Wallace A.C., Cohen F.E., Prusiner S.B. Prion Protein Selectively Binds copper(II) Ions. Biochemistry. 1998;37:7185–7193. doi: 10.1021/bi972827k. [DOI] [PubMed] [Google Scholar]
- 288.Ridge P.G., Zhang Y., Gladyshev V.N. Comparative Genomic Analyses of Copper Transporters and Cuproproteomes Reveal Evolutionary Dynamics of Copper Utilization and Its Link to Oxygen. PLoS ONE. 2008;3:e1378. doi: 10.1371/journal.pone.0001378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Vassallo N., Herms J. Cellular Prion Protein Function in Copper Homeostasis and Redox Signalling at the Synapse. J. Neurochem. 2003;86:538–544. doi: 10.1046/j.1471-4159.2003.01882.x. [DOI] [PubMed] [Google Scholar]
- 290.Majumder S., Chatterjee S., Pal S., Biswas J., Efferth T., Choudhuri S.K. The Role of Copper in Drug-Resistant Murine and Human Tumors. Biometals. 2009;22:377–384. doi: 10.1007/s10534-008-9174-3. [DOI] [PubMed] [Google Scholar]
- 291.Denoyer D., Masaldan S., La Fontaine S., Cater M.A. Targeting Copper in Cancer Therapy: “Copper That Cancer”. Metallomics. 2015;7:1459–1476. doi: 10.1039/C5MT00149H. [DOI] [PubMed] [Google Scholar]
- 292.Dong S.-L., Cadamuro S.A., Fiorino F., Bertsch U., Moroder L., Renner C. Copper Binding and Conformation of the N-Terminal Octarepeats of the Prion Protein in the Presence of DPC Micelles as Membrane Mimetic. Biopolymers. 2007;88:840–847. doi: 10.1002/bip.20860. [DOI] [PubMed] [Google Scholar]
- 293.Wong B.S., Vénien-Bryan C., Williamson R.A., Burton D.R., Gambetti P., Sy M.S., Brown D.R., Jones I.M. Copper Refolding of Prion Protein. Biochem. Biophys. Res. Commun. 2000;276:1217–1224. doi: 10.1006/bbrc.2000.3604. [DOI] [PubMed] [Google Scholar]
- 294.Evans E.G.B., Pushie M.J., Markham K.A., Lee H.-W., Millhauser G.L. Interaction between Prion Protein’s Copper-Bound Octarepeat Domain and a Charged C-Terminal Pocket Suggests a Mechanism for N-Terminal Regulation. Structure. 2016;24:1057–1067. doi: 10.1016/j.str.2016.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Alsiary R.A., Alghrably M., Saoudi A., Al-Ghamdi S., Jaremko L., Jaremko M., Emwas A.-H. Using NMR Spectroscopy to Investigate the Role Played by Copper in Prion Diseases. Neurol. Sci. 2020;41:2389–2406. doi: 10.1007/s10072-020-04321-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.M Passos Y., J do Amaral M., C Ferreira N., Macedo B., Chaves J.A.P., E de Oliveira V., P B Gomes M., L Silva J., Cordeiro Y. The Interplay between a GC-Rich Oligonucleotide and Copper Ions on Prion Protein Conformational and Phase Transitions. Int. J. Biol. Macromol. 2021;173:34–43. doi: 10.1016/j.ijbiomac.2021.01.097. [DOI] [PubMed] [Google Scholar]
- 297.Cox D.L., Pan J., Singh R.R.P. A Mechanism for Copper Inhibition of Infectious Prion Conversion. Biophys. J. 2006;91:L11–L13. doi: 10.1529/biophysj.106.083642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298.Giese A., Levin J., Bertsch U., Kretzschmar H. Effect of Metal Ions on de Novo Aggregation of Full-Length Prion Protein. Biochem. Biophys. Res. Commun. 2004;320:1240–1246. doi: 10.1016/j.bbrc.2004.06.075. [DOI] [PubMed] [Google Scholar]
- 299.Bocharova O.V., Breydo L., Salnikov V.V., Baskakov I.V. Copper(II) Inhibits in Vitro Conversion of Prion Protein into Amyloid Fibrils. Biochemistry. 2005;44:6776–6787. doi: 10.1021/bi050251q. [DOI] [PubMed] [Google Scholar]
- 300.Yen C.-F., Harischandra D.S., Kanthasamy A., Sivasankar S. Copper-Induced Structural Conversion Templates Prion Protein Oligomerization and Neurotoxicity. Sci. Adv. 2016;2:e1600014. doi: 10.1126/sciadv.1600014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Miura T., Hori-i A., Takeuchi H. Metal-Dependent Alpha-Helix Formation Promoted by the Glycine-Rich Octapeptide Region of Prion Protein. FEBS Lett. 1996;396:248–252. doi: 10.1016/0014-5793(96)01104-0. [DOI] [PubMed] [Google Scholar]
- 302.Cinar H., Winter R. The Effects of Cosolutes and Crowding on the Kinetics of Protein Condensate Formation Based on Liquid-Liquid Phase Separation: A Pressure-Jump Relaxation Study. Sci. Rep. 2020;10:17245. doi: 10.1038/s41598-020-74271-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 303.Ma S., Chen J., Feng J., Zhang R., Fan M., Han D., Li X., Li C., Ren J., Wang Y., et al. Melatonin Ameliorates the Progression of Atherosclerosis via Mitophagy Activation and NLRP3 Inflammasome Inhibition. Oxid. Med. Cell. Longev. 2018;2018:9286458. doi: 10.1155/2018/9286458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304.Cao Z., Fang Y., Lu Y., Tan D., Du C., Li Y., Ma Q., Yu J., Chen M., Zhou C., et al. Melatonin Alleviates Cadmium-Induced Liver Injury by Inhibiting the TXNIP-NLRP3 Inflammasome. J. Pineal Res. 2017;62:e12389. doi: 10.1111/jpi.12389. [DOI] [PubMed] [Google Scholar]
- 305.Zhang Y., Li X., Grailer J.J., Wang N., Wang M., Yao J., Zhong R., Gao G.F., Ward P.A., Tan D.-X., et al. Melatonin Alleviates Acute Lung Injury through Inhibiting the NLRP3 Inflammasome. J. Pineal Res. 2016;60:405–414. doi: 10.1111/jpi.12322. [DOI] [PubMed] [Google Scholar]
- 306.Mediavilla M.D., Cos S., Sánchez-Barceló E.J. Melatonin Increases p53 and p21WAF1 Expression in MCF-7 Human Breast Cancer Cells in Vitro. Life Sci. 1999;65:415–420. doi: 10.1016/S0024-3205(99)00262-3. [DOI] [PubMed] [Google Scholar]
- 307.Santoro R., Marani M., Blandino G., Muti P., Strano S. Melatonin Triggers p53Ser Phosphorylation and Prevents DNA Damage Accumulation. Oncogene. 2012;31:2931–2942. doi: 10.1038/onc.2011.469. [DOI] [PubMed] [Google Scholar]
- 308.Proietti S., Cucina A., Dobrowolny G., D’Anselmi F., Dinicola S., Masiello M.G., Pasqualato A., Palombo A., Morini V., Reiter R.J., et al. Melatonin down-Regulates MDM2 Gene Expression and Enhances p53 Acetylation in MCF-7 Cells. J. Pineal Res. 2014;57:120–129. doi: 10.1111/jpi.12150. [DOI] [PubMed] [Google Scholar]
- 309.Cai X., Chen J., Xu H., Liu S., Jiang Q.-X., Halfmann R., Chen Z.J. Prion-like Polymerization Underlies Signal Transduction in Antiviral Immune Defense and Inflammasome Activation. Cell. 2014;156:1207–1222. doi: 10.1016/j.cell.2014.01.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Samir P., Kanneganti T.-D. DDX3X Sits at the Crossroads of Liquid-Liquid and Prionoid Phase Transitions Arbitrating Life and Death Cell Fate Decisions in Stressed Cells. DNA Cell Biol. 2020;39:1091–1095. doi: 10.1089/dna.2020.5616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Silva J.L., De Moura Gallo C.V., Costa D.C.F., Rangel L.P. Prion-like Aggregation of Mutant p53 in Cancer. Trends Biochem. Sci. 2014;39:260–267. doi: 10.1016/j.tibs.2014.04.001. [DOI] [PubMed] [Google Scholar]
- 312.Shim D.-W., Lee K.-H. Posttranslational Regulation of the NLR Family Pyrin Domain-Containing 3 Inflammasome. Front. Immunol. 2018;9:1054. doi: 10.3389/fimmu.2018.01054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313.Song N., Li T. Regulation of NLRP3 Inflammasome by Phosphorylation. Front. Immunol. 2018;9:2305. doi: 10.3389/fimmu.2018.02305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314.Akther M., Haque M.E., Park J., Kang T.-B., Lee K.-H. NLRP3 Ubiquitination-A New Approach to Target NLRP3 Inflammasome Activation. Int. J. Mol. Sci. 2021;22:8780. doi: 10.3390/ijms22168780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315.Bode A.M., Dong Z. Post-Translational Modification of p53 in Tumorigenesis. Nat. Rev. Cancer. 2004;4:793–805. doi: 10.1038/nrc1455. [DOI] [PubMed] [Google Scholar]
- 316.Rodriguez M.S., Desterro J.M., Lain S., Lane D.P., Hay R.T. Multiple C-Terminal Lysine Residues Target p53 for Ubiquitin-Proteasome-Mediated Degradation. Mol. Cell. Biol. 2000;20:8458–8467. doi: 10.1128/MCB.20.22.8458-8467.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 317.Kahyo T., Nishida T., Yasuda H. Involvement of PIAS1 in the Sumoylation of Tumor Suppressor p53. Mol. Cell. 2001;8:713–718. doi: 10.1016/S1097-2765(01)00349-5. [DOI] [PubMed] [Google Scholar]
- 318.Kim Y., Myong S. RNA Remodeling Activity of DEAD Box Proteins Tuned by Protein Concentration, RNA Length, and ATP. Mol. Cell. 2016;63:865–876. doi: 10.1016/j.molcel.2016.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 319.Otvos L., Jr., Cudic M. Post-Translational Modifications in Prion Proteins. Curr. Protein Pept. Sci. 2002;3:643–652. doi: 10.2174/1389203023380440. [DOI] [PubMed] [Google Scholar]
- 320.Dear D.V., Young D.S., Kazlauskaite J., Meersman F., Oxley D., Webster J., Pinheiro T.J.T., Gill A.C., Bronstein I., Lowe C.R. Effects of Post-Translational Modifications on Prion Protein Aggregation and the Propagation of Scrapie-like Characteristics in Vitro. Biochim. Biophys. Acta. 2007;1774:792–802. doi: 10.1016/j.bbapap.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 321.Callender J.A., Sevillano A.M., Soldau K., Kurt T.D., Schumann T., Pizzo D.P., Altmeppen H., Glatzel M., Esko J.D., Sigurdson C.J. Prion Protein Post-Translational Modifications Modulate Heparan Sulfate Binding and Limit Aggregate Size in Prion Disease. Neurobiol. Dis. 2020;142:104955. doi: 10.1016/j.nbd.2020.104955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 322.Aguilar-Calvo P., Xiao X., Bett C., Eraña H., Soldau K., Castilla J., Nilsson K.P.R., Surewicz W.K., Sigurdson C.J. Post-Translational Modifications in PrP Expand the Conformational Diversity of Prions in vivo. Sci. Rep. 2017;7:43295. doi: 10.1038/srep43295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323.Valette N.M., Radford S.E., Harris S.A., Warriner S.L. Phosphorylation as a Tool to Modulate Aggregation Propensity and to Predict Fibril Architecture. ChemBioChem. 2012;13:271–281. doi: 10.1002/cbic.201100607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324.Portz B., Shorter J. Biochemical Timekeeping Via Reentrant Phase Transitions. J. Mol. Biol. 2021;433:166794. doi: 10.1016/j.jmb.2020.166794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 325.Walmsley A.R., Zeng F., Hooper N.M. The N-Terminal Region of the Prion Protein Ectodomain Contains a Lipid Raft Targeting Determinant. J. Biol. Chem. 2003;278:37241–37248. doi: 10.1074/jbc.M302036200. [DOI] [PubMed] [Google Scholar]
- 326.Taylor D.R., Hooper N.M. The Prion Protein and Lipid Rafts. Mol. Membr. Biol. 2006;23:89–99. doi: 10.1080/09687860500449994. [DOI] [PubMed] [Google Scholar]
- 327.Linden R., Martins V.R., Prado M.A.M., Cammarota M., Izquierdo I., Brentani R.R. Physiology of the Prion Protein. Physiol. Rev. 2008;88:673–728. doi: 10.1152/physrev.00007.2007. [DOI] [PubMed] [Google Scholar]
- 328.Mollinedo F., Gajate C. Lipid Rafts as Signaling Hubs in Cancer Cell Survival/death and Invasion: Implications in Tumor Progression and Therapy: Thematic Review Series: Biology of Lipid Rafts. J. Lipid Res. 2020;61:611–635. doi: 10.1194/jlr.TR119000439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 329.Zhong J., Yang C., Zheng W., Huang L., Hong Y., Wang L., Sha Y. Effects of Lipid Composition and Phase on the Membrane Interaction of the Prion Peptide 106-126 Amide. Biophys. J. 2009;96:4610–4621. doi: 10.1016/j.bpj.2009.01.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 330.Mei N., Robinson M., Davis J.H., Leonenko Z. Melatonin Alters Fluid Phase Co-Existence in POPC/DPPC/cholesterol Membranes. Biophys. J. 2020;119:2391–2402. doi: 10.1016/j.bpj.2020.10.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 331.Severcan F., Sahin I., Kazanci N. Melatonin Strongly Interacts with Zwitterionic Model Membranes—Evidence from Fourier Transform Infrared Spectroscopy and Differential Scanning Calorimetry. Biochim. Biophys. Acta. 2005;1668:215–222. doi: 10.1016/j.bbamem.2004.12.009. [DOI] [PubMed] [Google Scholar]
- 332.Bolmatov D., McClintic W.T., Taylor G., Stanley C.B., Do C., Collier C.P., Leonenko Z., Lavrentovich M.O., Katsaras J. Deciphering Melatonin-Stabilized Phase Separation in Phospholipid Bilayers. Langmuir. 2019;35:12236–12245. doi: 10.1021/acs.langmuir.9b01534. [DOI] [PubMed] [Google Scholar]
- 333.Acevedo-Morantes C.Y., Wille H. The Structure of Human Prions: From Biology to Structural Models-Considerations and Pitfalls. Viruses. 2014;6:3875–3892. doi: 10.3390/v6103875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 334.Zahn R., Liu A., Lührs T., Riek R., von Schroetter C., López García F., Billeter M., Calzolai L., Wider G., Wüthrich K. NMR Solution Structure of the Human Prion Protein. Proc. Natl. Acad. Sci. USA. 2000;97:145–150. doi: 10.1073/pnas.97.1.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 335.Riesner D. Biochemistry and Structure of PrP(C) and PrP(Sc) Br. Med. Bull. 2003;66:21–33. doi: 10.1093/bmb/66.1.21. [DOI] [PubMed] [Google Scholar]
- 336.Hill A.F., Antoniou M., Collinge J. Protease-Resistant Prion Protein Produced in Vitro Lacks Detectable Infectivity. Pt 1J. Gen. Virol. 1999;80:11–14. doi: 10.1099/0022-1317-80-1-11. [DOI] [PubMed] [Google Scholar]
- 337.Pan K.M., Baldwin M., Nguyen J., Gasset M., Serban A., Groth D., Mehlhorn I., Huang Z., Fletterick R.J., Cohen F.E. Conversion of Alpha-Helices into Beta-Sheets Features in the Formation of the Scrapie Prion Proteins. Proc. Natl. Acad. Sci. USA. 1993;90:10962–10966. doi: 10.1073/pnas.90.23.10962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 338.Simoneau S., Rezaei H., Salès N., Kaiser-Schulz G., Lefebvre-Roque M., Vidal C., Fournier J.-G., Comte J., Wopfner F., Grosclaude J., et al. In Vitro and in vivo Neurotoxicity of Prion Protein Oligomers. PLoS Pathog. 2007;3:e125. doi: 10.1371/journal.ppat.0030125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 339.Lau A.L., Yam A.Y., Michelitsch M.M.D., Wang X., Gao C., Goodson R.J., Shimizu R., Timoteo G., Hall J., Medina-Selby A., et al. Characterization of Prion Protein (PrP)-Derived Peptides That Discriminate Full-Length PrPSc from PrPC. Proc. Natl. Acad. Sci. USA. 2007;104:11551–11556. doi: 10.1073/pnas.0704260104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 340.Telling G.C., Parchi P., DeArmond S.J., Cortelli P., Montagna P., Gabizon R., Mastrianni J., Lugaresi E., Gambetti P., Prusiner S.B. Evidence for the Conformation of the Pathologic Isoform of the Prion Protein Enciphering and Propagating Prion Diversity. Science. 1996;274:2079–2082. doi: 10.1126/science.274.5295.2079. [DOI] [PubMed] [Google Scholar]
- 341.Khan M.Q., Sweeting B., Mulligan V.K., Arslan P.E., Cashman N.R., Pai E.F., Chakrabartty A. Prion Disease Susceptibility Is Affected by Beta-Structure Folding Propensity and Local Side-Chain Interactions in PrP. Proc. Natl. Acad. Sci. USA. 2010;107:19808–19813. doi: 10.1073/pnas.1005267107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 342.Kuwata K., Nishida N., Matsumoto T., Kamatari Y.O., Hosokawa-Muto J., Kodama K., Nakamura H.K., Kimura K., Kawasaki M., Takakura Y., et al. Hot Spots in Prion Protein for Pathogenic Conversion. Proc. Natl. Acad. Sci. USA. 2007;104:11921–11926. doi: 10.1073/pnas.0702671104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 343.Aguzzi A., Falsig J. Prion Propagation, Toxicity and Degradation. Nat. Neurosci. 2012;15:936–939. doi: 10.1038/nn.3120. [DOI] [PubMed] [Google Scholar]
- 344.Abskharon R.N.N., Giachin G., Wohlkonig A., Soror S.H., Pardon E., Legname G., Steyaert J. Probing the N-Terminal β-Sheet Conversion in the Crystal Structure of the Human Prion Protein Bound to a Nanobody. J. Am. Chem. Soc. 2014;136:937–944. doi: 10.1021/ja407527p. [DOI] [PubMed] [Google Scholar]
- 345.Kostylev M.A., Tuttle M.D., Lee S., Klein L.E., Takahashi H., Cox T.O., Gunther E.C., Zilm K.W., Strittmatter S.M. Liquid and Hydrogel Phases of PrPC Linked to Conformation Shifts and Triggered by Alzheimer’s Amyloid-β Oligomers. Mol. Cell. 2018;72:426–443.e12. doi: 10.1016/j.molcel.2018.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 346.Rösener N.S., Gremer L., Reinartz E., König A., Brener O., Heise H., Hoyer W., Neudecker P., Willbold D. A D-Enantiomeric Peptide Interferes with Heteroassociation of Amyloid-β Oligomers and Prion Protein. J. Biol. Chem. 2018;293:15748–15764. doi: 10.1074/jbc.RA118.003116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 347.Nieznanski K., Choi J.-K., Chen S., Surewicz K., Surewicz W.K. Soluble Prion Protein Inhibits Amyloid-β (Aβ) Fibrillization and Toxicity. J. Biol. Chem. 2012;287:33104–33108. doi: 10.1074/jbc.C112.400614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 348.Viola K.L., Klein W.L. Amyloid β Oligomers in Alzheimer’s Disease Pathogenesis, Treatment, and Diagnosis. Acta Neuropathol. 2015;129:183–206. doi: 10.1007/s00401-015-1386-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 349.Renner M., Lacor P.N., Velasco P.T., Xu J., Contractor A., Klein W.L., Triller A. Deleterious Effects of Amyloid Beta Oligomers Acting as an Extracellular Scaffold for mGluR5. Neuron. 2010;66:739–754. doi: 10.1016/j.neuron.2010.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 350.Haas L.T., Strittmatter S.M. Oligomers of Amyloid β Prevent Physiological Activation of the Cellular Prion Protein-Metabotropic Glutamate Receptor 5 Complex by Glutamate in Alzheimer Disease. J. Biol. Chem. 2016;291:17112–17121. doi: 10.1074/jbc.M116.720664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 351.Lacor P.N., Buniel M.C., Chang L., Fernandez S.J., Gong Y., Viola K.L., Lambert M.P., Velasco P.T., Bigio E.H., Finch C.E., et al. Synaptic Targeting by Alzheimer’s-Related Amyloid Beta Oligomers. J. Neurosci. 2004;24:10191–10200. doi: 10.1523/JNEUROSCI.3432-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 352.Um J.W., Kaufman A.C., Kostylev M., Heiss J.K., Stagi M., Takahashi H., Kerrisk M.E., Vortmeyer A., Wisniewski T., Koleske A.J., et al. Metabotropic Glutamate Receptor 5 Is a Coreceptor for Alzheimer Aβ Oligomer Bound to Cellular Prion Protein. Neuron. 2013;79:887–902. doi: 10.1016/j.neuron.2013.06.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 353.De Mario A., Castellani A., Peggion C., Massimino M.L., Lim D., Hill A.F., Sorgato M.C., Bertoli A. The Prion Protein Constitutively Controls Neuronal Store-Operated Ca(2+) Entry through Fyn Kinase. Front. Cell. Neurosci. 2015;9:416. doi: 10.3389/fncel.2015.00416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 354.Berridge M.J. Calcium Regulation of Neural Rhythms, Memory and Alzheimer’s Disease. J. Physiol. 2014;592:281–293. doi: 10.1113/jphysiol.2013.257527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 355.Matrone C., Petrillo F., Nasso R., Ferretti G. Fyn Tyrosine Kinase as Harmonizing Factor in Neuronal Functions and Dysfunctions. Int. J. Mol. Sci. 2020;21:4444. doi: 10.3390/ijms21124444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 356.Saito Y.D., Jensen A.R., Salgia R., Posadas E.M. Fyn: A Novel Molecular Target in Cancer. Cancer. 2010;116:1629–1637. doi: 10.1002/cncr.24879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 357.Elias D., Ditzel H.J. Fyn Is an Important Molecule in Cancer Pathogenesis and Drug Resistance. Pharmacol. Res. 2015;100:250–254. doi: 10.1016/j.phrs.2015.08.010. [DOI] [PubMed] [Google Scholar]
