Abstract
We have developed a fluorescence resonance energy transfer (FRET)-based assay to detect ciprofloxacin resistant (Cpr) mutants of the biothreat agent Yersinia pestis. We selected spontaneous mutants of the attenuated Y. pestis KIM 5 strain that were resistant to a ciprofloxacin (CIP) concentration of at least 1 μg/ml. DNA sequencing of gyrA encoded by 65 of these mutants revealed that all isolates contained one of four different point mutations within the quinolone resistance-determining region of gyrA. We developed a FRET-based assay that detected all of these mutations by using a single pair of fluorescent probes with sequences complementary to the wild-type Y. pestis gyrA sequence. Melting peak analysis revealed that the probe-PCR product hybrid was less stable when amplification occurred from any of the four mutant templates. This instability resulted in the PCR product obtained from the Cpr Y. pestis strains displaying a 4 to 11°C shift in probe melting temperature. Following optimization of the reaction conditions, we were able to detect approximately 10 pg of purified wild-type template DNA or the presence of approximately 4 CFU of wild-type Y. pestis KIM 5 or Cpr mutants in crude lysates. Taken together, our results demonstrate the utility of FRET-based assays for detection of Cpr mutants of Y. pestis. This method is both sensitive and rapid.
Resistance to antibiotics has become a major concern for the medical community over the past several years (13, 14, 16). Many organisms have become resistant to the common “drug of choice” used to treat the disease. A few examples are methicillin-resistant Staphylococcus aureus, vancomycin-resistant enterococci (18), and multiple-drug-resistant Mycobacterium tuberculosis (19), as well as organisms causing many enteric diseases. One of the current antibiotics that is effective in treating bacterial infectious diseases is ciprofloxacin (CIP), a fluorinated quinolone that blocks DNA replication through inhibition of gyrase activity (2, 24). Resistance to CIP does occur and is usually mediated by point mutations in DNA gyrases or, less commonly, through membrane alterations that reduce drug entry into the bacteria (28).
A critical piece of information necessary for the treatment of any bacterial disease is the antibiotic sensitivity profile of the infectious agent. Classically the sensitivity profile has been determined by growth of the organism in the presence of the antibiotic either in agar diffusion assays or by incubation of the organism in various concentrations of the drug for determination of the MIC. Both of these methods depend on growth of the bacterium after its initial isolation and are therefore time-consuming. DNA probe-based detection of antibiotic resistance offers the potential for increased speed. Among DNA-based techniques, PCR offers the best opportunity for speed, sensitivity, and specificity.
Recently it has become possible to couple PCR with real-time detection of the amplification product by use of fluorescent probes, thus eliminating the necessity to analyze the reaction product by gel electrophoresis. Fluorescence resonance energy transfer (FRET) is one of the available chemistries that can be used to detect the PCR product in these reactions. Roche Diagnostics has adopted this chemistry for its “Hybridization Probes” technology (5). Two DNA probes are used to bind to the amplification product when FRET chemistry is used to specifically detect the amplification product. The two light-activated molecules are positioned in close proximity at the 3′ and 5′ termini of the probes such that fluorescence increases as more PCR product accumulates and the two labeled probes bind next to each other.
The increase in antibiotic resistance coupled with the threat of modification of agents of biological warfare have prompted us to develop a hybridization probe assay for the detection of CIP resistance (Cpr) in Yersinia pestis. We chose Y. pestis as a model for our initial development of a Cpr assay for three reasons. First, it is the etiologic agent of a disease that has high potential for use as a biological terrorism or biological warfare agent (27). Second, it is likely that any biological used as a weapon would be made antibiotic resistant. Third, Y. pestis is relatively slow growing, and therefore the increased speed of DNA-based antibiotic resistance detection would improve our ability to properly treat infected individuals. Although our development of the assay used Y. pestis as a model, the method should be broadly applicable to the detection of antibiotic resistance encoded by point mutations in other organisms.
MATERIALS AND METHODS
Cultivation of bacteria, isolation of Cpr mutants, and antibiotic sensitivity testing.
The bacterium used in this study was an avirulent, pigmentation-negative (pgm-negative) mutant of Y. pestis KIM 5 and was obtained from Susan Straley, Department of Microbiology and Immunology, University of Kentucky, Lexington, Ky. Bacteria were grown on brain heart infusion agar (BHI; Difco Laboratories, Detroit, Mich.) plates for 48 h at 30°C or overnight in BHI broth at 30°C with aeration. After cultivation, the bacteria were collected, washed twice with phosphate-buffered saline (150 mM NaCl, 1.7 mM KH2PO4, 5 mM Na2PO4 [pH 7.4]) and suspended to yield a concentration of 1011 CFU/ml. For selection of Cpr mutants, a 100-μl sample of washed bacteria was plated on BHI agar plates containing 1 to 10 μg of CIP (Bayer, Leverkusen, Germany)/ml. Cpr mutants appeared after 48 to 72 h of incubation at 30°C. Colonies were purified by streaking on fresh BHI agar plates containing the appropriate concentration of CIP. The MIC for CIP was determined by using E Test (AB Biodisk, Piscataway, N.J.) antibiotic strips containing a continuous gradient of CIP. The E Test was performed by spreading 100 μl of bacterial culture onto BHI agar plates without antibiotic. After 48 h of incubation at 30°C, the MIC was read according to the manufacturer's instructions.
DNA isolation, gene amplification, and sequencing.
