Abstract
Pre-pandemic disparities placed Latinos at risk for COVID-19. This report describes the associations between increased viral exposure through social contact and material hardship and the uneven distribution of COVID-19 morbidity among Latino older adults using data from the recently released supplement to the National Social Life, Heath, and Aging Project (NSHAP) (N = 2672), a population-based panel study of adults born 1920–1965. Logistic regression revealed that material hardship and reliance on outside help were significantly correlated with COVID-19 infection, which may partially explain the disproportionate burden Latinos experience during the pandemic.
Keywords: COVID-19, health disparities, hispanics, Latinos
Pre-pandemic disparities in living and working conditions placed Latinos at higher risk for COVID-19. U.S. Latinos are three times as likely to get COVID-19 and twice as likely to die of it than the general population (Oppel et al., 2020), reducing life expectancy estimates from a survival advantage of more than 3 years to less than one (Andrasfay & Goldman, 2021). However, research on factors that have contributed to Latino older adults’ vulnerability during the pandemic has been thin (Sáenz & Garcia, 2021).
Latinos disproportionately live in dense neighborhoods and larger households, which pose barriers to social distancing (U.S. Census Bureau, 2020). They are more than twice as likely to live in multi-generational households (Cohn & Passel, 2016; Johnson & Appold, 2017) and four times as likely to live with their grandchildren (Chen et al., 2015) than non-Latino whites.
Latinos are overrepresented among essential workers in industries most affected by the pandemic (Rho et al., 2020), which increased their viral exposure (Hooper et al., 2020); only 16% of Latinos reported being able to work from home, compared to 31.4% of non-Latino Whites (Gould & Shierholz, 2020). This disparity is further accentuated among foreign-born Latinos and those residing in mixed citizenship-status households because many immigrants, even those with lawful status, may not qualify for federal pandemic relief and safety net programs (Gonzalez et al., 2020; Olayo-Méndez et al., 2021). Moreover, the inclination for people to associate with others who share their ethnicity, religion, education, and occupation reinforces the concentration of disadvantage for those who are already underprivileged (Smith et al., 2014), which means that for populations where disadvantage converges along racial/ethnic and class lines, we can expect to see disproportionate pandemic-related outcomes (Gauthier et al., 2021).
Economic hardships among Latinos are well-documented. Nationwide, 61% reported job or income loss in the household during COVID-19, far more than non-Latino Whites (38%) (Lopez et al., 2020). Karpman et al. (2020) found that 46% of Latinos (ages 18–64) reported material hardship—the inability to pay rent, mortgage, or utilities on time (or at all); ongoing food insecurity; and unmet medical needs—compared to 25% of non-Latino Whites. These vulnerabilities may motivate people to take unwanted health risks—such as increasing their involvement in an informal economy—to avoid material hardship (Venkatesh, 2006).
For this investigation, we used national data to investigate associations between increased viral exposure through social contact and material hardship and the uneven distribution of COVID-19 morbidity among Latino older adults.
Methods
Study Population and Data Source
We used data from a sample of community-dwelling older adults enrolled in the National Social Life, Health, and Aging Project (NSHAP), a population-based panel study of adults born 1920–1965 that began in 2005 (Waite et al., 2020). Sample recruitment and characteristics have been reported elsewhere (O’Muircheartaigh et al., 2009, 2014). The target sample for the recently released supplement study (NSHAP-COVID) was drawn from the 4777 respondents during the 2015–16 data collection (NSHAP-R3).
Data were collected between September 14, 2020, and January 27, 2021, using web, phone, and paper/pencil (PAPI) surveys; the projected sample size was 3390. Ultimately, 2650 individuals responded (79% of the target sample; 56% of the total NSHAP sample); 263 identified as Latino/Hispanic. All estimates are survey-weighted (using R3 weights) by the reciprocal of the probability of selection and adjusted for non-response based on age and urbanicity. Here, we compare these 263 Latinos with the sample’s 1913 non-Latino White participants; all provided written informed consent. National Opinion Research Center (NORC) at the University of Chicago (Protocol Number: 14.06.01) approved all protocols.