- 358.Yu J., Zhou Z., Wei Z., Wu J., OuYang J., Huang W., He Y., Zhang C. FYN Promotes Gastric Cancer Metastasis by Activating STAT3-Mediated Epithelial-Mesenchymal Transition. Transl. Oncol. 2020;13:100841. doi: 10.1016/j.tranon.2020.100841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 359.Hsieh M.-C., Ho Y.-C., Lai C.-Y., Chou D., Wang H.-H., Chen G.-D., Lin T.-B., Peng H.-Y. Melatonin Impedes Tet1-Dependent mGluR5 Promoter Demethylation to Relieve Pain. J. Pineal Res. 2017;63:e12436. doi: 10.1111/jpi.12436. [DOI] [PubMed] [Google Scholar]
- 360.Li Y., Zhang J., Wan J., Liu A., Sun J. Melatonin Regulates Aβ Production/clearance Balance and Aβ Neurotoxicity: A Potential Therapeutic Molecule for Alzheimer’s Disease. Biomed. Pharmacother. 2020;132:110887. doi: 10.1016/j.biopha.2020.110887. [DOI] [PubMed] [Google Scholar]
- 361.König A.S., Rösener N.S., Gremer L., Tusche M., Flender D., Reinartz E., Hoyer W., Neudecker P., Willbold D., Heise H. Structural Details of Amyloid β Oligomers in Complex with Human Prion Protein as Revealed by Solid-State MAS NMR Spectroscopy. J. Biol. Chem. 2021;296:100499. doi: 10.1016/j.jbc.2021.100499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 362.Nochebuena J., Quintanar L., Vela A., Cisneros G.A. Structural and Electronic Analysis of the Octarepeat Region of Prion Protein with Four Cu2+ by Polarizable MD and QM/MM Simulations. Phys. Chem. Chem. Phys. 2021;23:21568–21578. doi: 10.1039/D1CP03187B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 363.Surewicz W.K., Apostol M.I. Prion Protein and Its Conformational Conversion: A Structural Perspective. In: Tatzelt J., editor. Prion Proteins. Springer; Berlin/Heidelberg, Germany: 2011. pp. 135–167. [DOI] [PubMed] [Google Scholar]
- 364.Perera W.S., Hooper N.M. Ablation of the Metal Ion-Induced Endocytosis of the Prion Protein by Disease-Associated Mutation of the Octarepeat Region. Curr. Biol. 2001;11:519–523. doi: 10.1016/S0960-9822(01)00147-6. [DOI] [PubMed] [Google Scholar]
- 365.Jones C.E., Klewpatinond M., Abdelraheim S.R., Brown D.R., Viles J.H. Probing copper2+ Binding to the Prion Protein Using Diamagnetic nickel2+ and 1H NMR: The Unstructured N Terminus Facilitates the Coordination of Six copper2+ Ions at Physiological Concentrations. J. Mol. Biol. 2005;346:1393–1407. doi: 10.1016/j.jmb.2004.12.043. [DOI] [PubMed] [Google Scholar]
- 366.Salzano G., Brennich M., Mancini G., Tran T.H., Legname G., D’Angelo P., Giachin G. Deciphering Copper Coordination in the Mammalian Prion Protein Amyloidogenic Domain. Biophys. J. 2020;118:676–687. doi: 10.1016/j.bpj.2019.12.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 367.Jones C.E., Abdelraheim S.R., Brown D.R., Viles J.H. Preferential Cu2+ Coordination by His96 and His111 Induces Beta-Sheet Formation in the Unstructured Amyloidogenic Region of the Prion Protein. J. Biol. Chem. 2004;279:32018–32027. doi: 10.1074/jbc.M403467200. [DOI] [PubMed] [Google Scholar]
- 368.Jackson G.S., Murray I., Hosszu L.L., Gibbs N., Waltho J.P., Clarke A.R., Collinge J. Location and Properties of Metal-Binding Sites on the Human Prion Protein. Proc. Natl. Acad. Sci. USA. 2001;98:8531–8535. doi: 10.1073/pnas.151038498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 369.Dell’Acqua S., Massardi E., Monzani E., Di Natale G., Rizzarelli E., Casella L. Interaction between Hemin and Prion Peptides: Binding, Oxidative Reactivity and Aggregation. Int. J. Mol. Sci. 2020;21:7553. doi: 10.3390/ijms21207553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 370.Hooper N.M., Taylor D.R., Watt N.T. Mechanism of the Metal-Mediated Endocytosis of the Prion Protein. Pt 6Biochem. Soc. Trans. 2008;36:1272–1276. doi: 10.1042/BST0361272. [DOI] [PubMed] [Google Scholar]
- 371.Taylor D.R., Watt N.T., Perera W.S.S., Hooper N.M. Assigning Functions to Distinct Regions of the N-Terminus of the Prion Protein That Are Involved in Its Copper-Stimulated, Clathrin-Dependent Endocytosis. Pt 21J. Cell Sci. 2005;118:5141–5153. doi: 10.1242/jcs.02627. [DOI] [PubMed] [Google Scholar]
- 372.Sunyach C., Jen A., Deng J., Fitzgerald K.T., Frobert Y., Grassi J., McCaffrey M.W., Morris R. The Mechanism of Internalization of Glycosylphosphatidylinositol-Anchored Prion Protein. EMBO J. 2003;22:3591–3601. doi: 10.1093/emboj/cdg344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 373.Shyng S.L., Moulder K.L., Lesko A., Harris D.A. The N-Terminal Domain of a Glycolipid-Anchored Prion Protein Is Essential for Its Endocytosis via Clathrin-Coated Pits. J. Biol. Chem. 1995;270:14793–14800. doi: 10.1074/jbc.270.24.14793. [DOI] [PubMed] [Google Scholar]
- 374.Harmey J.H., Doyle D., Brown V., Rogers M.S. The Cellular Isoform of the Prion Protein, PrPc, Is Associated with Caveolae in Mouse Neuroblastoma (N2a) Cells. Biochem. Biophys. Res. Commun. 1995;210:753–759. doi: 10.1006/bbrc.1995.1723. [DOI] [PubMed] [Google Scholar]
- 375.Altmeppen H.C., Puig B., Dohler F., Thurm D.K., Falker C., Krasemann S., Glatzel M. Proteolytic Processing of the Prion Protein in Health and Disease. Am. J. Neurodegener. Dis. 2012;1:15–31. [PMC free article] [PubMed] [Google Scholar]
- 376.McMahon H.E., Mangé A., Nishida N., Créminon C., Casanova D., Lehmann S. Cleavage of the Amino Terminus of the Prion Protein by Reactive Oxygen Species. J. Biol. Chem. 2001;276:2286–2291. doi: 10.1074/jbc.M007243200. [DOI] [PubMed] [Google Scholar]
- 377.Posadas Y., López-Guerrero V.E., Segovia J., Perez-Cruz C., Quintanar L. Dissecting the Copper Bioinorganic Chemistry of the Functional and Pathological Roles of the Prion Protein: Relevance in Alzheimer’s Disease and Cancer. Curr. Opin. Chem. Biol. 2021;66:102098. doi: 10.1016/j.cbpa.2021.102098. [DOI] [PubMed] [Google Scholar]
- 378.Boland M.P., Hatty C.R., Separovic F., Hill A.F., Tew D.J., Barnham K.J., Haigh C.L., James M., Masters C.L., Collins S.J. Anionic Phospholipid Interactions of the Prion Protein N Terminus Are Minimally Perturbing and Not Driven Solely by the Octapeptide Repeat Domain. J. Biol. Chem. 2010;285:32282–32292. doi: 10.1074/jbc.M110.123398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 379.Liang J., Kong Q. α-Cleavage of Cellular Prion Protein. Prion. 2012;6:453–460. doi: 10.4161/pri.22511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 380.Mangé A., Béranger F., Peoc’h K., Onodera T., Frobert Y., Lehmann S. Alpha- and Beta- Cleavages of the Amino-Terminus of the Cellular Prion Protein. Biol. Cell. 2004;96:125–132. doi: 10.1016/j.biolcel.2003.11.007. [DOI] [PubMed] [Google Scholar]
- 381.Harris D.A., Huber M.T., van Dijken P., Shyng S.L., Chait B.T., Wang R. Processing of a Cellular Prion Protein: Identification of N- and C-Terminal Cleavage Sites. Biochemistry. 1993;32:1009–1016. doi: 10.1021/bi00055a003. [DOI] [PubMed] [Google Scholar]
- 382.Jarosz-Griffiths H.H., Corbett N.J., Rowland H.A., Fisher K., Jones A.C., Baron J., Howell G.J., Cowley S.A., Chintawar S., Cader M.Z., et al. Proteolytic Shedding of the Prion Protein via Activation of Metallopeptidase ADAM10 Reduces Cellular Binding and Toxicity of Amyloid-β Oligomers. J. Biol. Chem. 2019;294:7085–7097. doi: 10.1074/jbc.RA118.005364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 383.Hooper N.M. Roles of Proteolysis and Lipid Rafts in the Processing of the Amyloid Precursor Protein and Prion Protein. Pt 2Biochem. Soc. Trans. 2005;33:335–338. doi: 10.1042/BST0330335. [DOI] [PubMed] [Google Scholar]
- 384.Yadavalli R., Guttmann R.P., Seward T., Centers A.P., Williamson R.A., Telling G.C. Calpain-Dependent Endoproteolytic Cleavage of PrPSc Modulates Scrapie Prion Propagation. J. Biol. Chem. 2004;279:21948–21956. doi: 10.1074/jbc.M400793200. [DOI] [PubMed] [Google Scholar]
- 385.Hayashi H.K., Yokoyama T., Takata M., Iwamaru Y., Imamura M., Ushiki Y.K., Shinagawa M. The N-Terminal Cleavage Site of PrPSc from BSE Differs from that of PrPSc from Scrapie. Biochem. Biophys. Res. Commun. 2005;328:1024–1027. doi: 10.1016/j.bbrc.2005.01.065. [DOI] [PubMed] [Google Scholar]
- 386.Linsenmeier L., Altmeppen H.C., Wetzel S., Mohammadi B., Saftig P., Glatzel M. Diverse Functions of the Prion Protein-Does Proteolytic Processing Hold the Key? Biochim. Biophys. Acta Mol. Cell Res. 2017;1864:2128–2137. doi: 10.1016/j.bbamcr.2017.06.022. [DOI] [PubMed] [Google Scholar]
- 387.McDonald A.J., Dibble J.P., Evans E.G.B., Millhauser G.L. A New Paradigm for Enzymatic Control of α-Cleavage and β-Cleavage of the Prion Protein. J. Biol. Chem. 2014;289:803–813. doi: 10.1074/jbc.M113.502351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 388.Lewis V., Hill A.F., Haigh C.L., Klug G.M., Masters C.L., Lawson V.A., Collins S.J. Increased Proportions of C1 Truncated Prion Protein Protect against Cellular M1000 Prion Infection. J. Neuropathol. Exp. Neurol. 2009;68:1125–1135. doi: 10.1097/NEN.0b013e3181b96981. [DOI] [PubMed] [Google Scholar]
- 389.McDonald A.J., Millhauser G.L. PrP Overdrive: Does Inhibition of α-Cleavage Contribute to PrP(C) Toxicity and Prion Disease? Prion. 2014;8:183–191. doi: 10.4161/pri.28796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 390.Watt N.T., Taylor D.R., Gillott A., Thomas D.A., Perera W.S.S., Hooper N.M. Reactive Oxygen Species-Mediated Beta-Cleavage of the Prion Protein in the Cellular Response to Oxidative Stress. J. Biol. Chem. 2005;280:35914–35921. doi: 10.1074/jbc.M507327200. [DOI] [PubMed] [Google Scholar]
- 391.Collins S.J., Tumpach C., Groveman B.R., Drew S.C., Haigh C.L. Prion Protein Cleavage Fragments Regulate Adult Neural Stem Cell Quiescence through Redox Modulation of Mitochondrial Fission and SOD2 Expression. Cell. Mol. Life Sci. 2018;75:3231–3249. doi: 10.1007/s00018-018-2790-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 392.Chen W., Dong J., Haiech J., Kilhoffer M.-C., Zeniou M. Cancer Stem Cell Quiescence and Plasticity as Major Challenges in Cancer Therapy. Stem Cells Int. 2016;2016:1740936. doi: 10.1155/2016/1740936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 393.Aponte P.M., Caicedo A. Stemness in Cancer: Stem Cells, Cancer Stem Cells, and Their Microenvironment. Stem Cells Int. 2017;2017:5619472. doi: 10.1155/2017/5619472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 394.Bruschini S., Ciliberto G., Mancini R. The Emerging Role of Cancer Cell Plasticity and Cell-Cycle Quiescence in Immune Escape. Cell Death Dis. 2020;11:471. doi: 10.1038/s41419-020-2669-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 395.Schilling K.M., Tao L., Wu B., Kiblen J.T.M., Ubilla-Rodriguez N.C., Pushie M.J., Britt R.D., Roseman G.P., Harris D.A., Millhauser G.L. Both N-Terminal and C-Terminal Histidine Residues of the Prion Protein Are Essential for Copper Coordination and Neuroprotective Self-Regulation. J. Mol. Biol. 2020;432:4408–4425. doi: 10.1016/j.jmb.2020.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 396.Hopkins E., Sanvictores T., Sharma S. StatPearls. StatPearls Publishing; Treasure Island, FL, USA: 2021. Physiology, Acid Base Balance. [PubMed] [Google Scholar]
- 397.Kroschwald S., Maharana S., Mateju D., Malinovska L., Nüske E., Poser I., Richter D., Alberti S. Promiscuous Interactions and Protein Disaggregases Determine the Material State of Stress-Inducible RNP Granules. Elife. 2015;4:e06807. doi: 10.7554/eLife.06807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 398.Yoo H., Triandafillou C., Drummond D.A. Cellular Sensing by Phase Separation: Using the Process, Not Just the Products. J. Biol. Chem. 2019;294:7151–7159. doi: 10.1074/jbc.TM118.001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 399.Munder M.C., Midtvedt D., Franzmann T., Nüske E., Otto O., Herbig M., Ulbricht E., Müller P., Taubenberger A., Maharana S., et al. A pH-Driven Transition of the Cytoplasm from a Fluid- to a Solid-like State Promotes Entry into Dormancy. Elife. 2016;5:e09347. doi: 10.7554/eLife.09347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 400.Bera A., Biring S. A Quantitative Characterization of Interaction between Prion Protein with Nucleic Acids. Biochem. Biophys. Rep. 2018;14:114–124. doi: 10.1016/j.bbrep.2018.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 401.Bera A., Nandi P.K. Nucleic Acid Induced Unfolding of Recombinant Prion Protein Globular Fragment Is pH Dependent. Protein Sci. 2014;23:1780–1788. doi: 10.1002/pro.2573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 402.Sawyer W.H., Puckridge J. The Dissociation of Proteins by Chaotropic Salts. J. Biol. Chem. 1973;248:8429–8433. doi: 10.1016/S0021-9258(19)43151-7. [DOI] [PubMed] [Google Scholar]
- 403.Apetri A.C., Surewicz W.K. Atypical Effect of Salts on the Thermodynamic Stability of Human Prion Protein. J. Biol. Chem. 2003;278:22187–22192. doi: 10.1074/jbc.M302130200. [DOI] [PubMed] [Google Scholar]
- 404.Armstrong K.M., Baldwin R.L. Charged Histidine Affects Alpha-Helix Stability at All Positions in the Helix by Interacting with the Backbone Charges. Proc. Natl. Acad. Sci. USA. 1993;90:11337–11340. doi: 10.1073/pnas.90.23.11337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 405.Gabryelczyk B., Cai H., Shi X., Sun Y., Swinkels P.J.M., Salentinig S., Pervushin K., Miserez A. Hydrogen Bond Guidance and Aromatic Stacking Drive Liquid-Liquid Phase Separation of Intrinsically Disordered Histidine-Rich Peptides. Nat. Commun. 2019;10:5465. doi: 10.1038/s41467-019-13469-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 406.Van Lindt J., Bratek-Skicki A., Nguyen P.N., Pakravan D., Durán-Armenta L.F., Tantos A., Pancsa R., Van Den Bosch L., Maes D., Tompa P. A Generic Approach to Study the Kinetics of Liquid-Liquid Phase Separation under near-Native Conditions. Commun. Biol. 2021;4:77. doi: 10.1038/s42003-020-01596-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 407.Cleaves H.J.J. Isoelectric Point. In: Gargaud M., Amils R., Quintanilla J.C., Cleaves H.J.J., Irvine W.M., Pinti D.L., Viso M., editors. Encyclopedia of Astrobiology. Springer; Berlin/Heidelberg, Germany: 2011. p. 858. [DOI] [Google Scholar]
- 408.Adame-Arana O., Weber C.A., Zaburdaev V., Prost J., Jülicher F. Liquid Phase Separation Controlled by pH. Biophys. J. 2020;119:1590–1605. doi: 10.1016/j.bpj.2020.07.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 409.Shaw K.L., Grimsley G.R., Yakovlev G.I., Makarov A.A., Pace C.N. The Effect of Net Charge on the Solubility, Activity, and Stability of Ribonuclease Sa. Protein Sci. 2001;10:1206–1215. doi: 10.1110/ps.440101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 410.Fiorini M., Bongianni M., Zanusso G. Molecular Signature in Human and Animal Prion Disorders. In: Tutar Y., editor. Prion. IntechOpen; Rijeka, Yugoslavia: 2017. [DOI] [Google Scholar]
- 411.Miura T., Hori-i A., Mototani H., Takeuchi H. Raman Spectroscopic Study on the copper(II) Binding Mode of Prion Octapeptide and Its pH Dependence. Biochemistry. 1999;38:11560–11569. doi: 10.1021/bi9909389. [DOI] [PubMed] [Google Scholar]
- 412.Brown D.R., Qin K., Herms J.W., Madlung A., Manson J., Strome R., Fraser P.E., Kruck T., von Bohlen A., Schulz-Schaeffer W., et al. The Cellular Prion Protein Binds Copper in Vivo. Nature. 1997;390:684–687. doi: 10.1038/37783. [DOI] [PubMed] [Google Scholar]
- 413.Gaetke L.M., Chow C.K. Copper Toxicity, Oxidative Stress, and Antioxidant Nutrients. Toxicology. 2003;189:147–163. doi: 10.1016/S0300-483X(03)00159-8. [DOI] [PubMed] [Google Scholar]
- 414.Gaetke L.M., Chow-Johnson H.S., Chow C.K. Copper: Toxicological Relevance and Mechanisms. Arch. Toxicol. 2014;88:1929–1938. doi: 10.1007/s00204-014-1355-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 415.Linder M.C. Ceruloplasmin and Other Copper Binding Components of Blood Plasma and Their Functions: An Update. Metallomics. 2016;8:887–905. doi: 10.1039/C6MT00103C. [DOI] [PubMed] [Google Scholar]
- 416.Yim J., Kwon S.B., Han J.S., Kim J.-H., Lee E.H., Lee S.-G. Total and Exchangeable Copper Assay Using Inductively Coupled Plasma Mass Spectrometry and Establishment of a Pediatric Reference Interval. Arch. Pathol. Lab. Med. 2021;145:877–882. doi: 10.5858/arpa.2020-0029-OA. [DOI] [PubMed] [Google Scholar]
- 417.El Balkhi S., Poupon J., Trocello J.-M., Leyendecker A., Massicot F., Galliot-Guilley M., Woimant F. Determination of Ultrafiltrable and Exchangeable Copper in Plasma: Stability and Reference Values in Healthy Subjects. Anal. Bioanal. Chem. 2009;394:1477–1484. doi: 10.1007/s00216-009-2809-6. [DOI] [PubMed] [Google Scholar]
- 418.Kirsipuu T., Zadorožnaja A., Smirnova J., Friedemann M., Plitz T., Tõugu V., Palumaa P. Copper(II)-Binding Equilibria in Human Blood. Sci. Rep. 2020;10:5686. doi: 10.1038/s41598-020-62560-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 419.Kramer M.L., Kratzin H.D., Schmidt B., Römer A., Windl O., Liemann S., Hornemann S., Kretzschmar H. Prion Protein Binds Copper within the Physiological Concentration Range. J. Biol. Chem. 2001;276:16711–16719. doi: 10.1074/jbc.M006554200. [DOI] [PubMed] [Google Scholar]
