Abstract
Introduction
Condoliase is a newly approved drug that improves symptoms associated with lumbar disk herniation (LDH) by intradiscal administration. This study aimed to evaluate the mid-term outcomes of condoliase injection, examine the adverse events, including cases that required surgery after condoliase administration, and verify cases in which condoliase could be effective.
Methods
We enrolled patients with LDH who were treated conservatively for at least six weeks and received condoliase. We assessed the visual analog scale (VAS) score, Japanese Orthopaedic Association Back Pain Evaluation Questionnaire, Oswestry Disability Index, disk height, and disk degeneration for up to 6 months, and we examined the complications. Furthermore, a 50% or more improvement in leg pain VAS score was considered effective. Factors related to symptom improvement were investigated by determining whether lower limb pain improved in six months.
Results
In total, 84 patients were recruited (52 men, 32 women; mean age, 44.2 ± 17.1 [16-86 years]). The duration of illness was 6.7 ± 6.8 (1.5-30) months. All patient-based outcomes significantly improved at 4 weeks after the administration compared with pretreatment. The intervertebral disc height decreased significantly at four weeks after condoliase administration compared with that before administration. Progression of intervertebral disc degeneration occurred in 50% of the patients. Eleven patients underwent herniotomy due to poor treatment effects. Moreover, treatment in 77.4% of the patients was considered effective. A logistic regression analysis revealed that L5/S1 disk administration (p = 0.029; odds ratio, 5.94; 95% confidence interval, 1.20-29.45) were significantly associated with clinical effectiveness.
Conclusions
Condoliase disk administration improved pain and quality of life over time. Condoliase disk administration was more effective in L5/S1 intervertebral administration.
Keywords: Condoliase, disk administration, lumbar disk herniation, lower limb pain, conservative therapy, disk degeneration
Introduction
Lumbar disk herniation (LDH) is caused by degeneration of the nucleus pulposus and annulus fibrosus due to genetic factors and excessive load that cause the nucleus pulposus to protrude and compress the nerve roots1-3). Symptoms, such as buttocks and lower limb pain, are mainly related to the nerve root depending on the onset site. However, cauda equina symptoms may also be present. Sequestrated LDH is known to regress spontaneously, and conservative treatment improves symptoms in 70%-80% of cases4,5). However, some cases are resistant to conservative treatment and often require surgical intervention. Previous reports have indicated that early surgery is economically superior to conservative treatment due to expected early improvements in symptoms6). However, surgery can cause infections and exacerbate symptoms7).
The intradiscal injection is considered an option between conservative and surgical treatments, and various drugs have been administered8). A 10-year study of chymopapain reported improvement in lower limb pain in 78% of the patients. However, chymopapain is currently not available because of its fatal complications9,10). Chondroitin sulfate ABC endolyase (condoliase) is a mucopolysaccharide-degrading enzyme extracted from gram-negative rod Proteus vulgaris11). It specifically decomposes glycosaminoglycans in the nucleus pulposus, the moisture-retaining component of the vertebral disk, without decomposing the protein. Therefore, condoliase causes less damage to the surrounding tissues than chymopapain, which has a proteolytic effect and high safety level12-14). According to some basic studies, condoliase induced fewer side effects, such as bleeding or tissue necrosis, than other enzymes15,16). Moreover, a clinical trial showed its therapeutic efficacy compared with placebo17,18). Therefore, condoliase administration is considered a treatment method with few side effects and is expected to improve pain. Although several studies reported condoliase's effects19,20), few also reported on the frequency of its side effects and the transition of symptoms due to its administration. Thus, this study aimed to investigate the mid-term outcomes of condoliase injection, evaluate cases that require surgery, examine the adverse events after condoliase administration, and verify cases in which condoliase could be effective.
Materials and Methods
The current study was a multicenter, prospective observational study, and the ethics committee approved it of all the hospitals that registered the case. All patients were informed of the study's purpose, received information about the study, and provided consent for publication. We recruited consecutive patients scheduled to receive condoliase intervertebral disc administration for LDH between November 2018 and June 2020. The inclusion criteria were patients with sub-ligamentous extrusion type LDH who complained of radicular pain after more than 6 weeks of conservative treatment and patients who completed at least 6 months of follow-up. The diagnostic criteria for LDH were as follows: (i) lower back/leg pain, (ii) symptoms persisted even at rest, (iii) magnetic resonance imaging (MRI) showed sub-ligamentous extrusion of the intervertebral disc and absence of spinal canal stenosis, and (iv) symptoms and imaging findings matched. In all cases, disk puncture was performed under fluoroscopy, and condoliase was injected into the disk's center. Condoliase was administered during outpatient or short-term hospitalization, depending on the patients' request. Patients remained on bed rest for approximately two hours after condoliase administration.
