Abstract
Chlorophytum genus has been extensively studied due to its diverse biological activities. We evaluated the methanolic extract of leaves of Chlorophytum comosum (Green type) (Thunb.) Jacques, the species that is less studied compared to C. borivilianum. The aim was to identify phytoconstituents of the methanolic extract of leaves of C. comosum and biological properties of its different fractions. Water fraction was analyzed with matrix-assisted laser desorption/ionization time-of-flight (MALDI-TOF) mass spectrometry. Nineteen compounds belonging to different chemical classes were identified in the methanolic extract of leaves of C. comosum (Green type) (Thunb.) Jacques. In addition to several fatty acids, isoprenoid and steroid compounds were found among the most abundant constituents. One of the identified compounds, 4′-methylphenyl-1C-sulfonyl-β-d-galactoside, was not detected earlier in Chlorophytum extracts. The water fraction was toxic to HeLa cells but not to Vero cells. Our data demonstrate that methanolic extract of leaves of C. comosum can be a valuable source of bioactive constituents. The water fraction of the extract exhibited promising antitumor potential based on a high ratio of HeLa vs. Vero cytotoxicity.
Keywords: Chlorophytum comosum, antioxidant activity, cytotoxicity, herbal medicine, biological active substances
1. Introduction
Chlorophytum comosum belongs to the genus Chlorophytum that covers more than 200 species [1,2,3]. A number of Chlorophytum species are referred to as medicinal herbs in the traditional medicine of India [4,5], China [6,7] and Africa [8]. Several species are known as a source of ‘Safed musli’, a major ingredient of herbal preparations with immunomodulatory, adaptogenic, aphrodisiac and other activities [2,3,4,9,10].
Due to its long use in history in traditional medicine, the Chlorophytum genus has drawn the attention of researchers in evidence-based medicine. Preparations obtained from different Chlorophytum species have been studied for their biological activity and were found to possess immunomodulatory and anti-infectious [11,12,13,14,15,16], antibacterial [17], antinociceptive [18] and antioxidant activities [19,20,21,22,23,24,25,26] to improve male sexual health [27,28,29,30,31,32,33,34], to ameliorate manifestations of diabetes, hyperglycemia and hyperlipidemia [35,36,37,38] or toxic hepatic and testicular impairments [20,39,40].
The antitumor potential of the Chlorophytum genus has also been studied. Most studies have been performed in vitro with the use of herbal extracts, their fractions or purified constituents. Butanol extract of C. comosum roots was shown to inhibit proliferation and induce apoptosis in four cell lines, mostly of hematological origin. Corresponding to the provided data on the concentrations used in the study, the antiproliferative effect of the extract for T-cell leukemia CCRF-HSB-2 cells exceeded that of Actinomycin D 7- to 8-fold [41]. Crude methanol/dichloromethane extract and butanol (saponin) fraction of methanolic extract of C. borivilianum roots have been demonstrated to have relatively low toxicity with IC50 > 100 mkg/mL to three solid tumor cell lines [22]. Similar data were obtained for promyelocytic leukemia HL-60 cells treated with methanolic extracts or saponin fractions of roots of five Chlorophytum species [4].
Water extract of C. borivilianum roots was examined for antitumor activity in vivo. It has been shown that the extract suppressed the onset and progression of skin tumors induced by carcinogen/promoter application [25].
Phytochemistry studies have revealed compounds of various chemical classes to present in Chlorophytum plants. Both common and specific constituents have been isolated from underground parts of Chlorophytum species with the use of different extraction and fractionation methods [17,42,43,44,45]. The major class of phytochemicals of the Chlorophytum genus is represented by a versatile group of saponins that exert different biological activities [1,37,46,47,48,49,50,51,52].
In vitro cytotoxicity, studies were carried out with saponins purified from butanol fractions obtained from methanolic extracts of underground parts of C. comosum [46,47] and rhizomes of C. malayense [48] as well as ethanolic extract of roots of C. borivilianum [49]. Saponins from C. comosum inhibited tumor promoter effects and exhibited cytotoxicity towards cervical carcinoma HeLa cells, though quantitative data on cytotoxicity were not provided [47]. In seven cell lines originating from solid tumors, C. malayense saponin chloromaloside A has been shown to exert a cytotoxic effect that was weaker than that of microtubule destabilizing agent colchicine and topoisomerase II inhibitor ellipticine [48]. One of five spirostane-type saponins purified from C. borivilianum, borivilianoside H, was found to be highly toxic to colon tumor cell lines, much less toxic compared to microtubule targeting antitumor compound paclitaxel [49].
Studies published so far have been performed almost exclusively using the underground parts of plants, though secondary metabolite biosynthesis is believed to take place both in leaves and roots based on gene expression profiles [53]. Some of the leaf extracts of C. borivilianum obtained with solvents of different polarities exhibited antioxidant properties comparable to those of ascorbic acid and quercetin [54]. Aqueous, methanolic and ethanolic extracts of C. borivilianum leaves were shown to be toxic to BHK-21 cells [55] that are derived from normal newborn hamster fibroblasts [56]. Since crude leaf extracts are toxic to normal cells, they can be hardly considered as an efficient anticancer remedy and their biological activities have to be evaluated after further fractionation. Recently, ethanolic root and leaf extracts of C. comosum were studied and shown to be toxic to MCF-7, A549 and H1299 cells [57].
Here, we present the study of phytochemistry and biological activities of fractions obtained with serial fractionation of methanolic extract of C. comosum leaves. The extract was found to comprise a number of bioactive compounds with known biological activities. n-Hexane, chloroform, n-butanol and water fractions proved to be substantially different in their content and activity. Chloroform and n-butanol fractions possess the majority of antioxidant properties, whereas water fractions exhibited the most promising anti-tumor potential.
2. Results
2.1. GC-MS Analysis
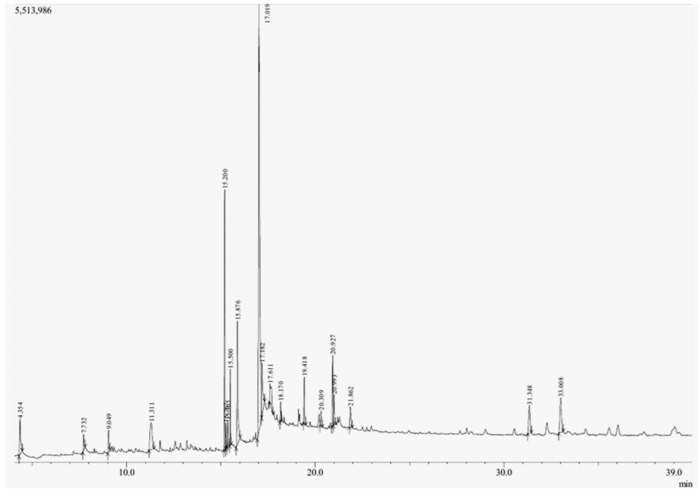
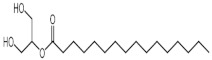
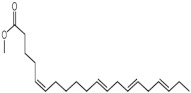
The GC-MS analysis of methanolic leaf extract of C.comosum (Figure 1) revealed nineteen constituents representing 100% of the extract. The detailed tabulations of GC-MS analysis of the extract are given in Table 1. Three major compounds with maximum content included 9,12-octadecadienoic acid (Z,Z)- (41.27%), neophytadiene (9.57%), and n-hexadecanoic acid (7.66%). Sucrose, γ-sitosterol, octadecanoic acid, 9,12-octadecadienoic acid (Z,Z)-, 2-hydroxy-1-(hydroxymethyl) ethyl ester, stigmasterol, 4′-methylphenyl-1C-sulfonyl-.beta.-d-galactoside, dihydroxyacetone, 3,7,11,15-tetramethyl-2-hexadecen-1-ol, hexadecanoic acid, 2-hydroxy-1-(hydroxymethyl) ethyl ester, and methyl (Z)-5,11,14,17-eicosatetraenoate were present at levels of circa 2–4.5% each. The residual compounds detected by GC-MS comprised less than 9% in total.
Figure 1.
GC-MS chromatogram of the methanolic extract of leaves of Chlorophytum comosum (Green type).
Table 1.
Phytoconstituents detected in the methanolic extract from leaves of Chlorophytum comosum (Green type).
| Peak No. | RT | Name of the Phytoconstituents |
Structure | Mol. Formula |
Molecular Weight |
Peak Area % |
LogPo/w | Chemical Class |
|---|---|---|---|---|---|---|---|---|
| 1 | 4.354 | 1,3-Dihydroxyacetone |
|
C3H6O3 | 90 | 2.85 | −1.95 | Saccharide |
| 2 | 7.732 | Glycerol |
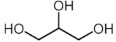
|
C3H8O3 | 92 | 1.01 | −1.93 * | Polyol |
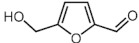
| 3 | 9.049 | 5-Hydroxymethylfurfural |
|
C6H6O3 | 126 | 1.15 | −0.17 * | Aromatic aldehyde |
| 4 | 11.311 | Sucrose |
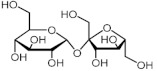
|
C12H22O11 | 342 | 4.5 | −2.63 * | Disaccharide |
| 5 | 15.2 | 7,11,15-trimethyl-3-methylidenehexadec-1-ene (Neophytadiene) |
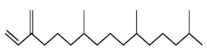
|
C20H38 | 278 | 9.57 | 8.12 * | Isoprenoid hydrocarbon |
| 6 | 15.267 | 2-Hexadecene, 3,7,11,15-tetramethyl-, [R-[R*,R*-(E)]]- (2-Phytene) |
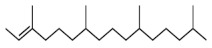
|
C20H40 | 280 | 1.15 | 8.81 * | Isoprenoid hydrocarbon |
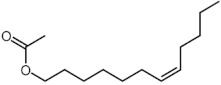
| 7 | 15.365 | E-6-Octadecen-1-ol acetate |
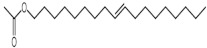
|
C20H38O2 | 310 | 1.57 | 8.34 * | Fatty alcohol ester |
| 8 | 15.5 | 3,7,11,15-Tetramethyl-2-hexadecen-1-ol (Phytol) |
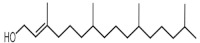
|
C20H40O | 296 | 2.75 | 7.89 * | Diterpene alcohol |
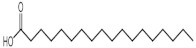
| 9 | 15.876 | n-Hexadecanoic acid(Palmitic acid) |
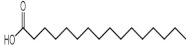
|
C16H32O2 | 256 | 7.66 | 7.17 | Fatty acid |
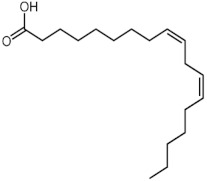
| 10 | 17.019 | 9,12-Octadecadienoic acid (Z,Z)- (Linoleic Acid) |
|
C18H32O2 | 280 | 41.27 | 7.05 [58] | Fatty acid |
| 11 | 17.182 | Octadecanoic acid (Stearic acid) |
|
C18H36O2 | 284 | 4.32 | 8.23 [58] | Fatty acid |
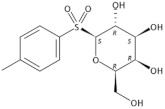
| 12 | 17.611 | 4′-Methylphenyl-1C-sulfonyl-β-d-galactoside |
|
C13H18O7S | 318 | 2.88 | −1.21 * | Sulfoneglycoside |
| 13 | 18.17 | cis-7-Dodecen-1-yl acetate (Looplure) |
|
C14H26O2 | 226 | 0.8 | 5.66 * | Fatty alcohol ester |
| 14 | 19.418 | Hexadecanoic acid, 2-hydroxy-1-(hydroxymethyl) ethyl ester (2-Palmitoylglycerol) |
|
C19H38O4 | 330 | 2.24 | 5.77 * | Fatty acid ester |
| 15 | 20.309 | Methyl 6-o-[1-methylpropyl]-β-d-galactopyranoside |
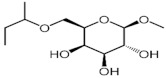
|
C11H22O6 | 250 | 2.66 | −0.30 * | Monosaccharide |
| 16 | 20.927 | 9,12-Octadecadienoic acid (Z,Z)-, 2-hydroxy-1-(hydroxymethyl) ethyl ester (2-Linoleoyl Glycerol) |
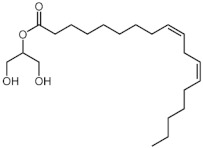
|
C21H38O4 | 354 | 4.04 | 5.55 * | Fatty acid ester |
| 17 | 20.993 | Methyl (Z)-5,11,14,17-eicosatetraenoate |
|
C21H34O4 | 318 | 2.05 | 6.82 * | Fatty acid ester |
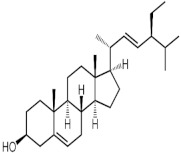
| 18 | 31.348 | Stigmasterol |
|
C29H48O | 412 | 3.09 | 6.95 * | Stigmastane |
| 19 | 33.008 | γ-Sitosterol |
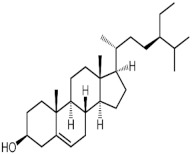
|
C29H50O | 414 | 4.44 | 7.27 * | Stigmastane |
*—Calculated with ALOGPS software [59].
