Abstract
Background:
Theory posits that macronutrient intake is regulated by protein consumption and adequate intake of protein results in consumption of less carbohydrates and fat. The current study investigates the effect of protein intake on calorie and macronutrient content using an ad libitum vending machine paradigm.
Methods:
Healthy volunteers (n=287; 177m; Age=36±11; BMI=32±8) were admitted to our clinical research unit. Macronutrient meal content (grams) and energy intake (Kcal) were quantified by specialized food processing software and collected on an hourly basis over a three-day period using a validated ad libitum vending machine paradigm. Body composition was assessed by DXA. Lagged multi-level models accounting for age, sex, race/ethnicity, fat and fat free mass indices were fitted to examine the impact of prior macronutrient content on subsequent meals.
Results:
Protein intake was associated with decreased energy intake (Kcal; B= −1.67 kcal, p = 0.0048), lower protein and carbohydrate intake (B= −0.08 grams, p=0.0006; B= −0.21 grams, p= 0.0003, respectively) at subsequent meals. Daily Macronutrient intake and subsequent intake were positively associated.
Conclusions:
Dietary protein exhibits a negative regulatory effect on a short-term meal-to-meal rather than day-to-day basis. In the setting of readily available food, protein intake impacts energy intake only over very short time courses.
Keywords: Food Intake, Macronutrient Content, Vending Machine, Calories, ad libitum, Macronutrient regulation
1. Introduction
Humans have evolved to adapt to availability of bioenergetic resources from external food sources to maintain basal somatic functions for survival. However, explanations regarding the hierarchy of macronutrient and energy consumption vary. Carbohydrates, given its bulk in diets, are hypothesized to be central in bodyweight maintenance. JP Flatt’s research indicated glycogen stores play a role in regulation of energy intake (1, 2, 3). Conversely, fat intake appears to be poorly regulated(1).
Protein regulation has also been implicated in determining control of energy intake and subsequent weight gain (4). Protein leverage presupposes that protein intake exerts control on carbohydrate and fat content via a combination of neurophysiological circuits (4, 5) which manifests through an organism’s coordinated behavior involving appetite, satiety, and food choices. The leverage point of protein may vary intra- and inter-individually by a number of key factors, including age, reproductive status, genetics, developmental history, and ecological constraints (5). Based on the presupposed tight regulation of protein intake, consumption of proteins should generally be stable while intake of carbohydrate and fat intake demonstrate greater variation (4). Indeed, evidence suggests that protein intake remains fairly stable across time (6) and populations (7).
Consequently, an individual who consumes protein content below an internal threshold may consume larger amounts of carbohydrates and fat to achieve the necessary protein balance but thereby increasing overall energy intake. Experimental and self-reported evidence suggests that protein intake potentially increases satiety, limiting the amount of energy intake (8, 9, 10). The protein leverage hypothesis proposes that the downstream effects of chronic and sustained inadequate consumption of protein (i.e., increased intake) may result in higher risk for obesity. The current study used ad libitum feeding data to examine whether there is evidence supporting the existence of target protein selection over a very short term (e.g., between meals) and slightly longer term (e.g., day to day). Using a 3-day ad libitum vend paradigm, we hypothesized that:
Higher protein intake from the meal prior would be associated with a lower energy intake, with lower protein, carbohydrate, and fat intake at the following meal.
Increased protein intake from the day prior would be associated with a lower energy intake, and lower protein, carbohydrates, and fat intake on the following day.
2. Method
2.1. Participants.
A subset of participants with complete vending machine data (n = 287) from The Food Intake Phenotype study (ClinicalTrials.gov identifier NCT00342732) was used for the present set of analyses. The Food Intake study was a 10-day clinical trial designed to examine and classify eating patterns and behavior in a sample of healthy participants without diabetes (see (11, 12, 13, 14, 15) for additional background and findings derived from this cohort). The trial began in November 1999 and is ongoing. Procedures for the clinical trial (described below) were approved by the NIDDK Institutional Review Board (OH99-DKN019). Participants enrolled in the study provided written informed consent.
2.2. Procedure.
Participants were healthy other than prediabetes and obesity as determined by history and physical examination and laboratory screening. Participants were admitted to the clinical unit and placed on a three-day weight-maintaining energy needs (WMEN) diet, as determined by sex and weight [WMENwomen = 9.5*weight (kg) + 1745; WMENmen = 9.5*weight (kg) + 1973] (14, 16). Physical characteristics, such as fat mass and fat free mass, were ascertained by dual energy X-ray absorptiometry (DPX-L; Lunar Corp, Madison, Wisconsin). After 3 days, a 75-g oral glucose tolerance test (OGTT) was administered for determination of glucose tolerance status and those with diabetes(17) were ineligible to continue. Admitted participants were asked to not engage in strenuous physical activity, but could engage in light activities (e.g., playing pool, watching television, reading the newspaper). Participants were additionally allowed scheduled, supervised visits outside of the hospital.
