Abstract
Cinnamon has been used as a flavoring and medicinal agent for centuries. Much research has focused on cinnamon bark powder, which contains antioxidants, flavonoids, carotenoids, vitamins, minerals, fiber, and small amounts of essential oil. However, isolated and concentrated cinnamon essential oil may also have important medicinal qualities, particularly in antidiabetic therapy. Some of the most common essential oil constituents identified in the literature include cinnamaldehyde, eugenol, and beta-caryophyllene. Due to their high concentration in cinnamon essential oil, these constituents are hypothesized to have the most significant physiological activity. Here, we present a brief review of literature on cinnamon oil and its constituents as they relate to glucose metabolism and diabetic pathogenesis. We also present molecular docking simulations of these cinnamon essential oil constituents (cinnamaldehyde, eugenol, beta-caryophyllene) that suggest interaction with several key enzymes in glucometabolic pathways.
Keywords: cinnamon, cinnamon essential oil, molecular docking, antidiabetic, glucose metabolism, cinnamaldehyde, beta-caryophyllene, eugenol
1. Introduction
Essential oils are complex mixtures of small, aromatic molecules produced by many plant taxa as secondary metabolites related to normal metabolic processes [1,2]. The diverse composition of these secondary metabolites is thought to reflect both genetic species’ individuality as well as an adaptation mechanism for plants to cope with environmental stressors such as pathogens, unfavorable temperature and pH, drought, high salinity, ultraviolet radiation, heavy-metal stress, and nutrient depletion [2,3]. Additionally, these molecules may be used by the plant for defense against herbivores and as an attractant for pollinators. Essential oil compounds are stored in microscopic sacs or glands in various parts of the plant.
Essential oil terpenoids are based on a basic isoprene unit: five carbons, (two of which are double-bonded) and eight hydrogens. Monoterpenes consist of two isoprene units bonded together (10 carbons), and sesquiterpenes are three isoprene units (15 carbons). Occasionally, heavier diterpene (4 isoprene units, 20 carbons) molecules can be represented in cold-pressed or solvent-extracted essential oils, but these molecules tend to be too heavy to be carried over by the steam during typical distillation. Monoterpenes and sesquiterpenes can either be straight-chain (acyclic) or contain various ring structures (monocyclic, bicyclic, etc.), and there is considerable variety in these structures. Most volatile essential oil compounds are produced along canonical biochemical pathways (see Table 1) from a variety of precursor molecules, including amino acids, carbohydrates, and fatty acids and their derivatives [4,5].
Table 1.
Canonical Biochemical Pathways for Production of Volatile Compounds in Plants.
| Biochemical Pathway | Classes of Compounds Produced |
Examples |
|---|---|---|
| Mevalonate | Terpenes and terpenoids | Beta-caryophyllene, limonene, pinenes, geraniol |
| Non-mevalonate, also called methylerythritol phosphate (MEP) | ||
| Shikimate | Alkaloids, phenylpropanoids, flavonoids, lignans, aromatic polyketides | Cinnamaldehyde, eugenol, coumarin |
| Derivation of fatty acids | Fatty alcohols | Octanol, decanol |
Some essential oils have been studied for their antidiabetic potential [6,7,8,9,10]. The US Centers for Disease Control reports that about 34.2 million people (around 10% of the total population) in the United States have diabetes, and about one in five of those people do not realize they have the disease [11]. Diabetics are at much higher risk of early mortality as well as comorbidities such as blindness, renal disease, heart disease, stroke, and lower-limb amputations [12]. New drugs based on complex mixtures of natural compounds may offer therapeutic potential for treatment of diabetes.
Understanding the interaction between small molecules and possible enzyme binding sites is key in discovering novel therapeutics [13]. The field of In silico modeling is becoming an important player in early-stage drug discovery to suggest possible interactions between ligands and proteins of interest, as well as predict the relative strength of those interactions.
The goal of this article is two-fold: (1) outline existing literature on anti-diabetic potential of cinnamon essential oil and its main constituents; and (2) through molecular docking simulations, suggest possible mechanisms of glucose metabolism modulation by cinnamon essential oil.
2. Cinnamon Essential Oil and Its Constituents
Cinnamon has been used as a flavoring and medicinal agent for centuries, with references back to Biblical times [14]. Medicinally, cinnamon has been used as a carminative and treatment for digestive issues such as dyspepsia, anorexia, and vomiting [15]. Other anecdotal uses of cinnamon include treatment for hemorrhage and bleeding ulcers [16], as a warming agent and stimulant [17], and treatment against various cancers [18]. Modern investigations have focused primarily on cinnamon’s antidiabetic and antilipidemic properties, although the therapeutic benefit and dosing parameters require further exploration [19]. Much of this research involves cinnamon bark powder, which contains small amounts of cinnamon essential oil along with antioxidants, flavonoids, carotenoids, vitamins, minerals, and fiber. However, concentrated, volatile cinnamon essential oil may also have important medicinal qualities.
There may be more than 200 Cinnamomum species, but several species of cinnamon have been identified as culturally or economically relevant: Cinnamomum zeylanicum (botanical synonym: C. verum, also called Ceylon cinnamon or true cinnamon), C. cassia, C. burmannii, C. tamala, C. loureirii, C. iners, C. pauciflorum, C. camphora and C. glaucescens [20]. Each species yields an essential oil of different chemistry and aroma. Only C. zeylanicum (Ceylon cinnamon) and C. cassia are currently produced on a commercial scale.
Cinnamomum zeylanicum trees are slender evergreens that can reach up to 65 feet in height. Cinnamon bark is harvested from the inner cambium of trees typically 3–4 years old. Trees are pruned repeatedly in order to curtail height for easier harvesting and encourage lateral growth of shoots suitable for collection [14,21]. Curls of bark (called quills) are cut from the tree and allowed to dry. Essential oil sacs are located within the cambium and tend to be in the range of 2–10 microns in diameter. Essential oil yield is about 1–4% from the cinnamon bark.
Cinnamon essential oil is a volatile, hydrophobic, mildly viscous liquid, usually yellowish in color. It has a sweet, spicy, woody aroma. The volatile oil is typically isolated by hydrodistillation from bark or leaves of cinnamon trees [22]. Physical characteristics are represented in Table 2. Both monoterpenes and sesquiterpenes, and their functional variations, are present in cinnamon essential oil. Several important cinnamon essential oil constituents identified in the literature include cinnamaldehyde, eugenol, and beta-caryophyllene [23]. These constituents are usually present in appreciable amounts in cinnamon oil, and will be the focus of this paper.
Table 2.
| Cinnamon Essential Oil | ||
|---|---|---|
| Physical Property | Typical Value | Range |
| Optical Rotation | −1 | −20–+20 |
| Specific Gravity | 1.02 | 1.01–1.07 |
| Refractive Index | 1.59 | 1.53–1.61 |
| Flash Point | 87 °C | 62–104 °C |
| Boiling Point | 248 °C | 248–249 °C |
| Color | Dark yellow | Yellow to light brown |
| Aroma | Spicy, sweet | Spicy, sharp, woody |
Cinnamaldehyde (3-phenylprop-2-enal) is a phenylpropanoid naturally synthesized along the shikimate pathway in plants from the precursor amino acid phenylalanine [26]. The molecule has the chemical formula C9H8O and contains a benzene ring, a short carbon chain, and an aldehyde group [27]. Both cis- and trans-cinnamaldehyde conformations exist in nature, but the majority of cinnamaldehyde in cinnamon bark tends to be the trans- stereoisomer. This constituent of cinnamon oil represents approximately 50–90% of total chemical makeup, depending on the species and plant part from which it was derived. Cinnamaldehyde is the primary contributor of the sweet, spicy aroma typically associated with cinnamon essential oil. However, as is often the case, multiple constituents contribute to the rich and complex aroma that distinguishes whole cinnamon bark essential oil from isolated cinnamaldehyde [28].
Eugenol (4-allyl-2-methoxyphenol) is a phenylpropanoid derived from guaiacol with an allyl chain substitution [29]. It is a member of the phenol class of compounds, synthesized along the shikimate pathway from the precursor amino acid phenylalanine. The molecule has the chemical formula C10H12O2 and contains a benzene ring, with a hydroxy group and an ether group in ortho-conformation and the allyl chain para to the hydroxy group. Eugenol is the main constituent of essential oil derived from cinnamon leaf, while in essential oil derived from bark, it is typically present in about 2–13% (see Table 3).
Table 3.
