Abstract
Objectives
This study investigated the determinants of undiagnosed hypertension among Indonesian adults.
Methods
This study involved an analysis of secondary data from the 2014 Indonesia Family Life Survey (IFLS) on 5914 Indonesian adults (≥40 years). The determinant variables examined in this cross-sectional study were education level, monthly per capita expenditures (PCE), whether the participant experienced headaches in the morning, and other general health variables. The outcome variable was undiagnosed hypertension, which was defined as participants with hypertension who had not received a hypertension diagnosis from a health professional and had never been prescribed medication for treating hypertension. The data were analyzed using logistic regression.
Results
A total of 3322 participants (56.2%) were found to have undiagnosed hypertension. The odds ratios (ORs) and 95% confidence intervals (CIs) of undiagnosed hypertension were significantly higher among those who completed primary school or lower (OR, 1.60; 95% CI, 1.29 to 1.98), had low monthly PCE (OR, 1.28; 95% CI, 1.13 to 1.43), did not report experiencing headaches in the morning (OR, 1.97; 95% CI, 1.76 to 2.21), and reported a general health status of healthy (OR, 2.05; 95% CI, 1.82 to 2.30) than those who had a higher education level, had high monthly PCE, experienced headaches in the morning, and were unhealthy.
Conclusions
Education level, monthly PCE, the experience of headaches in the morning, and general health status were associated with undiagnosed hypertension. The monitoring system for detecting undiagnosed hypertension cases must be strengthened. Health promotion is also necessary to reduce the prevalence of undiagnosed hypertension.
Keywords: Adult, Hypertension, Undiagnosed diseases, Indonesia
INTRODUCTION
Non-communicable diseases (NCDs), which are the leading cause of death globally and one of the major health challenges of the 21st century, are estimated to account for 71% of the 57 million annual global deaths. The burden is most significant in low-income and middle-income countries, where 77% of all NCD deaths and 85% of premature deaths occur [1].
Indonesia, as a lower-middle-income country, has faced a dramatic escalation of NCDs in recent years. According to the Indonesian Basic Health Research Survey (Riskesdas), the prevalence of NCDs (including stroke) among the Indonesian population significantly increased from 2007 and 2013, from 8.3% to 12.1%, respectively. Furthermore, 61% of total deaths in Indonesia are caused by NCDs [2].
In Indonesia, hypertension is a common condition and continues to be a leading risk factor for NCDs and other diseases [3]. The Riskesdas reported that the prevalence of high blood pressure (BP) among those aged 18 years and older in Indonesia increased from 25.8% in 2013 to 34.1% in 2018 [4]. Another study found that the prevalence of hypertension among Indonesia adults (≥15 years of age) was 33.4% [5].
Moreover, most individuals with hypertension are asymptomatic, which leads to a high rate of undiagnosed hypertension [6]. According to the 2013 Riskesdas, 63.2% of hypertension cases go undiagnosed in Indonesia [7]. Due to this phenomenon, undiagnosed hypertension may lead to serious health complications or even death [2]. The burden of hypertension would be far more significant than it is currently projected to be if more cases were to be discovered [5].
Previous study has examined the factors associated with undiagnosed hypertension in various countries [8]. To our knowledge, however, there is still a limited understanding of undiagnosed hypertension in Indonesia. Therefore, identifying the determinants of undiagnosed hypertension among Indonesian adults has become an important issue for planning effective strategies to reduce the burden of hypertension. Thus, this study investigated the determinants of undiagnosed hypertension among Indonesian adults based on data from the fifth cross-sectional Indonesia Family Life Survey (IFLS) conducted in 2014-2015 in Indonesia.
METHODS
Data Source
The data used for the present study were obtained from the fifth IFLS since it contained complete hypertension information on a large population of adult individuals [9]. The fifth IFLS, which is a cross-sectional study, was conducted from September 2014 to April 2015 [9,10].
The IFLS is an ongoing longitudinal study. The sample of the IFLS represents approximately 83% of the Indonesian population [11]. The study is conducted using in-person interviews with adult participants. Questionnaires are used to collect individual, family, and household information and information on health and education facilities in the respondents’ communities [9]. The IFLS has been conducted 5 times, in 1993, 1997, 2000, 2007, and 2014, and it has collected information from 50 148 individuals from 16 204 households. The sampling frame of the IFLS has been described in detail in other studies [10,11].