Patients
This study included 84 patients (52 men and 32 women) who underwent condoliase disc injection for sub-ligamentous extrusion type LDH. Their mean age was 44.2 ± 17.1 (16-86) years, and the duration of illness was 6.7 ± 6.8 (1.5-30) months. Herniation levels were L2/3 (n = 2), L3/4 (n = 4), L4/5 (n = 47), and L5/S1 (n = 31) (Table 1).
Table 1.
Demographic Data.
| No. of patients | 84 |
| Age, mean (range), years | 44.2±17.1 (16–86) |
| Sex (male / female) | 52 / 32 |
| Duration of illness, (range), months | 6.7±6.8 (1.5–30) |
| Herniation level | |
| L2/3 | 2 (2%) |
| L3/4 | 4 (5%) |
| L4/5 | 47 (56%) |
| L5/S1 | 31 (37%) |
Clinical outcome
We evaluated changes in clinical symptoms using the visual analog scale (VAS), with scores ranging from 0 (no pain) to 100 mm (extreme pain), Oswestry Disability Index (ODI) (0-100 points), and Japanese Orthopaedic Association Back Pain Evaluation Questionnaire (JOABPEQ). The JOABPEQ includes 25 items based on the Short-Form 36 and Roland-Morris Disability Questionnaire21,22). The time course of low back pain, lower limb pain, and lower limb numbness was evaluated using the VAS before and at 1, 2, 4, 12, and 24 weeks after condoliase administration. We evaluated changes in the quality of life (QOL) using the JOABPEQ and ODI before and at 4, 12, and 24 weeks after condoliase administration. Furthermore, each period's treatment response rate was calculated (treatment response rate = the number of cases in which lower limb pain VAS improved by more than 50% compared with before condoliase administration in each period/84 cases × 100). We also evaluated factors related to symptom improvement up to 24 weeks after condoliase administration. At this time, all patients who underwent surgery after condoliase administration were regarded as having no improvement.
Radiographic evaluation
The disk height and degeneration were evaluated by radiography and MRI. The heights of the treated intervertebral discs and adjacent vertebral bodies were measured before and at 4, 12, and 24 weeks after administration and evaluated based on the disk height index (DHI = intervertebral disc height/cranial adjacent vertebral body height) (Fig. 1). DHI at model preparation was set as 100%, and DHI changes after model preparation were expressed as % DHI (% DHI = postoperative DHI/preoperative DHI × 100)23,24). Two spine surgeons evaluated DHI, and its measurement demonstrated high precision with intraclass correlation coefficients of 0.93 and 0.84 for intra-rater and inter-rater reliability, respectively. In patients who underwent MRI before and 24 weeks after the treatment, intervertebral disc degeneration was evaluated using the MRI Pfirrmann grading system25).
Figure 1.
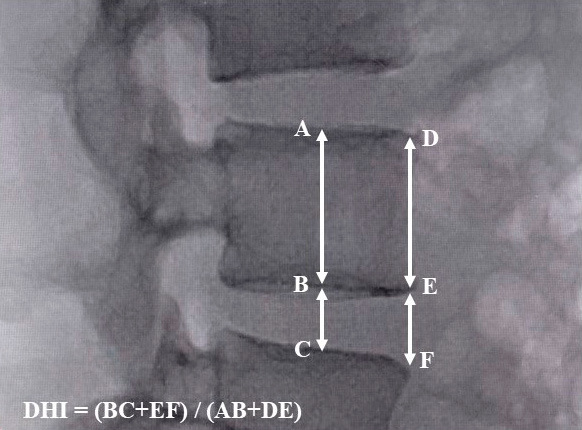
The measurement method of DHI. The formula of DHI is DHI = intervertebral disc height/cranial adjacent vertebral body height, where DHI = (BC + EF)/(AB + DE) in the figure.
DHI, disk height index
Adverse events
Adverse events after condoliase administration were examined. Cases in which treatment was switched to surgery after condoliase administration were also evaluated.