Comparative constituents of several cinnamon species. Common constituents in cinnamon essential oil extracted from various plant parts of Cinnamomum zeylanicum and Cinnamomum cassia [22,23,31,32,33,34].
| C. zeylanicum Bark | Composition | C. zeylanicum Leaf | Composition | C. cassia Bark | Composition | C. cassia Leaf | Composition |
|---|---|---|---|---|---|---|---|
| (E)-Cinnamaldehyde | 44.2–75.7% | Eugenol | 68.6–87.0% | (E)-Cinnamaldehyde | 42.4–89.4% | (E)-Cinnamaldehyde | 54.6–90.1% |
| Eugenol | 1.6–13.3% | Eugenyl acetate | 1.0–8.1% | (Z)-Cinnamaldehyde | 0.6–12.3% | (E)-Cinnamyl acetate | 1.4–12.5% |
| (E)-Cinnamyl acetate |
0.3–10.6% | Linalool | 0.2–5.0% | (E)-Cinnamyl acetate |
0.1–5.4% | (Z)-Cinnamaldehyde | 0.4–10.5% |
| Linalool | 0.2–7.0% | (E)-Cinnamyl acetate |
0.8–4.6% | Benzaldehyde | 0.4–2.3% | Benzaldehyde | 1.1–6.3% |
| beta-Phellandrene | 1.5–8% | Benzyl benzoate | trace–4.1% | alpha-Terpineol | trace–2.0% | Eugenol | trace–5.8% |
| Beta-Caryophyllene | 1.3–6.9% | Beta-Caryophyllene | 1.9–4.1% | Coumarin | trace–1.9% | Cinnamyl alcohol |
0–5.7% |
| p-Cymene | 1.7–4.0% | Safrole | 0–1.3% | Salicylaldehyde | 0.04–1.8% | Salicylaldehyde | 0.05–3.1% |
| 1,8-Cineole | 0.4–2.3% | (E)-Cinnamaldehyde | 0.6–1.1% | Borneol | trace–1.3% | ⍺-copaene | trace–3.0% |
| Benzaldehyde | trace–2.2% | p-Cymene | 0.3–0.8% | Benzyl benzoate | trace–1.0% | Benzyl benzoate | trace–2.9% |
| alpha-Terpineol | 0.4–1.6% | Cinnamyl alcohol | 0–0.6% | Cinnamyl alcohol | 0–0.04% | Delta-Cadinene | trace–2.6% |
| Camphor | trace–1.4% | 1,8-Cineole | trace–0.6% | Coumarin | 0.03–2.5% | ||
| Beta-Phellandrene | 0.2–0.5% | Phenylpropanol | trace–1.6% | ||||
| ⍺-Amorphene | trace–1.1% | ||||||
| Anisaldehyde | 0–1.0% | ||||||
| (E)-Cinnamic acid | trace–0.9% | ||||||
| Methyl eugenol | trace–0.1% |
Beta-caryophyllene, or (-)-trans-caryophyllene, is a bicyclic sesquiterpene found in several plants used for spice and flavoring, including cinnamon [30]. This molecule is produced along the mevalonate pathway in plants from precursor molecules of acetyl-CoA. In nature, beta-caryophyllene occurs along with alpha-humulene (formerly called alpha-caryophyllene), which has a ring-opened structure. Due both to its unique nine-membered double-ring structure, which is uncommon in nature, as well as its desirable sweet aroma and taste, beta-caryophyllene has attracted attention as a subject of research. In cinnamon oil, beta-caryophyllene is typically present at less than 10%.
3. Literature Review of Antidiabetic Properties of Cinnamon Essential Oil and Its Constituents
Table 4 outlines representative publications that specifically study the effects of cinnamon essential oil and its main chemical constituents on glucose metabolism pathways and diabetic endpoints. This review is not comprehensive for all preparations or uses of cinnamon. Specifically, we review studies that include distilled or hydrodistilled cinnamon volatile oil or isolated cinnamon oil constituents (specifically, cinnamaldehyde, eugenol, and beta-caryophyllene) for antidiabetic potential.
Table 4.
Experimental data for antidiabetic activity of cinnamon oil and some of its main constituents.
| Study Product | Study Type | Dosage | Effect | Reference |
|---|---|---|---|---|
| Cinnamon oil | Animal (Rat), KK-Ay | 25, 50, 100 mg/kg b.w. |
Significant decrease in fasting blood glucose, plasma C-peptide, serum triglyceride, total cholesterol, and blood urea nitrogen levels, with significant increase in high-density lipoprotein after 35 days. Glucose tolerance was improved and pancreatic islet β-cells showed increased immunoreactivity. |
Ping, Zhang, and Ren (2010) [7] |
| Cinnamon oil (encapsulated emulsion) | Animal (Rat), STZ | 200 or 400 mg/kg b.w. |
Both doses improved levels of glucose, insulin, SOD, GSH, amylase, lipid profile, and hepatic MDA. Gene expression was modulated to favor antidiabetic outcomes. Positive histological changes seen in liver and pancreas. | Mohammed, Ahmed, Sharaf, El-Nekeety, Abdel-Aziem, Mehaya, Abdel-Wahhab (2020) [35] |
| Cinnamon oil (encapsulated) |
Animal (Rat), STZ | 200 or 400 mg/kg b.w. |
Treatment with encapsulated cinnamon oil showed improvement in all diabetes-related markers in STZ-treated rats, including liver and kidney function, insulin and glucose levels, lipid profile, and antioxidant enzymes. | Mohammed (2020) [36] |
| Cinnamon oil | Animal (Rat), Alloxan | 5, 10, 20 mg/kg b.w., i.p. | Decreases in fasting blood glucose, total cholesterol, markers of kidney damage and glutathione were observed in treated animals. Histological studies of kidney showed reduced glomerular expansion and tubular dilatations. | Mishra, Bhatti, Singh, Ishar (2010) [37] |
| Cinnamon oil | Animal (Rat), STZ | 100, 200, or 400 mg/kg b.w. | Treatment with cinnamon oil showed significant improvement in histopathology of testicular organs compared to untreated diabetic rats. | Budiastuti, Safitri, Plumeriastuti, Srianto, Effendi (2020) [38] |
| Cinnamon oil | Human | 400 mg/day | Fasting blood glucose levels and insulin levels, along with Quality-of-Life measures, showed improvement after treatment with cinnamon oil, although results were not statistically significant. Pharmacokinetic data indicated low bioavailability. | Stevens (2020) [28] |
| Cinnamon oil | Animal (Mouse), Balb C |
0.2 and 1.0 μL/cage, inhalation |
Docking simulations showed interaction of cinnamon oil constituents with leptin receptor in olfactory bulb. In vivo studies confirmed interaction with leptin receptor resulting in decreased appetite and lower weight gain in treated mice. | Kusmardi, Tedjo, Fadilah, Arsianti, Paramita (2018) [39] |
| Cinnamon oil | Animal (Rat), STZ | 5% cinnamon oil in commercial chow | Treatment with cinnamon oil resulted in decreased blood glucose, triglycerides, LDL-cholesterol, and ALT, while levels of HDL-cholesterol were increased compared to diabetic rats. | Zari, Al-Logmani (2009) [40] |
| Cinnamon oil | Animal (Rat), Alloxan | 5, 10, 20 mg/kg b.w., i.p. | Cinnamon oil significantly ameliorated blood glucose levels and thermal hyperalgesia compared to untreated diabetic controls. | Bhatti, Kaur, Singh, Ishar (2009) [41] |
| Cinnamaldehyde | In vitro (HEK293 and 3T3-L1) | -- | Cinnamaldehyde induced expression of peroxisome proliferator-activated (PPAR) genes in 3T3-L1 adipocytes and increased target mRNA expression in HEK293- derived cells. |
Li, Futakawa, Yamamoto, Kasahara, Tagami, Liu, and Moriyama (2015) [42] |
| Cinnamaldehyde | Animal (Mouse), DIO-mice | 250 mg/kg/day | Cinnamaldehyde induced significant reduction in cumulative food intake, gastric emptying rates, and ghrelin. Upregulation of genes involved in fatty-acid oxidation was observed in adipose tissue, and mice showed improved glucose tolerance over 5 weeks. |
Camacho, Michlig, de Senarclens-Bezencon, Meylan, Meystre, Pezzoli, Markram, le Coutre (2015) [43] |
| Cinnamaldehyde | Animal (Mouse), db/db | 0.02% added to normal chow diet |
Treatment with cinnamaldehyde improved aortic tone and function and normalized elevated kidney markers. Treatment also ameliorated glomerular fibrosis and renal dysfunction. Authors suggest a protective effect against vascular dysfunction by inhibiting oxidative stress via Nrf2 signaling pathway activation. | Wang, Yang, Wang, Yang, Wan, Liu, Zhou, Yang (2020) [44] |
| Cinnamaldehyde | Animal (Rat), STZ | 20 mg/kg b.w. | Oral administration led to insulinotropic effects, with increased glucose uptake through GLUT4 receptors and improved function of pyruvate kinase and phosphoenolpyruvate carboxykinase. |
Anand, Murali, Tandon, Murthy, Chandra (2010) [45] |
| Cinnamaldehyde | Animal (Rat), FSD/STZ | 20 mg/kg b.w. | Gestating rats treated with cinnamaldehyde showed numerous improvements in health markers compared to diabetic controls, including improved lipid panels and glucose tolerance, more viable fetuses, and improved fetal glucose and insulin levels. | Hosni, Abdel-Moneim, Abdel-Reheim, Mohamed, Helmy (2017) [46] |
| Cinnamaldehyde | Animal (Rat), FSD/STZ | 20 mg/kg b.w. | In rats with gestational diabetes, treatment with cinnamaldehyde prevented development of placental vasculopathy and fetal hypoxia while also alleviating maternal and fetal hyperglycemia. | Hosni, El-Twab, Abdul- Hamid, Prinsen, AbdElgwad, Abdel-Moneim, Beemster (2021) [47] |
| Cinnamaldehyde | Animal (Mouse), STZ | 20 mg/kg/day | Treated mice showed significantly improved insulin sensitivity and glucose metabolism, as well as positive changes in gut microbiota. Authors suggest that modulating host metabolomics may directly or indirectly affect expression levels of genes related to glucose metabolism. | Zhao, Wu, Duan, Liu, Zhu, Zhang, Wang (2021) [48] |
