Abstract
Scrotal trauma is a rare incident but when it occurs it is typically among 6 to 12 years old boys. It is most commonly unilateral secondary to compression of the scrotal contents against the pubic bone. The majority of trauma to the scrotal region is blunt impact but serious injuries are rare despite the vulnerable position of the testicles. The combination of the cremasteric reflex and mobility/strength of the tunica albuginea contribute to reducing occurrences. However, serious injury can occur when the testicle is trapped against the pubic bone, varying from minimal extravasation to complete parenchymal destruction. Testicular rupture is a rare injury characterized by rupture of the tunica albuginea resulting in exposure of the seminiferous tubules. Prompt evaluation of these patients is crucial as a delay in surgical care may lead to loss of the injured testicle. We present a case of acute testicular rupture in an active duty male followed by a review of the literature.
Keywords: Testicular diseases, shock, traumatic, infertility, male
Case Report
We present a 20 year old active duty male with no past medical or surgical history who presented to the emergency department with increasing testicular pain of 3 days duration. The pain initiated following a collision during a basketball game 3 days prior to presentation. At the time of the accident, he felt a sharp, transient pain in the groin. Over the course of the next 72 hours his pain continued to worsen, prompting presentation to the emergency department for evaluation. His physical examination was notable for mild tenderness and significant swelling of the left testicle with visible ecchymosis of the left hemiscrotum (Figure 1). A high frequency ultrasound with Doppler was completed, which demonstrated left testicular rupture with arterial flow (Figure 2). The patient was immediately evaluated by the on call urologist and was taken to the operating room for prompt surgical management. A transverse incision was made over the left hemiscrotum and dissection was carried down to left tunica vaginalis. The tunica vaginalis had to be pared off the testicle due to inflammation. A large defect of the tunica albuginea was identified inferiorly with a significant amount of protrusion of seminiferous tubules. Hemostasis was obtained with light fulguration. A 4-0 Polydioxanone suture (PDS) was used to close the tunica albuginea defect in a running fashion. One interrupted 4-0 PDS was placed where the edges didn’t come together well with initial suture. The left testicle and wound were irrigated with 0.05% Chlorhexidine Gluconate (Irricept) solution. The left testicle remained viable peri-procedure (Figure 3). The left testicle was placed back into the left hemiscrotum in anatomical position. A cord block was performed with 0.25% Marcaine plain anesthetic. Dartos fascia was closed with running 3-0 vicryl. Marcaine 0.25% plain was injected for pain control post op. Skin was closed with interrupted horizontal mattress 4-0 monocryl stitches. Bacitracin, Telfa, Fluffs bandage, and a scrotal support was placed. Patient tolerated the procedure well with no complications. Patient was seen for follow up in the urology clinic 3 weeks after hospital discharge. At this time he denied any testicular pain or discomfort and was without evidence of testicular atrophy on physical examination.
Figure 1.