2.2. Phytochemical Screening of Fractions
All fractions of the methanolic extract were shown to contain phenolic compounds, flavonoids, chlorophylls, carotenoids, tannins and reducing sugars (Table 2). The largest amounts of chlorophylls and carotenoids were found in the n-hexane and chloroform fractions, whereas phenolic compounds and simple carbohydrates were most abundant in the n-butanol fraction and, to a lesser extent, yielded in the chloroform fraction.
Table 2.
Total bioactive compounds found in fractions of the methanolic extract of leaves of Chlorophytum comosum (Green type), mean ± SD (n = 10).
| Bioactive Compounds | n-Hexane Fraction | Chloroform Fraction | n-Butanol Fraction | Water Fraction |
|---|---|---|---|---|
| Relative content of dry matter, % | 19.9 ± 0.5 | 22.8 ± 0.57 | 23.4 ± 0.4 | 33.9 ± 0.7 |
| Concentration of extracted matter in DMSO, mg/mL | 50 ± 2.0 * | 100 ± 2.0 | 100 ± 3.0 | 100 ± 3.0 |
| Total phenolic content (TPC), mg GAE/mL | 1.08 ± 0.02 | 5.6 ± 0.1 | 19.9 ± 0.5 | 0.51 ± 0.02 |
| Tannins, mg/mL | 1.73 ± 0.04 | 4.22 ± 0.1 | 15.75 ± 0.4 | 1.77 ± 0.03 |
| Total flavonoid content (TFC), mg QE/mL | 0.05 ± 0.001 | ND ** | 0.09 ± 0.001 | ND |
| Chlorophyll a, mg/mL | 3.16 ± 0.05 | 0.16 ± 0.004 | ND | ND |
| Chlorophyll b, mg/mL | 1.77 ± 0.02 | 0.26 ± 0.01 | ND | ND |
| Carotenoids, mg/mL | 0.74 ± 0.02 | 0.62 ± 0.02 | ND | ND |
| Reducing sugars, mg/mL | 1.53 ± 0.03 | 9.18 ± 0.1 | 22.2 ± 0.5 | 1.28 ± 0.02 |
* The extracted matter in the n-hexane fraction had low solubility in DMSO. ** ND, not detected.
In the water fraction, little amounts of phenolic compounds and simple carbohydrates were detected; most of the remaining matter in the fraction was not identified.
2.3. Antioxidant Activity of Fractions
The chloroform and n-butanol fractions exhibit the highest reducing power and total antioxidant activity (Table 3). The antioxidant properties have to be attributed to phenolic compounds that are most abundant in these fractions.
Table 3.
Antioxidant activity of the fractions of methanolic extract from leaves of Chlorophytum comosum (Green type), mean ± SD (n = 10).
| Antioxidant Activity Criterion |
n-Hexane Fraction |
Chloroform Fraction |
n-Butanol Fraction |
Water Fraction |
| Reducing power, mg AAE eq/mL |
0.39 ± 0.01 | 6.25 ± 0.2 | 33.1 ± 2.5 | 0.58 ± 0.07 |
| ABTS radical scavenging activity, mg TEs/mL | 0.27 ± 0.01 | 0.36 ± 0.01 | 0.81 ± 0.05 | 0.27 ± 0.02 |
| Total antioxidant activity (TAA), mg AAE eq/mL | 9.7 ± 0.32 | 17.4 ± 0.6 | 35.9 ± 4.5 | 1.8 ± 0.9 |
2.4. Cytotoxicity
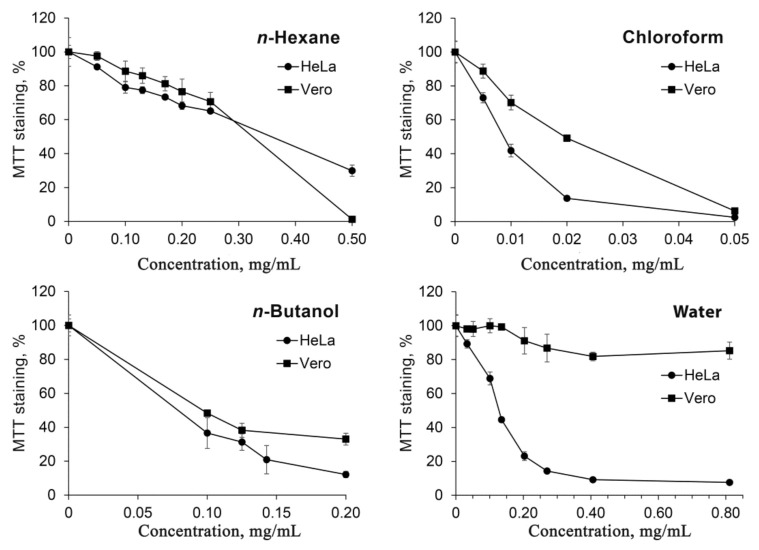
Human cervical carcinoma cell line HeLa and non-cancerous kidney epithelium cells of Cercopithecus aethiops Vero were used for the cytotoxicity studies (Figure 2). Chloroform fraction proved to be the most toxic to cells, with relatively higher (appr. two-fold) toxicity towards HeLa cells. n-Hexane and n-butanol fractions exhibited similar toxicity to both HeLa and Vero cells. On the other hand, the water fraction was shown to have a very high ratio of Hela to Vero toxicity. While the viability of HeLa cells was efficiently inhibited with IC50 value of 0.12 mg/mL, Vero cells were not affected by the water fraction at doses up to the maximum concentration limited by toxicity of the solvent.
Figure 2.
Cytotoxicity of fractions of methanolic extract of leaves of Chlorophytum comosum (Green type).
2.5. MALDI-TOF Mass Spectrometry of Water Fraction of Methanolic Extract of Leaves of C. comosum
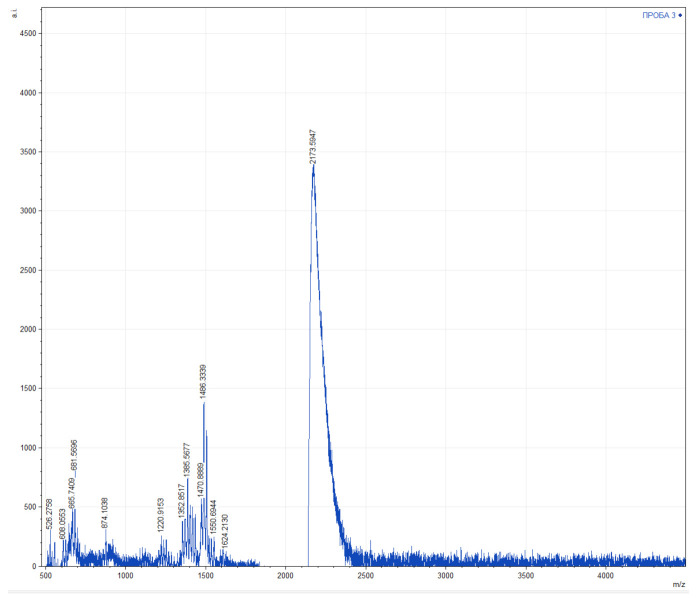
The obtained mass spectra of the water fraction contain signals of different intensities in the range of 500–2200 Da (Figure 3). There were 10 signals with m/z up to 1000 Da, 19 signals in the range of 1200–1700 Da and one signal of 2173 Da detected. The following signals were characterized by the highest intensity: 681 ± 5 Da, 1385 ± 5 Da, 1486 ± 5 Da, 1503 ± 5 Da, and 2173 ± 5 Da. Analysis of mass spectrometry data using the BIOPEP-UWM™ database [60], showed that of water fraction of methanolic extract of leaves of C. comosum may contain peptides with antibacterial, antifungal and anticancer activities, as well as enzyme inhibitors that could determine its activity in cell cultures (Table 4).
Figure 3.
Data of the MALDI-TOF mass spectrometry of water fraction of methanolic extract of leaves of Chlorophytum comosum (Green type).
Table 4.
Characterization of the proteomic analysis of water fraction of methanolic extract of leaves of Chlorophytum comosum (in accordance with the BIOPEP-UWM™ database).
| Chemical Mass, Da | ID | Sequence | Activity | Int. |
|---|---|---|---|---|
| 681 | - | - | - | 730 |
| - | 8252 | EQRPR | anticancer | - |
| 1385 | - | - | - | 675 |
| - | 3194 | FLPAIAGILSQLF~ | hemolytic | - |
| - | 8311 | FFVAPFPEVFGK | anticancer | - |
| - | 9291 | KKLFKKILKKL~ | antifungal | - |
| - | 9466 | FKCRRWQWR | antibacterial | - |
| 1486 | - | - | - | 1335 |
| 2979 | KKAVRRQEAVDAL | CaMKII inhibitor | - | |
| - | 2989 | KKALRRDEAVDAL | CaMKII inhibitor | - |
| - | 2990 | KKALRRNEAVDAL | CaMKII inhibitor | - |
| - | 2991 | KKALRRQEGVDAL | CaMKII inhibitor | - |
| - | 3190 | SSSKEENRIIPGGI | antibacterial | - |
| - | 5450 | GLFDAIGNLLGGLGLG | antibacterial | - |
| - | 5474 | GLFDIVKKIAGHIA | antibacterial | - |
| - | 8335 | SDIPNPIGSENSEK | antibacterial | - |
| - | 9458 | RWQWRWQWR | antibacterial | - |
| - | 9783 | GEHGGAGMGGGQFQPV | alpha-amylase inhibitor | |
| - | 9784 | GEHGGAGMGGGQFQPV | pancreatic lipase inhibitor | |
| 9785 | GEHGGAGMGGGQFQPV | lipoxygenase inhibitor | ||
| 9786 | GEHGGAGMGGGQFQPV | cyclooxygenase-1 inhibitor | ||
| 9787 | GEHGGAGMGGGQFQPV | cyclooxygenase-2 inhibitor | ||
| 1503 | - | - | - | 1083 |
| - | 2987 | KKALRREEAVDAL | CaMKII inhibitor | - |
| - | 3006 | KKALYRQEAVDAL | CaMKII inhibitor | - |
| - | 3008 | KKALRYQEAVDAL | CaMKII inhibitor | - |
| - | 3920 | GLFDIIKKIAESIG | antibacterial | - |
| - | 5454 | GLFDIIKKIAESIG | antibacterial | - |
| - | 5457 | LDIVKKVVGAFGSLG | antibacterial | - |
| - | 9294 | WKLFKKILKWL~ | antifungal | - |
| - | 9295 | WKLFKKILKWL~ | hemolytic | - |
| - | 9313 | WKLFKKILKKLG | antifungal | - |
| - | 9314 | WKLFKKILKKLG | hemolytic | - |
| 2173 | - | - | - | 2403 |
| 3822 | GLLRRLRKKIGEIFKKYG | antibacterial | - | |
| 7053 | KWKLFKKIKFLHSAKKF | anticancer | - |
3. Discussion
A number of compounds that were identified in the methanolic extract of leaves of Chlorophytum comosum (Green type) have been well characterized.
