Abstract
This Data in Brief article contains further sensitivity analysis data related to the article “Alcohol consumption and mortality: the Ludwigshafen Risk and Cardiovascular Health (LURIC) study” [1]. Alcohol consumption data of participants in LURIC was collected using a questionnaire. This data was used to calculate the amount of alcohol consumption in g ethanol per day by using standard volumes and standard vol-% in different beverages in Germany. The data shown here provide results from the LURIC study stratified by gender. Furthermore, the LURIC study results were reproduced using other classifications, which were stratified in different literature data. In addition, our analysis provides data of alcohol consumption for smokers and non-smokers in the LURIC study cohort separately.
Keywords: Gender-specific alcohol consumption, Sensitivity analysis, Mortality, Cardiovascular diseases, Diabetes mellitus, Atherosclerosis
Specification Table
| Subject | Medicine |
| Specific subject area | Cardiovascular diseases |
| Type of data | Tables, figures |
| How data were acquired | Alcohol consumption data of 3316 participants of the Ludwigshafen Risk and Cardiovascular Health Study (LURIC) was collected by a standardised questionnaire. This data was used to calculate the amount of alcohol consumption in g ethanol per day by using the standard volumes and alcohol vol% of different beverages in Germany. Association of alcohol consumption with mortality was investigated using Cox proportional hazard regression. |
| Data format | Analyzed |
| Parameters for data collection | For the LURIC study patients were recruited that had been referred for coronary angiography. Study participants filled out a questionnaire and blood samples were collected. |
| Description of data collection | Patients scheduled for coronary angiography at the Ludwigshafen Heart Center were asked to participate in the LURIC study between 1997 and 2000. After obtaining written informed consent, study participants filled out a questionnaire at study entry and blood samples were drawn and stored at -80°C. |
| Data source location | Ludwigshafen Heart Center in South-West Germany |
| Data accessibility | All data is presented in this article. Regarding the raw data the following applies: Due to the articles of Ludwigshafen Risk and Cardiovascular Health (LURIC) Study GmbH, which needs to acknowledge the German Data Protection Act and the consent given by the study participants, data cannot be released to the public domain Interested researchers are invited to address their request or proposal to Kai Grunwald (Kai.Grunwald@weitnauer.net) or to the Principal Investigator of the LURIC Study, Winfried März (winfried.maerz@luric-online.de). Finally, the authors confirm that they accessed these data upon approval by LURIC and that all other researchers can access the data in the same manner the authors did. |
| Related research article | AP. Moissl, GE. Delgado, BK. Krämer, C. Dawczynski, T. Stojakovic, W. März, ME. Kleber, S. Lorkowski, Alcohol consumption and mortality: The Ludwigshafen Risk and Cardiovascular Health (LURIC) study |
Value of the Data
-
•
The question whether moderate alcohol consumption confers benefits regarding cardiovascular risk is still not finally settled and has not been thoroughly investigated in a moderate to high cardiovascular risk cohort.
-
•
Both doctors and patients at cardiovascular risk benefit from a clear statement regarding moderate alcohol consumption. Due to high alcohol consumption, there is an increased overall and cardiovascular mortality risk in a cohort with a moderate to high cardiovascular risk. It is noticeable that very low alcohol consumption does not have any significant health benefits. Data from our study might be used to further investigate the association between alcohol intake and other biomarkers or diseases. We also show that standardisation of alcohol quantities is necessary for further studies on alcohol consumption to be able to compare them on a global perspective.
1. Data Description
Here we present sensitivity analyses of gender and subgroups stratified for distributions of alcohol consumption in the LURIC study. We used (i) the categories which are described in the manuscript “Alcohol consumption and mortality: The Ludwigshafen Risk and Cardiovascular Health (LURIC) study” [1] and (ii) additional categories as well as adjusted analyses of their association with all-cause mortality and cardiovascular mortality that extend the results reported in the manuscript “Alcohol consumption and mortality: The Ludwigshafen Risk and Cardiovascular Health (LURIC) study” [1].
Tables 1 and 2 show anthropometric, biochemical, and liver-specific characteristics for males and females of the five alcohol intake groups used in our main manuscript [1] for the complete cohort.
Table 1.
Only male study participants anthropometric, biochemical and liver-specific characteristics (mean (± SD) or median (25thto 75th percentile) data) according to five different alcohol intake groups in the main manuscript.
| Variable | Groups of total alcohol consumption |
||||||
|---|---|---|---|---|---|---|---|
| Male | No intake 0 g/d ethanol |
Low intake > 0 - 37.5 g/d ethanol |
Medium intake > 37.5 - 50.0 g/d ethanol |
High intake > 50 - 100 g/d ethanol |
Very high intake > 100 g/d ethanol |
Pa | FDR-Pb |
| N | 705 | 1083 | 302 | 184 | 36 | - | - |
| Age (years) | 61 ± 11.2 | 62.4 ± 10.7 | 62 ± 10.1 | 61.2 ± 8.78 | 57.9 ± 10.1 | 0.009 | 0.020 |
| BMI (kg/m2) | 27.6 ± 4.2 | 27.5 ± 3.61 | 27.5 ± 3.37 | 28.1 ± 3.86 | 27.8 ± 3.85 | 0.347 | 0.440 |
| LDL-cholesterol (mg/dl) | 113.0 ± 33.6 | 113.0 ± 31.6 | 113.0 ± 33.6 | 115.0 ± 32.9 | 121.0 ± 33.4 | 0.636 | 0.711 |
| HDL-cholesterol (mg/dl) | 34.6 ± 9.2 | 37.0 ± 9.56 | 39.2 ± 10.1 | 38.6 ± 10.7 | 40.0 ± 11.1 | <0.001 | <0.001 |
| Apolipoprotein A-I (mg/dl) | 119.0 ± 21.1 | 125.0 ± 22.0 | 130.0 ± 23.0 | 130.0 ± 24.9 | 132.0 ± 28.3 | <0.001 | <0.001 |
| Apolipoprotein A-II (mg/dl) | 38.9 ± 8.46 | 41.3 ± 9.31 | 43.2 ± 9.71 | 44.2 ± 10.0 | 43.7 ± 13.9 | <0.001 | <0.001 |
| Triglycerides (mg/dl) | 155 (111-202) | 146 (108-196) | 148 (115-198) | 158 (112-224) | 130 (92.8-202) | 0.046 | 0.072 |
| Fasting glucose (mg/dl) | 102 (93.6-121) | 103 (93.6-118) | 104 (96.8-116) | 105 (97.1-119) | 107 (98.1-116) | 0.446 | 0.529 |
| HbA1c (%) | 6.45 ± 1.36 | 6.17 ± 1.18 | 6.24 ± 1.03 | 6.23 ± 1.11 | 6.24 ± 1.04 | <0.001 | <0.001 |
| Systolic blood pressure (mmHg) | 140.0 ± 24.2 | 142.0 ± 22.9 | 140 ± 22.2 | 141 ± 22.6 | 136 ± 23.7 | 0.239 | 0.325 |
| Diastolic blood pressure (mmHg) | 80.9 ± 11.7 | 82.4 ± 11.6 | 81.1 ± 10.7 | 81.5 ± 10.7 | 78.4 ± 9.16 | 0.026 | 0.049 |
| eGFR (ml/min/1.73 m2) | 82.5 ± 21.8 | 83.8 ± 19.4 | 85.3 ± 18.3 | 85.8 ± 18.4 | 96.2 ± 15.3 | <0.001 | 0.001 |
| hsCRP (mg/L) | 3.6 (1.57-8.85) | 2.83 (1.1-7.59) | 3.22 (1.24-9.07) | 4.88 (1.56-9.27) | 7.39 (2.04-19.1) | <0.001 | <0.001 |
| NT-pro-BNP (pg/mL) | 302 (100-876) | 282 (97-835) | 289 (97-881) | 278 (101-881) | 374 (142-933) | 0.822 | 0.822 |
| Coronary artery disease (%) | 86.8 | 82.7 | 83.1 | 78.8 | 77.8 | 0.042 | 0.072 |
| Hypertension (%) | 72.2 | 71.2 | 70.9 | 71.2 | 61.1 | 0.710 | 0.749 |
| Diabetes mellitus type 2 (%) | 44.3 | 38.3 | 36.4 | 38.6 | 44.4 | 0.070 | 0.103 |
| Smoking (pack years) | 17.5 (1-37.5) | 12.5 (0.15-32) | 16.5 (3.1-33.4) | 22.5 (5.75-45) | 22.0 (9.38-34.6) | 0.005 | 0.012 |
| Smoking (active/former/ never (%)) | 29.4/47.5/23.1 | 21.7/53.4/24.9 | 27.2/52/20.9 | 35.9/46.2/17.9 | 41.7/41.7/16.7 | <0.001 | 0.001 |
| Alanine aminotransferase (U/L) | 10.0 (8.0-13.0) | 10.0 (8.0-13.0) | 11.0 (9.0-14.0) | 12.0 (9.0-16.0) | 11.0 (9.75-16.0) | 0.001 | 0.001 |
| Aspartate aminotransferase (U/L) | 13.0 (10.0-20.0) | 14.0 (10.0-21.0) | 14.0 (10.0-20.0) | 15.0 (11.0-24.0) | 14.0 (10.8-17.0) | 0.034 | 0.050 |
| De Ritis ratio | 1.35 (1.07-1.72) | 1.33 (1.07-1.69) | 1.32 (1.08-1.67) | 1.33 (1.11-1.6) | 1.24(0.93-1.55) | 0.473 | 0.473 |
| γ-Glutamyltransferase (mg/dl) | 17.0 (11.0-28.0) | 19.0 (12.0-30.0) | 21.0 (13.0-37.8) | 28.0 (17.0-51.2) | 40.0 (22.2-63.0) | <0.001 | <0.001 |
| Mean corpuscular volume (fL) | 88.6 (85.9-91.4) | 89.3 (86.5-92.3) | 89.8 (87.0-92.1) | 91.4 (88.1-94.2) | 91.5 (87.5-95.4) | <0.001 | <0.001 |
| Fibrinogen (mg/L) | 386 (325-465) | 365 (311-444) | 378 (321-464) | 398 (333-453) | 408 (337-496) | 0.003 | 0.006 |
| Fatty liver index | 55.2 (34.2-76.6) | 55.5 (35.3-76.8) | 62.3 (39.5-78.5) | 72.2 (48.3-86.5) | 75.1 (36.8-87.9) | <0.001 | <0.001 |
| Interleukin 6 (ng/L) | 3.39 (1.89-6.81) | 3.09 (1.78-5.6) | 3.21 (1.92-6.17) | 4.04 (2-7.59) | 3.32 (1.9-10.6) | 0.008 | 0.015 |
| Mean platelet volume (fL) | 8.9 (8.3-9.6) | 8.9 (8.3-9.6) | 8.9 (8.33-9.6) | 9.2 (8.4-9.9) | 8.95 (8.38-9.52) | 0.107 | 0.123 |
ANOVA (non-normally distributed variables were analysed by Kruskal-Wallis rank sum test) or Chi square test.
p-Value after FDR correction.