Participant Characteristics
Table 1 features the demographic characteristics of Latinos, non-Latino Whites, and the total sample. Compared to non-Latino Whites and the total sample, Latinos are younger (54% < 65 years). Nearly half (46%) were born outside the United States; 43% completed the survey in Spanish. Latinos reported lower levels of education; more than a third (34%) had less than high school. Non-Latino Whites preferred web-based (60%); Latinos favored data collection by phone (44%). Before the pandemic, most Latinos (91%) reported having enough (or more) income to meet basic needs; this number dropped to 66% during the pandemic. Compared to NSHAP-R3 Latino respondents, NSHAP-COVID Latino participants have higher levels of education, better self-rated health, and higher household income (p < .01).
Table 1.
Descriptive Statistics for Total Sample and by Latino/Non-Latino White Grouping.
| Variable | Total Sample | Latino | Non-Latino White | Group Contrast | |||
|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | p | |
| Sex | 2650 | 257 | 1913 | ||||
| Male | 43.95 | 50.37 | 44.01 | .047 | |||
| Female | 56.05 | 49.63 | 55.99 | ||||
| Age | 2650 | 257 | 1913 | ||||
| Mean (sd.) | 67.65 (9.65) | 64.80 (12.10) | 68.35 (8.86) | ||||
| < 65 | 42.41 | 53.90 | 39.44 | .003 | |||
| 65 < | 57.59 | 46.10 | 60.56 | .012 | |||
| Language of survey | 2650 | 257 | 1913 | ||||
| English | 96.86 | 56.96 | 100.00 | < .0001 | |||
| Spanish | 3.14 | 43.04 | 0.00 | ||||
| Nativity | 2384 | 222 | 1769 | ||||
| Foreign-born | 6.80 | 45.75 | 2.13 | < .0001 | |||
| Mode of survey | 2650 | 257 | 1913 | ||||
| Web | 56.59 | 42.56 | 59.52 | .003 | |||
| Phone | 34.12 | 44.34 | 31.61 | ||||
| Paper/pen | 9.29 | 13.10 | 8.87 | ||||
| Education | 2650 | 257 | 1913 | ||||
| Less than H.S. (High school) | 7.66 | 34.38 | 4.74 | < .0001 | |||
| H.S. diploma/equivalent | 21.06 | 14.04 | 21.67 | ||||
| Some college/professional degree | 35.97 | 28.13 | 36.29 | ||||
| College/Grad | 35.30 | 23.45 | 37.30 | ||||
| Married or partnered | 2650 | 74.95 | 257 | 75.63 | 1913 | 76.17 | .8841 |
| Income for basic needs (before COVID-19) | 2598 | 249 | 1881 | ||||
| More than enough | 45.39 | 26.16 | 50.88 | < .0001 | |||
| Enough | 45.98 | 65.02 | 41.82 | ||||
| Expenses somewhat greater than income | 6.63 | 6.47 | 5.77 | ||||
| Expenses much greater than income | 2.01 | 2.36 | 1.53 | ||||
| Ability to meet basic needs since COVID-19 | 2618 | 252 | 1894 | ||||
| Better off | 4.90 | 4.24 | 4.98 | ||||
| About the same | 75.10 | 62.70 | 77.51 | ||||
| Bit worse off | 15.97 | 24.48 | 14.02 | ||||
| Much worse off | 4.03 | 8.58 | 3.49 | ||||
| Since COVID-19, needed outside help with tasks | 2634 | 254 | 1906 | ||||
| Yes | 15.97 | 24.82 | 13.97 | .0011 | |||
| No | 84.03 | 75.18 | X | 75.18 | |||
| Work affected by COVID-19 | 2134 | 248 | 1886 | ||||
| Yes | 31.44 | 37.40 | 29.60 | .1441 | |||
| No | 20.70 | 21.99 | 20.54 | ||||
| Not working when it started | 47.85 | 40.61 | 49.86 | ||||
