Abstract
Objective
Vaccination misinformation is widespread on social media. Vaccine-promoting organisations are working to curb its influence, but face obstacles. We aimed to analyse their social media strategies and the challenges they encounter.
Methods
In this qualitative study, we purposively sampled 21 participants responsible for social media from vaccine-promoting organisations. We used Framework Analysis to explore the data.
Results
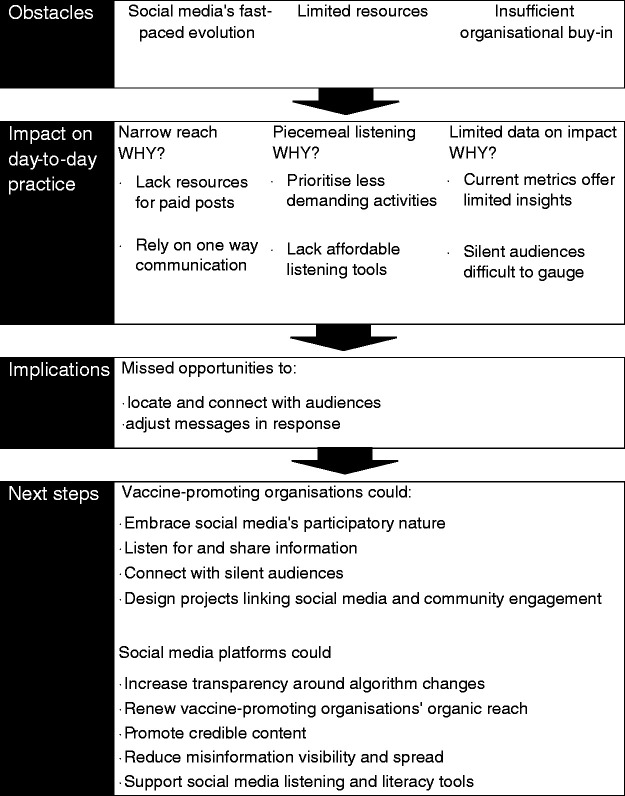
Vaccine-promoting organisations faced obstacles using social media, including fast-paced change, limited resources, and insufficient organisational buy-in. They experienced difficulties reaching audiences, exploiting social media listening, and measuring impact. Consequently, they may miss opportunities to counter misinformation, connect with groups low in vaccine confidence, and determine diverse audience responses. They lack strong evidence linking social media strategies with behaviour change, and have difficulty understanding silent audiences.
Conclusions
Vaccine-promoting organisations have an opportunity to embrace the participatory nature of social media. They could share listening insights with like-minded groups, and conduct research exploring associations between social media strategies and community attitude/behaviour change. Social media platforms could assist by renewing vaccine-promoting organisations' organic reach, supporting the development of tailored listening and credibility tools, and strengthening collaborations to promote credible content.
Keywords: Qualitative research, social media, health communication, communications media, vaccines, vaccination, immunisation, public health, health promotion
Introduction
Vaccination misinformation is prevalent on social media 1 and has potential to decrease public confidence or trust in the safety and effectiveness of vaccines. 2 , 3 From late 2018, under pressure from health authorities in the wake of measles outbreaks across America and Europe, 4 social media platforms launched measures to curtail vaccination misinformation spreading across their domains. 5 The success of these measures—blocking vaccine-related search results, reducing the visibility of groups posting misinformation, demonetising anti-vaccine content, and collaborating with leading public health bodies to promote credible content—remains to be seen.
Simultaneously, vaccine-promoting organisations are actively combating vaccination misinformation online. Our previous research found that such organisations have developed sophisticated strategies to work in this contested space, including open and authentic communication with audiences, being circumspect about responding to misinformation and anti-vaccine activists, creating safe and respectful spaces for audiences to ask questions, and fostering partnerships with like-minded organisations. 6 In addition to the challenges presented by misinformation, harnessing the full potential offered by social media presents them with myriad difficulties, such as shifting evidence on what comprises effective message content 7 , 8 and gaps in guidance for social media use in health contexts. 9 Vaccine-promoting organisations likely face many further hurdles in this environment, however our knowledge of their experiences using social media is limited. Prior research focuses largely on observable characteristics of campaigns and posts.10–12 Analysing the obstacles they face can inform future strategies and solutions to strengthen vaccination promotion online. This research aimed to understand and analyse the experiences of vaccine-promoting organisations on social media, including how they use it, and the challenges they face.
