Abstract
Objective
Testicular torsion is a common urological emergency, mainly in the younger population. Our aim is to evaluate the efficacy and value of testicular echogenicity in predicting testicular viability.
Methods
Patients who were older than 13 years of age and were discharged with the diagnosis of testicular torsion were reviewed. Data obtained included demographic data, history, physical examination results, ultrasound findings including size, color Doppler flow, and echotexture, torsion degrees, and surgical procedure. In addition, the histopathological findings of patients who underwent orchiectomy were reviewed.
Results
A total of 71 cases were diagnosed with testicular torsion between January 2016 to December 2018. The mean age at presentation was 20.4±7.0 years. The average time from the onset of pain until the presentation was 36.0±55.1 h. Out of the 71 ultrasound scans reviewed, 45.1% showed homogenous echotexture and 54.9% showed heterogeneous echotexture of the affected testis. On scrotal exploration, the mean degree of torsion was 475.7±301.8 degrees; 66.2% of the patients had a viable testis; and bilateral orchidopexy was done. The remaining 33.8% had a non-viable testis. Homogenous echotexture was after an average of 13.5 h of scrotal pain, while heterogeneous echotexture presented after 53.7 h of scrotal pain. There was a statistically significant difference between the time of presentation and echotexture changes on scrotal ultrasonography (p<0.01). The relationship between echotexture changes and testicular viability was statistically significant as well (p<0.001).
Conclusion
A long time since the onset of pain coupled with heterogeneous changes in testicular parenchyma is a good indicator of non-viability. However, we still advocate for surgical exploration as the gold standard in diagnosis and management.
Keywords: Testis, Testicular torsion, Orchiopexy, Orchiectomy, Ultrasound, Echotexture
1. Introduction
Testicular torsion involves twisting of the spermatic cord and its contents along with its longitudinal access with resultant ischemia. It is a urological emergency with an annual incidence of 4.5 per 100 000 in males younger than 25 years old, however, it can also occur at any age [1]. Predisposing factors include Bell-Clapper deformity, changes in temperature, which could activate cremasteric reflex, the rapid growth of testes during puberty, and cryptorchidism [[2], [3], [4]]. Furthermore, it has been reported that there could be a familial predisposition to torsion [5]. Clinically, a presentation of acute unilateral scrotal pain at rest is the most alarming symptom. Prompt work-up and management of this case is of paramount importance, as the time to diagnosis is directly proportional to testicular viability [6].
Imaging modalities have been known to aid in diagnosing testicular torsion. Although modalities such as radionuclide imaging of the testes have been previously used and offer good sensitivity and specificity, currently the most common imaging modality is color Doppler ultrasonography (CDU) due to its ease of use, availability and lack of radiation. CDU can be used to assess the size, shape, echogenicity, and perfusion status of both testes. The finding of a relative reduction or absence of blood flow usually indicates immediate surgical exploration [6]. CDU offers sensitivity and specificity rates of 63.6%–100.0% and 97%–100%, respectively [7].
Assessing echogenicity is useful in predicting the likelihood of testicular salvage on scrotal exploration. The affected testis’ parenchymal echotexture, compared with the contralateral testis, has been used as an indicator for viability. Middleton et al. [8] demonstrated that sonography could provide useful information regarding testicular viability. However, they recommend immediate surgical detorsion regardless of the findings. Kaye et al. [9] reported similar findings in a study involving 55 patients. Heterogeneous echotexture was predictive of organ loss with an accuracy rate of 96.4%. They stated that homogenous echotexture is predictive of organ viability, and thus justifies immediate surgical intervention. On the other hand, heterogeneous echotexture is predictive of organ loss, and accordingly, patients with this finding should not be exposed to the unnecessary risks associated with anesthesia and surgery. Instead, they could be offered an elective orchiectomy and contralateral orchiopexy later. Recent studies have further investigated the use of echogenicity via the implementation of an objective assessment tool known as the heterogeneity index (HI). The difference between the HI of the torsed and normal testis was expressed as ΔHI, and yielded a sensitivity and specificity of 100% and 94.5%, respectively [10]. Since ultrasonographic assessment may be used in the work-up of testicular torsion and can provide useful information regarding the status of the testis at the bedside, we aim to evaluate the efficacy and value of testicular echogenicity in predicting testicular viability.