Sample Size
The eligible population for the present study consisted of 14 787 men and women aged ≥40 years, among whom 13 031 had available BP and diagnosis data (Figure 1). We excluded 1756 participants with missing data for BP. A total of 6671 of the remaining participants were not diagnosed with hypertension or did not have hypertension based on BP data. Next, 446 participants were excluded who had missing data for monthly per capita expenditures (PCE). Thus, a total of 5914 participants were analyzed in this study.
Figure. 1.
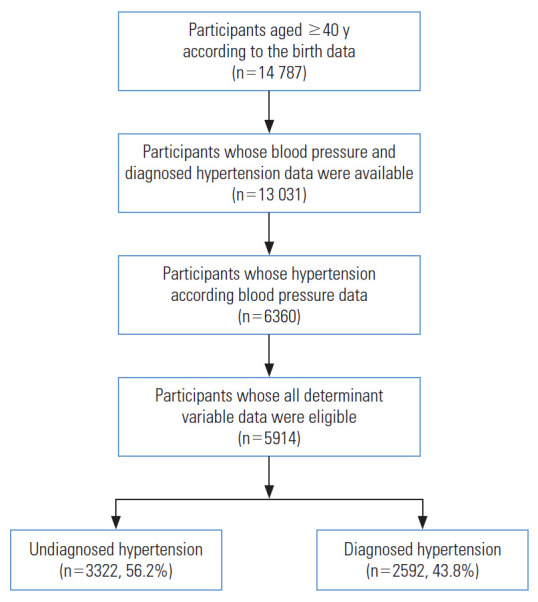
The determinants of undiagnosed hypertension in the adult Indonesian population: a cross-sectional study from the Indonesia Family Life Survey 2014-2015.
Study Variables
BP was the outcome variable of this study. This variable was measured 3 times while participants were in a seated position using an Omron meter (HEM-7203 AP; Omron Healthcare, Kyoto, Japan) by trained interviewers [5,9]. The Omron HEM-7203 displays quick and accurate readings for systolic BP and diastolic BP and pulse. The accuracy rate stands at ±3 mmHg for BP and ±5% for pulse rate [12]. The mean BP value of the 3 measurements was used to identify hypertension among the participants. BP was classified using the Joint National Committee 7 algorithm. A participant was considered to have hypertension if his or her mean systolic BP was ≥140 mmHg and/or his or her mean diastolic BP was ≥90 mmHg [8]. Participants who responded “yes” to the question “Have you been diagnosed with hypertension by a doctor/health professional?” were defined as having diagnosed hypertension. Participants who were hypertensive but did not report having received a hypertension diagnosis from a doctor were classified as having undiagnosed hypertension [8].
Marital status, education level, employment status, residence type, family size, monthly PCE, health insurance status, awareness of an accessible health care facilities, functional disability status, whether one experienced headaches in the morning, and general health status were the determinant factors for undiagnosed hypertension.
We divided marital status into 2 groups: married or unmarried (single, separated, divorced, or widowed). Education level was assessed using the following questions: (1) “Have you ever attended school?”, to which respondents answered “yes” or “no,” and (2) “What is the highest education level you attained?”, to which the possible answers were primary school, junior high school or the equivalent, senior high school or the equivalent, or college or university (D1, D2, D3). Education level was then classified into 1 of 3 groups: primary school or less (no schooling or primary school), secondary school (junior high school or senior high school), or graduate and above (college or university).
Employment status was categorized into 2 groups: employed (working/helping to earn income) or unemployed (for the responses “job searching,” “attending school,” “housekeeping,” “retired,” and “sick/disabled”). Residential areas were classified into 2 groups (urban or rural) based on data from the Central Bureau of Statistics [13,14]. Family size was defined as the number of family members in a household. We divided family size into 2 groups: ≤4 household members or >4 household members [15]. Health insurance status was classified as insured (the respondent had health insurance) or uninsured (the respondent did not have health insurance).