| Cinnamaldehyde | Animal (Rat), STZ | 20 mg/kg/day | Treatment with cinnamaldehyde prevented development of hyperglycemia and insulin resistance following STZ administration. | El-Bassossy, Fahmy, Dadawy (2011) [49] |
| Cinnamaldehyde | Animal (Rat), STZ | 10, 20, 40 mg/kg b.w., p.o. |
Rats treated with cinnamaldehyde showed reduced blood glucose levels and amelioration of neurochemical and behavioral deficits seen in diabetic rats. Reductions in IL-2 and TNF-⍺ levels were also noted. | Jawale, Datusalia, Bishnoi, Sharma (2016) [50] |
| Cinnamaldehyde | Rat | 125, 250, 500 mg/kg b.w. | Pharmacokinetic determination of Cmax in rats administered 125, 250, and 500 mg/kg b.w. cinnamaldehyde was 249, 121, and 82 ng/mL serum, respectively. Estimated half-life of cinnamaldehyde was 6.2–6.9 h. | Zhao, Xie, Yang, Cao, Tu, Cao, Wang (2014) [51] |
| Eugenol | Animal (Mouse), STZ | 100 mg/kg b.w. i.p., 2× per week for 2 weeks | Significant reduction in advanced glycation end-products (AGE) and blood glucose levels. |
Singh et al. (2014) [52] |
| Eugenol | Animal (Rat), STZ | Treatment with eugenol produced lower blood glucose, decrease in serum glycosylated hemoglobin (HbA1C), lipase, and angiotensin-converting enzyme. Lipid panel levels were also positively affected. | Mnafgui et al. (2013) [53] | |
| Eugenol | Animal (Rat), STZ | 2.5, 5, 10 mg/kg b.w. |
Eugenol improved blood glucose and HbA1C levels in diabetic rats and returned glucose metabolism enzyme levels to near normal. Body weight and liver function also improved. | Srinivasan et al. (2013) [54] |
| Eugenol | Animal (Rat), FSD/STZ | 10 mg/kg b.w. | Levels of fasting blood glucose, insulin, triglyceride, cholesterol, and low-density lipoprotein were all improved. Glutathione levels were increased, as were GLUT4 and AMPK levels in skeletal muscle. Homeostasis model assessment of insulin resistance (HOMA-IR) was significantly lower in rats treated with eugenol compared to diabetic controls. | Al-Trad, Alkhateeb, Alsmadi, Al-Zoubi (2019) [55] |
| Eugenol | Animal (Rat), HFD | 20, 40 mg/kg b.w. |
Plasma glucose and insulin levels decreased in a dose-dependent manner, and hepatic gluconeogenesis was inhibited via the CAMKK-AMPK-CREB signaling pathway. | Jeong, Kim, Quan, Jo, Kim, Chung (2014) [56] |
| Eugenol | Animal (Rat), STZ | 5, 10 mg/kg b.w. |
Diabetic neuropathy parameters (both blood markers and histological changes) were ameliorated in diabetic rats treated with eugenol. Overexpression of TGF-β1 associated with diabetes was also reduced. | Garud, Kulkarni (2017) [57] |
| Eugenol | Animal (Rat), STZ | 10 mg/kg b.w. |
Diabetic rats treated with eugenol showed diminished oxidative stress markers and increased antioxidants. In the brain, levels of acetylcholinesterase and calcium were attenuated. Authors postulate that eugenol may help ameliorate diabetic complications due to oxidative stress. | Prasad, Bharath, Muralidhara (2016) [58] |
| Eugenol | Animal (Rat), STZ | 2 mL/day of a 10% nanoemulsion |
Oxidative damage was attenuated, and levels of antioxidants were returned to near-normal levels in diabetic rats compared to untreated controls. | Boroujeni, Dehkordi, Sharifi, Taghian, Mazaheri (2021) [59] |
| Eugenol | In vitro (Islets of Langerhans cells from male mouse) | 50, 100, 200 μM | Total antioxidant capacity, superoxide dismutase, and catalase levels increased in cells treated with eugenol following exposure to hydrogen peroxide to induce oxidative stress. Eugenol can bolster antioxidant systems in islet cells that are particularly vulnerable to oxidative stress in diabetics. | Oroojan, Chenani, An’aam (2020) [60] |
| Eugenol | Animal (Rat), Alloxan | 5, 10, 15 mg/kg b.w. | Diabetic rats treated with eugenol showed lower fasting blood glucose, and improved morphology of liver and islet of Langerhans cells. | Hamdin, Utami, Muliasari, Prasedya, Sudarma (2019) [61] |
| β-caryophyllene | In silico | -- | β-caryophyllene showed affinity for interaction with insulin downstream signaling molecules such as IRS-1, cSrc, and Akt. | Mani, Balraj, Venktsan, Soundrapandiyan, Kasthuri, Danavel, Babu (2021) [62] |
| β-caryophyllene | Animal (Rat), STZ | 10 mg/kg b.w. |
Diabetic neuropathy was attenuated in rats treated with β-caryophyllene. Depression behavior and cytokine markers of diabetes were also reduced. | Aguilar-Ávila, Flores-Soto, Tapia-Vázquez, Pastor-Zarandona, López-Roa, Viveros-Paredes (2019) [63] |
| β-caryophyllene | Animal (Rat), STZ | 200 mg/kg b.w. |
Hyperglycemia was attenuated by treatment with β-caryophyllene, and oxidative stress was avoided through increased activity of antioxidant enzymes. | Basha, Sankaranarayanan (2016) [64] |
| β-caryophyllene | Animal (Rat), STZ | 200 mg/kg b.w. |
Plasma insulin levels were rescued to near-normal levels in diabetic rats treated with β-caryophyllene. | Basha, Sankaranarayanan (2015) [65] |
| β-caryophyllene | Animal (Rat), STZ | 100, 200, 400 mg/kg b.w. | Administration of β-caryophyllene ameliorated STZ-induced changes in blood glucose, insulin levels, and glucose metabolism enzymes. The antidiabetic and insulinotropic effects were most pronounced at the 200 mg/kg dose. | Basha, Sankaranarayanan (2014) [66] |
| β-caryophyllene | Animal (Rat), HFD | 30 mg/kg b.w. |
Treatment with β-caryophyllene improved glycemic and lipidemic markers and reduced vascular oxidative stress and inflammation. |
Youssef, El-Fayoumi, Mahmoud (2019) [67] |
| β-caryophyllene | In vitro (mesangial cells) | -- | β-caryophyllene modulated NF-κB and Nrf pathways and exhibited anti-inflammatory and nephroprotective activity in mesangial cells under high-glucose conditions. | Li, Wang, Chen, Yang (2020) [68] |
| β-caryophyllene | In vitro (C2C12 myotubes) | -- | β-caryophyllene significantly increased skeletal muscle uptake of glucose and glycolytic production of ATP through cannabinoid receptor-2-mediated pathways. | Geddo et al. (2021) [69] |
Studies on cinnamon essential oil demonstrate improvement of fasting blood glucose, fasting insulin, and improvement in both anatomy and function of kidney and liver cells. Improvement in enzyme function, both enzymes involved directly in glucose metabolism and enzymes involved in excretion, was also consistently noted. Studies including cinnamaldehyde also showed improvement of fasting blood glucose, increased insulin sensitivity, decreased appetite, and both up- and down-regulation of myriad proteins associated with glucose metabolism.
While most current in vitro and in vivo research focuses on cinnamaldehyde as the primary therapeutic agent in cinnamon oil, other constituents may also play a supporting role in this oil’s observed antidiabetic properties. Eugenol and beta-caryophyllene both show promising therapeutic benefits when tested in animal models. Research outlined in Table 4 suggests these constituents may function by enhancing native antioxidant systems and ameliorating oxidative damaged caused by development of diabetes.
Research to date suggests that cinnamon essential oil may have therapeutic benefit in modulating glucose metabolism along multiple pathways. Additional in vitro and in vivo studies are needed (particularly human clinical trials) to fully elucidate the activity and mechanisms of cinnamon oil’s potential antidiabetic effect.
Next, using In silico molecular modeling, we attempt to predict possible enzymatic mechanisms through which main constituents of cinnamon essential oil may exert effects. Models will also provide estimated binding affinities that forecast the likelihood of spontaneous interaction between ligand and target. These models offer an initial framework for further in vitro and in vivo validation.
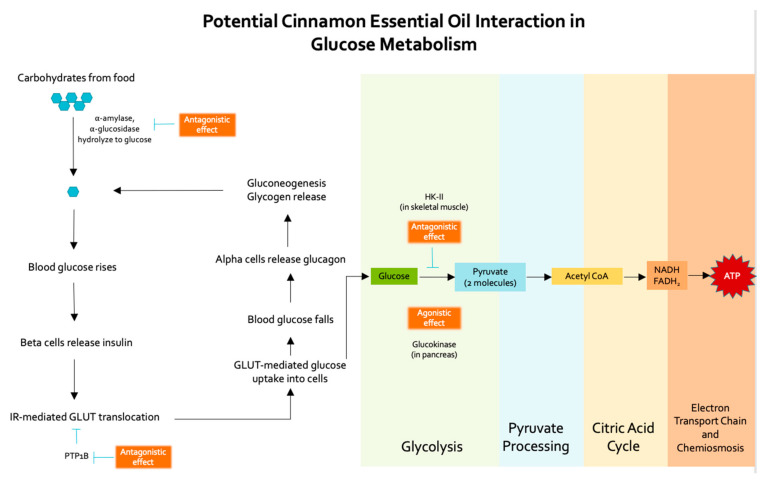
4. In Silico Docking Models
Three cinnamon essential oil constituents, cinnamaldehyde, eugenol, and beta-caryophyllene, combined comprise 60–70% of cinnamon essential oil. As suggested by the literature and because of their concentration in oil, these constituents are hypothesized to have the most significant physiological effects. Thus, cinnamaldehyde, eugenol, and beta-caryophyllene were selected for molecular docking analysis and simulated against enzymes involved in glucose metabolism or the glycolysis pathway (glucokinase, alpha-amylase, PTP1B, alpha-glucosidase, and hexokinase-II (HK-II). Hypothesized interactions of essential oil constituents with these glucose metabolism enzymes are represented in Figure 1.