| Household size | 2625 | 251 | 1905 | ||||
| 1 person | 19.44 | 13.26 | 20.16 | ||||
| 2 persons | 53.54 | 36.64 | 57.53 | < .0001 | |||
| 3 + persons | 27.02 | 50.10 | 22.31 | ||||
| Youth ( < 18) in household | 2592 | 235 | 1895 | ||||
| Yes | 12.56 | 26.67 | 9.57 | < .0001 | |||
| No | 87.44 | 73.33 | 90.43 | ||||
| Positive diagnosis for a household member | 2546 | 225 | 1867 | ||||
| Yes | 6.09 | 13.59 | 5.26 | .0089 | |||
| No | 93.91 | 86.41 | 94.74 | ||||
| Positive diagnosis (outside household) | 2594 | 247 | 1883 | ||||
| Yes | 55.38 | 64.61 | 54.55 | .0105 | |||
| No | 44.62 | 35.39 | 45.45 | ||||
| Diagnosed with COVID-19 self | 2534 | 3.38 | 223 | 9.58 | 1861 | 2.72 | .0060 |
| Spouse/partner | 2437 | 2.45 | 210 | 4.87 | 1799 | 2.06 | .1021 |
| Someone else in household | 2471 | 2.96 | 221 | 9.32 | 1812 | 2.14 | .0005 |
| Friend/family not in household | 2549 | 38.20 | 233 | 44.61 | 1862 | 36.96 | .0317 |
| Acquaintance | 2515 | 42.49 | 224 | 52.20 | 1848 | 41.94 | .0363 |
| COVID-19related death (within household) | 2536 | 225 | 1856 | .0001 | |||
| Yes | .14% | 1.37% | 0.00% | ||||
| No | 99.86% | 98.63% | 100.0% | ||||
| COVID-19related death (outside household) | 2596 | 244 | 1888 | ||||
| Yes | 21.44 | 41.48 | 17.37 | < .0001 | |||
| No | 78.56 | 58.52 | 82.63 | ||||
| COVID-19related deaths | |||||||
| Spouse/partner | 2509 | 0.01 | 223 | 1.38 | 1840 | 0.00 | .0001 |
| Someone else in household | 2508 | 0.11 | 220 | 1.09 | 1843 | 0.00 | .0363 |
| Friend/family not in household | 2555 | 10.09 | 229 | 21.48 | 1870 | 6.49 | < .0001 |
| Acquaintance | 2541 | 16.51 | 229 | 34.77 | 1870 | 14.23 | < .0001 |
| Family in-person visits since COVID-19 | 2151 | 249 | 1902 | ||||
| Weekly or more often | 36.55 | 26.21 | 38.28 | < .0001 | |||
| Less than once per week | 40.98 | 38.97 | 41.31 | ||||
| Never | 22.47 | 34.82 | 20.41 | ||||
| Frequency of family visits before pandemic | 2124 | 244 | 1880 | ||||
| More often | 7.97 | 9.55 | 7.01 | ||||
| Less often | 37.95 | 49.02 | 35.97 | .0002 | |||
| Same | 54.08 | 41.43 | 57.02 | ||||
| Friend in-person visits since COVID-19 | 2142 | 248 | 1894 | ||||
| Everyday | 2.27 | 0 | 2.65 | ||||
| Weekly | 28.05 | 19.93 | 29.51 | < .0001 | |||
| Less than once per week | 44.49 | 35.69 | 46.38 | ||||
| Never | 25.19 | 44.38 | 21.46 | ||||
| Frequency of friend visits before pandemic | 2118 | 238 | 1880 | ||||
| More often | 6.32 | 7.04 | 5.42 | ||||
| Less often | 40.16 | 44.02 | 40.07 | .324 | |||
| Same | 40.07 | 48.94 | 54.52 | ||||
Half of Latino respondents live in households of three or more, compared to 22% of non-Latino Whites. Among these, nearly a third of Latinos live with at least one minor, compared to only 12% of non-Latino Whites. More Latinos were working before the pandemic (60%) than non-Latino Whites (50%) or the total sample (53%). More employed Latinos experienced COVID-19-related changes in their work (37%) than non-Latinos (30%).