- 420.Shanbhag V.C., Gudekar N., Jasmer K., Papageorgiou C., Singh K., Petris M.J. Copper Metabolism as a Unique Vulnerability in Cancer. Biochim. Biophys. Acta Mol. Cell Res. 2021;1868:118893. doi: 10.1016/j.bbamcr.2020.118893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 421.Blockhuys S., Zhang X., Wittung-Stafshede P. Single-Cell Tracking Demonstrates Copper Chaperone Atox1 to Be Required for Breast Cancer Cell Migration. Proc. Natl. Acad. Sci. USA. 2020;117:2014–2019. doi: 10.1073/pnas.1910722117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 422.Brown D.R., Clive C., Haswell S.J. Antioxidant Activity Related to Copper Binding of Native Prion Protein. J. Neurochem. 2001;76:69–76. doi: 10.1046/j.1471-4159.2001.00009.x. [DOI] [PubMed] [Google Scholar]
- 423.Varela-Nallar L., Toledo E.M., Larrondo L.F., Cabral A.L.B., Martins V.R., Inestrosa N.C. Induction of Cellular Prion Protein Gene Expression by Copper in Neurons. Am. J. Physiol. Cell Physiol. 2006;290:C271–C281. doi: 10.1152/ajpcell.00160.2005. [DOI] [PubMed] [Google Scholar]
- 424.Qin K., Zhao L., Ash R.D., McDonough W.F., Zhao R.Y. ATM-Mediated Transcriptional Elevation of Prion in Response to Copper-Induced Oxidative Stress. J. Biol. Chem. 2009;284:4582–4593. doi: 10.1074/jbc.M808410200. [DOI] [PubMed] [Google Scholar]
- 425.Carroll J.A., Groveman B.R., Williams K., Moore R., Race B., Haigh C.L. Prion Protein N1 Cleavage Peptides Stimulate Microglial Interaction with Surrounding Cells. Sci. Rep. 2020;10:6654. doi: 10.1038/s41598-020-63472-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 426.Nguyen T.-S., Lalucque H., Malagnac F., Silar P. Chapter 5-Prions and Prion-Like Phenomena in Epigenetic Inheritance. In: Tollefsbol T.O., editor. Handbook of Epigenetics. 2nd ed. Academic Press; Cambridge, MA, USA: 2017. pp. 61–72. [DOI] [Google Scholar]
- 427.Limson J., Nyokong T., Daya S. The Interaction of Melatonin and Its Precursors with Aluminium, Cadmium, Copper, Iron, Lead, and Zinc: An Adsorptive Voltammetric Study. J. Pineal Res. 1998;24:15–21. doi: 10.1111/j.1600-079X.1998.tb00361.x. [DOI] [PubMed] [Google Scholar]
- 428.Romero A., Ramos E., de Los Ríos C., Egea J., Del Pino J., Reiter R.J. A Review of Metal-Catalyzed Molecular Damage: Protection by Melatonin. J. Pineal Res. 2014;56:343–370. doi: 10.1111/jpi.12132. [DOI] [PubMed] [Google Scholar]
- 429.Cao Y.-Y., Qi C.-D., Li S., Wang Z., Wang X., Wang J., Ren S., Li X., Zhang N., Guo Y.-D. Melatonin Alleviates Copper Toxicity via Improving Copper Sequestration and ROS Scavenging in Cucumber. Plant. Cell Physiol. 2019;60:562–574. doi: 10.1093/pcp/pcy226. [DOI] [PubMed] [Google Scholar]
- 430.Wang J., Wang X., He Y., Jia L., Yang C.S., Reiter R.J., Zhang J. Antioxidant and Pro-Oxidant Activities of Melatonin in the Presence of Copper and Polyphenols In Vitro and In Vivo. Cells. 2019;8:903. doi: 10.3390/cells8080903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 431.Galano A., Medina M.E., Tan D.X., Reiter R.J. Melatonin and Its Metabolites as Copper Chelating Agents and Their Role in Inhibiting Oxidative Stress: A Physicochemical Analysis. J. Pineal Res. 2015;58:107–116. doi: 10.1111/jpi.12196. [DOI] [PubMed] [Google Scholar]
- 432.Finnegan S., Percival S.L. EDTA: An Antimicrobial and Antibiofilm Agent for Use in Wound Care. Adv. Wound Care. 2015;4:415–421. doi: 10.1089/wound.2014.0577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 433.Díaz-Cervantes E., García-Revilla M.A., Soto-Arredondo K., Villaseñor-Granados T., Martínez-Alfaro M., Robles J. Computational Study of Metal Complexes Formed with EDTA, Melatonin, and Its Main Metabolites: Implications in Lead Intoxication and Clues to a Plausible Alternative Treatment. J. Mol. Model. 2019;25:18. doi: 10.1007/s00894-018-3898-y. [DOI] [PubMed] [Google Scholar]
- 434.Reina M., Martínez A. A New Free Radical Scavenging Cascade Involving Melatonin and Three of Its Metabolites (3OHM, AFMK and AMK) Comput. Theor. Chem. 2018;1123:111–118. doi: 10.1016/j.comptc.2017.11.017. [DOI] [Google Scholar]
- 435.Abadi S.H.M.H., Shirazi A., Alizadeh A.M., Changizi V., Najafi M., Khalighfard S., Nosrati H. The Effect of Melatonin on Superoxide Dismutase and Glutathione Peroxidase Activity, and Malondialdehyde Levels in the Targeted and the Non-Targeted Lung and Heart Tissues after Irradiation in Xenograft Mice Colon Cancer. Curr. Mol. Pharmacol. 2018;11:326–335. doi: 10.2174/1874467211666180830150154. [DOI] [PubMed] [Google Scholar]
- 436.de Fortunato Miranda N. Ph.D. Thesis. The University of Melbourne; Melbourne, Australia: 2021. The Dual Role of Cellular Prion Protein in Colorectal Cancer. [Google Scholar]
- 437.Vander Heiden M.G., Cantley L.C., Thompson C.B. Understanding the Warburg Effect: The Metabolic Requirements of Cell Proliferation. Science. 2009;324:1029–1033. doi: 10.1126/science.1160809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 438.Perona R., Serrano R. Increased pH and Tumorigenicity of Fibroblasts Expressing a Yeast Proton Pump. Nature. 1988;334:438–440. doi: 10.1038/334438a0. [DOI] [PubMed] [Google Scholar]
- 439.Kato Y., Ozawa S., Miyamoto C., Maehata Y., Suzuki A., Maeda T., Baba Y. Acidic Extracellular Microenvironment and Cancer. Cancer Cell Int. 2013;13:89. doi: 10.1186/1475-2867-13-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 440.Sharma M., Astekar M., Soi S., Manjunatha B.S., Shetty D.C., Radhakrishnan R. pH Gradient Reversal: An Emerging Hallmark of Cancers. Recent Pat. Anticancer Drug Discov. 2015;10:244–258. doi: 10.2174/1574892810666150708110608. [DOI] [PubMed] [Google Scholar]
- 441.Pérez-Herrero E., Fernández-Medarde A. The Reversed Intra- and Extracellular pH in Tumors as a Unified Strategy to Chemotherapeutic Delivery Using Targeted Nanocarriers. Acta Pharm Sin. B. 2021;11:2243–2264. doi: 10.1016/j.apsb.2021.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 442.Chen M., Chen C., Shen Z., Zhang X., Chen Y., Lin F., Ma X., Zhuang C., Mao Y., Gan H., et al. Extracellular pH Is a Biomarker Enabling Detection of Breast Cancer and Liver Cancer Using CEST MRI. Oncotarget. 2017;8:45759–45767. doi: 10.18632/oncotarget.17404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 443.Shirmanova M.V., Druzhkova I.N., Lukina M.M., Matlashov M.E., Belousov V.V., Snopova L.B., Prodanetz N.N., Dudenkova V.V., Lukyanov S.A., Zagaynova E.V. Intracellular pH Imaging in Cancer Cells in Vitro and Tumors in Vivo Using the New Genetically Encoded Sensor SypHer2. Biochim. Biophys. Acta. 2015;1850:1905–1911. doi: 10.1016/j.bbagen.2015.05.001. [DOI] [PubMed] [Google Scholar]
- 444.Damaghi M., Wojtkowiak J.W., Gillies R.J. pH Sensing and Regulation in Cancer. Front. Physiol. 2013;4:370. doi: 10.3389/fphys.2013.00370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 445.Webb B.A., Chimenti M., Jacobson M.P., Barber D.L. Dysregulated pH: A Perfect Storm for Cancer Progression. Nat. Rev. Cancer. 2011;11:671–677. doi: 10.1038/nrc3110. [DOI] [PubMed] [Google Scholar]
- 446.Gatenby R.A., Gawlinski E.T., Gmitro A.F., Kaylor B., Gillies R.J. Acid-Mediated Tumor Invasion: A Multidisciplinary Study. Cancer Res. 2006;66:5216–5223. doi: 10.1158/0008-5472.CAN-05-4193. [DOI] [PubMed] [Google Scholar]
- 447.Gillies R.J., Raghunand N., Karczmar G.S., Bhujwalla Z.M. MRI of the Tumor Microenvironment. J. Magn. Reson. Imaging. 2002;16:430–450. doi: 10.1002/jmri.10181. [DOI] [PubMed] [Google Scholar]
- 448.Martin G.R., Jain R.K. Noninvasive Measurement of Interstitial pH Profiles in Normal and Neoplastic Tissue Using Fluorescence Ratio Imaging Microscopy. Cancer Res. 1994;54:5670–5674. [PubMed] [Google Scholar]
- 449.Gillies R.J., Liu Z., Bhujwalla Z. 31P-MRS Measurements of Extracellular pH of Tumors Using 3-Aminopropylphosphonate. Pt 1Am. J. Physiol. 1994;267:C195–C203. doi: 10.1152/ajpcell.1994.267.1.C195. [DOI] [PubMed] [Google Scholar]
- 450.Busa W.B., Nuccitelli R. Metabolic Regulation via Intracellular pH. Pt 2Am. J. Physiol. 1984;246:R409–R438. doi: 10.1152/ajpregu.1984.246.4.R409. [DOI] [PubMed] [Google Scholar]
- 451.A Kurkdjian A., Guern J. Intracellular pH: Measurement and Importance in Cell Activity. Annu. Rev. 1989;40:271–303. doi: 10.1146/annurev.pp.40.060189.001415. [DOI] [Google Scholar]
- 452.Casey J.R., Grinstein S., Orlowski J. Sensors and Regulators of Intracellular pH. Nat. Rev. Mol. Cell Biol. 2010;11:50–61. doi: 10.1038/nrm2820. [DOI] [PubMed] [Google Scholar]
- 453.Persi E., Duran-Frigola M., Damaghi M., Roush W.R., Aloy P., Cleveland J.L., Gillies R.J., Ruppin E. Systems Analysis of Intracellular pH Vulnerabilities for Cancer Therapy. Nat. Commun. 2018;9:2997. doi: 10.1038/s41467-018-05261-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 454.Chiche J., Brahimi-Horn M.C., Pouysségur J. Tumour Hypoxia Induces a Metabolic Shift Causing Acidosis: A Common Feature in Cancer. J. Cell. Mol. Med. 2010;14:771–794. doi: 10.1111/j.1582-4934.2009.00994.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 455.Zheng T., Jäättelä M., Liu B. pH Gradient Reversal Fuels Cancer Progression. Int. J. Biochem. Cell Biol. 2020;125:105796. doi: 10.1016/j.biocel.2020.105796. [DOI] [PubMed] [Google Scholar]
- 456.Reshkin S.J., Greco M.R., Cardone R.A. Role of pHi, and Proton Transporters in Oncogene-Driven Neoplastic Transformation. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2014;369:20130100. doi: 10.1098/rstb.2013.0100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 457.Becker H.M., Deitmer J.W. Proton Transport in Cancer Cells: The Role of Carbonic Anhydrases. Int. J. Mol. Sci. 2021;22:3171. doi: 10.3390/ijms22063171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 458.Piao S., Amaravadi R.K. Targeting the Lysosome in Cancer. Ann. N. Y. Acad. Sci. 2016;1371:45–54. doi: 10.1111/nyas.12953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 459.Galenkamp K.M.O., Commisso C. The Golgi as a “Proton Sink” in Cancer. Front. Cell Dev. Biol. 2021;9:664295. doi: 10.3389/fcell.2021.664295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 460.Raghunand N., Mahoney B.P., Gillies R.J. Tumor Acidity, Ion Trapping and Chemotherapeutics. II. pH-Dependent Partition Coefficients Predict Importance of Ion Trapping on Pharmacokinetics of Weakly Basic Chemotherapeutic Agents. Biochem. Pharmacol. 2003;66:1219–1229. doi: 10.1016/S0006-2952(03)00468-4. [DOI] [PubMed] [Google Scholar]
- 461.Estrella V., Chen T., Lloyd M., Wojtkowiak J., Cornnell H.H., Ibrahim-Hashim A., Bailey K., Balagurunathan Y., Rothberg J.M., Sloane B.F., et al. Acidity Generated by the Tumor Microenvironment Drives Local Invasion. Cancer Res. 2013;73:1524–1535. doi: 10.1158/0008-5472.CAN-12-2796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 462.Omran Z., Scaife P., Stewart S., Rauch C. Physical and Biological Characteristics of Multi Drug Resistance (MDR): An Integral Approach Considering pH and Drug Resistance in Cancer. Semin. Cancer Biol. 2017;43:42–48. doi: 10.1016/j.semcancer.2017.01.002. [DOI] [PubMed] [Google Scholar]
- 463.Hao G., Xu Z.P., Li L. Manipulating Extracellular Tumour pH: An Effective Target for Cancer Therapy. RSC Adv. 2018;8:22182–22192. doi: 10.1039/C8RA02095G. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 464.Theparambil S.M., Weber T., Schmälzle J., Ruminot I., Deitmer J.W. Proton Fall or Bicarbonate Rise: GLYCOLYTIC RATE IN MOUSE ASTROCYTES IS PAVED BY INTRACELLULAR ALKALINIZATION. J. Biol. Chem. 2016;291:19108–19117. doi: 10.1074/jbc.M116.730143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 465.Ma Z., Cao M., Liu Y., He Y., Wang Y., Yang C., Wang W., Du Y., Zhou M., Gao F. Mitochondrial F1Fo-ATP Synthase Translocates to Cell Surface in Hepatocytes and Has High Activity in Tumor-like Acidic and Hypoxic Environment. Acta Biochim. Biophys. Sin. 2010;42:530–537. doi: 10.1093/abbs/gmq063. [DOI] [PubMed] [Google Scholar]
- 466.Kim B.-W., Choo H.-J., Lee J.-W., Kim J.-H., Ko Y.-G. Extracellular ATP Is Generated by ATP Synthase Complex in Adipocyte Lipid Rafts. Exp. Mol. Med. 2004;36:476–485. doi: 10.1038/emm.2004.60. [DOI] [PubMed] [Google Scholar]
- 467.Bae T.-J., Kim M.-S., Kim J.-W., Kim B.-W., Choo H.-J., Lee J.-W., Kim K.-B., Lee C.S., Kim J.-H., Chang S.Y., et al. Lipid Raft Proteome Reveals ATP Synthase Complex in the Cell Surface. Proteomics. 2004;4:3536–3548. doi: 10.1002/pmic.200400952. [DOI] [PubMed] [Google Scholar]
- 468.Wang X., Li Y., Qian Y., Cao Y., Shriwas P., Zhang H., Chen X. Extracellular ATP, as an Energy and Phosphorylating Molecule, Induces Different Types of Drug Resistances in Cancer Cells through ATP Internalization and Intracellular ATP Level Increase. Oncotarget. 2017;8:87860–87877. doi: 10.18632/oncotarget.21231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 469.Qian Y., Wang X., Liu Y., Li Y., Colvin R.A., Tong L., Wu S., Chen X. Extracellular ATP Is Internalized by Macropinocytosis and Induces Intracellular ATP Increase and Drug Resistance in Cancer Cells. Cancer Lett. 2014;351:242–251. doi: 10.1016/j.canlet.2014.06.008. [DOI] [PubMed] [Google Scholar]
- 470.Vasiliou V., Vasiliou K., Nebert D.W. Human ATP-Binding Cassette (ABC) Transporter Family. Hum. Genom. 2009;3:281–290. doi: 10.1186/1479-7364-3-3-281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 471.Sharma S., Kalra H., Akundi R.S. Extracellular ATP Mediates Cancer Cell Migration and Invasion Through Increased Expression of Cyclooxygenase 2. Front. Pharmacol. 2020;11:617211. doi: 10.3389/fphar.2020.617211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 472.Alvarez C.L., Troncoso M.F., Espelt M.V. Extracellular ATP and Adenosine in Tumor Microenvironment: Roles in Epithelial-Mesenchymal Transition, Cell Migration, and Invasion. J. Cell. Physiol. 2021 doi: 10.1002/jcp.30580. [DOI] [PubMed] [Google Scholar]
- 473.Cao Y., Wang X., Li Y., Evers M., Zhang H., Chen X. Extracellular and Macropinocytosis Internalized ATP Work Together to Induce Epithelial-Mesenchymal Transition and Other Early Metastatic Activities in Lung Cancer. Cancer Cell Int. 2019;19:254. doi: 10.1186/s12935-019-0973-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 474.Song J., Chen X. Abstract 3106: Roles of Extracellular ATP in Inducing Cancer Stem Cell (CSC)-like Changes in Non-Small Lung Cancer Cell Line. Cancer Res. 2021;81((Suppl. S36)):3106. doi: 10.1158/1538-7445.AM2021-3106. [DOI] [Google Scholar]
- 475.Dratkiewicz E., Simiczyjew A., Mazurkiewicz J., Ziętek M., Matkowski R., Nowak D. Hypoxia and Extracellular Acidification as Drivers of Melanoma Progression and Drug Resistance. Cells. 2021;10:862. doi: 10.3390/cells10040862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 476.Han Y.-S., Lee J.H., Yoon Y.M., Yun C.W., Noh H., Lee S.H. Hypoxia-Induced Expression of Cellular Prion Protein Improves the Therapeutic Potential of Mesenchymal Stem Cells. Cell Death Dis. 2016;7:e2395. doi: 10.1038/cddis.2016.310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 477.Sauer H., Dagdanova A., Hescheler J., Wartenberg M. Redox-Regulation of Intrinsic Prion Expression in Multicellular Prostate Tumor Spheroids. Free Radic. Biol. Med. 1999;27:1276–1283. doi: 10.1016/S0891-5849(99)00164-1. [DOI] [PubMed] [Google Scholar]
- 478.Matafora V., Farris F., Restuccia U., Tamburri S., Martano G., Bernardelli C., Sofia A., Pisati F., Casagrande F., Lazzari L., et al. Amyloid Aggregates Accumulate in Melanoma Metastasis Modulating YAP Activity. EMBO Rep. 2020;21:e50446. doi: 10.15252/embr.202050446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 479.Dec R., Puławski W., Dzwolak W. Selective and Stoichiometric Incorporation of ATP by Self-Assembling Amyloid Fibrils. J. Mater. Chem. B Mater. Biol. Med. 2021;9:8626–8630. doi: 10.1039/D1TB01976G. [DOI] [PubMed] [Google Scholar]
- 480.Brown D.R. ORGINAL ARTICLE Neurodegeneration and Oxidative Stress: Prion Disease Results from Loss of Antioxidant Defence. Folia Neuropathol. 2006;43:229–243. [PubMed] [Google Scholar]
- 481.Kim J.I., Choi S.I., Kim N.H., Jin J.K., Choi E.K., Carp R.I., Kim Y.S. Oxidative Stress and Neurodegeneration in Prion Diseases. Ann. N. Y. Acad. Sci. 2001;928:182–186. doi: 10.1111/j.1749-6632.2001.tb05648.x. [DOI] [PubMed] [Google Scholar]
- 482.Guentchev M., Voigtländer T., Haberler C., Groschup M.H., Budka H. Evidence for Oxidative Stress in Experimental Prion Disease. Neurobiol. Dis. 2000;7:270–273. doi: 10.1006/nbdi.2000.0290. [DOI] [PubMed] [Google Scholar]
- 483.Prasad K.N., Bondy S.C. Oxidative and Inflammatory Events in Prion Diseases: Can They Be Therapeutic Targets? Curr. Aging Sci. 2019;11:216–225. doi: 10.2174/1874609812666190111100205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 484.Boussadia Z., Lamberti J., Mattei F., Pizzi E., Puglisi R., Zanetti C., Pasquini L., Fratini F., Fantozzi L., Felicetti F., et al. Acidic Microenvironment Plays a Key Role in Human Melanoma Progression through a Sustained Exosome Mediated Transfer of Clinically Relevant Metastatic Molecules. J. Exp. Clin. Cancer Res. 2018;37:245. doi: 10.1186/s13046-018-0915-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 485.Stüwe L., Müller M., Fabian A., Waning J., Mally S., Noël J., Schwab A., Stock C. pH Dependence of Melanoma Cell Migration: Protons Extruded by NHE1 Dominate Protons of the Bulk Solution. Pt 2J. Physiol. 2007;585:351–360. doi: 10.1113/jphysiol.2007.145185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 486.Moreno A.C.R., de Freitas Saito R., Tiago M., Massaro R.R., Pagni R.L., Pegoraro R., da Cruz Souza P., Reiter R.J., Campa A., Soengas M.S., et al. Melatonin Inhibits Human Melanoma Cells Proliferation and Invasion via Cell Cycle Arrest and Cytoskeleton Remodeling. Melatonin Res. 2020;3:194–209. doi: 10.32794/mr11250057. [DOI] [Google Scholar]
- 487.Gonzalez R., Sanchez A., Ferguson J.A., Balmer C., Daniel C., Cohn A., Robinson W.A. Melatonin Therapy of Advanced Human Malignant Melanoma. Melanoma Res. 1991;1:237–243. doi: 10.1097/00008390-199111000-00003. [DOI] [PubMed] [Google Scholar]
