Abstract
Introduction
Early-onset of Electronic Nicotine Delivering Systems (ENDS) use puts users at higher risk of developing a regular ENDS use pattern and/or transitioning to combusted tobacco products. Previous studies on ENDS use among adolescents have not considered sexual orientation as a fluid trait that can change over time. Our objective was to evaluate whether ENDS initiation differed by sexual orientation in a longitudinal, population-based cohort of adolescents transitioning into young adulthood in Texas.
Methods
Sample (n = 1712) was drawn from the Texas Adolescent Tobacco and Marketing Surveillance System (waves 5–11) and stratified into three groups, representing sexual orientation: (1) respondents who reported being heterosexuals at each wave (straight), (2) those who consistently self-identified as lesbian, gay or bisexual individuals (LGB), and (3) subjects who reported sexual orientation mobility across waves (mobile). Nonparametric models for interval-censored data were used to estimate the cumulative distribution of age at ENDS initiation by sexual orientation group. Cox models for interval-censored data were used to evaluate whether ENDS initiation varied by sexual orientation group after adjusting for sex assigned at birth, race/ethnicity, cohort, and socioeconomic status.
Results
Compared to Straight adolescents, the risk of earlier-onset of ENDS use was higher among mobile individuals (HR = 1.43, 95% CI: 1.12 to 1.83) and LGB individuals (HR = 1.49, 95% CI: 1.13 to 1.98), respectively, after adjusting for sociodemographic risk factors. Differences between Straight adolescents and LGB/mobile individuals became more pronounced with increasing age.
Conclusion
Analyzing sexual mobility overtime is necessary for understanding the risk associated with youth ENDS initiation and subsequent use.
Implications
Future research should use more accurate sexual orientation assessments to explore further the relationship between sexual orientation mobility and early-onset Electronic Nicotine Delivering Systems (ENDS) use. Understanding the implications of sexual orientation mobility on ENDS initiation will be critical for developing inclusive public health programs aimed at preventing or delaying ENDS use and for providing practical recommendations at state and local levels.
Introduction
As the consumption of combustible cigarettes among youth in the United States (US) has declined over the decade, the use of Electronic Nicotine Delivering Systems (ENDS) or electronic cigarettes (e-cigarettes) has seen a drastic increase. Since 2014, ENDS have been the most commonly reported tobacco product currently used by youth; 16.6% and 34.5% of 8th and 12th graders reported past 30-day vaping in 2020, respectively.1 Apart from being detrimental to adolescent health due to the long-term neurobiological alterations associated with nicotine exposure,2,3 ENDS have also been associated with e-cigarette or vaping product use associated lung injury (EVALI) outbreak, which began in 2019.4 The clinical variability among adolescents diagnosed with EVALI can range from minimal or no supplemental oxygenation to invasive mechanical ventilation, admission to the intensive care unit, and death.5 While 82% of patients hospitalized with EVALI cases reported by the Centers for Disease Control and Prevention (CDC)4 were associated with tetrahydrocannabinol (THC)-containing product use, 57% of these patients reported using any nicotine-containing products, which cannot rule out the potential contribution of non-THC–containing products, such nicotine, in EVALI cases.
The overall consumption of tobacco products is disproportionately high among sexual and gender minority (SGM) youth.6–9 Tobacco use serves as a coping mechanism for sexual minority individuals (i.e., those with non-heterosexual sexual orientations), as well as gender minority individuals (i.e., those whose genders do not match their assigned sex at birth) to contend with stressors like stigma, discrimination, prejudice, violence, internalized homophobia, identity concealment, and fear of identity disclosure.10,11
Three in 10 lesbian, gay male, and bisexual (LGB) youth report current ENDS use, which is 25% higher than their heterosexual counterparts.12 In a cross-sectional analysis of Texas college students’ data, SGM individuals reported earlier ENDS initiation than their heterosexual counterparts.13 However, in most of these ENDS research efforts, sexual orientation is assumed as a rigid trait, while in truth, it can be fluid and subject to changes at any point in a person’s lifetime. The Kinsey Reports,14,15 and other research efforts,16–23 have provided substantial evidence that sexual orientation can be considered a continuum rather than a fixed category. This may be particularly relevant to adolescence and young adulthood when developmental changes across a wide range of behaviors occur quickly.24 Hence, assessing self-reported sexual orientation at one point in time can lead to misclassification bias and incorrect research conclusions, as it fails to consider this potential for mobility or fluidity, particularly during adolescent years.20 Since the late-1990s, a great deal of research has emerged about the conscious process of sexual orientation questioning and development across adolescence and young adulthood.25–27 Despite some increase in research raising awareness that sexual orientation is not a dichotomous, permanent trait,17,23,26,28–30 long-term mobility remains under-investigated, and its association with ENDS use remains unacknowledged.