Statistical analysis
Changes in scores of a patient-based questionnaire and %DHI from before to 24 weeks after condoliase administration were evaluated using a repeated-measures linear mixed-effects model with compound symmetry covariance structure. The Tukey-Kramer test was used in the post hoc comparison. Also, logistic regression analysis was performed to evaluate patient factors related to symptom improvement in the group that showed a response at 24 weeks after condoliase administration and the group that did not. Univariate and multiple logistic regression analyses were performed using binary data as objective variables and patient factors (such as age, sex, duration of illness, herniation level, and intervertebral disc degeneration before condoliase administration) as exploratory variables to evaluate relevant risk factors. Both variable selection procedures (stepwise forward and stepwise backward regressions) yielded the same final model. All data are reported as mean ± standard deviation unless otherwise indicated. We defined the significance level at 5% and used SAS version 9.4 in all statistical analyses.
Results
Clinical outcomes
Regarding the patient-based questionnaires, the scores improved over time after intradiscal condoliase injection. VAS scores improved over time; in particular, VAS scores for lower limb pain and numbness showed the most striking improvement on average from 76.5 ± 20.9 to 46.1 ± 25.4 and 60.2 ± 28.3 to 42.6 ± 25.1, respectively, in the first week after condoliase administration. Furthermore, there was a significant improvement between 4 and 12 weeks after administration (p < 0.01) (Fig. 2). Regarding changes in QOL, both JOABPEQ and ODI scores significantly improved at all time points after condoliase administration compared with baseline. Also, except for the psychological disorders in JOABPEQ, a significant improvement was observed at 12 and 24 weeks after administration compared with 4 weeks (Table 2). Of the 84 cases, the number of cases in which lower limb pain VAS improved by more than 50% compared with before condoliase administration was 44 at 4 weeks, 62 at 12 weeks, and 65 at 24 weeks, and the treatment response rate was 52.4%, 73.8%, and 77.4%, respectively (Table 3). In a multivariate analysis evaluating the relationship between treatment response rates and patient factors, the treatment response rate was related to the injected intervertebral level, and L5/S1 intervertebral disc administration was more effective (Table 4).
Figure 2.
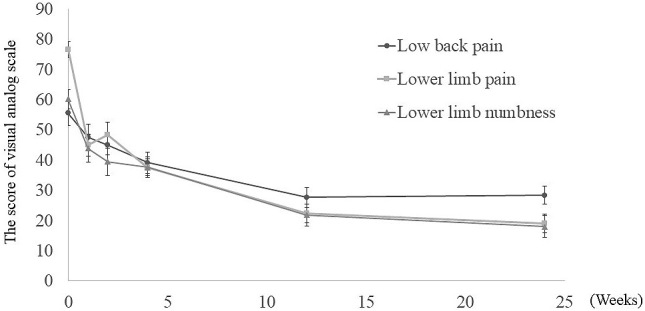
Changes in visual analog scale scores after intervertebral condoliase administration. Lower limb pain and numbness significantly improved compared with baseline in all periods. Moreover, all items significantly improved between 4 and 12 weeks after the administration.
Table 2.
Change in Patient-based Questionnaire after Condoliase Administration.
| Baseline | 4 weeks | 12 weeks | 24 weeks | |
|---|---|---|---|---|
| JOABPEQ | ||||
| Pain-related disorder | 30.1±33.7 | 54.0±35.7* | 74.7±30.2† | 74.3±33.7† |
| Lumbar spine dysfunction | 40.4±27.0 | 62.2±28.7* | 75.3±27.2† | 77.5±27.5† |
| Gait disturbance | 42.0±33.3 | 62.8±31.6* | 74.4±28.4† | 81.5±28.7† |
| Social life dysfunction | 39.4±23.1 | 53.7±23.9* | 66.8±23.4† | 71.5±25.9† |
| Phycological disorder | 49.6±20.2 | 56.4±15.4* | 60.9±17.3* | 64.3±17.3† |
| ODI | 44.2±15.1 | 34.2±14.9* | 26.4±19.7† | 19.8±16.7† |
* p>0.05 compared with baseline
† p>0.05 compared with both baseline and 4 weeks
JOABPEQ, Japanese Orthopaedic Association of Back Pain Evaluation Questionnaire; ODI, Oswestry Disability Index
Table 3.
