Abstract
Purpose
A metastatic cancer diagnosis is associated with high levels of distress in patients and caregivers, which may be alleviated by mindfulness interventions. Research on scalable, tailored, online mindfulness training programs is needed. We sought to test the feasibility and acceptability of a remotely delivered 8-week mindfulness-based intervention, Being Present 2.0 (BP2.0).
Methods
We performed a single-arm feasibility study of BP2.0 among patients with any metastatic gastrointestinal cancer receiving chemotherapy, with or without an informal caregiver. Participants were instructed to practice mindfulness using pre-recorded guided meditations 5 times per week using a study-specific website and to attend a weekly live, interactive virtual meeting facilitated by a trained instructor. The web-based platform enabled direct measurement of adherence.
Results
The study enrolled 46 of 74 (62%) patients contacted, together with 23 caregivers (69 participants total), from May to October 2018. Median patient age was 52 (range 20-70 years), 39% were male, 67% non-Hispanic white, 65% had colorectal cancer, and 78% lived outside of San Francisco. The top reasons cited for participation were to reduce stress/anxiety and learn how to meditate. Mean baseline National Comprehensive Cancer Network Distress Thermometer (NCCN DT) scores were 4.7 (patients) and 5.8 (caregivers). The study discontinuation rate was 20% (eight patients and six caregivers). Among the remaining 55 participants, 43 (78%) listened to at least one audio recording and/or attended at least one virtual meeting, although adherence data was incomplete. The retention rate was 71%, with 39 participants completing at least one follow-up assessment. In post-intervention qualitative interviews, 88% of respondents reported a positive experience. Compared to baseline, participants reported significantly reduced post-intervention NCCN DT scores (mean 3.1; P = .012).
Conclusion
The BP2.0 online mindfulness-based program is feasible and acceptable for patients with metastatic gastrointestinal cancer and caregivers. These results will guide plans for a follow-up efficacy study. ClinicalTrials.gov Identifier: NCT03528863.
Keywords: mindfulness, oncology, stress, integrative medicine, coping, home-based
Trial Registration; ClinicalTrials.gov Identifier: NCT03528863
Introduction
Patients living with metastatic cancer often experience high levels of psychological distress,1-5 leading to impairments in mental, emotional, and physical wellbeing. Distress has been linked to an increase in cancer-specific mortality and decreased overall survival.2,6-10 Due to the clinical significance of cancer-related distress, mandatory distress screening guidelines have been implemented in accredited cancer centers.5,11 The distress experienced by patients living with cancer can extend to their caregivers, negatively impacting caregiver health and quality of life.4,12-19 To decrease distress in cancer patients, it is important to also address the distress experienced by their caregivers.6,17,20 Mind–body therapies, specifically Mindfulness-based Stress Reduction (MBSR), have been shown to effectively reduce distress levels among cancer patients and survivors,1,18,21-24 particularly in those with breast cancer.25-28 However, there are limited data on the effectiveness of mindfulness therapies in patients with diagnoses other than breast cancer, patients with metastatic cancer, male 23 and non-white patients, and caregivers. In addition to being an understudied population in mindfulness-based interventions (MBIs), patients with gastrointestinal cancers are of interest because of high prevalence and mortality rates—more people in the United States die each year from gastrointestinal cancers than any other type of cancer. 29 In a pooled analysis of 16 prospective cohort studies that accounted for reverse causality, high psychological distress scores were an independent predictor of site-specific cancer mortality in patients with colorectal, pancreas, and esophageal malignancies. 10
Established MBIs frequently rely on in-person instruction and extended daily home practice, which can be challenging for patients with advanced cancer and their caregivers due to the burden of illness and illness-related responsibilities. 30 There is growing evidence that remotely delivered MBIs can be a feasible alternative to in-person programs to reduce distress levels among cancer patients.31-37 Our previous Being Present pilot study (BP1.0), demonstrated the promise of an audio-based mindfulness meditation program in reducing distress and anxiety in caregivers and patients with metastatic colorectal cancer while receiving chemotherapy. 16 However, there were also lessons learned that warranted a follow-up pilot study. Major limitations of BP1.0 included technological difficulties associated with use of MP3 players, reliance on participant-reported data to estimate intervention adherence, and the lack of an instructor to provide guidance during the 8-week meditation program. Pilot data collected during BP1.0 demonstrated that >90% of participants used a smartphone and email at least daily, irrespective of age. In post-study interviews, 62% of respondents indicated a preference for a smartphone app or web-based program. Some BP1.0 participants also requested guided meditations specific to their experience of cancer, as a patient or as a caregiver. 16 Similarities and differences between BP2.0 and BP1.0 are summarized in Supplementary Table S1.
The primary objective of this single-arm pilot study was to evaluate the feasibility and acceptability of an 8-week mindfulness-based program—delivered by web-based platform and including a weekly live interactive virtual meeting—among patients with any metastatic gastrointestinal cancer and their caregivers.
Methods
Being Present 2.0 Setting and Participants
The referral base for this study was the University of California, San Francisco (UCSF) Helen Diller Family Comprehensive Cancer Center (HDFCCC) Gastrointestinal Oncology Clinic. UCSF HDFCCC has a large catchment area covering all of Northern and Central California. The study protocol was approved by the UCSF Human Research Protection Program Institutional Review Board (18-24261).
Patient-specific eligibility requirements included a diagnosis of any metastatic gastrointestinal cancer; the expectation to receive chemotherapy for at least 12 weeks from the time of recruitment; a life expectancy of ≥6 months; and Eastern Cooperative Group (ECOG) Performance Status of ≤2. Caregivers (i.e., a family member or friend) were eligible if paired with a participating patient. All participants were required to be English speaking, with daily access to a mobile phone and internet service. Having a current meditation practice (>2 episodes or >1 hour total, weekly) or simultaneous enrollment in a stress reduction program were exclusion criteria. A protocol amendment (February 4, 2018) allowed caregivers with an existing meditation practice to participate to support the patients.
Potentially eligible patients were identified by reviewing the medical records of patients scheduled to be seen in the Gastrointestinal Oncology Clinic on a weekly basis. Patients were recruited in-person or by letter. A research coordinator reached out to patients and caregivers in-person, via email, or by phone. Upon consent, each participant was given a unique user log-in to gain access to the study website. Participants provided written informed consent prior to study procedures (Supplementary Table S2).
Web-Based Mindfulness Meditation Intervention Design
BP2.0 was a single-arm pilot feasibility study designed to address the limitations from BP1.0 by featuring a web-based platform that consolidates all study resources into an interface that directly measures adherence and offers live online sessions with a trained meditation instructor. A BP2.0 Advisory Council, comprised patients and caregivers, was convened to provide consultation during the BP2.0 intervention design process. Advisory Council members were asked to review three meditation scripts tailored for patients or caregivers, respectively, including a meditation explicitly addressing the patient or caregiver experience and a nature-themed guided imagery script. Feedback was solicited via email regarding overall impressions, rank order by preference, and responses to specific questions. Advisory Council members also participated in beta testing the web- and Zoom-based platforms.
Website
We chose a web-platform rather than a mobile application as it was more efficient and economical to develop, easier to update, and not subject to device incompatibilities. The web-based program also allows for passive collection of participant adherence data through website data capture instead of relying on participant self-reporting. 16 Separate patient and caregiver skins were designed.