Methods
This qualitative, interview-based study was approved by Macquarie University Human Research Ethics Committee. In October 2017, we assembled a list of Australian organisations promoting vaccination on Facebook, Australia's dominant social media platform, 13 and Twitter, known for information dissemination and debate relating to health issues. 14 We identified organisations via a search on these platforms, as well as via Google, using the keywords immunisation, immunise, vaccination, and vaccine. We purposively sampled from five organisational categories: advocacy groups, government health departments, health services, professional associations, and technical/scientific organisations. We excluded media and information websites and companies selling products or services because their activities were not unequivocally related to health promotion. We identified additional organisations using snowball sampling. Short-listed organisations were posting about vaccines on Facebook or Twitter at least monthly or had run a vaccination-related campaign in the last 12 months.
Eligible participants were consenting, English-speaking individuals responsible for routine social media activity or strategy in the identified vaccine-promoting organisations. If organisations employed separate individuals for strategy and routine social media activities, multiple participants from the same organisation were interviewed. Participants provided written consent to 60-minute, anonymous interviews (by phone or in person) after receiving written information about the study. Our research questions informed the interview schedule, as did concepts underlying effective communication developed from social media risk communication principles. 15 These concepts included: planning for using social media; tracking audience concerns; interacting to build credibility; building partnerships; and communicating in a forthcoming and human way. Semi-structured, in-depth interview questions covered purpose, strategies and challenges of using social media platforms. Interviews took place between November 2017 and July 2018; these were audio-recorded and transcribed using a confidential service.
Assisted by NVivo 11 (NVivo qualitative data analysis software; QSR International Pty Ltd. Version 11, 2015), we explored our data using Framework Analysis. 16 The organising framework consisted of items from the interview schedule. To ensure analytic rigour we employed investigator triangulation, reflexivity via memo-writing and group discussions, and attention to divergent cases. 17
Results
We interviewed 21 individuals from 17 organisations, sampling at least two organisations from each category (Table 1). Four of the organisations we approached declined to participate, citing lack of time. Eight organisations focused exclusively on vaccination; the remainder covered a broad range of health topics. Two-thirds of participants had a communications background; the remainder had science, health or advocacy backgrounds. Participants' responsibilities included posting on social media, engaging with audiences, moderating audience comments, and formulating strategy. Interviews lasted approximately one hour; most were by phone with a single interviewee. Participants were assigned pseudonyms.
Table 1.
Number of organisations and participants by organisation category.
| Organisation category | # of organisations | # of participants |
|---|---|---|
| Advocacy group | 8 | 8 |
| Government healthdepartment | 2 | 3 |
| Health service | 3 | 4 |
| Professional association | 2 | 2 |
| Technical/scientificorganisation | 2 | 4 |
| TOTAL | 17 | 21 |
Participants largely discussed experiences on Facebook, but also referred to Twitter and Instagram. One participating organisation used Twitter exclusively. Other social media platforms (LinkedIn, YouTube, Snapchat, etc.) were referred to less frequently. Facebook was favoured because of its direct access to audiences, who were mostly information-seeking parents. Participants viewed Twitter as valuable for networking with other organisations, the media and high-profile individuals, but less useful than Facebook for vaccine promotion to the public. Participants perceived Instagram as potentially useful but in practice used the platform infrequently.