Monthly PCE were calculated as the participant’s monthly total household expenditures divided by the number of household members. Household expenditures as measured in the IFLS have been described in detail elsewhere [16]. Individuals were considered to have low monthly PCE if their total monthly PCE were in the bottom 40% based on the definition of “poor” by the World Bank and World Health Organization [17]. Monthly PCE in the IFLS data were assessed using Indonesian rupiah (IDR) and then converted into US dollars (USD) using the 2014 exchange rate (USD 1=IDR 11 865.211) [18]. As a result, monthly PCE were categorized into 2 groups: ≤USD 60 or >USD 60 [19].
Awareness of accessible health care facilities was classified as “yes” (respondents who knew the location of at least 1 healthcare facility) or “no” (respondents who did not know the locations of any healthcare facilities). Functional disabilities were categorized as present (respondents who required help to perform daily activities) or absent (respondents who did not require help to perform daily activities). Whether respondents experienced headaches in the morning was determined by asking the question, “Do you often have a headache when you wake up in the morning?”, to which respondents answered “yes” or “no.” General health status was categorized as healthy (“very healthy” or “somewhat healthy”) or unhealthy (“somewhat unhealthy” or “unhealthy”) [20].
Statistical Analysis
Descriptive statistics were used to describe the study variables in the study population. Analysis of variance was used to examine the continuous variables, while the chi-square test was used to examine the categorical variables. A multivariateadjusted logistic regression model was used to estimate the odds ratios (ORs) and 95% confidence intervals (CIs) of the determinants of undiagnosed hypertension, with undiagnosed hypertension classified as the dichotomous outcome variable. Model 1 was adjusted for age. Model 2 was adjusted for age and sex. Model 3 was further adjusted for age, sex, and area of residence (urban or rural). The determinants of undiagnosed hypertension were categorized into dichotomous variables, except for education level, as follows: marital status (married [reference] or unmarried), education level (primary school or less, secondary school, or graduate and above [reference]), employment status (employed [reference] or unemployed), family size (≤4 [reference] or >4 household members), monthly PCE (≤60 or >60 USD [reference]), awareness of accessible health care facilities (yes [reference] or no), functional disabilities (yes or no [reference]), whether the participant experienced headaches in the morning (yes [reference] or no), and general health status (healthy or unhealthy [reference]).
The logistic regression model was conducted using SPSS version 26 (IBM Corp., Armonk, NY, USA). All statistical tests were 2-sided, and p-values of <0.05 were considered to indicate statistical significance.
Ethics Statement
The IFLS data used in the present study are publicly available. The surveys and procedures of the IFLS study were reviewed and approved by Institutional Review Boards at the RAND Corporation in the United States and the University of Gadjah Mada in Indonesia. Written informed consent was obtained from all participants before data collection began.
RESULTS
Table 1 shows the characteristics of participants according to their hypertension status. Overall, 56.2% of Indonesian adults were found to have undiagnosed hypertension. Participants with undiagnosed hypertension were more likely to be male and have a primary school education or lower. Those with undiagnosed hypertension were also more likely to be employed, live in a rural area, have ≤4 household members, have low monthly PCE, not know of an accessible health facility, not have functional disabilities, not experience headaches in the morning, and have a general health status of healthy.
Table 1.