The Texas Adolescent Tobacco and Marketing Surveillance System (TATAMS) is a study of ENDS use among a population-based cohort of adolescents (n = 3907; N = 460 069) living in major metropolitan areas of Texas (Houston, San Antonio, Dallas, Austin, and Fort Worth). Since 2014, data on ENDS use behaviors have been collected every 6 months, and in 2016, measures specific to sexual orientation were added.31 Because of the longitudinal nature of this study with repeated assessments, it is possible to determine the stability or shifting of sexual orientation among enrollees, as well as how this relates to the onset of ENDS use. In addition, examining the age of initiation of ENDS use will be vital to inform the development of preventive interventions, as early-onset ENDS users are at higher risk of developing a regular use pattern and/or transitioning to combusted tobacco products.32 To our knowledge, this study is the first research effort examining sexual orientation mobility and ENDS initiation among a longitudinal cohort of school-aged adolescents transitioning into young adulthood.
Method
Study Design and Participants
The study is a secondary analysis of longitudinal data from the Texas Adolescent Tobacco and Marketing Surveillance system (TATAMS). In 2014–2015, TATAMS recruited three population-based cohorts of adolescents (n = 3907; N = 460 069) in major metropolitan areas of Texas (Houston, San Antonio, Dallas, Austin, and Fort Worth) using a complex, multistage probability design.31 Participants were in 8th, 10th, and 12th grades at Wave 5; then in 12th grade, 1, and 3 years post-high school at Wave 11. Retention rates across these surveys ranged from 70% to 86% and did not vary by cohort. Additional description of this methodology has been published elsewhere.31 A web-based survey was administered to all study participants at baseline and every six months thereafter. Active, informed consent was obtained from parents and students (minors were asked for their assent), approved by the Center for the Protection of Human Subjects at the University of Texas Health Science Center at Houston (HSC-SPH-13-0377).
This analysis only uses data from Wave 5 (Fall, 2016) through Wave 11 (Spring, 2020), as Wave 5 was the first survey that included questions specific to assessing sexual orientation. The eligible sample for this analysis included any participant who had no missing data on birthdates or survey dates were never ENDS users at baseline (i.e., Wave 5 or later waves) and reported their sexual orientation at least in two waves (n = 1712).
Measures
ENDS Initiation
Our dependent variable was ENDS initiation. At each Wave, participants were asked “Have you EVER used an electronic cigarette, vape pen, or e-hookah, even one or two puffs? Marijuana does not count.” The question was preceded by a descriptive text that provided examples of electronic cigarettes, including JUUL, along with a picture. ENDS initiation was defined among baseline never ENDS users who responded “Yes” to the question above at a subsequent wave (Wave 6 to Wave 11), independently of other tobacco product use.
Age of ENDS Initiation
The exact date of ENDS initiation for each subject was not available due to the study design. However, a lower and upper age (by weeks) bound were observed, between which the ever ENDS initiation may occur, leading to an interval-censored outcome. The lower bound was the age at the last wave that the subject reported never ENDS use, and the upper bound was the first wave that the subject reported ever ENDS use. For those who were never users at the last wave, the upper bound was set to infinity.
Sexual Orientation
Our primary independent variable was a single question on sexual orientation: “Do you consider yourself to be…?” (a) “Straight;” (b) “Lesbian, gay, or bisexual”; (c) “I don’t identify with either of these;” (d) “I don’t know;” or (e) “I would prefer not to say.” This question was asked on all surveys, except Wave 7 and Wave 8. Combining answers to this question across Waves, we stratified the study sample into mutually-exclusive groups: (1) Straight: those who reported “straight” at each wave (n = 1381), (2) Lesbian, Gay, Bisexual (LGB): those who reported “lesbian, gay, or bisexual” at each wave (n = 139), and (3) mobile: those who reported a combination of “straight” and/or “LGB” and/or “I would prefer not to say” across waves (n = 192). No participant responded “I don’t know” at any wave. Those answering “I don’t identify with either of these” were excluded from the analysis (n = 59), as this category may have a distinct meaning to the respondent and not necessarily indicate belonging to any sexual minority group.