Contrary to expectations, Latinos had less contact weekly with family (26% vs 38%) and friends (20% vs 33%) than non-Latino Whites. Nearly half (49%) reported that they saw their family less often than before the pandemic, compared to 36% of non-Latino Whites; visits by friends follow this pattern. However, Latinos were more likely to receive outside help with tasks (17%) than non-Latino Whites (8%).
Outcome Variables
We examined factors associated with affirmations to the question, Has a doctor or other healthcare provider diagnosed (a) you, (b) spouse/partner, (c) someone else in the household, (d) friend or family member outside the household, or (e) acquaintance with COVID-19?
Independent Variables
We examined the main effects of three exposure factors: household size (lives alone, two persons, or three or more), reliance on outside help for everyday tasks (yes/no), and experience of a change in work due to the pandemic (yes/no/not working). The variable “task help” indicated responses to the question: Since the start of the COVID-19 pandemic, have you relied on someone outside your household to regularly help you with everyday tasks? These tasks included running errands, getting necessities, completing household repairs, or arranging for outside services. We also examined material hardship, measured by the question: How has the pandemic affected your income and ability to meet your basic expenses and pay your bills [same/better or same/worse]? We hypothesized that these exposure factors and material hardship would be positively associated with COVID-19 diagnosis.
Statistical Analyses
Analyses were performed using STATA SE 16.1. All except the correlation analyses were weighted to account for selection probability. We used descriptive statistics to summarize and compare characteristics for the overall sample, chi-squared tests to compare categorical variables, and t-tests for continuous variables.
We used logistic regressions to examine the relationship between exposure variables, material hardship, and a COVID-19 diagnosis in the household. The following modeling procedures were used. In Model 1, diagnosis was adjusted for demographic variables and survey mode. Model 2 adjusted for all covariates in Model 1 and added household size. Model 3 included all covariates in Model 1 plus whether working prior to COVID-19 or if work changed due to COVID-19. Model 4 adjusted for all covariates included in Model 1 and added reliance on outside help for everyday tasks. Model 5 included Model 1 and added material hardship. Model 6 included all the exposure variables and material hardship. Model 7 was constrained to significant variables found in Models 2–5. We also conducted sensitivity tests to check the influence of preference for English language use, a crude indicator of acculturation; 57% of the Latino sample and 97% of the total sample completed the survey in English. We used chi-squared tests to examine the characteristics of Latino NSHAP-R3 participants who did not participate in the NSHAP-COVID study.
Results
Rates of COVID Infections
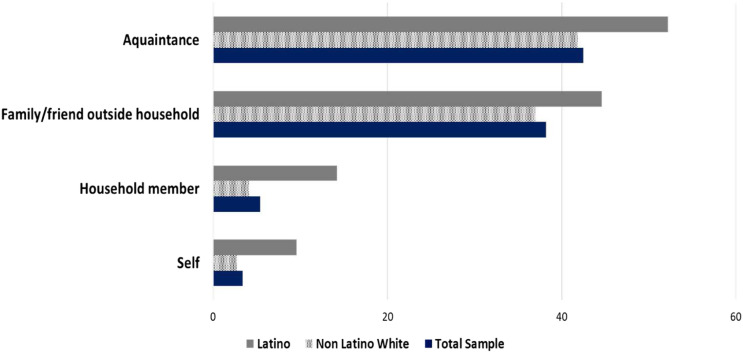
COVID-19 diagnoses were higher for Latinos than non-Latino Whites (see Figure 1). Nearly a quarter of Latino respondents reported that someone in their household had been diagnosed with COVID-19 compared to 7% of non-Latino Whites and 9% of the total sample. Diagnosis of COVID-19 among friends and family outside of the household were 45% for Latinos and 37% of non-Latino Whites.
