Abstract
Objectives:
Promoting respectful maternity care is a fundamental strategy for enhancing facility birth, which significantly reduces maternal and newborn mortality and morbidity. Despite these effects, disrespect and abusive childbirth care remain a challenge in Ethiopia. Therefore, this study aimed to determine the prevalence of respectful maternity care and its associated factors among laboring women in public hospitals of Benishangul Gumuz region, Ethiopia.
Methods:
A facility-based cross-sectional study design was employed, and trained external assessors observed the care provided to 404 laboring women in public hospitals using structured observation checklists. A focus group discussion and two key informant interviews were also conducted. A structured pre-tested questionnaire and a semi-structured guide were used to generate quantitative and qualitative data, respectively. Seven verification criteria were employed, and the mean value and above for each criterion were used to measure respectful maternity care.
Results:
Of the 404 client–provider interaction observations during childbirth, only 12.6% (n = 51) participants received respectful maternity care. Being from an urban area (adjusted odds ratio = 3.34, 95% confidence interval: 1.39, 8.08), giving childbirth at daytime (adjusted odds ratio = 2.59, 95% confidence interval: 1.26, 5.33), receiving the service from compassionate and respectful care trained provider (adjusted odds ratio = 4.54, 95% confidence interval: 1.63, 12.66), giving childbirth at general hospital (adjusted odds ratio = 3.03, 95% confidence interval: 1.39, 6.65) were positively associated with respectful maternity care. Staff workload, shortage of supply and equipment, partiality in providing timely care, yelling and insulting at clients and birth companions were also barriers to respectful maternity care.
Conclusion:
The observed respectful maternity care practices were low in the study area. Therefore, the findings of this study suggest that addressing respectful maternity care would require increased compassionate and respectful care trained providers, and sustained efforts to improve access to basic equipment and supply for maternity care with an emphasis on primary hospitals. Tailored interventions aimed at improving respectful maternity care should also target rural residents and nighttime parturients.
Keywords: Respectful care, maternity care, compassionate care, Benishangul Gumuz, Ethiopia
Introduction
Sub-Saharan African (SSA) countries have a disproportionate burden of maternal and neonatal mortality and morbidity, accounting for two-thirds (196,000) of maternal deaths. 1 The region has the highest rate (27/1000 live births) of neonatal mortality (NM) worldwide, 2 and the vulnerability to neonatal death is estimated to be 10 times higher than that in developed countries. 3
Ethiopia is 1 of the 10 countries globally that together contribute to almost 60% of all maternal deaths. 4 Despite Ethiopia’s remarkable progress in reducing infant and under-5 mortality, maternal and NM reduction is relatively low. Currently, the NM rate is 30 deaths per 1000 live births, which is higher than that in SSA (27/1000 live births). 5 The maternal mortality rate (MMR), 412 per 100,000 live births, is discriminately the highest in the world. 6
Although Sustainable Development Goals (SDGs) reaffirm to reduce the maternal mortality ratio to less than 70 per 100,000 live births, and stillbirth rate and NM rate to below 12 per 1000 live birth by 2030, 7 Ethiopia has the highest mortality in the world for all three indicators and still far off from reaching any of the three targets. 8 Lack of skilled assistance during pregnancy and childbirth significantly contributes to maternal mortality and morbidity in low- and middle-income countries (LMICs), and the burden is more pronounced in Ethiopia, where more than 50% of all births are not assisted by skilled providers.9,10 In an attempt to address the SDG targets, the Ethiopian Ministry of Health devised and implemented respectful maternity care (RMC) as one of the critical intervention approaches 11 to scale up the level of deliveries attended by skilled birth attendants. 12
RMC is a quality of care that women receive during the continuum of maternal care. 13 White ribbon alliance defines RMC as the human and dignified treatment of a childbearing woman throughout her pregnancy, birth, and the period following childbirth.14,15 It refers to care organized for and provided to all women in a manner that maintains their dignity, privacy, and confidentiality 16 and ensures women’s fundamental right to make informed choices during labor and delivery. 17
Disrespectful and abusive (D&A) treatment during childbirth remains a major barrier to institutional birth. It deters women from using health care facilities for the subsequent continuum of maternity care, thus deteriorating maternal and neonatal health outcomes in low-resource settings.18–21 Evidence from SSA countries has reported that around 44% of women had faced D&A during childbirth. 22 In Ethiopia, there were abundant reports of D&A treatment during labor in health facilities ranging from 67% to 98%.23–25
Several studies in Ethiopia indicated the practice of self-reported RMC during childbirth in a health facility.23–27 However, the findings from these studies inappropriately reported the proportion of RMC due to women not remembering all incidents of D&A (i.e. presence of recall bias), and women would not feel comfortable in reporting a negative experience while still at the health facility (i.e. presence of courtesy bias) or during the immediate postpartum period, women can be overwhelmed by feelings of exhaustion and relief. 28 Thus, there is a lack of empirical evidence on the actual burden of the problem, except for reports on RMC from the client’s perspective. Hence, this direct observational study offers evidence for developing intervention measures to increase RMC that subsequently encourage facility births. Therefore, this study aimed to determine the prevalence of RMC and its associated factors in the Benishangul Gumuz region, Ethiopia.
Methods and materials
Study setting, design, and period
A facility-based mixed cross-sectional study comprising a quantitative component followed by a qualitative component was conducted from 1 April to 20 May 2019 in Benishangul Gumuz region, Ethiopia. The region is located 634 km from Addis Ababa, Ethiopia’s capital city. Its population is estimated to be 1,127,001, assuming 572,815 men and 554,186 women in 2019. 10 There were 402 health posts, 46 health centers, 3 primary hospitals, 2 general hospitals, 1 regional laboratory center, and 2 blood banks in the region. Annually, an estimated 10,000 women give births to the region. Of these, approximately 6000 deliveries are in public hospitals.10,29
Source population and study population
Pregnant women who came for labor and delivery services in public hospitals in the Benishangul Gumuz region were used as the source population. Laboring women and their respective birth attendants throughout the data collection period were used as the study population. The unit of analysis was an observation that represented a unique woman, but not a unique provider since providers usually cared for multiple women during the observation period.