Covariates
Additional variables were included in the analysis to describe the study sample and/or to control for potential confounding variables or provide precise estimates of effect. Demographic indicators included age (in years), sex at birth (male or female), race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, Other), cohort (8th, 10th, or 12th grade at Wave 5), place of birth (i.e., United States, Other), county of residence (i.e., Travis, Bear, Dallas, Tarrant, Harris), and self-reported socioeconomic status (SES). To assess SES, participants were asked “In terms of income, what best describes your family’s standard of living in the home where you live most of the time?” and the response options provided were “Very well off,” “Living comfortably,” “Just getting by,” “Nearly poor” and “Poor.” “Very well off” was categorized as “High SES.” “Living comfortably” was categorized as “Middle SES” and “Just getting by.” Finally, “Nearly poor” and “Poor” were combined to derive “Low SES.” We also evaluated past 30-day use of combustible tobacco products (Yes/No), smokeless tobacco (Yes/No), and alcohol (Yes/No).
Data Analysis
At baseline, descriptive statistics were generated for all variables. Chi-square tests were used to compare sociodemographic variables between the three subgroups (straight, LGB, mobile) according to participants’ sexual orientation. For comparing continuous variables, an analysis of variance (ANOVA) test was used (Table 1).
Table 1.
Baseline characteristics of never ENDSa users by sexual orientation (n = 1712)
| Characteristic | Total n (%) |
Straight (n = 1381) (%) |
LGBb (n = 1391) (%) |
Mobilec (n = 192) (%) |
p value |
|---|---|---|---|---|---|
| Age (mean, ±SD d ) | 16 (1.5) | 16 (1.5) | 15 (1.7) | 16 (1.5) | 0.012 |
| Prospective cohorts | 0.002 | ||||
| 8th | 551 (32) | 32 | 44 | 25 | |
| 10th | 617 (36) | 37 | 26 | 35 | |
| 12th | 544 (32) | 31 | 30 | 40 | |
| Sex assigned at birth | <0.001 | ||||
| Female | 1006 (59) | 56 | 75 | 69 | |
| Male | 706 (41) | 44 | 25 | 31 | |
| Race/ethnicity | 0.268 | ||||
| White | 529 (31) | 31 | 37 | 29 | |
| African American | 259 (15) | 16 | 9 | 14 | |
| Latinx | 619 (36) | 36 | 37 | 37 | |
| Othere | 305 (18) | 17 | 18 | 21 | |
| Self-reported SES f | <0.001 | ||||
| High | 379 (22) | 22 | 20 | 24 | |
| Middle | 1082 (63) | 65 | 54 | 56 | |
| Low | 246 (15) | 13 | 27 | 19 | |
| County of residence | 0.305 | ||||
| Harris (Houston) | 388 (23) | 22 | 24 | 24 | |
| Bexar (San Antonio) | 50 (3) | 3 | 4 | 4 | |
| Dallas (Dallas) | 208 (12) | 13 | 12 | 7 | |
| Travis (Austin) | 575 (33) | 33 | 39 | 35 | |
| Tarrant (Fort Worth) | 491 (29) | 29 | 22 | 30 |
aENDS: electronic nicotine delivery systems. Includes vape pens, e-hookah, hookah pens, MODS, tank systems, and e-cigars.
bLesbian, gay, bisexual.
cMobile: study participants who reported a combination of “straight” and/or “LGB” and/or “I would prefer not to say” across waves.
dStandard deviation.
eIncludes Asian, n = 174; American Indian or Alaska Native, n = 21; Native Hawaiian or Other Pacific Islander, n = 10; and other (not listed), n = 100.
fSocio-economic status
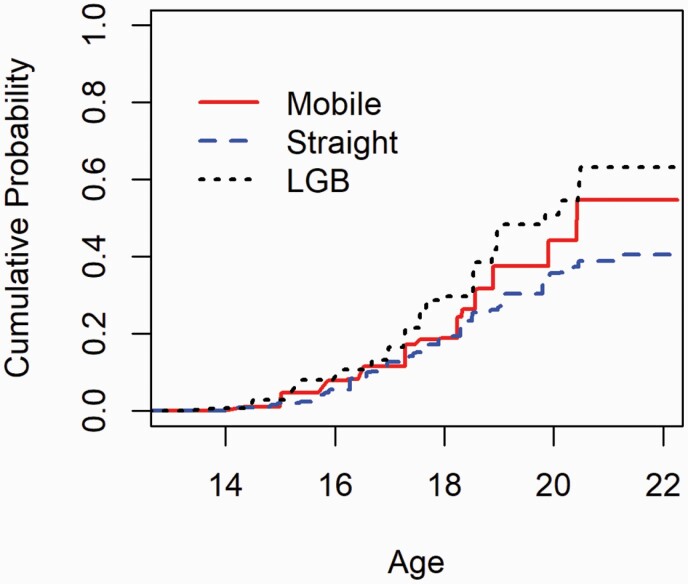
Nonparametric survival analyses for interval-censored data were implemented to estimate the hazards of ever ENDS initiation at different ages stratified by sexual orientation group (Figure 1). The generalized log-rank test was used to test the difference of the hazard of ever ENDS initiation among the sexual orientation groups.33
Figure 1.