As is seen from the GC-MS data, unsaturated fatty acids are among the major constituents of the methanolic extract. Linoleic acid (appr. 41% of GC-MS chromatogram area, Figure 1) is considered an essential nutrient with a variety of physiological functions, though there are concerns about the consequences of its excessive consumption for human health. [61,62]. Palmitic acid (7.66%) is one of the most abundant saturated fatty acids in organisms. Its homeostasis is tightly controlled, and its imbalance is related to different physiopathological conditions [63]. Stearic acid (4.32%), synthesized from palmitic acid, is one the most abundant saturated fatty acid in the Western diet. Its effects on cardiometabolic risk markers seem to be different from that of palmitic acid, and a stearic acid-reach diet could be beneficial compared to the ones that are rich with other saturated fatty acids [64,65].
Sucrose (4.5%) is an important nutrient energy source, but its imbalance or excessive consumption has multiple deleterious effects on human health [66,67]. It has been also demonstrated to exert pain preventive effect on infants [68,69].
Some of the constituents of C. comosum methanolic leaf extract have been shown to exhibit therapeutic potential. For the second most abundant compound detected with GC-MS, neophytadiene (appr. 10%), anti-inflammatory, antioxidant and cardioprotective activities have been demonstrated [70].
γ-Sitosterol (4.44%) was shown to exert hypocholesterolemic, antidiabetic effects [71].
Stigmasterol (3.09%) exerts antitumor [58,72,73,74], hypolipidemic [75,76,77,78,79,80], antidiabetic [81,82], antimutagenic [83], antiparasitic [84], and antinociceptive [85] effects. It can also alleviate manifestations of osteoarthritis [86,87], inflammation and autoimmune diseases [88,89,90,91], and mitigate central nerve system injuries and disorders in both neuroprotective and function-improving manner [92,93,94,95,96,97,98]. In several studies its antioxidant activity was also demonstrated [79,81,89,92,93,94]. Stigmasterol accumulation, however, can cause cardiac injury [99].
Phytol (2.75%) possesses antioxidant, antimicrobial, anticancer, antidiabetic, hypolipidemic, immunoadjuvant, anti-inflammatory, antimutagenic, antiteratogenic, antinociceptive, antispasmodic, anticonvulsant, anxiolytic, antidepressant activities; it can be used in cosmetics as an active substance or fragrance material [100,101].
5-Hydroxymethylfurfural (1.15%) has been found to exert both deleterious (organotoxic, mutagenic, carcinogenic, pro-oxidant) and beneficial (antihypoxic, anticancer, antioxidant, anti-allergen, antisickling) effects on health [102,103].
In addition to compounds identified by GC-MS, the methanolic leaf extract of C. comosum was shown to contain phenolic compounds including tannins that are most abundant in the n-butanol fraction (Table 2). Reducing sugars were also found at the highest levels in the n-butanol fraction. The chloroform fraction was found to contain two- to three-fold less phenolic compounds and reducing sugars, and n-hexane and water fractions had the least amounts of these constituents. Flavonoids were detected at low levels in n-hexane and n-butanol fractions. The larger part of chlorophylls was extracted from the methanolic extract by n-hexane; much lesser chlorophylls were also detected in chloroform fractions. Carotenoids were found in n-hexane and chloroform fractions at appr. equal levels.
The antioxidant activity of different fractions of the methanolic leaf extract of C. comosum (Table 3) was found to be partially related to the bioactive compound content. The highest reducing power, radical scavenging activity, and total antioxidant activity were found in n-butanol and chloroform fractions that correlated with the highest content of phenolic compounds. On the other hand, the reducing power and total antioxidant activity of n-hexane and water fractions did not correspond to the phenolic compounds content since water fraction had appr. 1.5-fold higher reducing power and appr. 5-fold lower total antioxidant activity, while both fractions contained similar levels of total phenolics and tannins. It is generally accepted that the antioxidant activity corresponds to the total phenolic content, but in some cases, controversial data were reported suggesting that antioxidant activity might be attributed to antioxidants other than compounds defined as total phenolics [104,105].
The cytotoxicity studies have revealed that the constituents of water fraction have very high toxicity to cancerous HeLa cells compared to non-cancerous Vero cells. In fact, there was no apparent toxicity of water fraction towards Vero cells (Figure 2). The chloroform fraction was shown to be most toxic to cells, but the selectivity towards HeLa cells was significantly lower compared to that of the water fraction.
The data obtained recently with use of n-butanol processed ethanolic extracts of defatted roots and leaves of C. comosum demonstrated that the extracts were toxic to breast (MCF-7) and lung cancer (A549 and H1299) cell lines but not to the L-132 cell line [57]. Though L-132 (ATCC® CCL-5™) cells cannot be considered non-cancerous since they have signs of HeLa contamination [106,107], these results, together with the data presented herein, suggest that C. comosum phytoconstituents can possess promising antitumor activity. Moreover, our data demonstrate that the selective antitumor compounds reside in the fraction obtained after successive removal of n-hexane-, chloroform- and n-butanol-soluble material.
The total phenolic content of root and leaf ethanolic extracts of C. comosum was in good agreement with their antioxidant activity but had poor correlation with cytotoxicity [57]. Our data obtained after more fractionation steps displayed evidence that cytotoxicity of fractions of methanolic leaf extract of C. comosum has no correlation with found bioactive compounds or antioxidant activity.
Further considering active substances that can be responsible for the observed cytotoxicity profile of water fraction, one could suggest that, because of negative LogPo/w values, some constituents of the methanolic extract (Table 1) could be present in water fraction. Unfortunately, cytotoxic activity demonstrated so far for that compound does not support any conclusions about an active substance to which the antitumor potential of water fraction could be attributed.
1,3-Dihydroxyacetone, the compound commonly used in sunless tanning products, was shown to be toxic to transformed HEK293T cells [108], A375P melanoma cells [109], and non-cancerous HaCaT cells [110,111]. The experimental settings in the mentioned papers were different, and it is not possible to conclude if dihydroxyacetone could be more toxic towards cancerous than to normal cells. 5-Hydroximethylfurfural, one of the toxicants produced during food processing, exerted moderate cytotoxicity, with IC50 values of millimolar range, to both cancerous and non-cancerous cells [112,113,114].
Glycerol is one of the cryoprotectants that is quite toxic to cells at 37 °C even under short exposure time [115,116], but it exhibits general cytotoxicity regardless of the origin of cells.
Sucrose is well tolerated by cells and affects the protein glycosylation processes rather than the cell viability [117].
The sulfone glycoside 4′-methylphenyl-1C-sulfonyl-β-d-galactoside is quite a rare phytoconstituent. To our knowledge, there is the only MS study that identified 4′-methylphenyl-1C-sulfonyl-β-d-galactoside in Rhodiola Rosea [118]. The biological activity of this compound is not known. The compound was synthesized in a survey of antimalarial agents, but no further studies were published since 1964 [119,120]. A structural analog of the compound with methylphenyl-sulfonyl moiety bound to the oxygen of the 6C atom, inhibited the sugar uptake process in bacteria [121].
Methyl 6-o-[1-methylpropyl]-β-d-galactopyranoside was found as one of four most abundant constituents in the ethanolic leaf extract of the Kofat cultivar of Catha edulis. The cytotoxicity studies did not reveal any selectivity in toxicity of the extracts towards cancer cells compared to normal fetal lung fibroblast [122].
MALDI-TOF mass spectrometry of the water fraction has revealed a number of compounds that may belong to bioactive peptides. The EQRPR pentapeptide, identified in rice bran, was shown to be toxic to several cancer cell lines, though at relatively high concentrations [123]. The peptide FFVAPFPEVFGK and its close analogs were found in skin extract of amphibians and hydrolysates of casein [124]. It was found to inhibit several proteinases involved in cancer progression though it did not exhibit cytotoxicity towards cancer cells [125]. The KWKLFKKIKKIKFLHSAKKF peptide, corresponding to CancerPPD database data [126], possesses mild cytotoxic activity against several cancer cell lines with IC50 values ranging at 65–100 µM. At the same time, this peptide is an artificial chimera of two antibacterial peptides of Hyalophora cecropia and Xenopus laevis [127], hence it is hardly possible that this compound is naturally produced by C. comosum.
Thus, the water fraction of the methanolic extracts of leaves of C. comosum contains compound(s) that have highly selective toxicity towards cancer cells. This anti-cancer cytotoxicity is apparently unrelated to antioxidant activity. Active compounds of the water fraction may be presented by both small molecules and bioactive peptides.
4. Materials and Methods
4.1. Chemicals
Methyl alcohol 99.9%, n-hexane 95%, chloroform 99%, n-butanol 99%, dimethyl sulfoxide (DMSO) 99.7%, aluminum chloride 99.9%, sodium acetate >99%, quercetin, acetone >99.5%, picric acid ≥98.0%, dextrose 99.5%, sodium carbonate 99.5%, phosphate buffered saline (pH 7.2 at 25 °C), potassium ferricyanide (III), trichloroacetic acid, α-Cyano-4-hydroxycinnamic acid (for MALDI-TOF MS), acetonitrile ≥99.0%, iron (III) chloride 99%, ascorbic acid ≥99%, sulfuric acid 99.9%, sodium phosphate 96%, ammonium molybdate, potassium persulfate ≥99.0%, 2,2′-azino-bis(3-ethylbenzothiazoline-6-sulfonic acid) diammonium salt (ABTS), 6-hydroxy-2,5,7,8-tetramethylchroman-2-carboxylic acid (Trolox) 97%, Folin–Denis’ reagent, gallic acid, tannin and chemical standards were purchased from Sigma-Aldrich.
EMEM and DMEM incubation media, L-glutamine, essential amino acids mixture, penicillin-streptomycin 100x lyophilized mixture, 0.25% trypsin solution and 0.02% versene solution were purchased from PanEco, Ltd. (Moscow, Russia), fetal bovine serum—from BioWest (Nuaillé, France), and MTT (3-(4,5-dimethylthiazole-2-yl)-2,5-diphenyl-tetrazolium bromide)—from Diaem, Ltd. (Moscow, Russia).
4.2. Plant Material
Chlorophytum comosum (Green type) (Thunb.) Jacques was kindly provided by the Botanical Garden of the North-Caucasus Federal University. Vegetative propagation of the plant was carried out in the Greenhouse of the Moscow Region State University. The plant was harvested in August 2019.
4.3. Sample Preparation
Freshly cut leaves were washed under running tap water for 30 s, chopped with scissors to pieces of 1–2 cm and subjected to freeze-drying. The material was frozen in SE10-45 (TEFCOLD, Viborg, Denmark) at a temperature of minus 39.0–40.0 °C for 72 h. Subsequent drying was carried out for 27–30 h in a light-protected chamber in LS-500 freeze dryer (Prointech, Puschino, Russia) with average working pressure in the dryer chamber of 90–100 Pa, the condenser temperature minus 47–49 °C. The residual moisture content of the dried material amounted to 5–6% as was measured using an Ohaus MB 25 moisture meter (Ohaus Corporation, Parsippany, NJ, USA) at a temperature of 100 °C in an automatic mode.