Figure 1.
Percentage of COVID-19 diagnoses by total sample (N = 2650) and by Latino (N = 257) and non-Latino White grouping (N = 1913).
Association of Exposure Variables and Material Hardship with Infection
Table 2 displays the odds ratios (OR) for the association between household size, task help, work change, material hardship, and a COVID-19 diagnosis across Models 2–4. Model 5 displays the inclusion of material hardship. Task help in Model 4 (OR, 1.73; p < 0.05) and material hardship (OR, 2.21; p < 0.01) in Model 5 were significantly associated with a COVID-19 diagnosis within a household. As additional risk factors were introduced into Models 2–7, the statistical weight of the Latino coefficient decreased.
Table 2.
Odds Ratios of a Positive Household COVID-19 Diagnosis on Household Size, Work Change, Task Help, Material Hardship, and Covariates for Latinos and non-Latino Whites.
| Model 0 | Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | Model 7 | |
|---|---|---|---|---|---|---|---|---|
| N | 2092 | 2092 | 2081 | 2059 | 2083 | 2070 | 2026 | 2066 |
| Age (≥ 65) | 0.53* (0.32, 0.87) | 0.57* (0.35, 0.92) | 0.57 (0.307, 1.04) | 0.50** (0.30, 0.84) | 0.60 (0.35, 1.03) | 0.63 (0.33, 1.17) | 0.56* (0.33, 0.97) | |
| Female | 1.02 (0.71, 1.47) | 1.07 (0.729, 1.56) | 1.01 (0.69, 1.47) | 0.96 (0.66, 1.39) | 1.015 (0.70, 1.47) | 1.99 (0.69, 1.53) | 0.99 (0.68, 1.43) | |
| High school edu. | 0.84 (0.39, 1.83) | 0.84 (0.38, 1.85) | 0.83 (0.38, 1.79) | 0.99 (0.43, 2.30) | 0.996 (0.43, 2.31) | 1.069 (0.45, 2.54) | 1.05 (0.45, 2.42) | |
| Mode (Ref = Web) | ||||||||
| Phone | 0.99 (0.40, 2.43) | 1.04 (0.42, 2.57) | 0.91 (0.41, 2.47) | 0.913 (0.33, 2.30) | 0.95 (0.39, 2.30) | 0.94 (0.37, 2.36) | 0.89 (0.36, 2.19) | |
| PAPI | 1.65 (0.88, 3.10) | 1.75 (0.92, 3.30) | 1.61 (0.92, 3.23) | 1.61 (0.86, 3.03) | 1.59 (0.85, 2.99 | 1.75 (0.92, 3.33) | 1.59 (0.85,2.99) | |
| Latino | 2.84** (1.27, 6.35) | 2.46* (1.03, 5.84) | 2.37 (0.96, 5.82) | 2.34 (0.97, 5.60) | 2.23 (0.95, 5.23) | 2.15 (0.90, 5.13) | 1.89 (0.78, 4.58) | 2.078 (0.89, 4.88) |
| Household size (Ref = 1) | ||||||||
| 2 persons | 1.63 (0.84, 3.18) | 1.92 (0.95, 3.87) | ||||||
| 3 + persons | 1.85 (0.78, 4.36) | 2.13 (0.86, 5.26) | ||||||
| Work affected by COVID-19 | ||||||||
| Work changed | 1.31 (0.64,2.69) | 1.12 (0.51, 2.42) | ||||||
| Working before COVID-19 | 0.92 (0.52, 1.62) | 0.94 (0.51, 1.74) | ||||||
| Task help | 1.73* (1.02, 2.93) | 1.54 (0.98, 2.54) | 1.54 (0.94, 2.5) | |||||
| Material hardship | 2.21** (1.35, 3.59) | 2.12** (1.27, 3.53) | 2.10** (1.31, 3.36) | |||||
Note. Regression results represent Latino and non-Latino White respondents and are weighted using Round 3 NSHAP survey weights, accounting for differential probabilities for selection and non-response based on age and urbanicity. Sample sizes vary by model to account for missing data. Significance level * p < .05, ** p < .01, *** p < .001.