- 488.Sonehara N.M., Lacerda J.Z., Jardim-Perassi B.V., de Paula R., Jr., Moschetta-Pinheiro M.G., Souza Y.S.T., de Andrade J.C.J., De Campos Zuccari D.A.P. Melatonin Regulates Tumor Aggressiveness under Acidosis Condition in Breast Cancer Cell Lines. Oncol. Lett. 2019;17:1635–1645. doi: 10.3892/ol.2018.9758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 489.Aust S., Brucker B., Graf J., Klimpfinger M., Thalhammer T. Melatonin Modulates Acid/base Transport in Human Pancreatic Carcinoma Cells. Cell. Physiol. Biochem. 2006;18:91–102. doi: 10.1159/000095173. [DOI] [PubMed] [Google Scholar]
- 490.Henry R.P. Multiple Roles of Carbonic Anhydrase in Cellular Transport and Metabolism. Annu. Rev. Physiol. 1996;58:523–538. doi: 10.1146/annurev.ph.58.030196.002515. [DOI] [PubMed] [Google Scholar]
- 491.Breton S. The Cellular Physiology of Carbonic Anhydrases. JOP. 2001;2((Suppl. S4)):159–164. [PubMed] [Google Scholar]
- 492.Tafreshi N.K., Lloyd M.C., Proemsey J.B., Bui M.M., Kim J., Gillies R.J., Morse D.L. Evaluation of CAIX and CAXII Expression in Breast Cancer at Varied O2 Levels: CAIX Is the Superior Surrogate Imaging Biomarker of Tumor Hypoxia. Mol. Imaging Biol. 2016;18:219–231. doi: 10.1007/s11307-015-0885-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 493.Potter C., Harris A.L. Hypoxia Inducible Carbonic Anhydrase IX, Marker of Tumour: Hypoxia, Survival Pathway and Therapy Target. Cell Cycle. 2004;3:159–162. doi: 10.4161/cc.3.2.618. [DOI] [PubMed] [Google Scholar]
- 494.Chiche J., Ilc K., Laferrière J., Trottier E., Dayan F., Mazure N.M., Brahimi-Horn M.C., Pouysségur J. Hypoxia-Inducible Carbonic Anhydrase IX and XII Promote Tumor Cell Growth by Counteracting Acidosis through the Regulation of the Intracellular pH. Cancer Res. 2009;69:358–368. doi: 10.1158/0008-5472.CAN-08-2470. [DOI] [PubMed] [Google Scholar]
- 495.de Lima Mota A., Jardim-Perassi B.V., de Castro T.B., Colombo J., Sonehara N.M., Nishiyama V.K.G., Pierri V.A.G., de Campos Zuccari D.A.P. Melatonin Modifies Tumor Hypoxia and Metabolism by Inhibiting HIF-1α and Energy Metabolic Pathway in the in Vitro and in Vivo Models of Breast Cancer. Melatonin Res. 2019;2:83–98. doi: 10.32794/mr11250042. [DOI] [Google Scholar]
- 496.Iyer N.V., Kotch L.E., Agani F., Leung S.W., Laughner E., Wenger R.H., Gassmann M., Gearhart J.D., Lawler A.M., Yu A.Y., et al. Cellular and Developmental Control of O2 Homeostasis by Hypoxia-Inducible Factor 1 Alpha. Genes Dev. 1998;12:149–162. doi: 10.1101/gad.12.2.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 497.Swenson E.R. Hypoxia and Its Acid-Base Consequences: From Mountains to Malignancy. Adv. Exp. Med. Biol. 2016;903:301–323. doi: 10.1007/978-1-4899-7678-9_21. [DOI] [PubMed] [Google Scholar]
- 498.Magovern G.J., Cartwright R.S., Neville J.F., Jr., Kent E.M. Metabolic Acidosis and the Dissociation Curve of Hemoglobin during Extracorporeal Circulation. J. Thorac. Cardiovasc. Surg. 1959;38:561–572. doi: 10.1016/S0022-5223(19)32419-5. [DOI] [PubMed] [Google Scholar]
- 499.Liu C., Lin Q., Yun Z. Cellular and Molecular Mechanisms Underlying Oxygen-Dependent Radiosensitivity. Radiat. Res. 2015;183:487–496. doi: 10.1667/RR13959.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 500.Kaufman D.P., Kandle P.F., Murray I., Dhamoon A.S. StatPearls. StatPearls Publishing; Treasure Island, FL, USA: 2021. Physiology, Oxyhemoglobin Dissociation Curve. [Google Scholar]
- 501.Darling R.C., Roughton F.J.W. The Effect Of Methemoglobin on the Equilibrium Between Oxygen and Hemoglobin. Am. J. Physiol.-Leg. Content. 1942;137:56–68. doi: 10.1152/ajplegacy.1942.137.1.56. [DOI] [Google Scholar]
- 502.Hirst D.G., Wood P.J. The Influence of Haemoglobin Affinity for Oxygen on Tumour Radiosensitivity. Br. J. Cancer. 1987;55:487–491. doi: 10.1038/bjc.1987.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 503.Kirkpatrick J.P., Cárdenas-Navia L.I., Dewhirst M.W. Predicting the Effect of Temporal Variations in pO2 on Tumor Radiosensitivity. Int. J. Radiat. Oncol. Biol. Phys. 2004;59:822–833. doi: 10.1016/j.ijrobp.2004.02.015. [DOI] [PubMed] [Google Scholar]
- 504.Thomas C.D., Chavaudra N., Martin L., Guichard M. Correlation between Radiosensitivity, Percentage Hypoxic Cells and pO2 Measurements in One Rodent and Two Human Tumor Xenografts. Radiat. Res. 1994;139:1–8. doi: 10.2307/3578725. [DOI] [PubMed] [Google Scholar]
- 505.Lamonte G., Tang X., Chen J.L.-Y., Wu J., Ding C.-K.C., Keenan M.M., Sangokoya C., Kung H.-N., Ilkayeva O., Boros L.G., et al. Acidosis Induces Reprogramming of Cellular Metabolism to Mitigate Oxidative Stress. Cancer Metab. 2013;1:23. doi: 10.1186/2049-3002-1-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 506.Ackerman D., Simon M.C. Hypoxia, Lipids, and Cancer: Surviving the Harsh Tumor Microenvironment. Trends Cell Biol. 2014;24:472–478. doi: 10.1016/j.tcb.2014.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 507.Rybner C., Finel-Szermanski S., Felin M., Sahraoui T., Rousseau C., Fournier J.G., Sève A.P., Botti J. The Cellular Prion Protein: A New Partner of the Lectin CBP70 in the Nucleus of NB4 Human Promyelocytic Leukemia Cells. J. Cell. Biochem. 2002;84:408–419. doi: 10.1002/jcb.10017. [DOI] [PubMed] [Google Scholar]
- 508.Hosokawa T., Tsuchiya K., Sato I., Takeyama N., Ueda S., Tagawa Y., Kimura K.M., Nakamura I., Wu G., Sakudo A., et al. A Monoclonal Antibody (1D12) Defines Novel Distribution Patterns of Prion Protein (PrP) as Granules in Nucleus. Biochem. Biophys. Res. Commun. 2008;366:657–663. doi: 10.1016/j.bbrc.2007.11.163. [DOI] [PubMed] [Google Scholar]
- 509.Strom A., Wang G.-S., Picketts D.J., Reimer R., Stuke A.W., Scott F.W. Cellular Prion Protein Localizes to the Nucleus of Endocrine and Neuronal Cells and Interacts with Structural Chromatin Components. Eur. J. Cell Biol. 2011;90:414–419. doi: 10.1016/j.ejcb.2010.11.015. [DOI] [PubMed] [Google Scholar]
- 510.Morel E., Fouquet S., Strup-Perrot C., Pichol Thievend C., Petit C., Loew D., Faussat A.-M., Yvernault L., Pinçon-Raymond M., Chambaz J., et al. The Cellular Prion Protein PrP(c) Is Involved in the Proliferation of Epithelial Cells and in the Distribution of Junction-Associated Proteins. PLoS ONE. 2008;3:e3000. doi: 10.1371/annotation/0b364095-9f93-4cb9-9a2e-aae5ed1bf362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 511.Yao Y., Dai W. Genomic Instability and Cancer. J. Carcinog. Mutagen. 2014;5:1000165. doi: 10.4172/2157-2518.1000165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 512.Hornshaw M.P., McDermott J.R., Candy J.M., Lakey J.H. Copper Binding to the N-Terminal Tandem Repeat Region of Mammalian and Avian Prion Protein: Structural Studies Using Synthetic Peptides. Biochem. Biophys. Res. Commun. 1995;214:993–999. doi: 10.1006/bbrc.1995.2384. [DOI] [PubMed] [Google Scholar]
- 513.Caputo A., Sarnataro D., Campana V., Costanzo M., Negro A., Sorgato M.C., Zurzolo C. Doppel and PrPC Co-Immunoprecipitate in Detergent-Resistant Membrane Domains of Epithelial FRT Cells. Biochem. J. 2009;425:341–351. doi: 10.1042/BJ20091050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 514.Martellucci S., Santacroce C., Santilli F., Manganelli V., Sorice M., Mattei V. Prion Protein in Stem Cells: A Lipid Raft Component Involved in the Cellular Differentiation Process. Int. J. Mol. Sci. 2020;21:4168. doi: 10.3390/ijms21114168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 515.Lee Y.J., Baskakov I.V. The Cellular Form of the Prion Protein Is Involved in Controlling Cell Cycle Dynamics, Self-Renewal, and the Fate of Human Embryonic Stem Cell Differentiation. J. Neurochem. 2013;124:310–322. doi: 10.1111/j.1471-4159.2012.07913.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 516.Zhang C.C., Steele A.D., Lindquist S., Lodish H.F. Prion Protein Is Expressed on Long-Term Repopulating Hematopoietic Stem Cells and Is Important for Their Self-Renewal. Proc. Natl. Acad. Sci. USA. 2006;103:2184–2189. doi: 10.1073/pnas.0510577103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 517.Dodelet V.C., Cashman N.R. Prion Protein Expression in Human Leukocyte Differentiation. Blood. 1998;91:1556–1561. doi: 10.1182/blood.V91.5.1556. [DOI] [PubMed] [Google Scholar]
- 518.Barba-Bon A., Nilam M., Hennig A. Supramolecular Chemistry in the Biomembrane. ChemBioChem. 2020;21:886–910. doi: 10.1002/cbic.201900646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 519.Martellucci S., Santacroce C., Manganelli V., Santilli F., Piccoli L., Cassetta M., Misasi R., Sorice M., Mattei V. Isolation, Propagation, and Prion Protein Expression During Neuronal Differentiation of Human Dental Pulp Stem Cells. J. Vis. Exp. 2019;18:e59282. doi: 10.3791/59282. [DOI] [PubMed] [Google Scholar]
- 520.Liang J., Ge F., Guo C., Luo G., Wang X., Han G., Zhang D., Wang J., Li K., Pan Y., et al. Inhibition of PI3K/Akt Partially Leads to the Inhibition of PrP(C)-Induced Drug Resistance in Gastric Cancer Cells. FEBS J. 2009;276:685–694. doi: 10.1111/j.1742-4658.2008.06816.x. [DOI] [PubMed] [Google Scholar]
- 521.Pushie M.J., Pickering I.J., Martin G.R., Tsutsui S., Jirik F.R., George G.N. Prion Protein Expression Level Alters Regional Copper, Iron and Zinc Content in the Mouse Brain. Metallomics. 2011;3:206–214. doi: 10.1039/c0mt00037j. [DOI] [PubMed] [Google Scholar]
- 522.Gasperini L., Meneghetti E., Legname G., Benetti F. In Absence of the Cellular Prion Protein, Alterations in Copper Metabolism and Copper-Dependent Oxidase Activity Affect Iron Distribution. Front. Neurosci. 2016;10:437. doi: 10.3389/fnins.2016.00437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 523.Osaki S., Johnson D.A., Frieden E. The Mobilization of Iron from the Perfused Mammalian Liver by a Serum Copper Enzyme, Ferroxidase, I.J. Biol. Chem. 1971;246:3018–3023. doi: 10.1016/S0021-9258(18)62284-7. [DOI] [PubMed] [Google Scholar]
- 524.Abbaspour N., Hurrell R., Kelishadi R. Review on Iron and Its Importance for Human Health. J. Res. Med. Sci. 2014;19:164–174. [PMC free article] [PubMed] [Google Scholar]
- 525.Singh A., Mohan M.L., Isaac A.O., Luo X., Petrak J., Vyoral D., Singh N. Prion Protein Modulates Cellular Iron Uptake: A Novel Function with Implications for Prion Disease Pathogenesis. PLoS ONE. 2009;4:e4468. doi: 10.1371/annotation/194f4e44-20f0-48eb-bbe9-14e21d18909b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 526.Singh A., Isaac A.O., Luo X., Mohan M.L., Cohen M.L., Chen F., Kong Q., Bartz J., Singh N. Abnormal Brain Iron Homeostasis in Human and Animal Prion Disorders. PLoS Pathog. 2009;5:e1000336. doi: 10.1371/journal.ppat.1000336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 527.Koppenol W.H., Bounds P.L., Dang C.V. Otto Warburg’s Contributions to Current Concepts of Cancer Metabolism. Nat. Rev. Cancer. 2011;11:325–337. doi: 10.1038/nrc3038. [DOI] [PubMed] [Google Scholar]
- 528.Marín-Hernández A., Gallardo-Pérez J.C., Rodríguez-Enríquez S., Encalada R., Moreno-Sánchez R., Saavedra E. Modeling Cancer Glycolysis. Biochim. Biophys. Acta. 2011;1807:755–767. doi: 10.1016/j.bbabio.2010.11.006. [DOI] [PubMed] [Google Scholar]
- 529.Feng J., Li J., Wu L., Yu Q., Ji J., Wu J., Dai W., Guo C. Emerging Roles and the Regulation of Aerobic Glycolysis in Hepatocellular Carcinoma. J. Exp. Clin. Cancer Res. 2020;39:126. doi: 10.1186/s13046-020-01629-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 530.Lorito N., Bacci M., Smiriglia A., Mannelli M., Parri M., Comito G., Ippolito L., Giannoni E., Bonechi M., Benelli M., et al. Glucose Metabolic Reprogramming of ER Breast Cancer in Acquired Resistance to the CDK4/6 Inhibitor Palbociclib. Cells. 2020;9:668. doi: 10.3390/cells9030668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 531.Wang X., Zhang H., Yang H., Bai M., Ning T., Deng T., Liu R., Fan Q., Zhu K., Li J., et al. Exosome-Delivered circRNA Promotes Glycolysis to Induce Chemoresistance through the miR-122-PKM2 Axis in Colorectal Cancer. Mol. Oncol. 2020;14:539–555. doi: 10.1002/1878-0261.12629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 532.Wagner W., Kania K.D., Blauz A., Ciszewski W.M. The Lactate Receptor (HCAR1/GPR81) Contributes to Doxorubicin Chemoresistance via ABCB1 Transporter up-Regulation in Human Cervical Cancer HeLa Cells. J. Physiol. Pharmacol. 2017;68:555–564. [PubMed] [Google Scholar]
- 533.Ruprecht B., Zaal E.A., Zecha J., Wu W., Berkers C.R., Kuster B., Lemeer S. Lapatinib Resistance in Breast Cancer Cells Is Accompanied by Phosphorylation-Mediated Reprogramming of Glycolysis. Cancer Res. 2017;77:1842–1853. doi: 10.1158/0008-5472.CAN-16-2976. [DOI] [PubMed] [Google Scholar]
- 534.Aldonza M.B.D., Hong J.-Y., Lee S.K. Paclitaxel-Resistant Cancer Cell-Derived Secretomes Elicit ABCB1-Associated Docetaxel Cross-Resistance and Escape from Apoptosis through FOXO3a-Driven Glycolytic Regulation. Exp. Mol. Med. 2017;49:e286. doi: 10.1038/emm.2016.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 535.Eriksson J.A., Wanka C., Burger M.C., Urban H., Hartel I., von Renesse J., Harter P.N., Mittelbronn M., Steinbach J.P., Rieger J. Suppression of Oxidative Phosphorylation Confers Resistance against Bevacizumab in Experimental Glioma. J. Neurochem. 2018;144:421–430. doi: 10.1111/jnc.14264. [DOI] [PubMed] [Google Scholar]
- 536.Fu J., Jiang H., Wu C., Jiang Y., Xiao L., Tian Y. Overcoming Cetuximab Resistance in Ewing’s Sarcoma by Inhibiting Lactate Dehydrogenase-A. Mol. Med. Rep. 2016;14:995–1001. doi: 10.3892/mmr.2016.5290. [DOI] [PubMed] [Google Scholar]
- 537.de Beauchamp L., Himonas E., Helgason G.V. Mitochondrial Metabolism as a Potential Therapeutic Target in Myeloid Leukaemia. Leukemia. 2021;36:1–12. doi: 10.1038/s41375-021-01416-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 538.Ricci J.-E., Chiche J. Metabolic Reprogramming of Non-Hodgkin’s B-Cell Lymphomas and Potential Therapeutic Strategies. Front. Oncol. 2018;8:556. doi: 10.3389/fonc.2018.00556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 539.Reyes-Castellanos G., Masoud R., Carrier A. Mitochondrial Metabolism in PDAC: From Better Knowledge to New Targeting Strategies. Biomedicines. 2020;8:270. doi: 10.3390/biomedicines8080270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 540.Salhi A., Jordan A.C., Bochaca I.I., Izsak A., Darvishian F., Houvras Y., Giles K.M., Osman I. Oxidative Phosphorylation Promotes Primary Melanoma Invasion. Am. J. Pathol. 2020;190:1108–1117. doi: 10.1016/j.ajpath.2020.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 541.Schöpf B., Weissensteiner H., Schäfer G., Fazzini F., Charoentong P., Naschberger A., Rupp B., Fendt L., Bukur V., Giese I., et al. OXPHOS Remodeling in High-Grade Prostate Cancer Involves mtDNA Mutations and Increased Succinate Oxidation. Nat. Commun. 2020;11:1487. doi: 10.1038/s41467-020-15237-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 542.Ashton T.M., McKenna W.G., Kunz-Schughart L.A., Higgins G.S. Oxidative Phosphorylation as an Emerging Target in Cancer Therapy. Clin. Cancer Res. 2018;24:2482–2490. doi: 10.1158/1078-0432.CCR-17-3070. [DOI] [PubMed] [Google Scholar]
- 543.Hirpara J., Eu J.Q., Tan J.K.M., Wong A.L., Clement M.-V., Kong L.R., Ohi N., Tsunoda T., Qu J., Goh B.C., et al. Metabolic Reprogramming of Oncogene-Addicted Cancer Cells to OXPHOS as a Mechanism of Drug Resistance. Redox Biol. 2019;25:101076. doi: 10.1016/j.redox.2018.101076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 544.Lee S., Lee J.-S., Seo J., Lee S.-H., Kang J.H., Song J., Kim S.-Y. Targeting Mitochondrial Oxidative Phosphorylation Abrogated Irinotecan Resistance in NSCLC. Sci. Rep. 2018;8:15707. doi: 10.1038/s41598-018-33667-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 545.Vellinga T.T., Borovski T., de Boer V.C.J., Fatrai S., van Schelven S., Trumpi K., Verheem A., Snoeren N., Emmink B.L., Koster J., et al. SIRT1/PGC1α-Dependent Increase in Oxidative Phosphorylation Supports Chemotherapy Resistance of Colon Cancer. Clin. Cancer Res. 2015;21:2870–2879. doi: 10.1158/1078-0432.CCR-14-2290. [DOI] [PubMed] [Google Scholar]
- 546.Lee J.-S., Lee H., Jang H., Woo S.M., Park J.B., Lee S.-H., Kang J.H., Kim H.Y., Song J., Kim S.-Y. Targeting Oxidative Phosphorylation Reverses Drug Resistance in Cancer Cells by Blocking Autophagy Recycling. Cells. 2020;9:2013. doi: 10.3390/cells9092013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 547.Denise C., Paoli P., Calvani M., Taddei M.L., Giannoni E., Kopetz S., Kazmi S.M.A., Pia M.M., Pettazzoni P., Sacco E., et al. 5-Fluorouracil Resistant Colon Cancer Cells Are Addicted to OXPHOS to Survive and Enhance Stem-like Traits. Oncotarget. 2015;6:41706–41721. doi: 10.18632/oncotarget.5991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 548.Salunkhe S., Mishra S.V., Ghorai A., Hole A., Chandrani P., Dutt A., Chilakapati M., Dutt S. Metabolic Rewiring in Drug Resistant Cells Exhibit Higher OXPHOS and Fatty Acids as Preferred Major Source to Cellular Energetics. Biochim. Biophys. Acta Bioenerg. 2020;1861:148300. doi: 10.1016/j.bbabio.2020.148300. [DOI] [PubMed] [Google Scholar]
- 549.Seyfried T.N., Arismendi-Morillo G., Mukherjee P., Chinopoulos C. On the Origin of ATP Synthesis in Cancer. iScience. 2020;23:101761. doi: 10.1016/j.isci.2020.101761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 550.Veech R.L., Lawson J.W., Cornell N.W., Krebs H.A. Cytosolic Phosphorylation Potential. J. Biol. Chem. 1979;254:6538–6547. doi: 10.1016/S0021-9258(18)50401-4. [DOI] [PubMed] [Google Scholar]
- 551.Veech R.L., King M.T., Pawlosky R., Bradshaw P.C., Curtis W. Relationship between Inorganic Ion Distribution, Resting Membrane Potential, and the ΔG’ of ATP Hydrolysis: A New Paradigm. FASEB J. 2019;33:13126–13130. doi: 10.1096/fj.201901942R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 552.Poljsak B., Kovac V., Dahmane R., Levec T., Starc A. Cancer Etiology: A Metabolic Disease Originating from Life’s Major Evolutionary Transition? Oxid. Med. Cell. Longev. 2019;2019:7831952. doi: 10.1155/2019/7831952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 553.Fiorito V., Chiabrando D., Petrillo S., Bertino F., Tolosano E. The Multifaceted Role of Heme in Cancer. Front. Oncol. 2019;9:1540. doi: 10.3389/fonc.2019.01540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 554.Wang Y., Yu L., Ding J., Chen Y. Iron Metabolism in Cancer. Int. J. Mol. Sci. 2018;20:95. doi: 10.3390/ijms20010095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 555.Kazan H.H., Urfali-Mamatoglu C., Gunduz U. Iron Metabolism and Drug Resistance in Cancer. Biometals. 2017;30:629–641. doi: 10.1007/s10534-017-0037-7. [DOI] [PubMed] [Google Scholar]