Inclusion criteria: All client–provider interactions during childbirth in public hospitals of the Benishangul Gumuz region.
Exclusion criteria: Women who visited the hospital after the second stage of labor, were fundamentally sick, and attended by undergraduate students were excluded from the study.
Moreover, postpartum mothers and senior maternal and neonatal health care (MNHC) providers were used as study participants for qualitative phase data inquiries.
Sample size and sampling procedure
The sample size was determined using the single population proportion formula (n = (Zα/2)2pq/d2) by considering the proportion of RMC in Bahir Dar, Ethiopia 57%, 30 95% confidence interval (CI), 5% marginal error, and adding 5% of non-response rate; the final sample size was determined to be 415. All public hospitals (five hospitals) in the region were included in this study, as each of these hospitals provides essential obstetrics and neonatal care. Based on a previous delivery report, the sample was allocated proportionally to each hospital. A systematic random sampling technique was employed to recruit study participants according to their admission order. A total of 51 obstetric care providers who were on duty during the data collection period were observed while attending the labor delivery process. On average, one obstetric care provider was observed while attending 7–10 unique laboring women. Purposive sampling was used to recruit postpartum women and senior health care providers for focus group discussion (FGD) and key informant interview (KII), respectively.
Data collection procedures
A structured and pre-tested interview administered questionnaire which was sorted from previous literature was used to generate quantitative data.23,30,31 For observation of labor and delivery, we used a validated tool adopted and accustomed from the Federal Ministry of Health guidelines and previous studies that were conducted on RMC.11,23,32
For direct observation of deliveries, the medical directors in charge of the selected health facilities were informed about the purpose of the study, and women were informed about the observers’ purpose in observing delivery care. Observations were made after obtaining written consent from survey participants and health care providers. Observational checklists were used to assess provider–client interactions during labor and delivery services. In total, 15 trained external assessors (two midwives and one health officer per facility) who were not working at the selected health facilities were recruited for data collection, and each assessor covered an 8-h shift per day. Assessors observed MNHC providers attending labor and delivery services day and night. The assessors did not intervene in the care provided to the women. In an event where the safety or life of the mother or newborn was in danger or when the client’s status was deteriorating, the assessors were trained to alert a senior clinician to intervene. The observation of women started in the second stage of labor and continued for 2 h post-delivery. The characteristics of health care providers providing delivery care to women were also recorded during the survey.
Qualitative data were collected after quantitative data assessment using a semi-structured probing guide questionnaire prepared in English and translated into the local language. Two authors (A.A. and B.A.) who were university lecturers with master’s degrees conducted the FGD and the KIIs. Qualitative data collection was performed using face-to-face interviews with the participants. The FGD was tape-recorded, and notes were taken. The FGD lasted approximately 1:20 h, and each session of KII lasted between 20 and 40 min. Daily, the discussions were analyzed to frame the themes set from the objectives. Data generation, transcription, and analysis were carried out by experts with prior experience in handling qualitative data.
Data quality control
To ensure data quality, each data collector went through a 3-day training workshop on the objectives of the study and data collection techniques. Each day, supervisors checked the completeness of the observational data. A pre-test was performed outside of the study area on 5% of the sample size to check the consistency of the tool. Subsequently, correction and modification of the instrument were undertaken accordingly.
Efforts were made to minimize the effect of observation on provider behavior, that is, the Hawthorne effect, by assuring providers that data collection was anonymous and that individual performance would not be reported to their supervisors or shared publicly (published reports only refer to aggregate data). Moreover, obstetric care providers were not aware of the topics and items on the checklists, so they could not prepare in any way.
Operational definitions
RMC: The level of RMC services was measured using seven performance standards (categories of disrespect and abuse) and their respective verification criteria developed by the Maternal and Child Health Integrated Program (MCHIP) as part of their RMC tool kit, 14 which includes (1) free of physical harm or ill-treatment, (2) woman’s right to information and informed consent, (3) women’s right to confidentiality and privacy, (4) women’s dignity or respect, (5) woman’s right to receive equitable care, (6) women’s right to never be left without care, and (7) women’s right to never be detained or confined against their will. A total of 28 verification criteria from the disrespect and abuse assessment checklist were used in the survey.
RMC—A score equal to or greater than the mean value of each of the seven criteria.11,23
Non-RMC—A score below the mean value for any of the seven criteria.11,23
Statistical analysis
After checking completeness, data were entered using Epi Data version 3.1 and then exported to SPSS version 20 for analysis. Descriptive summary measures, such as frequency, percentages, means, and standard deviation, were used to describe the characteristics of the participants. Bivariate analysis was used primarily to determine which variables were associated with the dependent variable. To control for possible confounding factors, variables with a p value of ⩽0.25 in the bivariate analysis were used in the multivariable analysis. Multicollinearity and model fitness were checked using standard error and Hosmer–Lemeshow tests, respectively. The adjusted odds ratio (AOR), with a 95% CI, was used to identify the independent variables associated with RMC. Statistical significance was declared at a p value of ⩽0.05. A thematic analysis was conducted for the qualitative study, and the findings were further used to improve the quantitative phase questionnaires.
Results
Sociodemographic characteristics of the mothers
A total of 404 mothers participated in the study, making a response of 97.3%. The mean (± SD) age of study participants was 26.2 ± 4.8 years, and more than half (55.2%) of the participants were within the age category of 25–34 years. More than one-third of the participants had no formal education. However, 58% of mothers were from the urban areas, and most (95%) of the study participants were married (Table 1).
Table 1.