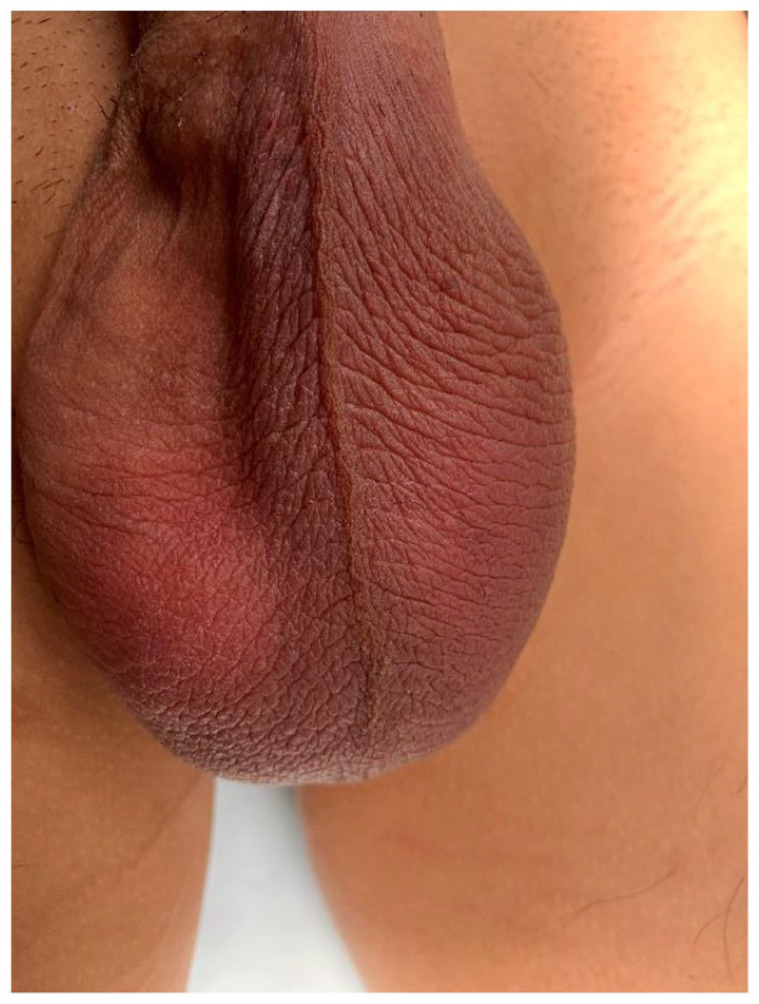
Left testicle is noted to be edematous, swollen, erythematous with a dusky hue extending from base of penis to bottom of testicle.
Figure 2.
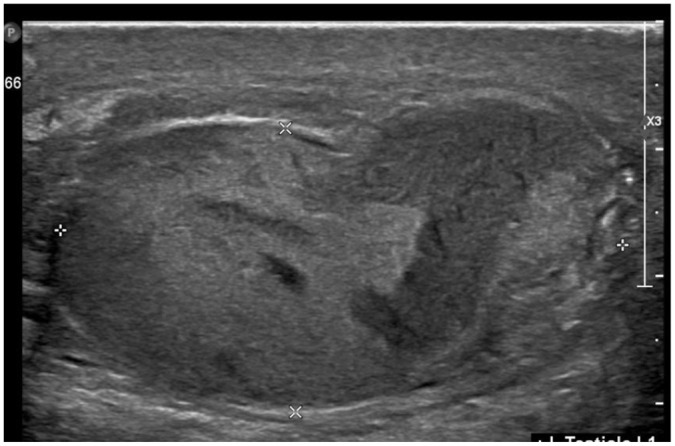
Ultrasound of left testicle: heterogeneous, dysmorphic left testicle with multiple large areas of internal hypoechogenicity, and a disruption of the capsule. Hypervascularity and edema within the epididymis.
Figure 3.
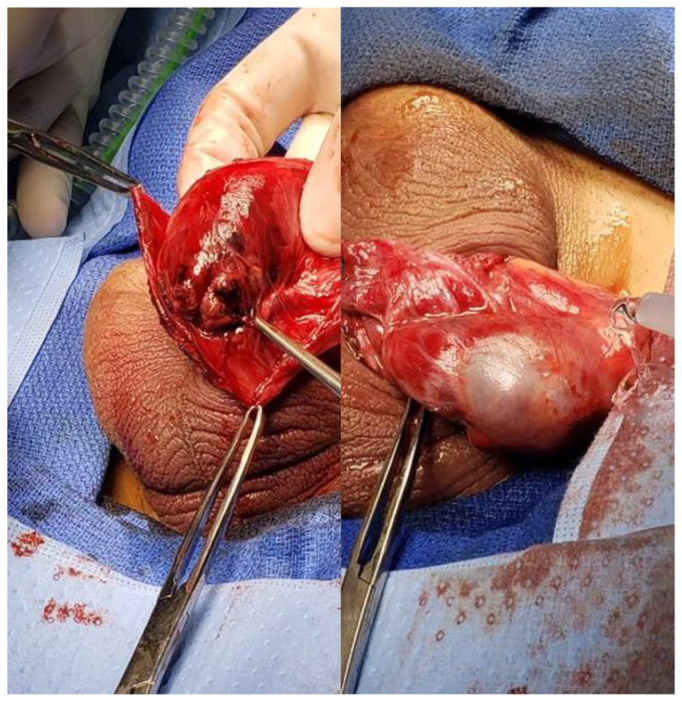
(a) Transverse incision over the left hemiscrotum, revealing inflamed tunica vaginalis, large defect of the tunica albuginea with protrusion of seminiferous tubules and (b) closure of tunica albuginea, viable testicle, and placed back into left hemiscrotum.