- 556.Forciniti S., Greco L., Grizzi F., Malesci A., Laghi L. Iron Metabolism in Cancer Progression. Int. J. Mol. Sci. 2020;21:2257. doi: 10.3390/ijms21062257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 557.Chen Y., Fan Z., Yang Y., Gu C. Iron Metabolism and Its Contribution to Cancer (Review) Int. J. Oncol. 2019;54:1143–1154. doi: 10.3892/ijo.2019.4720. [DOI] [PubMed] [Google Scholar]
- 558.Morales M., Xue X. Targeting Iron Metabolism in Cancer Therapy. Theranostics. 2021;11:8412–8429. doi: 10.7150/thno.59092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 559.Brown R.A.M., Richardson K.L., Kabir T.D., Trinder D., Ganss R., Leedman P.J. Altered Iron Metabolism and Impact in Cancer Biology, Metastasis, and Immunology. Front. Oncol. 2020;10:476. doi: 10.3389/fonc.2020.00476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 560.Bastide N., Morois S., Cadeau C., Kangas S., Serafini M., Gusto G., Dossus L., Pierre F.H., Clavel-Chapelon F., Boutron-Ruault M.-C. Heme Iron Intake, Dietary Antioxidant Capacity, and Risk of Colorectal Adenomas in a Large Cohort Study of French Women. Cancer Epidemiol. Biomarkers Prev. 2016;25:640–647. doi: 10.1158/1055-9965.EPI-15-0724. [DOI] [PubMed] [Google Scholar]
- 561.Bastide N.M., Chenni F., Audebert M., Santarelli R.L., Taché S., Naud N., Baradat M., Jouanin I., Surya R., Hobbs D.A., et al. A Central Role for Heme Iron in Colon Carcinogenesis Associated with Red Meat Intake. Cancer Res. 2015;75:870–879. doi: 10.1158/0008-5472.CAN-14-2554. [DOI] [PubMed] [Google Scholar]
- 562.Thomas C., Mackey M.M., Diaz A.A., Cox D.P. Hydroxyl Radical Is Produced via the Fenton Reaction in Submitochondrial Particles under Oxidative Stress: Implications for Diseases Associated with Iron Accumulation. Redox Rep. 2009;14:102–108. doi: 10.1179/135100009X392566. [DOI] [PubMed] [Google Scholar]
- 563.Oliver T., Sánchez-Baracaldo P., Larkum A.W., Rutherford A.W., Cardona T. Time-Resolved Comparative Molecular Evolution of Oxygenic Photosynthesis. Biochim. Biophys. Acta Bioenerg. 2021;1862:148400. doi: 10.1016/j.bbabio.2021.148400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 564.Lubitz W., Chrysina M., Cox N. Water Oxidation in Photosystem II. Photosynth. Res. 2019;142:105–125. doi: 10.1007/s11120-019-00648-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 565.Rantamäki S., Meriluoto J., Spoof L., Puputti E.-M., Tyystjärvi T., Tyystjärvi E. Oxygen Produced by Cyanobacteria in Simulated Archaean Conditions Partly Oxidizes Ferrous Iron but Mostly Escapes-Conclusions about Early Evolution. Photosynth. Res. 2016;130:103–111. doi: 10.1007/s11120-016-0231-4. [DOI] [PubMed] [Google Scholar]
- 566.Benger G., Govindjee The Mechanism of Photosynthetic Water Oxidation. Photosynth. Res. 1985;6:33–55. doi: 10.1007/BF00029045. [DOI] [PubMed] [Google Scholar]
- 567.Campbell G.R., Mahad D.J. A Method to Detect Cytochrome c Oxidase Activity and Mitochondrial Proteins in Oligodendrocytes. Methods Mol. Biol. 2019;1936:333–342. doi: 10.1007/978-1-4939-9072-6_19. [DOI] [PubMed] [Google Scholar]
- 568.Tsukihara T., Shimokata K., Katayama Y., Shimada H., Muramoto K., Aoyama H., Mochizuki M., Shinzawa-Itoh K., Yamashita E., Yao M., et al. The Low-Spin Heme of Cytochrome c Oxidase as the Driving Element of the Proton-Pumping Process. Proc. Natl. Acad. Sci. USA. 2003;100:15304–15309. doi: 10.1073/pnas.2635097100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 569.Nicholls P. Observations on the Oxidation of Cytochrome C. Arch. Biochem. Biophys. 1964;106:25–48. doi: 10.1016/0003-9861(64)90154-7. [DOI] [PubMed] [Google Scholar]
- 570.Hooda J., Shah A., Zhang L. Heme, an Essential Nutrient from Dietary Proteins, Critically Impacts Diverse Physiological and Pathological Processes. Nutrients. 2014;6:1080–1102. doi: 10.3390/nu6031080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 571.Reedy C.J., Gibney B.R. Heme Protein Assemblies. Chem. Rev. 2004;104:617–649. doi: 10.1021/cr0206115. [DOI] [PubMed] [Google Scholar]
- 572.Sachar M., Anderson K.E., Ma X. Protoporphyrin IX: The Good, the Bad, and the Ugly. J. Pharmacol. Exp. Ther. 2016;356:267–275. doi: 10.1124/jpet.115.228130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 573.Ajioka R.S., Phillips J.D., Kushner J.P. Biosynthesis of Heme in Mammals. Biochim. Biophys. Acta. 2006;1763:723–736. doi: 10.1016/j.bbamcr.2006.05.005. [DOI] [PubMed] [Google Scholar]
- 574.Fiorito V., Allocco A.L., Petrillo S., Gazzano E., Torretta S., Marchi S., Destefanis F., Pacelli C., Audrito V., Provero P., et al. The Heme Synthesis-Export System Regulates the Tricarboxylic Acid Cycle Flux and Oxidative Phosphorylation. Cell Rep. 2021;35:109252. doi: 10.1016/j.celrep.2021.109252. [DOI] [PubMed] [Google Scholar]
- 575.Quigley J.G., Yang Z., Worthington M.T., Phillips J.D., Sabo K.M., Sabath D.E., Berg C.L., Sassa S., Wood B.L., Abkowitz J.L. Identification of a Human Heme Exporter That Is Essential for Erythropoiesis. Cell. 2004;118:757–766. doi: 10.1016/j.cell.2004.08.014. [DOI] [PubMed] [Google Scholar]
- 576.Pan Z., Ding J., Yang Z., Li H., Ding H., Chen Q. LncRNA FLVCR1-AS1 Promotes Proliferation, Migration and Activates Wnt/β-Catenin Pathway through miR-381-3p/CTNNB1 Axis in Breast Cancer. Cancer Cell Int. 2020;20:1–12. doi: 10.1186/s12935-020-01247-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 577.Lin H., Shangguan Z., Zhu M., Bao L., Zhang Q., Pan S. lncRNA FLVCR1-AS1 Silencing Inhibits Lung Cancer Cell Proliferation, Migration, and Invasion by Inhibiting the Activity of the Wnt/β-Catenin Signaling Pathway. J. Cell. Biochem. 2019;120:10625–10632. doi: 10.1002/jcb.28352. [DOI] [PubMed] [Google Scholar]
- 578.Peng C., Song Y., Chen W., Wang X., Liu X., Wang F., Wu D., Ma S., Wang X., Gao C. FLVCR1 Promotes the Proliferation and Tumorigenicity of Synovial Sarcoma through Inhibiting Apoptosis and Autophagy. Int. J. Oncol. 2018;52:1559–1568. doi: 10.3892/ijo.2018.4312. [DOI] [PubMed] [Google Scholar]
- 579.Dey S., Kumari S., Kalainayakan S.P., Campbell J., 3rd, Ghosh P., Zhou H., FitzGerald K.E., Li M., Mason R.P., Zhang L., et al. The Vascular Disrupting Agent Combretastatin A-4 Phosphate Causes Prolonged Elevation of Proteins Involved in Heme Flux and Function in Resistant Tumor Cells. Oncotarget. 2018;9:4090–4101. doi: 10.18632/oncotarget.23734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 580.Hooda J., Cadinu D., Alam M.M., Shah A., Cao T.M., Sullivan L.A., Brekken R., Zhang L. Enhanced Heme Function and Mitochondrial Respiration Promote the Progression of Lung Cancer Cells. PLoS ONE. 2013;8:e63402. doi: 10.1371/journal.pone.0063402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 581.Kalainayakan S.P., FitzGerald K.E., Konduri P.C., Vidal C., Zhang L. Essential Roles of Mitochondrial and Heme Function in Lung Cancer Bioenergetics and Tumorigenesis. Cell Biosci. 2018;8:56. doi: 10.1186/s13578-018-0257-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 582.Panigaj M., Brouckova A., Glierova H., Dvorakova E., Simak J., Vostal J.G., Holada K. Underestimation of the Expression of Cellular Prion Protein on Human Red Blood Cells. Transfusion. 2011;51:1012–1021. doi: 10.1111/j.1537-2995.2010.02924.x. [DOI] [PubMed] [Google Scholar]
- 583.Holada K., Vostal J.G. Different Levels of Prion Protein (PrPc) Expression on Hamster, Mouse and Human Blood Cells. Br. J. Haematol. 2000;110:472–480. doi: 10.1046/j.1365-2141.2000.02158.x. [DOI] [PubMed] [Google Scholar]
- 584.Ogun A.S., Joy N.V., Valentine M. StatPearls. StatPearls Publishing; Treasure Island, FL, USA: 2021. Biochemistry, Heme Synthesis. [PubMed] [Google Scholar]
- 585.Marengo-Rowe A.J. Structure-Function Relations of Human Hemoglobins. Baylor University Medical Center. 2006;Volume 19:239–245. doi: 10.1080/08998280.2006.11928171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 586.Frey P.A., Reed G.H. The Ubiquity of Iron. ACS Chem. Biol. 2012;7:1477–1481. doi: 10.1021/cb300323q. [DOI] [PubMed] [Google Scholar]
- 587.Huang X., Groves J.T. Oxygen Activation and Radical Transformations in Heme Proteins and Metalloporphyrins. Chem. Rev. 2018;118:2491–2553. doi: 10.1021/acs.chemrev.7b00373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 588.Soutyrine A., Yogasingam N., Huang H., Mitchell G. Effects of Heme-PrP Complex on Cell-Free Conversion and Peroxidase-Linked Immunodetection of Prions in Blood-Based Assays. Res. Vet. Sci. 2015;101:168–174. doi: 10.1016/j.rvsc.2015.05.008. [DOI] [PubMed] [Google Scholar]
- 589.Lee K.S., Raymond L.D., Schoen B., Raymond G.J., Kett L., Moore R.A., Johnson L.M., Taubner L., Speare J.O., Onwubiko H.A., et al. Hemin Interactions and Alterations of the Subcellular Localization of Prion Protein. J. Biol. Chem. 2007;282:36525–36533. doi: 10.1074/jbc.M705620200. [DOI] [PubMed] [Google Scholar]
- 590.Wong B.S., Liu T., Li R., Pan T., Petersen R.B., Smith M.A., Gambetti P., Perry G., Manson J.C., Brown D.R., et al. Increased Levels of Oxidative Stress Markers Detected in the Brains of Mice Devoid of Prion Protein. J. Neurochem. 2001;76:565–572. doi: 10.1046/j.1471-4159.2001.00028.x. [DOI] [PubMed] [Google Scholar]
- 591.White A.R., Collins S.J., Maher F., Jobling M.F., Stewart L.R., Thyer J.M., Beyreuther K., Masters C.L., Cappai R. Prion Protein-Deficient Neurons Reveal Lower Glutathione Reductase Activity and Increased Susceptibility to Hydrogen Peroxide Toxicity. Am. J. Pathol. 1999;155:1723–1730. doi: 10.1016/S0002-9440(10)65487-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 592.Tamada M., Nagano O., Tateyama S., Ohmura M., Yae T., Ishimoto T., Sugihara E., Onishi N., Yamamoto T., Yanagawa H., et al. Modulation of Glucose Metabolism by CD44 Contributes to Antioxidant Status and Drug Resistance in Cancer Cells. Cancer Res. 2012;72:1438–1448. doi: 10.1158/0008-5472.CAN-11-3024. [DOI] [PubMed] [Google Scholar]
- 593.Cossu V., Bonanomi M., Bauckneht M., Ravera S., Righi N., Miceli A., Morbelli S., Orengo A.M., Piccioli P., Bruno S., et al. Two High-Rate Pentose-Phosphate Pathways in Cancer Cells. Sci. Rep. 2020;10:22111. doi: 10.1038/s41598-020-79185-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 594.Qiu J., Zheng Q., Meng X. Hyperglycemia and Chemoresistance in Breast Cancer: From Cellular Mechanisms to Treatment Response. Front. Oncol. 2021;11:628359. doi: 10.3389/fonc.2021.628359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 595.Chen Q., Meng Y.-Q., Xu X.-F., Gu J. Blockade of GLUT1 by WZB117 Resensitizes Breast Cancer Cells to Adriamycin. Anticancer Drugs. 2017;28:880–887. doi: 10.1097/CAD.0000000000000529. [DOI] [PubMed] [Google Scholar]
- 596.Ganapathy V., Thangaraju M., Prasad P.D. Nutrient Transporters in Cancer: Relevance to Warburg Hypothesis and beyond. Pharmacol. Ther. 2009;121:29–40. doi: 10.1016/j.pharmthera.2008.09.005. [DOI] [PubMed] [Google Scholar]
- 597.Simcox J.A., Mitchell T.C., Gao Y., Just S.F., Cooksey R., Cox J., Ajioka R., Jones D., Lee S.-H., King D., et al. Dietary Iron Controls Circadian Hepatic Glucose Metabolism through Heme Synthesis. Diabetes. 2015;64:1108–1119. doi: 10.2337/db14-0646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 598.Li Q.-Q., Sun Y.-P., Ruan C.-P., Xu X.-Y., Ge J.-H., He J., Xu Z.-D., Wang Q., Gao W.-C. Cellular Prion Protein Promotes Glucose Uptake through the Fyn-HIF-2α-Glut1 Pathway to Support Colorectal Cancer Cell Survival. Cancer Sci. 2011;102:400–406. doi: 10.1111/j.1349-7006.2010.01811.x. [DOI] [PubMed] [Google Scholar]
- 599.Mukherjee A., Soto C. Prion-Like Protein Aggregates and Type 2 Diabetes. Cold Spring Harb. Perspect. Med. 2017;7:a024315. doi: 10.1101/cshperspect.a024315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 600.Mukherjee S., Dey S.G. Heme Bound Amylin: Spectroscopic Characterization, Reactivity, and Relevance to Type 2 Diabetes. Inorg. Chem. 2013;52:5226–5235. doi: 10.1021/ic4001413. [DOI] [PubMed] [Google Scholar]
- 601.Zraika S., Hull R.L., Udayasankar J., Aston-Mourney K., Subramanian S.L., Kisilevsky R., Szarek W.A., Kahn S.E. Oxidative Stress Is Induced by Islet Amyloid Formation and Time-Dependently Mediates Amyloid-Induced Beta Cell Apoptosis. Diabetologia. 2009;52:626–635. doi: 10.1007/s00125-008-1255-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 602.Koppenol W.H., Stanbury D.M., Bounds P.L. Electrode Potentials of Partially Reduced Oxygen Species, from Dioxygen to Water. Free Radic. Biol. Med. 2010;49:317–322. doi: 10.1016/j.freeradbiomed.2010.04.011. [DOI] [PubMed] [Google Scholar]
- 603.Turrens J.F. Mitochondrial Formation of Reactive Oxygen Species. J. Physiol. 2003;552:335–344. doi: 10.1113/jphysiol.2003.049478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 604.Huang Y., Yang Z., Xu H., Zhang P., Gao Z., Li H. Insulin Enhances the Peroxidase Activity of Heme by Forming Heme-Insulin Complex: Relevance to Type 2 Diabetes Mellitus. Int. J. Biol. Macromol. 2017;102:1009–1015. doi: 10.1016/j.ijbiomac.2017.04.113. [DOI] [PubMed] [Google Scholar]
- 605.Moreno-Navarrete J.M., Rodríguez A., Ortega F., Becerril S., Sabater-Masdeu M., Latorre J., Ricart W., Frühbeck G., Fernández-Real J.M. Increased Adipose Tissue Heme Levels and Exportation Are Associated with Altered Systemic Glucose Metabolism. Sci. Rep. 2017;7:5305. doi: 10.1038/s41598-017-05597-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 606.Sawicki K.T., Chang H.-C., Ardehali H. Role of Heme in Cardiovascular Physiology and Disease. J. Am. Heart Assoc. 2015;4:e001138. doi: 10.1161/JAHA.114.001138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 607.Balla G., Jacob H.S., Eaton J.W., Belcher J.D., Vercellotti G.M. Hemin: A Possible Physiological Mediator of Low Density Lipoprotein Oxidation and Endothelial Injury. Arterioscler. Thromb. 1991;11:1700–1711. doi: 10.1161/01.ATV.11.6.1700. [DOI] [PubMed] [Google Scholar]
- 608.Laird M.D., Wakade C., Alleyne C.H., Jr., Dhandapani K.M. Hemin-Induced Necroptosis Involves Glutathione Depletion in Mouse Astrocytes. Free Radic. Biol. Med. 2008;45:1103–1114. doi: 10.1016/j.freeradbiomed.2008.07.003. [DOI] [PubMed] [Google Scholar]
- 609.Robinson S.R., Dang T.N., Dringen R., Bishop G.M. Hemin Toxicity: A Preventable Source of Brain Damage Following Hemorrhagic Stroke. Redox Rep. 2009;14:228–235. doi: 10.1179/135100009X12525712409931. [DOI] [PubMed] [Google Scholar]
- 610.Harvey J.W., Beutler E. Binding of Heme by Glutathione S-Transferase: A Possible Role of the Erythrocyte Enzyme. Blood. 1982;60:1227–1230. doi: 10.1182/blood.V60.5.1227.1227. [DOI] [PubMed] [Google Scholar]
- 611.Aft R.L., Mueller G.C. Degradation and Covalent Cross-Linking of Glutathione Reductase by Hemin. Life Sci. 1985;36:2153–2161. doi: 10.1016/0024-3205(85)90312-1. [DOI] [PubMed] [Google Scholar]
- 612.Ye W., Zhang L. Heme Controls the Expression of Cell Cycle Regulators and Cell Growth in HeLa Cells. Biochem. Biophys. Res. Commun. 2004;315:546–554. doi: 10.1016/j.bbrc.2004.01.092. [DOI] [PubMed] [Google Scholar]
- 613.Aboelella N.S., Brandle C., Kim T., Ding Z.-C., Zhou G. Oxidative Stress in the Tumor Microenvironment and Its Relevance to Cancer Immunotherapy. Cancers. 2021;13:986. doi: 10.3390/cancers13050986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 614.Tripathi A.K., Singh N. Prion Protein-Hemin Interaction Upregulates Hemoglobin Synthesis: Implications for Cerebral Hemorrhage and Sporadic Creutzfeldt-Jakob Disease. J. Alzheimers Dis. 2016;51:107–121. doi: 10.3233/JAD-151039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 615.Mense S.M., Zhang L. Heme: A Versatile Signaling Molecule Controlling the Activities of Diverse Regulators Ranging from Transcription Factors to MAP Kinases. Cell Res. 2006;16:681–692. doi: 10.1038/sj.cr.7310086. [DOI] [PubMed] [Google Scholar]
- 616.Padmanaban G., Venkateswar V., Rangarajan P.N. Haem as a Multifunctional Regulator. Trends Biochem. Sci. 1989;14:492–496. doi: 10.1016/0968-0004(89)90182-5. [DOI] [PubMed] [Google Scholar]
- 617.Zhu Y., Hon T., Zhang L. Heme Initiates Changes in the Expression of a Wide Array of Genes during the Early Erythroid Differentiation Stage. Biochem. Biophys. Res. Commun. 1999;258:87–93. doi: 10.1006/bbrc.1999.0586. [DOI] [PubMed] [Google Scholar]
- 618.Ulianov S.V., Galitsyna A.A., Flyamer I.M., Golov A.K., Khrameeva E.E., Imakaev M.V., Abdennur N.A., Gelfand M.S., Gavrilov A.A., Razin S.V. Activation of the Alpha-Globin Gene Expression Correlates with Dramatic Upregulation of Nearby Non-Globin Genes and Changes in Local and Large-Scale Chromatin Spatial Structure. Epigenetics Chromatin. 2017;10:35. doi: 10.1186/s13072-017-0142-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 619.Liao R., Zheng Y., Liu X., Zhang Y., Seim G., Tanimura N., Wilson G.M., Hematti P., Coon J.J., Fan J., et al. Discovering How Heme Controls Genome Function Through Heme-Omics. Cell Rep. 2020;31:107832. doi: 10.1016/j.celrep.2020.107832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 620.Caughey W.S., Raymond L.D., Horiuchi M., Caughey B. Inhibition of Protease-Resistant Prion Protein Formation by Porphyrins and Phthalocyanines. Proc. Natl. Acad. Sci. USA. 1998;95:12117–12122. doi: 10.1073/pnas.95.21.12117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 621.Sadrzadeh S.M., Graf E., Panter S.S., Hallaway P.E., Eaton J.W. Hemoglobin. A Biologic Fenton Reagent. J. Biol. Chem. 1984;259:14354–14356. doi: 10.1016/S0021-9258(17)42604-4. [DOI] [PubMed] [Google Scholar]
- 622.Richards R.S., Roberts T.K., Dunstan R.H., McGregor N.R., Butt H.L. Erythrocyte Antioxidant Systems Protect Cultured Endothelial Cells against Oxidant Damage. Biochem. Mol. Biol. Int. 1998;46:857–865. doi: 10.1080/15216549800204402. [DOI] [PubMed] [Google Scholar]