Direct and fast access to audiences—being where the audiences are—was the main perceived benefit of using social media, especially compared with other communication mediums. Low entry costs, opportunities to interact with and understand users, ease of targeting large or specific groups, and ability to evaluate campaigns were also mentioned as advantages unique to social media. Sharing information, raising awareness about vaccination, and developing a voice—primarily on Facebook—were their chief aims in using social media. Participants also cited joining public conversations about vaccination, creating communities, raising their public profile, and networking with the media and other organisations as further aims. A few explicitly mentioned countering anti-vaccine sentiment as a reason for engaging on social media.
Our analysis revealed six themes (Figure 1). Themes from the same dataset pertaining to how vaccine-promoting organisations respond to misinformation on social media are reported elsewhere. 6
Figure 1.
Difficulties faced by organisations promoting vaccination on social media; and next steps to support vaccination promotion efforts online.
Obstacles to maximising social media's potential
Participants were enthusiastic about using social media to promote vaccination, but identified obstacles to reaching large and diverse populations. The first three themes reflect these perceived stumbling blocks.
Social media's fast-paced evolution: Social media was depicted as relentlessly in flux, characterised by shifting algorithms and evolving audience behaviours; as described by Amelia (Advocacy group), “it's constantly reinventing itself”. Participants attached great importance to continuously updating their know-how; Alison (Health service) explained this as essential, “so we can keep up with how fast things are changing”. Keeping up, however, was an uphill battle:
“Almost every day there's something new in terms of how the technology works and what the latest trend is. Keeping on top of all of that is the biggest challenge… I find it exciting, but it can also be very exhausting. Sometimes you feel like you can't win.” (Sophie, Advocacy group)
Participants attributed their difficulties to an absence of ‘how-to' advice specific to vaccination contexts on social media, and insufficient resources to pay for external assistance. They also rendered themselves partially at fault: despite their apparent skills and experience, many portrayed social media as new ground and themselves as still on a learning curve: “We're in a slightly experimental stage with it still. We're still feeling our way a bit as to what works and what doesn't” (Olivia, Professional association).
Limited resources: Participants often described their teams as under-resourced and overwhelmed. Their ideal social media practice—focusing on meaningful exchanges with audiences—was contrasted with the reality of being frequently swamped with tasks and having to abandon efforts to interact:
“I'm pretty inundated at times. To be honest, I'm lucky if I have time to put out that initial tweet about something. It would be great if I could stay and have conversations with people… but I just don't have the capacity.” (Olivia, Professional association)
The divisive nature of vaccination as a topic was acknowledged as making interactions exceptionally resource-intensive. Despite the valuable access to audiences afforded by Facebook, one organisation abstained from this platform altogether because it was perceived as particularly polarised: “We don't have the resources to respond to any questions or controversy that vaccines will probably result in, so we're not on Facebook” (Zara, Technical/scientific organisation). Organisations dependent on charitable donations were unable to commit more resources; Amelia (Advocacy group) described running operations “off the smell of an oily rag”. For some better-funded organisations, however, scarce resources stemmed from lukewarm internal support for social media.
Insufficient organisational buy-in: Having to sell social media's value to high level decision-makers within their organisations was an obstacle for some participants. Insufficient organisational buy-in could manifest as inadequate resources allocated to social media teams, the relegation of social media responsibilities to less experienced staff, or restrictions on participants' capacity to engage in two-way communication. Some accounted for this reluctance to commit to social media by pointing to their leaders' limited personal experience with the medium: social media could be “a bit of a mystery” (Olivia, Professional association) to certain decision-makers. In contrast, anti-vaccine activists were perceived as having gained advantage by embracing social media:
“The anti-vaxxers were very quick to use social media as a platform for fear mongering, but healthcare organisations were always hesitant. It took us five years to convince people here to actually engage in social media. But by that time, that's five years of… anti-vaccination groups pumping information out there and you're already on the back foot.” (Charles, Health service)
Organisational reluctance was not an issue for all participants: advocacy groups often reported using social media as their primary channel for public outreach. Government participant Julian felt supported by managers enthused by successful campaigns:
“Right now, the executive is really positive about using digital tools and social media, so they're well and truly in… But it has been challenging in the past for us, and it's really just been about education…We've had to display and show what we can do with social media and how quickly we can respond to things.”