2. Methods
This is a retrospective observational study. All patients discharged with the diagnosis of testicular torsion from January 2016 to December 2018 in Salmaniya Medical Complex, which is the main public hospital in the Kingdom of Bahrain, were reviewed. Patients below the age of 13 years and those presenting for scrotal exploration due to testicular trauma were excluded from the study. All the patients were examined by a senior urologist. Data obtained from the records include the following: Demographic data, history, physical examination results, ultrasound findings including size, color Doppler flow and parenchymal echotexture of both testes, whether the patient underwent orchiectomy or bilateral orchiopexy on scrotal exploration and the degrees of cord rotation. For patients who underwent orchiectomy, the histopathological findings were also reviewed. Scrotal ultrasound was performed using a 7.5 MHz linear transducer with color and spectral flow Doppler to evaluate the affected testis and the normal contralateral testis.
For data analysis, measures of central tendency such as the mean, standard deviation, median, and range were used. Also, the sensitivity, specificity, positive predictive value, and negative predictive value of echotexture changes in predicting testicular salvage were calculated. The Chi-squared test and t-test were used to compare any significant differences between the groups. A multivariate regression analysis was done to assess if echotexture changes and pain time were independently predictive of organ loss. Data were expressed as mean±standard deviation. Statistical significance was set at p-value <0.05. Statistical analysis was done using Statistical Package for Social Sciences (SPSS) version 23 (IBM Corp. Armonk, NY, USA).
3. Results
Between January 2016 to December 2018, 71 cases of testicular torsion were recorded. The mean age at presentation was 20.4±7.0 years and the average time from the onset of pain till presentation at the emergency room was 36.0±55.1 h (median: 10 h, range: 1–336 h) (Table 1), with only 35% presenting within 6 h. All the patients presented to the hospital's Accident and Emergency Department with the complaint of unilateral scrotal pain.
Table 1.
Demographic data and patient characteristics.
| Characteristic | Value |
|---|---|
| Age, year | |
| Mean±SD | 20.4±7.0 |
| Range | 13–46 |
| Location on ultrasound scan, n (%) | |
| Right | 36 (50.7) |
| Left | 28 (39.4) |
| Not identified | 7 (9.9) |
| Time from pain onset, h | |
| Mean ± SD | 36.0±55.1 |
| Median | 10 |
| Range | 1–336 |
| Testicular size on ultrasound, cm3 | |
| Normal testis | 3.68±0.98 |
| Torsed testis | 3.96±0.98 |
| CDU findings, n (%) | |
| Normal flow | 9 (12.7) |
| Abnormal flow | 54 (76.1) |
| No report | 8 (11.3) |
| Echotexture changes, n (%) | |
| Homogenous | 32 (45.1) |
| Heterogeneous | 39 (54.9) |
| Degree of rotation, degree | |
| Viable | 405.0±273.1 |
| Non-viable | 652.5±314.5 |
| Testicular viability, n (%) | |
| Viable | 47 (66.2) |
| Non-viable | 24 (33.8) |
| Histopathology, n (%) | |
| Infarction/necrosis | 23 (95.8) |
| Malignancy | 1 (4.2) |
SD, standard deviation; CDU, color Doppler ultrasonography.
On ultrasound assessment, 50.7% and 39.4% of the cases were confirmed as either right or left testicular torsion respectively. Around 9.9% of the cases were reported to have no evidence of torsion. On color Doppler ultrasonography, most cases (56.3%) had an absent flow to the affected testis. It is worthy to note that 11.3% of the cases had no documentation of CDU, either due to missing reports or referrals from external centers. A finding of normal flow was reported in patients who presented within 17.4±16.1 h of pain (median: 11.5 h, range: 1.5–48.0 h) in comparison to an abnormal flow in patients who presented within 36.9±57.3 h of pain (median: 10 h, range: 1–366 h) (p<0.05). There was no association between abnormal CDU findings and parenchymal echotexture changes on ultrasonography (p>0.05) or testicular loss (p>0.05).