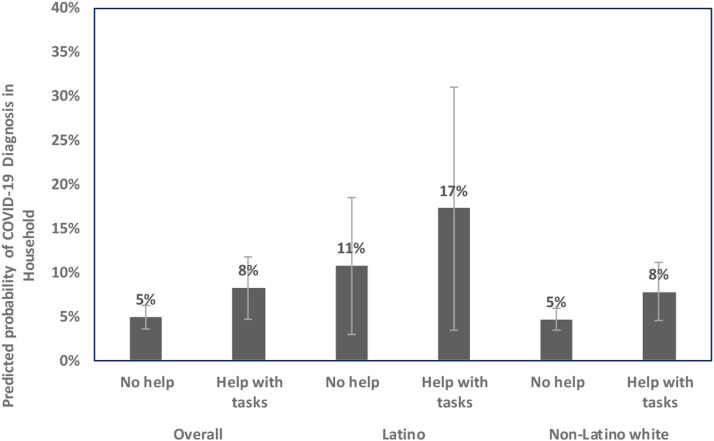
Figure 2 displays the probabilistic predictions of a COVID-19 diagnosis within a household given the presence of outside help with everyday tasks during the pandemic (Model 7). Latino respondents receiving help were 6 percentage points more likely to report a COVID-19 diagnosis within their household than those not receiving help. This difference among non-Latino White households and in the overall sample was 3 percentage points.
Figure 2.
Predicted probability of COVID-19 diagnosis in household for task help by overall sample (N = 2650), Latino (N = 257) and non-Latino White (N = 1913) groupings.Note. Predicted probability of COVID-19 diagnosis in household with controls for age, gender, education level, survey mode, Latino, material hardship, and task help (Model 7).
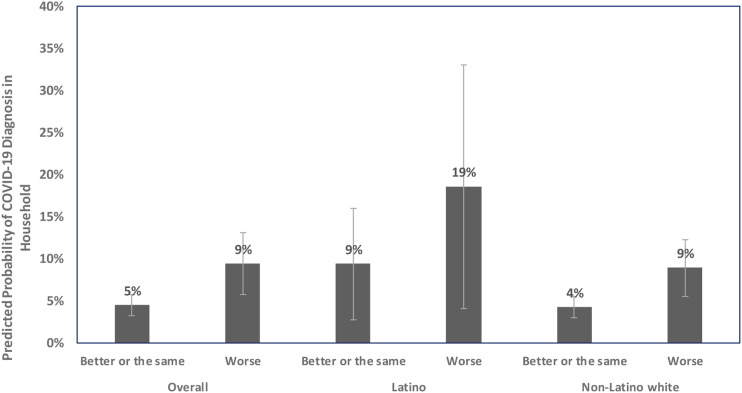
Figure 3 displays the probabilistic predictions of a COVID-19 diagnosis within a household by material hardship during the pandemic (Model 7). Latino respondents who reported being worse off financially during the pandemic were 10 percentage points more likely to report a COVID-19 diagnosis within their household than those who were financially better off or the same. In contrast, non-Latino Whites experiencing material hardship were 5 percentage points more likely to report a COVID-19 diagnosis.
Figure 3.
Predicted probability of COVID-19 diagnosis in household for material hardship by overall sample (N = 2650), Latino (N = 257) and non-Latino White (N = 1913) groupings.Note. Predicted probability of COVID-19 diagnosis in household with controls for age, gender, education level, survey mode, Latino, material hardship, and task help (Model 7).