Impact on day-to-day practice
The three themes described thus far depict the struggles vaccine-promoting organisations faced keeping pace with a changeable medium, stymied by limited resources and for some, insufficient buy-in from decision-makers within their organisations. As a result, several day-to-day activities—reaching audiences, social media listening, and measuring impact—were perceived as problematic.
Narrow audience reach: Participants sought to broaden the number of people seeing their content (reach) as a means of extending their influence. While some used paid promotion, most experimented with techniques to encourage people to engage—i.e. like, share or comment on a post—and thus broaden their reach organically (for free). Using humour or entertainment was one technique perceived as effective. For Alison (Health service), this meant diverging from messages “that just tell people what to do”:
“If people feel like they're just being fed health messaging, they'll lose interest. But if they feel like they're being entertained and we're trying to make them laugh, we're trying to make them feel something… then there might be a better response.”
Using emotion and personal stories was also seen as useful; Zoe (Advocacy group) observed that such posts routinely prompted large responses:
“They're the ones where we'll often see comments like ‘Wow, I never vaccinated my child but after seeing this we're going to the doctor to get up to date', that sort of thing. I think there's definitely a role for anecdotes. They help to support the narrative of how important vaccination is.”
More so than other strategies, however, interaction—joining conversations and answering questions—was seen as effective for fostering engagement. Liz (Advocacy group) characterised social media audiences as craving more than a one-way stream of information: “We don't want to just send links to people because they’re not going to click on those things. They want conversations”.
Despite their array of strategies, reaching broad, diverse audiences without paying was almost universally problematic. Factors perceived as out of their control, such as fierce competition for audience attention, were apportioned blame: “We're competing with cats chasing dogs on videos, and babies throwing spaghetti across the room that everyone thinks is funny and fantastic” (Charles, Health service). So too were changes to Facebook algorithms that limited organic reach: “Facebook wants you to pay for every single post. So some of our posts only get seen by 200 people, whereas a couple of years ago we were being seen by half of our audience, which right now is 13 thousand” (Joy, Technical/scientific organisation).
Internal deficiencies were also noted, such as too few people on staff to interact with audiences. Government and health services in particular were impeded by multi-tiered approval processes: “Communicating with people online is difficult, because we have a lot of sign-offs, and a lot of rules and regulations about what we can say to people” (Julian, Government). Furthermore, some participants felt obliged to communicate as “a faceless organisation” (John, Professional association), which they felt thwarted attempts to engage audiences authentically.
Piecemeal listening: Participants understood social media listening—tracking and analysing conversations—as valuable for staying abreast of emerging issues and audience sentiment. Some used misinformation uncovered in anti-vaccine Facebook groups to inform their advocacy efforts: “I like to read what they're all saying. It just gives me a perspective of parents who have doubts about vaccines” (Vicky, Advocacy group).
Approaches to gathering and acting on information, however, were piecemeal. Participants described listening as a sporadic and largely manual activity, comprising physical keyword searches or scanning Facebook parenting groups or news media pages. Only a handful used commercial monitoring tools, which were described as expensive and not necessarily designed specifically for use in health contexts. Finite resources, prioritisation of less labour-intensive activities and lack of expertise impeded their ability to exploit insights gathered through listening, for example by detecting particular audience group concerns and adapting messages accordingly: “We're not resourced enough or sophisticated enough to be listening to health concerns in terms of what drives our content” (Alison, Health service).
Difficulty measuring impact: Participants sought to measure their impact as a means of evaluating strategies and, for some, justifying funding. Methods varied: a government participant reported using population surveys and vaccination uptake data to detect attitude and behaviour changes concurrent with campaigns; a health service participant described a pilot project investigating whether a Facebook post about a new vaccination clinic drove attendance; some advocacy group participants described relying on informal audience feedback.