- 623.Rifkind J.M., Nagababu E. Hemoglobin Redox Reactions and Red Blood Cell Aging. Antioxid. Redox Signal. 2013;18:2274–2283. doi: 10.1089/ars.2012.4867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 624.Franco R., Navarro G., Martínez-Pinilla E. Antioxidant Defense Mechanisms in Erythrocytes and in the Central Nervous System. Antioxidants. 2019;8:46. doi: 10.3390/antiox8020046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 625.Mansouri A., Perry C.A. Hemoglobin Autoxidation at Physiological Concentrations. Hemoglobin. 1987;11:353–371. doi: 10.3109/03630268709042854. [DOI] [PubMed] [Google Scholar]
- 626.Kanias T., Acker J.P. Biopreservation of Red Blood Cells—The Struggle with Hemoglobin Oxidation. FEBS J. 2010;277:343–356. doi: 10.1111/j.1742-4658.2009.07472.x. [DOI] [PubMed] [Google Scholar]
- 627.Winterbourn C.C. Free-Radical Production and Oxidative Reactions of Hemoglobin. Environ. Health Perspect. 1985;64:321–330. doi: 10.1289/ehp.8564321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 628.Kassa T., Jana S., Meng F., Alayash A.I. Differential Heme Release from Various Hemoglobin Redox States and the Upregulation of Cellular Heme Oxygenase-1. FEBS Open Bio. 2016;6:876–884. doi: 10.1002/2211-5463.12103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 629.Hultquist D.E., Passon P.G. Catalysis of Methaemoglobin Reduction by Erythrocyte Cytochrome B5 and Cytochrome B5 Reductase. Nat. New Biol. 1971;229:252–254. doi: 10.1038/newbio229252a0. [DOI] [PubMed] [Google Scholar]
- 630.Siendones E., SantaCruz-Calvo S., Martín-Montalvo A., Cascajo M.V., Ariza J., López-Lluch G., Villalba J.M., Acquaviva-Bourdain C., Roze E., Bernier M., et al. Membrane-Bound CYB5R3 Is a Common Effector of Nutritional and Oxidative Stress Response through FOXO3a and Nrf2. Antioxid. Redox Signal. 2014;21:1708–1725. doi: 10.1089/ars.2013.5479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 631.Bulbarelli A., Valentini A., DeSilvestris M., Cappellini M.D., Borgese N. An Erythroid-Specific Transcript Generates the Soluble Form of NADH-Cytochrome b5 Reductase in Humans. Blood. 1998;92:310–319. doi: 10.1182/blood.V92.1.310.413k24_310_319. [DOI] [PubMed] [Google Scholar]
- 632.Passon P.G., Hultquist D.E. Soluble Cytochrome B 5 Reductase from Human Erythrocytes. Biochim. Biophys. Acta. 1972;275:62–73. doi: 10.1016/0005-2728(72)90024-2. [DOI] [PubMed] [Google Scholar]
- 633.Choury D., Leroux A., Kaplan J.C. Membrane-Bound Cytochrome b5 Reductase (methemoglobin Reductase) in Human Erythrocytes. Study in Normal and Methemoglobinemic Subjects. J. Clin. Investig. 1981;67:149–155. doi: 10.1172/JCI110007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 634.Borgese N., Pietrini G., Gaetani S. Concentration of NADH-Cytochrome b5 Reductase in Erythrocytes of Normal and Methemoglobinemic Individuals Measured with a Quantitative Radioimmunoblotting Assay. J. Clin. Investig. 1987;80:1296–1302. doi: 10.1172/JCI113205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 635.Samhan-Arias A.K., Garcia-Bereguiain M.A., Martin-Romero F.J., Gutierrez-Merino C. Clustering of Plasma Membrane-Bound Cytochrome b5 Reductase within “Lipid Raft” Microdomains of the Neuronal Plasma Membrane. Mol. Cell. Neurosci. 2009;40:14–26. doi: 10.1016/j.mcn.2008.08.013. [DOI] [PubMed] [Google Scholar]
- 636.Ito A., Hayashi S., Yoshida T. Participation of a Cytochrome b5-like Hemoprotein of Outer Mitochondrial Membrane (OM Cytochrome B) in NADH-Semidehydroascorbic Acid Reductase Activity of Rat Liver. Biochem. Biophys. Res. Commun. 1981;101:591–598. doi: 10.1016/0006-291X(81)91300-0. [DOI] [PubMed] [Google Scholar]
- 637.Fiaschi T., Chiarugi P. Oxidative Stress, Tumor Microenvironment, and Metabolic Reprogramming: A Diabolic Liaison. Int. J. Cell Biol. 2012;2012:762825. doi: 10.1155/2012/762825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 638.Ogasawara Y., Funakoshi M., Ishii K. Glucose Metabolism Is Accelerated by Exposure to T-Butylhydroperoxide during NADH Consumption in Human Erythrocytes. Blood Cells Mol. Dis. 2008;41:237–243. doi: 10.1016/j.bcmd.2008.05.007. [DOI] [PubMed] [Google Scholar]
- 639.Crespi F., Ratti E., Trist D.G. Melatonin, a Hormone Monitorable in Vivo by Voltammetry? Analyst. 1994;119:2193–2197. doi: 10.1039/an9941902193. [DOI] [PubMed] [Google Scholar]
- 640.Koppenol W.H., Liebman J.F. The Oxidizing Nature of the Hydroxyl Radical. A Comparison with the Ferryl Ion (FeO2+) J. Phys. Chem. 1984;88:99–101. doi: 10.1021/j150645a024. [DOI] [Google Scholar]
- 641.Tesoriere L., D’Arpa D., Conti S., Giaccone V., Pintaudi A.M., Livrea M.A. Melatonin Protects Human Red Blood Cells from Oxidative Hemolysis: New Insights into the Radical-Scavenging Activity. J. Pineal Res. 1999;27:95–105. doi: 10.1111/j.1600-079X.1999.tb00602.x. [DOI] [PubMed] [Google Scholar]
- 642.Tan D.-X., Manchester L.C., Sainz R.M., Mayo J.C., Leon J., Hardeland R., Poeggeler B., Reiter R.J. Interactions between Melatonin and Nicotinamide Nucleotide: NADH Preservation in Cells and in Cell-Free Systems by Melatonin. J. Pineal Res. 2005;39:185–194. doi: 10.1111/j.1600-079X.2005.00234.x. [DOI] [PubMed] [Google Scholar]
- 643.Hardeland R., Reiter R.J., Poeggeler B., Tan D.X. The Significance of the Metabolism of the Neurohormone Melatonin: Antioxidative Protection and Formation of Bioactive Substances. Neurosci. Biobehav. Rev. 1993;17:347–357. doi: 10.1016/S0149-7634(05)80016-8. [DOI] [PubMed] [Google Scholar]
- 644.Martinez G.R., Almeida E.A., Klitzke C.F., Onuki J., Prado F.M., Medeiros M.H.G., Di Mascio P. Measurement of Melatonin and Its Metabolites: Importance for the Evaluation of Their Biological Roles. Endocrine. 2005;27:111–118. doi: 10.1385/ENDO:27:2:111. [DOI] [PubMed] [Google Scholar]
- 645.Morabito R., Remigante A., Marino A. Melatonin Protects Band 3 Protein in Human Erythrocytes against H2O2-Induced Oxidative Stress. Molecules. 2019;24:2741. doi: 10.3390/molecules24152741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 646.Morabito R., Romano O., La Spada G., Marino A. H2O2-Induced Oxidative Stress Affects SO4= Transport in Human Erythrocytes. PLoS ONE. 2016;11:e0146485. doi: 10.1371/journal.pone.0146485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 647.Han Y.S., Kim S.M., Lee J.H., Lee S.H. Co-Administration of Melatonin Effectively Enhances the Therapeutic Effects of Pioglitazone on Mesenchymal Stem Cells Undergoing Indoxyl Sulfate-Induced Senescence through Modulation of Cellular Prion Protein Expression. Int. J. Mol. Sci. 2018;19:367. doi: 10.3390/ijms19051367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 648.Han Y.-S., Yoon Y.M., Go G., Lee J.H., Lee S.H. Melatonin Protects Human Renal Proximal Tubule Epithelial Cells Against High Glucose-Mediated Fibrosis via the Cellular Prion Protein-TGF-β-Smad Signaling Axis. Int. J. Med. Sci. 2020;17:1235–1245. doi: 10.7150/ijms.42603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 649.Alvarez-Artime A., Cernuda-Cernuda R., Artime-Naveda F., Cepas V., Gonzalez-Menendez P., Fernadez-Vega S., Quiros-Gonzalez I., Sainz R.M., Mayo J.C. Melatonin-Induced Cytoskeleton Reorganization Leads to Inhibition of Melanoma Cancer Cell Proliferation. Int. J. Mol. Sci. 2020;21:548. doi: 10.3390/ijms21020548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 650.Jing X., Yang F., Shao C., Wei K., Xie M., Shen H., Shu Y. Role of Hypoxia in Cancer Therapy by Regulating the Tumor Microenvironment. Mol. Cancer. 2019;18:157. doi: 10.1186/s12943-019-1089-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 651.Roma-Rodrigues C., Mendes R., Baptista P.V., Fernandes A.R. Targeting Tumor Microenvironment for Cancer Therapy. Int. J. Mol. Sci. 2019;20:840. doi: 10.3390/ijms20040840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 652.Milane L., Duan Z., Amiji M. Role of Hypoxia and Glycolysis in the Development of Multi-Drug Resistance in Human Tumor Cells and the Establishment of an Orthotopic Multi-Drug Resistant Tumor Model in Nude Mice Using Hypoxic Pre-Conditioning. Cancer Cell Int. 2011;11:3. doi: 10.1186/1475-2867-11-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 653.Pourhasanzade F., Sabzpoushan S.H. A New Mathematical Model for Controlling Tumor Growth Based on Microenvironment Acidity and Oxygen Concentration. Biomed. Res. Int. 2021;2021:8886050. doi: 10.1155/2021/8886050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 654.Mu Q., Najafi M. Modulation of the Tumor Microenvironment (TME) by Melatonin. Eur. J. Pharmacol. 2021;907:174365. doi: 10.1016/j.ejphar.2021.174365. [DOI] [PubMed] [Google Scholar]
- 655.Emami Nejad A., Najafgholian S., Rostami A., Sistani A., Shojaeifar S., Esparvarinha M., Nedaeinia R., Haghjooy Javanmard S., Taherian M., Ahmadlou M., et al. The Role of Hypoxia in the Tumor Microenvironment and Development of Cancer Stem Cell: A Novel Approach to Developing Treatment. Cancer Cell Int. 2021;21:62. doi: 10.1186/s12935-020-01719-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 656.Bastani S., Akbarzadeh M., Rastgar Rezaei Y., Farzane A., Nouri M., Mollapour Sisakht M., Fattahi A., Akbarzadeh M., Reiter R.J. Melatonin as a Therapeutic Agent for the Inhibition of Hypoxia-Induced Tumor Progression: A Description of Possible Mechanisms Involved. Int. J. Mol. Sci. 2021;22:874. doi: 10.3390/ijms221910874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 657.Finger E.C., Giaccia A.J. Hypoxia, Inflammation, and the Tumor Microenvironment in Metastatic Disease. Cancer Metastasis Rev. 2010;29:285–293. doi: 10.1007/s10555-010-9224-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 658.Bristow R.G., Hill R.P. Hypoxia and Metabolism. Hypoxia, DNA Repair and Genetic Instability. Nat. Rev. Cancer. 2008;8:180–192. doi: 10.1038/nrc2344. [DOI] [PubMed] [Google Scholar]
- 659.Vaupel P. The Role of Hypoxia-Induced Factors in Tumor Progression. Oncologist. 2004;9((Suppl. S5)):10–17. doi: 10.1634/theoncologist.9-90005-10. [DOI] [PubMed] [Google Scholar]
- 660.Fuller G.G., Han T., Freeberg M.A., Moresco J.J., Ghanbari Niaki A., Roach N.P., Yates J.R., 3rd, Myong S., Kim J.K. RNA Promotes Phase Separation of Glycolysis Enzymes into Yeast G Bodies in Hypoxia. Elife. 2020;9:e48480. doi: 10.7554/eLife.48480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 661.Jin M., Fuller G.G., Han T., Yao Y., Alessi A.F., Freeberg M.A., Roach N.P., Moresco J.J., Karnovsky A., Baba M., et al. Glycolytic Enzymes Coalesce in G Bodies under Hypoxic Stress. Cell Rep. 2017;20:895–908. doi: 10.1016/j.celrep.2017.06.082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 662.Garai S., Citu, Singla-Pareek S.L., Sopory S.K., Kaur C., Yadav G. Complex Networks of Prion-Like Proteins Reveal Cross Talk Between Stress and Memory Pathways in Plants. Front. Plant. Sci. 2021;12:707286. doi: 10.3389/fpls.2021.707286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 663.Godet I., Mamo M., Thurnheer A., Rosen D.M., Gilkes D.M. Post-Hypoxic Cells Promote Metastatic Recurrence after Chemotherapy Treatment in TNBC. Cancers. 2021;13:5509. doi: 10.3390/cancers13215509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 664.Gomatou G., Syrigos N., Vathiotis I.A., Kotteas E.A. Tumor Dormancy: Implications for Invasion and Metastasis. Int. J. Mol. Sci. 2021;22:4862. doi: 10.3390/ijms22094862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 665.Perego M., Tyurin V.A., Tyurina Y.Y., Yellets J., Nacarelli T., Lin C., Nefedova Y., Kossenkov A., Liu Q., Sreedhar S., et al. Reactivation of Dormant Tumor Cells by Modified Lipids Derived from Stress-Activated Neutrophils. Sci. Transl. Med. 2020;12 doi: 10.1126/scitranslmed.abb5817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 666.van der Kamp M.W., Daggett V. Influence of pH on the Human Prion Protein: Insights into the Early Steps of Misfolding. Biophys. J. 2010;99:2289–2298. doi: 10.1016/j.bpj.2010.07.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 667.Reithmeier R.A.F., Casey J.R., Kalli A.C., Sansom M.S.P., Alguel Y., Iwata S. Band 3, the Human Red Cell Chloride/bicarbonate Anion Exchanger (AE1, SLC4A1), in a Structural Context. Pt ABiochim. Biophys. Acta. 2016;1858:1507–1532. doi: 10.1016/j.bbamem.2016.03.030. [DOI] [PubMed] [Google Scholar]
- 668.Pushkin A., Kurtz I. SLC4 Base (HCO3−, CO32−) Transporters: Classification, Function, Structure, Genetic Diseases, and Knockout Models. Am. J. Physiol -Ren. Physiol. 2006;290:F580–F599. doi: 10.1152/ajprenal.00252.2005. [DOI] [PubMed] [Google Scholar]
- 669.Passow H. Reviews of Physiology, Biochemistry and Pharmacology. Volume 103. Springer; Berlin/Heidelberg, Germany: 1986. Molecular Aspects of Band 3 Protein-Mediated Anion Transport across the Red Blood Cell Membrane; pp. 61–203. [DOI] [PubMed] [Google Scholar]
- 670.Rivera-Santiago R., Harper S.L., Sriswasdi S., Hembach P., Speicher D.W. Full-Length Anion Exchanger 1 Structure and Interactions with Ankyrin-1 Determined by Zero Length Crosslinking of Erythrocyte Membranes. Structure. 2017;25:132–145. doi: 10.1016/j.str.2016.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 671.Li H., Lykotrafitis G. Erythrocyte Membrane Model with Explicit Description of the Lipid Bilayer and the Spectrin Network. Biophys. J. 2014;107:642–653. doi: 10.1016/j.bpj.2014.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 672.Grey J.L., Kodippili G.C., Simon K., Low P.S. Identification of Contact Sites between Ankyrin and Band 3 in the Human Erythrocyte Membrane. Biochemistry. 2012;51:6838–6846. doi: 10.1021/bi300693k. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 673.Hamasaki N. The Role of Band 3 Protein in Oxygen Delivery by Red Blood Cells. Indian, J. Clin. Biochem. 1999;14:49–58. doi: 10.1007/BF02869151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 674.van den Akker E., Satchwell T.J., Williamson R.C., Toye A.M. Band 3 Multiprotein Complexes in the Red Cell Membrane; of Mice and Men. Blood Cells Mol. Dis. 2010;45:1–8. doi: 10.1016/j.bcmd.2010.02.019. [DOI] [PubMed] [Google Scholar]
- 675.Sleep J., Wilson D., Simmons R., Gratzer W. Elasticity of the Red Cell Membrane and Its Relation to Hemolytic Disorders: An Optical Tweezers Study. Biophys. J. 1999;77:3085–3095. doi: 10.1016/S0006-3495(99)77139-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 676.Xu Z., Dou W., Wang C., Sun Y. Stiffness and ATP Recovery of Stored Red Blood Cells in Serum. Microsyst Nanoeng. 2019;5:51. doi: 10.1038/s41378-019-0097-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 677.Huisjes R., Bogdanova A., van Solinge W.W., Schiffelers R.M., Kaestner L., van Wijk R. Squeezing for Life-Properties of Red Blood Cell Deformability. Front. Physiol. 2018;9:656. doi: 10.3389/fphys.2018.00656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 678.Baier D., Müller T., Mohr T., Windberger U. Red Blood Cell Stiffness and Adhesion Are Species-Specific Properties Strongly Affected by Temperature and Medium Changes in Single Cell Force Spectroscopy. Molecules. 2021;26:2771. doi: 10.3390/molecules26092771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 679.de Oliveira S., Saldanha C. An Overview about Erythrocyte Membrane. Clin. Hemorheol. Microcirc. 2010;44:63–74. doi: 10.3233/CH-2010-1253. [DOI] [PubMed] [Google Scholar]
- 680.Cabrales P. Effects of Erythrocyte Flexibility on Microvascular Perfusion and Oxygenation during Acute Anemia. Am. J. Physiol. Heart Circ. Physiol. 2007;293:H1206–H1215. doi: 10.1152/ajpheart.00109.2007. [DOI] [PubMed] [Google Scholar]
- 681.Chien S. Red Cell Deformability and Its Relevance to Blood Flow. Annu. Rev. Physiol. 1987;49:177–192. doi: 10.1146/annurev.ph.49.030187.001141. [DOI] [PubMed] [Google Scholar]
- 682.Fraser G.M., Dias G.M., Goldman D., Ellis C. Red Blood Cell Flux in Isolated Capillary Bifurcations. FASEB J. 2009;23:949.5. doi: 10.1096/fasebj.23.1_supplement.949.5. [DOI] [Google Scholar]
- 683.Kimura H., Braun R.D., Ong E.T., Hsu R., Secomb T.W., Papahadjopoulos D., Hong K., Dewhirst M.W. Fluctuations in Red Cell Flux in Tumor Microvessels Can Lead to Transient Hypoxia and Reoxygenation in Tumor Parenchyma. Cancer Res. 1996;56:5522–5528. [PubMed] [Google Scholar]
- 684.Mohanty J.G., Nagababu E., Rifkind J.M. Red Blood Cell Oxidative Stress Impairs Oxygen Delivery and Induces Red Blood Cell Aging. Front. Physiol. 2014;5:84. doi: 10.3389/fphys.2014.00084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 685.Çimen M.Y.B. Free Radical Metabolism in Human Erythrocytes. Clin. Chim. Acta. 2008;390:1–11. doi: 10.1016/j.cca.2007.12.025. [DOI] [PubMed] [Google Scholar]
- 686.Barodka V.M., Nagababu E., Mohanty J.G., Nyhan D., Berkowitz D.E., Rifkind J.M., Strouse J.J. New Insights Provided by a Comparison of Impaired Deformability with Erythrocyte Oxidative Stress for Sickle Cell Disease. Blood Cells Mol. Dis. 2014;52:230–235. doi: 10.1016/j.bcmd.2013.10.004. [DOI] [PubMed] [Google Scholar]
- 687.Wang Q., Zennadi R. The Role of RBC Oxidative Stress in Sickle Cell Disease: From the Molecular Basis to Pathologic Implications. Antioxidants. 2021;10:1608. doi: 10.3390/antiox10101608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 688.Fertrin K.Y., Costa F.F. Genomic Polymorphisms in Sickle Cell Disease: Implications for Clinical Diversity and Treatment. Expert Rev. Hematol. 2010;3:443–458. doi: 10.1586/ehm.10.44. [DOI] [PubMed] [Google Scholar]
- 689.Bunn H.F. Pathogenesis and Treatment of Sickle Cell Disease. N. Engl. J. Med. 1997;337:762–769. doi: 10.1056/NEJM199709113371107. [DOI] [PubMed] [Google Scholar]
- 690.Spector J., Kodippili G.C., Ritchie K., Low P.S. Single Molecule Studies of the Diffusion of Band 3 in Sickle Cell Erythrocytes. PLoS ONE. 2016;11:e0162514. doi: 10.1371/journal.pone.0162514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 691.Efferth T., Schwarzl S.M., Smith J., Osieka R. Role of Glucose-6-Phosphate Dehydrogenase for Oxidative Stress and Apoptosis. Cell Death Differ. 2006;13:527–528. doi: 10.1038/sj.cdd.4401807. [DOI] [PubMed] [Google Scholar]