Sociodemographic characteristics of mother attended for delivery service in public hospitals Benishangul Gumuz region, Ethiopia, 2019 (n = 404).
| Variables | Variable category | Frequency (N) | % |
|---|---|---|---|
| Residence | Urban | 236 | 58.4 |
| Rural | 168 | 41.6 | |
| Age (years) | <25 | 159 | 39.3 |
| 25–34 | 223 | 55.2 | |
| ⩾35 | 22 | 5.5 | |
| Educational status | Have no formal education | 159 | 39.4 |
| Primary school | 81 | 20.0 | |
| Secondary school | 64 | 15.8 | |
| College and above | 100 | 24.8 | |
| Ethnicity | Berta | 94 | 23.3 |
| Amhara | 128 | 31.7 | |
| Gumuz | 40 | 9.9 | |
| Oromo | 55 | 13.6 | |
| Shinasha | 42 | 10.4 | |
| Agew | 29 | 7.1 | |
| Other a | 16 | 4.0 | |
| Religion | Orthodox | 200 | 49.5 |
| Muslim | 152 | 37.6 | |
| Protestant | 46 | 11.4 | |
| Other b | 6 | 1.5 | |
| Marital status | Married | 384 | 95.0 |
| Not married | 20 | 5.0 | |
| Occupation | House wife | 182 | 45.0 |
| Government employee | 124 | 30.7 | |
| Merchant | 79 | 19.5 | |
| Other c | 19 | 4.7 |
Kambata, Wolayita, Gurage, Tigre.
Catholic and Wakefeta.
Daily laborer, student.
Obstetric and maternal health service history and characteristics of MNHC provider
Of the observed 404 deliveries, 334 were in general hospitals and 70 were in primary hospitals. Nearly two-thirds (63.4%) of the participants were multiparous, and most (89.6%) had a history of antenatal care (ANC) follow-up with the current pregnancy. Regarding the frequency of ANC visits, nearly half (47.3%) of the participants had four and above ANC visits. As depicted in Table 2, almost two-thirds of parturients were admitted in the daytime, and more than half of them gave birth at night. Most (86.6%) women did not experience complications during labor and delivery. The observed deliveries were managed by 51 MNHC providers in five public hospitals. On average, 7 to 10 women were observed per provider while attending deliveries. Female MNHC providers attended more than two-thirds of the observed deliveries. The majority of the observed deliveries were managed by midwives (67.6% or n = 273) (Table 2).
Table 2.
Obstetric and maternal health service history and characteristics of MNHC provider in public hospitals Benishangul Gumuz, Ethiopia, 2019 (n = 404).
| Variables | Categories | Frequency (N) | % |
|---|---|---|---|
| Maternal ANC follow-up | Yes | 362 | 89.6 |
| No | 42 | 10.4 | |
| No. of ANC follow-up | <4 | 213 | 52.7 |
| ⩾4 | 191 | 47.3 | |
| No. of parities | Primipara | 147 | 36.4 |
| Multiparas | 257 | 63.6 | |
| Time of admission | Day | 250 | 61.9 |
| Night | 154 | 38.1 | |
| Complication during labor and delivery | Yes | 54 | 13.4 |
| No | 350 | 86.6 | |
| Time of delivery | Day | 194 | 48.0 |
| Night | 210 | 52.0 | |
| Childbirths by hospital level | Primary | 70 | 17.3 |
| General | 334 | 82.7 | |
| Sex of the care providers who assisted the observed deliveries | Male | 17 | 33.4 |
| Female | 34 | 66.6 | |
| No. of observed childbirths based on the sex of birth attendant | Male | 131 | 32.4 |
| Female | 273 | 67.6 | |
| No. of observed childbirths based on the profession of birth attendants | Midwife | 324 | 80.2 |
| Emergency surgery | 62 | 15.3 | |
| Other a | 18 | 4.5 | |
| No. of observed childbirths based on the monthly salary of birth attendants (ETB) | <5000 | 270 | 66.8 |
| ⩾5000 | 134 | 33.2 | |
| Observed childbirths based on status of CRC-training | Yes | 270 | 66.8 |
| No | 134 | 33.2 |
ANC: antenatal care; MNHC: maternal and neonatal health care; ETB: Ethiopian Birr; CRC: compassionate and respectful care.
Nurse, medical doctor, health officer.
The observed practice of disrespect and abusive treatment of women during childbirth
As indicated in Table 3, the observations documented a high incidence of disrespectful and abusive behaviors. For instance, from the four verification criteria used to identify whether a mother was protected from physical harm or ill-treatment during childbirth, 67.1% (n = 271) of the participants were observed to experience at least one form of abusive care, either shouting at women, scolding, or slapping. Similarly, the majority, 84.2% (n = 340), of the women did not receive comfort or pain relief measures as necessary.
Table 3.
Observed practice of RMC on each verification criteria in public hospitals of Benishangul Gumuz, Ethiopia, 2019 (n = 404).