Treatment Response Rate after Condoliase Administration.
| Effective (n) | Treatment response rate (%) | |
|---|---|---|
| 4 weeks | 44 | 52.4 |
| 12 weeks | 62 | 73.8 |
| 24 weeks | 65 | 77.4 |
Table 4.
Patient Factors Involved in Symptom Improvement after Condoliase Administration.
| Univariate logistic regression | Multivariate logistic regression | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P value | OR | 95% CI | P value | |
| Age | 0.99 | 0.97; 1.03 | 0.737 | |||
| Sex (Male) | 1.24 | 0.44; 3.52 | 0.683 | |||
| Duration of illness | 0.95 | 0.88; 1.01 | 0.111 | |||
| Herniation level (L5 / S1) | 4.04 | 1.07; 15.21 | 0.039 | 5.94 | 1.20; 29.45 | 0.029 |
| Pfirrmann grading scale (I, II) | 0.32 | 0.08; 1.25 | 0.101 | |||
OR, odds ratio; CI, confidence interval
Image evaluation
In the radiographic evaluation, the %DHI was 86.1 ± 9.7 at 4 weeks, 86.8 ± 13.5 at 12 weeks, and 89.3 ± 14.2 at 24 weeks, significantly decreasing compared with those before condoliase administration. The intervertebral disc height decreased 4 weeks after condoliase administration. However, no difference in intervertebral disc height changes occurred after 4, 12, and 24 weeks (Fig. 3). MRI was performed in 46 cases at 24 weeks after condoliase administration. Progression of disk degeneration according to the Pfirrmann classification was observed in 23 (50%) of 46 cases (Table 5). Compared with the state before condoliase administration, herniated mass often decreased at 6 months. However, intervertebral disc degeneration progressed in 50% of cases (Fig. 4). No progression of vertebral body slippage or instability was observed within 6 months after condoliase administration.
Figure 3.
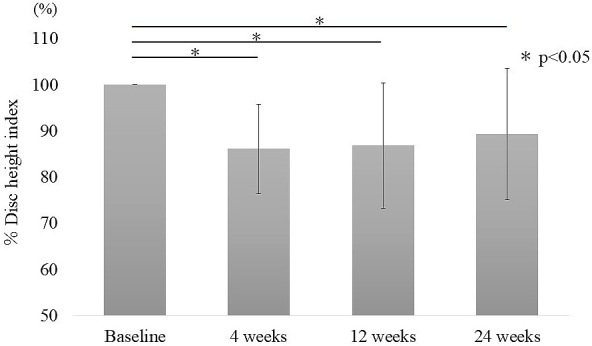
Change in the DHI (%) after intervertebral condoliase administration. The DHI (%) significantly decreased 4 weeks after the administration compared with that before administration, and no difference was observed at 4, 12, and 24 weeks after administration.
DHI, disk height index
Table 5.
Change in Pfirrmann Grading Scale (n=46).
| 24 weeks after the administration | |||||
|---|---|---|---|---|---|
| II | III | IV | V | ||
| Baseline | II | 4 | 1 | ||
| III | 10 | 17 | 1 | ||
| IV | 12 | ||||
| V | 1 | ||||
Figure 4.
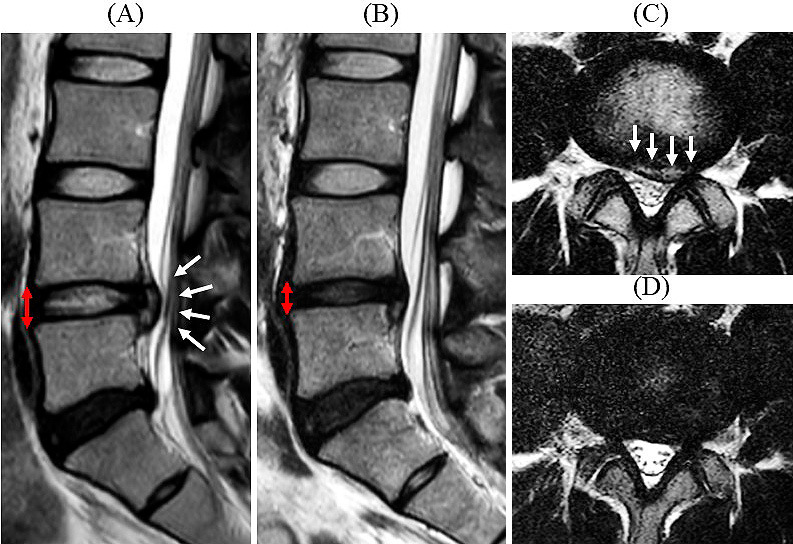
T2-weighted magnetic resonance images before (A, C) and 24 weeks after L4/5 intradiscal condoliase administration (B, D). The disk herniation at L4/5 disappeared at 6 months (white arrow). However, the disk height decreased (red arrow), and disc degeneration progressed.