Discussion
Blunt testicular trauma is a rare event which warrants rapid diagnosis and prompt surgical attention. The anatomical lay of the testes in combination with the increasing use of protective cups has made this an increasingly uncommon event. 1 The right testis is more commonly injured due to its position and propensity in being trapped against the pubic bone. Previous studies have revealed that about 50 kg of force is required to rupture a testis.1,2 The clinical examination of the traumatized scrotum can be challenging due to the pain and swelling with misdiagnosis often common. Due to misdiagnoses, there has been an increased rate of traumatic sequelae to include: orchiectomy, atrophy, and infertility. 3
The initial presentation of patients with testicular rupture can be very non-specific with symptoms of scrotal swelling and severe pain, but the classic signs and symptoms include swelling, ecchymosis, persistent pain, abnormal testicular position, and abnormal testicular contour. Clinical examination can be profoundly difficult due to the pain and swelling, with concomitant reluctance for examination by the patient. 2 The differential diagnosis is vast and includes epididymitis, testicular fracture, testicular torsion, dislocated testes, hydrocele, or hematocele. However, as seen in our patient, rupture may be present with little to no pain, which may alter clinical examination and triage of injury. 2
Current urological guidelines recommend the immediate utilization of ultrasound in blunt scrotal trauma as first line evaluation as prompt diagnosis and surgical exploration allows for the highest rates of testicular salvage. 3 High frequency ultrasound with a linear array transducer is an important tool to identify the normal tunica albuginea versus rupture with greater ease than other tools. 4 It is easily accessible, allowing for early recognition of testicular rupture and prompt referral for urgent surgical management. It is performed with the patient in a supine position, testes supported by a towel, then examined in longitudinal and transverse planes. 4 Bilateral comparison occurs with the asymptomatic testis and color Doppler is applied to evaluate arterial flow on affected/unaffected sides. Previous studies with Guichard et al 3 has demonstrated a sensitivity of 100%, and specificity of 65% in a series of 33 patients. Buckley et al5,6 demonstrated a sensitivity of 100% and a specificity of 93.5% for testicular rupture on the basis of ultrasound findings of heterogeneous echotexture and contour abnormality. Bhatt and Dogra 4 examined 63 patients with testicular trauma, with no rupture found in those with an intact tunica albuginea. Hence ultrasound is a quick diagnostic tool with profound ability to help triage clinical decision making.
There are several potential sequelae which invariably occur following the treatment course of testicular rupture. The most commonly reported issue is loss of the testicle secondary to hypo perfusion and ischemia.1,2,7 Rates of this have decreased overtime with the advent of the ultrasound and prompt clinical triage. The second most common adverse outcome, although rare, is development of sperm antibodies. 7 The blood-sperm barrier is unique, and disruption of this fragile barrier can lead to contact with the immune system and development of antibodies which can affect future fertility. However, previous case reports have demonstrated the incidence to be very low and hence testicular parenchyma is still preserved.