The lyophilized leaves were ground to a powder with particle size of 1 mm or less using a VT-1541 VK grinder (Vitek, SuZhou, China). The powdered samples were stored at 4 °C in a dark hermetically sealed container until testing for no more than one week.
4.4. Extraction and Fractionation
Of the powdered lyophilized leaves, 42.0 g was extracted with 420.0 mL of methanol for 14 days at room temperature (23 ± 0.5 °C). The extract was filtered through cheesecloth and paper filters and then dried using a rotary evaporator RV 10 Basic V (IKA, Germany) at a temperature of 45–50 °C until complete solvent removal [128,129]. The yield of dry matter was 7.0 ± 0.1 g.
The methanolic extract was subjected to fractionation according to Singh et al. (2009) [130] with slight modifications. The extract (7.0 g) was dissolved in a methanol:water (9:1) mixture and the solution was successively divided into fractions with n-hexane, chloroform and n-butanol using a separatory funnel. Organic solvents were removed using a rotary evaporator, water from the final aqueous fraction was removed by lyophilization. The resulting dried pellets were dissolved in DMSO to a concentration of 50 mg/mL for n-hexane fraction and 100 mg/mL for chloroform, n-butanol and water fractions.
4.5. Gas Chromatography-Mass Spectrometry (GC-MS) Analysis of Methanolic Leaf Extract
Of the powdered lyophilized leaves, 5 g was extracted with 100 mL of methanol for 24 h at room temperature (23 ± 0.5 °C). The extract was filtered through 0.22 μm PTFE syringe filters (Merck Millipore, Burlington, MA, USA).
For GC-MS analysis, a GCMS-QP2010 Ultra (Shimadzu, Japan) system with a DB-5MS capillary column (5% diphenyl – 95% dimethylsiloxane copolymer, 60 m long, inner diameter 0.25 mm, film thickness of the stationary phase 0.25 μm) was used. The carrier gas (helium) flow rate was 1.38 mL/min. The temperature program was as follows: isothermal for 4 min at 100 °C, increased at 15 °C/min to 300 °C, isothermal for 26 min. The ionization voltage was 70 eV. The scanning speed was 3333 s over the 30–550 m/z range. For qualitative analysis of the essential oil components, the NISTO.5a mass spectra library was used.
4.6. Matrix-Assisted Laser Desorption/Ionization (MALDI) Time-of-Flight (TOF) Mass Spectrometry
Water fraction was subjected to proteomic analysis using MALDI-TOF mass spectrometry. The solution was centrifuged at 7000 g for 4 min. The supernatant (1 microliter) was deposited on the MALDI plate. Pretreated and untreated samples were overlaid with 1 microliter of matrix solution (saturated solution of α-cyano-4-hydroxycinnamic acid in 50% acetonitrile and 2.5% trifluoroacetic acid). The matrix sample was cocrystallized by air drying at room temperature. Measurements were performed with a Microflex mass spectrometer (Bruker Daltonik, Bremen, Germany) using Daltonics FlexControl software (version 3.3.64). Spectra were recorded in the positive linear mode (laser frequency, 60 Hz; ion source 1 voltage, 19.4 kV; ion source 2 voltage, 17.3 kV; lens voltage, 9.1 kV; mass range, 0 to 20,000 Da). The internal calibration was performed using the mass test standard MBT (Bruker Daltonics, Bremen, Germany). For each spectrum, 4000 shots from different positions of the target spot (automatic mode) were collected and analyzed. Protein identification was performed using the BIOPEP-UWM™ database [60].
4.7. Determination of Total Phenolics
The total phenolic content was measured according to Swain and Hillis method [131]. Then, 100 μL of a DMSO-dissolved fraction was mixed with 0.5 mL of the Folin–Denis’ reagent. After 3 min, 1 mL of 20% Na2CO3 was added, and volume of the mixture was brought to 10.0 mL with distilled water. After incubation in the dark for 90 min, absorbance of the resulting blue complex was measured at 750 nm using an SF-102 spectrophotometer (NPO Interfotofizika, Moscow, Russia). Gallic acid was used as a standard. The total phenolic content was expressed in mg equivalent of gallic acid per 1 mL of sample (mg GAEs/mL).
4.8. Determination of Total Tannins
The total tannin content was determined according to the Price and Butler method [132] with modifications. A DMSO dissolved extract was diluted 500-fold with distilled water to a concentration of 100–200 μg/mL. An aliquot of 0.5 mL of diluted sample was added to 1 mL of 1% FeCl3, then the volume was adjusted to 10 mL with distilled water. After 5 min incubation at room temperature, the optical density was measured at 720 nm. Tannin was used as a standard.
4.9. Determination of Total Flavonoids
The flavonoid content was studied with the aluminum chloride colorimetric method [133] with slight modifications. An aliquot of 50 μL of DMSO dissolved extract was mixed with 1.5 mL of ethanol, 100 μL of 10% aluminum chloride, 100 μL of 1M sodium acetate and 2.8 mL of distilled water. The resulting mixture was incubated at room temperature for 30 min in the dark, then absorbance at 415 nm was read. Quercetin was used as a standard. The total flavonoid content was expressed in mg equivalent of quercetin per 1 mL of sample (mg QEs/mL).
4.10. Determination of Chlorophyll a, Chlorophyll b, and Total Carotenoid
The content of chlorophylls a and b and total carotenoid was measured spectrophotometrically. The DMSO dissolved samples were diluted 1000-fold with 80% acetone and clarified with centrifugation at 10,000× g at 4 °C for 15 min. The absorbance of the supernatant was measured at 470 nm, 646.8 nm, and 663.2 nm, and the concentrations of chlorophyll a, chlorophyll b and carotenoids (μg/mL) were calculated using equations for 80% acetone as described [134].
4.11. Determination of Carbohydrates
Reducing sugars were measured with the use of alkaline picric acid method [135,136]. In brief, 1 mL of 1% picric acid was added to 0.5 mL of a test fraction, then 3 mL of 20% sodium carbonate was added. Samples were boiled for 30 min, cooled and adjusted to 10.0 mL by distilled water. The absorbance was read at a wavelength of 460 nm. Glucose was used as a standard.
4.12. Ferric Reducing Power Assay
The assay was carried out as described [137,138] with slight modifications. As such, 10 μL of DMSO dissolved fractions was mixed with 2 mL of 0.2 M sodium phosphate buffer, pH 6.6, and 1 mL of 1% potassium ferricyanide. The resulting mixture was incubated at 50 °C for 20 min. The reaction was terminated by addition of 1 mL of 10% trichloroacetic acid. The mixture was centrifuged at 3000× g for 10 min, then 0.5 mL of freshly prepared 0.1% FeCl3 was added to the supernatant, and the absorption was measured at 700 nm. Ascorbic acid was used as a standard. The reducing power was expressed in mg equivalent of ascorbic acid per 1 mL of sample (mg AAEs/mL).
4.13. Assessment of Total Antioxidant Activity (TAA)
The total antioxidant activity was assayed with the use of the phosphomolybdenum method [138,139]. As such, 50 μL of DMSO dissolved fractions was mixed with 4 mL of the reagent solution (0.6 M sulfuric acid, 28 mM sodium phosphate and 4 mM ammonium molybdenum). The mixture was incubated at 95 °C for 90 min, then cooled to room temperature. The absorbance was measured at 695 nm. Ascorbic acid was used as a standard. The TAA was expressed in mg equivalent of ascorbic acid per 1 mL of sample (mg AAEs/mL).
4.14. Trolox Equivalent Antioxidant Capacity (TEAC) Assay
The assay was carried out according to described by Piskov et al. (2020), Rzhepakovsky et al. (2021) method [140,141]. 2,29-azinobis-(3-ethylbenzothiazoline-6-sulfonic acid) (ABTS) was dissolved in water to a concentration of 7 mM. The ABTS•+ cationic radical generation was initiated by addition of 1 mL of 14.7 mM potassium persulfate to 5 mL of ABTS. The resulting mixture was kept in the dark at room temperature for 24 h before use. To perform the assay, the ABTS solution was diluted with distilled water to an optical density of 0.70 (±0.02) at 734 nm, then 5 μL of DMSO dissolved fractions were added to 2 mL of ABTS solution. The absorbance at 734 nm was measured 3 min after mixing. Trolox solution at a concentration of 1 mM was used as a standard. The antioxidant capacity was expressed in mg equivalent of Trolox per 1 mL of sample (mg TEs/mL).
4.15. Cytotoxicity Assay
Cancer cells HeLa (human cervical epithelioid carcinoma cell line, subclone M) and non-cancerous Vero cells (African green monkey renal epithelial cells) were purchased from the Russian Cell Culture Collection (Institute of Cytology RAS, St., Russia). The HeLa and Vero cells were grown in EMEM and DMEM media, respectively. The incubation media were supplemented with 10% fetal bovine serum, penicillin (100 U/mL) and streptomycin (100 µg/mL). The cells were cultured at 37 °C in a humidified atmosphere of 5% CO2. Cytotoxicity of C. comosum fractions was studied with the use of the MTT staining method [142]. Cells were plated in 96-well plates (5 × 103 cells/well). Then, 24 h after plating, growth medium was replaced by medium containing different quantities of fractions dissolved in DMSO. The final concentration of DMSO did not exceed 1%. Then, 24 h after addition of samples, 10 µL of MTT stock solution (5 mg/mL) was added into each well and plates were incubated for 4 h. The media were then removed and MTT formazan was dissolved in DMSO (100 µL/well). The absorption of the samples was read at 570 nm (reference wavelength 650 nm). MTT staining of control samples treated with DMSO was taken as 100%.
5. Conclusions
Our data demonstrate that methanolic extract of leaves of Chlorophytum comosum (Green type) (Thunb.) Jacques can be a source of a number of bioactive compounds including those that can be used as dietary supplements as well as constituents with broad biological activity and therapeutic potential. We have found that water fraction of the methanolic extract obtained after successive removal of n-hexane, chloroform and n-butanol soluble matter comprises compound(s) with high selectivity of cytotoxicity towards cancer cells. The exact nature of this antitumor potential has to be elucidated.
Acknowledgments
The work was carried out using the Center for Collective Use of the North Caucasus Federal University (NCFU) with the financial support of the Ministry of Education and Science of the Russian Federation (project RF ---- 2296.61321X0029, Agreement No. 075-15-2021-687).
Abbreviations
ABTS: 2,29-azinobis-(3-ethylbenzothiazoline-6-sulfonic acid); MTT, 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide; DMEM, Dulbecco’s modified Eagle medium; DMSO, dimethyl sulfoxide; EMEM, Eagle’s minimum essential medium; GC-MS, gas chromatography-mass spectrometry; MALDI TOF MS, matrix assisted laser desorption ionization time-of-flight mass spectrometry, TAA, total antioxidant activity; TEAC, Trolox equivalent antioxidant capacity.