Total-cell DNA was extracted from 5-ml cultures of Y. pestis or Cpr mutants with the Puregene DNA Isolation Kit (Gentra Systems, Minneapolis, Minn.). Initially primers to amplify the quinolone resistance-determining region (QRDR) (30) of gyrA were selected from the published Escherichia coli sequence (GenBank accession number AE000312) (3) using Primerselect software (Lasergene, Madison, Wis.). PCR amplification primers gyrA51 and gyrA31 were ATGAGCGACCTTGCGAGAG and TGTTCCATCAGCCCTTCAATG, respectively. We used PCR and direct DNA sequencing to identify Y. pestis gyrA mutations. PCR was carried out with AmpliTaq Gold (Perkin-Elmer, Foster City, Calif.) according to the manufacturer's directions. Initial activation of AmpliTaq Gold and denaturation of template DNA were carried out at 95°C for 10 min, followed by 30 cycles of 95°C for 30 s, 55°C for 30 s, and 72°C for 1 min, with a final extension step of 72°C for 7 min. Amplification products were examined for size and purity by fractionation of a 10-μl sample on 1.5% agarose gels or 10% polyacrylamide gels (Novex Corporation, San Diego, Calif.). PCR products were purified for automated DNA sequencing with a QIAquick PCR Purification Kit (Qiagen, Valencia, Calif.). Nucleotide sequence determination was performed by the dideoxy chain-termination method using the Applied Biosystems International (ABI, Foster City, Calif.) PRISM dichloRhodamine Dye Terminator Sequencing Kit with AmpliTaq DNA polymerase. DNA sequencing reactions were analyzed on an ABI 377XL automated DNA sequencher. Sequence data were edited and assembled into contiguous sequences using the Sequencher program (Gene Codes, Ann Arbor, Mich.). The Y. pestis KIM 5 wild-type gyrA nucleotide sequence was determined using the gyrA51 and gyrA31 primers used in the initial PCR. The DNA sequences of the mutant gyrA genes were determined using oligonucleotide primers gyrA51seq and gyrA31seq, which had the sequences AAATAACACCGGTCAACATC and ATATAAGCCAGACAGCCATCA, respectively. Template DNA for sequencing of the Y. pestis gyrA mutants was prepared by using 2.5-μl boiled overnight bacterial culture as the template in a 50-μl PCR mixture with gyrA51 and gyrA31 as the primers. The purified PCR product obtained from the mutants was sequenced as described above for wild-type Y. pestis gyrA.
The QRDR regions of Y. pestis gyrB and parC were amplified using oligonucleotide primer pairs GyrB51 (TCGAATTCTTATGACTCCTCCAG)–GyrB31 (CAATACCGTCTTTTTCAGTGGAG) and ParC53 (GACCGTGCGTTGCCGTTTATTGG)–ParC39 (TTGGCTAAGTGGCGGAGTTTC). These primers were selected by using the E. coli GyrB (GenBank accession number P06982) and ParC (P20083) protein sequences (3) to search the Y. pestis CO92 genome database at http://www.sanger.ac.uk/Projects/Y_pestis/blast_server.shtml (1). Contiguous sequences that could encode proteins 78% identical to GyrB and 80% identical to ParC over the entire length of the E. coli proteins were found in the Y. pestis CO92 genome database. The contiguous DNA sequences from the genome database were used to obtain the potential coding regions for Y. pestis KIM 5 GyrB and ParC.
FRET probe detection of Cpr mutants.
Y. pestis Cpr mutants were detected using hybridization probe (FRET) reactions with the LightCycler (Roche Diagnostics, Mannheim, Germany). The primers for hybridization probe reactions were LC3 (GATTATGCGATGTCCGTTATTGTC) and LC4 (GAAGTTACCCTGCCCATCCAC). Primers LC3 and LC4 were designed using Primerselect (Lasergene). Sequence-specific hybridization probes were probe 1 (GCATGGTGACAGCGCGGTC-fluorescein) and probe 2 (Lightcycler Red 640-ACGACACTATCGTGCGTATGGCCCA-PO4). The probes were chosen using Primerselect (Lasergene) software according to the guidelines suggested by Roche Diagnostics. Operon Technologies, Inc. (Alameda, Calif.), or Synthegen LLC (Houston, Tex.) synthesized the fluorescent-labeled FRET probes. Mutant sequence detection was performed with primers LC3 and LC4 plus probe 1 and probe 2 and the Roche Diagnostics DNA Master Hybridization Probes kit. The optimized reaction mixture contained template DNA in 2 μl of water, 5 mM MgCl2, 1 μM primers LC3 and LC4, 0.4 μM (each) probe1 and probe2, and 1× LightCycler DNA Master Hybridization Probes buffer, according to the manufacturer's directions (Roche Diagnostics). Crude lysates of Cpr mutants were analyzed by a simple growth and boiling procedure. A 2-μl portion of the clarified supernatant obtained from crude boiled lysates was used as a template in the hybridization probe Cpr detection assay as described above. All PCRs were performed on a LightCycler (Roche Diagnostics) using channel F2 (640 nm). The Y. pestis gyrA target sequences were amplified by a single incubation at 95°C for 1 min, followed by 40 cycles of 95°C for 0 s, 58°C for 15 s, and 72°C for 15 s. The melting curve for the annealing of the PCR product with the FRET probes was determined by monitoring the fluorescence of channel F2 from 40 to 95°C with a temperature transition rate of 0.1°C per s. Lightcycler amplification results were verified by electrophoresis of 10 μl of the PCR product on 1.5% agarose gels. Data were analyzed with LightCycler software, version 3.1, according to the manufacturer's instructions.