Out of the 71 reports reviewed, 45.1% showed homogenous echotexture and 54.9% showed heterogeneous echotexture of the affected testis. On scrotal exploration and testicular delivery, the affected testis was rotated an average of 475.7±301.8 degrees. Moreover, 66.2% of the patients had a viable testis and a bilateral orchidopexy was done. The remaining 33.8% had a non-viable testis and thus orchiectomy was done (Figure 1, Figure 2). Histopathological findings going with testicular torsion were found in 95.8% of the orchiectomy specimens, while 4.2% also had a finding of a testicular tumor as well (Table 1).
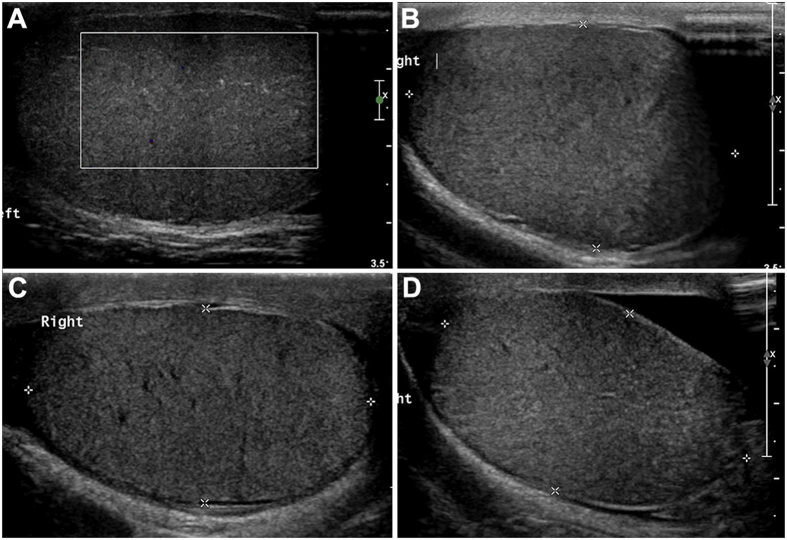
Figure 1.
Testes with homogenous echotexture. Figures A–C were viable on exploration; Figure D was non-viable and orchiectomy was done.
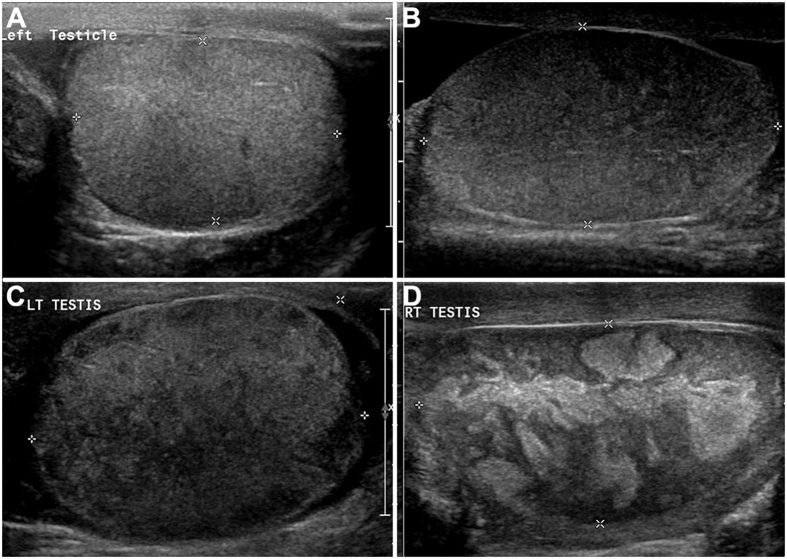
Figure 2.