Early surgical exploration and repair of the ruptured capsule is a first line recommendation in order to achieve the best results. Often this requires evacuation of the hematoma and a debridement of the seminiferous tubules to achieve closure of the tunica albuginea. However, this technique results in loss of viable testicular tissue with increased rates of subfertility. 8 Previous attempts to preserve tissues with polytetrafluoroethylene has been unsuccessful and increased rate of infection has been documented. 9 A novel technique, as utilized in our case above, involving apposition of the free edges of the tunica vaginalis was reported by Molokwu et al, 8 in which they demonstrated viability and stability in testes size 3 months post-operatively. In a recent case report by Keating et al, 10 they suggest the use of Papaverine as a form of salvage therapy for testicular rupture associated with inadequate perfusion. Papaverine has been utilized in subarachnoid hemorrhage to improve cerebral arterial flow but few studies are available to suggest a role for testicular hypoperfusion and therefore will warrant further investigation.
Conclusion
Testicular rupture is a rare occurrence which warrants rapid diagnosis and prompt surgical attention. Ultrasound is the diagnostic modality of choice with excellent sensitivity and specificity. Early surgical exploration is warranted but medical therapy may also be utilized in appropriate cases. Patients should be counseled and followed closely for potential subfertility.
Acknowledgments
We would like to thank Dr. Goertzen for his assistance in providing a name for this article.
Footnotes
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: The authors confirm contribution to the paper as follows: Study conception and design: Francis Essien D.O., Joshua Tate M.D., Zachary Eagle M.D. Data collection: Francis Essien D.O., Joshua Tate M.D., Austin Barber M.D. Analysis and interpretation of results: Francis Essien D.O., Joshua Tate M.D., Austin Barber M.D. Draft manuscript preparation: Francis Essien D.O., Joshua Tate M.D. Zachary Eagle M.D. All authors discussed the results and contributed to the final manuscript.
Informed Consent: Informed consent was obtained from the patient(s) for their anonymized information to be published in this article.
Ethical Approval: No approval was required for this study/
Guarantor: Francis Essien D.O.
ORCID iD: Francis Essien  https://orcid.org/0000-0001-5337-2463
https://orcid.org/0000-0001-5337-2463
References
- 1. Holliday TL, Robinson KS, Dorinzi N, et al. Testicular rupture: a tough nut to crack. Clin Pract Cases Emerg Med. 2017;1:221-224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Blok D, Flannigan M, Jones J. Testicular rupture following blunt scrotal trauma. Case Rep Emerg Med. 2019;2019:1-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Guichard G, El Ammari J, Del Coro C, et al. Accuracy of ultrasonography in diagnosis of testicular rupture after blunt scrotal trauma. Urology. 2008;71:52-56. [DOI] [PubMed] [Google Scholar]
- 4. Bhatt S, Dogra VS. Role of US in testicular and scrotal trauma. Radiographics. 2008;28:1617-1629. [DOI] [PubMed] [Google Scholar]
- 5. Buckley JC, McAninch JW. Use of ultrasonography for the diagnosis of testicular injuries in blunt scrotal trauma. J Urol. 2006. Jan;175(1):175-178. [DOI] [PubMed] [Google Scholar]
- 6. Akay S, Kaygisiz M, Oztas M, Turgut MS. Surgically confirmed intra- and extratesticular hematoma clinically mimicing epididymo-orchitis and radiologically mimicing traumatic torsion. Pol J Radiol. 2015;80:486-489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Moynihan MJ, Manganiello M. Bilateral testes fractures from blunt scrotal trauma. Urol Case Rep. 2020;28:101026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Molokwu CN, Doull RI, Townell NH. A novel technique for repair of testicular rupture after blunt trauma. Urology. 2010;76:1002-1003. [DOI] [PubMed] [Google Scholar]
- 9. Ferguson GG, Brandes SB. Gunshot wound injury of the testis: the use of tunica vaginalis and polytetrafluoroethylene grafts for reconstruction. Urol J. 2007;178:2462-2465. [DOI] [PubMed] [Google Scholar]
- 10. Keating K, Dreher PC, Levy J, McGreen B, Edwards D, Tarry S. Intra-testicular papaverine injection for testicular salvage after blunt testicular trauma: a case report. Curr Urol. 2019;13:110-112. [DOI] [PMC free article] [PubMed] [Google Scholar]