Primarily, however, participants measured impact using social media metrics, such as reach, number of followers, and engagement. Nevertheless, these metrics were acknowledged as inadequate measures of real-world attitude or behaviour change, as Charles (Health service) explained:
“There are a lot of posts with a sick little baby and everyone will go, ‘Aww' and ‘like' it. It doesn't do anything other than that. We need to move to making sure our posts motivate people to go and actually get immunised… Just seeing how many people you've reached doesn't prove you've done a great job.”
Metrics were also recognised as ineffective for evaluating impact on silent audiences, i.e. social media users who were reached by their posts but did not respond in any visible way: “Social media can sometimes be a very one way street, where you're posting things out and people might be seeing them, but they're not reacting and you just don't know what's going on” (Chloe, Advocacy group). Advocacy group participants in particular characterised silent audiences as wary of making themselves publicly visible and thus difficult to gauge.
Discussion
Study participants expressed optimism about social media's potential for promoting vaccination, but identified obstacles to exploiting its promise. They struggled to keep knowledge and skillsets up to date with rapidly evolving social media platforms. Insufficient managerial support, as well as incorrect assumptions about the costs required to engage on social media, resulted in under-resourced social media teams. These obstacles impacted on participants' day-to-day practice in several ways, most notably their ability to reach diverse audiences, listen comprehensively, and measure impact beyond social media metrics.
As a result of these difficulties, vaccine-promoting organisations are likely missing opportunities to understand and connect with diverse audiences, and adjust communications in response to online and real-world feedback. With narrow reach, they risk overlooking people who lack confidence in the safety and effectiveness of vaccines and who may be responsive to interventions. 18 Through piecemeal listening, they risk building an incomplete picture of audience sentiment, and forgo opportunities to adapt messages to a range of audience needs, as well as respond to distorted information and events such as safety scares.19–21 By relying on metrics to measure success, they are unable to adjust messages to appeal to silent audiences, i.e. users observing but not responding in any visible way. They also lack certainty about how to develop effective approaches to encourage behaviour change.
Despite these difficulties and risks, the vaccine-promoting organisations that participated in this study were committed to creating a presence on social media. In keeping with risk communication concepts, they recognised their efforts as affording them a means of listening and responding promptly to audience concerns in this landscape. 22 This is key, as much of their audience is already using social media to learn and communicate about health topics, like vaccination. 23
To address their difficulties, we recommend that vaccine-promoting organisations commit to the participatory nature of social media. Health organisations have been observed broadcasting information on social media in a one-way manner, which can result in lacklustre engagement. 24 Two-way interactions, in contrast, stimulate audience engagement, which in turn amplifies reach. 25 , 26 Direct replies lend individuals status and motivation to continue engaging; 27 authentic interactions resonate especially well with audiences. 15 While paid posts have a place, organisations have much to gain by reaching users—especially those whose confidence in vaccines is low—via networks of family and friends, who can influence attitudes and behaviour in ways that paid posts may not. 7 , 28
Risk-averse organisations may be reluctant to engage in two-way communication to avoid protracted dialogue with anti-vaccine activists. 6 In an environment where information is largely controlled by users, dialogue can be challenging for those organisations intent on controlling the content and spread of messages, 29 especially concerning volatile topics like vaccination. This approach has been described as ‘old power', characterised by top-down governance structures and wariness of inclusive participation. Conversely, ‘new power' is enabled by the participation of the crowd. 30 Such organisations, however, must embrace two-way communication or risk losing audiences. 21 Joining conversations and interacting authentically are key principles for effectively using social media to communicate and manage risk. 15 While controlling information on social media is unrealistic, hesitant decision-makers approving two-way interactions may be reassured by strategies that can curtail misinformation, such as close moderation of comments and avoiding hostile interactions. 6 Recent measures to control misinformation enacted by social media platforms may also assist. Two-way communication, however, still requires substantial input. For those without ready access to resources, harnessing ‘new power' may offer a lateral solution: encouraging audiences to converse amongst themselves can also foster audience engagement, although organisations must intervene to protect users when necessary. 21 , 26 , 30
We also recommend vaccine-promoting organisations prioritise social media listening across a range of platforms, which would bring further sophistication to their practice, and is in keeping with the risk communication principle of environmental scanning to listen to audience concerns. 15 , 31 , 32 By detecting significant information events, such as public controversies, 19 vaccine-promoting organisations could target low-confidence communities with interventions to counter misinformation. Sharing information with like-minded organisations would amplify their listening capacity; the development of affordable alternatives to commercial listening tools, by researchers or not-for-profit groups for example, is also essential. Any new tool must detect a post’s topic, sentiment, location, and influence (not just volume), and reveal populations in need of support.