Model 6 in Table 2 illustrates that in the single model including the three exposure factors and material hardship, material hardship remained significantly associated with a COVID-19 diagnosis within the household (OR, 2.12; p < .01). Similarly, in Model 7, material hardship alone was significantly associated with a COVID-19 diagnosis (OR, 2.10; p < .01).
Discussion
Our findings corroborate claims that the pandemic disproportionally affected older Latinos (Hooper et al., 2020; Sáenz & Garcia, 2021) and that these consequences are associated with pre-pandemic disadvantage (Gauthier et al., 2021). On average, Latinos live in larger households and experience worse material hardship. Material hardship and reliance on outside help emerged as the two most significant correlates, likely because they made social distancing difficult but also perhaps because they encouraged contact with informal economic networks that were less likely to adhere to public health mandates.
Study limitations include, first, limited generalizability. Although NSHAP is renowned for its rigorous data collection and high response rate (c.f., O’Muircheartaigh et al., 2014), the NSHAP-COVID respondents were younger, more likely to be female, White, highly educated, married, and in better health than R3 participants. Latino NSHAP-COVID respondents reported better self-rated health, more education, and less material hardship than Latino R3 participants. These comparisons suggest that our findings are understated; material hardship and the need for outside help likely heightened vulnerability to a greater degree than our findings reflect. Second, we have no way to ascertain the citizenship status of our participants (legal or otherwise) or whether they live in a mixed-status households, factors which coincided with worse material hardship during the pandemic. Third, although we tested for mortality, the small numbers of COVID-19 deaths precluded our ability to draw conclusions. However, we noted a similar trend for those who knew someone who died of COVID-19 and those who experienced a COVID-19 diagnosis in the household (analyses available upon request). Future research should consider the long-term impacts of the pandemic on Latinos, especially for those enduring material hardship and who must rely on outside help with daily tasks.
Acknowledgments
We wish to thank Kristen Wroblewski and Janet Liechty for their thoughtful comments, suggestions, and support. Thanks also to the JAG reviewers for their insightful feedback, which helped sharpen and strengthen the report.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: All research reported in this publication was supported by the National Institute on Aging of the National Institutes of Health (grant numbers: R01AG048511 and R01AG04538). The National Social Life, Health and Aging Project COVID-19 study (PI: Louise Hawkley) was supported with grant number AG043538-08S1. The lead author (Lissette Piedra) is supported by an administrative supplement (R01AG048511-08S1). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
ORCID iD
Lissette M. Piedra https://orcid.org/0000-0002-5201-5170
References
- Andrasfay T., Goldman N. (2021). Reductions in 2020 US life expectancy due to COVID-19 and the disproportionate impact on the Black and Latino populations. Proceedings of the National Academy of Sciences, 118(5), 1–6. 10.1073/pnas.2014746118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen F., Mair C. A., Bao L., Yang Y. C. (2015). Race/ethnic differentials in the health consequences of caring for grandchildren for grandparents. The Journals of Gerontology: Series B, 70(5), 793–803. 10.1093/geronb/gbu160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohn D. V., Passel J. S. (2016). A record 60.6 million Americans live in multigenerational households. Pew Research Center. https://www.pewresearch.org/fact-tank/2018/04/05/a-record-64-million-americans-live-in-multigenerational-households/ [Google Scholar]
