Hybrid peripheral nerve sheath tumor (HPNST) is a newly recognized entity of peripheral nerve sheath tumor with two or three tumor components of conventional nerve sheath tumors, including neurofibroma, schwannoma, and perineurioma. HPNST mainly occurs in the subcutaneous soft tissue; it is sometimes associated with hereditary tumor syndrome (HTS)1-3). Spinal HPNST is extremely rare. This article describes the first reported case of HPNST in the cervical spine in a patient without HTS.
A 56-year-old man presented with an exacerbation of paresthesia of both hands and the right lower limb. He had experienced mild walking disturbance for five years and had no significant medical history and no family history of HTS.
A neurological examination revealed hyperreflexia in the muscle stretch reflex in the extremities, indicating myelopathy despite normal muscle strength. Plain X-ray and computed tomography showed no calcification within the tumor. Magnetic resonance imaging (MRI) of the cervical spine showed an intraspinal mass with T1 hypo- and T2 iso-intensity, continuing to the C3 spinal nerve root at the C2-3 levels. The mass was also entirely enhanced after intravenous gadolinium-diethylenetriaminepentaacetic acid administration (Fig. 1). The patient did not meet any of the criteria of HTS, including neurofibromatosis type 1 (NF1), neurofibromatosis type 2 (NF2), and schwannomatosis4-6).
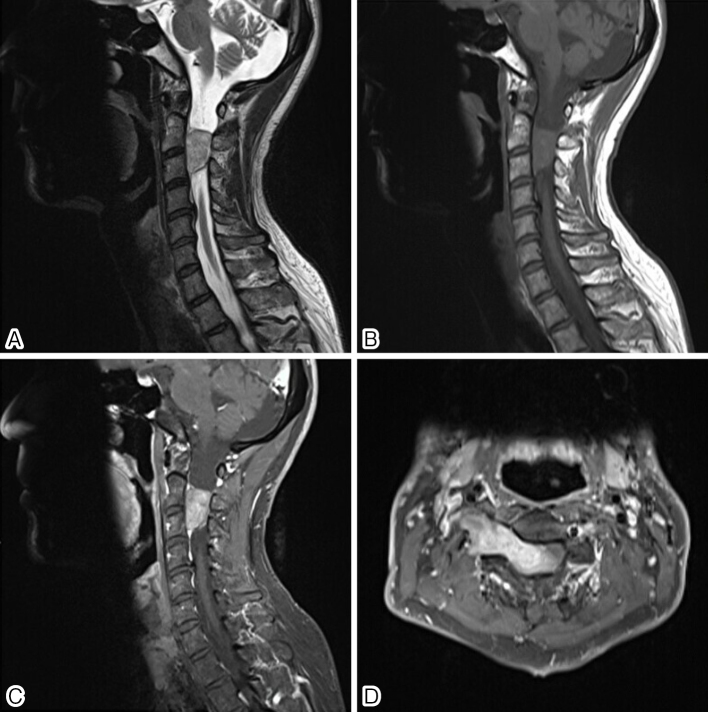
Figure 1.
Magnetic resonance imaging (MRI) of the cervical spine showed an intraspinal mass continuing to the C3 nerve root, with high intensity on T2-weighted imaging (A) and iso-intensity on T1-weighted imaging (B). The mass was enhanced by gadolinium-diethylenetriaminepentaacetic acid (C, D).
The patient underwent right C3-hemilaminotomy and right C2-3 facetectomy with right C3 nerve root sacrifice, and gross total resection of the tumor mass was achieved (Fig. 2).
Figure 2.
An intraoperative view of the tumor mass continuing to the C3 nerve root (A). The tumor was surgically excised (B).
The tumor consisted of two distinctive morphologic and immunophenotypic features. Tumor cells in the schwannomatous areas showed a fascicular growth pattern and nuclear palisading. Immunohistochemically, these cells were positive for S-100 protein and SOX10 and negative for CD34. In the neurofibromatous areas, the tumor showed low cellularity and loose arrangement with collagen bundles. A subpopulation of tumor cells was positive for S-100 protein and SOX10. Stromal cells were positive for CD34 (Fig. 3). The MIB-1 index of this tumor was about 5%.