Author Contributions
I.V.R. and D.A.A. designed and performed the experiment; S.S.A., N.V.F. and M.A.K. developed methodology and carried out the experiment; V.P.K. and L.D.T. provided intellectual support; A.V.K. and S.G.K. provided all material resources; M.N.S., A.A.T., M.M.T. and S.I.P. investigated all objects, prepared figures and tables and wrote the manuscript; W.D.G. and A.A.N. were involved in methodology and data analysis, writing and editing of the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
The work was carried out using the Center for Collective Use of the North Caucasus Federal University (NCFU) with the financial support of the Ministry of Education and Science of the Russian Federation (project RF ---- 2296.61321X0029, Agreement No. 075-15-2021-687). The study of cytotoxicity was carried out within the framework of the State Task of the Ministry of Science and Higher Education of the Russian Federation No. AAAA-A19-119092390041-5. Analytical research and methodology were performed under the contract No. AAAA-A19 119071890015-6 by the Ministry of Science and Higher Education of the Russian Federation. Chemicals and materials used in the work were obtained with financial support of InCom LLC.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data of the research is available is on request to the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Sample Availability
Samples of the research are available from the authors.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kaushik N. Saponins of Chlorophytum species. Phytochem. Rev. 2005;4:191–196. doi: 10.1007/s11101-005-2607-5. [DOI] [Google Scholar]
- 2.Patil S.M., Chandanshive V.V., Tamboli A.S., Adsul A.A., Yadav S.R., Govindwar S.P. Analysis of genetic variability in endemic medicinal plants of genus Chlorophytum from the Indian subcontinent using amplified fragment length polymorphism marker. Comptes Rendus Biol. 2015;338:838–845. doi: 10.1016/j.crvi.2015.09.006. [DOI] [PubMed] [Google Scholar]
- 3.Munyao J.N., Dong X., Yang J.-X., Mbandi E.M., Wanga V.O., Oulo M.A., Saina J.K., Musili P.M., Hu G.-W. Complete Chloroplast Genomes of Chlorophytum comosum and Chlorophytum gallabatense: Genome Structures, Comparative and Phylogenetic Analysis. Plants. 2020;9:296. doi: 10.3390/plants9030296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Deore S.L., Jajoo N.B., Chittam K.P., Deshmukh T.A. Comparative Pharmacognostic, Phytochemical and Biological evaluation between five Chlorophytum species. Pharmacogn. J. 2015;7:317–325. doi: 10.5530/pj.2015.5.12. [DOI] [Google Scholar]
- 5.Khare C.P. Indian Medicinal Plants. In: Khare C.P., editor. An Illustrated Dictionary. Springer; Berlin/Heidelberg, Germany: 2007. p. 68. [DOI] [Google Scholar]
- 6.Yang X., Chen A., Ma Y., Gao Y., Gao Z., Fu B., Sun F., Qiao J., Li Q., Wan S., et al. Encyclopedic Reference of Traditional Chinese Medicine. Springer; Berlin/Heidelberg, Germany: 2007. p. 567. [DOI] [Google Scholar]
- 7.Fan C., Jin H., Wu L., Zhang Y., Ye R.D., Zhang W., Zhang Y. An Exploration of Traditional Chinese Medicinal Plants with Anti-Inflammatory Activities. Evid. Based. Complement. Alternat. Med. 2017;2017:1231820. doi: 10.1155/2017/1231820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tabuti J.R., Lye K.A., Dhillion S.S. Traditional herbal drugs of Bulamogi, Uganda: Plants, use and administration. J. Ethnopharmacol. 2003;88:19–44. doi: 10.1016/S0378-8741(03)00161-2. [DOI] [PubMed] [Google Scholar]
- 9.Vijaya N.K., Chavan P.D. Chlorophytum borivilianum (Safed musli): A Review. Pharmacogn. Rev. 2009;3:154–169. [Google Scholar]
- 10.Chauhan R., Quraishi A., Jadhav S.K., Keshavkant S. A comprehensive review on pharmacological properties and biotechnological aspects of Genus Chlorophytum. Acta Physiol. Plant. 2016;38:116. doi: 10.1007/s11738-016-2132-8. [DOI] [Google Scholar]
- 11.Thakur M., Bhargava S., Dixit V.K. Immunomodulatory Activity of Chlorophytum borivilianum Sant. F. Evid. Based Complement. Alternat. Med. 2007;4:419–423. doi: 10.1093/ecam/nel094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Giri S.S., Sen S.S., Chi C., Kim H.J., Yun S., Park S.C., Sukumaran V. Chlorophytum borivilianum Polysaccharide Fraction Provokes the Immune Function and Disease Resistance of Labeo rohita against Aeromonas hydrophila. J. Immunol. Res. 2015;2015:256510. doi: 10.1155/2015/256510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kaur R., Kaur S. Protective efficacy of Chlorophytum borivilianum root extract against murine visceral leishmaniasis by immunomodulating the host responses. J. Ayurveda Integr. Med. 2020;11:53–61. doi: 10.1016/j.jaim.2017.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thakur M., Connellan P., Deseo M.A., Morris C., Dixit V.K. Immunomodulatory Polysaccharide from Chlorophytum borivilianum Roots. Evid. Based Complement. Alternat. Med. 2011;2011:598521. doi: 10.1093/ecam/neq012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kanwar A.S., Bhutani K.K. Effects of Chlorophytum arundinaceum, Asparagus adscendens and Asparagus racemosus on pro-inflammatory cytokine and corticosterone levels produced by stress. Phytother. Res. 2010;24:1562–1566. doi: 10.1002/ptr.3218. [DOI] [PubMed] [Google Scholar]
- 16.Lande A.A., Ambavade S.D., Swami U.S., Adkar P.P., Ambavade P.D., Waghamare A.B. Saponins isolated from roots of Chlorophytum borivilianum reduce acute and chronic inflammation and histone deacetylase. J. Integr. Med. 2015;13:25–33. doi: 10.1016/S2095-4964(15)60157-1. [DOI] [PubMed] [Google Scholar]
- 17.O’Donnell G., Bucar F., Gibbons S. Phytochemistry and antimycobacterial activity of Chlorophytum inornatum. Phytochemistry. 2006;67:178–182. doi: 10.1016/j.phytochem.2005.10.023. [DOI] [PubMed] [Google Scholar]
- 18.Abubakar A., Nazifi A.B., Odoma S., Shehu S., Danjuma N.M. Antinociceptive activity of methanol extract of Chlorophytum alismifolium tubers in murine model of pain: Possible involvement of α2-adrenergic receptor and KATP channels. J. Tradit. Complement. Med. 2019;10:1–6. doi: 10.1016/j.jtcme.2019.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Visavadiya N.P., Soni B., Dalwadi N., Madamwar D. Chlorophytum borivilianum as potential terminator of free radicals in various in vitro oxidation systems. Drug. Chem. Toxicol. 2010;33:173–182. doi: 10.3109/01480540903311068. [DOI] [PubMed] [Google Scholar]
- 20.Sharma G., Kumar M. Antioxidant and modulatory role of Chlorophytum borivilianum against arsenic induced testicular impairment. J. Environ. Sci. 2012;24:2159–2165. doi: 10.1016/S1001-0742(11)61019-X. [DOI] [PubMed] [Google Scholar]
- 21.Narasimhan S., Govindarajan R., Vijayakumar M., Mehrotra S. Free radical scavenging potential of Chlorophytum tuberosum Baker. J. Ethnopharmacol. 2006;104:423–425. doi: 10.1016/j.jep.2005.09.029. [DOI] [PubMed] [Google Scholar]
- 22.Ashraf M.F., Abd Aziz M., Stanslas J., Ismail I., Abdul Kadir M. Assessment of antioxidant and cytotoxicity activities of saponin and crude extracts of Chlorophytum borivilianum. Sci. World J. 2013;2013:216894. doi: 10.1155/2013/216894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kenjale R.D., Shah R.K., Sathaye S.S. Anti-stress and anti-oxidant effects of roots of Chlorophytum borivilianum (Santa Pau & Fernandes) Indian J. Exp. Biol. 2007;45:974–979. [PubMed] [Google Scholar]
- 24.Narasimhan S., Govindarajan R., Madhavan V., Thakur M., Dixit V.K., Mehrotra S., Madhusudanan K.P. Action of (2-->1)Fructo-oligopolysaccharide fraction of Chlorophytum borivilianum against Streptozotocin-Induced oxidative stress. Planta Med. 2006;72:1421–1424. doi: 10.1055/s-2006-951705. [DOI] [PubMed] [Google Scholar]
- 25.Kumar M., Meena P., Verma S., Kumar M., Kumar A. Anti-tumour, anti-mutagenic and chemomodulatory potential of Chlorophytum borivilianum. Asian Pac. J. Cancer Prev. 2010;11:327–334. [PubMed] [Google Scholar]
- 26.Shinde S.S., Patil S.M., Rane N.R., Adsul A.A., Gholve A.R., Pawar P.K., Yadav S.R., Govindwar S.P. Comprehensive investigation of free radical quenching potential, total phenol, flavonoid and saponin content, and chemical profiles of twelve Chlorophytum Ker Gawl species. Indian J. Nat. Prod. Resour. 2016;7:125–134. [Google Scholar]
- 27.Thakur M., Thompson D., Connellan P., Deseo M.A., Morris C., Dixit V.K. Improvement of penile erection, sperm count and seminal fructose levels in vivo and nitric oxide release in vitro by ayurvedic herbs. Andrologia. 2011;43:273–277. doi: 10.1111/j.1439-0272.2010.01068.x. [DOI] [PubMed] [Google Scholar]
- 28.Mahajan G.K., Mahajan A.Y., Mahajan R.T. Efficacy of aphrodisiac plants towards improvement in semen quality and motility in infertile males. J. Complement. Integr. Med. 2012;9:6. doi: 10.1515/1553-3840.1520. [DOI] [PubMed] [Google Scholar]
- 29.Rath S.K., Panja A.K. Clinical evaluation of root tubers of Shweta Musali (Chlorophytum borivilianum L.) and its effect on semen and testosterone. Ayu. 2013;34:273–275. doi: 10.4103/0974-8520.123118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kenjale R., Shah R., Sathaye S. Effects of Chlorophytum borivilianum on sexual behaviour and sperm count in male rats. Phytother. Res. 2008;22:796–801. doi: 10.1002/ptr.2369. [DOI] [PubMed] [Google Scholar]
- 31.Ray S., Chatterjee K., De D., Ghosh D. Bioefficacy of hydromethanolic extract of tuber of Chlorophytum borivilianum (Safed Musli) for the management of male infertility in cyproterone acetate-treated albino rats. Andrologia. 2014;46:659–671. doi: 10.1111/and.12133. [DOI] [PubMed] [Google Scholar]
- 32.Thakur M., Chauhan N.S., Bhargava S., Dixit V.K. A comparative study on aphrodisiac activity of some ayurvedic herbs in male albino rats. Arch. Sex. Behav. 2009;38:1009–1015. doi: 10.1007/s10508-008-9444-8. [DOI] [PubMed] [Google Scholar]
- 33.Thakur M., Bhargava S., Praznik W., Loeppert R., Dixit V.K. Effect of Chlorophytum borivilianum Santapau and Fernandes on sexual dysfunction in hyperglycemic male rats. Chin. J. Integr. Med. 2009;15:448–453. doi: 10.1007/s11655-009-0448-6. [DOI] [PubMed] [Google Scholar]
- 34.Das S., Singhal S., Kumar N., Rao C.M., Sumalatha S., Dave J., Dave R., Nandakumar K. Standardised extract of Safed Musli (Chlorophytum borivilianum) increases aphrodisiac potential besides being safe in male Wistar rats. Andrologia. 2016;48:1236–1243. doi: 10.1111/and.12567. [DOI] [PubMed] [Google Scholar]
- 35.Giribabu N., Kumar K.E., Rekha S.S., Muniandy S., Salleh N. Chlorophytum borivilianum (Safed Musli) root extract prevents impairment in characteristics and elevation of oxidative stress in sperm of streptozotocin-induced adult male diabetic Wistar rats. BMC Complementary Altern. Med. 2014;14:291. doi: 10.1186/1472-6882-14-291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Giribabu N., Kumar K.E., Rekha S.S., Muniandy S., Salleh N. Chlorophytum borivilianum root extract maintains near normal blood glucose, insulin and lipid profile levels and prevents oxidative stress in the pancreas of streptozotocin-induced adult male diabetic rats. Int. J. Med. Sci. 2014;11:1172–1784. doi: 10.7150/ijms.9056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lakshmi V., Kumar R., Pandey K., Joshi B.S., Roy R., Madhusudanan K.P., Tiwari P., Srivastava A.K. Structure and activities of a steroidal saponin from Chlorophytum nimonii (Grah) Dalz. Nat. Prod. Res. 2009;23:963–972. doi: 10.1080/14786410902986597. [DOI] [PubMed] [Google Scholar]