Table 2.
Only female study participants anthropometric, biochemical, and liver-specific characteristics (mean (±SD) or median (25th to 75th percentile) data) according to four different alcohol intake groups in the main manuscript.
| Variable | Groups of total alcohol consumption |
|||||
|---|---|---|---|---|---|---|
| Female | No intake 0 g/d ethanol |
Low intake > 0 - 37.5 g/d ethanol |
Medium intake > 37.5 - 50.0 g/d ethanol |
High intake > 50 - 100 g/d ethanol |
Pa | FDR-Pb |
| N | 578 | 366 | 55 | 7 | - | - |
| Age (years) | 64.7 ± 10.5 | 64.9 ± 9.91 | 63.7 ± 9.31 | 65 ± 11.6 | 0.897 | 0.947 |
| BMI (kg/m2) | 27.6 ± 4.86 | 27.0 ± 4.37 | 26.9 ± 4.34 | 24.7 ± 3.53 | 0.076 | 0.132 |
| LDL-cholesterol (mg/dl) | 123 ± 37 | 124 ± 38.2 | 125 ± 32.5 | 122 ± 24.4 | 0.980 | 0.980 |
| HDL-cholesterol (mg/dl) | 42.2 ± 11.3 | 44.5 ± 11.9 | 47.1 ± 12.5 | 43.4 ± 12.4 | 0.002 | 0.014 |
| Apolipoprotein A-I (mg/dl) | 139 ± 25.7 | 144 ± 26.7 | 147 ± 26.2 | 146 ± 20.1 | 0.012 | 0.058 |
| Apolipoprotein A-II (mg/dl) | 41.5 ± 8.82 | 43.9 ± 9.95 | 47.8 ± 9.55 | 43.1 ± 13.5 | <0.001 | <0.001 |
| Triglycerides (mg/dl) | 145 (109-204) | 133 (101-192) | 136 (114-194) | 114 (103-136) | 0.296 | 0.433 |
| Fasting glucose (mg/dl) | 102 (93.3-120) | 98.9 (91.5-115) | 101 (92.2-113) | 101 (92.2-102) | 0.055 | 0.105 |
| HbA1c (%) | 6.48 ± 1.33 | 6.28 ± 1.24 | 6.51 ± 1.51 | 5.66 ± 0.32 | 0.045 | 0.095 |
| Systolic blood pressure (mmHg) | 142 ± 25.4 | 140 ± 23.7 | 136 ± 20.7 | 146 ± 26.3 | 0.287 | 0.433 |
| Diastolic blood pressure (mmHg) | 79 ± 11.2 | 80.2 ± 11.8 | 79.3 ± 10.7 | 79.1 ± 7.48 | 0.502 | 0.596 |
| eGFR (ml/min/1.73 m²) | 76.1 ± 20.8 | 77.2 ± 18.6 | 78 ± 17.8 | 80.5 ± 19.6 | 0.723 | 0.808 |
| hsCRP (mg/L) | 4.06 (1.71-8.99) | 2.89 (1.29-8.12) | 2.8 (1.19-9.52) | 6.86 (3.06-8.81) | 0.023 | 0.079 |
| NT-pro-BNP (pg/mL) | 348 (147-935) | 290 (114-786) | 302 (173-750) | 207 (136-624) | 0.408 | 0.534 |
| Coronary artery disease (%) | 69.6 | 57.7 | 60.0 | 71.4 | 0.002 | 0.014 |
| Hypertension (%) | 77.7 | 74.0 | 70.9 | 85.7 | 0.422 | 0.534 |
| Diabetes mellitus type 2 (%) | 42.9 | 36.1 | 36.4 | 0.0 | 0.025 | 0.079 |
| Smoking (pack years) | 0.15 (0.15-5.75) | 0.15 (0.15-5.75) | 0.15 (0.15-3.25) | 15.0 (0.15-32.8) | 0.172 | 0.286 |
| Smoking (active/ex/ never (%)) | 18.0/19.6/62.5 | 13.9/19.1/66.9 | 23.6/14.5/61.8 | 57.1/0.0/42.9 | 0.035 | 0.082 |
| Alanine aminotransferase (U/L) | 9.0 (8.0-12.0) | 10.0 (8.0-13.0) | 11.0 (8.0-14.0) | 12.0 (9.0-16.0) | <0.001 | <0.001 |
| Aspartate aminotransferase (U/L) | 12.0 (8.0-18.0) | 13.0 (9.0-19.0) | 14.0 (10.0-20.0) | 15.0 (11.0-23.0) | <0.001 | <0.001 |
| De Ritis ratio | 1.25 (1.0-1.58) | 1.28 (1.0-1.62) | 1.3 (1.0-1.67) | 1.33 (1.08-1.59) | 0.036 | 0.041 |
| γ-Glutamyltransferase (mg/dl) | 15.0 (9.0-25.0) | 17.0 (11.0-29.0) | 20.0 (13.0-36.0) | 27.0 (16.5-49.5) | <0.001 | <0.001 |
| Mean corpuscular volume (fL) | 88.2 (85.5-91.0) | 89.1 (86.4-92) | 89.8 (86.7-92.2) | 91.5 (88.1-94.2) | <0.001 | <0.001 |
| Fibrinogen (mg/L) | 388 (327-458) | 365 (312-440) | 378 (321-467) | 398 (330-452) | <0.001 | <0.001 |
| Fatty liver index | 51.8 (27.5-73.7) | 51.4 (31.5-74.0) | 60.0 (37.0-77.1) | 71.7 (45.2-86.2) | <0.001 | <0.001 |
| Interleukin 6 (ng/L) | 3.4 (1.84-6.45) | 3.02 (1.75-5.56) | 3.21 (1.87-6.08) | 4.0 (1.98-7.63) | 0.001 | 0.002 |
| Mean platelet volume (fL) | 8.9 (8.3-9.6) | 8.9 (8.3-9.6) | 8.9 (8.4-9.7) | 9.2 (8.4-9.9) | 0.055 | 0.059 |
ANOVA (non-normally distributed variables were analysed by Kruskal-Wallis rank sum test) or Chi square test.
p-Value after FDR correction.
Our sensitivity analysis describes genders separately. It is of note that males consume significantly more alcohol than females. With increasing alcohol consumption, the levels of HDL-cholesterol, LDL-cholesterol and apolipoprotein A-II increase in males. Apolipoprotein A-I is significantly higher in females in the highest alcohol intake category (> 50-100 g ethanol per day) than in males. Liver markers alanine aminotransferase (ALAT) and the De ritis ratio, γ-glutamyltransferase (γGT) as well as the mean corpuscular volume (MCV), interleukin-6 concentrations and fatty liver index (FLI) rise with increasing alcohol consumption and show higher significance in women than in men. Blood pressure decreases in males with increasing alcohol consumption, while it increases in females. The proportion of diabetes mellitus type 2 is higher in males with higher alcohol consumption compared to females. It is also remarkable that eGFR increases in males and females with increasing alcohol consumption. In both genders the amount of alcohol consumption correlates with the consumption of cigarettes.