- 692.Aziz H., Mohiuddin S.S. StatPearls. StatPearls Publishing; Treasure Island, FL, USA: 2021. Biochemistry, Hexose Monophosphate Pathway. [PubMed] [Google Scholar]
- 693.van Zwieten R., Verhoeven A.J., Roos D. Inborn Defects in the Antioxidant Systems of Human Red Blood Cells. Free Radic. Biol. Med. 2014;67:377–386. doi: 10.1016/j.freeradbiomed.2013.11.022. [DOI] [PubMed] [Google Scholar]
- 694.Davidson W.D., Tanaka K.R. Factors Affecting Pentose Phosphate Pathway Activity in Human Red Cells. Br. J. Haematol. 1972;23:371–385. doi: 10.1111/j.1365-2141.1972.tb08884.x. [DOI] [PubMed] [Google Scholar]
- 695.Omachi A., Scott C.B., Parry T.E. Influence of Glycolysis on NADH Content in Human Erythrocytes. Am. J. Physiol. 1969;216:527–530. doi: 10.1152/ajplegacy.1969.216.3.527. [DOI] [PubMed] [Google Scholar]
- 696.Rapoprot I., Berger H., Rapoport S.M., Elsner R., Gerber G. Response of the Glycolysis of Human Erythrocytes to the Transition from the Oxygenated to the Deoxygenated State at Constant Intracellular pH. Biochim. Biophys. Acta. 1976;428:193–204. doi: 10.1016/0304-4165(76)90120-3. [DOI] [PubMed] [Google Scholar]
- 697.Stefanovic M., Puchulu-Campanella E., Kodippili G., Low P.S. Oxygen Regulates the Band 3-Ankyrin Bridge in the Human Erythrocyte Membrane. Biochem. J. 2013;449:143–150. doi: 10.1042/BJ20120869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 698.Grygorczyk R., Orlov S.N. Effects of Hypoxia on Erythrocyte Membrane Properties-Implications for Intravascular Hemolysis and Purinergic Control of Blood Flow. Front. Physiol. 2017;8:1110. doi: 10.3389/fphys.2017.01110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 699.Anong W.A., Weis T.L., Low P.S. Rate of Rupture and Reattachment of the Band 3-Ankyrin Bridge on the Human Erythrocyte Membrane. J. Biol. Chem. 2006;281:22360–22366. doi: 10.1074/jbc.M513839200. [DOI] [PubMed] [Google Scholar]
- 700.Low P.S., Allen D.P., Zioncheck T.F., Chari P., Willardson B.M., Geahlen R.L., Harrison M.L. Tyrosine Phosphorylation of Band 3 Inhibits Peripheral Protein Binding. J. Biol. Chem. 1987;262:4592–4596. doi: 10.1016/S0021-9258(18)61234-7. [DOI] [PubMed] [Google Scholar]
- 701.Lewis I.A., Campanella M.E., Markley J.L., Low P.S. Role of Band 3 in Regulating Metabolic Flux of Red Blood Cells. Proc. Natl. Acad. Sci. USA. 2009;106:18515–18520. doi: 10.1073/pnas.0905999106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 702.Campanella M.E., Chu H., Wandersee N.J., Peters L.L., Mohandas N., Gilligan D.M., Low P.S. Characterization of Glycolytic Enzyme Interactions with Murine Erythrocyte Membranes in Wild-Type and Membrane Protein Knockout Mice. Blood. 2008;112:3900–3906. doi: 10.1182/blood-2008-03-146159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 703.Pantaleo A., Ferru E., Pau M.C., Khadjavi A., Mandili G., Mattè A., Spano A., De Franceschi L., Pippia P., Turrini F. Band 3 Erythrocyte Membrane Protein Acts as Redox Stress Sensor Leading to Its Phosphorylation by P (72) Syk. Oxid. Med. Cell. Longev. 2016;2016:6051093. doi: 10.1155/2016/6051093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 704.Ferru E., Giger K., Pantaleo A., Campanella E., Grey J., Ritchie K., Vono R., Turrini F., Low P.S. Regulation of Membrane-Cytoskeletal Interactions by Tyrosine Phosphorylation of Erythrocyte Band 3. Blood. 2011;117:5998–6006. doi: 10.1182/blood-2010-11-317024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 705.Pantaleo A., Ferru E., Giribaldi G., Mannu F., Carta F., Matte A., de Franceschi L., Turrini F. Oxidized and Poorly Glycosylated Band 3 Is Selectively Phosphorylated by Syk Kinase to Form Large Membrane Clusters in Normal and G6PD-Deficient Red Blood Cells. Biochem. J. 2009;418:359–367. doi: 10.1042/BJ20081557. [DOI] [PubMed] [Google Scholar]
- 706.Jarolim P., Lahav M., Liu S.C., Palek J. Effect of Hemoglobin Oxidation Products on the Stability of Red Cell Membrane Skeletons and the Associations of Skeletal Proteins: Correlation with a Release of Hemin. Blood. 1990;76:2125–2131. doi: 10.1182/blood.V76.10.2125.2125. [DOI] [PubMed] [Google Scholar]
- 707.Liu S.C., Zhai S., Lawler J., Palek J. Hemin-Mediated Dissociation of Erythrocyte Membrane Skeletal Proteins. J. Biol. Chem. 1985;260:12234–12239. doi: 10.1016/S0021-9258(17)39015-4. [DOI] [PubMed] [Google Scholar]
- 708.An X.L., Takakuwa Y., Nunomura W., Manno S., Mohandas N. Modulation of Band 3-Ankyrin Interaction by Protein 4.1. Functional Implications in Regulation of Erythrocyte Membrane Mechanical Properties. J. Biol. Chem. 1996;271:33187–33191. doi: 10.1074/jbc.271.52.33187. [DOI] [PubMed] [Google Scholar]
- 709.Schmitt T.H., Frezzatti W.A., Jr., Schreier S. Hemin-Induced Lipid Membrane Disorder and Increased Permeability: A Molecular Model for the Mechanism of Cell Lysis. Arch. Biochem. Biophys. 1993;307:96–103. doi: 10.1006/abbi.1993.1566. [DOI] [PubMed] [Google Scholar]
- 710.Ludlow J.T., Wilkerson R.G., Nappe T.M. StatPearls. StatPearls Publishing; Treasure Island, FL, USA: 2021. Methemoglobinemia. [PubMed] [Google Scholar]
- 711.Wright R.O., Lewander W.J., Woolf A.D. Methemoglobinemia: Etiology, Pharmacology, and Clinical Management. Ann. Emerg. Med. 1999;34:646–656. doi: 10.1016/S0196-0644(99)70167-8. [DOI] [PubMed] [Google Scholar]
- 712.Zhang Y., Manning L.R., Falcone J., Platt O., Manning J.M. Human Erythrocyte Membrane Band 3 Protein Influences Hemoglobin Cooperativity: POSSIBLE EFFECT ON OXYGEN TRANSPORT. J. Biol. Chem. 2003;278:39565–39571. doi: 10.1074/jbc.M303352200. [DOI] [PubMed] [Google Scholar]
- 713.Chu H., McKenna M.M., Krump N.A., Zheng S., Mendelsohn L., Thein S.L., Garrett L.J., Bodine D.M., Low P.S. Reversible Binding of Hemoglobin to Band 3 Constitutes the Molecular Switch That Mediates O2 Regulation of Erythrocyte Properties. Blood. 2016;128:2708–2716. doi: 10.1182/blood-2016-01-692079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 714.Walder J.A., Chatterjee R., Steck T.L., Low P.S., Musso G.F., Kaiser E.T., Rogers P.H., Arnone A. The Interaction of Hemoglobin with the Cytoplasmic Domain of Band 3 of the Human Erythrocyte Membrane. J. Biol. Chem. 1984;259:10238–10246. doi: 10.1016/S0021-9258(18)90956-7. [DOI] [PubMed] [Google Scholar]
- 715.Chu H., Breite A., Ciraolo P., Franco R.S., Low P.S. Characterization of the Deoxyhemoglobin Binding Site on Human Erythrocyte Band 3: Implications for O2 Regulation of Erythrocyte Properties. Blood. 2008;111:932–938. doi: 10.1182/blood-2007-07-100180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 716.Stromme J.H., Eldjarn L. The Role of the Pentose Phosphate Pathway in the Reduction of Methaemoglobin in Human Erythrocytes. Biochem. J. 1962;84:406–410. doi: 10.1042/bj0840406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 717.Hlutkin S., Zinchuk V. Effect of Melatonin on the Blood Oxygen Transport during Hypothermia and Rewarming in Rats. Adv. Med. Sci. 2008;53:234–239. doi: 10.2478/v10039-008-0035-7. [DOI] [PubMed] [Google Scholar]
- 718.Ditlev J.A. Membrane-Associated Phase Separation: Organization and Function Emerge from a Two-Dimensional Milieu. J. Mol. Cell Biol. 2021;13:319–324. doi: 10.1093/jmcb/mjab010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 719.Zhang C., Rabouille C. Membrane-Bound Meet Membraneless in Health and Disease. Cells. 2019;8:1000. doi: 10.3390/cells8091000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 720.Vernon R.M., Chong P.A., Tsang B., Kim T.H., Bah A., Farber P., Lin H., Forman-Kay J.D. Pi-Pi Contacts Are an Overlooked Protein Feature Relevant to Phase Separation. Elife. 2018;7:e31486. doi: 10.7554/eLife.31486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 721.Lee I.-H., Imanaka M.Y., Modahl E.H., Torres-Ocampo A.P. Lipid Raft Phase Modulation by Membrane-Anchored Proteins with Inherent Phase Separation Properties. ACS Omega. 2019;4:6551–6559. doi: 10.1021/acsomega.9b00327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 722.Hicks M.R., Gill A.C., Bath I.K., Rullay A.K., Sylvester I.D., Crout D.H., Pinheiro T.J.T. Synthesis and Structural Characterization of a Mimetic Membrane-Anchored Prion Protein. FEBS J. 2006;273:1285–1299. doi: 10.1111/j.1742-4658.2006.05152.x. [DOI] [PubMed] [Google Scholar]
- 723.Zeng F., Watt N.T., Walmsley A.R., Hooper N.M. Tethering the N-Terminus of the Prion Protein Compromises the Cellular Response to Oxidative Stress. J. Neurochem. 2003;84:480–490. doi: 10.1046/j.1471-4159.2003.01529.x. [DOI] [PubMed] [Google Scholar]
- 724.Baron G.S., Caughey B. Effect of Glycosylphosphatidylinositol Anchor-Dependent and -Independent Prion Protein Association with Model Raft Membranes on Conversion to the Protease-Resistant Isoform. J. Biol. Chem. 2003;278:14883–14892. doi: 10.1074/jbc.M210840200. [DOI] [PubMed] [Google Scholar]
- 725.Sanghera N., Pinheiro T.J.T. Binding of Prion Protein to Lipid Membranes and Implications for Prion Conversion. J. Mol. Biol. 2002;315:1241–1256. doi: 10.1006/jmbi.2001.5322. [DOI] [PubMed] [Google Scholar]
- 726.Wang F., Yang F., Hu Y., Wang X., Wang X., Jin C., Ma J. Lipid Interaction Converts Prion Protein to a PrPSc-like Proteinase K-Resistant Conformation under Physiological Conditions. Biochemistry. 2007;46:7045–7053. doi: 10.1021/bi700299h. [DOI] [PubMed] [Google Scholar]
- 727.Chen W., van der Kamp M.W., Daggett V. Structural and Dynamic Properties of the Human Prion Protein. Biophys. J. 2014;106:1152–1163. doi: 10.1016/j.bpj.2013.12.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 728.Kumar J., Sreeramulu S., Schmidt T.L., Richter C., Vonck J., Heckel A., Glaubitz C., Schwalbe H. Prion Protein Amyloid Formation Involves Structural Rearrangements in the C-Terminal Domain. ChemBioChem. 2010;11:1208–1213. doi: 10.1002/cbic.201000076. [DOI] [PubMed] [Google Scholar]
- 729.Thakur A.K., Srivastava A.K., Srinivas V., Chary K.V.R., Rao C.M. Copper Alters Aggregation Behavior of Prion Protein and Induces Novel Interactions between Its N- and C-Terminal Regions. J. Biol. Chem. 2011;286:38533–38545. doi: 10.1074/jbc.M111.265645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 730.Spagnolli G., Rigoli M., Orioli S., Sevillano A.M., Faccioli P., Wille H., Biasini E., Requena J.R. Full Atomistic Model of Prion Structure and Conversion. PLoS Pathog. 2019;15:e1007864. doi: 10.1371/journal.ppat.1007864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 731.Kabani M., Cosnier B., Bousset L., Rousset J.-P., Melki R., Fabret C. A Mutation within the C-Terminal Domain of Sup35p That Affects [PSI+] Prion Propagation. Mol. Microbiol. 2011;81:640–658. doi: 10.1111/j.1365-2958.2011.07719.x. [DOI] [PubMed] [Google Scholar]
- 732.Zanusso G., Petersen R.B., Jin T., Jing Y., Kanoush R., Ferrari S., Gambetti P., Singh N. Proteasomal Degradation and N-Terminal Protease Resistance of the Codon 145 Mutant Prion Protein. J. Biol. Chem. 1999;274:23396–23404. doi: 10.1074/jbc.274.33.23396. [DOI] [PubMed] [Google Scholar]
- 733.Westergard L., Turnbaugh J.A., Harris D.A. A Naturally Occurring C-Terminal Fragment of the Prion Protein (PrP) Delays Disease and Acts as a Dominant-Negative Inhibitor of PrPSc Formation. J. Biol. Chem. 2011;286:44234–44242. doi: 10.1074/jbc.M111.286195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 734.McLennan N.F., Brennan P.M., McNeill A., Davies I., Fotheringham A., Rennison K.A., Ritchie D., Brannan F., Head M.W., Ironside J.W., et al. Prion Protein Accumulation and Neuroprotection in Hypoxic Brain Damage. Am. J. Pathol. 2004;165:227–235. doi: 10.1016/S0002-9440(10)63291-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 735.Shyu W.-C., Lin S.-Z., Chiang M.-F., Ding D.-C., Li K.-W., Chen S.-F., Yang H.-I., Li H. Overexpression of PrPC by Adenovirus-Mediated Gene Targeting Reduces Ischemic Injury in a Stroke Rat Model. J. Neurosci. 2005;25:8967–8977. doi: 10.1523/JNEUROSCI.1115-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 736.Spudich A., Frigg R., Kilic E., Kilic U., Oesch B., Raeber A., Bassetti C.L., Hermann D.M. Aggravation of Ischemic Brain Injury by Prion Protein Deficiency: Role of ERK-1/-2 and STAT-1. Neurobiol. Dis. 2005;20:442–449. doi: 10.1016/j.nbd.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 737.Weise J., Sandau R., Schwarting S., Crome O., Wrede A., Schulz-Schaeffer W., Zerr I., Bähr M. Deletion of Cellular Prion Protein Results in Reduced Akt Activation, Enhanced Postischemic Caspase-3 Activation, and Exacerbation of Ischemic Brain Injury. Stroke. 2006;37:1296–1300. doi: 10.1161/01.STR.0000217262.03192.d4. [DOI] [PubMed] [Google Scholar]
- 738.Vriend J., Reiter R.J. Breast Cancer Cells: Modulation by Melatonin and the Ubiquitin-Proteasome System—A Review. Mol. Cell. Endocrinol. 2015;417:1–9. doi: 10.1016/j.mce.2015.09.001. [DOI] [PubMed] [Google Scholar]
- 739.Song J., Ma S.-J., Luo J.-H., Zhang H., Wang R.-X., Liu H., Li L., Zhang Z.-G., Zhou R.-X. Melatonin Induces the Apoptosis and Inhibits the Proliferation of Human Gastric Cancer Cells via Blockade of the AKT/MDM2 Pathway. Oncol. Rep. 2018;39:1975–1983. doi: 10.3892/or.2018.6282. [DOI] [PubMed] [Google Scholar]
- 740.Wang Y., Zeng S. Melatonin Promotes Ubiquitination of Phosphorylated Pro-Apoptotic Protein Bcl-2-Interacting Mediator of Cell Death-Extra Long (BimEL) in Porcine Granulosa Cells. Int. J. Mol. Sci. 2018;19:3431. doi: 10.3390/ijms19113431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 741.Armstrong C.L., Marquardt D., Dies H., Kučerka N., Yamani Z., Harroun T.A., Katsaras J., Shi A.-C., Rheinstädter M.C. The Observation of Highly Ordered Domains in Membranes with Cholesterol. PLoS ONE. 2013;8:e66162. doi: 10.1371/journal.pone.0066162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 742.Almeida P.F.F., Pokorny A., Hinderliter A. Thermodynamics of Membrane Domains. Biochim. Biophys. Acta. 2005;1720:1–13. doi: 10.1016/j.bbamem.2005.12.004. [DOI] [PubMed] [Google Scholar]
- 743.Simons K., Toomre D. Lipid Rafts and Signal Transduction. Nat. Rev. Mol. Cell Biol. 2000;1:31–39. doi: 10.1038/35036052. [DOI] [PubMed] [Google Scholar]
- 744.Bagnat M., Keränen S., Shevchenko A., Shevchenko A., Simons K. Lipid Rafts Function in Biosynthetic Delivery of Proteins to the Cell Surface in Yeast. Proc. Natl. Acad. Sci. USA. 2000;97:3254–3259. doi: 10.1073/pnas.97.7.3254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 745.Ikonen E. Roles of Lipid Rafts in Membrane Transport. Curr. Opin. Cell Biol. 2001;13:470–477. doi: 10.1016/S0955-0674(00)00238-6. [DOI] [PubMed] [Google Scholar]
- 746.Preta G. New Insights Into Targeting Membrane Lipids for Cancer Therapy. Front. Cell Dev. Biol. 2020;8:571237. doi: 10.3389/fcell.2020.571237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 747.Greenlee J.D., Subramanian T., Liu K., King M.R. Rafting Down the Metastatic Cascade: The Role of Lipid Rafts in Cancer Metastasis, Cell Death, and Clinical Outcomes. Cancer Res. 2021;81:5–17. doi: 10.1158/0008-5472.CAN-20-2199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 748.Codini M., Garcia-Gil M., Albi E. Cholesterol and Sphingolipid Enriched Lipid Rafts as Therapeutic Targets in Cancer. Int. J. Mol. Sci. 2021;22:726. doi: 10.3390/ijms22020726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 749.Gomà A., Mir R., Martínez-Soler F., Tortosa A., Vidal A., Condom E., Pérez-Tomás R., Giménez-Bonafé P. Multidrug Resistance Protein 1 Localization in Lipid Raft Domains and Prostasomes in Prostate Cancer Cell Lines. Onco. Targets. Ther. 2014;7:2215–2225. doi: 10.2147/OTT.S69530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 750.Ye D.M., Ye S.C., Yu S.Q., Shu F.F., Xu S.S., Chen Q.Q., Wang Y.L., Tang Z.T., Pan C. Drug-Resistance Reversal in Colorectal Cancer Cells by Destruction of Flotillins, the Key Lipid Rafts Proteins. Neoplasma. 2019;66:576–583. doi: 10.4149/neo_2018_180820N633. [DOI] [PubMed] [Google Scholar]
- 751.Taylor D.R., Whitehouse I.J., Hooper N.M. Glypican-1 Mediates Both Prion Protein Lipid Raft Association and Disease Isoform Formation. PLoS Pathog. 2009;5:e1000666. doi: 10.1371/journal.ppat.1000666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 752.Fremuntova Z., Mosko T., Soukup J., Kucerova J., Kostelanska M., Hanusova Z.B., Filipova M., Cervenakova L., Holada K. Changes in Cellular Prion Protein Expression, Processing and Localisation during Differentiation of the Neuronal Cell Line CAD 5. Biol. Cell. 2020;112:1–21. doi: 10.1111/boc.201900045. [DOI] [PubMed] [Google Scholar]
- 753.Martellucci S., Santacroce C., Santilli F., Piccoli L., Delle Monache S., Angelucci A., Misasi R., Sorice M., Mattei V. Cellular and Molecular Mechanisms Mediated by recPrPC Involved in the Neuronal Differentiation Process of Mesenchymal Stem Cells. Int. J. Mol. Sci. 2019;20:345. doi: 10.3390/ijms20020345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 754.Nieznanski K. Interactions of Prion Protein with Intracellular Proteins: So Many Partners and No Consequences? Cell. Mol. Neurobiol. 2010;30:653–666. doi: 10.1007/s10571-009-9491-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 755.Kourie J.I. Mechanisms of Prion-Induced Modifications in Membrane Transport Properties: Implications for Signal Transduction and Neurotoxicity. Chem. Biol. Interact. 2001;138:1–26. doi: 10.1016/S0009-2797(01)00228-9. [DOI] [PubMed] [Google Scholar]
- 756.Singh N., Gu Y., Bose S., Kalepu S., Mishra R.S., Verghese S. Prion Peptide 106-126 as a Model for Prion Replication and Neurotoxicity. Front. Biosci. 2002;7:a60–a71. doi: 10.2741/A740. [DOI] [PubMed] [Google Scholar]
- 757.Forloni G., Chiesa R., Bugiani O., Salmona M., Tagliavini F. Review: PrP 106-126-25 Years after. Neuropathol. Appl. Neurobiol. 2019;45:430–440. doi: 10.1111/nan.12538. [DOI] [PubMed] [Google Scholar]
- 758.Salmona M., Forloni G., Diomede L., Algeri M., De Gioia L., Angeretti N., Giaccone G., Tagliavini F., Bugiani O. A Neurotoxic and Gliotrophic Fragment of the Prion Protein Increases Plasma Membrane Microviscosity. Neurobiol. Dis. 1997;4:47–57. doi: 10.1006/nbdi.1997.0133. [DOI] [PubMed] [Google Scholar]