| Components of RMC | Verification criteria | Yes n (%) |
No n (%) |
|---|---|---|---|
| The woman is protected from physical harm or ill-treatment. | The woman is not slapped, ping or hit by the provider | 133 (32.9) | 271 (67.1) |
| Her baby is not separated from her unless medically necessary | 377 (93.3) | 27 (6.7) | |
| Encourage the woman to take food/fluid during labor unless medically necessitated | 352 (87.1) | 52 (12.9) | |
| Provider gives comfort/pain relief as necessary | 64 (15.8) | 340 (84.2) | |
| The woman’s right to information, informed consent, and choice/preferences is protected. |
Provider introduces self to a woman during the first contact | 42 (10.4) | 362 (89.6) |
| Encourages companion to remain with a woman whenever possible | 291 (72.0) | 113 (28.0) | |
| Encourages the woman to ask questions related to care | 251 (62.1) | 153 (37.9) | |
| Responds to questions with respect and truthfulness | 310 (76.7) | 94 (23.3) | |
| Explains what is being done and what to expect throughout labor | 224 (55.4) | 180 (44.6) | |
| Gives information regarding newborn vaccination to the mother | 72 (17.8) | 332 (82.2) | |
| Gives periodic updates on status and progress of labor | 283 (70.0) | 121 (30.0) | |
| Advice a woman to move around during the first stage | 321 (79.5) | 83 (20.5) | |
| Ask information or verbal consent before performing interventions | 71 (17.5) | 333 (82.5) | |
| Woman’s right to confidentiality and privacy | Woman’s files are stored in locked cabinets | 33 (8.2) | 371 (91.8) |
| Uses curtains or other visual barrier during procedures | 213 (52.7) | 191 (47.3) | |
| Uses drapes or covering appropriate to protect woman’s privacy | 161 (39.9) | 243 (60.1) | |
| The woman is treated with dignity and respect. | Speaks politely to a woman and her companion | 342 (84.7) | 62 (15.3) |
| Never makes insults, intimidation, threats, or coerces woman | 369 (91.3) | 35 (8.7) | |
| Shows the place of toilet and disposal system for women/ companion | 88 (21.8) | 316 (78.2) | |
| Allows women or birth campanion to do cultural practices/belief which is not harmfull to the mother or baby | 354 (87.6) | 50 (12.4) | |
| Women get adequate bed | 34 (8.4) | 370 (91.6) | |
| The woman receives equitable care, free of discrimination. | Speaks to the woman at a language-level that she understands | 370 (91.6) | 34 (8.4) |
| Equal treatment and respect without varying on any specific attributes | 367 (90.8) | 37 (9.2) | |
| Not show verbal or physical disrespect to women based on attribute | 356 (88.1) | 48 (11.9) | |
| Wear a gown when he or she gives care | 288 (71.3) | 116 (28.7) | |
| The woman receives equitable care, free of discrimination. | Encourages the woman to call if needed. | 316 (78.2) | 88 (21.8) |
| Comes quickly when woman calls (within 1 min) | 240 (59.4) | 164 (40.6) | |
| Never leaves a woman alone or unattended | 178 (44.1) | 226 (55.9) | |
| Woman is never detained or confined against her will. | The facility does not have the policy to detain women who do not pay | 404 (100) | — |
RMC: respectful maternity care.
Regarding the categories of disrespect and abuse (the woman’s right to information, informed consent, and choice/preferences are protected) that used nine verification criteria, most, 89.6% (n = 362), of the service providers did not introduce themselves to clients. In addition, information or verbal consent was not provided in 82.5% (n = 333) of cases. Service providers have not done curtains or other visual barriers during procedures for more than 47% of the respondents, and over 60% of participants were not draped or covered appropriately to protect their privacy.
Concerning a woman is being treated with dignity and respect; most (91.6%) of the participants did not get an adequate bed (required to share a bed in the postnatal ward or observed women were put in beds in the postnatal ward that was not clean) (Table 3).
Prevalence of RMC
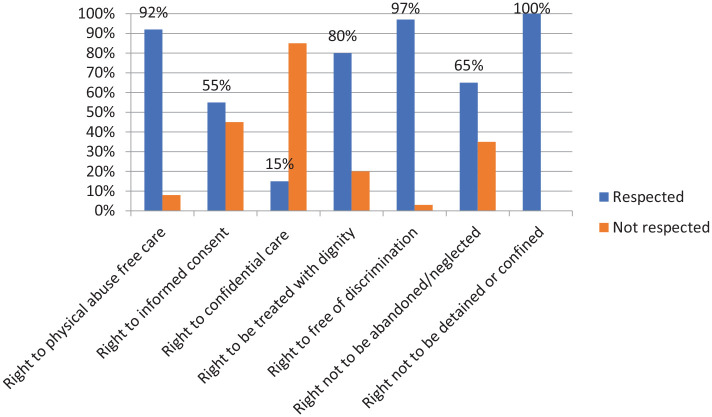
Of the 404 observations of client–provider interactions during labor and delivery, only 12.6% (95% CI: 9.6, 16.4) of the participants received RMC services. Of the seven categories of women’s rights during childbirth, the right to not be detained or confined for not paying hospital costs was totally (100%) respected. Almost all (97%) of the women had received the right to free of discrimination care. However, the majority (85%) of the observed laboring women did not receive the right to confidential care (Figure 1).
Figure 1.
The seven women’s rights of women during labor and delivery in public hospitals of Benishangul Gumuz region, Ethiopia, 2019 (n = 404).
Factors associated with RMC
After controlling for confounding factors using multivariable analysis, variables, such as being urban residents, giving daytime childbirth, receiving services from CRC-trained MNHC providers, and giving birth at general hospitals were significantly associated with RMC.
Women from urban areas were three times more likely to receive RMC during labor and delivery than those from rural areas (AOR = 3.34 (95% CI: 1.19, 8.08)). The current study indicated that the odds of receiving RMC were 2.59 times higher among women who gave birth in the daytime compared to those who gave birth in the nighttime (AOR = 2.59 (95% CI: 1.26, 5.33)). Women who received labor delivery services by CRC-trained MNHC providers were 4.5 times more likely to receive RMC than their counterparts (AOR = 4.54 (95% CI: 1.63, 12.67)). The likelihood of getting RMC was three times more common among women who gave childbirth at general hospital hospitals compared to women who gave birth at primary hospitals (AOR = 3.00 (95% CI: 1.39,6.65)) (Table 4).
Table 4.
Bivariate and multivariable logistic regression result for factors associated with RMC in public hospitals of Benishangul Gumuz region, Ethiopia, 2019 (n = 404).