Guided Meditations
The 8-week cumulative mindfulness-based program started with mindful breathing exercises in weeks 1–2; expanded to encompass various forms of body awareness, attention awareness and finally, loving kindness and self-guided meditations in week 8 (Supplementary Table S3). The meditation exercises were written by J.P.R., a clinical psychology-researcher with expertise in the development and implementation of mindfulness interventions, with contributions from E.E. and C.E.A. The BP2.0 Advisory Council provided feedback on new patient- and caregiver-specific mindfulness meditation exercises, which was incorporated into the final content. Additional suggestions from BP1.0 participants that were incorporated into BP2.0 included building on favorite tracks (breathing exercises and progressive muscle relaxation were each expanded into two tracks) and providing longer and shorter track options. All tracks were recorded in a female and a male voice and were engineered for uniform length per track. The median track length was 17.3 minutes (range 10–30 minutes). Participants were instructed to listen to and practice with one track per day, at least 5 days per week, for 8 weeks (40 plays total).
Webinars
To provide participants with real-time guidance, BP2.0 integrated weekly, group-based interactive virtual meetings (webinars) facilitated by a meditation instructor (details in Supplemental Methods). Objectives of the webinars were to enable participants to experience meditation in a group setting; to provide teaching on helpful qualities for the cultivation of mindfulness; to address questions related to the teaching content or establishment of a meditation practice; and to promote adherence through a sense of accountability. The standardized 8-session webinar curriculum was developed and manualized by E.E. The curriculum builds upon the BP1.0 themes (Supplementary Table S4). The live weekly webinars were held every Tuesday evening from 7:30–8:30 pm (PST) via an encrypted Zoom Video Communications platform. For privacy, participants had the option to use an alias and turn their video off. The webinars were hosted by a trained meditation teacher. Each session started with roll call, followed by approximately 15 minutes of teaching, 20 minutes of guided meditation, and time for questions and answers. Two trained meditation teachers alternated leading the webinars each week.
Reminders about upcoming webinar sessions were sent via text message and email. The webinars were recorded and shared on the website with current participants to allow them to replay or make up missed sessions. The webinars were offered continuously for the duration of the study. Participants could enter at any point in the webinar cycle.
Text Messages and Emails
Similar to in BP1.0, participants received daily text messages and weekly emails. 16 The text messages contained motivational quotes and tips, serving as practice reminders to help maintain the container of the 8-week program (Supplementary Table S5). Emails contained reminders of practice instructions and/or links to survey assessments. Throughout the program participants were given suggestions for how to incorporate meditation and other mindfulness practices into daily living (see examples in Supplementary Table S5). Upon completion of the program, participants were provided with a list of Resources for Continued Practice in addition to ongoing access to the recordings from BP2.0.
Study Objectives and Assessments
The primary objective of the BP2.0 study was to assess feasibility and acceptability, for which the endpoints were: recruitment rate; reasons for ineligibility or refusal to participate; rates and causes of attrition; level of adherence to the practice instructions and the retention rate. For the sample size calculation, an attrition rate of 23% was anticipated based on BP1.0 16 and feasibility was based on a retention rate of ≥70% (i.e., ≥70% of participants completing any follow-up assessment). Qualitative information about acceptability and the overall intervention experience derived from semi-structured interviews.
The secondary objective was to estimate efficacy of the tailored, virtual mindfulness-based program, measured via responses on validated survey instruments, using a pretest-posttest design. Semi-structured exit interviews with participants were also used to estimate the potential for clinical benefit. Exploratory objectives were to evaluate for differences in feasibility, acceptability, and efficacy based on clinical and demographic characteristics; in caregivers vs patients; in patient-caregiver pairs vs unpaired patients; and based on level of adherence to the practice instructions.
Instruments
Upon enrollment, participants were asked to complete questionnaires in REDCap 38 (link sent via email). The baseline surveys included information on demographics, expectations, 39 symptoms, and wellbeing. The instruments included in the symptoms and wellbeing survey were: the National Comprehensive Cancer Network Distress thermometer (NCCN DT)40,41; National Institutes of Health Patient Reported Outcomes Measurement Information System (NIH PROMIS) Anxiety 4a, Depression 6a, Global Health—Mental 2a, Self-Efficacy for Managing Emotions 4a (baseline only), and Sleep Disturbance 4a; Five Facet Mindfulness Questionnaire Short Form (FFMQ-SF); and the “Are You at Peace?” one-item spiritual probe.42-44 At weeks 4 and 8, participants were asked to repeat the symptoms and wellbeing questionnaires and to provide feedback about the intervention in a study assessment survey. At weeks 3 and 6, participants were sent a single question survey to evaluate for potential adverse effects from study participation.
Qualitative Interviews
Interviews were requested with each study participant at baseline and after finishing the program (week 8). These recorded interviews were conducted either in person or over the phone. A semi-structured script was used for each interview to collect qualitative data regarding participants’ baseline expectations; experiences of the intervention; and plans for continued mindfulness meditation practice after completing the program (Supplemental Methods). Audio from the pre- and post-study interviews was professionally transcribed.
Adherence
Adherence data to recorded meditation practice was passively collected using Google Analytics when participants logged on to the website and played each track. Webinar attendance was logged using a roll call at the beginning of each session by the instructors. The research coordinator called participants to inquire about barriers to participation if their webinar attendance or meditation practice was low. Qualitative aspects of adherence were also addressed during the post-study interviews.
Analysis
Descriptive statistics were used to summarize demographics, clinicopathologic characteristics, baseline levels/sources of distress, and feasibility and acceptability endpoints. Frequency distributions and percentages were used to summarize categorical measures. Means (standard deviation, SD) and medians (range or interquartile range, IQR) were used to describe symmetric and skewed continuous measures. Baseline characteristics of evaluable and non-evaluable participants were compared using t-tests for continuous and Fisher’s exact tests for categorical measures. These methods were also used to analyze the survey data. Effect sizes were calculated for pre–post difference data as mean change over standard deviation of change.
Transcripts of the pre- and post-intervention interviews were coded using Atlas. ti software for qualitative data analysis by at least two investigators. Disputes in coding were resolved through discussion among three investigators. Qualitative thematic analysis of the interviews followed the framework method (Supplemental Methods).16,45 Thematic saturation was achieved.
Results
Advisory Council
The BP2.0 Advisory Council was composed of seven patients and seven caregivers, with an even balance of men and women. Advisory Council members had a range of prior meditation experiences, and all but one participant was involved in BP1.0. 16 Based on the impressions of meditation scripts and rankings received, we concluded that different meditations were appealing for different individuals and in different scenarios; therefore, revised versions of all of the guided meditations were included as options in the final BP2.0 program. The Advisory Council confirmed the importance of offering separate patient- and caregiver-specific meditations. There was remarkable consistency in comments from patients and from caregivers, delineating the overlapping yet distinct viewpoints of each group. Comments from patients focused on thinking positively, including cultivating joy, gratitude, and healing/wellness. For caregivers, cultivation of ease, peace, and gratitude was more accessible than wishes for joy/happiness or health. Another theme was that caregivers consistently sought a self-care focus.
Web-Based Mindfulness Meditation Intervention
Recruitment and Retention
Recruitment occurred over five months, from May to October 2018. Seventy-four patients were approached about the study, with prioritization of in-person introductions (81%) rather than invitation by mail (19%) (Supplementary Figure S1). Reasons for declining participation included feeling overstretched or having alternate strategies for coping. Ten patients expressed interest in participating but were ineligible because they were not actively receiving chemotherapy for a metastatic gastrointestinal cancer, or they had an active meditation practice. Non-English speakers were pre-screened out.