Figure 1.
Hypothesized interactions of cinnamon essential oil constituents with enzymes along glucose metabolism pathways.
As interactions with small molecules can result in a variety of enzymatic responses, it is important to note the overall effect of the binding model. Most commonly, a xenobiotic substance can be:
Agonistic: behaving like the natural ligand, agonist molecules bind to the receptor and trigger signaling. When a small molecule is simulated to bind in the same active site as a drug or mimetic with known biological effects, it is considered an agonist.
Antagonistic: inhibiting the effect of the natural ligand or agonist by blocking the active site of the enzyme (competitive agonist), by binding elsewhere on the enzyme and altering the biological function (noncompetitive antagonist), or by covalently altering the binding site (irreversible agonist). A small molecule binding in this manner would inhibit the activity of the enzyme and alter downstream pathway outcomes.
In the case of glucose metabolism enzymes, both agonistic and antagonistic activities may be useful therapeutics for treating Type II Diabetes. In alpha-amylase and alpha-glucosidase, antagonistic effects from essential oil constituents are desirable; specifically, small molecules bind in the active site and block the binding and subsequent hydrolysis of the physiologic ligands (complex carbohydrates). Essential oil constituents shown to interact at this site may serve to slow the rise in blood glucose following food intake.
In PTP1B, antagonistic effects from essential oil constituents are also desirable. Specifically, small molecules bind in the active site and block the binding of the natural ligand (phosphate group on insulin receptors [70]). This effectively inhibits the PTP1B enzyme, allowing the insulin receptor to remain phosphorylated, and ultimately allowing increased GLUT4 translocation to the cell surface. If essential oil constituents bind at this site, lower blood glucose levels may result as a higher volume of glucose molecules is cleared from the blood through uptake by GLUT4.
In glucokinase, the natural ligand (glucose) is converted to glucose-6-phosphate as the initial step in glycolysis, and this process is an important regulator in insulin release and glucose metabolism [71]. Glucokinase serves as both a glucose sensor in pancreatic beta-cells and as a rate-controlling enzyme for glycogen synthesis and hepatic glucose clearance [72]. For this enzyme, activation is hypothesized to occur through ligand binding at an allosteric site rather than the active site. This allows the active site to remain available for glucose metabolism. Small molecules, such as essential oil constituents, that can bind in the allosteric pocket could serve glucokinase agonists, increasing glucose metabolism and allowing for more sensitive glucose homeostasis.
Hexokinases catalyze the conversion of glucose to glucose-6-phosphate, the first step in many glucose metabolism pathways. Overexpression of hexokinase is common in certain cancers due to its ability to reduce serum levels of glucose, insulin, and insulin-like growth factor [73]. Antagonistic reduction in hexokinase activity has therapeutic implications for diabetes as well; the drug metformin works in part by reducing activity of hexokinase. HK-II is the predominant form found in skeletal muscle and is insulin-dependent. Recently, a compound called benserazide has demonstrated ability to selectively inhibit HK-II [74]; other compounds binding in the same site as HK-II antagonists could provide new therapeutic targets for diabetes.
5. Materials and Methods
Molecular Docking
In silico molecular docking simulations were performed using the AutoDock Vina [75] (Scripps Research, La Jolla, CA, USA, version 1.1.2) module within UCSF Chimera [76] (University of California, San Francisco, CA, USA, version 1.13.1). Protein crystal structures were downloaded from Protein Data Bank (www.rcsb.org (accessed on 3 December 2021)). Criteria for crystal structure selection included unmutated proteins from Homo sapiens with complete structure representation and resolution less than or equal to 3 angstroms. Protein models were prepared for docking using the Mac Command Line interface and the Dock Prep tool in UCSF Chimera. Docked models were qualitatively visualized in UCSF Chimera (1.13.1). Ligand structures were downloaded from MolView (molview.org (accessed on 2 December 2021)) prepared for docking within UCSF Chimera.
Modeled enzymes included: alpha-amylase, alpha-glucosidase, glucokinase, PTP1B, and HK-II (PDB ID: 1HNY, 3TOP, 5V4W, 1BZJ, and 2NZT, respectively [77,78,79,80,81]). Simulations were run with essential oil constituents cinnamaldehyde, eugenol, and beta-caryophyllene. Positive controls included known antagonist acarbose for alpha-amylase and alpha-glucosidase, known glucokinase agonist piragliatin, known PTP1B antagonist TPICOOH, and known HK-II antagonist, benserazide [74].
6. Modeling Results and Discussion
Models were initially evaluated by strength of predicted interactions. Proteins were probed for interaction with essential oil constituents or a positive control both at active sites and at possible allosteric binding locations. Binding affinities that were estimated to have a change in Gibbs free energy (ΔG) of −6.0 kcal/mol or more negative were considered to represent activity through spontaneous physiologic interaction [82].
All simulated binding affinities are represented in Table 5. Overall, beta-caryophyllene showed the highest binding affinity across multiple proteins. Cinnamaldehyde and eugenol also showed potential interaction with select proteins.
Table 5.
Binding affinities of cinnamon essential oil constituents against selected glucose metabolism enzymes (all results in units of kcal/mol).
| Essential Oil Ligand | PTP1B | α-Glucosidase | Glucokinase | α-Amylase | HK-II |
| β-caryophyllene | −5.6 | −6.6 | −6.3 | −6.9 | −6.6 |
| Cinnamaldehyde | −6.5 | −6.1 | −5.8 | −5.4 | −5.5 |
| Eugenol | −6.0 | −6.7 | −6.0 | −5.6 | −5.6 |
| Positive Controls | PTP1B | α-Glucosidase | Glucokinase | α-Amylase | HK-II |
| Acarbose | -- | −8.3 | -- | −7.3 | -- |
| Piragliatin | -- | -- | −9.5 | -- | -- |
| TPICOOH | −9.7 | -- | -- | -- | -- |
| Benserazide | -- | -- | -- | -- | −7.4 |
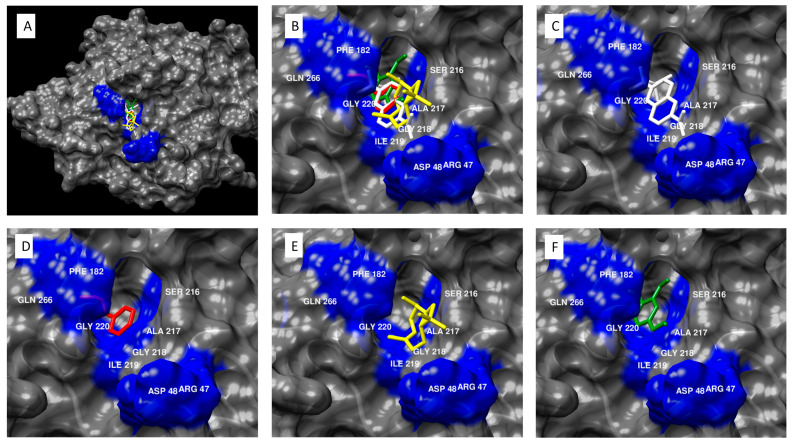
The PTP1B active site includes the following residues (Figure 2): ARG 47, ASP 48, PHE 182, SER 216, ALA 217, GLY 218, ILE 219, GLY 220, ARG 221, and GLN 266 [80]. Binding in the active site of PTP1B serves to inhibit the enzyme (which itself inhibits the insulin receptor-mediated GLUT4 translocation to the membrane). Cinnamaldehyde and eugenol from cinnamon essential oil showed binding affinity for the PTP1B active site. These constituents demonstrated binding affinities stronger than −6.0 kcal/mol, indicating a high likelihood that the binding reaction will occur spontaneously. While none of the modeled essential oil constituents demonstrated binding affinities as strong as the positive control, known PTP1B antagonist TPICOOH, it is interesting to consider the implications of an essential oil with broad chemistry that may be able to interact along multiple points of a pathway and with several different constituents.
Figure 2.
Molecular modeling of cinnamon essential oil constituents docked with PTP1B. (A) PTP1B antagonist TPICOOH and essential oil compounds cinnamaldehyde, beta-caryophyllene, and eugenol docked in the active site of PTB1B. (B) Close view of PTB1B antagonist TPICOOH and essential oil compounds cinnamaldehyde, beta-caryophyllene, and eugenol docked in the active site of PTB1B, specifically, near residues ARG47, ASP48, PHE182, SER216, ALA217, GLY218, ILE219, GLY220, ARG221, and GLN266. (C) TPICOOH docked in the active pocket of PTB1B, with a binding affinity of −9.7 kcal/mol. (D) Cinnamaldehyde docked in the active pocket of PTB1B, with a binding affinity of −6.5 kcal/mol. (E) Beta-caryophyllene docked in the active pocket of PTB1B, with a binding affinity of −5.6 kcal/mol. (F) Eugenol docked in the active pocket of PTB1B, with a binding affinity of −6.0 kcal/mol.