Testes with heterogeneous echotexture. All four were non-viable on scrotal exploration.
Echotexture changes on ultrasound were related to how long patients waited before seeking help after the onset of pain. Patients with homogenous echotexture presented to the accident and emergency department after an average of 13.5±15.1 h of scrotal pain (median: 5.5 h, range: 2.0–48.0 h), while patients with heterogeneous echotexture presented after 53.7±67.7 h of scrotal pain (median: 48.0 h, range: 1.0–336.0 h). There was a statistically significant difference between the mean time of presentation and echotexture changes on scrotal ultrasonography (p<0.01). Orchidopexy was done for patients presenting after an average of 13.7±17.3 h of pain (median: 5.0 h, range: 1.5–72.0 h), while orchiectomy was done for patients presenting with an average of 77.9±74.9 h of pain (median: 60.0 h, range: 1.0–336.0 h) (Table 1). Testicular loss was associated with longer durations of pain before seeking medical care (p<0.001). Likewise, heterogeneous parenchymal changes on ultrasound were associated with testicular loss (p<0.001). Based on our data, using echotexture changes in ultrasound to predict testicular viability yielded a sensitivity of 95.8% (23/24), specificity 66.0% (31/47), positive predictive value 59.0% (23/39) and negative predictive value 96.9% (31/32) (Table 2). There were no significant differences in echotexture changes with the average degrees of torsion (p>0.05); however, we found that viable testes had an average of 405.0±273.1 degrees of torsion in contrast to 652.5±314.5 degrees in non-viable testes (p<0.05). A multivariate analysis was carried out to evaluate the relationship between pain time and heterogeneity with organ loss. We found that both pain time (OR: 1.04, 95% CI 1.012–1.078, p<0.01) and heterogeneity (OR: 0.05, 95% CI: 0.006–0.494, p=0.01) were correlated with the risk of organ loss.
Table 2.
Comparison of the surgical outcomes depending on ultrasonographic echotexture changes.
| Label | Non-viable (orchiectomy), n | Viable (bilateral orchidopexy), n | Total, n |
|---|---|---|---|
| Heterogeneous echotexture (positive test) | 23 | 16 | 39 |
| Homogenous echotexture (negative test) | 1 | 31 | 32 |
| Total | 24 | 47 | 71 |
4. Discussion
Traditionally, 6 h has been identified as the cut point for ischemia. The likelihood of testicular viability after this period decreases substantially, with the chances of viability decreasing from 97% to 100% at 6 h to 0%–9% after 24 h [8]. The assessment of pain duration relies mainly on the patient's recall during the clinical interview and could be distorted. A literature review of similar studies shows that testicular torsion cases have an organ loss rate of 14.5%–34% [1,[10], [11], [12], [13], [14], [15]]. We report a mean pain time of 36 h (range: 1–336 h), which is fairly longer than what was described in the literature, and only 33.8% (n=24) required orchiectomy. Although our loss rate is within the reported range, it is still relatively high. This can be attributed to the delayed presentation of patients to the hospital. It is suggested that prolonged symptoms increase the risk of finding a non-viable testis at exploration, with the primary cut point being 6 h of pain [8]. In our study, orchidopexy was done for patients presenting after an average of 13.7 h of pain, while orchiectomy was done for patients presenting after an average of 77.9 h of pain (p<0.01). Although our data go with the literature, we report a longer time of pain at presentation [9,12,16]. Likewise, we found that organ loss is also associated with the degree of torsion. Viable testes had lesser twists than their non-viable counterparts (405.0 degrees vs. 652.5 degrees, p<0.05). This finding was first reported on a large scale by Filho et al. [17], who demonstrated that a higher degree of cord rotation increases the risk of testicular non-viability on exploration. Among 117 patients reviewed, orchiectomy patients had higher degrees of cord rotation than orchidopexy patients (median: 450 degrees vs. 360 degrees, p<0.001). These findings were supported by a more recent study that reported similar results in viable and non-viable testes of 81 patients diagnosed with testicular torsion (median: 360 degrees vs. 540 degrees, p = 0.06) [18].