Nucleotide sequence accession numbers.
The DNA sequences of wild-type Y. pestis KIM 5 and of the four examples of Y. pestis KIM 5 Cpr gyrA point mutants have been deposited in GenBank and assigned accession numbers AF217736 through AF217740. The Y. pestis gyrB and parC sequences have been given GenBank accession numbers AF221694 and AF221695, respectively. To promote ease of analysis and comparison with previous studies, we have adopted the convention of using the E. coli GyrA (GenBank accession number P09097) numbering throughout this paper when referring to specific amino acid residues.
RESULTS
Isolation of Cpr Y. pestis mutants.
We performed 11 independent experiments to isolate Cpr mutants. The average mutation frequency observed for all of these experiments was 2.6 × 10−10. These mutant isolations resulted in 682 Cpr Y. pestis KIM 5 strains. We chose 65 mutants at random for further single-colony isolation and characterization. We performed initial experiments to determine the influence of plating cell density on the CIP MIC observed by using E Test antibiotic sensitivity strips. Inoculation of BHI agar plates with approximately 107 or 108 cells produced MICs that were similar to each other. However, inoculation of BHI agar plates for the E Test with cell concentrations above or below 107 or 108 CFU produced significantly higher or lower observed MICs, respectively. Accordingly, we chose to plate Y. pestis KIM 5 at 107 CFU per plate in order to determine the observed MIC for CIP in all later experiments. Our observed CIP MIC for the wild-type Y. pestis strain KIM 5 was 0.026 μg/ml. For all the Cpr mutants, MICs at least 40 times greater than that for the wild type, i.e., between 1.1 and 4.6 μg/ml, were observed (Fig. 1B).
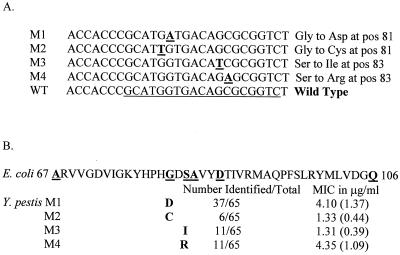
FIG. 1.
Nucleotide sequence and protein changes in Y. pestis Cpr mutants. (A) DNA sequences of wild-type (WT) Y. pestis gyrA and the four point mutants, identified as M1 through M4, corresponding to their designations in the text. Underlined nucleotides in the WT sequence denote the FRET assay probe 1. Nucleotide substitutions in mutants M1 through M4 are boldfaced and underlined. Amino acid substitutions and the position relative to E. coli GyrA (3) are given on the right. (B) Amino acid changes, isolation frequency, and CIP MIC for the various Cpr mutants. Amino acid numbering (67 to 106) is relative to the E. coli GyrA sequence (3) and is indicated to the left and right of the sequence. Boldfaced, underlined letters indicate amino acid changes in the QRDR of E. coli GyrA that have been shown to result in Cpr. MICs for the Y. pestis mutants determined by duplicate E Tests in five independent experiments are shown as averages with standard deviations in parentheses. Amino acid changes for mutants M1 through M4 are shown as boldfaced letters below the corresponding positions in the E. coli QRDR.
Sequencing of wild-type Y. pestis and Cpr mutants.
We obtained a single, approximately 630-bp fragment of DNA from the Y. pestis KIM 5 genome using oligonucleotide primers gyrA51 and gyrA31 in PCRs. After determination of the sequence of this fragment on both strands of DNA, a BLASTN (1) search of GenBank (http://www.ncbi.nlm.nih.gov/blast/blast.cgi) revealed that our sequence had a high degree of homology (probability value, 1e−137) with Serratia marcescens gyrA (GenBank accession number AF052260) (26). The final 492-bp Y. pestis KIM 5 gyrA sequence was 88% identical to S. marcescens gyrA at the nucleotide level, suggesting that it was the plague homologue of the gyrase A gene. Further evidence was obtained by performing protein searches of the nonredundant GenBank database. The protein database search revealed that the putative protein product translated from our DNA sequence was 96% identical over a 164-amino-acid overlap with S. marcescens GyrA (AAC68576) (26) as well as many other E. coli GyrA homologues. Our analysis of the predicted Y. pestis KIM 5 GyrA sequence obtained from the PCR product using Megalign (Lasergene) revealed that the nucleotide sequence changes encoded six conservative amino acid substitutions compared to S. marcescens GyrA. Our results revealed that the Y. pestis KIM 5 GyrA sequence within the QRDR was identical to that of E. coli. Accordingly, we designated our sequence Y. pestis gyrA.
We amplified the DNA encoding the QRDR from all of the Cpr Y. pestis mutants we isolated using the gyrA51–gyrA31 primer pair. The DNA sequences for each of these mutants were determined on both strands using oligonucleotide primers gyrA51seq and gyrA51seq. Each of the mutants revealed a single-nucleotide change in the QRDR of gyrA, and these substitutions belonged to one of four groups (Fig. 1A). The largest group of mutants isolated had a transition of guanine to adenine such that Gly-81 (relative to E. coli numbering, GenBank accession number P09097) was changed to Asp in that position (mutant M1 in Fig. 1). The smallest group of mutants had a guanine altered to a thymine such that Gly-81 was changed to Cys (mutant M2 in Fig. 1). The final two groups of mutants were found in equal numbers as shown in Fig. 1. We identified mutations in Y. pestis gyrA that were guanine-to-thymine transversions. These mutants coded for an Ile residue at position 83 instead of the Ser residue in the wild-type protein sequence (mutant M3 in Fig. 1). The last group of mutants had a transversion of cytosine to adenine such that amino acid Ser-83 was changed to Arg (mutant M4 in Fig. 1). The position of the amino acid substitution encoded by the mutant did not correlate with the level of Cpr, since we observed MICs of approximately 1 and 4 μg/ml for strains with mutations at either codon 81 or codon 83 within gyrA (Fig. 1B).