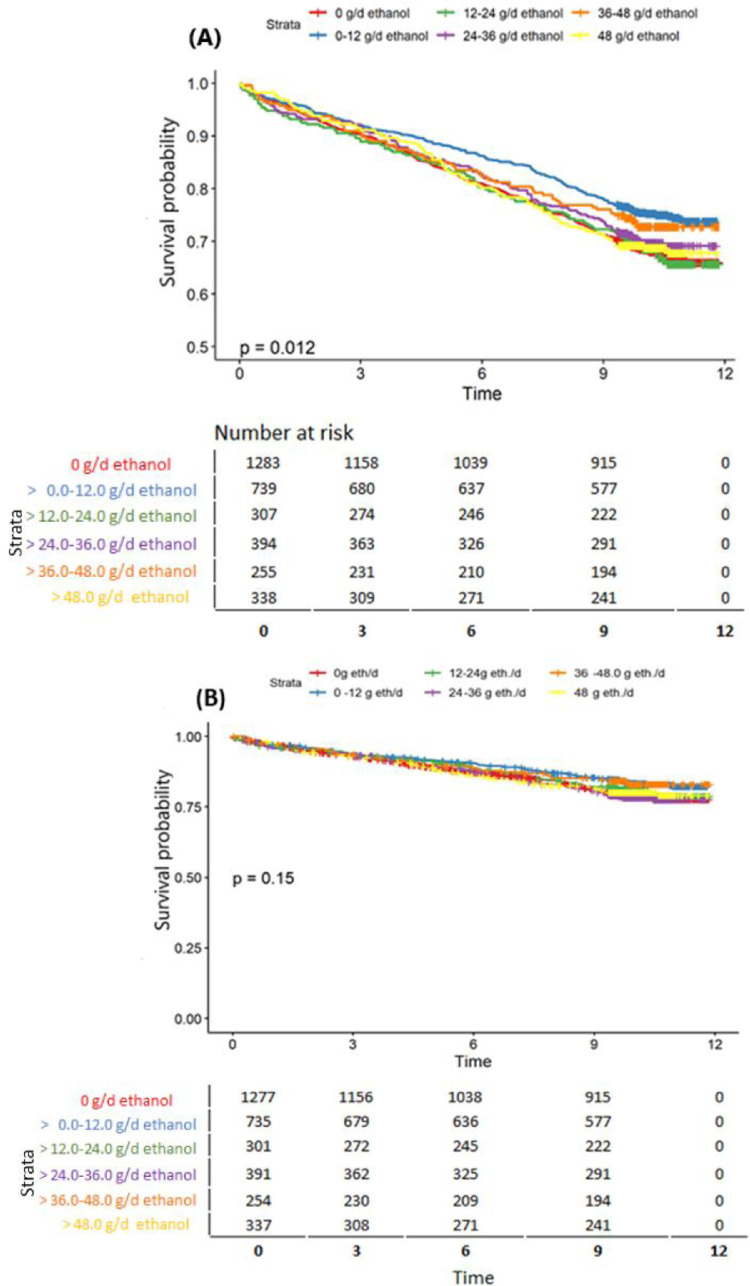
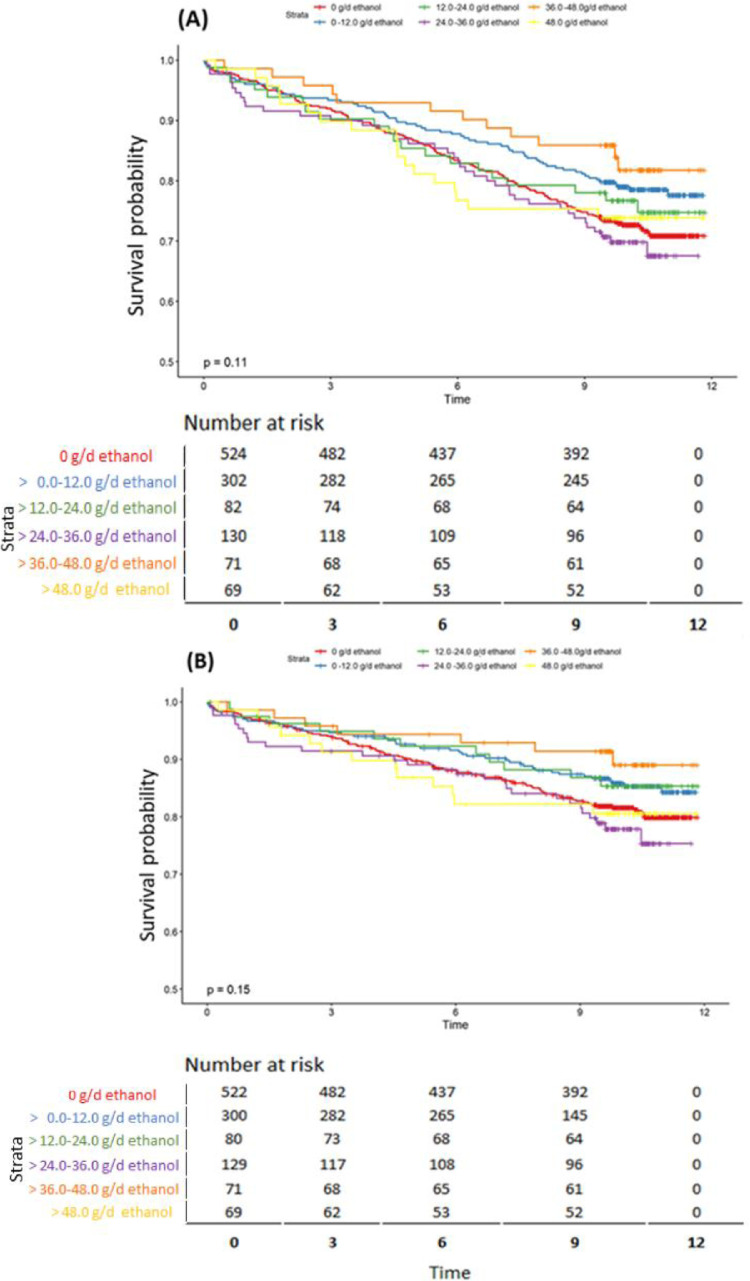
In Fig. 1 the interrelation between alcohol and mortality stratified for ethanol consumption is shown for overall mortality and cardiovascular mortality by using six different alcohol consumption groups (”no consumption” [0 g ethanol per day], “very low consumption” [> 0.0 - 12.0 g ethanol per day], “low consumption” [> 12.0 - 24.0 g ethanol per day], “medium consumption”[> 24.0 - 36.0 g ethanol per day], “high consumption” [> 36.0 −48.0 g ethanol per day], and “very high consumption” [> 48.0 g ethanol per day]). Alcohol consumption in the group of” no consumption” [0 g ethanol per day] and “low consumption” [> 12.0 - 24.0 g ethanol per day] associates with higher mortality risk and the “very low consumption” group shows lower risk for all-cause mortality. Cardiovascular mortality risk is higher for no consumption [0 g ethanol per day] and medium consumption [> 24.0 - 36.0 g ethanol per day], and very low consumption [> 0.0 - 12.0 g ethanol per day] has lower cardiovascular mortality risk.
Fig. 1.
Interrelation between alcohol consumption and mortality stratified for amount of ethanol consumption for all-cause mortality (A) and cardiovascular mortality (B) with six alcohol groups of ”no consumption” (0 g ethanol per day), “very low consumption” (> 0.0 - 12.0 g ethanol per day), “low consumption” (> 12.0 - 24.0 g ethanol per day), “medium consumption” (> 24.0 - 36.0 g ethanol per day), “high consumption” (> 36.0 - 48.0 g ethanol per day) and “very high consumption” (> 48.0 g ethanol per day).
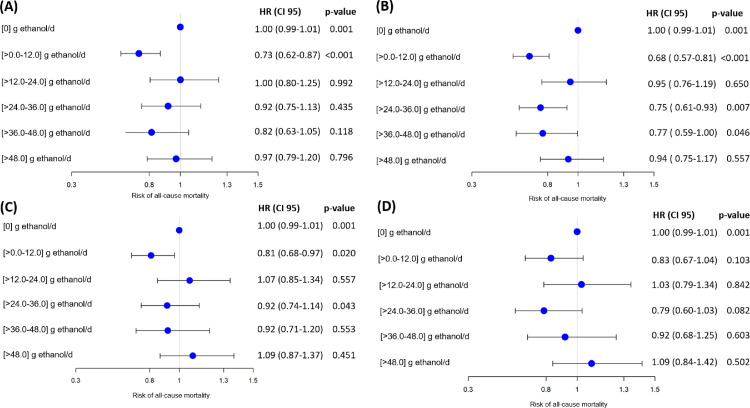
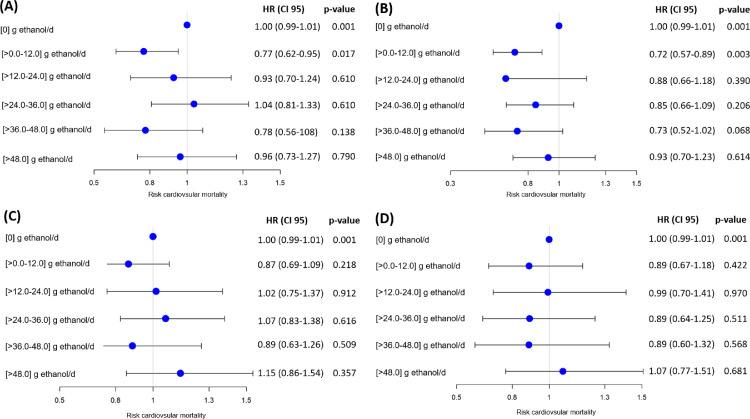
We next studied the specific risk on alcohol groups of all-cause mortality and cardiovascular mortality using four different adjustment models (see Fig. 2 and 3): (A) a crude model, and adjustment for (B) age and gender, (C) age, gender, body mass index (BMI), triglycerides, low-density lipoprotein (LDL) cholesterol, high-density lipoprotein (HDL) cholesterol, estimated glomerular filtration rate (eGFR), N-terminal prohormone of brain natriuretic peptide (NT-pro-BNP), high-sensitive C-reactive protein (hsCRP), glycated hemoglobin A1c (HbA1c), blood pressure, hypertension, diabetes mellitus type 2 and smoking (current, ex, never), and (D)age, gender, BMI, LDL-cholesterol, HDL-cholesterol, triglycerides, hsCRP, eGFR, NT-pro-BNP, blood pressure, HbA1c, hypertension, diabetes mellitus type 2 and smoking (pack years).Hazard ratios with 95% confidence intervals (CI) and p-values for each category in each model were calculated.
Fig. 2.
Group-specific risk of all-cause mortality: (A) crude; (B) for age and gender adjusted; (C) for age, gender, BMI, LDL-C, HDL-C, triglycerides, hsCRP, eGFR, NT-pro-BNP, blood pressure, HbA1c, hypertension, diabetes mellitus type 2 and smoking (current, ex, never) adjusted; and (D) for age, gender, BMI, LDL-C, HDL-C, triglycerides, hsCRP, eGFR, NT-pro-BNP, blood pressure, HbA1c, hypertension, diabetes mellitus and smoking (pack years) adjusted. Abbreviations used: HR (hazard ratios with 95% confidence intervals, CI) and p-values.
Fig. 3.
Group-specific risk of cardiovascular mortality: (A) crude; (B) for age and gender adjusted; (C) for age, gender, BMI, LDL-C, HDL-C, triglycerides, hsCRP, eGFR, NT-pro-BNP, blood pressure, HbA1c, hypertension, diabetes mellitus and smoking (current, ex, never) adjusted; and (D) for age, gender, BMI, LDL-C, HDL-C, triglycerides, hsCRP, eGFR, NT-pro-BNP, blood pressure, HbA1c, hypertension, diabetes mellitus and smoking (pack year) adjusted. Abbreviations used: HR (hazard ratios with 95% confidence intervals, CI) and p-values.