Prior literature has considered heterogeneity as a tool to assess testicular viability post torsion. It was found that a Doppler flow proving testicular torsion with heterogeneous parenchymal changes predicted testicular non-viability upon exploration [8,9]. Middleton et al. [8] reported these findings in 1997, where they concluded that heterogeneity was the best predictor for testicular viability. Their cohort included 16 patients with all heterogeneous testes being non-viable on scrotal exploration. Our findings support the aforementioned study in that echotexture changes are predictive of testicular viability (p<0.001). However, our numbers are less accurate, with a sensitivity of 95.8%, specificity 66.0%, positive predictive value 59.0%, and negative predictive value 96.9%. Moreover, a multivariate analysis to heterogeneity as a predictive factor independent of pain time for testicular loss yielded positive results. Currently, there are other more accurate emerging uses of ultrasonography that aid in the prediction of organ loss. Objective measurement tools such as heterogeneity index [10] and dynamic range [19] have been studied with good results reaching up to 100% sensitivity and 94.5% specificity. These methods include using a dithering technique based on the Floyd-Steinberg algorithm, in which ultrasound image pixels are converted into a binary map from which the echotexture is assessed against a set cut-off point. However, the major limitations behind both methods are the need for proprietary software, which limits their access, and retrospective application, thus lacking real-time application to assess their reliability in acute settings.
Regarding the management of testicular torsion, the standard of care is prompt surgical exploration. Kaye et al. [9] recommend otherwise in patients with heterogeneous changes on ultrasonography. They studied a cohort of 55 patients who underwent scrotal exploration with the diagnosis of torsion. All the patients with heterogeneous echotexture changes (n=37) had a non-viable testis on scrotal exploration [9]. They concluded that preoperative heterogeneity on ultrasound was a predictive marker for organ loss with an accuracy of 96.5% (p<0.001). They recommended an emergency surgical exploration for patients with homogenous echotexture changes. On the other hand, elective orchiectomy was recommended for a patient with heterogenous testicular echotexture as heterogeneity is an indicator of necrosis and testicular non-viability. It was found that anesthesia and surgery were unnecessary given the low chances of testicular salvage. Instead, a better alternative would be to reschedule the surgery as an elective orchiectomy with contralateral orchiopexy. Based on our study's findings, we disagree with the suggestion put forward by Kaye et al. [9]. First, the accuracy of ultrasonography is operator dependent, and hence results could vary greatly depending on the operator's experience, facilities available and examination setting. Second, our data show that the salvage rate among patients with heterogeneous echotexture is much lower than the homogenous counterpart (41.0% [16/39] vs. 96.8% [31/32]) (Table 2). This goes with the general trend of post-exploration viability; however, the number of viable testes with heterogeneous echotexture that we report is very high compared to what was reported by Kaye et al. [9] and Middleton et al. [8] (0% and 0%). Therefore using echotexture changes to guide management is not reliable. Instead, we can use echotexture changes on ultrasound to predict viability and to help us with patient counseling. Regardless, we still advocate early exploration of any suspected case of testicular torsion as the accuracy of ultrasound is heavily operator dependent. We agree with Middleton et al. [8] in this approach as ultrasonography findings are not definitive, and an incorrect assessment of non-viability can lead to disastrous outcomes.