Since other gene products such as GyrB (8, 12, 31) and ParC (6, 11, 20) have been shown to be involved in resistance to CIP, we amplified the QRDRs of these genes from a randomly selected group of our Cpr mutants and compared the DNA sequences for both Y. pestis KIM 5 gyrB and parC. The DNA sequences of the wild type Y. pestis KIM 5 gyrB and parC loci were determined as described in Materials and Methods. In order to confirm that the genes we amplified did encode the expected proteins, our nucleotide sequences were translated into predicted proteins and used to search the GenBank protein database. The protein product predicted by translation of the wild-type Y. pestis gyrB sequence was highly homologus (probability value, 1e−102) with E. coli GyrB (AAC76722) (3). The entire protein sequence predicted by translation of Y. pestis KIM 5 parC was 86% identical with the E. coli ParC sequence (P20082) (3), amino acids 12 through 394. Accordingly, the putative function of the proteins encoded by our PCR product obtained after Y. pestis gyrB and parC amplification was confirmed by protein homologies in the database. The DNA sequence of gyrB carried by 12 of our 65 Y. pestis Cpr mutants was determined from randomly selected strains regardless of observed MIC and was found to be identical with the wild-type sequence. Similarly, the parC sequence encoding the QRDR was determined for 36 of the 65 Cpr mutants and was found to be identical to the wild-type DNA sequence.
Amplification and detection of gyrA in the LightCycler.
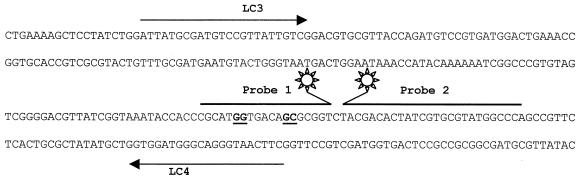
We designed PCR primers and hybridization probes for detection of Y. pestis KIM 5 gyrA as shown in Fig. 2. Oligonucleotide primers LC3 and LC4 were designed to amplify a 261-bp region of gyrA that included all of the point mutations within the QRDR we had detected in our Cpr mutant isolation (Fig. 1). As shown in Fig. 2, the FRET detection probe 1 was chosen to have the same sequence as wild-type Y. pestis gyrA and to encompass all four of the point mutations within the gene that resulted in Cpr. FRET probe 2 was selected such that the 5′ end of the oligonucleotide containing the LightCycler-Red-640 label was positioned 1 bp away from the probe 1 3′ end (Fig. 2). The predicted melting temperatures (Tm) for probe 1 and probe 2 were 59.6 and 64.9°C, respectively. We reasoned that we would be able to detect the mutant genes through melting curve analysis by using a single probe, since probe 1 was based on the wild-type allele and included the region where all of the Cpr point mutations occurred in gyrA.
FIG. 2.
Schematic representation of the hybridization probe assay for Cpr in Y. pestis. PCR primers are represented by arrows above or below the Y. pestis gyrA sequence and are labeled LC3 and LC4. Probe 1 and probe 2 are shown between LC3 and LC4. The starbursts at the 3′ and 5′ termini of probe 1 and probe 2, respectively, indicate light reactive labels. Probe 1 is homologous with the wild-type Y. pestis gyrA sequence. The positions of the four point mutations described in Fig. 1A are indicated (boldfaced, underlined letters) in the wild-type DNA sequence below probe 1. The Tm of probe 1 was chosen to be less than that of probe 2 such that detection of melting of the probes from the PCR product would be dependent on the stability of probe 1 with the product.
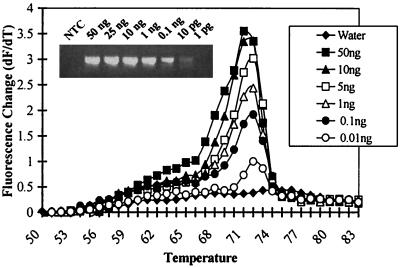
We tested the ability of the hybridization probe assay to detect Y. pestis gyrA sequences using purified genomic DNA as a template. Melting peak analysis revealed that the change in fluorescence with the change in time versus temperature was also proportional to the amount of template DNA used in the reaction (Fig. 3). The ability to detect a change in fluorescence signal above background (no template controls) was proportional to the template concentration (Fig. 3). The hybridization probe assay was routinely able to detect Y. pestis gyrA sequences at concentrations of 10 pg of genomic DNA per reaction. Using a Y. pestis KIM 5 genome size of 4.4 Mbp (17), we calculate that our lower limit of detection of gyrA is approximately 2,100 genomic equivalents using purified DNA as a template in the reaction. We found that a single product of approximately 261 bp (Fig. 3, inset) was amplified in a template concentration-dependent manner similar to that seen on the FRET probe assay.
FIG. 3.
Sensitivity of the hybridization probe CIP assay. The graph shows the melting peak analysis of the probe-PCR product hybrid as the change in fluorescence with the change in time (dF/dT) versus hybrid temperature at the various DNA concentrations. The 0.001-ng template reaction mixture was indistinguishable from the no-template control (water). NTC, no-template control.