- 38.Visavadiya N.P., Narasimhacharya A.V. Ameliorative effect of Chlorophytum borivilianum root on lipid metabolism in hyperlipaemic rats. Clin. Exp. Pharmacol. Physiol. 2007;34:244–249. doi: 10.1111/j.1440-1681.2007.04579.x. [DOI] [PubMed] [Google Scholar]
- 39.Areshidze D.A., Timchenko L.D., Gulyukin M.I., Kozlova M.A., Rzhepakovsky I.V., Syomin I.A., Andreyuk V.A. Hepatoprotective effect of preparations produced from Chlorophytum comosum (L.) at experimental toxic damage in wistar rats. Pharmacologyonline. 2016;2:81–90. [Google Scholar]
- 40.Areshidze D., Timchenko L., Kozlova M. The use of enzymatic hydrolyzate of Chlorophytum comosum with experimental toxic liver damage in rats. Am. J. Biomed. Sci. Res. 2013;1:32–36. doi: 10.11648/j.ajbls.20130101.16. [DOI] [Google Scholar]
- 41.Matsushita H., Kuwabara H., Ishikawa S., Mochizuki M. Apoptosis Induced in Human Cell Lines by a Butanol Extract from Chlorophytum comosum Roots. J. Health Sci. 2005;51:341–345. doi: 10.1248/jhs.51.341. [DOI] [Google Scholar]
- 42.Tandon M., Shukla Y.N. A bibenzyl xyloside from Chlorophytum arundinaceum. Phytochemistry. 1993;32:1624–1625. doi: 10.1016/0031-9422(93)85195-W. [DOI] [Google Scholar]
- 43.Deore S.L., Khadabadi S.S. Isolation and characterization of phytoconstituents from Chlorophytum borivilianum. Pharmacogn. Res. 2010;2:343–349. doi: 10.4103/0974-8490.75452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Patil V.N., Deokule S.S. Pharmacognostic study of Chlorophytum tuberosum Baker. Int. J. Ayurveda Res. 2010;1:237–242. doi: 10.4103/0974-7788.76788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tandon M., Shukla Y.N., Thakur R.S. 4-hydroxy-8,11-oxidoheneicosanol and other constituents from Chlorophytum arundinaceum roots. Phytochemistry. 1992;31:2525–2526. doi: 10.1016/0031-9422(92)83315-P. [DOI] [Google Scholar]
- 46.Mimaki Y., Kanmoto T., Sashida Y., Nishino A., Satomi Y., Nishino H. Steroidal saponins from the underground parts of Chlorophytum comosum and their inhibitory activity on tumour promoter-induced phospholipids metabolism of HeLa cells. Phytochemistry. 1996;41:1405–1410. doi: 10.1016/0031-9422(95)00789-X. [DOI] [PubMed] [Google Scholar]
- 47.Rizvi M.Z., Kukreja A.K., Bisht N.S. In vitro propagation of an endangered medicinal herb Chlorophytum borivilianum Sant. et Fernand. through somatic embryogenesis. Physiol. Mol. Biol. Plants. 2010;16:249–257. doi: 10.1007/s12298-010-0026-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Qiu S.X., Li X.C., Xiong Y., Dong Y., Chai H., Fransworth N.R., Pezzuto J.M., Fong H.H. Isolation and characterization of cytotoxic saponin chloromaloside A from Chlorophytum malayense. Planta Med. 2000;66:587–590. doi: 10.1055/s-2000-8600. [DOI] [PubMed] [Google Scholar]
- 49.Acharya D., Mitaine-Offer A.C., Kaushik N., Miyamoto T., Paululat T., Mirjolet J.F., Duchamp O., Lacaille-Dubois M.A. Cytotoxic spirostane-type saponins from the roots of Chlorophytum borivilianum. J. Nat. Prod. 2009;72:177–181. doi: 10.1021/np800559z. [DOI] [PubMed] [Google Scholar]
- 50.Sharma R., Thakur G.S., Sanodiya B.S., Pandey M., Bisen P.S. Saponin: A Wonder Drug from Chlorophytum Species. Glob. J. Res. Med. Plants Indig. Med. 2012;1:503–515. [Google Scholar]
- 51.Tabopda T.K., Mitaine-Offer A.C., Paululat T., Delemasure S., Dutartre P., Ngadjui B.T., Lacaille-Dubois M.A. Steroidal saponins from Chlorophytum deistelianum. Phytochemistry. 2016;126:34–40. doi: 10.1016/j.phytochem.2016.03.003. [DOI] [PubMed] [Google Scholar]
- 52.Acharya D., Mitaine-Offer A.C., Kaushik N., Miyamoto T., Paululat T., Mirjolet J.F., Duchamp O., Lacaille-Dubois M.A. Steroidal saponins from Chlorophytum orchidastrum. J. Nat. Prod. 2010;73:7–11. doi: 10.1021/np900443q. [DOI] [PubMed] [Google Scholar]
- 53.Kumar S., Kalra S., Kumar S., Kaur J., Singh K. Differentially expressed transcripts from leaf and root tissue of Chlorophytum borivilianum: A plant with high medicinal value. Gene. 2012;511:79–87. doi: 10.1016/j.gene.2012.09.046. [DOI] [PubMed] [Google Scholar]
- 54.Chakraborthy G.S. Antioxidant Activity of the Successive Extracts of Chlorophytum borivilianum Leaves. Asian J. Chem. 2008;20:5782–5784. [Google Scholar]
- 55.Joshi A., Chauhan R.S. Cytotoxicity studies of Chlorophytum borivilianum against BHK-21 cells. J. Biol. Chem. Res. 2013;30:302–309. [Google Scholar]
- 56.Dill V., Pfaff F., Zimmer A., Beer M., Eschbaumer M. Adherent and suspension baby hamster kidney cells have a different cytoskeleton and surface receptor repertoire. PLoS ONE. 2021;16:e0246610. doi: 10.1371/journal.pone.0246610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Adhami S., Farooqi H., Abdin M.Z., Prasad R., Malik A.A. Chemical Profiling of Chlorophytum comosum (Thunb.) Jaques by GCMS/LC-ESI-MS and its Antiproliferative Effects on Human Carcinoma Cell Lines. Anticancer Agents Med. Chem. 2020;21:1697–1707. doi: 10.2174/1871520620666201123085300. [DOI] [PubMed] [Google Scholar]
- 58.Pandey P., Bajpai P., Siddiqui M.H., Sayyed U., Tiwari R., Shekh R., Mishra K., Kapoor V.K. Elucidation of the Chemopreventive Role of Stigmasterol Against Jab1 in Gall Bladder Carcinoma. Endocr. Metab. Immune Disord. Drug Targets. 2019;19:826–837. doi: 10.2174/1871530319666190206124120. [DOI] [PubMed] [Google Scholar]
- 59.Tetko I.V., Poda G.I. Application of ALOGPS 2.1 to predict log D distribution coefficient for Pfizer proprietary compounds. J. Med. Chem. 2004;47:5601–5604. doi: 10.1021/jm049509l. [DOI] [PubMed] [Google Scholar]
- 60.Minkiewicz P., Iwaniak A., Darewicz M. BIOPEP-UWM Database of Bioactive Peptides: Current Opportunities. Int. J. Mol. Sci. 2019;20:5978. doi: 10.3390/ijms20235978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Jandacek R.J. Linoleic Acid: A Nutritional Quandary. Healthcare. 2017;5:25. doi: 10.3390/healthcare5020025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Choque B., Catheline D., Rioux V., Legrand P. Linoleic acid: Between doubts and certainties. Biochimie. 2014;96:14–21. doi: 10.1016/j.biochi.2013.07.012. [DOI] [PubMed] [Google Scholar]
- 63.Carta G., Murru E., Banni S., Manca C. Palmitic Acid: Physiological Role, Metabolism and Nutritional Implications. Front Physiol. 2017;8:902. doi: 10.3389/fphys.2017.00902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Van Rooijen M.A., Mensink R.P. Palmitic Acid Versus Stearic Acid: Effects of Interesterification and Intakes on Cardiometabolic Risk Markers—A Systematic Review. Nutrients. 2020;12:615. doi: 10.3390/nu12030615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Sampath H., Ntambi J.M. The fate and intermediary metabolism of stearic acid. Lipids. 2005;40:1187–1191. doi: 10.1007/s11745-005-1484-z. [DOI] [PubMed] [Google Scholar]
- 66.Qi X., Tester R.F. Lactose, Maltose, and Sucrose in Health and Disease. Mol. Nutr. Food Res. 2020;64:e1901082. doi: 10.1002/mnfr.201901082. [DOI] [PubMed] [Google Scholar]
- 67.Kluch M., Socha-Banasiak A., Pacześ K., Borkowska M., Czkwianianc E. The role of disaccharidases in the digestion—Diagnosis and significance of their deficiency in children and adults. Pol Merkur Lek. 2020;49:275–278. [PubMed] [Google Scholar]
- 68.McCall J.M., DeCristofaro C., Elliott L. Oral sucrose for pain control in nonneonate infants during minor painful procedures. J. Am. Assoc. Nurse Pract. 2013;25:244–252. doi: 10.1111/j.1745-7599.2012.00783.x. [DOI] [PubMed] [Google Scholar]
- 69.Puertolas M.V., Fifi A.C. The Role of Disaccharidase Deficiencies in Functional Abdominal Pain Disorders-A Narrative Review. Nutrients. 2018;10:1835. doi: 10.3390/nu10121835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Bhardwaj M., Sali V.K., Mani S., Vasanthi H.R. Neophytadiene from Turbinaria ornata Suppresses LPS-Induced Inflammatory Response in RAW 264.7 Macrophages and Sprague Dawley Rats. Inflammation. 2020;43:937–950. doi: 10.1007/s10753-020-01179-z. [DOI] [PubMed] [Google Scholar]
- 71.Balamurugan R., Duraipandiyan V., Ignacimuthu S. Antidiabetic activity of γ-sitosterol isolated from Lippia nodiflora L. in streptozotocin induced diabetic rats. Eur. J. Pharmacol. 2011;667:410–418. doi: 10.1016/j.ejphar.2011.05.025. [DOI] [PubMed] [Google Scholar]
- 72.Li K., Yuan D., Yan R., Meng L., Zhang Y., Zhu K. Stigmasterol exhibits potent antitumor effects in human gastric cancer cells mediated via inhibition of cell migration, cell cycle arrest, mitochondrial mediated apoptosis and inhibition of JAK/STAT signalling pathway. J. BUON. 2018;23:1420–1425. [PubMed] [Google Scholar]
- 73.Kangsamaksin T., Chaithongyot S., Wootthichairangsan C., Hanchaina R., Tangshewinsirikul C., Svasti J. Lupeol and stigmasterol suppress tumor angiogenesis and inhibit cholangiocarcinoma growth in mice via downregulation of tumor necrosis factor-α. PLoS ONE. 2017;12:e0189628. doi: 10.1371/journal.pone.0189628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ali H., Dixit S., Ali D., Alqahtani S.M., Alkahtani S., Alarifi S. Isolation and evaluation of anticancer efficacy of stigmasterol in a mouse model of DMBA-induced skin carcinoma. Drug Des. Devel. Ther. 2015;9:2793–2800. doi: 10.2147/DDDT.S83514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Feng S., Dai Z., Liu A.B., Huang J., Narsipur N., Guo G., Yang C.S. Intake of stigmasterol and β-sitosterol alters lipid metabolism and alleviates NAFLD in mice fed a high-fat western-style diet. Biochim. Biophys. Acta Mol. Cell Biol. Lipids. 2018;1863:1274–1284. doi: 10.1016/j.bbalip.2018.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Batta A.K., Xu G., Honda A., Miyazaki T., Salen G. Stigmasterol reduces plasma cholesterol levels and inhibits hepatic synthesis and intestinal absorption in the rat. Metabolism. 2006;55:292–299. doi: 10.1016/j.metabol.2005.08.024. [DOI] [PubMed] [Google Scholar]
- 77.Chandler R.F., Hooper S.N., Ismail H.A. Antihypercholesterolemic studies with sterols: Beta-sitosterol and stigmasterol. J. Pharm. Sci. 1979;68:245–247. doi: 10.1002/jps.2600680235. [DOI] [PubMed] [Google Scholar]
- 78.Andriamiarina R., Laraki L., Pelletier X., Debry G. Effects of stigmasterol-supplemented diets on fecal neutral sterols and bile acid excretion in rats. Ann. Nutr. Metab. 1989;33:297–303. doi: 10.1159/000177548. [DOI] [PubMed] [Google Scholar]
- 79.Li C., Liu Y., Xie Z., Lu Q., Luo S. Stigmasterol protects against Ang II-induced proliferation of the A7r5 aortic smooth muscle cell-line. Food Funct. 2015;6:2266–2272. doi: 10.1039/C5FO00031A. [DOI] [PubMed] [Google Scholar]