The association between determinant factors and undiagnosed hypertension in the 2014-2015 Indonesia Family Life Survey1
| Variables | Undiagnosed hypertension | Diagnosed hypertension | p-value |
|---|---|---|---|
| No. of participants (n = 5914) | 3322 (56.2) | 2592 (43.8) | |
| Age, mean±SD (y) | 57.06±12.05 | 57.90±21.87 | 0.06 |
| Sex | |||
| Male | 1616 (64.5) | 888 (35.5) | <0.01 |
| Female | 1706 (50.0) | 1704 (50.0) | |
| Marital status | |||
| Unmarried | 853 (54.9) | 702 (45.1) | 0.23 |
| Married | 2469 (56.6) | 1890 (43.4) | |
| Education level | |||
| Primary school or less | 2249 (57.4) | 1167 (42.6) | <0.05 |
| Secondary school | 846 (54.3) | 712 (45.7) | |
| Graduate and above | 277 (51.6) | 213 (48.4) | |
| Employment status | |||
| Unemployed | 1301 (49.6) | 1324 (50.4) | <0.01 |
| Employed | 2021 (61.4) | 1268 (38.6) | |
| Area of residence | |||
| Rural | 1490 (58.8) | 1043 (41.2) | <0.01 |
| Urban2 | 1832 (54.2) | 1549 (45.8) | |
| Family size (household members) | |||
| ≤4 | 2230 (58.0) | 1618 (42.0) | <0.01 |
| >4 | 1092 (52.9) | 974 (47.1) | |
| Monthly PCE (USD)3 | |||
| ≤60 | 1407 (59.5) | 959 (40.5) | <0.01 |
| >60 | 1915 (54.0) | 1633 (46.0) | |
| Health insurance status | |||
| Uninsured | 1660 (56.8) | 1262 (43.2) | 0.34 |
| Insured | 1662 (55.5) | 1330 (44.5) | |
| Awareness of accessible health care facility | |||
| No | 2972 (57.3) | 2218 (42.7) | <0.01 |
| Yes | 350 (48.3) | 374 (51.7) | |
| Functional disability status | |||
| No | 2446 (58.9) | 1709 (41.1) | <0.01 |
| Yes | 876 (49.8) | 83 (50.2) | |
| Experienced headaches in the morning | |||
| No | 2424 (62.7) | 1442 (37.3) | <0.01 |
| Yes | 898 (43.8) | 1150 (56.2) | |
| General health status | |||
| Healthy | 2456 (63.7) | 1999 (36.3) | <0.01 |
| Unhealthy | 866 (42.1) | 1193 (57.9) |
Values are presented as number (%).
SD, standard deviation; PCE, per-capita expenditures; USD, US dollar; IDR, Indonesian rupiah.
Obtained using 1-factor analysis of variance for continuous variables and the chi-square test for categorical variables.
Central Bureau of Statistics (BPS) Indonesia’s definition (population density of 5000 persons per km2; 25% or less of the households work in the agricultural sector; and having 8 or more specific kinds of urban facilities, including primary schools, junior high schools, senior high schools, hospitals, maternity [mother-child] hospitals, primary health care centers, roads [to accommodate 3- and 4-wheeled motorized vehicles], telephones, post offices, markets, cinemas, banks, shopping centers, factories, and restaurants).
Total monthly household expenditures divided by the number of household members; USD at the 2014 exchange rate (USD 1=IDR 12 440).
Table 2 shows the association between determinant factors and undiagnosed hypertension. In the unadjusted logistic regression model, we found that sex, marital status, education level, employment status, family size, functional disability status, whether the participant experienced headaches in the morning, and general health status were significantly associated with undiagnosed hypertension. In model 3, the OR for undiagnosed hypertension was 1.60 (95% CI, 1.29 to 1.98) for those with an education level of primary school or less when compared to participants with a high education level (model 3, p<0.05).
Table 2.
Logistic regression analysis of the determinants of undiagnosed hypertension in the 2014-2015 Indonesia Family Life Survey1
| Variables | Unadjusted | Model 12 | Model 23 | Model 34 | |
|---|---|---|---|---|---|
| Age (y) | 0.19 (0.99, 1.00) | - | - | - | |
| Sex (male) | 1.85 (1.63, 2.09)** | 1.81 (1.60, 2.05)** | - | - | |
| Marital status (unmarried) | 1.22 (1.06, 1.40)* | 1.18 (1.03, 1.35)* | 1.02 (0.89, 1.16) | 1.02 (0.89, 1.16) | |
| Education level | |||||
| Secondary school | 1.36 (1.09, 1.70)* | 1.37 (1.10, 1.71)* | 1.31 (1.05, 1.64)* | 1.31 (1.05, 1.64)* | |
| Primary school or less | 1.79 (1.43, 2.23)** | 1.76 (1.42, 2.20)** | 1.56 (1.26, 1.94)** | 1.60 (1.29, 1.98)** | |
| Employment status (unemployed) | 0.82 (0.24, 0.92)* | 0.80 (0.71, 0.90)** | 0.68 (0.60, 0.76)** | 0.67 (0.60, 0.75)** | |
| Area of residence (rural) | 1.10 (0.98, 1.24) | 1.10 (0.98, 1.23) | 1.11 (0.99, 1.24) | - | |
| Family size (>4 household members) | 0.82 (0.73, 0.93)* | 0.83 (0.74, 0.93)* | 0.83 (0.74, 0.93)* | 0.82 (0.73, 0.93)* | |
| Monthly PCE (≤USD 60)5 | 1.25 (1.11, 1.41)** | 1.25 (1.11, 1.41)** | 1.26 (1.12, 1.42)** | 1.28 (1.13, 1.43)** | |
| Awareness of health care facility (no) | 1.28 (1.08, 1.52)* | 1.28 (1.08, 1.51)* | 1.28 (1.08, 1.51)* | 1.29 (1.09, 1.53)* | |
| Functional disability status (yes) | 0.79 (0.70, 0.90)** | 0.78 (0.69, 0.88)** | 0.84 (0.74, 0.94)* | 0.84 (0.74, 0.95)* | |
| Experienced headaches in the morning (no) | 1.92 (1.71, 2.16)** | 1.91 (1.70, 2.14)** | 1.97 (1.76, 2.21)** | 1.97 (1.76, 2.21)** | |
| General health status (healthy) | 2.07 (1.84, 2.33)** | 2.08 (1.85, 2.34)** | 2.05 (1.82, 2.30)** | 2.05 (1.82, 2.30)** | |
Values are presented as odds ratio (95% confidence interval).