Fig. 2 shows the results for the four models for all-cause mortality risk. In models (A), (B) and (C), the lowest mortality risk was found for the group with very low alcohol consumption [> 0.0 - 12.0 g ethanol per day]. As compared to no alcohol consumption, the crude model (A) hazard ratios (95% CI) for overall mortality were 0.73 (0.62-0.87), 1.00 (0.80-1.25), 0.92 (0.75-1.13), 0.82 (0.63-1.05) and 0.97 (0.79-1.20) for groups of very low-, low-, medium-, high- and very high alcohol consumption, respectively.
Model (B), as compared to no alcohol consumption, adjusted for age- and sex shows hazard ratios (95% CI) for overall mortality of 0.68 (0.57-0.81), 0.95 (0.76-1.19), 0.75 (0.61-0.93), 0.77 (0.59-1.00) and 0.94 (0.75-1.17) for groups of very low-, low-, medium-, high- and very high alcohol consumption, respectively. No significant associations were found with further adjustment. Model (C), compared to no alcohol consumption shows, hazard ratios (95% CI) for overall mortality of 0.81 (0.68-0.97), 1.07 (0.85-1.34), 0.92 (0.74-1.14), 0.92 (0.71-1.20) and 1.09 (0.87-1.37) for groups of very low-, low-, medium-, high-, and very high alcohol consumption, respectively. In model (D), as compared to no alcohol consumption, hazard ratios (95% CI) for overall mortality were 0.83 (0.67-1.04), 1.03 (0.79-1.34), 0.79 (0.60-1.03), 0.92 (0.68-1.25), and 1.09 (0.84-1.42) for groups of very low-, low-, medium-, high- and very high alcohol consumption, respectively.
The risk of cardiovascular mortality in various categories of alcohol consumption is shown in Fig. 3; it is striking that the very low alcohol consumption group [> 0.0 - 12.0 g ethanol per day] has the lowest mortality risk in adjustment models (A) and (B). As compared to the no alcohol consumption group, the crude model (A) hazard ratios (95% CI) for cardiovascular mortality were 0.77 (0.62-0.95), 0.93 (0.70-1.24), 1.04 (0.81-1.33), 0.78 (0.56-1.08) and 0.96 (0.73-1.27) for very low-, low-, medium-, high- and very high alcohol consumption groups, respectively. As compared to the no alcohol consumption group, adjustment for age- and sex- hazard ratios (95% CI) for cardiovascular mortality were 0.72 (0.57-0.89), 0.88 (0.66-1.18), 0.85 (0.66-1.09), 0.73 (0.52-1.02), and 0.93 (0.70-1.23) for very low-, low-, medium-, high- and very high alcohol consumption groups, respectively. With further adjustments in models (C) and (D) the associations were not significant anymore. In model (C), compared to the no alcohol consumption group, hazard ratios (95% CI) were 0.87 (0.69-1.09), 1.02 (0.75-1.37), 1.07 (0.83-1.38), 0.89 (0.63-1.26), and 1.15 (0.86-1.54) for very low-, low-, medium-, high- and very high alcohol consumption group, respectively. In model (D), compared to the no alcohol consumption group, hazard ratios (95% CI) for cardiovascular mortality were 0.89 (0.67-1.18), 0.99 (0.70-141), 0.89 (0.64-1.25), 0.89 (0.60-1.32), and 1.07 (0.77-1.51) for very low-, low-, medium-, high- and very high alcohol consumption group, respectively.
In Tables 3 and 4 we describe the anthropometric and biochemical characteristics as well as liver associated characteristics of the LURIC study participants according to six different alcohol consumption groups as means ± standard deviation (SD) or medians (25th to 75th percentile) data that are different from that used in the analyses of our main manuscript published in Atherosclerosis [1]. We observe significantly increasing levels of apolipoprotein A-I and increased eGFR with increasing alcohol consumption and a positive relationship between smoking and the amount of alcohol consumption per day. When considering the entire cohort, a significant increase in liver markers can be observed with increasing alcohol intake as expected.
Table 3.
Six different groups of alcohol consumption for all study participants characterised by anthropometric and biochemical biomarkers (mean (±SD) or median (25th to 75th percentile) data).
| Variable | Groups of total alcohol consumption |
|||||||
|---|---|---|---|---|---|---|---|---|
| No consumption 0 g/d ethanol |
Very Low consumption > 0 - 12.0 g/d ethanol |
Low consumption > 12.0 - 24.0 g/d ethanol |
Medium consumption > 24.0 - 36.0 g/d ethanol |
High consumption > 36.0 - 48.0 g/d ethanol |
Very high consumption > 48.0 g/d ethanol |
Pa | FDR-Pb | |
| N | 1283 | 739 | 307 | 394 | 255 | 338 | - | - |
| Age (years) | 62.7 ± 11.0 | 62.6 ± 10.9 | 61.8 ± 11.0 | 64.9 ± 9.51 | 62.1 ± 10.3 | 61.4 ± 9.17 | <0.001 | <0.001 |
| Male sex (%) | 45.1 | 30.7 | 14.7 | 23.9 | 14.9 | 7.1 | <0.001 | <0.001 |
| BMI (kg/m2) | 27.6 ± 4.51 | 27.3 ± 3.9 | 27.5 ± 3.83 | 27.4 ± 3.7 | 27.4 ± 3.42 | 27.8 ± 3.85 | 0.476 | 0.501 |
| LDL-cholesterol (mg/dl) | 118.0 ± 35.5 | 117.0 ± 33.2 | 117.0 ± 32.8 | 114.0 ± 35.5 | 119.0 ± 36.5 | 114.0 ± 32.9 | 0.248 | 0.292 |
| HDL-cholesterol (mg/dl) | 38.0 ± 10.9 | 38.5 ± 10.6 | 38.7 ± 10.7 | 39.9 ± 10.8 | 40.2 ± 10.3 | 39.7 ± 11.3 | 0.003 | 0.006 |
| Apolipoprotein A-I (mg/dl) | 128 ± 25.3 | 129.0 ± 24.9 | 130.0 ± 24.6 | 131.0 ± 24.5 | 131.0 ± 23.3 | 132.0 ± 25.7 | 0.034 | 0.048 |
| Apolipoprotein A-II (mg/dl) | 40.1 ± 8.71 | 41.4 ± 9.79 | 43.5 ± 9.5 | 41.6 ± 9.03 | 43.7 ± 9.84 | 44.1 ± 10.4 | <0.001 | <0.001 |
| Triglycerides (mg/dl) | 150 (110-203) | 139 (103-194) | 159 (120-214) | 138 (106-188) | 146 (114-190) | 150 (111-220) | <0.001 | <0.001 |
| Fasting glucose (mg/dl) | 102 (93.5-121) | 100 (92.1-115) | 103 (94.4-121) | 103 (94.9-117) | 103 (96.2-115) | 104 (96.9-119) | 0.029 | 0.044 |
| HbA1c (%) | 6.47 ± 1.39 | 6.19 ± 1.17 | 6.19 ± 1.34 | 6.22 ± 1.14 | 6.3 ± 1.17 | 6.21 ± 1.06 | <0.001 | <0.001 |
| Systolic blood pressure (mmHg) | 141.0 ± 24.7 | 142.0 ± 23.5 | 143.0 ± 23.0 | 141.0 ± 22.5 | 138.0 ± 21.6 | 141.0 ± 22.7 | 0.192 | 0.240 |
| Diastolic blood pressure (mmHg) | 80.1 ± 11.5 | 81.6 ± 11.9 | 82.2 ± 11.4 | 82.1 ± 11.5 | 80.5 ± 10.6 | 81.1 ± 10.5 | 0.004 | 0.006 |
| eGFR (ml/min/1.73 m2) | 79.6 ± 21.5 | 82.2 ± 19.6 | 83.9 ± 20.3 | 80.3 ± 18.2 | 84.5 ± 18.3 | 86.3 ± 18.4 | <0.001 | <0.001 |
| hsCRP (mg/L) | 3.84 (1.61-8.91) | 2.83 (1.12-7.84) | 2.89 (1.2-8.28) | 2.86 (1.19-6.91) | 3.42 (1.25-9.96) | 4.22 (1.32-9.72) | <0.001 | <0.001 |
| NT-pro-BNP (pg/mL) | 322 (116-916) | 253 (94.5-730) | 271 (98-950) | 322 (121-916) | 311 (97-900) | 285 (112-878) | 0.047 | 0.063 |
| Coronary artery disease (%) | 79 | 75.9 | 76.9 | 76.6 | 80 | 78.7 | 0.553 | 0.553 |
| Hypertension (%) | 74.7 | 72.3 | 73.9 | 69.5 | 69.8 | 71.3 | 0.287 | 0.318 |
| Diabetes mellitus type 2 (%) | 43.6 | 37.2 | 37.1 | 39.6 | 38 | 36.1 | 0.022 | 0.037 |
| Smoking (pack years) | 6 (0.15-29.4) | 6.25 (0.15-25) | 15 (0.15-31.2) | 9.95 (0.15-28) | 12.5 (0.15-30) | 20 (3.12-42.4) | <0.001 | <0.001 |
| Smoking (active/ex/ never, %) | 24.2/34.9/40.8 | 20.3/38.8/40.9 | 25.4/47.9/26.7 | 14.5/52.5/33 | 23.9/48.2/27.8 | 35.5/44.1/20.4 | <0.001 | <0.001 |
ANOVA (non-normally distributed variables were analysed by Kruskal-Wallis rank sum test) or Chi square test.
p-Value after FDR correction.
Table 4.