Moving beyond a reliance on metrics would help vaccine-promoting organisations understand silent audiences, a group which likely represents a meaningful proportion of audiences in environments where health information is being shared. 33 , 34 Metrics poorly represent silent audiences: reach may indicate their presence but not how they are reacting to posts. To better understand their impact on silent audiences, vaccine-promoting organisations could create closed groups or encourage private messaging to allow wary audiences to share their views with confidence. 6 While the data is challenging to gather, researchers could also collaborate with vaccine-promoting organisations to study silent audiences and their responses, and inform messaging design.
Finding ways to directly link social media activity with changes in attitudes or behaviour would prove invaluable for refining communications, 35 as well as for persuading decision-makers to adequately resource social media teams. While measuring behaviour change is a complex endeavour, organisations could conduct their own investigations by designing and evaluating projects that provide users with simple ways to convert their social media activity into engagement with a real-world service, 36 for example providing a portal to register for reminders or book vaccines, which users could then share with their networks.
Social media platforms could play an important role in vaccine promotion if they continue developing and testing standards for moderating content, and broaden existing collaborations with credible vaccine-promoting organisations to prioritise accurate information. Platforms could acknowledge vaccine-promoting organisations' valuable contribution to the health of online communities by renewing their organic reach, and informing them of changes to algorithms determining post priority so they can adjust their strategies accordingly. Platforms could also support the development of tools that help users assess the credibility of information, or that facilitate social media listening specifically for health contexts, ensuring such tools are developed with transparency and respect user privacy. 37
Limitations
There are several limitations to this study. The number of vaccine-promoting organisations included in the study, as well as the omission of any organisations active exclusively on Instagram, Snapchat or other platforms other than Facebook or Twitter, may have affected the breadth and depth of our findings. By restricting our sample to Australian organisations, our findings may not fully translate to international contexts.
Conclusions
Vaccine-promoting organisations using social media face obstacles to success, including social media's fast paced evolution, limited resources and lukewarm internal support. This impacts on their ability to reach diverse audiences, exploit social media listening, and measure impact. Consequently, they may miss vital information about audience sentiment and opportunities to counter misinformation or connect with groups low in vaccine confidence. They lack evidence for strategies that prompt behaviour change and an understanding of how silent audiences are influenced by posts.
This study makes several recommendations. To boost engagement and amplify reach, vaccine-promoting organisations must increase authentic two-way communication. To improve listening capacity, they could share insights with like-minded groups. To measure impact, organisations could design projects that link social media activity with changes in community attitudes and behaviour. In turn, social media platforms must be transparent about algorithm changes determining post priority, renew vaccine-promoting organisations' organic reach, and continue reducing the visibility of misinformation and collaborating to prioritise credible information. Platforms could support the development of tools that assess information credibility, as well as affordable and sensitive social media listening tools as part of their contribution to combating misinformation.
Acknowledgements
N/A.
Footnotes
Contributorship: MS, AD, KW and JL all contributed to the development of research questions and study design. MS collected the data, and led the analysis and interpretation of the dataset, and the writing of the manuscript. MS, AD, KW and JL all contributed to the generation and interpretation of themes, and the writing and revising of the manuscript. MS, AD, KW and JL all read and approved the final version.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: This study was granted ethical and scientific approval by the Macquarie University Human Research Ethics Committee (HREC (Medical Sciences) – Reference No: 5201700977). We obtained written informed consent from all participants via an information and consent sheet detailing the purpose of the study.