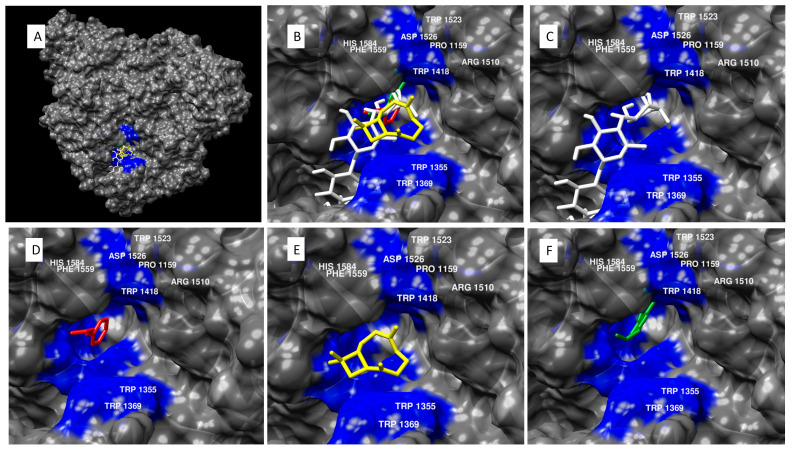
Alpha-glucosidase inhibition takes place at the active pocket (Figure 3), which includes the following residues: HIS 1584, ASP 1279, TYR 1251, TRP 1523, TRP 1418, ARG 1510, TRP 1355, PHE 1559, ASP 1526, TRP 1369, and PRO 1159 [78]. Acarbose, a known alpha-glucosidase antagonist and frontline drug in diabetic therapy [83], was shown to bind in the same pocket. Once again, two of the main constituents from cinnamon essential oil (cinnamaldehyde and eugenol) showed △G more negative than −6.0 kcal/mol.
Figure 3.
Molecular modeling of cinnamon essential oil constituents docked with alpha-glucosidase. (A) Alpha-glucosidase antagonist acarbose and essential oil compounds cinnamaldehyde, beta-caryophyllene, and eugenol docked in the active site of alpha-glucosidase. (B) Close view of alpha-glucosidase antagonist acarbose and essential oil compounds cinnamaldehyde, beta-caryophyllene, and eugenol docked in the active site of alpha-glucosidase, specifically, near residues HIS 1584, TRP 1523, TRP 1418, ARG 1510, TRP 1355, PHE 1559, ASP 1526, TRP 1369, and PRO 1159. (C) Acarbose docked in the active pocket of alpha-glucosidase, with a binding affinity of −8.3 kcal/mol. (D) Cinnamaldehyde docked in the active pocket of alpha-glucosidase, with a binding affinity of −6.1 kcal/mol. (E) Beta-caryophyllene docked in the active pocket of alpha-glucosidase, with a binding affinity of −6.6 kcal/mol. (F) Eugenol docked in the active pocket of alpha-glucosidase, with a binding affinity of −6.7 kcal/mol.
The active site of the alpha-amylase enzyme includes the following residues: ASP 197, GLU223, and ASP300 [77] (see Supplemental Materials, Figure S1). Beta-caryophyllene demonstrated notable binding affinity in this active site, at −6.9 kcal/mol, especially considering acarbose interacted at −7.3 kcal/mol at the same site. Cinnamaldehyde and eugenol did not demonstrate significant binding affinity.
For glucokinase binding simulations, essential oil constituents were modeled against the positive control piragliatin, a relatively new glucokinase agonist studied in patients with Type II Diabetes [84,85,86]. All constituents showed qualitative binding in an allosteric site bordered by residues VAL 62, ARG 63, TRP 99, TYR 214, MET 235, LYS 458, LYS 459, and LEU 451 (see Supplemental Materials, Figure S2). This is consistent with modeling conducted by Liu et al. [87], who noted that all known glucokinase agonists bind at the same allosteric site. None of the constituents bound as strongly as the positive control (△G = −9.5 kcal/mol); however, beta-caryophyllene and eugenol demonstrated relatively strong binding affinity (△G = −6.3 and −6.0 kcal/mol, respectively).
In a previous publication, the compound benserazide showed strong inhibition of HK-II, interacting with residues GLY 681, THR 680, and ASN 656 [74] (see Supplemental Materials, Figure S3). In our simulations, benserazide interacted at this site with a binding affinity of −7.4 kcal/mol. Beta-caryophyllene demonstrated comparatively strong binding affinity of −6.6 kcal/mol, while the other essential oil constituents all scored greater than −6.0 kcal/mol. However, beta-caryophyllene and cinnamaldehyde interacted at a different site than the control, so additional in vitro testing is needed to elucidate whether this interaction translates into modulation of enzymatic activity.
7. Limitations
In silico modeling does not replace in vitro and in vivo work; while it predicts possible mechanisms of interaction between essential oil constituents and enzymes of interest, these must be confirmed through additional testing. Modeling software may incorrectly predict binding due to underlying assumptions or errors in protein crystal structure determination. In addition, although docking simulations, in vitro, and in vivo studies all point toward therapeutic antidiabetic activities of cinnamon essential oil and some of its main constituents, high-quality clinical studies are needed to confirm these activities in complex human systems.
8. Conclusions
In vitro, in vivo, and In silico testing indicate that volatile cinnamon oil and some of its main constituents possess antidiabetic properties along different pathways. As reviewed here, numerous studies validate cinnamon oil’s antioxidant properties and suggest that the reduction in oxidative stress is one mechanism through which it may exert antidiabetic effects. In silico molecular docking simulations suggest that constituents in cinnamon essential oil may affect multiple enzymes along glucose metabolism pathways, including alpha-glucosidase, alpha-amylase, PTP1B, glucokinase, and HK-II. While none of the modeled essential oil constituents demonstrated binding affinities as strong as their comparator drugs, they may be able to exert diverse effects across multiple metabolic pathways, potentially increasing net therapeutic benefit. To our knowledge, this is the first In silico study of this set of glucose metabolism enzymes and their theoretical interactions with volatile cinnamon oil constituents, highlighting their antidiabetic potential.
As additional studies are conducted, particularly human clinical trials, the potential therapeutic benefits of volatile cinnamon compounds will be further evaluated. Although cinnamon oil has been part of the human diet in small amounts for millennia and is considered relatively safe, critical safety studies must also be conducted to determine the feasibility of using volatile cinnamon compounds in chronic, therapeutic modalities.
Acknowledgments
The authors would like to thank Brian Lawrence for his valuable contributions on botany and chemistry of Cinnamomum species, and Russell Osguthorpe for his support on the publication.
Supplementary Materials
The following are available online. Figure S1: Molecular modeling of cinnamon essential oil constituents docked with alpha-amylase. (A) Alpha-amylase antagonist acarbose and essential oil compounds cinnamaldehyde, beta-caryophyllene, and eugenol docked in the active site of alpha-amylase. (B) Close view of alpha-amylase antagonist acarbose and essential oil compounds cinnamaldehyde, beta-caryophyllene, and eugenol docked in the active site of alpha-amylase, specifically near residues ASP197, GLU233, and ASP300. (C) Acarbose docked in the active pocket of alpha-amylase, with a binding affinity of −7.3 kcal/mol. (D) Cinnamaldehyde docked in the active pocket of alpha-amylase, with a binding affinity of −5.4 kcal/mol. (E) Beta-caryophyllene docked in the active pocket of alpha-amylase, with a binding affinity of −6.9 kcal/mol. (F) Eugenol docked in the active pocket of alpha-amylase, with a binding affinity of −5.6 kcal/mol. Figure S2: Molecular modeling of cinnamon essential oil constituents docked with glucokinase. (A) Glucokinase agonist piragliatin and essential oil compounds cinnamaldehyde, beta-caryophyllene, and eugenol docked in the active site of glucokinase. (B) Close view of glucokinase agonist piragliatin and essential oil compounds cinnamaldehyde, beta-caryophyllene, and eugenol docked in the active site of alpha-glucosidase, specifically near residues VAL 62, ARG 63, TRP 99, TYR 214, MET 235, LYS 458, LYS 459, and LEU 451. (C) Piragliatin docked in the active pocket of glucokinase, with a binding affinity of −9.5 kcal/mol. (D) Cinnamaldehyde docked in the active pocket of glucokinase, with a binding affinity of −5.8 kcal/mol. (E) Beta-caryophyllene docked in the active pocket of glucokinase, with a binding affinity of −6.3 kcal/mol. (F) Eugenol docked in the active pocket of glucokinase, with a binding affinity of −6.0 kcal/mol. Figure S3: Molecular modeling of cinnamon essential oil constituents docked with hexokinase-II (HK-II). (A) HK-II antagonist benserazide and essential oil compounds cinnamaldehyde, beta-caryophyllene, and eugenol docked in the active site of HK-II. (B) Close view of HK-II antagonist benserazide and essential oil compounds cinnamaldehyde, beta-caryophyllene, and eugenol docked in the active site of HK-II, specifically near residues ASN656, THR680, and GLY681. (C) Benserazide docked in the active pocket of HK-II, with a binding affinity of −7.4 kcal/mol. (D) Cinnamaldehyde docked in the active pocket of HK-II, with a binding affinity of −5.5 kcal/mol. (E) Beta-caryophyllene docked in the active pocket of HK-II, with a binding affinity of −6.6 kcal/mol. (F) Eugenol docked in the active pocket of HK-II, with a binding affinity of −5.6 kcal/mol.