Cumulative probabilities of ever ENDS use by age and sexual orientation, among never ENDS users at baseline (n = 1712).
We used Cox proportional hazards regression with interval-censored data and the piecewise constant baseline hazard function to test for differences in the age of initiation of ever ENDS use by sexual orientation group, adjusting for sociodemographic variables: sex assigned at birth, race/ethnicity, cohort, and SES.34 The hazard ratio (HR) and its 95% CI are reported (Table 2). All analyses were conducted using SAS. Significance was set at p < 0.05, and 95% CIs were reported throughout the paper. All p values were two-sided.
Table 2.
Differences in the age of initiation of ENDS use by sexual orientation.
| Stratified variable | Description | HRa | 95% CIb | |
|---|---|---|---|---|
| Unadjusted HR | ||||
| Mobilec vs. LGBd (ref) | 0.787 | 0.561 | 1.106 | |
| Mobile vs. Straight (ref) | 1.362 | 1.067 | 1.738 | |
| LGB vs. Straight (ref) | 1.730 | 1.315 | 2.274 | |
| Adjusted HRe | ||||
| Mobile vs. LGB (ref) | 0.956 | 0.677 | 1.349 | |
| Mobile vs. Straight (ref) | 1.427 | 1.116 | 1.828 | |
| LGB vs. Straight (ref) | 1.494 | 1.126 | 1.982 |
aHazard ratio.
bConfidence intervals.
cMobile: study participants who reported a combination of “straight” and/or “LGB” and/or “I would prefer not to say” across waves.
dLesbian, gay, bisexual.
eAdjusted by race/ethnicity, sex at birth, cohort, and SES. However, only race/ethnicity is reported as it was the only significant variable in the model.
Results
Sample Characteristics
A total of 1712 individuals were included in the study sample (Table 1). At baseline (2016), the average age of participants was 16 years; at Wave 11 (2020), the average age was 19 years. Regarding birth-assigned sex, most of the study participants were female assigned (59%). The majority self-identified as Latinx (36%) and White (31%), followed by African Americans (15%) and other races and ethnicities (18%). Almost two-thirds of the individuals (63%) were classified as middle class. One-third of the participants were recruited in the city of Austin (33%). The rest of the sample was recruited in Fort Worth (29%), Houston (23%), Dallas (12%), and San Antonio (3%).
Sexual Orientation
A total of 1381 (81%) of study participants consistently self-identified as Straight individuals, 139 (8%) consistently self-identified as LGB individuals, and 192 (11%) were categorized as mobile individuals whose sexual orientation changed across waves. Among mobile group, about 56% of participants moved from Straight to LGB and 13% moved from LGB to straight, while the rest of respondents in this group changed their response three or more times during the five points of data collection. Mobile and straight individuals were slightly older than LGB individuals (p = 0.012), and a larger proportion of mobile and LGB individuals were assigned female at birth compared to Straight individuals (p < 0.001). Across the groups (straight, LGB, mobile), statistical significance was reported for cohort (p = 0.002) and self-reported SES (p < 0.001).
ENDS Initiation
By age 18, 19% of Straight individuals, 30% of LGB individuals, and 19% of mobile individuals reported ENDS initiation (p < 0.001). The hazard plot (Figure 1) shows that compared to straight youth, the hazard of ever ENDS initiation peaked earlier for LGB individuals (HR = 1.73, 95% CI: 1.32 to 2.27) and mobile individuals (HR = 1.36, 95% CI: 1.07 to 1.74) throughout the whole study period, in unadjusted models. The null hypothesis (ENDS initiation’s hazards are equal across the groups: straight, LGB, mobile) was rejected (p < 0.001), and these differences between groups increased over the observation period, from 13 years old through the age of 22.
Use of Other Tobacco Products and Alcohol Consumption
Since very few of these individuals reported past 30-day use of combustible tobacco products (0.4%), past 30-day use of smokeless tobacco (0.2%), and past 30-day alcohol consumption (8%) at baseline (Wave 5), these variables were not included in further analyses.