Funding: This work was supported by Macquarie University Research Training Program Scholarship No. 2017438 and National Health & Medical Research Council Project Grant APP1128968. The funding bodies played no role in the study design; collection, analysis, and interpretation of data; or in writing the manuscript.
Availability of data and material: The dataset generated and analysed during this study is not publicly available to comply with ethics approval, and to protect the privacy of and abide by the consent of individual participants. However, de-identified interview responses are available from the corresponding author on reasonable request and with approval from the Macquarie University Human Research Ethics Committee.
Guarantor: MS.
Peer review: James Kite, The University of Sydney Faculty of Medicine and Health has reviewed this manuscript.
ORCID iD: Maryke S Steffens https://orcid.org/0000-0002-4720-3986
References
- 1.Wang Y, McKee M, Torbica A, et al. Systematic literature review on the spread of health-related misinformation on social media. Soc Sci Med 2019; 240: 112552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Larson HJ. The biggest pandemic risk? Viral misinformation. Nature 2018; 562: 309. [DOI] [PubMed] [Google Scholar]
- 3.Larson HJ, Wilson R, Hanley S, et al. Tracking the global spread of vaccine sentiments: the global response to Japan’s suspension of its HPV vaccine recommendation. Hum Vaccin Immunother 2014; 10: 2543–2550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. Weekly epidemiological record. Wkly Epidemiol Rec 2018; 93: 649–660. [Google Scholar]
- 5.Goodman E. How social media companies are tackling anti-vaccination misinformation. The London School of Economics and Political Science Media Policy Project Blog, https://blogs.lse.ac.uk/mediapolicyproject/2019/07/24/how-social-media-companies-are-tackling-anti-vaccination-misinformation/ (accessed 17 September 2019).
- 6.Steffens MS, Dunn AG, Wiley KE, et al. How organisations promoting vaccination respond to misinformation on social media: a qualitative investigation. BMC Public Health 2019; 19: 1348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kite J, Grunseit A, Li V, et al. Generating engagement on the make healthy normal campaign facebook page: analysis of facebook analytics. JMIR Public Health Surveill 2019; 5: e11132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Klassen KM, Borleis ES, Brennan L, et al. What people “like”: analysis of social media strategies used by food industry brands, lifestyle brands, and health promotion organizations on facebook and instagram. J Med Internet Res 2018; 20: e10227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moorhead SA, Hazlett DE, Harrison L, et al. A new dimension of health care: Systematic review of the uses, benefits, and limitations of social media for health communication. J Med Internet Res 2013; 15: e85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Park H Reber BH andChon MG.. Tweeting as health communication: health organizations’ use of twitter for health promotion and public engagement. J Health Commun 2016; 21: 188–198. [DOI] [PubMed] [Google Scholar]
- 11.Ramanadhan S, Mendez SR, Rao M, et al. Social media use by community-based organizations conducting health promotion: a content analysis. J Med Internet Res 2013; 13: 1129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thackeray R, Neiger BL, Smith AK, et al. Adoption and use of social media among public health departments. BMC Public Health 2012; 12: 242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yellow. Yellow social media report 2018, https://www.yellow.com.au/wp-content/uploads/2018/06/Yellow-Social-Media-Report-2018-Consumer.pdf (2018). [Google Scholar]
- 14.Chapman S andFreeman B.. Who has Australia’s most-followed twitter accounts in health and medicine? Public Heal Res Pract 2015; 25: e2531534. [DOI] [PubMed] [Google Scholar]
- 15.Veil SR Buehner T andPalenchar MJ.. A work-in-process literature review: Incorporating social media in risk and crisis communication. J Contin Cris Man 2011; 19: 110–122. [Google Scholar]