PCE, per-capita expenditures; USD, US dollar; IDR, Indonesian rupiah.
Logistic regression model.
Model 1: adjusted for age.
Model 2: adjusted for age, sex.
Model 3: adjusted for age, sex, residence (urban or rural).
Total monthly household expenditures divided by the number of household members; USD at the 2014 exchange rates (USD 1=IDR 12 440).
p<0.05,
p<0.01.
In model 3, participants who were unemployed, had >4 household members, or had functional disabilities tended to have a lower probability of undiagnosed hypertension (OR, 0.67; 95% CI, 0.60 to 0.75; OR, 0.82; 95% CI, 0.73 to 0.93; and OR, 0.84; 95% CI, 0.74 to 0.95, respectively) than those who were employed, had ≤4 household members, and did not have functional disabilities.
Furthermore, the odds of having undiagnosed hypertension among participants with lower monthly PCE had an OR of 1.28 (95% CI, 1.13 to 1.43) compared to those with higher monthly PCE. The results also show that participants who did know of any accessible healthcare facilities had a higher probability of undiagnosed hypertension (OR, 1.29; 95% CI, 1.09 to 1.53) than those who did know of an accessible health care facility.
The probability of undiagnosed hypertension was also significantly higher among those who did not report experiencing headaches in the morning than among those who did, with a multivariate-adjusted OR of 1.97 (95% CI, 1.76 to 2.21) in model 3. The results also showed that participants who considered themselves to be healthy tended to have a higher probability of undiagnosed hypertension, with a multivariate-adjusted OR of 2.05 (95% CI, 1.82 to 2.30) in model 3.
DISCUSSION
In this cross-sectional study, we investigated the determinants of undiagnosed hypertension among Indonesian adults. Our study found that undiagnosed hypertension was more prevalent among males than among females. Moreover, our results suggested that those who had a low education level, had low monthly PCE, did not experience headaches in the morning, or had a general health status of healthy had a significantly higher probability of undiagnosed hypertension. To the best of our knowledge, the present study is the first to identify associations between determinant factors and undiagnosed hypertension among Indonesian adults.
Our findings showed a 56.2% prevalence of undiagnosed hypertension among Indonesian adults. This result is in line with other studies from other Asian countries [21-23]. The reason for this might be a lack of awareness of routine health check-ups, accessibility difficulties related to screening services, and a lack of interest in seeking health services until health complications arise among Indonesian adults. Our study showed that participants with undiagnosed hypertension most likely did not know about accessible healthcare facilities in their area. Therefore, screening and improving awareness of such services are important goals for healthcare experts and community healthcare workers.
The present study also revealed that those with a high probability of undiagnosed hypertension tended to also have a low education level (primary school or less) and lower monthly PCE (indicating low socioeconomic status). This is likely because, in Indonesia, there is inequality in access to health care services, and health care services tend to be more accessible to the rich than to the poor [24]. In addition, those with little education and low socioeconomic status tend to have less knowledge and awareness about hypertension [5,21,25]. Thus, education level and household income are among the most important factors for addressing undiagnosed hypertension in Indonesia.