Potential Predictors of ENDS Initiation
The results from the Cox regression analysis showed that after adjusting for sex assigned at birth, race/ethnicity, prospective cohort, and SES, the onset of ENDS use occurred at earlier ages among mobile individuals (HR = 1.43, 95% CI: 1.12 to 1.83) and LGB individuals (HR = 1.49, 95% CI: 1.13 to 1.98), compared to straight adolescents.
Discussion
Since 2014, ENDS have become the most commonly used tobacco product reported by youth, surpassing traditional cigarette use.35 Previous reports assessing the prevalence of ever ENDS use among youth have indicated that those identified as lesbian, gay, bisexual, and queer/questioning youth vape at higher rates than their heterosexual counterparts.6,13,36,37 In the current study, we expanded upon the existing scientific literature by examining ENDS initiation prospectively to account for changes in individuals’ patterns of sexual orientation over time.
Our work provides evidence that over the study period and compared to straight subjects, the hazard of becoming an ENDS user peaked earlier not only for LGB adolescents and youth, but also for mobile individuals who experienced at least one change in sexual orientation over time. Further, this risk difference was statistically significant even after accounting for potential confounders. Findings of this research effort shed light on the potential misclassification of at-risk populations when sexual orientation data is not regularly collected and accurately recorded, which ultimately may underestimate the true risk among mobile individuals, but also negatively impact the effectiveness of any ENDS use prevention program among adolescents and young adults who are particularly prone to experience changes in their sexual orientation (e.g., attraction, behavior, and identity) through adulthood.
In our sample, while 81% of the study participants consistently self-identified as Straight individuals (81%) and 8% as LGB youth, 11% prospectively reported sexual orientation mobility across waves. This clearly indicates that defining sexual minority groups based on a single measure of sexual orientation at one point in time may lead to misidentification and underreporting. For research purposes, placing the sexual orientation question around behavior items rather than among demographics could increase data collection accuracy and decrease response bias.38 However, further testing should be conducted among adolescents and youth to determine best practices for placing, structuring, and wording sexual orientation and gender identity questions; understanding how these items perform; and determining levels of nonresponse across subgroups. In any case, routinely documenting sexual orientation at every available opportunity (e.g., study assessments, clinical visits, etc.) seems to be a necessary first step to lay the ground work for effectively identifying vulnerable groups, so as to increase the effectiveness of tobacco prevention and control programs.
Research has begun to study differences in certain health conditions by individuals’ changes in same-sex or other-sex desire across both short-term and long-term periods.20,39,40 In a cross-sectional study conducted among adult individuals, shifts in the directionality of sexual orientation during the lifetime were significantly associated with adverse mental health outcomes such as stress, anxiety, and depression.41 In a cohort study from a nationally representative sample, changing sexual orientation across waves was associated with cigarette smoking initiation and current smoking.42 While there is compelling evidence of the association between mental health problems and ENDS use among adolescents and young adults,43,44 sexual orientation changes over time in this particular vulnerable population is not well-established. Therefore, sexual orientation mobility may present more of a challenge for ENDS prevention and control programs targeting youth.
A web-based search conducted in 2020 by Liu et al. identified eight ENDS prevention programs, seven ENDS cessation programs, and one program that addressed both ENDS prevention and cessation among adolescents. Most of these programs have shown promising results at changing adolescent perceptions and behavior about e-cigarette use.45 However, the effectiveness of these programs among SGM groups remains unknown. In 2016, the US Food and Drug Administration (FDA) launched “This Free Life” campaign through out-of-home advertising (e.g., billboards, print media, and events), social media platforms and influencers to prevent and reduce tobacco consumption among SGM adults aged 18–24.46 This large-scale public educational campaign proved to elevate the awareness of the health damage caused by tobacco products, including ENDS, among SGM young adults. However, similar educational efforts for SGM adolescents transitioning into young adulthood are lacking. Therefore, our findings provide relevant information that can inform the design of evidence-based interventions targeting SGM teens and youth.
However, this study had a few limitations. We did not consider ENDS use pattern (daily vs. nondaily use) or distinguish between different types of ENDS products (e.g., cig-a-like, vape pen, pod, mod, among others)47 in this analysis, given limited sample size. Therefore, differences in ENDS use patterns after initiation and product type might differ by sexual orientation. This should be explored in future research. Due to a lack of sexual orientation data collection in the TATAMS study between Waves 1 and 4, our sample was limited to respondents participating in Wave 5 or later waves. Also, we did not include in the survival models past use of combustible tobacco products, smokeless tobacco, or past 30-day alcohol consumption due to low reporting among study participants at baseline.