Consent to participate was obtained from 46 eligible patients (72% of those invited). Among consented patients, the median age was 52 years (range 20–70), 39% were male; and 67% identified as non-Hispanic white (Table 1). Two-thirds of patients had a diagnosis of metastatic colorectal cancer and 78% resided outside of San Francisco. Of the 46 patients who participated, 23 (50%) had a caregiver who also consented to participate.
Table 1.
Baseline demographic and clinical characteristics.
| Patients (N) | 46 |
| Gender, male (N, %) | 18 (39.1) |
| Age, years (median, range) | 52 (20–70) |
| Race (N, %) a | |
| White | 35 (76.1) |
| Asian | 9 (19.6) |
| Other/unknown | 3 (6.5) |
| Black | 1 (2.2) |
| Ethnicity, Latino, or Hispanic (N, %) | 4 (8.7) |
| Primary tumor site (N, %) | |
| Colorectal | 30 (65.2) |
| Appendix/small bowel | 6 (13.0) |
| Cholangiocarcinoma/gallbladder | 4 (8.7) |
| Pancreas | 3 (6.5) |
| Gastric/esophageal | 2 (4.4) |
| Anal | 1 (2.2) |
| Time since diagnosis, months (median, range) | 10 (2-235) |
| Metastatic at diagnosis (N, %) | 36 (78.3) |
| Treated with curative intent (N, %) | 4 (8.7) |
| Line of chemotherapy (N, %) | |
| First | 24 (52.2) |
| Second | 8 (17.4) |
| Third | 9 (19.5) |
| Fourth–sixth | 5 (10.9) |
| New chemotherapy start (N, %) b | 13 (28.3) |
| Hospitalization during BP2.0 | 8 (17.4) |
| Survival status as of September 1, 2019 c | |
| Alive | 29 (63.0) |
| Died | 17 (37.0) |
| Time to death, months (median, range) d | 6 (1-13) |
| Distance from home to UCSF, miles (median, range) | 25 (1-2340) |
| Lives outside San Francisco (N, %) | 36 (78.3) |
| Caregivers (N) | 23 |
| Gender, male (N, %) | 12 (52.2) |
| Caregiver relationship to patient | |
| Spouse/partner | 15 (65.2) |
| Parent | 4 (17.4) |
| Sibling | 3 (13.0) |
| Friend | 1 (4.4) |
aMultiple races selected by some patients.
bNew chemotherapy start is defined as starting a new regimen within 1 month of enrolling in BP2.0.
cMedian follow-up time: 14.1 months (range 10.4–15.9 months).
dTime in months between consent to participate in BP2.0 and death.
Overall, 54 of the 69 total participants completed the baseline demographic survey (78% response rate). Among respondents, the median education level was college graduate (Bachelor’s degree) and median household income bracket was $100,000 to $199,999; 39% of patients and 73% of caregivers were working at least part-time (Supplementary Table S6). The most common caregiver relationship was significant other, 15/23 (65%); half of participating caregivers were male (Table 1). Following the study amendment relaxing the eligibility criteria for caregivers, two caregivers with an existing meditation practice enrolled in BP2.0.
The attrition rate was 20% (14/69); eight patients and six caregivers discontinued study participation early. Of those who discontinued, five patients had progressive, late stage disease, living a median of 6 months (range 1–9 months) from the time of consent, and three patients initiating first line chemotherapy cited feeling overwhelmed (Supplementary Figure S1). Five caregivers who discontinued study participation were paired with these eight patients. One additional caregiver withdrew consent prior to intervention start due to time constraints. Clinical and demographic characteristics, as well as baseline distress scores, were similar in the early discontinuation and evaluable groups (Table 1).
Baseline Assessments
A baseline expectations survey was completed by 56 participants (41 patients and 15 caregivers), recording numerical ratings from 0 (“not at all helpful”) to 10 (“extremely helpful”). The median rating for “How helpful do you believe participating in Being Present will be for you overall?” was 8 [interquartile range (IQR): 7–9]. Ratings were similar among patients and caregivers, as well as for the more specific questions related to expected helpfulness for distress reduction and for managing mood and emotions (both mean 8, IQR: 6–9).
In pre-intervention interviews, the top reasons cited for participation were to learn a new skill and reduce stress/anxiety; 75% of caregivers reported joining to support a patient (Table 2 and Supplementary Table S6). Expectations or perceived benefits from study participation included gaining perspective or insight, social support, and stress management (Tables 2 and S7).41,46 Mean baseline NCCN DT scores were 4.7 [standard deviation (SD): 2.1, N = 42] in patients and 5.8 (SD: 2.1, N = 17) in caregivers, signifying clinically elevated distress levels.46,47 The top source of distress reported by 58 respondents, including 41 patients, was worry (78% overall; 83% of patients). Among caregivers (N = 17), worry was the second leading source of distress (64%), after family health issues, cited by 88%. The other sources of distress reported by over half of respondents were fears, sadness, fatigue, and sleep (Supplementary Table S8).
Table 2.
Quantitative analysis of qualitative data from pre-study interviews.
| Pre-study Interview Analysis (N, %) | Patients (N = 43) | Caregivers (N = 20) | Total (N = 63) |
|---|---|---|---|
| Prior meditation or related experience | |||
| Prior meditation exposure | 32 (74.4) | 13 (65.0) | 45 (71.4) |
| No prior related experience | 7 (16.3) | 4 (20.0) | 11 (17.5) |
| Reasons for participation | |||
| Learn a new skill | 17 (40.0) | 3 (15.0) | 20 (31.7) |
| Reduce anxiety/stress | 12 (28.0) | 7 (35.0) | 19 (30.2) |
| Curiosity | 10 (23.3) | 2 (10.0) | 12 (19.0) |
| Learn how to live with cancer | 9 (21.9) | 1 (5.0) | 10 (15.9) |
| Family/friend recommendation | 5 (11.6) | 1 (5.0) | 6 (9.5) |
| Find a more positive outlook | 5 (11.6) | 1 (5.0) | 6 (9.5) |
| Learn how to be present | 3 (7.0) | 1 (5.0) | 4 (6.3) |
| Find a community | 1 (2.3) | 0 (0.0) | 1 (1.6) |
| Caregiver joining to support patient | 15 (75.0) | ||
| Expectations/perceived benefits | |||
| Gain perspective or insight | 22 (51.2) | 8 (40.0) | 30 (47.6) |
| Social support | 20 (46.5) | 10 (50.0) | 30 (47.6) |
| Stress management | 16 (37.2) | 12 (60.0) | 28 (44.4) |
| Being in the moment | 12 (28.0) | 5 (25.0) | 17 (27.0) |
| Develop a structured practice | 10 (23.3) | 5 (25.0) | 15 (23.8) |
| Positive effect on cancer | 9 (21.9) | 1 (5.0) | 10 (15.9) |
| Pain relief | 6 (14.0) | 0 (0.0) | 6 (9.5) |
| Accept living with cancer | 4 (9.3) | 3 (15.0) | 7 (11.1) |
| Unsure/no expectations | 3 (7.0) | 1 (5.0) | 4 (6.3) |
| Anticipated challenges | |||
| Finding time | 12 (28.0) | 8 (40.0) | 20 (31.7) |
| Illness/fatigue | 5 (11.6) | 2 (10.0) | 7 (11.1) |
| Adherence | 4 (9.3) | 0 (0.0) | 4 (6.3) |
| Sharing in a group | 4 (9.3) | 3 (15.0) | 7 (11.1) |
| Discomfort with technology | 4 (9.3) | 2 (10.0) | 6 (9.5) |
| Perceived impact on communication/personal relationships | |||
| Improve personal relationships/communication | 27 (62.8) | 14 (70.0) | 41 (65.1) |
| Inspire others to meditate | 7 (16.3) | 1 (5.0) | 8 (12.7) |
| No impact | 5 (11.6) | 2 (10.0) | 7 (11.1) |
Adherence
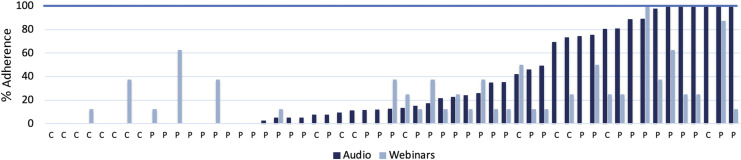
Overall, 43 of 55 participants (78%) were confirmed to have listened to at least one audio recording and/or participated in at least one webinar; however, sources of missing data were identified. Among the 55 evaluable participants, the median number of recorded audio plays of guided meditations was 5.1 plays (IQR: 0–29.3 plays) during the 8-week intervention period. Partial audio plays were uncommon; in such cases, the data were reported as the fraction of the complete track length. Greater than 50% adherence to the practice instructions to play the audio tracks at least 40 times was recorded for 17 participants (31%); 15 participants (27%) had >70% adherence; and 6 participants (11%) had >100% adherence, that is, playing the audio tracks >40 times (Table 3 and Figure 1). No audio plays were recorded for 17 participants, but six patient-caregiver pairs reported practicing together and used the same device, thus adherence was underreported.