Six different groups of alcohol consumption for all study participants characterised by liver-specific biomarkers (mean (±SD) or median (25th to 75th percentile) data).
| Variable | Groups of total alcohol consumption |
|||||||
|---|---|---|---|---|---|---|---|---|
| No consumption 0 g/d ethanol |
Very low consumption > 0.0 - 12.0 g/d ethanol |
Low consumption > 12.0 - 24.0 g/d ethanol |
Medium consumption > 24.0 - 36.0 g/d ethanol |
High consumption > 36.0 - 48.0 g/d ethanol |
Very high consumption > 48.0 g/d ethanol |
Pa | FDR-Pb | |
| N | 1283 | 739 | 307 | 394 | 255 | 338 | - | - |
| Alanine Aminotransferase (U/L) | 9 (8-12) | 10 (8-12) | 10 (8-13) | 10 (8.25-13) | 11 (8-14) | 11 (9-15) | <0.001 | <0.001 |
| Aspartate Aminotransferase (U/L) | 12 (8-18) | 13 (9-18) | 13 (9-19) | 13 (9.25-20) | 14 (10-20) | 14 (10-21) | <0.001 | <0.001 |
| De Ritis ratio | 1.25 (1-1.58) | 1.25 (1-1.6) | 1.29 (1-1.67) | 1.29 (1-1.61) | 1.33 (1-1.67) | 1.31 (1.07-1.57) | 0.128 | 0.136 |
| γ-Glutamyltransferase (mg/dl) | 15 (9-25) | 16 (10-27.5) | 18 (12-30) | 17 (11-29.8) | 19 (13-35) | 25 (15-45) | <0.001 | <0.001 |
| Mean corpuscular volume (fL) | 88.2 (85.5-91) | 88.8 (86.3-91.3) | 90 (86.9-92.9) | 89.2 (86.6-92.2) | 89.4 (86.4-92.2) | 90.8 (87.9-93.9) | <0.001 | <0.001 |
| Fibrinogen (mg/L) | 388 (327-458) | 368 (312-443) | 365 (312-448) | 363 (311-426) | 386 (326-466) | 385 (325-458) | <0.001 | 0.001 |
| Fatty liver index | 51.9 (27.8-73.8) | 49.5 (28.2-71.9) | 55.5 (35.9-80.1) | 52.3 (32-71.8) | 58.6 (36.8-75.1) | 68.1 (40.8-85) | <0.001 | <0.001 |
| Interleukin 6 (ng/L) | 3.4 (1.84-6.45) | 2.9 (1.75-5.33) | 3.15 (1.9-6.39) | 3.01 (1.68-5.29) | 3.34 (1.82-6.44) | 3.35 (1.94-7.14) | 0.001 | 0.001 |
| Mean platelet volume (fL) | 8.9 (8.3-9.6) | 8.8 (8.2-9.5) | 8.9 (8.2-9.65) | 9.1 (8.4-9.7) | 9.1 (8.4-9.7) | 9.1 (8.3-9.7) | 0.002 | 0.002 |
ANOVA (non-normally distributed variables were analysed by Kruskal-Wallis rank sum test) or Chi square test.
p-Value after FDR correction.
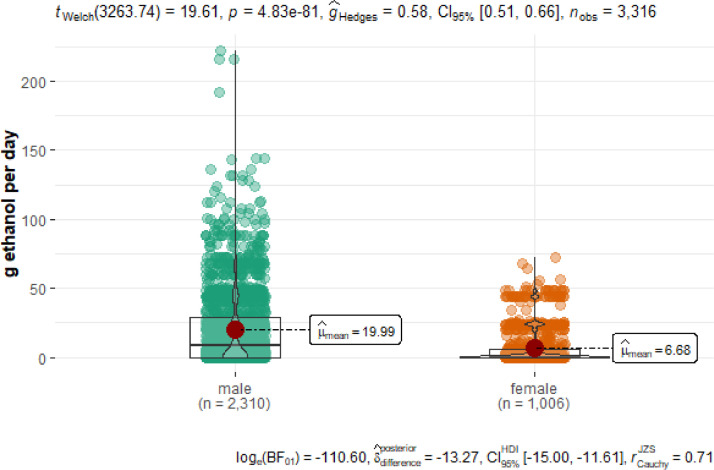
Fig. 4 shows that male participants drink significantly more alcohol than female ones. The number of males in the LURIC cohort is twice as large as the number of females.
Fig. 4.
Interrelation between alcohol consumption and gender. Boxplot showing the distribution of total alcohol consumption in g per day ethanol in the LURIC cohort stratified by gender. The interquartile ranges (IQR) are represented in the boxes, mid values are demonstrated as red point.
Tables 5,6,7 and 8 show the anthropometric and biochemical characteristics as well as liver-specific data for the gender-specific sensitivity analyses. Males drink more alcohol daily than females. Only a few females are represented in the two groups of high alcohol intake (> 36.0 - 48.0 g ethanol per day) and very high alcohol intake” (> 48.0 g ethanol per day). Further, with increasing alcohol consumption both gender show independently a significant increase of HDL-cholesterol, apolipoprotein A-I and II, an increase in eGFR and a positive correlation with smoking. Dose-dependent significant increases in liver markers are more pronounced in male study participants. In females an increase in the mean corpuscular volume (MCV) is observed. In contrast, a trend for a decreasing of liver markers was seen in the highest alcohol consumption group after an increase up to the high intake group.
Table 5.
For male study participants: Anthropometric and biochemical characteristics (mean (±SD) or median (25th to 75th percentile) data) according to six different alcohol consumption groups.
| Variable | Groups of total alcohol consumption |
|||||||
|---|---|---|---|---|---|---|---|---|
| Male | No consumption 0 g/d ethanol |
Very low consumption > 0.0 - 12.0 g/d ethanol |
Low consumption > 12.0 - 24.0 g/d ethanol |
Medium consumption > 24.0 - 36.0 g/d ethanol |
High consumption > 36.0 - 48.0 g/d ethanol |
Very high consumption > 48.0 g/d ethanol |
Pa | FDR-Pb |
| N | 312 | 188 | 104 | 121 | 82 | 117 | - | - |
| Age (years) | 61 ± 11.2 | 61.7 ± 11.0 | 61.5 ± 11.1 | 64.5 ± 9.71 | 61.8 ± 10.5 | 61.2 ± 9.09 | <0.001 | 0.001 |
| BMI (kg/m2) | 27.6 ± 4.2 | 27.4 ± 3.74 | 27.5 ± 3.65 | 27.6 ± 3.39 | 27.4 ± 3.26 | 28.0 ± 3.77 | 0.405 | 0.450 |
| LDL-cholesterol (mg/dl) | 113 ± 33.6 | 114.0 ± 32.0 | 116.0 ± 31.7 | 110.0 ± 30.8 | 117.0 ± 37.0 | 113.0 ± 33.0 | 0.222 | 0.277 |
| HDL-Cholesterol (mg/dl) | 34.6 ± 9.2 | 36.2 ± 9.26 | 37.5 ± 9.88 | 37.9 ± 9.66 | 39.1 ± 9.83 | 39.1 ± 10.8 | <0.001 | <0.001 |
| Apolipoprotein A-I (mg/dl) | 119.0 ±21.1 | 123.0 ± 21.5 | 127.0 ± 23.2 | 126.0 ± 21.7 | 129.0 ± 22.5 | 131.0 ± 25.0 | <0.001 | <0.001 |
| Apolipoprotein A-II (mg/dl) | 38.9 ±8.46 | 40.8 ± 9.95 | 42.8 ± 8.8 | 40.6 ± 8.5 | 43.2 ± 9.84 | 43.8 ± 10.3 | <0.001 | <0.001 |
| Triglycerides (mg/dl) | 155 (111-202) | 142 (105-195) | 160 (119-216) | 138 (111-184) | 146 (114-196) | 152 (112-220) | 0.001 | 0.002 |
| Fasting glucose (mg/dl) | 102 (93.6-121) | 101 (92.6-116) | 104 (95.4-121) | 104 (95.3-118) | 103 (96.6-115) | 105 (97.2-119) | 0.133 | 0.178 |
| HbA1c (%) | 6.47 ± 1.43 | 6.15 ± 1.12 | 6.23 ± 1.37 | 6.17 ± 1.11 | 6.23 ± 1.04 | 6.22 ± 1.08 | <0.001 | <0.001 |
| Systolic blood pressure (mmHg) | 140.0 ± 24.2 | 142.0 ± 23.5 | 144.0 ± 22.7 | 141.0 ± 22.2 | 139.0 ± 21.7 | 140.0 ± 22.8 | 0.264 | 0.310 |
| Diastolic blood pressure (mmHg) | 80.9 ± 11.7 | 82.5 ± 11.9 | 82.5 ± 11.5 | 82.2 ± 11.2 | 80.8 ± 10.5 | 81.2 ± 10.6 | 0.100 | 0.152 |
| eGFR (ml/min/1.73 m2) | 82.5 ± 21.8 | 84.3 ± 19.6 | 84.8 ± 20.0 | 81.6 ± 18.5 | 85.8 ± 17.9 | 86.8 ± 18.5 | 0.004 | 0.009 |
| hsCRP (mg/L) | 3.6 (1.57-8.85) | 2.87 (1.04-7.68) | 2.78 (1.15-8.35) | 2.79 (1.11-6.62) | 3.47 (1.25-9.98) | 4.3 (1.41-9.72) | 0.002 | 0.004 |
| NT-pro-BNP (pg/mL) | 302 (100-890) | 246 (89.8-696) | 292 (94-1010) | 320 (107-937) | 322 (88-967) | 276 (108-874) | 0.429 | 0.451 |
| Coronary artery disease (%) | 86.8 | 83.8 | 80.5 | 82.7 | 82.5 | 80.6 | 0.087 | 0.146 |
| Hypertension (%) | 72.2 | 70.5 | 75.2 | 68.7 | 69.6 | 71 | 0.591 | 0.591 |
| Diabetes mellitus type 2 (%) | 44.3 | 36.7 | 39.7 | 40.3 | 37.8 | 37.3 | 0.107 | 0.152 |
| Smoking (pack years) | 17.5 (1-37.5) | 10.1 (0.15-30) | 18.8 (3.15-35) | 13.8 (1-30.5) | 16 (3.4-30) | 20 (5-45) | 0.001 | 0.002 |
| Smoking (active/ex/ never, %) | 29.4/47.5/23.1 | 22.3/48.8/28.9 | 27.9/51.9/20.2 | 15.7/61.7/22.7 | 24.9/54.4/20.7 | 35/46.5/18.5 | <0.001 | <0.001 |
ANOVA (non-normally distributed variables were analysed by Kruskal-Wallis rank sum test) or Chi square test.
p value after FDR correction.