Given that most ENDS users are at higher risk of becoming multiple tobacco users (ENDS users who simultaneously use any other tobacco product) and that multiple tobacco use may reinforce nicotine addiction,48 it is important to investigate further the link of these behaviors with ENDS use uptake and/or progression, especially by sexual orientation. In addition, findings are limited to adolescents in Texas and may not generalize to other geographic locations. While the population in Texas has become increasingly urban, a comprehensive national report indicates that between 15% and 20% of sexual and gender minority groups in the US live in rural areas. These individuals may experience discrimination and stress substantially differently from their urban counterparts due to “the [relative] lack of community, resource, and services in rural areas.” 49 Our results are also limited to LGB adolescents and youth, not necessarily encompassing all sexual minority groups with a non-heterosexual sexual orientation. Also, future longitudinal studies with larger samples are needed to better differentiate the directionality of sexual orientation mobility among adolescents and youth, as well as the timing, frequency, and duration of those changes over the observation period. Finally, there could be significant intragroup differences in early ENDS initiation among study participants categorized in the LGB group, indicating the need for enhanced research efforts with large study samples that broaden the possible data range and form a better analysis picture for ENDS initiation among lesbian, bisexual female, gay, and bisexual male adolescents and youth.
Notwithstanding the above limitations, to the best of our knowledge, this is the first study examining whether ENDS initiation differs across subgroups defined by their sexual orientation- straight, LGB, and mobile individuals- in a contemporary sample of adolescents (13–22 years of age) over time (2016-2020). Understanding the implications of sexual orientation mobility on early-onset of ENDS use will be critical for developing inclusive public health programs aimed at preventing or delaying ENDS use and for providing practical recommendations at state and local levels.
Supplementary Material
A Contributorship Form detailing each author’s specific involvement with this content, as well as any supplementary data, are available online at https://academic.oup.com/ntr.
Since the data collection process is still ongoing, research data from The Texas Adolescent Tobacco and Marketing Surveillance Study (TATAMS) 2.0 cannot be shared.
Acknowledgments
This work was supported by grant number 1 P50 CA180906 from the National Cancer Institute and the Food and Drug Administration Center for Tobacco Products (FDA CTP). This project is funded by the National Cancer Institute (NCI) through the grant [R01-CA239097] to Principal Investigator Melissa Harrell. It has also been partially supported by the NCI under award number 1K22CA237639 to Principal Investigator Irene Tami-Maury. The content is solely the authors’ responsibility and does not necessarily represent the official views of the National Institutes of Health or the Food and Drug Administration.
Declaration of Interests
Dr Melissa B. Harrell is a consultant in litigation involving the vaping industry. Other authors have no conflicts of interest to disclose.
References
- 1. Monitoring the Future 2020 Survey Results. https://www.drugabuse.gov/drug-topics/related-topics/trends-statistics/infographics/monitoring-future-2020-survey-results. Accessed February 12, 2021.
- 2. Smith RF, McDonald CG, Bergstrom HC, Ehlinger DG, Brielmaier JM. Adolescent nicotine induces persisting changes in development of neural connectivity. Neurosci Biobehav Rev. 2015;55:432–443. [DOI] [PubMed] [Google Scholar]
- 3. Thorpe HHA, Hamidullah S, Jenkins BW, Khokhar JY. Adolescent neurodevelopment and substance use: Receptor expression and behavioral consequences. Pharmacol Ther. 2020;206:107431. [DOI] [PubMed] [Google Scholar]
- 4. Krishnasamy VP, Hallowell BD, Ko JY, et al. ; Lung Injury Response Epidemiology/Surveillance Task Force. Update: characteristics of a nationwide outbreak of E-cigarette, or vaping, product use-associated lung injury – United States, August 2019–January 2020. MMWR Morb Mortal Wkly Rep. 2020;69(3):90–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rao DR, Maple KL, Dettori A, et al. Clinical features of e-cigarette, or vaping, product use–associated lung injury in teenagers. Pediatrics. 2020;146(1):e20194104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dai H. Tobacco product use among lesbian, gay, and bisexual adolescents. Pediatrics. 2017;139(4):e20163276. [DOI] [PubMed] [Google Scholar]