Table 3.
Validated survey results at baseline and end of study.
| All Participants (N = 21) a | <50% Adherence (N = 10) | >50% Adherence (N = 11) | |||||
|---|---|---|---|---|---|---|---|
| Possible score Range | Baseline mean (SD) | Week 8 mean (SD) | d | p | p | p | |
| NCCN distress thermometer NIH PROMIS short forms | 0–10 | 4.6 (2.8) | 3.1 (2.6) | .59 | .01 | .47 | .01 |
| Anxiety 4a | 4–20 | 8.6 (3.2) | 8.3 (2.5) | .11 | .62 | .88 | .16 |
| Depression 4a | 4–20 | 8.0 (3.2) | 6.8 (3.0) | .63 | .01 | .35 | .02 |
| Global Mental Health | 4–20 | 6.7 (1.7) | 7.2 (1.8) | .30 | .18 | .14 | .02 |
| Fatigue 6a | 6–30 | 15.4 (6.2) | 13.8 (5.6) | .37 | .10 | .47 | .15 |
| Sleep Disturbance 4a | 4–20 | 9.9 (2.6) | 8.2 (1.3) | .61 | .01 | .07 | .10 |
| FFMQ-SF | |||||||
| Acting with awareness | 5–25 | 17.1 (3.3) | 18.3 (3.4) | .39 | .09 | .76 | .05 |
| Describing | 5–25 | 18.0 (3.5) | 19.3 (3.0) | .57 | .02 | .42 | .02 |
| Non-judging | 5–25 | 16.8 (4.1) | 17.4 (4.3) | 1 | .40 | .76 | .33 |
| Non-reacting | 5–25 | 15.0 (3.0) | 17.1 (3.4) | .58 | .01 | .46 | .02 |
| Observing | 4–20 | 13.9 (2.4) | 15.1 (2.6) | .59 | .01 | .15 | .06 |
| “Are you at Peace?” b | 1–5 | 3.3 (.86) | 3.4 (1.1) | .11 | 0.63 | 0.17 | .03 |
| Self-efficacy 4a c | 4–20 | 13.2 (2.9) | --- | 0.90 | |||
aParticipants who completed baseline and week 8 surveys. N = 21 with 11 in higher adherence group, except Distress: N = 22 with 12 in higher adherence group. Depression N = 19; 8 in low adherence group. Adherence is in reference to the practice instructions to play the meditation tracks at least 40 times. d, effect size calculated for pre-post difference data; p, P-values from paired t-tests. P-values <.05 are in bold. National Comprehensive Cancer Network (NCCN) Distress Thermometer distress screening instrument; National Institutes of Health Patient Reported Outcomes Measurement Information System (NIH PROMIS); Five Facet Mindfulness Questionnaire Short Form (FFMQ-SF).
b“Are You at Peace?” one-item spiritual probe: 1 = not at all; 2 = a little bit; 3 = a moderate amount; 4 = quite a bit; 5 = completely.
cNIH PROMIS Self-Efficacy for Managing Emotions was administered at baseline only. Baseline self-efficacy scores were compared in the <50 and >50% adherence groups, P-value from unpaired t-test.
Figure 1.
Adherence by evaluable participants. Percent adherence to the practice instructions to play the audio mediation tracks 40 times and to attend 8 webinars. Plays of recorded webinars are not included due to incomplete web capture. Bars are truncated at 100% adherence (6 of the 55 participants completed more than the assigned sessions). Patients (P) and Caregivers (C) are ordered on the X-axis by increasing number of audio plays.
The median number of live webinars attended was 1 (IQR: 0–2). Six participants (11%) had at least 50% attendance, and only one attended all eight webinars (Figure 1). Seventy percent of webinar attendees had video on. Twenty-five (45.5%) participants did not attend any live webinars. Due to a technical error, plays of audio recordings of the live webinars were not captured from the website until July 1, 2018. Among 33 participants with complete data, eight (24%) listened to the recorded webinars, with a median of 2.5 (range: 1–35) plays.
The demographic and clinical characteristics of participants in the lowest and highest adherence tertiles were compared in an exploratory analysis (Supplementary Table S9). The webinar instructors’ adherence to the webinar curriculum was also assessed as a measure of intervention fidelity (Supplemental Methods and Supplementary Table S10). Both instructors consistently covered all of the required sections and topics in the teaching manual (Supplementary Table S4). The discussion section was shorter than the planned 20 minutes, corresponding to the low attendance. Participants’ assessments of the meditation instructors, solicited in the study assessment surveys and in the post-study interviews, were uniformly positive.
Participant-Reported Outcomes
Overall, 39 (71%) participants completed any follow-up assessment, thus meeting the protocol-defined feasibility endpoint of a retention rate of ≥70%. Twenty-one participants (16 patients and 5 caregivers) completed surveys at baseline and end of study (week 8); one additional caregiver completed only the NCCN DT at both timepoints. In a pretest–posttest comparison, these participants reported statistically significant reductions in distress, depressive symptoms, and sleep disturbance; as well as significant improvements in the mindfulness facets: describing, non-reactivity to inner experience, and observing—all with medium effect sizes (Table 3). Mean distress scores decreased from 4.6 (SD 2.8) to 3.1 (SD 2.6), P = .012 (Supplementary Figure S2). The effect size for change in distress was .59.