Interestingly, unemployed participants tended to have a low probability of undiagnosed hypertension. In contrast, a previous study found that undiagnosed hypertension was lower among individuals who were employed than among those who were not [26]. In that study, 1301 respondents had undiagnosed hypertension and were unemployed. These individuals had a mean age of ≥62 years and tended to have health insurance and live in urban areas. Thus, in the present study, since the typical retirement age in Indonesia is around 60 years old, one possible reason for this finding may be that many of the participants who were considered unemployed were retired with health insurance and lived in urban areas. In Indonesia, urban residents are more likely to have access to formal healthcare services than those who live in rural areas [24]. Therefore, these groups tend to have easy access to healthcare services and can attend routine health check-ups or health screenings. We also performed a sex-stratified analysis to examine the possibility that differences in employment status between male and female might affect undiagnosed hypertension. However, the results for this analysis did not show substantial changes, with ORs of 0.54 (95% CI, 0.45 to 0.65) and 0.85 (95% CI, 0.74 to 0.98) for male and female, respectively (Supplemental Material 1).
This study also found that participants with undiagnosed hypertension tended to be less likely to experience headaches in the morning and were more likely to have a general health status of healthy. A previous study found that the probability of undiagnosed hypertension was higher among participants who had a self-rated health status of healthy and lower among those who reported experiencing headaches in the morning [8], which is in accordance to our findings. Therefore, it is important to promote routine physical examinations related to hypertension in Indonesia, especially among adults.
In addition, participants with a household size of ≥4 people had a lower probability of undiagnosed hypertension. A previous study reported that individuals from households of 6 or more members were more likely to seek treatment from formal health care providers than those from households with fewer members [27].
Our findings also showed that participants who did not have knowledge of nearby accessible healthcare facilities had a higher probability of undiagnosed hypertension. A previous study reported that a lack of awareness of accessible healthcare facilities posed a potential barrier to healthcare services [28]; thus, these individuals tend to be unaware of their conditions.
In addition, the present study showed that participants with functional disabilities were less likely to have undiagnosed hypertension than those without disabilities. A prior study found that people with functional disabilities were more likely to seek treatment from formal healthcare providers and often required more specialized health care [27]. Therefore, their conditions are more likely to be detected.
The strengths of the present study are as follows. First, since this study used data from the 5th IFLS, which included a nationally representative sample, the findings can be considered highly representative of the population at large. Second, the IFLS used calibrated tools to measure hypertension, height, and weight and used validated questionnaires for data collection. Third, all interviewers for the IFLS were trained to understand all parts of the survey including the methodology and the content of the questionnaire.
However, this study also has several limitations. First, the cross-sectional design may not allow generalization of the results to the whole population. Second, we used self-reported data for the participants’ past history of illness, whether they experienced headaches in the morning, and their general health status, which might compromise the validity of the reported level of predictive factors. Third, since excluding individuals with missing data for determinant factors could have caused a bias, all 6360 participants, including those for whom such data were missing, were analyzed. However, the association between determinant factors and undiagnosed hypertension did not change substantially. Therefore, the association between determinant factors and undiagnosed hypertension is unlikely to have resulted from selection bias.
The high prevalence of undiagnosed hypertension poses a significant challenge. Indonesian adults with a low education level, low monthly PCE, no awareness of an accessible healthcare facility, no experience of headaches in the morning, and a reported general health status of healthy have a high risk of undiagnosed hypertension. Our findings also indicate that there may be a general lack of awareness about high BP among Indonesian adults. Our results suggest that the current system for detecting undiagnosed cases must be strengthened. The results of the present study also suggest that efforts to promote awareness of NCDs—especially hypertension—at the community level, particularly among those with little education and low socioeconomic status—are necessary in order to reduce the prevalence of undiagnosed hypertension.
Acknowledgments
The authors would like to thank the RAND Corporation for making the data publicly available at http://www.rand.org/labor/FLS/IFLS.html.
CONFLICT OF INTEREST
The authors have no conflicts of interest associated with the material presented in this paper.
FUNDING
None.