Recently, there has been a debate on the necessity of pre-operative ultrasound, as it can lead to unnecessary delays in management. Per our institute's policies, all the patients in this study had a preoperative ultrasound. We think that ultrasonography should be done to all patients presenting with the clinical features of testicular torsion. Although ultrasonographic findings such as color Doppler flow and testicular echogenicity may not dictate the management of cases that are direct and clear, we believe it can be of value in equivocal presentations and patients presenting after pain durations that exceed the known timeframe for organ viability. This radiological information provides a good estimate of the testis' viability and the likelihood of orchiectomy after scrotal exploration, both of which are very important to know when counseling patients preoperatively. Furthermore, our institute policies acknowledge that testicular torsion is a clinical diagnosis. However, they still mandate that all patients presenting with acute scrotum, namely suspected cases of torsion, be evaluated with a scrotal ultrasound on arrival and referred to urology immediately. Therefore, ultrasound is readily available in the emergency room and is done at the bedside while the patient is being prepared for theater. This practice has been useful at our institution as it has increased detection rates and minimized the risk of missing a case of torsion by either the emergency physician or urologist. Nevertheless, studies in the literature do not share our experience with the universal usage of ultrasonography in such cases. Chen and Esler [20] found that a preoperative ultrasound resulted in a mean delay of 3.5 h. Another study in New Zealand also reported similar findings, although no statistical significance was found (p>0.05) [21].
Lastly, we found that only 35% of our patients sought medical attention within 6 h from the onset of scrotal pain. Such a finding is alarming, as presentation beyond 6 h increases the rate of orchiectomy [8]. Another issue we noticed was that none of the patients in our cohort could be followed up in the urology clinics after the first post-operative appointment. We attempted to contact and invite all the patients to our clinics for clinical examination, hormonal profile, and semen analysis, but none came. This could indicate a shortcoming in the public's knowledge and awareness of testicular torsion as a urological emergency and its long-term implications. Alyami et al. [22] surveyed 200 parents and found that only 19% of the parents whose children were patients in the pediatric urology clinic and 14% in the general pediatrics clinic were aware of the condition and its consequences. Comparable results were also reported by Friedman et al. [23] and Ubee et al. [24]. Another study in Nigeria targeting at undergraduate male students found that only 28.2% were aware that testicular torsion was an emergency condition [25]. Bahrain is a small island nation of less than 1000 km2 in land area, and healthcare is accessible and universal. There are no geographical, economical, or cultural barriers that explain the delayed time of presentation seen in this study. The only plausible explanation is that there is a relatively low level of public awareness about testicular torsion. We believe that the public's knowledge and awareness of testicular torsion in Bahrain need to be assessed. Consequently, a more comprehensive approach towards raising awareness should be put in action to make sure that the gravity and long-term consequences of this condition are understood.
A potential limitation of this study is that it is a retrospective cohort study with a relatively small sample size. Also, the duration of scrotal pain was mainly based on the patient's recall and is subject to recall bias. We believe that a larger sample could provide us with a more holistic assessment and possibly raise other research questions that need to be answered. Another limitation is the lack of long-term follow-up as none of our patients visited our clinic after the first post-operative appointment. This deprives us of valuable information about the difference between salvaged testes' long-term outcomes with either homogenous or heterogeneous echotexture changes. We advocate to further this study prospectively and compare the prognostic value of different emerging objective measures such as the logarithmic modules versus parenchymal echotexture changes on ultrasonography at the bedside in similar conditions.
5. Conclusion
Echotexture changes on ultrasound, namely heterogeneous changes, aid in evaluating the prognosis of testicular viability. A long time since the onset of pain and heterogeneous changes in testicular parenchyma are good indicators of non-viability. Although an objective measurement tool is still needed, we believe that coupling pain time and echotexture changes can provide us with valuable information when managing testicular torsion cases. In our experience, echotexture changes did well as a predictive tool. However, 41% (16/39) of testes with heterogeneous were still viable on scrotal exploration and underwent orchidopexy. Therefore, we still advocate that surgical exploration of the testis is the best next step in management and should be done regardless of the ultrasonographic findings.
Author contributions
Study Design: Omran Hasan, Mohamed Mubarak, S. Mohamed Jawad Alwedaie.
Data Collection: Husain Alaradi, Ali Alaradi, Ameer Alarayedh.
Data Analysis and Interpretation: Omran Hasan, Mohamed Mubarak, Hasan Bakhsh.