Author Contributions
N.S. was primarily responsible for literature review. K.A. was primarily responsible for docking simulations. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
N.S. and K.A. are employees of dōTERRA International, a company that researches and manufactures essential oils. The authors declare no conflict of interest.
Sample Availability
Samples of the compounds are not available from the authors.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Santos-Sánchez N.F., Salas-Coronado R., Hernández-Carlos B., Villanueva-Cañongo C. Plant Physiological Aspects of Phenolic Compounds. IntechOpen; London, UK: 2019. Shikimic acid pathway in biosynthesis of phenolic compounds. [DOI] [Google Scholar]
- 2.Dewick P. Medicinal Natural Products. John Wiley & Sons; Chichester, UK: 2009. The shikimate pathway: Aromatic amino acids and phenylpropanoids. [Google Scholar]
- 3.Bourgaud F., Gravot A., Milesi S., Gontier E. Production of plant secondary metabolites: A historical perspective. Plant Sci. 2001;161:839–851. doi: 10.1016/S0168-9452(01)00490-3. [DOI] [Google Scholar]
- 4.Sun P., Schuurink R.C., Caissard J.-C., Hugueney P., Baudino S. My Way: Noncanonical Biosynthesis Pathways for Plant Volatiles. Trends Plant Sci. 2016;21:884–894. doi: 10.1016/j.tplants.2016.07.007. [DOI] [PubMed] [Google Scholar]
- 5.Aharoni A., Jongsma M.A., Bouwmeester H.J. Volatile science? Metabolic engineering of terpenoids in plants. Trends Plant Sci. 2005;10:594–602. doi: 10.1016/j.tplants.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 6.Berraaouan A., Abid S., Bnouham M. Antidiabetic oils. Curr. Diabetes Rev. 2013;9:499–505. doi: 10.2174/15733998113096660081. [DOI] [PubMed] [Google Scholar]
- 7.Ping H., Zhang G., Ren G. Antidiabetic effects of cinnamon oil in diabetic KK-Ay mice. Food Chem. Toxicol. 2010;48:2344–2349. doi: 10.1016/j.fct.2010.05.069. [DOI] [PubMed] [Google Scholar]
- 8.Bakirel T., Bakirel U., Keleş O.U., Ulgen S.G., Yardibi H. In vivo assessment of antidiabetic and antioxidant activities of rosemary (Rosmarinus officinalis) in alloxan-diabetic rabbits. J. Ethnopharmacol. 2008;116:64–73. doi: 10.1016/j.jep.2007.10.039. [DOI] [PubMed] [Google Scholar]
- 9.El-Soud N.A., El-Laithy N., El-Saeed G., Wahby M.S., Khalil M., Morsy F., Shaffie N. Antidiabetic activities of Foeniculum vulgare Mill. essential oil in streptozotocin-induced diabetic rats. Maced. J. Med. Sci. 2011;4:139–146. [Google Scholar]
- 10.Verspohl E.J., Bauer K., Neddermann E. Antidiabetic effect of Cinnamomum cassia and Cinnamomum zeylanicum In vivo and in vitro. Phytother. Res. 2005;19:203–206. doi: 10.1002/ptr.1643. [DOI] [PubMed] [Google Scholar]
- 11.National Diabetes Statistics Report | Data & Statistics|Diabetes|CDC. [(accessed on 21 February 2020)]; Available online: https://www.cdc.gov/diabetes/data/statistics/statistics-report.html.
- 12.Diabetes Infographics|Social Media|Press & Social Media|Diabetes|CDC. [(accessed on 21 February 2020)]; Available online: https://www.cdc.gov/diabetes/library/socialmedia/infographics.html.
- 13.de Ruyck J., Brysbaert G., Blossey R., Lensink M.F. Molecular docking as a popular tool in drug design, an In silico travel. Adv. Appl. Bioinform. Chem. 2016;9:1–11. doi: 10.2147/AABC.S105289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Barceloux D.G. Cinnamon (Cinnamomum Species) Dis. A-Mon. 2009;55:327–335. doi: 10.1016/j.disamonth.2009.03.003. [DOI] [PubMed] [Google Scholar]
- 15.Felter H.W., Lloyd J. Kings American Dispensatory. 3rd ed. Volume II Eclectic Medical Publications; Cincinnati, OH, USA: 1898. [Google Scholar]
- 16.Moore M. Specific Indications for Herbs in General Use. 2nd ed. Southwest School of Botanical Medicine; Bisbee, ARI, USA: 1997. [(accessed on 29 November 2021)]. Available online: http://swsbm.henriettesherbal.com/ManualsMM/SpecIndic3.pdf. [Google Scholar]
- 17.Scheid V., Bensky D., Ellis A., Barolet R. Chinese Herbal Medicine: Formulas & Strategies, 2nd Revised Edition. Eastland Press; Vista, CA, USA: 2009. [(accessed on 29 November 2021)]. Available online: https://westminsterresearch.westminster.ac.uk/item/90z76/chinese-herbal-medicine-formulas-strategies-2nd-revised-edition. [Google Scholar]
- 18.Hartwell J.L. Plants used against cancer. A survey. [Continued] Lloydia. 1970;33:97–194. [PubMed] [Google Scholar]
- 19.Abascal K. The Medicinal Uses of Cinnamon. Integr. Med. A Clin. J. 2010;9:28–32. [Google Scholar]
- 20.Baruah A., Nath S.C. Systematics and diversities of Cinammomum species used as “cinnamon” spice in north-east India. J. Econ. Taxon. Bot. 2007;31:872–887. [Google Scholar]
- 21.Anandaraj M., Devasahayam B., Krishnamoorthy B., Matthew P., Rema J. Cinnamon (Extension Pamphlet) Indian Institute of Spices Research; Kozhikode, India: 2005. [(accessed on 16 March 2020)]. Available online: http://iisr.agropedias.iitk.ac.in/sites/default/files/cinnamon.pdf. [Google Scholar]
- 22.Jeyaratnam N., Nour A.H., Kanthasamy R., Nour A.H., Yuvaraj A.R., Akindoyo J.O. Essential oil from Cinnamomum cassia bark through hydrodistillation and advanced microwave assisted hydrodistillation. Ind. Crops Prod. 2016;92:57–66. doi: 10.1016/j.indcrop.2016.07.049. [DOI] [Google Scholar]
- 23.Tisserand R., Young R. Essential Oil Safety: A Guide for Health Care Professionals. 2nd ed. Elsevier Ltd.; Edinburgh, UK: 2013. [Google Scholar]
- 24.Janick J., Whipkey A., editors. Issues in New Crops and New Uses. ASHS Press; Alexandria, VA, USA: 2007. [(accessed on 10 December 2021)]. Available online: https://www.hort.purdue.edu/newcrop/ncnu07/pdfs/koroch338-341.pdf. [Google Scholar]
- 25.PubChem Cassia Oil. [(accessed on 10 December 2021)]; Available online: https://pubchem.ncbi.nlm.nih.gov/compound/6850781.
- 26.Averesch N.J.H., Krömer J.O. Metabolic engineering of the shikimate pathway for production of aromatics and derived compounds—Present and future strain construction strategies. Front. Bioeng. Biotechnol. 2018;6:32. doi: 10.3389/fbioe.2018.00032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.PubChem Cinnamaldehyde. [(accessed on 27 August 2019)]; Available online: https://pubchem.ncbi.nlm.nih.gov/compound/637511.
- 28.Stevens N. Ph.D. Thesis. University of Miami; Miami, FL, USA: 2020. [(accessed on 1 December 2021)]. Cinnamon Bark Essential Oil and a Novel Essential Oil Blend as Potential Modulators of Glucose Metabolism. Available online: https://scholarship.miami.edu/esploro/outputs/doctoral/Cinnamon-Bark-Essentialoil-and-a/991031454482202976. [Google Scholar]
- 29.PubChem Eugenol. [(accessed on 27 August 2019)]; Available online: https://pubchem.ncbi.nlm.nih.gov/compound/3314.
- 30.PubChem Beta-Caryophyllene. [(accessed on 27 August 2019)]; Available online: https://pubchem.ncbi.nlm.nih.gov/compound/5281515.