AUTHOR CONTRIBUTIONS
Conceptualization: Mahwati Y, Nurrika D, Latief K. Data curation Mahwati: Y, Nurrika D, Latief K. Formal analysis: Mahwati Y. Funding acquisition: None. Methodology: Mahwati Y, Nurrika D, Latief K. Visualization: Mahwati Y, Nurrika N. Writing – original draft: Mahwati Y, Nurrika D. Writing – review & editing Mahwati Y, Nurrika D, Latief K.
SUPPLEMENTAL MATERIALS
Supplemental material is available at https://doi.org/10.3961/jpmph.21.500.
Logistic regression analyses of the association between employment status and undiagnosed hypertension in the Indonesia Family Life Survey (IFLS) 2014-2015 stratified by sex1.
REFERENCES
- 1.World Health Organization Noncommunicable diseases. 2021. [cited 2021 Jul 23]. Available from: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases.
- 2.Ministry of Health of the Republic of Indonesia National strategic action plan for the prevention and control of noncommunicable diseases. 2017. [cited 2020 Mar 20]. Available from: http://p2ptm.kemkes.go.id/uploads/VHcrbkVobjRzUDN3UCs4eUJ0dVBndz09/2018/10/Buku_Rencana_Aksi_Nasional_2015_2019.pdf (Indonesian)
- 3.Ministry of Health of the Republic of Indonesia Hypertension. 2014. [cited 2020 Mar 23]. Available from: https://pusdatin.kemkes.go.id/resources/download/pusdatin/infodatin/infodatin-hipertensi.pdf (Indonesian)
- 4.Agency for Health Research and Development Indonesia Basic Health Research (RISKESDAS) 2018. 2019. [cited 2021 Jul 23]. Available from: http://labdata.litbang.kemkes.go.id/images/download/laporan/RKD/2018/Laporan_Nasional_RKD2018_FINAL.pdf (Indonesian)
- 5.Peltzer K, Pengpid S. The prevalence and social determinants of hypertension among adults in Indonesia: a cross-sectional population-based national survey. Int J Hypertens. 2018;2018:5610725. doi: 10.1155/2018/5610725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Souffront K, Gestal C, Melkus GD, Richardson L. Recognition of asymptomatic hypertension in an urban emergency department: where are we now? Adv Emerg Nurs J. 2016;38(4):320–326. doi: 10.1097/TME.0000000000000118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ministry of Health of the Republic of Indonesia General guidelines of post non-communicable diseases integrated counseling. 2014. [cited 2021 Jan 29]. Available from: http://p2ptm.kemkes.go.id/uploads/2016/10/Pedoman-Umum-Pos-Pembinaan-Terpadu-Penyakit-Tidak-Menular.pdf (Indonesian)
- 8.Zhou J, Fang S. Association between undiagnosed hypertension and health factors among middle-aged and elderly Chinese population. Int J Environ Res Public Health. 2019;16(7):1214. doi: 10.3390/ijerph16071214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Strauss J, Witoelar F, Sikoki B. The fifth wave of the Indonesia Family Life Survey: overview and field report volume 1. 2016. [cited 2018 Nov 1]. Available from: https://www.rand.org/pubs/working_papers/WR1143z1.html.
- 10.Strauss J, Witoelar Fi, Sikoki B. The fourth wave of the Indonesia Family Life Survey (IFLS 4): overview and field report. 2009. [cited 2018 Nov 1]. Available from: https://microdata.worldbank.org/index.php/catalog/1044/download/20909.
- 11.Frankenberg E, Karoly LA, Gertler P, Achmad S, Agung IG, Hatmadji SH, et al. The 1993 Indonesian Family Life Survey: overview and field report. 1995. [cited 2021 Oct 27]. Available from: https://www.rand.org/pubs/drafts/DRU1195z1.html.
- 12. Sri Anchana Diagnostics Distributors. Omron BP monitor upper arm (HEM-7203) [cited 2021 Oct 27]. Available from: http://www.srianchanadiagnosticgroup.com/images/instruments/PDF/16/16.BLOOD%20PRESSURE%20MONITOR%20-%20OMRON.pdf.