In pre-specified exploratory subset analyses, we did not find notable differences in baseline to week 8 survey results between patients and caregivers or between patient-caregiver pairs and unpaired patients. The differences in patient-reported outcomes were prominent; however, when we stratified based on adherence to the instructions to practice with the guided meditations five times per week (40 plays total over 8 weeks) (Table 3). Among 10 participants with “low” (<50%) adherence to the practice instructions, the median adherence was 12% (i.e., 4.8 plays), range 0–49%. Among 12 participants with paired survey data and “high” (>50%) adherence, the median adherence was 88% (35.2 plays), range 69–203%, with six participants having played the meditation recordings >40 times. In the “low” adherence subset, no statistically significant changes in patient-reported outcomes were observed, although there was a trend toward improvement in sleep disturbance (d .66). In the “high” adherence subset, there were statistically significant improvements in domains where benefits were reported in the overall group: distress (d .88), depressive symptoms (d .82), and the mindfulness facets: describing (d .82) and non-reactivity to inner experience (d .86). Additionally, there were non-significant improvements in sleep disturbance (d .54) and observing (d .63). Moreover, statistically significant improvements limited to the “high” adherence subset were reported for global mental health (d .80), acting with awareness (d .67), and feeling at peace (d .79), along with a trend toward improvement in anxiety (d .46). In the “low” adherence group, mean distress scores decreased from 4.4 (SD 3.1) to 3.9 (SD 3.0), p 0.47, d .23. By contrast, in the “high” adherence group, mean distress scores decreased from 4.75 (SD 2.6) to 2.5 (SD 2.1), p .01, d .88. Baseline self-efficacy for managing emotions did not correlate with adherence (Table 3).
Adverse Effects
No adverse effects were reported, including among the 33 respondents to the survey question sent at week 3: “Have you experienced any negative effects from your participation in the Being Present 2.0 study?” In post-intervention interviews, 5 of 23 respondents reported feeling guilty about low levels participation (Table 4).
Table 4.
Quantitative analysis of qualitative data from post-study interviews.
| Post-study interview responses | Patients | Caregivers | Total | |||
|---|---|---|---|---|---|---|
| N a | N (%) | N a | N (%) | N a | N (%) | |
| Reports having benefited from study | 18 | 17 (88.9) | 7 | 5 (71.4) | 25 | 22 (88.0) |
| Positive experiences b | 20 | 9 | 29 | |||
| Emotional calming effect | 5 (25.0) | 2 (22.2) | 7 (24.1) | |||
| Physical calming effect | 2 (10.0) | 1 (11.1) | 3 (10.3) | |||
| Provided tools for coping | 4 (20.0) | 0 (0.0) | 4 (13.8) | |||
| More control over thoughts | 3 (15.0) | 3 (33.3) | 6 (20.7) | |||
| Relationship effects | ||||||
| Improved relationships and connections | 16 | 8 (50.0) | 5 | 3 (60.0) | 21 | 11 (52.4) |
| Participating with partner increased motivation to meditate | 15 | 5 (33.3) | 4 | 2 (50.0) | 20 | 7 (35.0) |
| Enjoyed text messages | 17 | 14 (82.4) | 5 | 4 (80.0) | 22 | 19 (86.4) |
| Found website easy to navigate | 17 | 14 (82.4) | 7 | 5 (71.4) | 24 | 19 (79.2) |
| Positive webinar feedback | ||||||
| Wanted to keep webinars | 17 | 11 (64.7) | 5 | 2 (40.0) | 22 | 13 (59.1) |
| Provided a sense of community/support | 16 | 13 (65.0) | 6 | 2 (33.3) | 22 | 15 (68.2) |
| Webinar critiques b | 20 | 9 | 29 | |||
| Webinars were at an inconvenient time | 10 (50.0) | 4 (44.4) | 14 (48.3) | |||
| Technical difficulties | 5 (25.0) | 2 (22.2) | 7 (24.1) | |||
| Too long | 4 (20.0) | 2 (22.2) | 6 (20.7) | |||
| Felt participants were not engaged | 3 (15.0) | 2 (22.2) | 5 (17.2) | |||
| Distractions interfered with concentration | 3 (15.0) | 1 (11.1) | 4 (13.8) | |||
| Were sole participant during a webinar | 3 (15.0) | 1 (11.1) | 4 (13.8) | |||
| Webinar alternatives | ||||||
| Endorses a blog | 17 | 12 (70.6) | 6 | 3 (50.0) | 23 | 15 (65.2) |
| Endorses a podcast | 17 | 9 (52.9) | 7 | 4 (57.1) | 24 | 13 (54.2) |
| General study critiques b | 20 | 9 | 29 | |||
| Difficulty accessing meditations on cell phone/tablet | 3 (15.0) | 1 (11.1) | 4 (13.8) | |||
| Meditation recordings were too quiet | 2 (10.0) | 1 (11.1) | 3 (10.3) | |||
| Wanted more website or Zoom training | 2 (10.0) | 1 (11.1) | 3 (10.3) | |||
| Wanted more meditation materials | 1 (5.0) | 1 (11.1) | 2 (6.9) | |||
| Negative effects from participation | ||||||
| No negative effects | 16 | 14 (87.5) | 7 | 4 (57.1) | 23 | 18 (78.3) |
| Felt guilty about low participation | 16 | 2 (12.5) | 7 | 3 (42.8) | 23 | 5 (21.7) |
| Barriers to participation | 15 | 6 | 21 | |||
| Personal/time conflicts | 6 (40.0) | 3 (50.0) | 9 (42.9) | |||
| Prefers alternative meditation | 3 (20.0) | 3 (50.0) | 6 (28.6) | |||
| Difficulty focusing | 3 (20.0) | 0 (0.0) | 3 (14.3) | |||
| Cancer content avoidance | 2 (13.3) | 1 (16.7) | 3 (14.3) | |||
| Health problems related to cancer | 2 (13.3) | 0 (0.0) | 2 (9.5) | |||
| Meditation plans post-study | ||||||
| Plans to continue a meditation practice | 16 | 15 (93.8) | 8 | 7 (87.5) | 24 | 22 (91.7) |
| Plans to continue meditating using BP2.0 materials +/− alternatives | 15 | 5 (33.3) | 7 | 4 (57.1) | 22 | 9 (40.9) |
| Plans to continue meditating using alternative meditation methods | 15 | 10 (66.7) | 7 | 3 (42.3) | 22 | 13 (59.1) |
aN is number of participants who were asked the corresponding semi-structured interview question.
bSpontaneously reported responses, not tied to a specific interview question: denominator N is the total number of interviews conducted.
Post-Intervention Interviews
In semi-structured interviews conducted upon completion of the 8-week meditation program, 22 of 25 participants (88%) reported benefits from participation in the study (Table 4). Positive experiences reported in response to open-ended questions included an emotional and physical calming effect from meditating, developing tools for coping, and having more control over thoughts. Numerous participants described their new distress management skills similarly, such as: “using the breath to re-center oneself” and “letting go of fear” (Supplementary Table S11). The majority of interviewees enjoyed receiving daily text messages (86%) and reported ease of use with the website (79%). Improved relationships and connections with others as a result of study participation was reported by 52% of interviewees and 92% planned to continue some type of meditation practice.
Barriers to full study participation included competing demands, avoidance of content related to cancer, and preferences for an alternative meditation option (Table 4). As an example, one 49-year-old male patient explained that the weekly webinars, scheduled at a time in the evening that he usually spent with family, were not feasible because “it was just one more thing I had to do that reminded me of cancer.” Some caregivers reported feeling uncomfortable sharing their own struggles during the webinars, as they were not the ones with cancer (Supplementary Table S11). Regarding overall critiques of the webinar portion of the study, 48% of interviewees indicated the webinars were at an inconvenient time, and 24% experienced technical difficulties. Despite these critiques, 59% of interviewees felt that the webinars added value as part of the study, and 68% felt the webinars provided a sense of community and support. When asked about potential alternatives to the webinars, 65% of respondents endorsed a blog, and 54% endorsed a podcast. Among 27 respondents to the study evaluation question: “On a scale of 0-10, how likely is it that you would recommend Being Present 2.0 to a family member or friend in a similar situation?” the median rating was 9 (IQR: 6-10).