Table 6.
For male study participants: Liver-specific characteristics (mean (±SD) or median (25th to 75th percentile) data) according to six different alcohol consumption groups.
| Variable | Groups of total alcohol consumption |
|||||||
|---|---|---|---|---|---|---|---|---|
| Male | No consumption 0 g/d ethanol |
Very low consumption > 0.0 - 12.0 g/d ethanol |
Low consumption > 12.0 - 24.0 g/d ethanol |
Medium consumption > 24.0 - 36.0 g/d ethanol |
High consumption > 36.0 - 48.0 g/d ethanol |
Very high consumption > 48.0 g/d ethanol |
Pa | FDR-Pb |
| N | 312 | 188 | 104 | 121 | 82 | 117 | - | - |
| Alanine Aminotransferase (U/L) | 10.0 (8-13) | 10.0 (8-13) | 10.0 (8-13) | 11.0 (9-14) | 11.0 (9-14) | 11.0 (9-16) | <0.001 | 0.001 |
| Aspartate Aminotransferase (U/L) | 13.0 (10-20) | 13.5 (10-21) | 13.0 (9.25-20) | 14.0 (11-21.2) | 14.0 (10-20) | 15.0 (11-22) | 0.051 | 0.062 |
| De Ritis ratio | 1.35 (1.07-1.72) | 1.3 (1.07-1.7) | 1.33 (1-1.69) | 1.38 (1.08-1.67) | 1.33 (1.04-1.67) | 1.33 (1.08-1.59) | 0.936 | 0.936 |
| γ-Glutamyltransferase (mg/dl) | 17.0 (11-28) | 18.0 (12-29) | 19.0 (13-31) | 18.0 (11-31) | 21.0 (13-37) | 27.0 (16-46.8) | <0.001 | <0.001 |
| Mean corpuscular volume (fL) | 88.6 (85.9-91.4) | 88.8 (86.3-91.7) | 90.0 (86.9-93.2) | 89.4 (86.8-92.6) | 89.7 (86.8-92.3) | 90.8 (87.9-93.8) | <0.001 | <0.001 |
| Fibrinogen (mg/L) | 386 (325-465) | 368 (311-444) | 365 (319-451) | 360 (310-427) | 386 (321-467) | 388 (327-458) | 0.006 | 0.009 |
| Fatty liver index | 55.2 (34.2-76.6) | 54.1 (34-74.4) | 58.9 (36.6-80.8) | 56.3 (37-75) | 60 (37.9-76.7) | 68.8 (44.1-85.5) | <0.001 | <0.001 |
| Interleukin 6 (ng/L) | 3.39 (1.89-6.81) | 3.06 (1.76-5.52) | 3.16 (1.94-6.55) | 3.04 (1.75-5.3) | 3.32 (1.84-6.46) | 3.46 (1.98-7.46) | 0.010 | 0.014 |
| Mean platelet volume (fL) | 8.9 (8.3-9.6) | 8.8 (8.2-9.5) | 8.9 (8.2-9.7) | 9.1 (8.5-9.7) | 9.0 (8.4-9.6) | 9.1 (8.3-9.7) | 0.013 | 0.018 |
ANOVA (non-normally distributed variables were analysed by Kruskal-Wallis rank sum test) or Chi square test.
p value after FDR correction.
Table 7.
For female study participants: Anthropometric and biochemical characteristics (mean (±SD) or median (25th to 75th percentile) data) according to six different alcohol consumption groups.
| Variable | Groups of total alcohol consumption |
|||||||
|---|---|---|---|---|---|---|---|---|
| Female | No consumption 0 g/d ethanol |
Very low consumption > 0.0 - 12.0 g/d ethanol |
Low consumption > 12.0 - 24.0 g/d ethanol |
Medium consumption > 24.0 - 36.0 g/d ethanol |
High consumption > 36.0 - 48.0 g/d ethanol |
Very high consumption > 48.0 g/d ethanol |
Pa | FDR-Pb |
| N | 578 | 227 | 45 | 94 | 38 | 24 | - | - |
| Age (years) | 64.7 ± 10.5 | 64.6 ±10.3 | 63.8 ± 10.2 | 66.2 ± 8.75 | 63.6 ± 9.4 | 64.4 ± 9.84 | 0.715 | 0.783 |
| BMI (kg/m2) | 27.6 ± 4.86 | 27.1 ± 4.24 | 27.1 ± 4.78 | 26.7 ± 4.5 | 27.6 ± 4.27 | 25.0 ± 3.9 | 0.065 | 0.136 |
| LDL-cholesterol (mg/dl) | 123.0 ± 37.0 | 123.0 ± 34.9 | 124.0 ± 38.4 | 127.0 ± 45.4 | 127 ± 32.1 | 120.0 ±30.8 | 0.926 | 0.926 |
| HDL-cholesterol (mg/dl) | 42.2 ± 11.3 | 43.7 ± 11.6 | 45.3 ± 13.0 | 46.1 ± 12.0 | 46.1 ± 10.9 | 47.5 ± 14.8 | 0.003 | 0.040 |
| Apolipoprotein A-I (mg/dl) | 139.0 ±25.7 | 142.0 ± 27.0 | 147.0 ± 25.6 | 147.0 ± 26.6 | 146.0 ± 23.4 | 150 ± 28.8 | 0.013 | 0.044 |
| Apolipoprotein A-II (mg/dl) | 41.5 ± 8.82 | 42.8 ± 9.29 | 47.2 ± 12.3 | 45.0 ± 9.91 | 47.0 ± 9.34 | 47.8 ± 11.3 | <0.001 | <0.001 |
| Triglycerides (mg/dl) | 145 (109-204) | 129 (100-192) | 157 (122-185) | 132 (98.5-197) | 138 (116-175) | 118 (104-204) | 0.237 | 0.340 |
| Fasting glucose (mg/dl) | 102 (93.3-120) | 98.3 (91.5-115) | 97.1 (88.1-117) | 101 (94.7-113) | 102 (90.7-113) | 99.6 (93.5-105) | 0.166 | 0.294 |
| HbA1c (%) | 6.48 ±1.33 | 6.3 ± 1.25 | 6.0 ± 1.2 | 6.37 ± 1.21 | 6.67 ± 1.71 | 6.01 ± 0.76 | 0.037 | 0.096 |
| Systolic blood pressure (mmHg) | 142.0 ± 25.4 | 141.0 ± 23.7 | 140.0 ± 24.4 | 138.0 ± 23.6 | 133.0 ± 20.9 | 143.0 ± 21.3 | 0.269 | 0.364 |
| Diastolic blood pressure (mmHg) | 79.0 ± 11.2 | 79.5 ± 11.7 | 80.4 ± 10.8 | 81.6 ± 12.5 | 79 ± 11.3 | 79.6 ± 8.7 | 0.453 | 0.579 |
| eGFR (ml/min/1.73 m2) | 76.1 ± 20.8 | 77.5± 19.0 | 78.2 ± 20.9 | 76.0 ±16.7 | 77.2 ± 19.0 | 80 ± 16 | 0.847 | 0.886 |
| hsCRP (mg/L) | 4.06 (1.71-8.99) | 2.53 (1.19-8.2) | 3.59 (1.54-7.4) | 3.18 (1.38-7.85) | 3.12 (1.39-8.86) | 3.06 (0.872-9.66) | 0.135 | 0.259 |
| NT-pro-BNP (pg/mL) | 350 (147-935) | 272 (104-830) | 212 (120-568) | 322 (148-834) | 272 (156-631) | 362 (182-949) | 0.232 | 0.340 |
| Coronary artery disease (%) | 69.6 | 58.1 | 55.6 | 57.4 | 65.8 | 54.2 | 0.009 | 0.044 |
| Hypertension (%) | 77.7 | 76.2 | 66.7 | 72.3 | 71.1 | 75 | 0.511 | 0.619 |
| Diabetes mellitus type 2 (%) | 42.9 | 38.3 | 22.2 | 37.2 | 39.5 | 20.8 | 0.032 | 0.092 |
| Smoking (pack years) | 0.15 (0.15-10) | 0.15 (0.15-6.62) | 0.15 (0.15-4) | 0.15 (0.15-5) | 0.15 (0.15-2.5) | 0.675 (0.15-13.5) | 0.575 | 0.661 |
| Smoking (active/ex/ never, %) | 18/19.6/62.5 | 15.9/16.3/67.8 | 11.1/24.4/64.4 | 10.6/23.4/66 | 18.4/13.2/68.4 | 41.7/12.5/45.8 | 0.051 | 0.118 |
ANOVA (non-normally distributed variables were analysed by Kruskal-Wallis rank sum test) or Chi square test.
p value after FDR correction.
Table 8.