FRET probe detection of Cpr gyrA DNA sequences.
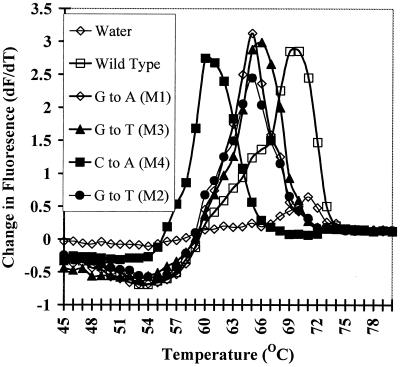
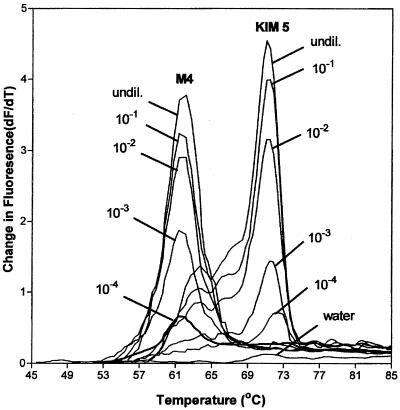
Using the FRET probe assay, we were able to differentiate Y. pestis KIM 5 gyrA mutants (Cpr) from wild-type (Cps) organisms. As shown in Fig. 4, the melting peak temperature was dependent on the homology between probe 1 and the amplified PCR product. All of the mutant PCR products formed a less-stable hybrid with probe 1 than did the wild-type gyrA sequence. The largest difference in melting peak was seen with the cytosine-to-adenosine mutation (M4 in Fig. 1A), which was closest to the 3′ fluorescein label on probe 1. Interestingly, the most-stable probe1-mutant PCR product hybrid was formed with the guanine-to-thymine transversion mutant (Fig. 1A and 4). This mutation was located 1 bp 5′ to the mutation in the strain that formed the least-stable hybrid with probe 1 (M3 in Fig. 1A). However, the two mutations that were the most distal to the 3′ end of probe 1 (M1 and M2 in Fig. 1A) had an intermediate Tm. The mutant gyrA-probe1 Tm was easily differentiated from those generated with wild-type templates. The minimum Tm decrease compared to that for the wild-type sequence was with mutant M3, for which the Tm was consistently 4°C (Fig. 4). The maximum Tm shift compared to Y. pestis KIM 5 was greater than 11°C for the M4 mutant. Furthermore, we found the Tm of the melting peaks to be consistent between experiments. We performed five independent Tm determinations for all four mutants and the wild-type organism. The maximum standard deviation of the melting peak temperature obtained for each of these mutants from these experiments was 0.93°C. In all experiments the ΔTm (defined as the Tm of the wild type − the Tm of the mutant) was also consistent and varied less than 0.5°C.
FIG. 4.
FRET assay for Cpr detection using purified template DNA of mutant and wild-type Y. pestis. Wild-type and mutant templates were used in the PCR amplification followed by melting peak analysis. The graph is of the change in fluorescence as a function of time (dF/dT) versus the temperature of the reaction products. The templates used in the various reactions are given in the key. Mutant designations in parentheses are as shown in Fig. 1A. All mutant templates produced a lower Tm than did the 100% match between probe 1 and the wild-type template. The template concentration was 10 μg/ml for all reactions.
Colony assay for Cpr Y. pestis
In order to test the utility of our FRET assay for identification of Cpr Y. pestis, we performed the assay on crude lysates of bacteria. Initially, we used boiled lysates from a single colony suspended in 100 μl of water as the template in these reactions without any further growth of the cells. We found that we could identify the Cpr mutants in dilutions up to and including 1,000-fold (data not shown). The minimum number of CFU we could detect in our initial FRET PCRs was approximately 500. Since our goal was to develop our assay to cover as wide a range of template concentrations as possible, we tested the effect of growing the bacteria for a short time in liquid culture on the sensitivity of the assay. We found that growth for only 3 h in BHI broth allowed us to detect the presence of Y. pestis gyrA at dilutions up to 10,000-fold as shown in Fig. 5. This result represented an approximately 100-fold increase over reactions performed on suspended bacteria that were not allowed to replicate before analysis by the FRET assay. The FRET PCR generated from the 10−4 dilution of bacteria (Fig. 5) contained the equivalent of approximately 4 CFU of Y. pestis. Use of crude lysates as template DNA resulted in melting peak shifts for the Cpr mutants that were similar to those seen with purified templates. The data shown in Fig. 5 are for the wild-type gyrA allele and mutant M4. Mutants M1, M2, and M3 all displayed melting peak temperature shifts similar to those shown in Fig. 4 (data not shown). Dilutions of cell suspensions greater than 10−4 resulted in melting peaks that could not be distinguished from those for negative controls. In order to compare melting peak analysis results with the amount of PCR product produced, we analyzed a 10-μl sample of the Y. pestis KIM 5 reaction products on agarose gels. We did not detect any gyrA PCR product in the reaction products produced with the 10−5 and 10−6 dilutions (data not shown).
FIG. 5.