Adverse events
Perioperative complications comprised drug eruption within two days of condoliase administration in three cases, in which one case was severe and hospitalized with intravenous steroid administration. Eleven patients underwent herniotomy for the same intervertebral level after condoliase administration. Surgery was performed within six weeks of condoliase administration in six cases, 6-12 weeks in 7 cases. Surgery was performed because one patient presented with a drop foot 1 week after condoliase administration to the L5/S1 intervertebral disc, and other patients had increased pain within 6 weeks of administration. In the case of drop foot, there was no obvious change in the size of the hernia mass, but a narrowing of the intervertebral disc height and leg pain enhancement occurred one week after administration, and condoliase may have been involved. Approximately 12 weeks later, seven patients were scheduled to undergo surgery because symptoms did not improve. Indications for surgery and its optimum timing were all decided by the attending physician. All patients who underwent surgery had improved leg pain after surgery. Other adverse events included exacerbation of low back pain than baseline in 16 (19%) of 84 cases within 4 weeks after administration. However, only three cases of persistent low back pain were observed, and 13 cases showed a gradual improvement of low back pain within 12 weeks. There was no association between the exacerbation of low back pain and the progression of disk degeneration.
Discussion
This study evaluated the clinical results of 6 months of condoliase disk administration for LDH. Regarding the clinical symptoms, all patient-based outcome scores showed improvement over time after condoliase administration. Especially in lower limb pain VAS, the symptoms improved most at the initial stage of condoliase administration, and a significant improvement also occurred after 4 and 12 weeks of administration. On the contrary, concerning image changes, a decrease in intervertebral disc height of 10% or more was observed after condoliase administration, and intervertebral disc degeneration progressed in half of the cases.
In this study, 77.4% of the patients showed improvements in VAS scores of lower limb pain by 50% or more after 6 months of condoliase administration. The pain improved the most 1-2 weeks after condoliase administration, and the improvement also occurred over time. At the onset of symptoms, studies reported that in more than 90% of the patients with LDH the symptoms were relieved within a few months, and lower limb pain almost disappeared at 6 months postoperatively regardless of the onset time26,27). Regarding the speed of pain improvement after surgery, Peul et al. reported that pain improved nearly 4 weeks after lumbar disk herniotomy and remained unchanged after that28). Although it was difficult to compare the effectiveness of condoliase administration and surgical treatment, condoliase was found to reduce pain slowly compared with surgical treatment. However, surgery was avoidable in 87% (73/84 cases) of the patients refractory to conservative therapy. Previous studies have reported that condoliase administration into the center of the intervertebral disc, trans-ligamentous extrusion type, and herniation with high-signal intensity on T2-weighted images was effective19,20). In the present study, L5/S1 disk administration had significantly larger effects on treatment. With regard to the injected disk level, L5/S1 had a larger hernia mass in patients who underwent surgery than did other levels29). Since the spinal canal was large in L5/S1 and the proportion of hernia mass in the spinal canal was reduced after condoliase administration, it was considered that L5/S1 was more effective than did other levels.
Patients who underwent surgery within 6 weeks after condoliase administration presented with drop foot or exacerbated lower limb pain. The condoliase administration reduces the intervertebral disc pressure, which consecutively reduces the disk height. In this regard, symptoms may be induced if the decrease in intervertebral disc height has a stronger effect than the reduction of herniated mass. Therefore, caution is required in cases with large hernia mass and cases with foraminal stenosis.