- 16.Ritchie J andSpencer L.. Qualitative data analysis for applied policy research. In: Bryman B, Burgess R. (eds) Analyzing qualitative data. London: Routledge, 1994, pp.179–194. [Google Scholar]
- 17.Mays N andPope C.. Assessing quality in qualitative research. BMJ 2000; 320: 50–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Betsch C Korn L andHoltmann C.. Don’t try to convert the antivaccinators, instead target the fence-sitters. Proc Natl Acad Sci U S A 2015; 112: E6725–E6726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bahk CY, Cumming M, Paushter L, et al. Publicly available online tool facilitates real-time monitoring of vaccine conversations and sentiments. Health Aff (Millwood) 2016; 35: 341–347. [DOI] [PubMed] [Google Scholar]
- 20.Signorini A Segre AM andPolgreen PM.. The use of twitter to track levels of disease activity and public concern in the U.S. during the influenza a H1N1 pandemic. PLoS One 2011; 6: e19467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Heldman A Schindelar J andWeaver J.. Social media engagement and public health communication: implications for public health organizations being truly “social.” Public Health Rev 2013; 35: 1–18. [Google Scholar]
- 22.Covello VT. Best practices in public health risk and crisis communication. J Health Commun 2003; 8: 5–8. [DOI] [PubMed] [Google Scholar]
- 23.Zhao Y andZhang J.. Consumer health information seeking in social media: a literature review. Health Info Libr J 2017; 34: 268–283. [DOI] [PubMed] [Google Scholar]
- 24.Capurro D, Cole K, Echavarria MI, et al. The use of social networking sites for public health practice and research: a systematic review. J Med Internet Res 2014; 16: e79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kite J, Foley BC, Grunseit AC, et al. Please like me: Facebook and public health communication. PLoS One 2016; 11: e0162765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Veale HJ, Sacks-Davis R, Weaver ER, et al. The use of social networking platforms for sexual health promotion: identifying key strategies for successful user engagement. BMC Public Health 2015; 15: 85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lampel J andBhalla A.. The role of status seeking in online communities: giving the gift of experience. J Comput Commun 2007; 12: 434–455. [Google Scholar]
- 28.Abroms LC andLefebvre RC.. Obama’s wired campaign: lessons for public health communication. J Health Commun 2009; 14: 415–423. [DOI] [PubMed] [Google Scholar]
- 29.Lefebvre RC. The new technology: the consumer as participant rather than target audience. Soc Mar Q 2007; 13: 31–42. [Google Scholar]
- 30.Perera K Timms H andHeimans J.. New power versus old: to beat antivaccination campaigners we need to learn from them. BMJ 2019; 367: l6447. [DOI] [PubMed] [Google Scholar]
- 31.Effing R andSpil TAM.. The social strategy cone: towards a framework for evaluating social media strategies. Int J Inf Manage 2016; 36: 1–8. [Google Scholar]
- 32.CDC. Crisis and emergency risk communication (CERC) manual: social media and mobile media devices. 2014. Retrieved from : https://emergency.cdc.gov/cerc/ppt/CERC_Social Media and Mobile Media Devices.pdf
- 33.Merchant G, Weibel N, Patrick K, et al. Click “like” to change your behavior: a mixed methods study of college students’ exposure to and engagement with facebook content designed for weight loss. J Med Internet Res 2014; 16: e158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Crawford K. Following you: disciplines of listening in social media. Continuum 2009; 23: 525–535. [Google Scholar]
- 35.Freeman B, Potente S, Rock V, et al. Social media campaigns that make a difference: what can public health learn from the corporate sector and other social change marketers? Public Heal Res Pract 2015; 25: e2521517. [DOI] [PubMed] [Google Scholar]
- 36.Cameron AM, Massie AB, Alexander CE, et al. Social media and organ donor registration: the facebook effect. Am J Transplant 2013; 13: 2059–2065. [DOI] [PubMed] [Google Scholar]
- 37.Isaak J andHanna MJ.. User data privacy: Facebook, Cambridge analytica, and privacy protection. Computer 2018; 51: 56–59. [Google Scholar]