Detection of Cpr mutations in crude whole-cell lysates. Single colonies were grown in broth for 3 h at 30°C before being harvested. Shown is a melting peak analysis of various concentrations of wild-type Y. pestis or Cpr mutant M4. Bacteria used in the reactions are given above each melting peak. Curves obtained with each dilution are labeled. The sample labeled “undil.” represents the reaction obtained with undiluted bacterial suspensions. The 2-μl sample used in the FRET PCR labeled “undil.” contained 4 × 104 CFU. Suspensions of bacteria were diluted before lysis by boiling to simulate different concentrations of organisms that might be obtained after the 3-h growth period. The curve labeled “water” represents the no-template control sample.
DISCUSSION
Although Cpr in Y. pestis is currently of no concern to public health officials, the organism is of major concern as a potential agent for biological warfare or bioterrorism (27). Given that CIP is a new-generation antibiotic under consideration for inclusion in a national antibiotic stockpile (9), a rapid method for the detection of Cpr agents of bioterrorism is highly desirable. We have developed a simple and rapid PCR assay to detect Cpr using FRET probes and the Roche Diagnostics LightCycler. The assay was able to detect four different point mutations within Y. pestis KIM 5 gyrA using a single probe pair with as few as approximately 2,100 copies of purified target sequence. Cpr Y. pestis could also be detected in crude lysates prepared from fresh colonies isolated on petri plates at levels below 10 CFU per reaction. The difference in detection level between pure and crude templates is most likely due to the tendency of Y. pestis to grow as chains under culture conditions similar to those used here (L. E. Lindler, unpublished data). Using our assay, we were able to determine if the bacteria growing on solid medium were Cpr within 4 h using melting peak analysis. Furthermore, the FRET assay was able to reliably identify Cpr Y. pestis at CFU concentrations of 4 to 40,000 per reaction. This finding is particularly important if the method is to be useful in a clinical laboratory, since the assay will identify Cpr bacteria over a wide range of template concentrations, thus reducing the possibility of false-negative reactions.
Given that FRET depends on the interaction of two fluorochromes in proximity with each other, it might be expected that the location of the base mismatch within probe 1 would strongly influence the melting peak. However, our results indicate that the position of the mismatch within probe 1 does not greatly influence this stability. This fact was suggested by our observation that mutant M4 and M3 produced the largest and smallest Tm values in our FRET assay and were located only 1 bp apart. The stability of these mutant templates was especially noteworthy, since M3 and M4 are located nearest the 3′ terminus of probe 1 and therefore might be expected to decrease the excitation of probe 2. If the position of the mismatch within the probe 1 sequence were a major factor in probe-template stability, then mutants M1 and M2 (Fig. 1A) might be expected to reduce the observed Tm to a lesser degree than mutant M3. However, the melting peaks of M1, M2, and M3 were very similar, further suggesting that the position of the mismatch did not influence probe 1 binding to the PCR product to any great degree. Taken together, our results suggest that the greatest influence on the observed melting peak using the FRET assay is due to the sequence of the base pair mismatch rather than the position of the mismatch within the donor probe.
Currently, the standard method of determining Cpr is by agar diffusion tests. This method requires the isolation of the pathogen followed by an extra day of incubation with disks or strips. DNA-based methods for Cpr detection, such as mismatch amplification mutation assay (MAMA) combined with DNA sequencing (32) and single-stranded confirmation polymorphism (23), have been developed. All of these methods require electrophoresis of reaction products to determine if a mutant allele of a cellular gyrase is encoded by the isolate. Also, both of the techniques above require equipment that does not easily lend itself to use in a clinical laboratory environment. Most recently, Wilson et al. (29) developed a 5′ nuclease assay to detect Cpr in Campylobacter jejuni by PCR allelic discrimination (AD). These researchers were able to distinguish mutations at codon 86 by use of a pair of fluorescent probes and comparison of binding of those probes with either mutant or wild-type PCR products. Although this assay was shown to be sensitive to the femtogram level of template DNA, it has not been tested for the ability to distinguish Cpr mutants from sensitive strains using crude whole-cell lysates as we have demonstrated here. Furthermore, we believe the FRET-based assay is more applicable because the use of a single pair of FRET probes allows the detection of four different linked point mutations in gyrA. In contrast, detection of the point mutations described here would require at least five different probes to be developed for an AD assay, assuming that one wild-type probe could be paired with a probe that binds to each individual point mutation in gyrA.
The mutations in Y. pestis gyrA all occurred at position 81 or 83 relative to the E. coli protein sequence. Although we did not determine the sequences of gyrB and parC for every Cpr mutant we identified, our random sampling of these gene sequences suggests that they were most probably wild type in the mutants we characterized. Specifically, the observed MICs for all of the individual members of our four mutant classes were similar, and secondary alterations in gyrB and/or parC have been shown to result in increased levels of Cpr (7, 11, 20). Taken together, our random DNA sequencing of known secondary mutation sites and our MIC data strongly suggest that the Y. pestis Cpr strains we characterized did not encode mutations in the gyrB and/or parC QRDR.
Six different amino acid substitutions in E. coli GyrA have been identified in Cpr strains following in vitro selection (4, 10, 22, 30). Among our 65 Y. pestis Cpr mutants we found only two amino acid positions in GyrA that had been changed. The substitutions in Y. pestis GyrA were Gly-81 to Asp or Cys and Ser-83 to Ile or Arg. All of the amino acid substitutions we identified in Y. pestis GyrA have been found in other organisms (4, 15, 20, 23, 25, 30). Based on the results of our characterization of 65 Y. pestis Cpr mutants, the most common site of mutation in GyrA is Gly-81. Other studies have indicated that Ser-83 is the most common hotspot for changes in gyrA that result in Cpr (7, 11, 20, 21, 23, 30). The fact that Gly-81 appears to be a hotspot for mutation in Y. pestis may reflect a difference in the organism's DNA repair capabilities or a difference in the tertiary structure of GyrA. Alternatively, this finding may be due to the limited number of Cpr isolates we characterized.