- 80.Lifsey H.C., Kaur R., Thompson B.H., Bennett L., Temel R.E., Graf G.A. Stigmasterol stimulates transintestinal cholesterol excretion independent of liver X receptor activation in the small intestine. J. Nutr. Biochem. 2020;76:108263. doi: 10.1016/j.jnutbio.2019.108263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Panda S., Jafri M., Kar A., Meheta B.K. Thyroid inhibitory, antiperoxidative and hypoglycemic effects of stigmasterol isolated from Butea monosperma. Fitoterapia. 2009;80:123–126. doi: 10.1016/j.fitote.2008.12.002. [DOI] [PubMed] [Google Scholar]
- 82.Wang J., Huang M., Yang J., Ma X., Zheng S., Deng S., Huang Y., Yang X., Zhao P. Anti-diabetic activity of stigmasterol from soybean oil by targeting the GLUT4 glucose transporter. Food Nutr. Res. 2017;61:1364117. doi: 10.1080/16546628.2017.1364117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Lim J.C., Park J.H., Budesinsky M., Kasal A., Han Y.H., Koo B.S., Lee S.I., Lee D.U. Antimutagenic constituents from the thorns of Gleditsia sinensis. Chem. Pharm. Bull. 2005;53:561–564. doi: 10.1248/cpb.53.561. [DOI] [PubMed] [Google Scholar]
- 84.Aminu R., Umar I.A., Rahman M.A., Ibrahim M.A. Stigmasterol retards the proliferation and pathological features of Trypanosoma congolense infection in rats and inhibits trypanosomal sialidase in vitro and in silico. Biomed. Pharmacother. 2017;89:482–489. doi: 10.1016/j.biopha.2017.02.068. [DOI] [PubMed] [Google Scholar]
- 85.Walker C.I.B., Oliveira S.M., Tonello R., Rossato M.F., da Silva Brum E., Ferreira J., Trevisan G. Anti-nociceptive effect of stigmasterol in mouse models of acute and chronic pain. Naunyn Schmiedeberg Arch. Pharmacol. 2017;390:1163–1172. doi: 10.1007/s00210-017-1416-x. [DOI] [PubMed] [Google Scholar]
- 86.Chen W.P., Yu C., Hu P.F., Bao J.P., Tang J.L., Wu L.D. Stigmasterol blocks cartilage degradation in rabbit model of osteoarthritis. Acta Biochim. Pol. 2012;59:537–541. doi: 10.18388/abp.2012_2088. [DOI] [PubMed] [Google Scholar]
- 87.Gabay O., Sanchez C., Salvat C., Chevy F., Breton M., Nourissat G., Wolf C., Jacques C., Berenbaum F. Stigmasterol: A phytosterol with potential anti-osteoarthritic properties. Osteoarthr. Cartil. 2010;18:106–116. doi: 10.1016/j.joca.2009.08.019. [DOI] [PubMed] [Google Scholar]
- 88.Antwi A.O., Obiri D.D., Osafo N., Essel L.B., Forkuo A.D., Atobiga C. Stigmasterol Alleviates Cutaneous Allergic Responses in Rodents. Biomed. Res. Int. 2018;2018:3984068. doi: 10.1155/2018/3984068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Antwi A.O., Obiri D.D., Osafo N. Stigmasterol Modulates Allergic Airway Inflammation in Guinea Pig Model of Ovalbumin-Induced Asthma. Mediat. Inflamm. 2017;2017:2953930. doi: 10.1155/2017/2953930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Antwi A.O., Obiri D.D., Osafo N., Forkuo A.D., Essel L.B. Stigmasterol inhibits lipopolysaccharide-induced innate immune responses in murine models. Int. Immunopharmacol. 2017;53:105–113. doi: 10.1016/j.intimp.2017.10.018. [DOI] [PubMed] [Google Scholar]
- 91.Ahmad Khan M., Sarwar A.H.M.G., Rahat R., Ahmed R.S., Umar S. Stigmasterol protects rats from collagen induced arthritis by inhibiting proinflammatory cytokines. Int. Immunopharmacol. 2020;85:106642. doi: 10.1016/j.intimp.2020.106642. [DOI] [PubMed] [Google Scholar]
- 92.Sun J., Li X., Liu J., Pan X., Zhao Q. Stigmasterol Exerts Neuro-Protective Effect Against Ischemic/Reperfusion Injury Through Reduction Of Oxidative Stress And Inactivation Of Autophagy. Neuropsychiatr. Dis. Treat. 2019;15:2991–3001. doi: 10.2147/NDT.S220224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Liang Q., Yang J., He J., Chen X., Zhang H., Jia M., Liu K., Jia C., Pan Y., Wei J. Stigmasterol alleviates cerebral ischemia/reperfusion injury by attenuating inflammation and improving antioxidant defenses in rats. Biosci Rep. 2020;40:BSR20192133. doi: 10.1042/BSR20192133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Adebiyi O.E., Olopade J.O., Olayemi F.O. Sodium metavanadate induced cognitive decline, behavioral impairments, oxidative stress and down regulation of myelin basic protein in mice hippocampus: Ameliorative roles of β-spinasterol, and stigmasterol. Brain Behav. 2018;8:e01014. doi: 10.1002/brb3.1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Haque M.N., Moon I.S. Stigmasterol promotes neuronal migration via reelin signaling in neurosphere migration assays. Nutr. Neurosci. 2020;23:679–687. doi: 10.1080/1028415X.2018.1544970. [DOI] [PubMed] [Google Scholar]
- 96.Haque M.N., Bhuiyan M.M.H., Moon I.S. Stigmasterol activates Cdc42-Arp2 and Erk1/2-Creb pathways to enrich glutamatergic synapses in cultures of brain neurons. Nutr. Res. 2018;56:71–78. doi: 10.1016/j.nutres.2018.04.022. [DOI] [PubMed] [Google Scholar]
- 97.Haque M.N., Moon I.S. Stigmasterol upregulates immediate early genes and promotes neuronal cytoarchitecture in primary hippocampal neurons as revealed by transcriptome analysis. Phytomedicine. 2018;46:164–175. doi: 10.1016/j.phymed.2018.04.012. [DOI] [PubMed] [Google Scholar]
- 98.Park S.J., Kim D.H., Jung J.M., Kim J.M., Cai M., Liu X., Hong J.G., Lee C.H., Lee K.R., Ryu J.H. The ameliorating effects of stigmasterol on scopolamine-induced memory impairments in mice. Eur. J. Pharmacol. 2012;676:64–70. doi: 10.1016/j.ejphar.2011.11.050. [DOI] [PubMed] [Google Scholar]
- 99.Tao C., Shkumatov A.A., Alexander S.T., Ason B.L., Zhou M. Stigmasterol accumulation causes cardiac injury and promotes mortality. Commun. Biol. 2019;2:20. doi: 10.1038/s42003-018-0245-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Islam M.T., de Alencar M.V., da Conceição Machado K., da Conceição Machado K., de Carvalho Melo-Cavalcante A.A., de Sousa D.P., de Freitas R.M. Phytol in a pharma-medico-stance. Chem. Biol. Interact. 2015;240:60–73. doi: 10.1016/j.cbi.2015.07.010. [DOI] [PubMed] [Google Scholar]
- 101.McGinty D., Letizia C.S., Api A.M. Fragrance material review on phytol. Food Chem. Toxicol. 2010;48:S59–S63. doi: 10.1016/j.fct.2009.11.012. [DOI] [PubMed] [Google Scholar]
- 102.Farag M.R., Alagawany M., Bin-Jumah M., Othman S.I., Khafaga A.F., Shaheen H.M., Samak D., Shehata A.M., Allam A.A., Abd El-Hack M.E. The Toxicological Aspects of the Heat-Borne Toxicant 5-Hydroxymethylfurfural in Animals: A Review. Molecules. 2020;25:1941. doi: 10.3390/molecules25081941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Shapla U.M., Solayman M., Alam N., Khalil M.I., Gan S.H. 5-Hydroxymethylfurfural (HMF) levels in honey and other food products: Effects on bees and human health. Chem. Cent. J. 2018;12:35. doi: 10.1186/s13065-018-0408-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Arnous A., Makris D.P., Kefalas P. Effect of principal polyphenolic components in relation to antioxidant characteristics of aged red wines. J. Agric. Food Chem. 2001;49:5736–5742. doi: 10.1021/jf010827s. [DOI] [PubMed] [Google Scholar]
- 105.Petropoulos S.A., Fernandes A., Barros L., Ferreira I.C. A comparison of the phenolic profile and antioxidant activity of different Cichorium spinosum L. ecotypes. J. Sci. Food Agric. 2018;98:183–189. doi: 10.1002/jsfa.8453. [DOI] [PubMed] [Google Scholar]
- 106.Gartler S.M. Apparent Hela cell contamination of human heteroploid cell lines. Nature. 1968;217:750–751. doi: 10.1038/217750a0. [DOI] [PubMed] [Google Scholar]
- 107.Lavappa K.S. Survey of ATCC stocks of human cell lines for HeLa contamination. In Vitro. 1978;14:469–475. doi: 10.1007/BF02616110. [DOI] [PubMed] [Google Scholar]
- 108.Smith K.R., Hayat F., Andrews J.F., Migaud M.E., Gassman N.R. Dihydroxyacetone Exposure Alters NAD(P)H and Induces Mitochondrial Stress and Autophagy in HEK293T Cells. Chem. Res. Toxicol. 2019;32:1722–1731. doi: 10.1021/acs.chemrestox.9b00230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Smith K.R., Granberry M., Tan M.C.B., Daniel C.L., Gassman N.R. Dihydroxyacetone induces G2/M arrest and apoptotic cell death in A375P melanoma cells. Environ. Toxicol. 2018;33:333–342. doi: 10.1002/tox.22520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Petersen A.B., Wulf H.C., Gniadecki R., Gajkowska B. Dihydroxyacetone, the active browning ingredient in sunless tanning lotions, induces DNA damage, cell-cycle block and apoptosis in cultured HaCaT keratinocytes. Mutat. Res. 2004;560:173–186. doi: 10.1016/j.mrgentox.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 111.Perer J., Jandova J., Fimbres J., Jennings E.Q., Galligan J.J., Hua A., Wondrak G.T. The sunless tanning agent dihydroxyacetone induces stress response gene expression and signaling in cultured human keratinocytes and reconstructed epidermis. Redox Biol. 2020;36:101594. doi: 10.1016/j.redox.2020.101594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Janzowski C., Glaab V., Samimi E., Schlatter J., Eisenbrand G. 5-Hydroxymethylfurfural: Assessment of mutagenicity, DNA-damaging potential and reactivity towards cellular glutathione. Food Chem. Toxicol. 2000;38:801–809. doi: 10.1016/S0278-6915(00)00070-3. [DOI] [PubMed] [Google Scholar]
- 113.Severin I., Dumont C., Jondeau-Cabaton A., Graillot V., Chagnon M.C. Genotoxic activities of the food contaminant 5-hydroxymethylfurfural using different in vitro bioassays. Toxicol. Lett. 2010;192:189–194. doi: 10.1016/j.toxlet.2009.10.022. [DOI] [PubMed] [Google Scholar]
- 114.Hou Y.N., Wang Y.R., Zheng C.H., Feng K. Biotransformation of 5-hydroxymethylfurfural into 2,5-dihydroxymethylfuran by Ganoderma sessile and toxicological assessment of both compounds. AMB Express. 2020;10:88. doi: 10.1186/s13568-020-01023-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Nemes D., Kovacs R., Nagy F., Mezo M., Poczok N., Ujhelyi Z., Peto A., Feher P., Fenyvesi F., Varadi J., et al. Interaction between Different Pharmaceutical Excipients in Liquid Dosage Forms-Assessment of Cytotoxicity and Antimicrobial Activity. Molecules. 2018;23:1827. doi: 10.3390/molecules23071827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Davidson A.F., Glasscock C., McClanahan D.R., Benson J.D., Higgins A.Z. Toxicity Minimized Cryoprotectant Addition and Removal Procedures for Adherent Endothelial Cells. PLoS ONE. 2015;10:e0142828. doi: 10.1371/journal.pone.0142828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Hossler P., McDermott S., Racicot C., Chumsae C., Raharimampionona H., Zhou Y., Ouellette D., Matuck J., Correia I., Fann J., et al. Cell culture media supplementation of uncommonly used sugars sucrose and tagatose for the targeted shifting of protein glycosylation profiles of recombinant protein therapeutics. Biotechnol. Prog. 2014;30:1419–1431. doi: 10.1002/btpr.1968. [DOI] [PubMed] [Google Scholar]
- 118.Yu Y.C., Yu M.M. Mass spectrum of Heterocycloalkanes of Rhodiola Rosea. 2018. [(accessed on 17 December 2021)]. Available online: https://www.researchgate.net/publication/328447521_Mass_spectrum_of_Heterocycloalkanes_of_Rhodiola_Rosea_hongjingtian?channel=doi&linkId=5bce9a2b4585152b144ebadb&showFulltext=true.