- 7. Johnson SE, Holder-Hayes E, Tessman GK, King BA, Alexander T, Zhao X. Tobacco product use among sexual minority adults: findings from the 2012–2013 national adult tobacco survey. Am J Prev Med. 2016;50(4):e91–e100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wang TW, Asman K, Gentzke AS, et al. Tobacco product use among adults – United States, 2017. MMWR Morb Mortal Wkly Rep. 2018;67(44):1225–1232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Tamí-Maury I, Lin MT, Lapham HL, et al. A pilot study to assess tobacco use among sexual minorities in Houston, Texas. Am J Addict. 2015;24(5):391–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Livingston NA, Flentje A, Heck NC, Szalda-Petree A, Cochran BN. Ecological momentary assessment of daily discrimination experiences and nicotine, alcohol, and drug use among sexual and gender minority individuals. J Consult Clin Psychol. 2017;85(12):1131–1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Rosario M, Schrimshaw EW, Hunter J. Disclosure of sexual orientation and subsequent substance use and abuse among lesbian, gay, and bisexual youths: critical role of disclosure reactions. Psychol Addict Behav. 2009;23(1):175–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kann L, Olsen EOM, McManus T, et al. Sexual identity, sex of sexual contacts, and health-related behaviors among students in grades 9–12—United States and selected sites, 2015. MMWR Morb Mortal Wkly Rep., Surveill. Summ. 2016;65(9):1–202. [DOI] [PubMed] [Google Scholar]
- 13. Hinds JT, Loukas A, Perry CL. Sexual and gender minority college students and tobacco use in Texas. Nicotine Tob Res. 2018;20(3):383–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kinsey AC, Pomeroy WR, Martin CE. Sexual behavior in the human male. 1948. Am J Public Health. 2003;93(6):894–898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kinsey AC, Pomeroy WB, Martin CE, Gebhard PH.. Sexual Behavior in the Human Female. Bloomington and Indianapolis: Indiana University Press; 1998. [Google Scholar]
- 16. Ott MQ, Corliss HL, Wypij D, Rosario M, Austin SB. Stability and change in self-reported sexual orientation identity in young people: application of mobility metrics. Arch Sex Behav. 2011;40(3):519–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Savin-Williams RC, Ream GL. Prevalence and stability of sexual orientation components during adolescence and young adulthood. Arch Sex Behav. 2007;36(3):385–394. [DOI] [PubMed] [Google Scholar]
- 18. Dickson N, Paul C, Herbison P. Same-sex attraction in a birth cohort: prevalence and persistence in early adulthood. Soc Sci Med. 2003;56(8):1607–1615. [DOI] [PubMed] [Google Scholar]
- 19. Graber JA, Archibald AB. Psychosocial change at puberty and beyond: Understanding adolescent sexuality and sexual orientation. In: D’Augelli A.R. and Patterson C.J., eds. Lesbian, Gay, and Bisexual Identities and Youth: Psychological Perspectives. New York: Oxford University Press; 2001:3–26. [Google Scholar]
- 20. Ott MQ, Wypij D, Corliss HL, et al. Repeated changes in reported sexual orientation identity linked to substance use behaviors in youth. J Adolesc Health. 2013;52(4):465–472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Rosario M, Schrimshaw EW, Hunter J. Different patterns of sexual identity development over time: implications for the psychological adjustment of lesbian, gay, and bisexual youths. J Sex Res. 2011;48(1):3–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mock SE, Eibach RP. Stability and change in sexual orientation identity over a 10-year period in adulthood. Arch Sex Behav. 2012;41(3):641–648. [DOI] [PubMed] [Google Scholar]
- 23. Rosario M, Schrimshaw EW, Hunter J, Braun L. Sexual identity development among gay, lesbian, and bisexual youths: consistency and change over time. J Sex Res. 2006;43(1):46–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Arnett JJ. Emerging adulthood. A theory of development from the late teens through the twenties. Am Psychol. 2000;55(5):469–480. [PubMed] [Google Scholar]
- 25. Saewyc EM. Research on adolescent sexual orientation: development, health disparities, stigma and resilience. J Res Adolesc. 2011;21(1):256–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Diamond LM. Development of sexual orientation among adolescent and young adult women. Dev Psychol. 1998;34(5):1085–1095. [DOI] [PubMed] [Google Scholar]
- 27. Rotheram-Borus MJ, Gwadz M, Fernandez MI, Srinivasan S. Timing of HIV interventions on reductions in sexual risk among adolescents. Am J Community Psychol. 1998;26(1):73–96. [DOI] [PubMed] [Google Scholar]