| Variables | Categories | Respectful care | COR (95% CI) | AOR (95% CI) |
p | |
|---|---|---|---|---|---|---|
| Yes | No | |||||
| Residence | Urban | 38 | 198 | 2.29 (1.18, 4.45) | 3.34 (1.39, 8.08) * | 0.007 |
| Rural | 13 | 155 | 1 | 1 | ||
| Occupation of the mother | Housewife | 16 | 166 | 1 | 1 | |
| Government employee | 22 | 102 | 2.24 (1.12, 4.46) | 1.62 (0.70, 3.74) | 0.259 | |
| Other a | 13 | 85 | 1.59 (0.73, 3.45) | 1.42 (0.59, 3.44) | 0.438 | |
| ANC visit | Yes | 198 | 164 | 1.9 (1.78, 9.15) | 1.4 (0.58, 3.70) | 0.454 |
| No | 18 | 24 | 1 | |||
| Time of delivery | Day | 36 | 158 | 2.96 (1.57, 5.60) | 2.59 (1.26, 5.33) * | 0.012 |
| Night | 15 | 195 | 1 | 1 | ||
| Complication during labor and delivery | Yes | 14 | 40 | 2.96 (1.47, 5.95) | 2.18 (0.88, 5.28) | 0.086 |
| No | 37 | 313 | 1 | 1 | ||
| Level of hospital | General | 18 | 52 | 3.16 (1.66, 6.02) | 3.00 (1.39, 6.65) * | 0.005 |
| Primary | 33 | 301 | 1 | 1 | ||
| Sex of the provider attended delivery | Male | 8 | 123 | 1 | 1 | |
| Female | 43 | 230 | 2.87 (1.31, 6.31) | 1.59 (0.64, 3.9) | 0.312 | |
| No. of observed childbirths based on the profession of the care provider | Midwife | 131 | 203 | 2.56 (1.36, 4.84) | 1.1 (0.41, 2.95) | 0.843 |
| Emergency surgery | 39 | 23 | 2.78 (1.97, 5.95) | 3.45 (0.76, 3.25) | 0.672 | |
| Others b | 18 | 62 | 1 | 1 | ||
| CRC-trained | Yes | 46 | 224 | 5.30 (2.05, 13.67) | 4.54 (1.63, 12.66) * | 0.004 |
| No | 5 | 129 | 1 | 1 | ||
| No. of observed childbirth based on care provider salary (ETB) | <5000 | 23 | 247 | 1 | 1 | |
| ⩾5000 | 28 | 106 | 2.84 (1.56, 5.15) | 1.59 (0.68,3.7) | 0.284 | |
COR: crude odds ratio; CI: confidence interval; AOR: adjusted odds ratio; ETB: Ethiopian Birr; CRC: compassionate and respectful care; ANC: antenatal care.
Merchant, student, daily laborer.
Nurse, medical doctor, health officer.
Statistically significant at p ⩽ 0.05.
Barriers to RMC
Almost all FGD participants and key informants reported that lack of basic equipment and supply for maternity care, inadequate maternity waiting rooms, and shortage of MNHC providers were the impeding factors for the provision of RMC. The FGD participants also expressed that the absence of impartiality in getting timely care to all clients, non-dignified care and shouting to parturients, and insulting of birth companions were widely practiced forms of mistreatment in the hospital.
Facility-related factors
Most of the participants in the qualitative interview viewed the importance of RMC for enhancing facility birth. However, lack of basic infrastructure for maternity care services was the determinate cause for the mistreatments of women during childbirth. The discussants and key informants explained that the shortage of hospital supplies and equipment, such as bed and bedsheets, blankets, water, and shower room, was the barrier to the delivery of RMC. The participants also extend that the absence of personal protective equipment, an inadequate number of coaches, and insufficient maternal waiting room for the clients remains the challenge for RMC.
There is a shortage of beds. No waiting room for the patient as well as for the birth companion, we just roam around the facility. And, even after my childbirth, I couldn’t get a bed to rest. (FGD, 28 years)
The key informant from the providers’ perspective described that mistreatment of the women during childbirth was strongly associated with workload and tiredness which is caused by very high patient loads coupled with inadequate staff number. Dealing with numerous birth companions alongside one parturient also exacerbates the tiredness of the care providers.
A 45-year-old senior obstetric care provider said that “numbers of care providers are not enough to attend all laboring women appropriately, especially during the night time, the assigned MNHC providers do not surpass four, while there are more than ten cases at a time. Hence, this would deter women-centered care.”
Service-related factors
The key informants from two hospitals stated that with all the available resources, the MNHC providers strive to offer dignified, timely, and non-discriminatory care to all laboring women.
I provided equal care for all mothers irrespective of their status and background because it is my responsibility to respect the fundamental right of the women and unborn child. (MNHCP, 32 years)
However, to a large extent, FGD participants described that the providers did not offer equal and timely care to all clients that result in long periods of either waiting or being left alone without care. A rushed care from the providers and unsanitary rooms also discouraged women from seeking facility birth.
. . .The MNHC providers didn’t assess and evaluate me on time. But after my birth companion called his friend Dr. X. who was working in this hospital, they immediately started to assess and evaluate me properly as indicated. I think in this hospital, no one can get appropriate and timely care unless you have friends/relatives from MNHC providers. Generally, the service was biased. (FGD, mother 34 years)
They also expressed that the care providers did not have respect for clients, and insulting and yelling at clients and birth companions were common. Some of the health care providers were not competent enough in diagnosing and providing appropriate maternity care.
. . .Health professionals have no value and respect for clients and birth companions. Currently, employed health professionals are purchasing their certificate or degree from a private college and are then hired in the health facility through relatives. (Mother, 31 years)
Discussion
Despite concerted national efforts to reduce the mortality of women during childbirth, maternal mortality continues to be a significant cause of death among women in Ethiopia. 6 One of the important components to decrease maternal mortality is to improve the quality of care received by women during delivery. 12 Promoting RMC during childbirth is one of the pillars to ensure quality maternity care through establishing women-centered care. However, D&A during childbirth remains a major concern in the public health system of Ethiopia, and these broad spectrum forms of D&A are inappropriately reported and normalized by a large segment of the population that needs stringent measures. Hence, this direct observation study aimed to determine the practice of RMC and its associated factors in the Benishangul Gumuz region, Ethiopia.