- 13.Central Bureau of Statistics Regulation of head statistical centre number 37 year 2010 about classification urban and rural in Indonesia. 2010. [cited 2021 Jul 23]. Available from: https://sirusa.bps.go.id/webadmin/doc/MFD_2010_Buku_1.pdf (Indonesian)
- 14.Mulyana W. Rural-urban linkages: Indonesia case study. Working paper series No. 126. 2014. [cited 2021 Jul 23]. Available from: https://www.rimisp.org/wp-content/files_mf/files_mf/1421349176126_R_ULinkages_Indonesia_countrycase_Final_edited.pdf.
- 15.Ozawa S, Grewal S, Bridges JF. Household size and the decision to purchase health insurance in Cambodia: results of a discretechoice experiment with scale adjustment. Appl Health Econ Health Policy. 2016;14(2):195–204. doi: 10.1007/s40258-016-0222-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Witoelar F, World Bank Note on the construction of the IFLS consumption expenditure aggregates. 2009. [cited 2021 Jul 26]. Available from: https://dokumen.tips/documents/ifls-consumption-expenditure-aggregatespdf.html.
- 17.World Health Organization Monitoring progress towards universal health coverage at country and global levels: framework, measures and targets. 2014. [cited 2021 Jul 26]. Available from: https://apps.who.int/iris/handle/10665/112824. [DOI] [PMC free article] [PubMed]
- 18.Organization for Economic Cooperation and Development Exchange rates. 2021. [cited 2021 Jul 23]. Available from: https://data.oecd.org/conversion/exchange-rates.htm.
- 19.Nurrika D, Zhang S, Discacciati A, Tomata Y, Liu Y, Sugawara Y, et al. Education level, monthly per-capita expenditure, and healthy aging in the older Indonesian population: the Indonesia Family Life Survey 2007 and 2014. Tohoku J Exp Med. 2020;250(2):95–108. doi: 10.1620/tjem.250.95. [DOI] [PubMed] [Google Scholar]
- 20.Cao J, Rammohan A. Social capital and healthy ageing in Indonesia. BMC Public Health. 2016;16:631. doi: 10.1186/s12889-016-3257-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ahmed S, Tariqujjaman M, Rahman MA, Hasan MZ, Hasan MM. Inequalities in the prevalence of undiagnosed hypertension among Bangladeshi adults: evidence from a nationwide survey. Int J Equity Health. 2019;18(1):33. doi: 10.1186/s12939-019-0930-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Haider MR, Das Gupta R. Inequalities in undiagnosed hypertension among adult Nepalese population: evidence from a nationally representative survey. Int J Cardiol Hypertens. 2020;5:100026. doi: 10.1016/j.ijchy.2020.100026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lim OW, Yong CC. The risk factors for undiagnosed and known hypertension among Malaysians. Malays J Med Sci. 2019;26(5):98–112. doi: 10.21315/mjms2019.26.5.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Johar M, Soewondo P, Pujisubekti R, Satrio HK, Adji A. Inequality in access to health care, health insurance and the role of supply factors. Soc Sci Med. 2018;213:134–145. doi: 10.1016/j.socscimed.2018.07.044. [DOI] [PubMed] [Google Scholar]
- 25.Hasan MM, Tasnim F, Tariqujjaman M, Ahmed S, Cleary A, Mamun A. Examining the prevalence, correlates and inequalities of undiagnosed hypertension in Nepal: a population-based cross-sectional study. BMJ Open. 2020;10(10):e037592. doi: 10.1136/bmjopen-2020-037592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Seyed Reza SR, Bayani M, Zabihi A, Shakerian M, Habibian T, Bijani A. Undiagnosed hypertension and diabetes among the elderly in Amirkola, North of Iran. Caspian J Intern Med. 2019;10(3):303–308. doi: 10.22088/cjim.10.3.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Talukdar JR, Mahmud I, Rashid SF. Primary health care seeking behaviour of people with physical disabilities in Bangladesh: a cross-sectional study. Arch Public Health. 2018;76:43. doi: 10.1186/s13690-018-0293-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Scheppers E, van Dongen E, Dekker J, Geertzen J, Dekker J. Potential barriers to the use of health services among ethnic minorities: a review. Fam Pract. 2006;23(3):325–348. doi: 10.1093/fampra/cmi113. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Logistic regression analyses of the association between employment status and undiagnosed hypertension in the Indonesia Family Life Survey (IFLS) 2014-2015 stratified by sex1.