For female study participants: Liver-specific characteristics (mean (±SD) or median (25th to 75th percentile) data) according to six different alcohol consumption groups.
| Variable | Groups of total alcohol consumption |
|||||||
|---|---|---|---|---|---|---|---|---|
| Female | No consumption 0 g/d ethanol |
Very low consumption > 0.0 - 12.0 g/d ethanol |
Low consumption > 12.0 - 24.0 g/d ethanol |
Medium consumption > 24.0 - 36.0 g/d ethanol |
High consumption > 36.0 - 48.0 g/d ethanol |
Very high consumption > 48.0 g/d ethanol |
Pa | FDR-Pb |
| N | 578 | 227 | 45 | 94 | 38 | 24 | - | - |
| Alanine Aminotransferase (U/L) | 9.0 (7-11) | 9.0 (7-11) | 9.0 (7-12) | 10.0 (8-12) | 9.0 (8-10.8) | 9.0 (7.75-12) | 0.091 | 0.155 |
| Aspartate Aminotransferase (U/L) | 10.0 (7-15) | 10.0 (8-14) | 11.0 (8-15) | 10.0 (8-14) | 13.0 (9-16) | 10.0 (8-13.2) | 0.314 | 0.393 |
| De Ritis ratio | 1.14 (0.917-1.43) | 1.14 (1-1.38) | 1.09 (0.9-1.38) | 1.0 (0.849-1.33) | 1.29 (1-1.61) | 1.0 (0.865-1.36) | 0.580 | 0.658 |
| γ-Glutamyltransferase (mg/dl) | 12.0 (8-21) | 12 (8-22) | 12 (6-18) | 13.0 (9-22) | 14.5 (12-24) | 13.0 (9.75-23.2) | 0.080 | 0.155 |
| Mean corpuscular volume (fL) | 87.6 (85-90.4) | 88.6 (86.3-90.4) | 89.5 (87-92.4) | 88.9 (86.2-91.5) | 88.2 (85.5-91.9) | 91.1 (88.9-94.1) | <0.001 | 0.002 |
| Fibrinogen (mg/L) | 388.0 (329-453) | 369 (316-436) | 367.0 (295-415) | 372.0 (324-424) | 382.0 (344-451) | 368.0 (302-478) | 0.079 | 0.155 |
| Fatty liver index | 45.5 (19.5-68.5) | 37.8 (16.4-61.2) | 41.3 (23.4-57.8) | 39.1 (18.1-59.9) | 49.2 (26.3-66.4) | 23.4 (14.2-68.9) | 0.073 | 0.155 |
| Interleukin 6 (ng/L) | 3.41 (1.74-6.08) | 2.52 (1.62-4.8) | 3.09 (1.85-6.1) | 2.8 (1.48-5.17) | 3.91 (1.87-6.24) | 2.36 (1.62-4.4) | 0.089 | 0.155 |
| Mean platelet volume (fL) | 8.9 (8.2-9.6) | 8.8 (8.15-9.5) | 8.8 (8.4-9.3) | 9.0 (8.3-9.5) | 9.2 (8.4-10.1) | 8.85 (8.35-10.2) | 0.324 | 0.393 |
ANOVA (non-normally distributed variables were analysed by Kruskal-Wallis rank sum test) or Chi square test
p value after FDR correction
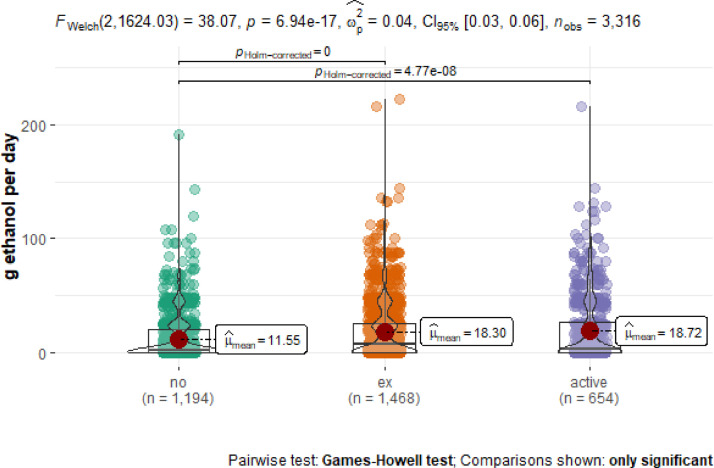
The association between smoking (never smoker, ex-smoker (<30 d), and active smoker) and alcohol consumption is shown in Fig. 5. The group of never smokers includes 1194 study participants, the group of ex-smokers 1468 persons, and the group of active smokers 654 study participants. All three smoking groups show a similar profile of alcohol consumption ranging from 0 g ethanol per day up to more than 100 g ethanol per day. There are few participants who drank more than 200 g of ethanol per day in both categories, ex-smokers and active smokers. Next, we analysed the relationship between alcohol consumption and all-cause mortality as well as cardiovascular mortality for never smokers, ex-smokers and current smokers separately (Figs. 6 and 7).
Fig. 5.
Alcohol consumption and smoking in the LURIC study cohort according to the groups never smokers, ex-smokers (< 30 d), and active smokers. The interquartile ranges (IQR) are represented in the boxes, mid values are demonstrated as red point.
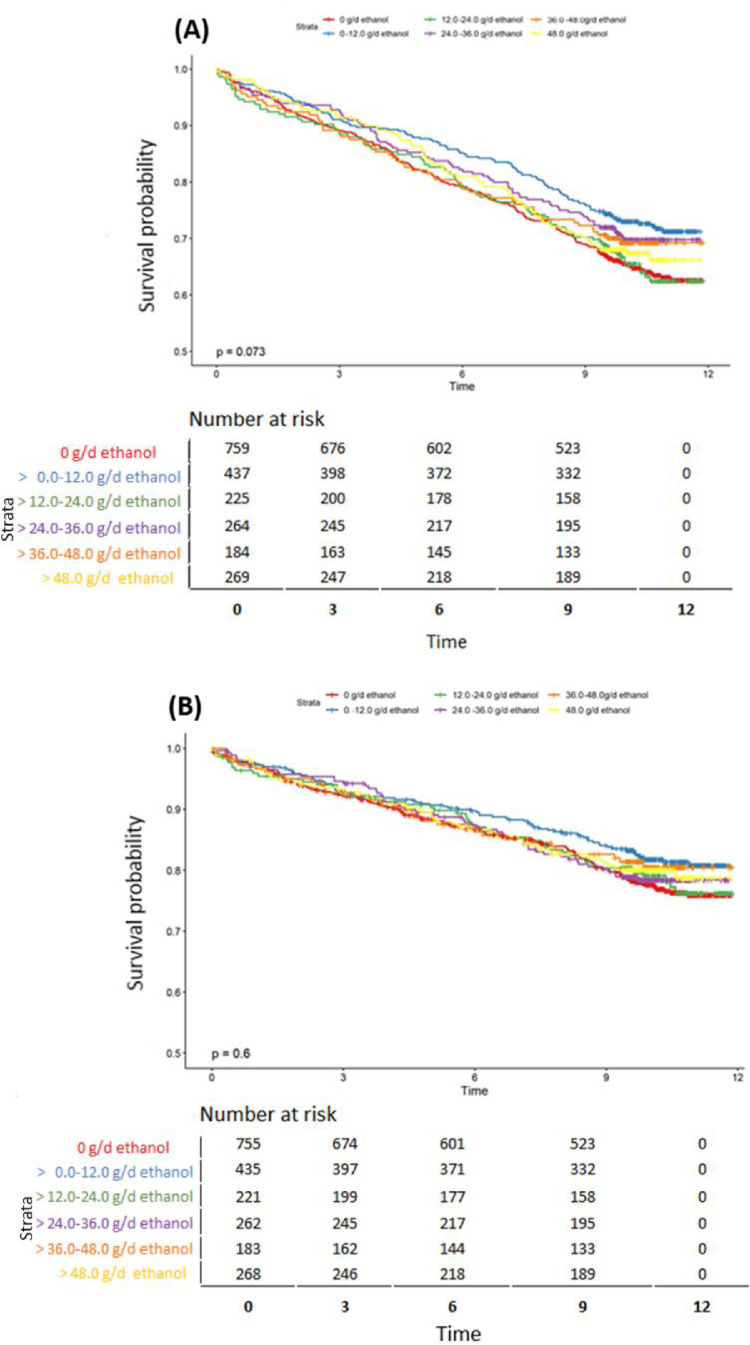
Fig. 6.
Interrelations between alcohol consumption and mortality in never smokers stratified for ethanol consumption for all-cause mortality (A) and cardiovascular mortality (B).
Fig. 7.
Interrelations between alcohol consumption and mortality in current smokers and ex-smokers stratified for ethanol consumption for all-cause mortality (A) and cardiovascular mortality.
For never smokers (Fig. 6), the overall and cardiovascular mortality risk is higher for the medium alcohol consumption group (> 24.0 - 36.0 g ethanol per day) followed by the group of no alcohol consumption (0 g ethanol per day) and very high consumption group (> 48.0 g ethanol per day), and a lower risk was observed for high alcohol consumption (> 36.0 - 48.0 g ethanol per day).
For current smokers and ex-smokers, the all-cause mortality risk is higher for no alcohol consumption (0 g ethanol per day) and for low alcohol consumption (> 12.0 - 24.0 g ethanol per day) and is lower for very low alcohol consumption (> 0.0 - 12.0 g ethanol per day). The cardiovascular mortality risk for current smokers and ex-smokers is higher in the group of no alcohol and low alcohol consumption and a lower risk is found for the group of very low alcohol consumption (Fig. 7).
2. Experimental Design, Materials and Methods
2.1. Subjects
The LURIC study enrolled 3316 participants of Western European ancestry who had an indication for coronary angiography. Recruitment took place between 1997 and 2000 at the Ludwigshafen Heart Center in South-West Germany. A detailed description of the study is provided by Winkelmann et al. [2]. The study was approved by the ‘Landesärztekammer’ Ethics Committee of the Rheinland-Pfalz state in Germany (LURIC,#83725597(1394)) Informed written consent was obtained from all participants.
2.2. Laboratory procedures
Blood samples of study participants were taken by venepuncture at study entry and the assay methods have been reported in detailed elsewhere. [2] at Apolipoproteins were measured by turbidimetry (Rolf-Greiner Biochemica, Flacht, Germany). Creatinine was measured using the CREA assay (Roche, Germany) on a Hitachi 717 analyser. Briefly, triglyceride concentrations, high-density lipoprotein (HDL) cholesterol, and total cholesterol were determined enzymatically with a Synchron LX-20 (Beckman Coulter, Munich, Germany). Low-density lipoprotein (LDL) cholesterol and very low-density lipoprotein (VLDL) cholesterol were separated by ultracentrifugation in a Beckman LM-8 ultracentrifuge in 100-μl volumes with a VT-51.2 rotor (Beckman Coulter). Glucose was measured with an enzymatic assay on a Hitachi 717 analyzer. Glycated hemoglobin was measured with immunoassay (hemoglobin A1c UNIMATE 5; Hoffmann-LaRoche, Grenzach-Whylen, Germany) [2].