In this study, merely 12.6% (95% CI: 9.6, 16.4) of the participants were observed to receive RMC. This finding is notably lower than studies reported from SSA (56.0%), India (71%), 33 Tanzania (85%), 34 Kenya (81%), 35 and Ethiopia (57%).27,30 This lower observed practice of RMC in our study was due to the method of assessment that we employed to determine RMC, while the previous studies used a self-reported investigation for RMC which could have overestimated the presence of RMC. Higher findings of RMC in a self-report assessment are expected as women are potentially hesitant to report abuse conducted within the facility while still in care.34,36
Contrary to the above justifications, an observational assessment study conducted in Tanzania and India demonstrated a higher prevalence of RMC, that is, 30% and 77.6%, respectively37,38 compared to our study finding. These differences may be attributed to not only to a variation in sociodemographic backgrounds and study period but also maternal and child health service utilization and access to quality maternal and newborn health services. 39 It is noted that D&A is inflicted not only by individual providers but also by health systems as a whole when the conditions in facilities deviate greatly from accepted standards of care and infrastructure, staff, equipment, and supplies needed to deliver that care. 40
However, the result of this study is higher than a study conducted in Arba Minch town, Ethiopia (1.1%), Pakistan (3%), and Nigeria (2%).41–43 The possible discrepancy could be due to the differences in study settings and variations in sociodemographic backgrounds or the practice of some obsolete procedures. For instance, in the study conducted in Arba Minch town, birth attendants apply fundal pressure to expel babies, which can put women at health risk, and suturing of episiotomies without the use of local anesthesia is considered as physical abuse that significantly drops women’s status of RMC.
From the category of confidentiality and privacy care, around 60% of the parturient were observed to experience examination procedures without the use of drapes or were not covered appropriately to protect their privacy which is similar to the report of the study conducted in selected health centers of Amhara and the southern region, Ethiopia. 44 Although asking women for consent is an important measure of showing respect for the laboring mother, the majority (82%) of women were observed to experienced non-consented care in this study, which is consistent with the previous study reported from Addis Ababa, Ethiopia (94.8%). 31
In this study, the use of physical force/abrasive behavior with the woman was pervasive as more than two-thirds (67%) of the participants experienced physical abuses, including scolding, shouting, or even slapping. This is one of the first systematic measures of abusive practices in health facilities and indicates a worrisome picture of the quality of maternity care in Ethiopia.17,40 Hence proactive measures have to be implemented by stakeholders to solve the maternity care crisis in the health facilities of the region.
From the category of women’s right to be treated with dignity and respect, most (92%) of the participants did not get a suitable bed, as such majority of the observed women were required to share a bed in the postnatal ward, a place that was likely to compromise their privacy, confidentiality, and dignity. Furthermore, women were put in beds in the postnatal ward that was not clean or even, has no bedsheets. The findings of this form of mistreatment in our study bear similarity with a study reported from Tanzania where more than 84% of women have been observed to part a bed in the postnatal ward or instructed to rest on bedsheets that were not clean. 34
The current study illustrated that women who gave childbirth in the daytime were three times more likely to get respectful care than women who gave birth at night. Consistent with our finding, a study conducted in Ethiopia and Kenya also showed that delivering at daytime was associated with a higher practice of RMC.24,35 The higher burden of non-reverential care during the night shift is possibly explained by the unavailability of adequate staff to offer nighttime maternity care services. As a result, obstetric care providers become tired because of workload or a sleeping disturbance that may engender physical or verbal abuse to parturient.
It is widely recognized that compassionate and respectful care training is crucial to capacitate MNHC providers to offer human-centered care, serve patients ethically with respect, remember to adhere to a professional oath, and encourage providers to deliver acceptable service quality to the clients.45,46 Similarly, the current study indicated that receiving labor delivery care from CRC-trained providers increases the odds of getting RMC by fourfolds. A similar association was also noted in the previous studies.37,47
In congruence with a previous study, 30 the current study reveals that women who were residents of urban areas were three times more likely to be valued and respected during labor and delivery than mothers who were residents of rural areas. The possible explanation for this association may be that participants from urban areas are cognizant of their basic rights, and the providers are vigilant and cautious to realize some of the fundamental rights of the women.
In Ethiopia, primary hospitals are structured under a primary health care unit that provides all services offered by health centers and emergency surgical services, such as cesarean sections and blood transfusions. However, primary hospitals cannot provide all services that are offered under the second-tier system, that is, general hospitals. This is because general hospitals are capacitated with infrastructure and skilled human resources better than primary hospitals. 48 Hence, having appropriate supply and infrastructure reinforced with adequately experienced health care providers would facilitate a reverential and cordial service to laboring women. Likewise, our study revealed that the likelihood of getting RMC service was observed to be high among women who gave birth at the general hospital than those who gave birth at a primary hospital.
Strength and limitation of the study
The use of direct observation of client–provider interactions during labor and delivery in this study has the following strength. First, it avoids recall bias as clients may not exactly remember the broad spectrum of D&A. Second, it avoids the inherent interpersonal perception of the clients about D&A. Third, the study would significantly avoid courtesy biases. Finally, this study’s triangulation of quantitative with the qualitative inquiry is also important to capture robust data in determining factors affecting RMC services. Despite these strengths, the study was unable to conduct a pilot study to minimize the presence of possible Hawthorne effect, and the study also did not consider data saturation for the qualitative inquiry of the study participants.
Conclusion
Merely 12.6% of participants were observed to receive RMC during labor and delivery in this study. Being an urban resident, giving birth in the daytime, receiving care from CRC-trained MNHC providers, and receiving service from the general hospital were positively associated with RMC. Staff workload, unavailability of adequate infrastructures, shortage of supply and equipment partiality in providing timely care, and misunderstanding with MNHC providers and birth companions were the barriers to RMC. Therefore, health institutions and other stakeholders should increase the number of compassionate and respectful care trained providers and reinforce monitoring and evaluation mechanisms for MNHC providers to avoid mistreatment and support them in offering women-friendly care. Furthermore, the provision of basic equipment and supplies to the health facilities should be given due attention.
Acknowledgments
The authors thank Bahir Dar University College of Medicine and Health Sciences for letting to conduct this study. They also thank MNHC providers working in public hospitals of the Benishangul Gumuz region, data collectors, supervisors, and study participants for their invaluable support to make this study real.
Footnotes
Authors’ contributions: All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; gave final approval of the version to be published; and agreed to be accountable for all aspects of the work.