- Gauthier G. R., Smith J. A., García C., Garcia M. A., Thomas P. A. (2021). Exacerbating inequalities: Social networks, racial/ethnic disparities, and the COVID-19 pandemic in the United States. The Journals of Gerontology: Series B, 76(3), Article e88–e92. 10.1093/geronb/gbaa117. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7454830/pdf/gbaa117.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez D., Karpman M., Kenney G. M., Zuckerman S. (2020). Hispanic adults in families with noncitizens disproportionately feel the economic fallout from COVID-19. Urban Publication. https://www.urban.org/sites/default/files/publication/102170/hispanic-adults-in-families-with-noncitizens-disproportionately-feel-the-economic-fallout-from-covid-19_0.pdf [Google Scholar]
- Gould E., Shierholz H. (2020). Not everybody can work from home: Black and Hispanic workers are much less likely to be able to telework. Economic Policy Institute. https://www.epi.org/blog/black-and-hispanic-workers-are-much-less-likely-to-be-able-to-work-from-home/ [Google Scholar]
- Hooper M. W., Nápoles A., Pérez-Stable E. (2020). COVID-19 and racial/ethnic disparities. JAMA, 323(24), 2466–2467. 10.1001/jama.2020.8598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson J. H., Appold S. (2017). U.S. older adults: Demographics, living arrangements, and barriers to aging in place. Kenan Institute. http://www.kenaninstitute.unc.edu/wp-content/uploads/2017/06/AgingInPlace_06092017.pdf [Google Scholar]
- Karpman M, Zuckerman S, Gonzalez D, Kenney G. M. (2020). The COVID-19 pandemic is straining families’ abilities to afford basic needs: Low-income and Hispanic families the hardest hit. Washington, DC: Urban Institute. https://www.urban.org/sites/default/files/publication/102124/the-covid-19-pandemic-is-straining-families-abilities-to-afford-basic-needs_2.pdf. [Google Scholar]
- Lopez M. H., Rainie L., Budiman A. (2020). Financial and health impacts of COVID-19 vary widely by race and ethnicity. Fact tank. Pew research center. https://pewrsr.ch/2L15rwr. [Google Scholar]
- Olayo-Méndez A., Vidal De Haymes M., García M., Cornelius L. J. (2021). Essential, disposable, and excluded: The experience of Latino immigrant workers in the US during COVID-19. Journal of Poverty, 25(17), 612-628. 10.1080/10875549.2021.1985034. [DOI] [Google Scholar]
- O’Muircheartaigh C., Eckman S., Smith S. (2009). Statistical design and estimation for the national social life, health, and aging project. Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 64(Suppl_1), i12–i19. 10.1093/geronb/gbp045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Muircheartaigh C., English N., Pedlow S., Kwok P. K. (2014). Sample design, sample augmentation, and estimation for Wave 2 of the NSHAP. Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 69(Suppl_2), S15–S26. 10.1093/geronb/gbu053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oppel R. A., Gebeloff R., Lai K. R., Wright W., Smith M. (2020). The fullest look yet at the racial inequity of coronavirus. New York Times. https://www.nytimes.com/interactive/2020/07/05/us/coronavirus-latinos-african-americans-cdc-data.html. [Google Scholar]
- Rho H. J., Brown H., Fremstad S. (2020). A basic demographic profile of workers in frontline industries. https://mronline.org/wp-content/uploads/2020/06/2020-04-Frontline-Workers.pdf. [Google Scholar]
- Sáenz R., Garcia M. A. (2021). The disproportionate impact of COVID-19 on older Latino mortality: The rapidly diminishing Latino paradox. The Journals of Gerontology: Series B, 76(3), Article e81–e87. 10.1093/geronb/gbaa158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith J. A., McPherson M., Smith-Lovin L. (2014). Social distance in the United States: Sex, race, religion, age, and education homophily among confidants, 1985 to 2004. American Sociological Review, 79(3), 432–456. 10.1177/0003122414531776. [DOI] [Google Scholar]
- U.S. Census Bureau . (2020). America’s families and living arrangements: 2020 – table AVG1. https://www.census.gov/data/tables/2020/demo/families/cps-2020.html. [Google Scholar]
- Venkatesh S. A. (2006). Off the books: The underground economy of the urban poor. Harvard University Press. [Google Scholar]
- Waite L. J., Cagney K. A., Cornwell B., Dale W., Hawkley L., Huang E., Lauderdale D., Laumann E., McClintock M., O'Muircheartaigh C., Schumm L. P. (2020). National social life, health, and aging project (NSHAP). NORC at the University of Chicago. https://www.norc.org/Research/Projects/Pages/national-social-life-health-and-aging-project.aspx. [Google Scholar]