In summary, we have developed a pair of FRET probes that can easily detect four closely linked point mutations in Y. pestis gyrA by use of melting peak analysis. This FRET-based Cpr detection method is sensitive, reproducible, and applicable over a wide range of template concentrations. In order for this assay to be useful in a clinical laboratory setting, it should be possible to perform the analysis as quickly after initial isolation of the organism as possible. We have demonstrated that this is possible by use of crude whole-cell lysates as templates in our reactions. Further testing of specificity is planned for future experiments. However, currently we envision that the FRET assay described here could be incorporated into a general DNA-based identification panel that would include Y. pestis-specific primers. Accordingly, it may be possible in the future to identify organisms and determine their antibiotic sensitivity profiles simultaneously. The development of our FRET-based Cpr assay is a first step toward this goal.
ACKNOWLEDGMENTS
We thank Peter Schwartz for technical assistance. We also gratefully acknowledge the support of Erik Henchal.
This work is part of the U.S. Army Medical Research and Material Command Research Area Director IV sponsored programs.
REFERENCES
- 1.Altschul S F, Gish W, Miller W, Myers E W, Lipman D J. Basic local alignment search tool. J Mol Biol. 1990;215:403–410. doi: 10.1016/S0022-2836(05)80360-2. [DOI] [PubMed] [Google Scholar]
- 2.Balfour J A, Faulds D. Oral ciprofloxacin: a pharmacoeconomic evaluation of its use in the treatment of serious infections. Pharmacoeconomics. 1993;3:398–421. doi: 10.2165/00019053-199303050-00007. [DOI] [PubMed] [Google Scholar]
- 3.Blattner F R, Plunkett III G, Bloch C A, Perna N T, Burland V, Riley M, Collado-Vides J, Glasner J D, Rode C K, Mayhew G F, Gregor J, Davis N W, Kirkpatrick H A, Goeden M A, Rose D J, Mau B, Shao Y. The complete genome sequence of Escherichia coli K-12. Science. 1997;277:1453–1474. doi: 10.1126/science.277.5331.1453. [DOI] [PubMed] [Google Scholar]
- 4.Cambau E, Bordon F, Collatz E, Gutmann L. Novel gyrA point mutation in a strain of Escherichia coli resistant to fluoroquinolones but not to nalidixic acid. Antimicrob Agents Chemother. 1993;37:1247–1252. doi: 10.1128/aac.37.6.1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Caplin B E, Rasmussen R P, Bernard P S, Wittwer C T. LightCycler hybridization probes: the most direct way to monitor PCR amplification for quantitation and mutation detection. Biochemica. 1999;1:5–9. [Google Scholar]
- 6.Chu Y W, Houang E T, Cheng A F. Novel combination of mutations in the DNA gyrase and topoisomerase IV genes in laboratory-grown fluoroquinolone-resistant Shigella flexneri mutants. Antimicrob Agents Chemother. 1998;42:3051–3052. doi: 10.1128/aac.42.11.3051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Deguchi T, Fukuoka A, Yasuda M, Nakano M, Ozeki S, Kanematsu E, Nishino Y, Ishihara S, Ban Y, Kawada Y. Alterations in the GyrA subunit of DNA gyrase and the ParC subunit of topoisomerase IV in quinolone-resistant clinical isolates of Klebsiella pneumoniae. Antimicrob Agents Chemother. 1997;41:699–701. doi: 10.1128/aac.41.3.699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gensberg K, Jin Y F, Piddock L J. A novel gyrB mutation in a fluoroquinolone-resistant clinical isolate of Salmonella typhimurium. FEMS Microbiol Lett. 1995;132:57–60. doi: 10.1111/j.1574-6968.1995.tb07810.x. . (Erratum, 137:293, 1996.) [DOI] [PubMed] [Google Scholar]
- 9.Grabenstein J, Downs K, Dotson D. Extraordinary infections: a focus on bioterrorism. J Am Pharm Assoc (Washington, DC) 2000;40:S36–S37. [PubMed] [Google Scholar]
- 10.Hallett P, Maxwell A. Novel quinolone resistance mutations of the Escherichia coli DNA gyrase A protein: enzymatic analysis of the mutant proteins. Antimicrob Agents Chemother. 1991;35:335–340. doi: 10.1128/aac.35.2.335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Heisig P. Genetic evidence for a role of parC mutations in development of high-level fluoroquinolone resistance in Escherichia coli. Antimicrob Agents Chemother. 1996;40:879–885. doi: 10.1128/aac.40.4.879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Heisig P. High-level fluoroquinolone resistance in a Salmonella typhimurium isolate due to alterations in both gyrA and gyrB genes. J Antimicrob Chemother. 1993;32:367–377. doi: 10.1093/jac/32.3.367. [DOI] [PubMed] [Google Scholar]
- 13.Jack D B. Drug-resistant bacteria: responding to the infectious disease crisis. Mol Med Today. 1996;2:499–502. doi: 10.1016/s1357-4310(97)81453-0. [DOI] [PubMed] [Google Scholar]
- 14.Jones R N, Pfaller M A. Bacterial resistance: a worldwide problem. Diagn Microbiol Infect Dis. 1998;31:379–388. doi: 10.1016/s0732-8893(98)00037-6. [DOI] [PubMed] [Google Scholar]