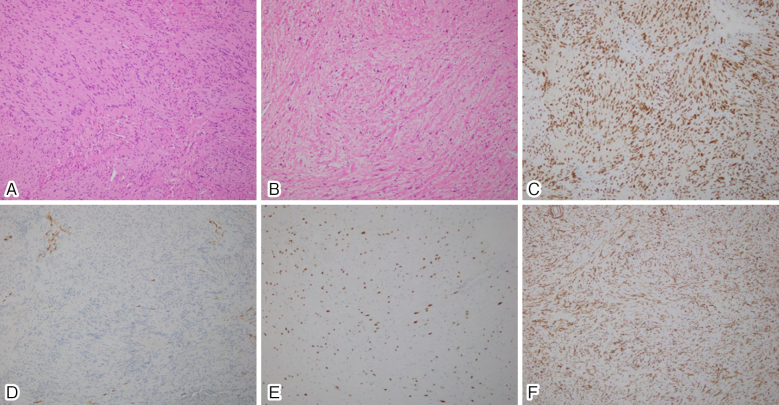
Figure 3.
Spindle cells are arranged in short bundles with nuclear palisading. HE ×100 (A). Small spindle-shaped cells are loosely arranged with collagen fibers (B). Immunohistochemical findings. The Schwann cells expressed SOX10 (C). The tumor cells in the schwannomatous component were CD34-negative (D). The spindle cells in the neurofibromatous component were partially SOX10-positive (E). Stromal cells were CD34-positive (F).
The patient reported subtle sensory disturbance around the auricle after surgery. His gait disturbance gradually improved after surgery. He was able to run at the 12-month follow-up. At two years postoperatively, there was no recurrence on cervical MRI (Fig. 4).
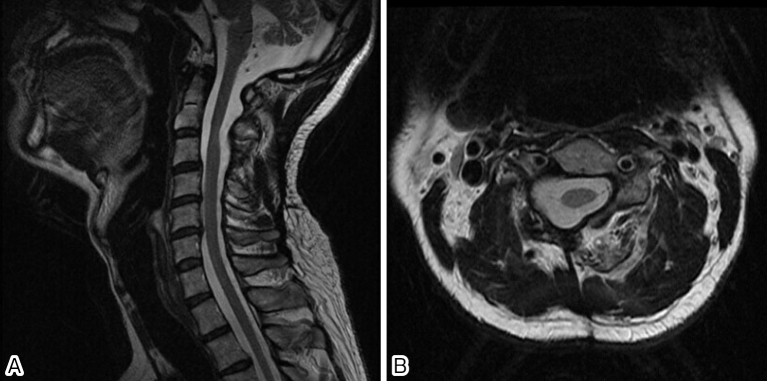
Figure 4.
MRI of the cervical spine performed two years after surgery showed no recurrence.
There are various combinations of HPNST, including neurofibroma-schwannoma, neurofibroma-perineurioma, schwannoma-perineurioma, and schwannoma-neurofibroma- perineurioma3,7). Hybrid neurofibroma-schwannoma has been reported to be frequently associated with NF1, NF2, or schwannomatosis and rarely sporadically occur3,7). However, our case of spinal hybrid neurofibroma-schwannoma was not associated with any HTS. Therefore, clinicians should keep in mind the potential risk of hybrid neurofibroma-schwannoma in spinal cord tumor, even if the patient does not show any signs of HTS.