- 759.Lin M.C., Mirzabekov T., Kagan B.L. Channel Formation by a Neurotoxic Prion Protein Fragment. J. Biol. Chem. 1997;272:44–47. doi: 10.1074/jbc.272.1.44. [DOI] [PubMed] [Google Scholar]
- 760.Kourie J.I., Culverson A. Prion Peptide Fragment PrP[106–126] Forms Distinct Cation Channel Types. J. Neurosci. Res. 2000;62:120–133. doi: 10.1002/1097-4547(20001001)62:1<120::AID-JNR13>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- 761.Kourie J.I., Shorthouse A.A. Properties of Cytotoxic Peptide-Formed Ion Channels. Am. J. Physiol. Cell Physiol. 2000;278:C1063–C1087. doi: 10.1152/ajpcell.2000.278.6.C1063. [DOI] [PubMed] [Google Scholar]
- 762.DeArmond S.J., Qiu Y., Wong K., Nixon R., Hyun W., Prusiner S.B., Mobley W.C. Abnormal Plasma Membrane Properties and Functions in Prion-Infected Cell Lines. Cold Spring Harb. Symp. Quant. Biol. 1996;61:531–540. [PubMed] [Google Scholar]
- 763.Wong K., Qiu Y., Hyun W., Nixon R., VanCleff J., Sanchez-Salazar J., Prusiner S.B., DeArmond S.J. Decreased Receptor-Mediated Calcium Response in Prion-Infected Cells Correlates with Decreased Membrane Fluidity and IP3 Release. Neurology. 1996;47:741–750. doi: 10.1212/WNL.47.3.741. [DOI] [PubMed] [Google Scholar]
- 764.Pan J., Sahoo P.K., Dalzini A., Hayati Z., Aryal C.M., Teng P., Cai J., Rodriguez Gutierrez H., Song L. Membrane Disruption Mechanism of a Prion Peptide (106-126) Investigated by Atomic Force Microscopy, Raman and Electron Paramagnetic Resonance Spectroscopy. J. Phys. Chem. B. 2017;121:5058–5071. doi: 10.1021/acs.jpcb.7b02772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 765.Mahal S.P., Jablonski J., Suponitsky-Kroyter I., Oelschlegel A.M., Herva M.E., Oldstone M., Weissmann C. Propagation of RML Prions in Mice Expressing PrP Devoid of GPI Anchor Leads to Formation of a Novel, Stable Prion Strain. PLoS Pathog. 2012;8:e1002746. doi: 10.1371/journal.ppat.1002746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 766.Roseboom P.H., Namboodiri M.A., Zimonjic D.B., Popescu N.C., Rodriguez I.R., Gastel J.A., Klein D.C. Natural Melatonin “Knockdown” in C57BL/6J Mice: Rare Mechanism Truncates Serotonin N-Acetyltransferase. Brain Res. Mol. Brain Res. 1998;63:189–197. doi: 10.1016/S0169-328X(98)00273-3. [DOI] [PubMed] [Google Scholar]
- 767.Vivien-Roels B., Malan A., Rettori M.C., Delagrange P., Jeanniot J.P., Pévet P. Daily Variations in Pineal Melatonin Concentrations in Inbred and Outbred Mice. J. Biol. Rhythms. 1998;13:403–409. doi: 10.1177/074873098129000228. [DOI] [PubMed] [Google Scholar]
- 768.Dupiereux I., Zorzi W., Lins L., Brasseur R., Colson P., Heinen E., Elmoualij B. Interaction of the 106-126 Prion Peptide with Lipid Membranes and Potential Implication for Neurotoxicity. Biochem. Biophys. Res. Commun. 2005;331:894–901. doi: 10.1016/j.bbrc.2005.04.012. [DOI] [PubMed] [Google Scholar]
- 769.Oku N., Shibamoto S., Ito F., Gondo H., Nango M. Low pH Induced Membrane Fusion of Lipid Vesicles Containing Proton-Sensitive Polymer. Biochemistry. 1987;26:8145–8150. doi: 10.1021/bi00399a019. [DOI] [PubMed] [Google Scholar]
- 770.Connor J., Yatvin M.B., Huang L. pH-Sensitive Liposomes: Acid-Induced Liposome Fusion. Proc. Natl. Acad. Sci. USA. 1984;81:1715–1718. doi: 10.1073/pnas.81.6.1715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 771.Yang S.-T., Kreutzberger A.J.B., Lee J., Kiessling V., Tamm L.K. The Role of Cholesterol in Membrane Fusion. Chem. Phys. Lipids. 2016;199:136–143. doi: 10.1016/j.chemphyslip.2016.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 772.Taraboulos A., Scott M., Semenov A., Avrahami D., Laszlo L., Prusiner S.B. Cholesterol Depletion and Modification of COOH-Terminal Targeting Sequence of the Prion Protein Inhibit Formation of the Scrapie Isoform. J. Cell Biol. 1995;129:121–132. doi: 10.1083/jcb.129.1.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 773.Tobert J.A. Lovastatin and beyond: The History of the HMG-CoA Reductase Inhibitors. Nat. Rev. Drug Discov. 2003;2:517–526. doi: 10.1038/nrd1112. [DOI] [PubMed] [Google Scholar]
- 774.Kuzmin P.I., Akimov S.A., Chizmadzhev Y.A., Zimmerberg J., Cohen F.S. Line Tension and Interaction Energies of Membrane Rafts Calculated from Lipid Splay and Tilt. Biophys. J. 2005;88:1120–1133. doi: 10.1529/biophysj.104.048223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 775.Tsai W.-C., Feigenson G.W. Lowering Line Tension with High Cholesterol Content Induces a Transition from Macroscopic to Nanoscopic Phase Domains in Model Biomembranes. Biochim. Biophys. Acta (BBA)-Biomembr. 2019;1861:478–485. doi: 10.1016/j.bbamem.2018.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 776.Ayuyan A.G., Cohen F.S. Lipid Peroxides Promote Large Rafts: Effects of Excitation of Probes in Fluorescence Microscopy and Electrochemical Reactions during Vesicle Formation. Biophys. J. 2006;91:2172–2183. doi: 10.1529/biophysj.106.087387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 777.Mollinedo F., Gajate C. Lipid Rafts and Clusters of Apoptotic Signaling Molecule-Enriched Rafts in Cancer Therapy. Future Oncol. 2010;6:811–821. doi: 10.2217/fon.10.34. [DOI] [PubMed] [Google Scholar]
- 778.Cedó L., Reddy S.T., Mato E., Blanco-Vaca F., Escolà-Gil J.C. HDL and LDL: Potential New Players in Breast Cancer Development. J. Clin. Med. Res. 2019;8:853. doi: 10.3390/jcm8060853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 779.Jamnagerwalla J., Howard L.E., Allott E.H., Vidal A.C., Moreira D.M., Castro-Santamaria R., Andriole G.L., Freeman M.R., Freedland S.J. Serum Cholesterol and Risk of High-Grade Prostate Cancer: Results from the REDUCE Study. Prostate Cancer Prostatic Dis. 2018;21:252–259. doi: 10.1038/s41391-017-0030-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 780.Li Y.C., Park M.J., Ye S.-K., Kim C.-W., Kim Y.-N. Elevated Levels of Cholesterol-Rich Lipid Rafts in Cancer Cells Are Correlated with Apoptosis Sensitivity Induced by Cholesterol-Depleting Agents. Am. J. Pathol. 2006;168:1107–1118; quiz 1404–1405. doi: 10.2353/ajpath.2006.050959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 781.Kopecka J., Trouillas P., Gašparović A.Č., Gazzano E., Assaraf Y.G., Riganti C. Phospholipids and Cholesterol: Inducers of Cancer Multidrug Resistance and Therapeutic Targets. Drug Resist. Updat. 2020;49:100670. doi: 10.1016/j.drup.2019.100670. [DOI] [PubMed] [Google Scholar]
- 782.Yan A., Jia Z., Qiao C., Wang M., Ding X. Cholesterol Metabolism in Drug-resistant Cancer (Review) Int. J. Oncol. 2020;57:1103–1115. doi: 10.3892/ijo.2020.5124. [DOI] [PubMed] [Google Scholar]
- 783.Brindisi M., Fiorillo M., Frattaruolo L., Sotgia F., Lisanti M.P., Cappello A.R. Cholesterol and Mevalonate: Two Metabolites Involved in Breast Cancer Progression and Drug Resistance through the ERRα Pathway. Cells. 2020;9:1819. doi: 10.3390/cells9081819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 784.Yun U.-J., Lee J.-H., Koo K.H., Ye S.-K., Kim S.-Y., Lee C.-H., Kim Y.-N. Lipid Raft Modulation by Rp1 Reverses Multidrug Resistance via Inactivating MDR-1 and Src Inhibition. Biochem. Pharmacol. 2013;85:1441–1453. doi: 10.1016/j.bcp.2013.02.025. [DOI] [PubMed] [Google Scholar]
- 785.Magarkar A., Dhawan V., Kallinteri P., Viitala T., Elmowafy M., Róg T., Bunker A. Cholesterol Level Affects Surface Charge of Lipid Membranes in Saline Solution. Sci. Rep. 2014;4:5005. doi: 10.1038/srep05005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 786.Finot E., Leonenko Y., Moores B., Eng L., Amrein M., Leonenko Z. Effect of Cholesterol on Electrostatics in Lipid-Protein Films of a Pulmonary Surfactant. Langmuir. 2010;26:1929–1935. doi: 10.1021/la904335m. [DOI] [PubMed] [Google Scholar]
- 787.Eckert G.P., Kirsch C., Leutz S., Wood W.G., Müller W.E. Cholesterol Modulates Amyloid Beta-Peptide’s Membrane Interactions. Pharmacopsychiatry. 2003;36((Suppl. S2)):136–143. doi: 10.1055/s-2003-43059. [DOI] [PubMed] [Google Scholar]
- 788.Choi Y., Attwood S.J., Hoopes M.I., Drolle E., Karttunen M., Leonenko Z. Melatonin Directly Interacts with Cholesterol and Alleviates Cholesterol Effects in Dipalmitoylphosphatidylcholine Monolayers. Soft Matter. 2014;10:206–213. doi: 10.1039/C3SM52064A. [DOI] [PubMed] [Google Scholar]
- 789.Bongiorno D., Ceraulo L., Ferrugia M., Filizzola F., Giordano C., Ruggirello A., Liveri V.T. H-NMR and FT-IR Study of the State of Melatonin Confined in Membrane Models: Location and Interactions of Melatonin in Water Free Lecithin and AOT Reversed Micelles. Arkivoc. 2004;2004:251–262. doi: 10.3998/ark.5550190.0005.522. [DOI] [Google Scholar]
- 790.Rudzite V., Jurika E., Jirgensons J. Changes in Membrane Fluidity Induced by Tryptophan and Its Metabolites. In: Huether G., Kochen W., Simat T.J., Steinhart H., editors. Tryptophan, Serotonin, and Melatonin: Basic Aspects and Applications. Springer US; Boston, MA, USA: 1999. pp. 353–367. [DOI] [PubMed] [Google Scholar]
- 791.de Lima V.R., Caro M.S.B., Munford M.L., Desbat B., Dufourc E., Pasa A.A., Creczynski-Pasa T.B. Influence of Melatonin on the Order of Phosphatidylcholine-Based Membranes. J. Pineal Res. 2010;49:169–175. doi: 10.1111/j.1600-079X.2010.00782.x. [DOI] [PubMed] [Google Scholar]
- 792.Drolle E., Kučerka N., Hoopes M.I., Choi Y., Katsaras J., Karttunen M., Leonenko Z. Effect of Melatonin and Cholesterol on the Structure of DOPC and DPPC Membranes. Biochim. Biophys. Acta. 2013;1828:2247–2254. doi: 10.1016/j.bbamem.2013.05.015. [DOI] [PubMed] [Google Scholar]
- 793.Fernández-Pérez E.J., Sepúlveda F.J., Peters C., Bascuñán D., Riffo-Lepe N.O., González-Sanmiguel J., Sánchez S.A., Peoples R.W., Vicente B., Aguayo L.G. Effect of Cholesterol on Membrane Fluidity and Association of Aβ Oligomers and Subsequent Neuronal Damage: A Double-Edged Sword. Front. Aging Neurosci. 2018;10:226. doi: 10.3389/fnagi.2018.00226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 794.Dies H., Cheung B., Tang J., Rheinstädter M.C. The Organization of Melatonin in Lipid Membranes. Biochim. Biophys. Acta. 2015;1848:1032–1040. doi: 10.1016/j.bbamem.2015.01.006. [DOI] [PubMed] [Google Scholar]
- 795.Venegas C., García J.A., Escames G., Ortiz F., López A., Doerrier C., García-Corzo L., López L.C., Reiter R.J., Acuña-Castroviejo D. Extrapineal Melatonin: Analysis of Its Subcellular Distribution and Daily Fluctuations. J. Pineal Res. 2012;52:217–227. doi: 10.1111/j.1600-079X.2011.00931.x. [DOI] [PubMed] [Google Scholar]
- 796.Jin Y., Liang Q., Tieleman D.P. Interactions between Band 3 Anion Exchanger and Lipid Nanodomains in Ternary Lipid Bilayers: Atomistic Simulations. J. Phys. Chem. B. 2020;124:3054–3064. doi: 10.1021/acs.jpcb.0c01055. [DOI] [PubMed] [Google Scholar]
- 797.Ciana A., Achilli C., Minetti G. Membrane Rafts of the Human Red Blood Cell. Mol. Membr. Biol. 2014;31:47–57. doi: 10.3109/09687688.2014.896485. [DOI] [PubMed] [Google Scholar]
- 798.Murphy S.C., Samuel B.U., Harrison T., Speicher K.D., Speicher D.W., Reid M.E., Prohaska R., Low P.S., Tanner M.J., Mohandas N., et al. Erythrocyte Detergent-Resistant Membrane Proteins: Their Characterization and Selective Uptake during Malarial Infection. Blood. 2004;103:1920–1928. doi: 10.1182/blood-2003-09-3165. [DOI] [PubMed] [Google Scholar]
- 799.Yeagle P.L. Cholesterol and the Cell Membrane. Biochim. Biophys. Acta. 1985;822:267–287. doi: 10.1016/0304-4157(85)90011-5. [DOI] [PubMed] [Google Scholar]
- 800.Cooper R.A. Influence of Increased Membrane Cholesterol on Membrane Fluidity and Cell Function in Human Red Blood Cells. J. Supramol. Struct. 1978;8:413–430. doi: 10.1002/jss.400080404. [DOI] [PubMed] [Google Scholar]
- 801.Maneri L.R., Low P.S. Structural Stability of the Erythrocyte Anion Transporter, Band 3, in Different Lipid Environments. A Differential Scanning Calorimetric Study. J. Biol. Chem. 1988;263:16170–16178. doi: 10.1016/S0021-9258(18)37574-4. [DOI] [PubMed] [Google Scholar]
- 802.Groves J.D., Wang L., Tanner M.J. Complementation Studies with Co-Expressed Fragments of Human Red Cell Band 3 (AE1): The Assembly of the Anion-Transport Domain in Xenopus Oocytes and a Cell-Free Translation System. Pt 1Biochem. J. 1998;332:161–171. doi: 10.1042/bj3320161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 803.Hargreaves W.R., Giedd K.N., Verkleij A., Branton D. Reassociation of Ankyrin with Band 3 in Erythrocyte Membranes and in Lipid Vesicles. J. Biol. Chem. 1980;255:11965–11972. doi: 10.1016/S0021-9258(19)70228-2. [DOI] [PubMed] [Google Scholar]
- 804.Cordeiro R.M. Reactive Oxygen Species at Phospholipid Bilayers: Distribution, Mobility and Permeation. Pt BBiochim. Biophys. Acta. 2014;1838:438–444. doi: 10.1016/j.bbamem.2013.09.016. [DOI] [PubMed] [Google Scholar]
- 805.Oliveira M.C., Yusupov M., Bogaerts A., Cordeiro R.M. Lipid Oxidation: Role of Membrane Phase-Separated Domains. J. Chem. Inf. Model. 2021;61:2857–2868. doi: 10.1021/acs.jcim.1c00104. [DOI] [PubMed] [Google Scholar]
- 806.Wong-Ekkabut J., Xu Z., Triampo W., Tang I.-M., Tieleman D.P., Monticelli L. Effect of Lipid Peroxidation on the Properties of Lipid Bilayers: A Molecular Dynamics Study. Biophys. J. 2007;93:4225–4236. doi: 10.1529/biophysj.107.112565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 807.Kaplán P., Racay P., Lehotský J., Mézesová V. Change in Fluidity of Brain Endoplasmic Reticulum Membranes by Oxygen Free Radicals: A Protective Effect of Stobadine, Alpha-Tocopherol Acetate, and Butylated Hydroxytoluene. Neurochem. Res. 1995;20:815–820. doi: 10.1007/BF00969693. [DOI] [PubMed] [Google Scholar]
- 808.Miller Y.I., Navia-Pelaez J.M., Corr M., Yaksh T.L. Lipid Rafts in Glial Cells: Role in Neuroinflammation and Pain Processing: Thematic Review Series: Biology of Lipid Rafts. J. Lipid Res. 2020;61:655–666. doi: 10.1194/jlr.TR119000468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 809.Sviridov D., Mukhamedova N., Miller Y.I. Lipid Rafts as a Therapeutic Target: Thematic Review Series: Biology of Lipid Rafts. J. Lipid Res. 2020;61:687–695. doi: 10.1194/jlr.TR120000658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 810.Balakrishnan M., Kenworthy A.K. Lipid Peroxidation Enhances LO/LD Domain Phase Separation in Giant Plasma Membrane Vesicles. Biophys. J. 2021;120:324a. doi: 10.1016/j.bpj.2020.11.2044. [DOI] [Google Scholar]
- 811.Dies H., Toppozini L., Rheinstädter M.C. The Interaction between Amyloid-β Peptides and Anionic Lipid Membranes Containing Cholesterol and Melatonin. PLoS ONE. 2014;9:e99124. doi: 10.1371/journal.pone.0099124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 812.Ceraulo L., Ferrugia M., Tesoriere L., Segreto S., Livrea M.A., Turco Liveri V. Interactions of Melatonin with Membrane Models: Portioning of Melatonin in AOT and Lecithin Reversed Micelles. J. Pineal Res. 1999;26:108–112. doi: 10.1111/j.1600-079X.1999.tb00570.x. [DOI] [PubMed] [Google Scholar]
- 813.Aikens J., Dix T.A. Perhydroxyl Radical (HOO.) Initiated Lipid Peroxidation. The Role of Fatty Acid Hydroperoxides. J. Biol. Chem. 1991;266:15091–15098. doi: 10.1016/S0021-9258(18)98591-1. [DOI] [PubMed] [Google Scholar]
- 814.Brazier M.W., Lewis V., Ciccotosto G.D., Klug G.M., Lawson V.A., Cappai R., Ironside J.W., Masters C.L., Hill A.F., White A.R., et al. Correlative Studies Support Lipid Peroxidation Is Linked to PrP(res) Propagation as an Early Primary Pathogenic Event in Prion Disease. Brain Res. Bull. 2006;68:346–354. doi: 10.1016/j.brainresbull.2005.09.010. [DOI] [PubMed] [Google Scholar]
- 815.Rofstad E.K., Mathiesen B., Kindem K., Galappathi K. Acidic Extracellular pH Promotes Experimental Metastasis of Human Melanoma Cells in Athymic Nude Mice. Cancer Res. 2006;66:6699–6707. doi: 10.1158/0008-5472.CAN-06-0983. [DOI] [PubMed] [Google Scholar]
- 816.Lee M.Y., Ryu J.M., Lee S.H., Park J.H., Han H.J. Lipid Rafts Play an Important Role for Maintenance of Embryonic Stem Cell Self-Renewal. J. Lipid Res. 2010;51:2082–2089. doi: 10.1194/jlr.M001545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 817.Alomari M., Almohazey D., Almofty S.A., Khan F.A., Al Hamad M., Ababneh D. Role of Lipid Rafts in Hematopoietic Stem Cells Homing, Mobilization, Hibernation, and Differentiation. Cells. 2019;8:630. doi: 10.3390/cells8060630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 818.Shi G., Jin Y. Role of Oct4 in Maintaining and Regaining Stem Cell Pluripotency. Stem Cell Res. Ther. 2010;1:39. doi: 10.1186/scrt39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 819.Kim J., Orkin S.H. Embryonic Stem Cell-Specific Signatures in Cancer: Insights into Genomic Regulatory Networks and Implications for Medicine. Genome Med. 2011;3:75. doi: 10.1186/gm291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 820.Liu A., Yu X., Liu S. Pluripotency Transcription Factors and Cancer Stem Cells: Small Genes Make a Big Difference. Chin. J. Cancer. 2013;32:483–487. doi: 10.5732/cjc.012.10282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 821.Lim J.H., Go G., Lee S.H. PrPC Regulates the Cancer Stem Cell Properties via Interaction With c-Met in Colorectal Cancer Cells. Anticancer Res. 2021;41:3459–3470. doi: 10.21873/anticanres.15133. [DOI] [PubMed] [Google Scholar]
- 822.Zhang W., Wang N., Zhang T., Wang M., Ge W., Wang X. Roles of Melatonin in Goat Hair Follicle Stem Cell Proliferation and Pluripotency Through Regulating the Wnt Signaling Pathway. Front. Cell Dev. Biol. 2021;9:686805. doi: 10.3389/fcell.2021.686805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 823.Georgiev G.N., Marinova E., Konakchieva R., Todorov P. Melatonin Selectively Influences the Transcription of Pluripotency and Differentiation Markers in Human Non-Cancer Cells. Biotechnol. Biotechnol. Equip. 2019;33:286–293. doi: 10.1080/13102818.2019.1571440. [DOI] [Google Scholar]
- 824.Akbarzadeh M., Movassaghpour A.A., Ghanbari H., Kheirandish M., Fathi Maroufi N., Rahbarghazi R., Nouri M., Samadi N. The Potential Therapeutic Effect of Melatonin on Human Ovarian Cancer by Inhibition of Invasion and Migration of Cancer Stem Cells. Sci. Rep. 2017;7:17062. doi: 10.1038/s41598-017-16940-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.