- 15.Korten V, Huang W M, Murray B E. Analysis by PCR and direct DNA sequencing of gyrA mutations associated with fluoroquinolone resistance in Enterococcus faecalis. Antimicrob Agents Chemother. 1994;38:2091–2094. doi: 10.1128/aac.38.9.2091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Koshland D E., Jr The biological warfare of the future. Science. 1994;264:327. doi: 10.1126/science.8153609. [DOI] [PubMed] [Google Scholar]
- 17.Lucier T S, Brubaker R R. Determination of genome size, macrorestriction pattern polymorphism, and nonpigmentation-specific deletion in Yersinia pestis by pulsed-field gel electrophoresis. J Bacteriol. 1992;174:2078–2086. doi: 10.1128/jb.174.7.2078-2086.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Michel M, Gutmann L. Methicillin-resistant Staphylococcus aureus and vancomycin-resistant enterococci: therapeutic realities and possibilities. Lancet. 1997;349:1901–1906. doi: 10.1016/s0140-6736(96)11192-2. [DOI] [PubMed] [Google Scholar]
- 19.Moss A R, Alland D, Telzak E, Hewlett D, Jr, Sharp V, Chiliade P, LaBombardi V, Kabus D, Hanna B, Palumbo L, Brudney K, Weltman A, Stoeckle K, Chirgwin K, Simberkoff M, Moghazeh S, Eisner W, Lutfey M, Kreiswirth B. A city-wide outbreak of a multiple-drug-resistant strain of Mycobacterium tuberculosis in New York. Int J Tuberc Lung Dis. 1997;1:115–121. [PubMed] [Google Scholar]
- 20.Mouneimne H, Robert J, Jarlier V, Cambau E. Type II topoisomerase mutations in ciprofloxacin-resistant strains of Pseudomonas aeruginosa. Antimicrob Agents Chemother. 1999;43:62–66. doi: 10.1128/aac.43.1.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ruiz J, Marco F, Goni P, Gallardo F, Mensa J, Trilla A, Jimenez de Anta T, Vila J. High frequency of mutations at codon 83 of the gyrA gene of quinolone-resistant clinical isolates of Escherichia coli. J Antimicrob Chemother. 1995;36:737–738. doi: 10.1093/jac/36.4.737. [DOI] [PubMed] [Google Scholar]
- 22.Swanberg S L, Wang J C. Cloning and sequencing of the Escherichia coli gyrA gene coding for the A subunit of DNA gyrase. J Mol Biol. 1987;197:729–736. doi: 10.1016/0022-2836(87)90479-7. [DOI] [PubMed] [Google Scholar]
- 23.Takenouchi T, Sakagawa E, Sugawara M. Detection of gyrA mutations among 335 Pseudomonas aeruginosa strains isolated in Japan and their susceptibilities to fluoroquinolones. Antimicrob Agents Chemother. 1999;43:406–409. doi: 10.1128/aac.43.2.406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Thomson C J. The global epidemiology of resistance to ciprofloxacin and the changing nature of antibiotic resistance: a 10 year perspective. J Antimicrob Chemother. 1999;43(Suppl. A):31–40. doi: 10.1093/jac/43.suppl_1.31. [DOI] [PubMed] [Google Scholar]
- 25.Truong Q C, Nguyen Van J C, Shlaes D, Gutmann L, Moreau N J. A novel, double mutation in DNA gyrase A of Escherichia coli conferring resistance to quinolone antibiotics. Antimicrob Agents Chemother. 1997;41:85–90. doi: 10.1128/aac.41.1.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Weigel L M, Steward C D, Tenover F C. gyrA mutations associated with fluoroquinolone resistance in eight species of Enterobacteriaceae. Antimicrob Agents Chemother. 1998;42:2661–2667. doi: 10.1128/aac.42.10.2661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Weller R E, Lyu C W, Wolters C, Atlas R M. Universities and the biological and toxin weapons convention. ASM News. 1999;65:403–409. [Google Scholar]
- 28.Wiedemann B, Heisig P. Mechanisms of quinolone resistance. Infection. 1994;22:S73–S79. doi: 10.1007/BF01793570. [DOI] [PubMed] [Google Scholar]
- 29.Wilson D L, Abner S R, Newman T C, Mansfield L S, Linz J E. Identification of ciprofloxacin-resistant Campylobacter jejuni by use of a fluorogenic PCR assay. J Clin Microbiol. 2000;38:3971–3978. doi: 10.1128/jcm.38.11.3971-3978.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yoshida H, Bogaki M, Nakamura M, Nakamura S. Quinolone resistance-determining region in the DNA gyrase gyrA gene of Escherichia coli. Antimicrob Agents Chemother. 1990;34:1271–1272. doi: 10.1128/aac.34.6.1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yoshida H, Bogaki M, Nakamura M, Yamanaka L M, Nakamura S. Quinolone resistance-determining region in the DNA gyrase gyrB gene of Escherichia coli. Antimicrob Agents Chemother. 1991;35:1647–1650. doi: 10.1128/aac.35.8.1647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zirnstein G, Li Y, Swaminathan B, Angulo F. Ciprofloxacin resistance in Campylobacter jejuni isolates: detection of gyrA resistance mutations by mismatch amplification mutation assay PCR and DNA sequence analysis. J Clin Microbiol. 1999;37:3276–3280. doi: 10.1128/jcm.37.10.3276-3280.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]