Discussion
The purpose of Being Present 2.0 was to design and test the feasibility and acceptability of a mindfulness-based program for distress reduction in patients with metastatic gastrointestinal cancers and their caregivers. By design, BP2.0 features all of the essential ingredients of a mindfulness-based program, which include addressing distress, present moment focus, development of self-regulation (attentional, emotional, and behavioral) as well as positive qualities (such as compassion) through a sustained experiential training under the guidance of skilled teachers. 48 Flexible ingredients, including program delivery (online), structure (session length), and certain curriculum elements (e.g., inclusion of patient- and caregiver-specific meditation tracks, progressive muscle relaxation, and nature-themed guided imagery) were tailored with input from the target the population, differentiating BP2.0 from other technology-supported MBIs.31-37
The results of BP2.0 provide insight into the implementation of a MBI in a patient population that has been understudied to date. The BP2.0 online program was of interest to patients receiving chemotherapy and their caregivers: 72% of eligible patients consented to participate, and half of participating patients were joined by a caregiver. Cited reasons for study participation, expectations and perceived benefits corresponded with participant-reported baseline sources of distress (Table 2 and Supplementary Table S8). We hypothesized that ≥70% of participants would listen to the meditation recordings via the website platform and/or participate in webinars and complete any follow-up assessment, thus meeting our prospectively defined metrics for intervention feasibility. By these criteria, the intervention was feasible. The retention rate and favorable study evaluations further support the feasibility and acceptability of the intervention. While not powered for efficacy, the results from BP2.0 additionally suggest the potential for clinical benefit, including a clinically meaningful reduction in distress scores46,47 and 88% of participants reporting benefit in post-study interviews.
We acknowledge that BP2.0 had several limitations, including sample size, lack of a control arm, use of multiple comparisons, and importantly, low interactive webinar attendance. To address low webinar attendance, we worked on expectation setting by conveying that the webinars were an essential part of the BP2.0 program during the consent process. To mitigate frequent technical difficulties during the webinars, additional technical support was provided to the meditation instructors and participants. In addition to weekly emails, reminders about the webinars were sent via text messaging. We also instituted follow-up calls from the research coordinator after the initial webinar and any missed webinar sessions. None of these strategies appreciably improved webinar attendance. Although the use of Zoom for the BP2.0 webinars was a barrier during our study, we anticipate that this will be less of a hurdle for future studies due to increased utilization of the Zoom platform for virtual meetings during the COVID-19 pandemic.
While our study met criteria for feasibility, adherence was variable, highlighting challenges that may be inherent to studies designed to support patients in active treatment for metastatic cancer and their caregivers. Measures of adherence were based on the practice instruction to play the meditation tracks at least 5 times per week for 8 weeks; webinars were not included in the adherence measurement as, due to a technical error, plays of audio recordings of the live webinars were not captured from the website for the first two months that the study was open. Roughly one-third of BP2.0 participants had ≥70% adherence (Supplementary Table S9); whereas, a similar proportion had no recorded use of the audio tracks. In another recent study of a mobile/online MBI, 33% of cancer patients achieved at least 70% adherence to the practice instructions. 36 While that study by Kubo et al reported somewhat higher adherence overall, it is notable that nearly half of patients had received curative intent therapy within the past 6 months, vs 91% of patients receiving palliative chemotherapy for an incurable cancer on BP2.0 (and the remaining patients were actively undergoing curative intent treatment for metastatic disease).
In pre-specified exploratory subset analyses, no notable differences were observed in baseline to week 8 survey results between patients and caregivers or between patient-caregiver pairs and unpaired patients. This marks a difference from original pilot study, BP1.0,16 where data suggested a greater benefit in patient-caregiver pairs vs unpaired patients. We had hypothesized that this finding may be recapitulated in BP2.0, reflecting interdependency in distress among dyads.6,17,20 On the other hand, similarities between BP1.0 and BP2.0 included remarkably consistent demographics except that, in BP2.0, one-third of patients had non-colorectal cancer gastrointestinal malignancies. Baseline sources and levels of distress were similar (in patients and caregivers), as were reasons for study participation. The attrition rate was equivalent in both studies, with worsening illness as the major reason for early discontinuation. The motivational text messages were positively received, with some participants reporting that they felt supported by this practice container even if they did not otherwise fully engage in the intervention. The main negative effect of study participation was a feeling of guilt reported by a minority of enrollees who did not adhere to the practice instructions. In both BP1.0 and BP2.0, comparable, statistically significant reductions in distress scores were observed. With both studies, the majority of interviewees reported plans to continue mindfulness meditation practice. A key distinction with BP2.0 was the collection of more complete adherence data via web capture.
In another pre-specified exploratory subset analysis, participants who practiced more reported increased benefit, including statistically significant improvements not only in distress, but also in depression, global mental health, feeling at peace, and three of the five facets of mindfulness. Adherence accounting for webinar attendance in addition to playing the guided meditation audio tracks separated participants into nearly identical subsets and did not substantively change the results, again noting low webinar attendance overall. There was no indication from surveys or interviews that the meditation instructors or the curriculum were drivers of low attendance, although formal MBI teaching assessment criteria were not applied. 49 Rolling enrollment, with patients and caregivers included in the same webinar, was a pragmatic design decision given the unstable health of patients with metastatic cancer. Feedback from caregivers suggests that fixed caregiver- and patient-specific cohorts could have improved cohesion and ease in sharing, motivating attendance. 50 However, this would not eliminate the fear of interacting with sicker or otherwise more distressed participants. We chose a time for the webinars that was unlikely to interfere with work, school, medical appointments, and other daily activities; still the main critique of the live webinars was that they were at an inconvenient time—an hour in the evening when some participants did not want to think about cancer.
In the future, we seek to test a stepped care study design, to accommodate patients/caregivers with the highest capacity for full participation and those with great needs, yet lower capacity for engagement. All participants will have access to high quality video recordings of webinar content (a podcast model) and the ability to submit questions. The more intensive option may feature one-on-one or dyadic sessions via teleconference with a meditation instructor, 51 thus addressing several of the challenges that were encountered with the group webinars. For scalability, the frequency and/or duration of the live sessions will be lessened. We will reduce survey burden and offer a monetary incentive to improve survey completion rates. 36 Leveraging recruitment from shared infusion centers, Being Present eligibility will be extended to enroll patients with any metastatic cancer diagnosis. Additional design modifications are needed to increase racial, ethnic, and socioeconomic diversity. A future research question is whether the average level of adherence that defines success of a feasible, safe, and inexpensive distress reduction strategy for patients with metastatic cancer may need to be lower than that which would be expected among cancer survivors.
Conclusions
The Being Present 2.0 online mindfulness-based program is appealing to, feasible, and acceptable for patients with metastatic gastrointestinal cancer undergoing active treatment and their caregivers. The high recruitment rate highlights the demand for remote delivered interventions to reduce distress in this population. Meanwhile, challenges encountered related to adherence underscore the need to tailor expectations, as well as interventions, in the advanced cancer setting. Positive preliminary data from BP2.0 provide support for a clinical trial to definitively evaluate the efficacy of this safe, simple, and inexpensive mindfulness intervention to reduce distress and improve quality of life among cancer patients and their caregivers.