- 31.Schmidt E., Jirovetz L., Buchbauer G., Eller G.A., Stoilova I., Krastanov A., Stoyanova A., Geissler M. Composition and Antioxidant Activities of the Essential Oil of Cinnamon (Cinnamomum zeylanicum Blume) Leaves from Sri Lanka. J. Essent. Oil Bear. Plants. 2006;9:170–182. doi: 10.1080/0972060X.2006.10643490. [DOI] [Google Scholar]
- 32.Jantan I.B., Karim Moharam B.A., Santhanam J., Jamal J.A. Correlation Between Chemical Composition and Antifungal Activity of the Essential Oils of Eight Cinnamomum. Species. Pharm. Biol. 2008;46:406–412. doi: 10.1080/13880200802055859. [DOI] [Google Scholar]
- 33.Chang C.-T., Chang W.-L., Hsu J.-C., Shih Y., Chou S.-T. Chemical composition and tyrosinase inhibitory activity of Cinnamomum cassia essential oil. Bot. Stud. 2013;54:10. doi: 10.1186/1999-3110-54-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lee H.-S. Chemical Composition of Cinnamomum cassia Leaf Oils and Suppression Effect of Cinnamyl Alcohol on Nitric Oxide Synthase. J. Korean Soc. Appl. Biol. Chem. 2009;52:480–485. doi: 10.3839/jksabc.2009.082. [DOI] [Google Scholar]
- 35.Mohammed K.A.A., Ahmed H.M.S., Sharaf H.A., El-Nekeety A.A., Abdel-Aziem S.H., Mehaya F.M., Abdel-Wahhab M.A. Encapsulation of cinnamon oil in whey protein counteracts the disturbances in biochemical parameters, gene expression, and histological picture of the liver and pancreas of diabetic rats. Env. Sci. Pollut. Res. Int. 2020;27:2829–2843. doi: 10.1007/s11356-019-07164-w. [DOI] [PubMed] [Google Scholar]
- 36.Mohammed K.A.A. Efficiency of encapsulated cinnamon oil in the treatment of diabetes in rats. [(accessed on 1 December 2021)];CU Theses. 2020 Available online: http://erepository.cu.edu.eg/index.php/cutheses/article/view/8618. [Google Scholar]
- 37.Mishra A., Bhatti R., Singh A., Singh Ishar M.P. Ameliorative effect of the cinnamon oil from Cinnamomum zeylanicum upon early stage diabetic nephropathy. Planta Med. 2010;76:412–417. doi: 10.1055/s-0029-1186237. [DOI] [PubMed] [Google Scholar]
- 38.Budiastuti B., Safitri Y., Plumeriastuti H., Srianto P., Effendi M., Helmi M. Effect of Cinnamon (Cinnamomum burmannii) Bark Oil on Testicular Histopathology in Streptozotocin Induced Diabetic Wistar Male Rats. J. Glob. Pharm. Technol. 2020;12:901–907. [Google Scholar]
- 39.Kusmardi K., Tedjo A., Fadilah F., Arsianti A., Paramita R. Identification by Docking Simulation and in vivo Effect of Essential Oil from Cinnamommum burmannii as Anti-obesity with Leptin Receptor in the Olfactory System of Mice Balb C. Pharmacogn. J. 2018;10:875–879. doi: 10.5530/pj.2018.5.147. [DOI] [Google Scholar]
- 40.Zari T.A., Al-Logmani A.S. Long–term effects of Cinnamomum zeylanicum Blume oil on some physiological parameters in streptozotocin-diabetic and non-diabetic rats. Boletín Latinoam. Y Caribe Plantas Med. Y Aromáticas. 2009;8:266–274. [Google Scholar]
- 41.Bhatti R., Kaur S., Singh J., Ishar M. Ameliorative effect of volatile oil from Cinnamomum zeylanicum on hyperalgesia in alloxan diabetic rats. Can. J. Pure Appl. Sci. 2009;3:887–895. [Google Scholar]
- 42.Li J.-E., Futawaka K., Yamamoto H., Kasahara M., Tagami T., Liu T.-H., Moriyama K. Cinnamaldehyde Contributes to Insulin Sensitivity by Activating PPARδ, PPARγ, and RXR. Am. J. Chin. Med. 2015;43:879–892. doi: 10.1142/S0192415X15500512. [DOI] [PubMed] [Google Scholar]
- 43.Camacho S., Michlig S., de Senarclens-Bezençon C., Meylan J., Meystre J., Pezzoli M., Markram H., le Coutre J. Anti-Obesity and Anti-Hyperglycemic Effects of Cinnamaldehyde via altered Ghrelin Secretion and Functional impact on Food Intake and Gastric Emptying. Sci. Rep. 2015;5:7919. doi: 10.1038/srep07919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wang P., Yang Y., Wang D., Yang Q., Wan J., Liu S., Zhou P., Yang Y. Cinnamaldehyde Ameliorates Vascular Dysfunction in Diabetic Mice by Activating Nrf2. Am. J. Hypertens. 2020;33:610–619. doi: 10.1093/ajh/hpaa024. [DOI] [PubMed] [Google Scholar]
- 45.Anand P., Murali K.Y., Tandon V., Murthy P.S., Chandra R. Insulinotropic effect of cinnamaldehyde on transcriptional regulation of pyruvate kinase, phosphoenolpyruvate carboxykinase, and GLUT4 translocation in experimental diabetic rats. Chem. Biol. Interact. 2010;186:72–81. doi: 10.1016/j.cbi.2010.03.044. [DOI] [PubMed] [Google Scholar]
- 46.Hosni A.A., Abdel-Moneim A.A., Abdel-Reheim E.S., Mohamed S.M., Helmy H. Cinnamaldehyde potentially attenuates gestational hyperglycemia in rats through modulation of PPARγ, proinflammatory cytokines and oxidative stress. Biomed. Pharm. 2017;88:52–60. doi: 10.1016/j.biopha.2017.01.054. [DOI] [PubMed] [Google Scholar]
- 47.Hosni A., El-Twab S.A., Abdul-Hamid M., Prinsen E., AbdElgawad H., Abdel-Moneim A., Beemster G.T.S. Cinnamaldehyde mitigates placental vascular dysfunction of gestational diabetes and protects from the associated fetal hypoxia by modulating placental angiogenesis, metabolic activity and oxidative stress. Pharm. Res. 2021:105426. doi: 10.1016/j.phrs.2021.105426. [DOI] [PubMed] [Google Scholar]
- 48.Zhao H., Wu H., Duan M., Liu R., Zhu Q., Zhang K., Wang L. Cinnamaldehyde Improves Metabolic Functions in Streptozotocin-Induced Diabetic Mice by Regulating Gut Microbiota. Drug Des. Dev. 2021;15:2339–2355. doi: 10.2147/DDDT.S288011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.El-Bassossy H.M., Fahmy A., Badawy D. Cinnamaldehyde protects from the hypertension associated with diabetes. Food Chem. Toxicol. 2011;49:3007–3012. doi: 10.1016/j.fct.2011.07.060. [DOI] [PubMed] [Google Scholar]
- 50.Jawale A., Datusalia A.K., Bishnoi M., Sharma S.S. Reversal of diabetes-induced behavioral and neurochemical deficits by cinnamaldehyde. Phytomedicine. 2016;23:923–930. doi: 10.1016/j.phymed.2016.04.008. [DOI] [PubMed] [Google Scholar]
- 51.Zhao H., Xie Y., Yang Q., Cao Y., Tu H., Cao W., Wang S. Pharmacokinetic study of cinnamaldehyde in rats by GC–MS after oral and intravenous administration. J. Pharm. Biomed. Anal. 2014;89:150–157. doi: 10.1016/j.jpba.2013.10.044. [DOI] [PubMed] [Google Scholar]
- 52.Singh V.P., Bali A., Singh N., Jaggi A.S. Advanced glycation end products and diabetic complications. Korean J. Physiol. Pharm. 2014;18:1–14. doi: 10.4196/kjpp.2014.18.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mnafgui K., Kaanich F., Derbali A., Hamden K., Derbali F., Slama S., Allouche N., Elfeki A. Inhibition of key enzymes related to diabetes and hypertension by Eugenol in vitro and in alloxan-induced diabetic rats. Arch. Physiol. Biochem. 2013;119:225–233. doi: 10.3109/13813455.2013.822521. [DOI] [PubMed] [Google Scholar]
- 54.Srinivasan S., Sathish G., Jayanthi M., Muthukumaran J., Muruganathan U., Ramachandran V. Ameliorating effect of eugenol on hyperglycemia by attenuating the key enzymes of glucose metabolism in streptozotocin-induced diabetic rats. Mol. Cell. Biochem. 2014;385:159–168. doi: 10.1007/s11010-013-1824-2. [DOI] [PubMed] [Google Scholar]
- 55.Al-Trad B., Alkhateeb H., Alsmadi W., Al-Zoubi M. Eugenol ameliorates insulin resistance, oxidative stress and inflammation in high fat-diet/streptozotocin-induced diabetic rat. Life Sci. 2019;216:183–188. doi: 10.1016/j.lfs.2018.11.034. [DOI] [PubMed] [Google Scholar]
- 56.Jeong K.J., Kim D.Y., Quan H.-Y., Jo H.K., Kim G.W., Chung S.H. Effects of eugenol on hepatic glucose production and AMPK signaling pathway in hepatocytes and C57BL/6J mice. Fitoterapia. 2014;93:150–162. doi: 10.1016/j.fitote.2013.12.023. [DOI] [PubMed] [Google Scholar]
- 57.Garud M.S., Kulkarni Y.A. Eugenol ameliorates renal damage in streptozotocin-induced diabetic rats. Flavour Fragr. J. 2017;32:54–62. doi: 10.1002/ffj.3357. [DOI] [Google Scholar]
- 58.Prasad S.N., Bharath M.M.S. Muralidhara Neurorestorative effects of eugenol, a spice bioactive: Evidence in cell model and its efficacy as an intervention molecule to abrogate brain oxidative dysfunctions in the streptozotocin diabetic rat. Neurochem. Int. 2016;95:24–36. doi: 10.1016/j.neuint.2015.10.012. [DOI] [PubMed] [Google Scholar]
- 59.Shareghi Boroujeni A., Jalali Dehkordi K., Sharifi G., Taghian F., Mazaheri Z. Effect of Nano-eugenol and Aerobic Exercise Against the Streptozotocin Toxicity and Inflammatory Mediators P38-MAPK, NPY, and A-Rα2A in the Dorsal Root Ganglia of Diabetic Rats. Iran. J. Toxicol. 2021;15:205–214. doi: 10.32598/IJT.15.3.822.1. [DOI] [Google Scholar]