Data availability: Datasets used in the current study are available from the corresponding author on reasonable request.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical considerations: Ethical clearance was obtained from the ethical review committee of the institute of public health, college of medicine and health sciences, Bahir Dar University with an approval number of BDU H/R/E/C/D/03/301/2011. Support letters were also obtained from Benishangul Gumuz Region Health Bureau and formal letters were written to all public Hospital Managers, and permission was secured at all levels. The investigators along with data collectors explained the aims of the study to the hospitals’ managers, labor delivery team leaders, and health care providers in labor/delivery wards. Before data collection consensus was once reached between data collectors and health care providers after explaining the objective and method of the study. Finally, written informed consent was obtained from all the laboring women and the care providers who assisted the birth after clarifying the purpose and procedure of the study. All the procedures of the ethical evaluation of this study were followed the Helsinki Declaration of human research.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Written informed consent was obtained from all the laboring women and the care providers who assisted the birth.
ORCID iDs: Yitagesu Sintayehu  https://orcid.org/0000-0002-4325-4241
https://orcid.org/0000-0002-4325-4241
Alekaw Sema  https://orcid.org/0000-0002-7519-065X
https://orcid.org/0000-0002-7519-065X
Nigus Kassie  https://orcid.org/0000-0002-7947-115X
https://orcid.org/0000-0002-7947-115X
Abel Tibebu  https://orcid.org/0000-0003-0818-4169
https://orcid.org/0000-0003-0818-4169
Getahun Tiruye  https://orcid.org/0000-0002-0441-0440
https://orcid.org/0000-0002-0441-0440
References
- 1. World Health Organization (WHO). Trends in maternal mortality 2000 to 2017: estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. WHO, 2019, https://www.unfpa.org/featured-publication/trends-maternal-mortality-2000-2017#:~:text=The%20global%20maternal%20mortality%20ratio%20in%202017%20is%20estimated%20at,ratio%20was%202.9%20per%20cent. [Google Scholar]
- 2. UNICEF. UNICEF data: monitoring the situation of children and women. UNICEF, New York, 2020. [Google Scholar]
- 3. Hug L, Alexander M, You D, et al. National, regional, and global levels and trends in neonatal mortality between 1990 and 2017, with scenario-based projections to 2030: a systematic analysis. Lancet Glob Health 2019; 7(6): e710–e720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. World Health Organization (WHO). Trends in maternal mortality: 1990 to 2015: estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. WHO, 2015, http://apps.who.int/iris/bitstream/handle/10665/193994/WHO_RHR_15.23_eng.pdf;jsessionid=366A9A220CF9E41A29705A1929E5FBFE?sequence=1 [Google Scholar]
- 5. Requejo J, Bryce J, Victora C, et al. Accountability for maternal, newborn and child survival: the 2013 update. Geneva: World Health Organization and UNICEF, 2013. [Google Scholar]
- 6. Kassebaum NJ, Bertozzi-Villa A, Coggeshall MS, et al. Global, regional, and national levels and causes of maternal mortality during 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014; 384(9947): 980–1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sachs JD. From millennium development goals to sustainable development goals. Lancet 2012; 379(9832): 2206–2211. [DOI] [PubMed] [Google Scholar]
- 8. Boerma T, Requejo J, Victora CG, et al. Countdown to 2030: tracking progress towards universal coverage for reproductive, maternal, newborn, and child health. Lancet 2018; 391(10129):1538–1548. [DOI] [PubMed] [Google Scholar]
- 9. Paxton A, Maine D, Freedman L, et al. The evidence for emergency obstetric care. Int J Gynaecol Obstet 2005; 88(2): 181–193. [DOI] [PubMed] [Google Scholar]
- 10. Central Statistical Authority (CSA) [Ethiopia]. 2016 Ethiopia demographic and health survey, Addis Ababa, Ethiopia and Calverton, Maryland, USA, 2016, https://dhsprogram.com/pubs/pdf/FR328/FR328.pdf
- 11. Federal Ministry of Health (FMOH). Respectful Maternity Care (RMC) and partograph training resource package. FMOH, Addis Ababa, Ethiopia, 2015. [Google Scholar]
- 12. Federal Ministry of Health (FMOH). Health sector transformation plan (2015/16–2019/20). FMOH, Addis Ababa, Ethiopia, 2015. [Google Scholar]
- 13. USAID. Ending preventable maternal mortality: USAID maternal health vision for action, June 2014, https://www.usaid.gov/sites/default/files/documents/1864/MCHVision.pdf
- 14. White Ribbon Alliance. Respectful maternity care: the universal rights of childbearing women. White Ribbon Alliance, Washington, DC, 2012. [Google Scholar]
- 15. Ndwiga C, Warren CE, Abuya T, et al. Promoting respectful maternity care: a training guide for facility—based workshops—facilitator’s guide. New York: Population Council, 2015. [Google Scholar]
- 16. World Health Organization (WHO). WHO recommendation on respectful maternity care during labour and childbirth. Geneva: WHO, 2018. [Google Scholar]
- 17. Bowser D, Hill K. Exploring evidence for disrespect and abuse in facility-based childbirth. Boston, MA: USAID-TRAction Project, Harvard School of Public Health, 2010, p. 3. [Google Scholar]
- 18. Miller S, Lalonde A. The global epidemic of abuse and disrespect during childbirth: History, evidence, interventions, and FIGO’s mother-baby friendly birthing facilities initiative. Int J Gynaecol Obstet 2015; 131(Suppl. 1): S49–S52. [DOI] [PubMed] [Google Scholar]
- 19. Sheferaw ED, Mengesha TZ, Wase SB. Development of a tool to measure women’s perception of respectful maternity care in public health facilities. BMC Pregnancy Childbirth 2016; 16(1): 67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kruk ME, Kujawski S, Mbaruku G, et al. Disrespectful and abusive treatment during facility delivery in Tanzania: a facility and community survey. Health Policy Plan 2018; 33(1): e26–e33. [DOI] [PubMed] [Google Scholar]