HPNSTs commonly arise in the superficial soft tissues, including the skin and subcutaneous tissue3,7); however, but recent reports have shown that HPNSTs also occur in other anatomical locations, such as the nasal cavity8), bone9), and spinal or cranial nerves2). Heretofore, only one case of spinal HPNST has been described in detail, in which two schwannoma-perineurioma tumors, suggesting HTS, originated from the posterior nerve root in the thoracic level and the cauda equina in the lumbar level, respectively. In contrast in the present case, the patient required reoperation due to local recurrence at only five months after initial surgery of tumor resection10). In our case, we did not observe recurrence of the tumor at the final follow-up (two years after surgery). Although further studies are needed to clarify the risk factors for malignancy in spinal HPNST, the histological subtype of HPNST, presence of HTS, and level at which the tumor develops may be associated with the risk of malignancy.
Conflicts of Interest: The authors declare that there are no relevant conflicts of interest.
Author Contributions: KI designed and executed the experiments and wrote the manuscript. YI was a major contributor in writing the manuscript. HK contributed in introducing the concept of pathology. ET, TM, SI, YK, YT, AH, and SI contributed in introducing the concept of orthopedic surgery and helped write the manuscript. HC is a supervisor and edited the manuscript. All authors reviewed and approved the final manuscript.
Informed Consent: Informed consent was obtained from this patient in this study.
References
- 1.Hornick JL, Michal M. Hybrid nerve sheath tumors. In: Fletcher CDM, Bridge JA, Hogendoorn PCW, Mertens F, editors. WHO Classification of Tumors of Soft Tissue and Bone. 4th ed. IARC: Lyon; 2013. [Google Scholar]
- 2.Antonescu CR, Stemmer-Rachamimov AO, Perry A. Hybrid nerve sheath tumors. In: Louis DN, Ohgaki H, Wiestler OD, Cavenec WK, Ellison DW, et al., editors. WHO Classification of Tumors of the Central Nervous System Revised. 4th ed. IARC: Lyon; 2016. p. 224-5. [Google Scholar]
- 3.Ud Din N, Ahmad Z, Abdul-Ghafar J, et al. Hybrid peripheral nerve sheath tumors: report of five cases and detailed review of literature. BMC Cancer. 2017;17(1):349. doi: 10.1186/s12885-017-3350-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Institutes of Health Consensus Development Conference Statement: Neurofibromatosis Arch Neurol Chicago. 1988;45:p. 575-578. [PubMed] [Google Scholar]
- 5.Baser ME, Friedman JM, Wallace AJ, et al. Evaluation of clinical diagnostic criteria for neurofibromatosis 2. Neurology. 2002;59(11):1759-65; doi: 10.1212/01.WNL.0000035638.74084.F4 [DOI] [PubMed] [Google Scholar]
- 6.Plotkin SR, Blakeley JO, Evans DG, et al. Update from the 2011 International Schwannomatosis Workshop: From genetics to diagnostic criteria. Am J Med Genet A. 2013;161A(3):405-16. Published online 2013 Feb 7. doi: 10.1002/ajmg.a.35760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Michal M, Kazakov DV, Michal M. Hybrid peripheral nerve sheath tumors: A review. Cesk Patol. 2017;53(2):81-8. [PubMed] [Google Scholar]
- 8.Kuroda N, Kazakov DV, Hes O. Hybrid peripheral nerve sheath tumor of the nasal cavity showing schwannomatous, neurofibromatous, and perineuriomatous areas. Med Mol Morphol. 2010;43(2):82-5. doi: 10.1007/s00795-008-0418-7. [DOI] [PubMed] [Google Scholar]
- 9.Chow LT. Primary intraosseous hybrid nerve sheath tumor of femur: a hitherto undescribed occurrence in bone with secondary aneurysmal bone cyst formation resulting in pathological fracture. Pathol Res Pract. 2015;211(5):409-14. doi: 10.1016/j.prp.2014.10.014. [DOI] [PubMed] [Google Scholar]
- 10.Hayashi T, Hirose T, Nishimura Y, et al. Hybrid schwannoma/perineurioma of the spinal nerve: multifocal occurrence, and recurrence as an intraneural perineurioma. Pathol Int. 2013;63(7):368-73. doi: 10.1111/pin.12073. [DOI] [PubMed] [Google Scholar]