This study has several limitations. First, because it was not a comparative study, the effect of improvement due to intervertebral disc administration itself could not be ruled out. Therefore, clinical trials comparing the effects of condoliase with placebo on lower limb pain improvement are required. Second, the follow-up period was only 6 months. Since condoliase affected the intervertebral disc itself, long-term follow-up is necessary, and further studies are required. Third, since treatments such as medications were not unified after administration, condoliase administration's effect could not be strictly determined. Based on this study's results, condoliase disk injection could improve pain in patients with LDH resistant to conservative treatment. However, long-term follow-up of intervertebral disc degeneration and side effects of the drug remains necessary. Also, condoliase is effective in treatment-resistant LDH, which previously required surgery and had the potentials to evade surgery. Condoliase disk injection is also very useful as a minimally invasive treatment.
Conclusions
We evaluated the 6-month clinical results of patients who underwent intervertebral disc administration of condoliase for treatment-resistant LDH. Condoliase disk administration improved pain and QOL over time. Also, condoliase disk administration was more effective in L5/S1 intervertebral administration, and it has proved useful as a less invasive treatment. On the contrary, the progression of intervertebral disc degeneration was observed in approximately 50% of the cases. Finally, although pain relief has been achieved in many cases, long-term follow-up is warranted in the future.
Disclaimer: Sumihisa Orita is one of the Editors of Spine Surgery and Related Research and on the journal's Editorial Committee. He was not involved in the editorial evaluation or decision to accept this article for publication at all.
Conflicts of Interest: The authors declare that there are no relevant conflicts of interest.
Sources of Funding: We received no funding.
Ethical Approval: The approval code is No.2030 of Chiba university school of medicine.
Informed Consent: All participants were informed about the purpose of the study, received information, and provided written consent.
Acknowledgement
We gratefully acknowledge the work of members of our related institution involved in collecting the data.
References
- 1.Wilder DG, Pope MH, Frymoyer JW. The biomechanics of lumbar disc herniation and the effect of overload and instability. J Spinal Disord. 1988;1(1):16-32. [PubMed] [Google Scholar]
- 2.Zhang, YG, Zhang F, Sun Z, et al. A controlled case study of the relationship between environmental risk factors and apoptotic gene polymorphism and lumbar disc herniation. Am J Pathol. 2013;182(1):56-63. [DOI] [PubMed] [Google Scholar]
- 3.Seidler A, Bolm-Audorff U, Siol T, et al. Occupational risk factors for symptomatic lumbar disc herniation; a case-control study. Occup Environ Med. 2003;60(11):821-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Komori H, Okawa A, Haro H, et al. Contrast-enhanced magnetic resonance imaging in conservative management of lumbar disc herniation. Spine (Phila Pa 1976). 1998;23(1):67-73. [DOI] [PubMed] [Google Scholar]
- 5.Bush K, Cowan N, Katz DE, et al. The natural history of sciatica associated with disc pathology. A prospective study with clinical and independent radiologic follow-up. Spine (Phila Pa 1976). 1992;17(10):1205-12. [DOI] [PubMed] [Google Scholar]
- 6.Koenig L, Dall TM, Gu Q, et al. How does accounting for worker productivity affect the measured cost-effectiveness of lumbar discectomy? Clin Orthop Relat Res. 2014;472(4):1069-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stolke D, Sollmann WP, Seifert V. Intra-and postoperative complications in lumbar disc surgery. Spine (Phila Pa 1976). 1989;14(1):56-9. [DOI] [PubMed] [Google Scholar]
- 8.Khot A, Bowditch M, Powell J, et al. The use of intradiscal steroid therapy for lumbar spinal discogenic pain: a randomized controlled trial. Spine (Phila Pa 1976). 2004;29(8):833-6. [DOI] [PubMed] [Google Scholar]
- 9.Tregonning G, Transfeldt EE, McCulloch JA, et al. Chymopapain versus conventional surgery for lumbar disc herniation. 10-year results of treatment. J Bone Joint Surg Br. 1991;73(3):481-6. [DOI] [PubMed] [Google Scholar]