- 60.Oroojan A.A., Chenani N., An’aam M. Antioxidant Effects of Eugenol on Oxidative Stress Induced by Hydrogen Peroxide in Islets of Langerhans Isolated from Male Mouse. Int. J. Hepatol. 2020;2020:e5890378. doi: 10.1155/2020/5890378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hamdin C.D., Utami S.W., Muliasari H., Prasedya E.S., Sudarma I.M. Histological pattern on pancreas and liver of diabetic rats after treatment of eugenol isolated from leaves of Syzygium aromaticum. AIP Conf. Proc. 2019;2199:060004. doi: 10.1063/1.5141313. [DOI] [Google Scholar]
- 62.Mani V., Balraj M., Venktsan G., Soundrapandiyan J., Kasturi R., Danavel A., Babu S. Molecular docking analysis of beta-caryophyllene with IRS-1, cSrc and Akt. Bioinformation. 2021;17:916–920. doi: 10.6026/97320630017916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Aguilar-Ávila D.S., Flores-Soto M.E., Tapia-Vázquez C., Pastor-Zarandona O.A., López-Roa R.I., Viveros-Paredes J.M. β-Caryophyllene, a Natural Sesquiterpene, Attenuates Neuropathic Pain and Depressive-Like Behavior in Experimental Diabetic Mice. J. Med. Food. 2019;22:460–468. doi: 10.1089/jmf.2018.0157. [DOI] [PubMed] [Google Scholar]
- 64.Basha R.H., Sankaranarayanan C. β-Caryophyllene, a natural sesquiterpene lactone attenuates hyperglycemia mediated oxidative and inflammatory stress in experimental diabetic rats. Chem. Biol. Interact. 2016;245:50–58. doi: 10.1016/j.cbi.2015.12.019. [DOI] [PubMed] [Google Scholar]
- 65.Basha R.H., Sankaranarayanan C. Protective role of β-caryophyllene, a sesquiterpene lactone on plasma and tissue glycoprotein components in streptozotocin-induced hyperglycemic rats. J. Acute Med. 2015;5:9–14. doi: 10.1016/j.jacme.2015.02.001. [DOI] [Google Scholar]
- 66.Basha R.H., Sankaranarayanan C. β-Caryophyllene, a natural sesquiterpene, modulates carbohydrate metabolism in streptozotocin-induced diabetic rats. Acta Histochem. 2014;116:1469–1479. doi: 10.1016/j.acthis.2014.10.001. [DOI] [PubMed] [Google Scholar]
- 67.Youssef D.A., El-Fayoumi H.M., Mahmoud M.F. Beta-caryophyllene alleviates diet-induced neurobehavioral changes in rats: The role of CB2 and PPAR-γ receptors. Biomed. Pharmacother. 2019;110:145–154. doi: 10.1016/j.biopha.2018.11.039. [DOI] [PubMed] [Google Scholar]
- 68.Li H., Wang D., Chen Y., Yang M. β-Caryophyllene inhibits high glucose-induced oxidative stress, inflammation and extracellular matrix accumulation in mesangial cells. Int. Immunopharmacol. 2020;84:106556. doi: 10.1016/j.intimp.2020.106556. [DOI] [PubMed] [Google Scholar]
- 69.Geddo F., Antoniotti S., Querio G., Salaroglio I.C., Costamagna C., Riganti C., Gallo M.P. Plant-Derived Trans-β-Caryophyllene Boosts Glucose Metabolism and ATP Synthesis in Skeletal Muscle Cells through Cannabinoid Type 2 Receptor Stimulation. Nutrients. 2021;13:916. doi: 10.3390/nu13030916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Galic S., Hauser C., Kahn B.B., Haj F.G., Neel B.G., Tonks N.K., Tiganis T. Coordinated regulation of insulin signaling by the protein tyrosine phosphatases PTP1B and TCPTP. Mol. Cell. Biol. 2005;25:819–829. doi: 10.1128/MCB.25.2.819-829.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Sweet I.R., Li G., Najafi H., Berner D., Matschinsky F.M. Effect of a glucokinase inhibitor on energy production and insulin release in pancreatic islets. Am. J. Physiol. 1996;271:E606–E625. doi: 10.1152/ajpendo.1996.271.3.E606. [DOI] [PubMed] [Google Scholar]
- 72.Matschinsky F.M., Zelent B., Doliba N., Li C., Vanderkooi J.M., Naji A., Sarabu R., Grimsby J. Glucokinase activators for diabetes therapy. Diabetes Care. 2011;34:S236–S243. doi: 10.2337/dc11-s236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Marini C., Salani B., Massollo M., Amaro A., Esposito A.I., Orengo A.M., Capitanio S., Emionite L., Riondato M., Bottoni G., et al. Direct inhibition of hexokinase activity by metformin at least partially impairs glucose metabolism and tumor growth in experimental breast cancer. Cell Cycle. 2013;12:3490–3499. doi: 10.4161/cc.26461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Li W., Zheng M., Wu S., Gao S., Yang M., Li Z., Min Q., Sun W., Chen L., Xiang G., et al. Benserazide, a dopadecarboxylase inhibitor, suppresses tumor growth by targeting hexokinase 2. J. Exp. Clin. Cancer Res. 2017;36:58. doi: 10.1186/s13046-017-0530-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Trott O., Olson A.J. AutoDock Vina: Improving the speed and accuracy of docking with a new scoring function, efficient optimization, and multithreading. J. Comput. Chem. 2010;31:455–461. doi: 10.1002/jcc.21334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Pettersen G., Huang C., Greenblatt M.F. UCSF Chimera--a visualization system for exploratory research and analysis—PubMed. J. Comput. Chem. 2004;25:1605–1612. doi: 10.1002/jcc.20084. [DOI] [PubMed] [Google Scholar]
- 77.Brayer G.D., Luo Y., Withers S.G. The structure of human pancreatic α-amylase at 1.8 Å resolution and comparisons with related enzymes. Protein Sci. 1995;4:1730–1742. doi: 10.1002/pro.5560040908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ren L., Qin X., Cao X., Wang L., Bai F., Bai G., Shen Y. Structural insight into substrate specificity of human intestinal maltase-glucoamylase. Protein Cell. 2011;2:827–836. doi: 10.1007/s13238-011-1105-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Cheruvallath Z.S., Gwaltney S.L., Sabat M., Tang M., Wang H., Jennings A., Hosfield D., Lee B., Wu Y., Halkowycz P., et al. Discovery of potent and orally active 1,4-disubstituted indazoles as novel allosteric glucokinase activators. Bioorganic Med. Chem. Lett. 2017;27:2678–2682. doi: 10.1016/j.bmcl.2017.04.041. [DOI] [PubMed] [Google Scholar]
- 80.Groves M.R., Yao Z.-J., Roller P.P., Burke T.R., Barford D. Structural basis for inhibition of the protein tyrosine phosphatase 1B by phosphotyrosine peptide mimetics. Biochemistry. 1998;37:17773–17783. doi: 10.1021/bi9816958. [DOI] [PubMed] [Google Scholar]
- 81.Nawaz M.H., Ferreira J.C., Nedyalkova L., Zhu H., Carrasco-López C., Kirmizialtin S., Rabeh W.M. The catalytic inactivation of the N-half of human hexokinase 2 and structural and biochemical characterization of its mitochondrial conformation. Biosci. Rep. 2018;38:BSR20171666. doi: 10.1042/BSR20171666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Shityakov S., Förster C. In silico Predictive Model to Determine Vector-Mediated Transport Properties for the Blood-Brain Barrier Choline Transporter. [(accessed on 12 August 2019)]. Available online: https://www.dovepress.com/in-silico-predictive-model-to-determine-vector-mediated-transport-prop-peer-reviewed-article-AABC. [DOI] [PMC free article] [PubMed]
- 83.Bischoff H. The mechanism of alpha-glucosidase inhibition in the management of diabetes. Clin. Investig. Med. 1995;18:303–311. [PubMed] [Google Scholar]
- 84.Sarabu R., Bizzarro F.T., Corbett W.L., Dvorozniak M.T., Geng W., Grippo J.F., Haynes N.-E., Hutchings S., Garofalo L., Guertin K.R., et al. Discovery of piragliatin—First glucokinase activator studied in Type 2 Diabetic patients. J. Med. Chem. 2012;55:7021–7036. doi: 10.1021/jm3008689. [DOI] [PubMed] [Google Scholar]
- 85.Bonadonna R.C., Heise T., Arbet-Engels C., Kapitza C., Avogaro A., Grimsby J., Zhi J., Grippo J.F., Balena R. Piragliatin (RO4389620), a novel glucokinase activator, lowers plasma glucose both in the postabsorptive state and after a glucose challenge in patients with Type 2 Diabetes Mellitus: A mechanistic study. J. Clin. Endocrinol. Metab. 2010;95:5028–5036. doi: 10.1210/jc.2010-1041. [DOI] [PubMed] [Google Scholar]
- 86.Zhi J., Zhai S. Effects of piragliatin, a glucokinase activator, on fasting and postprandial plasma glucose in patients with Type 2 Diabetes Mellitus. J. Clin. Pharmacol. 2016;56:231–238. doi: 10.1002/jcph.589. [DOI] [PubMed] [Google Scholar]
- 87.Liu S., Ammirati M.J., Song X., Knafels J.D., Zhang J., Greasley S.E., Pfefferkorn J.A., Qiu X. Insights into Mechanism of Glucokinase Activation: Observation of multiple distinct protein conformations. J. Biol. Chem. 2012;287:13598–13610. doi: 10.1074/jbc.M111.274126. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.