Supplemental Material
Supplemental Material, sj-pdf-1-gam-10.1177_21649561211044693 for Being Present 2.0: Online Mindfulness-Based Program for Metastatic Gastrointestinal Cancer Patients and Caregivers by Hannah M. Dragomanovich, Anand Dhruva, Eve Ekman, Kelly L. Schoenbeck, Ai Kubo, Erin L. Van Blarigan, Hala T. Borno, Mikaela Esquivel, Bryant Chee, Matthew Campanella, Errol J. Philip, John P. Rettger, Blake Rosenthal, Katherine Van Loon, Alan P. Venook, Christy Boscardin, Patricia Moran, Frederick M. Hecht and Chloe E. Atreya in Global Advances in Health and Medicine
Acknowledgments
We extend gratitude to all Being Present 2.0 study participants and Advisory Council members; to the UCSF Clinical Innovation Center (CIC) Inside Out Accelerator Team: Jessica Chao, Pelin Cinar, Ralph Gonzales, Anke Hebig Prophet, Zii (Yoon-Ji) Kim, and Jan Yeager; Lucid Dawn, Mark Silva and Michael Starita (meditation recordings); Anand Parikshak, Lani Potts, and James Mitchell (meditation instructors); Anthony Riberi at Y3ti and Patty Nason (technical support); Kameron Allen (logo design); and to the Helen Diller Family Foundation, UCSF CIC Inside Out Accelerator Award, the Mount Zion Health Fund, NCI K07CA197077, and NIH/NCI K08CA175 for funding.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: This work was partially supported by a grant from the UCSF Inside Out Accelerator Program, funded by Genentech (Principal Investigator, Dr Boscartin: G-58161). Genentech had no involvement in study design; collection, analysis, and interpretation of the data or writing of the report. There are no restrictions regarding the submission of the report for publication.
Supplementray Material: Supplemental material for this article is available online.
References
- 1.Carlson LE. Distress management through mind-body therapies in oncology. J Natl Cancer Inst Monogr. 2017;2017(52). [DOI] [PubMed] [Google Scholar]
- 2.Schuurhuizen C, Braamse AMJ, Beekman ATF, et al. Screening and stepped care targeting psychological distress in patients with metastatic colorectal cancer: the tes cluster randomized trial. J Natl Compr Cancer Netw. 2019;17(8):911-920. [DOI] [PubMed] [Google Scholar]
- 3.Carlson LE, Angen M, Cullum J, et al. High levels of untreated distress and fatigue in cancer patients. Br J Cancer. 2004;90(12):2297-2304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Palliative Care in Cancer . National Cancer Institute. https://www.cancer.gov/about-cancer/advanced-cancer/care-choices/palliative-care-fact-sheet. 2017. Accessed April 27, 2020. [Google Scholar]
- 5.Zabora J, BrintzenhofeSzoc K, Curbow B, Hooker C, Piantadosi S. The prevalence of psychological distress by cancer site. Psycho Oncol. 2001;10(1):19-28. [DOI] [PubMed] [Google Scholar]
- 6.Hodges LJ, Humphris GM, Macfarlane G. A meta-analytic investigation of the relationship between the psychological distress of cancer patients and their carers. Soc Sci Med. 2005;60(1):1-12. [DOI] [PubMed] [Google Scholar]
- 7.Lu D, Andrae B, Valdimarsdottir U, et al. Psychological distress is associated with cancer-specific mortality among patients with cervical cancer. Cancer Res. 2019. [DOI] [PubMed] [Google Scholar]
- 8.Quinten C, Coens C, Mauer M, et al. Baseline quality of life as a prognostic indicator of survival: a meta-analysis of individual patient data from EORTC clinical trials. Lancet Oncol. 2009;10(9):865-871. [DOI] [PubMed] [Google Scholar]
- 9.Giese-Davis J, Collie K, Rancourt KM, Neri E, Kraemer HC, Spiegel D. Decrease in depression symptoms is associated with longer survival in patients with metastatic breast cancer: A secondary analysis. J Clin Oncol. 2011;29(4):413-420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Batty GD, Russ TC, Stamatakis E, Kivimaki M. Psychological distress in relation to site specific cancer mortality: Pooling of unpublished data from 16 prospective cohort studies. BMJ. 2017;356:j108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pirl WF, Fann JR, Greer JA, et al. Recommendations for the implementation of distress screening programs in cancer centers: Report from the American Psychosocial Oncology Society (APOS), Association of Oncology Social Work (AOSW), and Oncology Nursing Society (ONS) joint task force. Cancer. 2014;120(19):2946-2954. [DOI] [PubMed] [Google Scholar]
- 12.Braun M, Mikulincer M, Rydall A, Walsh A, Rodin G. Hidden morbidity in cancer: spouse caregivers. J Clin Oncol. 2007;25(30):4829-4834. [DOI] [PubMed] [Google Scholar]
- 13.Pitceathly C, Maguire P. The psychological impact of cancer on patients’ partners and other key relatives: A review. Eur J Cancer. 2003;39(11):1517-1524. [DOI] [PubMed] [Google Scholar]
- 14.Golant M, Haskins NV. ”Other cancer survivors”: The impact on family and caregivers. Cancer J. 2008;14(6):420-424. [DOI] [PubMed] [Google Scholar]
- 15.Trevino KM, Prigerson HG, Maciejewski PK. Advanced cancer caregiving as a risk for major depressive episodes and generalized anxiety disorder. Psycho Oncol. 2018;27(1):243-249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Atreya CE, Kubo A, Borno HT, et al. Being Present: A single-arm feasibility study of audio-based mindfulness meditation for colorectal cancer patients and caregivers. PLoS One. 2018;13(7):e0199423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kim Y, van Ryn M, Jensen RE, Griffin JM, Potosky A, Rowland J. Effects of gender and depressive symptoms on quality of life among colorectal and lung cancer patients and their family caregivers. Psycho Oncol. 2015;24(1):95-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shaw JM, Young JM, Butow PN, et al. Improving psychosocial outcomes for caregivers of people with poor prognosis gastrointestinal cancers: A randomized controlled trial (Family Connect). Support Care Cancer. 2016;24(2):585-595. [DOI] [PubMed] [Google Scholar]
- 19.Piet J, Wurtzen H, Zachariae R. The effect of mindfulness-based therapy on symptoms of anxiety and depression in adult cancer patients and survivors: A systematic review and meta-analysis. J Consult Clin Psychol. 2012;80(6):1007-1020. [DOI] [PubMed] [Google Scholar]
- 20.Hagedoorn M, Sanderman R, Bolks HN, Tuinstra J, Coyne JC. Distress in couples coping with cancer: A meta-analysis and critical review of role and gender effects. Psychol Bull. 2008;134(1):1-30. [DOI] [PubMed] [Google Scholar]
- 21.Carlson LE, Doll R, Stephen J, et al. Randomized controlled trial of Mindfulness-based cancer recovery versus supportive expressive group therapy for distressed survivors of breast cancer. J Clin Oncol. 2013;31(25):3119-3126. [DOI] [PubMed] [Google Scholar]
- 22.Lengacher CA, Kip KE, Barta M, et al. A pilot study evaluating the effect of mindfulness-based stress reduction on psychological status, physical status, salivary cortisol, and interleukin-6 among advanced-stage cancer patients and their caregivers. J Holist Nurs. 2012;30(3):170-185. [DOI] [PubMed] [Google Scholar]
- 23.Chambers SK, Occhipinti S, Foley E, et al. Mindfulness-based cognitive therapy in advanced prostate cancer: A randomized controlled trial. J Clin Oncol. 2017;35(3):291-297. [DOI] [PubMed] [Google Scholar]