Drafting of Manuscript: Omran Hasan, Mohamed Mubarak, S. Mohamed Jawad Alwedaie, Hasan Bakhsh.
Critical Revision of the Manuscript: Husain Alaradi, Abdolsalam Ahmadi, Akbar Jalal.
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Peer review under responsibility of Tongji University.
References
- 1.Mansbach J.M., Forbes P., Peters C. Testicular torsion and risk factors for orchiectomy. Arch Pediatr Adolesc Med. 2005;159:1167–1171. doi: 10.1001/archpedi.159.12.1167. [DOI] [PubMed] [Google Scholar]
- 2.Chiu B., Chen C.S., Keller J.J., Lin C.C., Lin H.C. Seasonality of testicular torsion: A 10-year nationwide population based study. J Urol. 2012;187:1781–1785. doi: 10.1016/j.juro.2011.12.104. [DOI] [PubMed] [Google Scholar]
- 3.Chen J.S., Lin Y.M., Yang W.H. Diurnal temperature change is associated with testicular torsion: A nationwide, population based study in Taiwan. J Urol. 2013;190:228–232. doi: 10.1016/j.juro.2013.02.013. [DOI] [PubMed] [Google Scholar]
- 4.Arce J.D., Cortes M., Vargas J.C. Sonographic diagnosis of acute spermatic cord torsion. Rotation of the cord: A key to the diagnosis. Pediatr Radiol. 2002;32:485–491. doi: 10.1007/s00247-002-0701-z. [DOI] [PubMed] [Google Scholar]
- 5.Cubillos J., Palmer J.S., Friedman S.C., Freyle J., Lowe F.C., Palmer L.S. Familial testicular torsion. J Urol. 2011;185(Suppl 6):2469–2473. doi: 10.1016/j.juro.2011.01.022. [DOI] [PubMed] [Google Scholar]
- 6.Sharp V.J., Kieran K., Arlen A.M. Testicular torsion: Diagnosis, evaluation, and management. Am Fam Physician. 2013;88:835–840. [PubMed] [Google Scholar]
- 7.Radmayr C., Bogaert G., Dogan H.S., Nijman J.M., Rawashdeh Y.F.H., Silay M.S., et al. EAU paediatric urology guidelines. https://uroweb.org/wp-content/uploads/EAU-Guidelines-on-Paediatric-Urology-2021.pdf [Accessed 10 January 2020]
- 8.Middleton W.D., Middleton M.A., Dierks M., Keetch D., Dierks S. Sonographic prediction of viability in testicular torsion: Preliminary observations. J Ultrasound Med. 1997;16:23–27. doi: 10.7863/jum.1997.16.1.23. quiz 29-30. [DOI] [PubMed] [Google Scholar]
- 9.Kaye J.D., Shapiro E.Y., Levitt S.B., Friedman S.C., Gitlin J., Freyle J., et al. Parenchymal echo texture predicts testicular salvage after torsion: Potential impact on the need for emergent exploration. J Urol. 2008;180(Suppl 4):1733–1736. doi: 10.1016/j.juro.2008.03.104. [DOI] [PubMed] [Google Scholar]
- 10.Cost N.G., Bush N.C., Barber T.D., Huang R., Baker L.A. Pediatric testicular torsion: Demographics of national orchiopexy versus orchiectomy rates. J Urol. 2011;185:2459–2463. doi: 10.1016/j.juro.2011.01.016. [DOI] [PubMed] [Google Scholar]
- 11.Waldert M., Klatte T., Schmidbauer J., Remzi M., Lackner J., Marberger M. Color Doppler sonography reliably identifies testicular torsion in boys. Urology. 2010;75:1170–1174. doi: 10.1016/j.urology.2009.07.1298. [DOI] [PubMed] [Google Scholar]
- 12.Al-Hunayan A.A., Hanafy A.M., Kehinde E.O., Al-Awadi K.A., Ali Y.M., Al-Twheed A.R., et al. Testicular torsion: A perspective from the Middle East. Med Princ Pract. 2004;13:255–259. doi: 10.1159/000079523. [DOI] [PubMed] [Google Scholar]