- 10.Nordby EJ, Wright PH, Schofield SR. Safety of chemonucleolysis. Adverse effects reported in the United States, 1982-1991. Clin Orthop Relat Res. 1993;(293):122-34. [PubMed] [Google Scholar]
- 11.Yamagata T, Saito H, Habuchi O, et al. Purification and properties of bacterial chondroitinases and chondrosulfatases. J Biol Chem. 1968;243(7):1523-35. [PubMed] [Google Scholar]
- 12.Olmarker K, Danielsen N, Nordborg C, et al. Effects of chondroitinase ABC on intrathecal and peripheral nerve tissue. An in vivo experimental study on rabbits. Spine (Phila Pa 1976). 1991;16(1):43-5. [DOI] [PubMed] [Google Scholar]
- 13.Olmarker K, Strömberg J, Blomquist J, et al. Chondroitinase ABC (pharmaceutical grade) for chemonucleolysis. Functional and structural evaluation after local application on intraspinal nerve structures and blood vessels. Spine (Phila Pa 1976). 1996;21(17):1952-6. [DOI] [PubMed] [Google Scholar]
- 14.Sugimura T, Kato F, Mimatsu K, et al. Experimental chemonucleolysis with chondroitinase ABC in monkeys. Spine (Phila Pa 1976). 1996;21(2):161-5. [DOI] [PubMed] [Google Scholar]
- 15.Ando T, Kato F, Mimatsu K, et al. Effects of chondroitinase ABC on degenerative intervertebral discs. Clin Orthop Relat Res. 1995;(318):214-21. [PubMed] [Google Scholar]
- 16.Eurell JA, Brown MD, Ramos M. The effects of chondroitinase ABC on the rabbit intervertebral disc. A roentgenographic and histologic study. Clin Orthop Relat Res. 1990;(256):238-43. [PubMed] [Google Scholar]
- 17.Chiba K, Matsuyama Y, Seo T, et al. Condoliase for the treatment of lumbar disc herniation: a randomized controlled trial. Spine (Phila Pa 1976). 2018;43(15):E869-E876. [DOI] [PubMed] [Google Scholar]
- 18.Matsuyama Y, Chiba K, Iwata H, et al. A multicenter, randomized, double-blind, dose-finding study of condoliase in patients with lumbar disc herniation. J Neurosurg Spine. 2018;28(5):499-511. [DOI] [PubMed] [Google Scholar]
- 19.Banno T, Hasegawa T, Yamato Y, et al. Clinical outcome of condoliase injection treatment for lumbar disc herniation: Indications for condoliase therapy. J Orthop Sci. 2021;26(1):79-85. [DOI] [PubMed] [Google Scholar]
- 20.Okada E, Suzuki S, Nori S, et al. The effectiveness of chemonucleolysis with condoliase for treatment of painful lumbar disc herniation. J Orthop Sci. 2020;23. [DOI] [PubMed] [Google Scholar]
- 21.Sekiguchi M, Wakita T, Otani K, et al. Lumbar spinal stenosis-specific symptom scale: validity and responsiveness. Spine (Phila Pa 1976). 2014;39(23):E1388-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Eguchi Y, Suzuki M, Yamanaka H, et al. Assessment of clinical symptoms in lumbar foraminal stenosis using the Japanese Orthopaedic Association back pain evaluation questionnaire. Korean J Spine. 2017;14(1):1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chiang ER, Ma HL, Wang JP, et al. Use of allogeneic hypoxic mesenchymal stem cells for treating disc degeneration in rabbits. J Orthop Res. 2019;37(6):1440-50. [DOI] [PubMed] [Google Scholar]
- 24.Hudson WR, Gee JE, Billys JB, et al. Hybrid dynamic stabilization with posterior spinal fusion in the lumbar spine. SAS J. 2011;5(2):36-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pfirrmann CW, Metzdorf A, Zanetti M, et al. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976). 2001;26(17):1873-8. [DOI] [PubMed] [Google Scholar]
- 26.Jacobs WC, van Tulder M, Arts M, et al. Surgery versus conservative management of sciatica due to a lumbar herniated disc: a systematic review. Eur Spine J. 2011;20(4):513-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Akagi R, Aoki Y, Ikeda Y, et al. Comparison of early and late surgical intervention for lumbar disc herniation: is earlier better? J Orthop Sci. 2010;15(3):294-8. [DOI] [PubMed] [Google Scholar]
- 28.Peul WC, van den Hout WB, Brand R, et al. Prolonged conservative care versus early surgery in patients with sciatica caused by lumbar disc herniation: two year results of a randomised controlled trial. BMJ. 2008;336(7657):1355-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Carlisle E, Luna M, Tsou PM, et al. Percent spinal canal compromise on MRI utilized for predicting the need for surgical treatment in single-level lumbar intervertebral disc herniation. Spine J. 2005;5(6):608-14. [DOI] [PubMed] [Google Scholar]