Liver markers AST, ALT and GGT were measured on a Hitachi 717 analyser using the AST (ASAT/GOT), ALT (ALAT/GPT), GGT assay, respectively (all from Roche, Mannheim, Germany). High-sensitive C-reactive protein (CRP) and cystatin C were measured by immunonephelometry (N-High-Sensitive CRP; N-Latex Cystatin C, Dade Behring, Marburg, Germany) using a Behring nephelometer II. NT-pro-BNP was measured by electro-chemoluminescence on an Elecsys 2010 (Roche Diagnostics) [2].
2.3. Definition of clinical variables and endpoints
Alcohol consumption of the participants was assessed using a questionnaire at study entry. Information on the frequency of the consumption of beer, wine and spirits was collected and the specified alcohol portions were converted into volume measures as follows: a bottle of beer corresponds to 300 ml; a glass of wine corresponds to 100 ml and 1 measure of spirits corresponds to 30 ml. These quantities are common standard sizes in Germany. [3]).
The total amount of alcohol consumption was calculated as follows: one millilitre of alcohol weighs approximately 0.8 g and the amount of pure alcohol consumed in grams was calculated by multiplying volume [ml] by vol % and 0.8 [g/ml]. The following mean values (vol-%) were used for the alcohol content of the individual spirits (mean values for Germany [3]): beer, 5 vol %; wine, 12 vol %; spirits, 43% by volume.
We used two different methods to define groups of alcohol intake: 1) groups defined by visual inspection of a hazard ratio plot (“J-curve”, see [1]) and 2) groups defined by the intake of standard glasses (in Germany, a standard glass corresponds to 12 g pure ethanol [3]), a method that has been used by a number of previous studies, e.g. the Global Burden of Disease (GBD) Study [4].
An exclusion criteria for participating in the LURIC study was any acute illness other than acute coronary syndromes (decompensate heart failure, acute non-cardiac diseases), such as infection or endocrine disease [2]. The definition of clinical endpoints is described in detail in [1,2].
The CKD-EPI-eGFR-Creat-Cys equation from 2012 was used to estimate the glomerular filtration rate [4]. The vital status of the study participants was requested from local registries. Cardiovascular mortality was classified as sudden cardiac death (n = 259, 7.9%), fatal myocardial infarction (n = 106, 3.2%), death from congestive heart failure (n = 148, 4.5%), death after treatment intervention for CHD (n = 26.), 0.8%), fatal stroke (n = 61, 1.8%) and other causes of death due to CHD (n = 19, 0.6%) were counted.
2.4. Statistical analyses
Since this Data in Brief article is a supplement to our main manuscript, we used the same methods for the statistical analyses as outlined in the main manuscript [1].
For anthropometric, biochemical and liver-specific characteristics R software version 3.6.3 (http://www.r-project.org) was used.
Normal distribution was assessed by visual inspection of histograms and by comparison of mean and median values. Continuous data are presented as mean ± (SD) when following normal distribution or as median and 25th and 75th percentile when non-normally distributed.
Categorical data were presented as percentages. Statistical differences between groups were determined using ANOVA or Kruskal-Wallis test (continuous variables) or the Chi square test (categorical variables). Cox proportional hazard models were created to assess the effect of alcohol on mortality.
All tests were carried out two-sided and a p-value < 0.05 was considered statistically significant.
Correction for multiple tests was made using the false detection rate (FDR) method.
All analyses were carried out with R version 3.6.3 (http://www.r-project.org). Hazard ratio plots were created with the R package ``rms'' version 6.0-1.
Restricted cubic splines were calculated using the “rcs” function from the rms package. The function sets the knots automatically at tenth, fiftieth, and ninetieth percentiles of the total alcohol distribution.
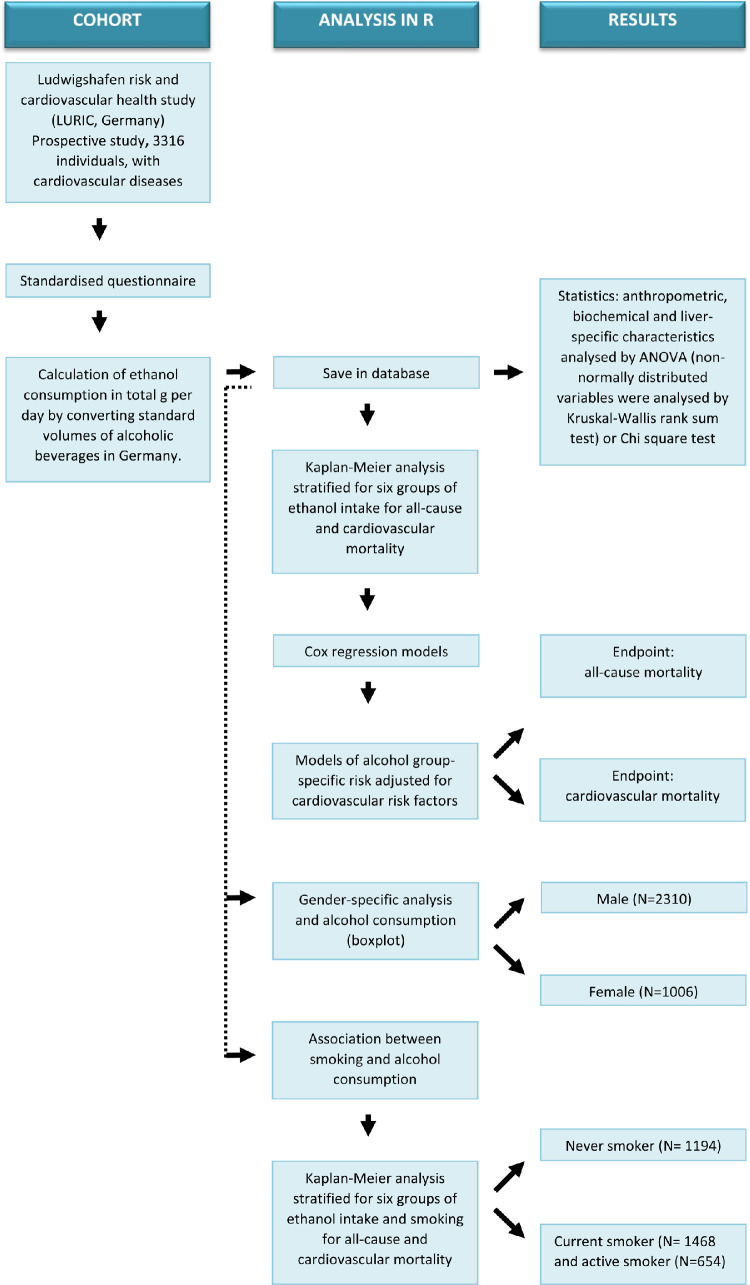
Fig. 8 shows a workflow which describes the experimental design and the analyses pathway.
Fig. 8.
Workflow on experimental design and analysis in R.
The association of groups of alcohol consumption with overall mortality and cardiovascular mortality was visualized by Kaplan-Meier curves that were created using the R package “survminer" version 0.4.9.
Four models of alcohol group-specific risk adjusted for cardiovascular risk factors were calculated using Cox proportional hazards regression, separately for the endpoints all-cause mortality and cardiovascular mortality, and visualized by forest plots.
In addition, the relationship between gender and smoking status with alcohol consumption was analysed using ANOVA and t-test and visualized as box plots.
Ethics Statement
The study was approved by the ‘Landesärztekammer’ Ethics Committee of the Rheinland-Pfalz state in Germany (LURIC, #83725597(1394)). Informed written consent was obtained from all participants.
CRediT Author Statement
Angela P. Moissl: Conceptualization, Methodology, Software, Statistical analysis, Writing- Original draft preparation, Visualization, Investigation, Software, Validation. Graciela E. Delgado: Conceptualization, Methodology, Software, Data curation, Statistical analysis, Critical review of the manuscript. Bernhard K. Krämer: Conceptualization, Methodology, Software, Writing- Original draft preparation. Christine Dawczynski: Conceptualization, Methodology, Software, Critical review of the manuscript. Tatjana Stojakovic: Conceptualization, Methodology, Software, Critical review of the manuscript. Winfried März: Conceptualization, Methodology, Software, Data curation, Writing- Original draft preparation. Marcus E. Kleber: Conceptualization, Methodology, Software, Statistical analysis, Writing- Original draft preparation, Software, Validation. Stefan Lorkowski: Conceptualization, Methodology, Software, Writing- Original draft preparation, Supervision.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships which have or could be perceived to have influenced the work reported in this article.
Acknowledgments
Acknowledgments
We thank the laboratory staff of the Klinikum Ludwigshafen and the universities of Freiburg, Ulm and Heidelberg in Germany, in addition the members of the LURIC study team who were either temporarily or permanently involved in patient recruitment as well as sample and data handling.
Grant Support
LURIC was supported by the 7th Framework Program RiskyCAD (grant agreement number 305739) of the European Union and the Competence Custer for Nutrition and Cardiovascular Health (nutriCARD) Halle-Jena-Leipzig which is funded by the German Federal Ministry for Education and Research (BMBF; grant agreement number 01EA1808A).
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.dib.2022.107873.
Appendix. Supplementary Materials
References
- 1.Moissl A.P., Delgado G.E., Krämer B.K., Dawczynski C., Stojakovic T., März W., Kleber M.E., Lorkowski S. Alcohol consumption and mortality: The Ludwigshafen Risk and Cardiovascular Health (LURIC) study. Atherosclerosis. 2021 doi: 10.1016/j.atherosclerosis.2021.08.014. [DOI] [PubMed] [Google Scholar]
- 2.Winkelmann B.R., März W., Boehm B.O., Zotz R., Hager J., Hellstern P., Senges J. Rationale and design of the LURIC study–a resource for functional genomics, pharmacogenomics and long-term prognosis of cardiovascular disease. Pharmacogenomics. 2001;2:S1–73. doi: 10.1517/14622416.2.1.S1. [DOI] [PubMed] [Google Scholar]
- 3.Bundesamt für Gesundheit . 2021. Das standardglas -Alkohol.https://www.alcohol-facts.ch/de/das-standardglas-alkohol (accessed 6 June 2021) [Google Scholar]
- 4.Alcohol use and burden for 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2018;392:1015–1035. doi: 10.1016/S0140-6736(18)31310-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.