- 13.Lee S.M., Huh J.S., Baek M., Yoo K.H., Min G.E., Lee H.L., et al. A nationwide epidemiological study of testicular torsion in Korea. J Kor Med Sci. 2014;29:1684–1687. doi: 10.3346/jkms.2014.29.12.1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Huang W.Y., Chen Y.F., Chang H.C., Yang T.K., Hsieh J.T., Huang K.H. The incidence rate and characteristics in patients with testicular torsion: A nationwide, population-based study. Acta Paediatr. 2013;102 doi: 10.1111/apa.12275. e363-7. [DOI] [PubMed] [Google Scholar]
- 15.Zhao L.C., Lautz T.B., Meeks J.J., Maizels M. Pediatric testicular torsion epidemiology using a national database: Incidence, risk of orchiectomy and possible measures toward improving the quality of care. J Urol. 2011;186:2009–2013. doi: 10.1016/j.juro.2011.07.024. [DOI] [PubMed] [Google Scholar]
- 16.Dunne P., O'Loughlin B. Testicular torsion: Time is the enemy. Aust N Z J Surg. 2000;70:441–442. doi: 10.1046/j.1440-1622.2000.01853.x. [DOI] [PubMed] [Google Scholar]
- 17.Filho A.C.D., Alves J.R., Filho H.B., de Oliveira P.G. The amount of spermatic cord rotation magnifies the time related orchidectomy risk in intravaginal testicular torsion. Int Braz J Urol. 2016;42:1210–1219. doi: 10.1590/S1677-5538.IBJU.2016.0166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Howe A.S., Vasudevan V., Kongnyuy M., Rychik K., Thomas L.A., Matuskova M., et al. Degree of twisting and duration of symptoms are prognostic factors of testis salvage during episodes of testicular torsion. Transl Androl Urol. 2017;6:1159–1166. doi: 10.21037/tau.2017.09.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ghorayeb S., Hartman C., Samson P., Yamashita Y., Palmer S. Paper presented at the proceedings of the 2nd international conference on biomedical engineering and systems, Barcelona, Spain. 2015. Ultrasonic evaluation of heterogeneity levels in normal and torsed testes.http://www.avestia.com/EECSS2015_Proceedings/files/papers/ICBES297.pdf No. 297. [Google Scholar]
- 20.Chen M., Esler R. Accuracy and delay of using ultrasound in testicular torsion. J Urol Surg. 2019;6:273–277. [Google Scholar]
- 21.Johnston J.W., Larsen P., El-Haddawi F.H., Fancourt M.W., Farrant G.J., Gilkison W.T., et al. Time delays in presentation and treatment of acute scrotal pain in a provincial hospital. ANZ J Surg. 2015;85:330–333. doi: 10.1111/ans.12601. [DOI] [PubMed] [Google Scholar]
- 22.Alyami F.A., Modahi N.H., Alharbi A.M., Alkhelaif A.A., Alhazmi H., Trbay M.S., et al. Parents' awareness and knowledge of testicular torsion: A cross-sectional study. Urol Ann. 2019;11:58–61. doi: 10.4103/UA.UA_62_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Friedman A.A., Ahmed H., Gitlin J.S., Palmer L.S. Standardized education and parental awareness are lacking for testicular torsion. J Pediatr Urol. 2016;12 doi: 10.1111/apa.12275. 166.e1–8. [DOI] [PubMed] [Google Scholar]
- 24.Ubee S.S., Hopkinson V., Srirangam S.J. Parental perception of acute scrotal pain in children. Ann R Coll Surg Engl. 2014;96:618–620. doi: 10.1308/003588414X14055925058878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bayo S.O., Fredrick O.O., Obafemi S.J. Awareness and sources of information relating to testicular self-examination and torsion among male undergraduates in a Nigerian university. Int J Med Med Sci. 2014;1:143–150. [Google Scholar]