- 119.Clingman A.L., Richtmyer N.K. Aryl Thioglycopyranosides, Aryl Glycopyranosyl Sulfones, and the Novel Oxidation-Acetylation of Aryl 1-Thio-β-D-glucopyranosides to 6-O-Acetyl-β-D-glucopyranosyl Aryl Sulfones. J. Org. Chem. 1964;29:1782–1787. doi: 10.1021/jo01030a028. [DOI] [Google Scholar]
- 120.Coatney G.R., Cooper W.C., Eddy N.B., Greenbeeg J. Chemotherapy of Plasmodium gallinaceum Infections; Toxicity; Correlation of Structure and Action. 9th ed. Public health monograph; Government Printing Office; Washington, DC, USA: 1953. Survey of antimalarial agents; p. 214. [PubMed] [Google Scholar]
- 121.Hays J.B., Sussman M.L., Glass T.W. Inhibition by 6-O-tosyl galactosides of beta-galactoside phosphorylation and transport by the lactose phosphotransferase system of Staphylococcus aureus. J. Biol. Chem. 1975;250:8834–8839. doi: 10.1016/S0021-9258(19)40749-7. [DOI] [PubMed] [Google Scholar]
- 122.Alsanosy R., Alhazmi H.A., Sultana S., Abdalla A.N., Ibrahim Y., Al Bratty M., Banji D., Khardali I., Khalid A. Phytochemical Screening and Cytotoxic Properties of Ethanolic Extract of Young and Mature Khat Leaves. J. Chem. 2020;2020:7897435. doi: 10.1155/2020/7897435. [DOI] [Google Scholar]
- 123.Kannan A., Hettiarachchy N.S., Lay J.O., Liyanage R. Human cancer cell proliferation inhibition by a pentapeptide isolated and characterized from rice bran. Peptides. 2010;31:1629–1634. doi: 10.1016/j.peptides.2010.05.018. [DOI] [PubMed] [Google Scholar]
- 124.Simmaco M., De Biase D., Severini C., Aita M., Erspamer G.F., Barra D., Bossa F. Purification and characterization of bioactive peptides from skin extracts of Rana esculenta. Biochim. Biophys. Acta. 1990;1033:318–323. doi: 10.1016/0304-4165(90)90140-R. [DOI] [PubMed] [Google Scholar]
- 125.Juillerat-Jeanneret L., Robert M.C., Juillerat M.A. Peptides from Lactobacillus hydrolysates of bovine milk caseins inhibit prolyl-peptidases of human colon cells. J. Agric. Food Chem. 2011;59:370–377. doi: 10.1021/jf102803a. [DOI] [PubMed] [Google Scholar]
- 126.Tyagi A., Tuknait A., Anand P., Gupta S., Sharma M., Mathur D., Joshi A., Singh S., Gautam A., Raghava G.P. CancerPPD: A database of anticancer peptides and proteins. Nucleic Acids Res. 2015;43:D837–D843. doi: 10.1093/nar/gku892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Oh D., Shin S.Y., Lee S., Kang J.H., Kim S.D., Ryu P.D., Hahm K.S., Kim Y. Role of the hinge region and the tryptophan residue in the synthetic antimicrobial peptides, cecropin A(1-8)-magainin 2(1-12) and its analogues, on their antibiotic activities and structures. Biochemistry. 2000;39:11855–11864. doi: 10.1021/bi000453g. [DOI] [PubMed] [Google Scholar]
- 128.Emran T.B., Rahman M.A., Uddin M.M.N., Rahman M.M., Uddin M.Z., Dash R., Layzu C. Effects of organic extracts and their different fractions of five Bangladeshi plants on in vitro thrombolysis. BMC Complementary Altern. Med. 2015;15:128. doi: 10.1186/s12906-015-0643-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Ali Redha A., Siddiqui S.A., Ibrahim S.A. Advanced extraction techniques for Berberis species phytochemicals: A review. Int. J. Food Sci. Technol. 2021;56:5485–5496. doi: 10.1111/ijfs.15315. [DOI] [Google Scholar]
- 130.Singh M., Shakya S., Soni V.K., Dangi A., Kumar N., Bhattacharya S.M. The n-Hexane and Chloroform Fractions of Piper Betle, L. Trigger Different Arms of Immune Responses in BALB/c Mice and Exhibit Antifilarial Activity Against Human Lymphatic Filarid Brugia Malayi. Int. Immunopharmacol. 2009;9:716–728. doi: 10.1016/j.intimp.2009.02.012. [DOI] [PubMed] [Google Scholar]
- 131.Barabanov P.V., Gerasimov A.V., Blinov A.V., Kravtsov A.A., Kravtsov V.A. Influence of nanosilver on the efficiency of pisum sativum crops germination. Ecotoxicol. Environ. Saf. 2018;147:715–719. doi: 10.1016/j.ecoenv.2017.09.024. [DOI] [PubMed] [Google Scholar]
- 132.Siddiqui S.A., Blinov A.V., Serov A.V., Gvozdenko A.A., Kravtsov A.A., Nagdalian A.A., Raffa V.V., Maglakelidze D.G., Blinova A.A., Kobina A.V., et al. Effect of Selenium Nanoparticles on Germination of Hordeum Vulgare Barley Seeds. Coatings. 2021;11:862. doi: 10.3390/coatings11070862. [DOI] [Google Scholar]
- 133.Chang C.C., Yang M.H., Wen H.M., Chern J.C. Estimation of Total Flavonoid Content in Propolis by Two Complementary Colorimetric Methods. J. Food Drug Anal. 2002;10:178–182. doi: 10.38212/2224-6614.2748. [DOI] [Google Scholar]
- 134.Sumanta N., Haque C.I., Nishika J., Suprakash R. Spectrophotometric analysis of chlorophylls and carotenoids from commonly grown fern species by using various extracting solvents. Res. J. Chem. Sci. 2014;4:63–69. [Google Scholar]
- 135.Rajan K. Analytical Techniques in Biochemistry and Molecular Biology. Springer; New York, NY, USA: 2011. pp. 67–77. [DOI] [Google Scholar]
- 136.Nawaz A., Li E., Khalifa I., Walayat N., Liu J., Muhammad Ahsan H., Irshad S., Barakat H., Lorenzo J.M., Pateiro M., et al. Effectof Structurally Different Pectin onDough Rheology, Structure, Pastingand Water Distribution Properties of Partially Meat-Based Sugar Snap Cookies. Foods. 2021;10:2692. doi: 10.3390/foods10112692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Hazra B., Biswas S., Mandal N. Antioxidant and free radical scavenging activity of Spondias pinnata. BMC Complementary Altern. Med. 2008;8:63. doi: 10.1186/1472-6882-8-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Moualek I., Aiche G.I., Guechaoui N.M., Lahcene S., Houali K. Antioxidant and anti-inflammatory activities of Arbutus unedo aqueous extract. Asian Pac. J. Trop. Biomed. 2016;6:937–944. doi: 10.1016/j.apjtb.2016.09.002. [DOI] [Google Scholar]
- 139.Rao A.S.V.G., Reddy S.G., Babu P.P., Reddy A.R. The antioxidant and antiproliferative activities of methanolic extracts from Njavara rice bran. BMC Complementary Altern. Med. 2010;10:4. doi: 10.1186/1472-6882-10-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Piskov S., Timchenko L., Grimm W.D., Rzhepakovsky I., Avanesyan S., Sizonenko M., Kurchenko V. Effects of various drying methods on some physico-chemical properties and the antioxidant profile and ACE inhibition activity of oyster mushrooms (Pleurotus ostreatus) Foods. 2020;9:160. doi: 10.3390/foods9020160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Rzhepakovsky I., Siddiqui S.A., Avanesyan S., Benlidayi M., Dhingra K., Dolgalev A., Enukashvily N., Fritsch T., Heinz V., Kochergin S., et al. Anti-arthritic effect of chicken embryo tissue hydrolyzate against adjuvant arthritis in rats (X-ray microtomographic and histopathological analysis) Food Sci. Nutr. 2021;9:5648–5669. doi: 10.1002/fsn3.2529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Heikal A., Elsebai M., Salama A., Taha H. Comparative study between in vivo- and in vitro-derived extracts of cactus (Opuntis ficus-indica L. Mill) against prostate and mammary cancer cell lines. Heliyon. 2021;7:e08016. doi: 10.1016/j.heliyon.2021.e08016. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data of the research is available is on request to the corresponding author.