- 24.Birnie K, Garland SN, Carlson LE. Psychological benefits for cancer patients and their partners participating in mindfulness-based stress reduction (MBSR). Psycho Oncol. 2010;19(9):1004-1009. [DOI] [PubMed] [Google Scholar]
- 25.Xunlin NG, Lau Y, Klainin-Yobas P. The effectiveness of mindfulness-based interventions among cancer patients and survivors: A systematic review and meta-analysis. Support Care Cancer. 2020;28(4):1563-1578. [DOI] [PubMed] [Google Scholar]
- 26.Oberoi S, Yang J, Woodgate RL, et al. Association of mindfulness-based interventions with anxiety severity in adults with cancer: A systematic review and meta-analysis. JAMA Netw Open. 2020;3(8):e2012598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cillessen L, Johannsen M, Speckens AEM, Zachariae R. Mindfulness-based interventions for psychological and physical health outcomes in cancer patients and survivors: A systematic review and meta-analysis of randomized controlled trials. Psycho Oncol. 2019;28(12):2257-2269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schell LK, Monsef I, Wockel A, Skoetz N. Mindfulness-based stress reduction for women diagnosed with breast cancer. Cochrane Database Syst Rev. 2019;3:CD011518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Society AC. Cancer Facts & Figures 2020. American Cancer Society, Inc. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2020/cancer-facts-and-figures-2020.pdf. 2020. Accessed July 20, 2020. [Google Scholar]
- 30.Eyles C, Leydon GM, Hoffman CJ, et al. Mindfulness for the self-management of fatigue, anxiety, and depression in women with metastatic breast cancer: A mixed methods feasibility study. Integr Cancer Ther. 2015;14(1):42-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zernicke KA, Campbell TS, Speca M, et al. The eCALM Trial-eTherapy for cancer appLying mindfulness: online mindfulness-based cancer recovery program for underserved individuals living with cancer in Alberta: Protocol development for a randomized wait-list controlled clinical trial. BMC Compl Altern Med. 2013;13:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fish J, Brimson J, Lynch S. Mindfulness interventions delivered by technology without facilitator involvement: What research exists and what are the clinical outcomes? Mindfulness (N Y). 2016;7(5):1011-1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lengacher CA, Reich RR, Ramesar S, et al. Feasibility of the mobile mindfulness-based stress reduction for breast cancer (mMBSR(BC)) program for symptom improvement among breast cancer survivors. Psycho Oncol. 2018;27(2):524-531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Altschuler A, Rosenbaum E, Gordon P, Canales S, Avins AL. Audio recordings of mindfulness-based stress reduction training to improve cancer patients’ mood and quality of life--a pilot feasibility study. Support Care Cancer. 2012;20(6):1291-1297. [DOI] [PubMed] [Google Scholar]
- 35.Compen F, Bisseling E, Schellekens M, et al. Face-to-face and internet-based mindfulness-based cognitive therapy compared with treatment as usual in reducing psychological distress in patients with cancer: A multicenter randomized controlled trial. J Clin Oncol. 2018;36(23):2413-2421. [DOI] [PubMed] [Google Scholar]
- 36.Kubo A, Kurtovich E, McGinnis M, et al. A randomized controlled trial of mhealth mindfulness intervention for cancer patients and informal cancer caregivers: A feasibility study within an integrated health care delivery system. Integr Cancer Ther. 2019;18:1534735419850634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mikolasek M, Berg J, Witt CM, Barth J. effectiveness of mindfulness- and relaxation-based eHealth interventions for patients with medical conditions: A systematic review and synthesis. Int J Behav Med. 2018;25(1):1-16. [DOI] [PubMed] [Google Scholar]
- 38.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inf. 2009;42(2):377-381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kalauokalani D, Cherkin DC, Sherman KJ, Koepsell TD, Deyo RA. Lessons from a trial of acupuncture and massage for low back pain: patient expectations and treatment effects. Spine (Phila Pa 1976). 2001;26(13):1418-1424. [DOI] [PubMed] [Google Scholar]
- 40.National Comprehensive Cancer Network . Distress management. Clinical practice guidelines. J Natl Compr Cancer Netw. 2003;1(3):344-374. [DOI] [PubMed] [Google Scholar]
- 41.Network NCC. NCCN Distress Thermometer . https://www.nccn.org/patients/resources/life_with_cancer/pdf/nccn_distress_thermometer.pdf. 2020. Accessed April 27, 2020.
- 42.Broderick JE, DeWitt EM, Rothrock N, Crane PK, Forrest CB. Advances in patient-reported outcomes: The NIH PROMIS((R)) measures. EGEMS (Wash DC). 2013;1(1):1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bohlmeijer E, ten Klooster PM, Fledderus M, Veehof M, Baer R. Psychometric properties of the five facet mindfulness questionnaire in depressed adults and development of a short form. Assessment. 2011;18(3):308-320. [DOI] [PubMed] [Google Scholar]
- 44.Steinhauser KE, Voils CI, Clipp EC, Bosworth HB, Christakis NA, Tulsky JA. “"Are you at peace?”: one item to probe spiritual concerns at the end of life. Arch Intern Med. 2006;166(1):101-105. [DOI] [PubMed] [Google Scholar]
- 45.Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. 2013;13:117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cutillo A, O’Hea E, Person S, Lessard D, Harralson T, Boudreaux E. The distress thermometer: Cutoff points and clinical use. Oncol Nurs Forum. 2017;44(3):329-336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Donovan KA, Grassi L, McGinty HL, Jacobsen PB. Validation of the distress thermometer worldwide: State of the science. Psycho Oncol. 2014;23(3):241-250. [DOI] [PubMed] [Google Scholar]
- 48.Crane RS, Brewer J, Feldman C, et al. What defines mindfulness-based programs? The warp and the weft. Psychol Med. 2017;47(6):990-999. [DOI] [PubMed] [Google Scholar]
- 49.Crane RS, Hecht FM. Intervention integrity in mindfulness-based research. Mindfulness (N Y). 2018;9(5):1370-1380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Thompson-Lastad A, Atreya CE, Chao MT, et al. Improving access to integrative oncology through group medical visits: A pilot implementation project. J Alternative Compl Med. 2019;25(7):733-739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Milbury K, Li Y, Durrani S, et al. A mindfulness-based intervention as a supportive care strategy for patients with metastatic non-small cell lung cancer and their spouses: Results of a three-arm pilot randomized controlled trial. Oncologist. 2020;25(11):e1794-e1802. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-pdf-1-gam-10.1177_21649561211044693 for Being Present 2.0: Online Mindfulness-Based Program for Metastatic Gastrointestinal Cancer Patients and Caregivers by Hannah M. Dragomanovich, Anand Dhruva, Eve Ekman, Kelly L. Schoenbeck, Ai Kubo, Erin L. Van Blarigan, Hala T. Borno, Mikaela Esquivel, Bryant Chee, Matthew Campanella, Errol J. Philip, John P. Rettger, Blake Rosenthal, Katherine Van Loon, Alan P. Venook, Christy Boscardin, Patricia Moran, Frederick M. Hecht and Chloe E. Atreya in Global Advances in Health and Medicine