- 28. Diamond LM. Sexual identity, attractions, and behavior among young sexual-minority women over a 2-year period. Dev Psychol. 2000;36(2):241–250. [DOI] [PubMed] [Google Scholar]
- 29. Diamond LM. Was it a phase? Young women’s relinquishment of lesbian/bisexual identities over a 5-year period. J Pers Soc Psychol. 2003;84(2):352–364. [PubMed] [Google Scholar]
- 30. Diamond LM. Female bisexuality from adolescence to adulthood: results from a 10-year longitudinal study. Dev Psychol. 2008;44(1):5–14. [DOI] [PubMed] [Google Scholar]
- 31. Pérez A, Harrell MB, Malkani RI, et al. Texas adolescent tobacco and marketing surveillance system’s design. Tob Regul Sci. 2017;3(2):151–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Berry KM, Fetterman JL, Benjamin EJ, et al. Association of electronic cigarette use with subsequent initiation of tobacco cigarettes in US Youths. JAMA Netw Open. 2019;2(2):e187794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Sun J. A non-parametric test for interval-censored failure time data with application to AIDS studies. Stat Med. 1996;15(13):1387–1395. [DOI] [PubMed] [Google Scholar]
- 34. Finkelstein DM. A proportional hazards model for interval-censored failure time data. Biometrics. 1986:845–854. [PubMed] [Google Scholar]
- 35. U.S. Department of Health and Human Services. E-Cigarette Use Among Youth and Young Adults. A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2016. [Google Scholar]
- 36. Kann L, McManus T, Harris WA, et al. Youth risk behavior surveillance – United States, 2017. MMWR Surveill Summ. 2018;67(8):1–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Johnson SE, O’Brien EK, Coleman B, Tessman GK, Hoffman L, Delahanty J. Sexual and gender minority US youth tobacco use: Population Assessment of Tobacco and Health (PATH) Study Wave 3, 2015–2016. Am J Prev Med. 2019;57(2):256–261. [DOI] [PubMed] [Google Scholar]
- 38. American Psychological Association. Resolution on Data about Sexual Orientation and Gender Identity . http://www.apa.org/about/policy/data-sexual-orientation.aspx. Accessed July 20, 2021.
- 39. Everett B. Sexual orientation identity change and depressive symptoms: a longitudinal analysis. J Health Soc Behav. 2015;56(1):37–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Fish JN, Pasley K. Sexual (Minority) trajectories, mental health, and alcohol use: a longitudinal study of youth as they transition to adulthood. J Youth Adolesc. 2015;44(8):1508–1527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Katz-Wise SL, Williams DN, Keo-Meier CL, Budge SL, Pardo S, Sharp C. Longitudinal associations of sexual fluidity and health in transgender men and cisgender women and men. Psychol Sex Orientat Gend Divers. 2017;4(4):460–471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Harlow AF, Lundberg D, Raifman JR, et al. Association of coming out as lesbian, gay, and bisexual+ and risk of cigarette smoking in a nationally representative sample of youth and young adults. JAMA Pediatr. 2021;175(1):56–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Becker TD, Arnold MK, Ro V, Martin L, Rice TR. Systematic review of electronic cigarette use (vaping) and mental health comorbidity among adolescents and young adults. Nicotine Tobacco Res. 2020;23(3):415–425. [DOI] [PubMed] [Google Scholar]
- 44. Tobore TO. On the potential harmful effects of E-Cigarettes (EC) on the developing brain: the relationship between vaping-induced oxidative stress and adolescent/young adults social maladjustment. J Adolesc. 2019;76:202–209. [DOI] [PubMed] [Google Scholar]
- 45. Liu J, Gaiha SM, Halpern-Felsher B. A breath of knowledge: overview of current adolescent e-cigarette prevention and cessation programs. Curr Addict Rep. 2020;7(4):520–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Hoffman L, Delahanty J. To speak to me, address us: Insights from LGBT Young Adults to inform public education campaigns. Health Promot Pract. 2020;22(5):641–648. [DOI] [PubMed] [Google Scholar]
- 47. Sumbe A, Clendennen SL, Opara SC, et al. ENDS Device type and initiation of combustible tobacco products among adolescents. Nicotine Tob Res. 2020;23(3):479–486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Soneji S, Sargent J, Tanski S. Multiple tobacco product use among US adolescents and young adults. Tob Control. 2016;25(2):174–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Where We Call Home: LGBT People in Rural America. Movement Advancement Project ; 2019. www.lgbtmap.org/rural-lgbt. Accessed July 5, 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.