- 21. Patabendige M, Agampodi SB, Jayawardane A, et al. Perceptions on respectful maternity care in Sri Lanka: study protocol for a mixed-methods study of patients and providers. PLoS One 2021; 16(5): e0250920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kassa ZY, Tsegaye B, Abeje A. Disrespect and abuse of women during the process of childbirth at health facilities in sub-Saharan Africa: a systematic review and meta-analysis. BMC Int Health Hum Rights 2020; 20: 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Asefa A, Bekele D. Status of respectful and non-abusive care during facility-based childbirth in a hospital and health centers in Addis Ababa, Ethiopia. Reprod Health 2015; 12(1): 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Wassihun B, Deribe L, Worede N, et al. Prevalence of disrespect and abuse of women during child birth and associated factors in Bahir Dar town, Ethiopia. Epidemiol Health 2018; 40: e2018029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ukke GG, Gurara MK, Boynito WG. Disrespect and abuse of women during childbirth in public health facilities in Arba Minch town, South Ethiopia—a cross-sectional study. PLoS One 2019; 14(4): e0205545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Bante A, Teji K, Seyoum B, et al. Respectful maternity care and associated factors among women who delivered at Harar hospitals, eastern Ethiopia: a cross-sectional study. BMC Pregnancy Childbirth 2020; 20(1): 86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Yosef A, Kebede A, Worku N. Respectful maternity care and associated factors among women who attended delivery services in referral hospitals in Northwest Amhara, Ethiopia: a cross-sectional study. J Multidiscip Healthc 2020; 13: 1965–1973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Waldenström U. Why do some women change their opinion about childbirth over time? Birth 2004; 31(2): 102–107. [DOI] [PubMed] [Google Scholar]
- 29. Benshangul Gumuz Regional State. Benshangul Gumuz Regional State Health Bureau planning programming service office, 2019, https://businessguide.ezega.com/Default.aspx?action=BussinessDetail&bid=1328055
- 30. Wassihun B, Zeleke S. Compassionate and respectful maternity care during facility based child birth and women’s intent to use maternity service in Bahir Dar, Ethiopia. BMC Pregnancy Childbirth 2018; 18(1): 294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Sheferaw ED, Bazant E, Gibson H, et al. Respectful maternity care in Ethiopian public health facilities. Reprod Health 2017; 14: 60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Rosen HE, Lynam PF, Carr C, et al. Direct observation of respectful maternity care in five countries: a cross-sectional study of health facilities in East and Southern Africa. BMC Pregnancy Childbirth 2015; 15: 306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Bhattacharya S, Sundari Ravindran T. Silent voices: institutional disrespect and abuse during delivery among women of Varanasi district, northern India. BMC Pregnancy Childbirth 2018; 18(1): 338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Sando D, Ratcliffe H, McDonald K, et al. The prevalence of disrespect and abuse during facility-based childbirth in urban Tanzania. BMC Pregnancy Childbirth 2016; 16(1): 185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Abuya T, Ndwiga C, Ritter J, et al. The effect of a multi-component intervention on disrespect and abuse during childbirth in Kenya. BMC Pregnancy Childbirth 2015; 15(1): 224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Blanc AK, Warren C, McCarthy KJ, et al. Assessing the validity of indicators of the quality of maternal and newborn health care in Kenya. J Glob Health 2016; 6(1): 010405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Dey A, Shakya HB, Chandurkar D, et al. Discordance in self-report and observation data on mistreatment of women by providers during childbirth in Uttar Pradesh, India. Reprod Health 2017; 14: 149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Freedman LP, Kujawski SA, Mbuyita S, et al. Eye of the beholder? Observation versus self-report in the measurement of disrespect and abuse during facility-based childbirth. Reprod Health Matters 2018; 26(53): 107–122. [DOI] [PubMed] [Google Scholar]
- 39. Jena BH, Biks GA, Gelaye KA, et al. Magnitude and trend of perinatal mortality and its relationship with inter-pregnancy interval in Ethiopia: a systematic review and meta-analysis. BMC Pregnancy Childbirth 2020; 20: 432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Freedman LP, Kruk ME. Disrespect and abuse of women in childbirth: challenging the global quality and accountability agendas. Lancet 2014; 384: e42–e44. [DOI] [PubMed] [Google Scholar]
- 41. Gendisha Ukke G, Gurara MK, Godana W. Disrespect and abuse of women during childbirth in public health facilities in Arba Minch town, South Ethiopia—a cross-sectional study. PLoS One 2019; 14: e0205545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Hameed W, Avan BI. Women’s experiences of mistreatment during childbirth: a comparative view of home-and facility-based births in Pakistan. PLoS One 2018; 13(3): e0194601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Okafor II, Ugwu EO, Obi SN. Disrespect and abuse during facility-based childbirth in a low-income country. Int J Gynaecol Obstet 2015; 128(2): 110–113. [DOI] [PubMed] [Google Scholar]
- 44. Banks KP, Karim AM, Ratcliffe HL, et al. Jeopardizing quality at the frontline of healthcare: prevalence and risk factors for disrespect and abuse during facility-based childbirth in Ethiopia. Health Policy Plan 2018; 33: 317–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Chapin HL, Darnall BD, Seppala EM, et al. Pilot study of a compassion meditation intervention in chronic pain. J Compassionate Health Care 2014; 1: 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Shea S, Lionis C. Introducing the journal of compassionate health care. J Compassionate Health Care 2014; 1: 7. [Google Scholar]
- 47. Chaturvedi S, Upadhyay S, De Costa A. Competence of birth attendants at providing emergency obstetric care under India’s JSY conditional cash transfer program for institutional delivery: an assessment using case vignettes in Madhya Pradesh province. BMC Pregnancy Childbirth 2014; 14: 174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. World Health Organization (WHO). Primary health care systems (PRIMASYS): case study from Ethiopia, abridged version. Licence: CC BY-NC-SA 3.0 IGO. Geneva: WHO, 2017. [Google Scholar]