2.2.1. Ad Libitum Food Vending Paradigm.
In the final three study days, participants were given 23.5-hour access to self-select their daily meals and snacks from a refrigerated and automated ad-libitum vending machine system (participants were admitted individually and had no interaction with other individuals during study; please see figure 1 for a visual representation of the vending machines). Self-reported intermediate hedonic food ratings (preference rating scores between 4 and 8 from a 9-point scale) from the 80-item food preference questionnaire (18) informed the 40 food choices stocked in the vending machine for participants. The 80-item food choices were based on a previously validated paradigm that systematically varied the combination of macronutrient content of the stocked foods (e.g., high fat/high sugar, high fat/ high complex carbohydrates, high fat/ low carbohydrates/high protein, low fat/high sugar, low fat/high complex carbohydrates, low fat/low carbohydrates/high protein(18)).The vending machine was stocked daily with the same food selections and included a range of foods appropriate for different mealtimes (e.g., breakfast foods, snacks, etc.). Daily access to pre-weighed beverages, bread, and condiments were also made available to participants and were included in the energy intake and macronutrient content calculations. Vending machines were stored in a lunchroom where participants consume the food alone and without access to television or cellular phones. Food that required heating were heated based on package instructions. Uneaten food and packaging were returned to study staff for processing. Remaining food was re-weighed, along with original packaging, and a new weight calculated.
Figure 1. Ad Libitum Food Vending Paradigm.
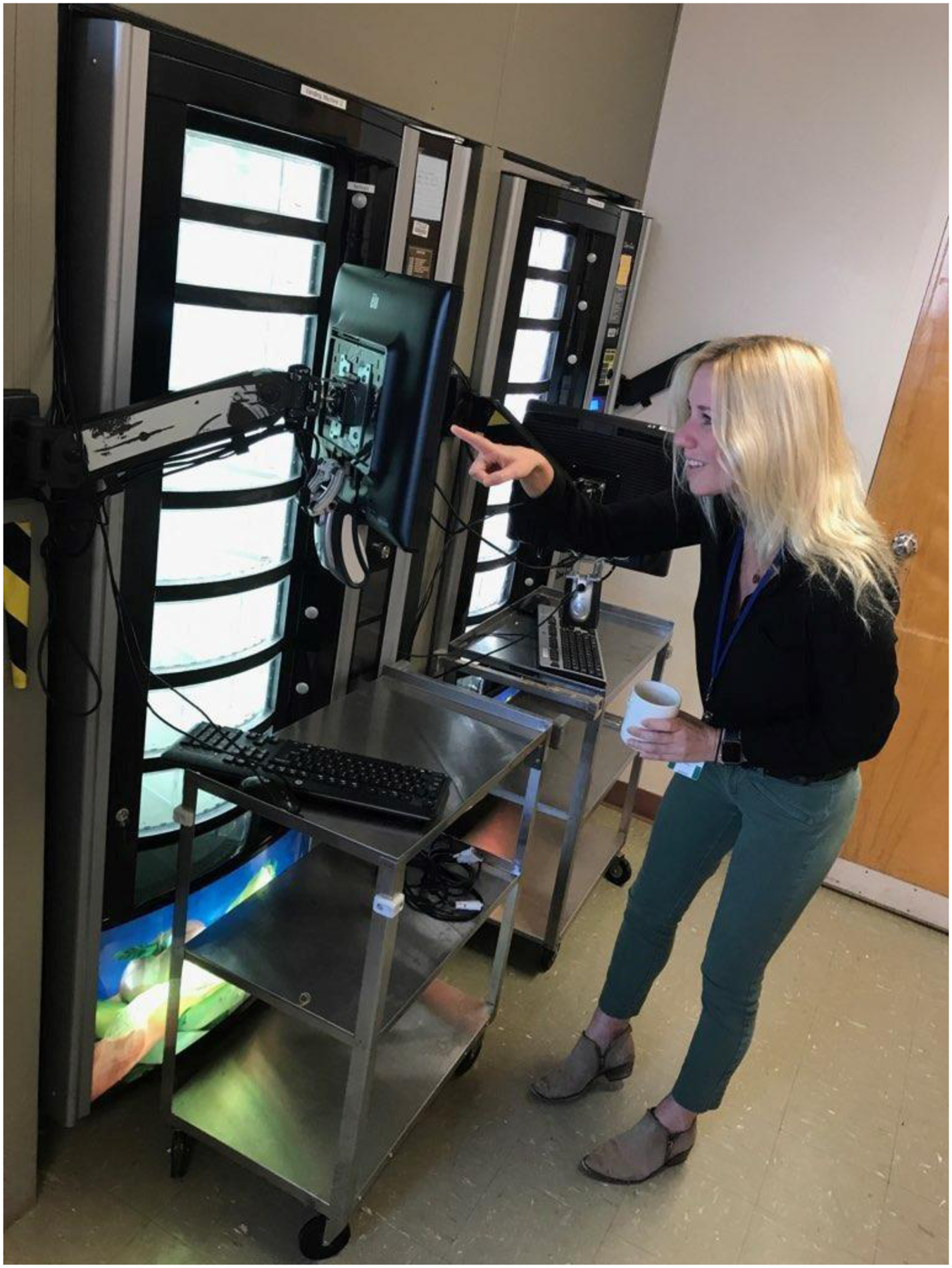
The Obesity and Diabetes Clinical Research Section (ODCRS) uses an automated vending machine to enact an ad libitum food vending paradigm. Studies that use the paradigm will give participants 23.5 hours to access the personalized vending machine (machine is stocked with a selection of 40 foods out of 80 that were rated between 4 and 8 on a 9-point scale). Participants selected their foods by typing the appropriate code onto the keypad, which releases the food from the vending machine. Food choices vary based on time of day (e.g., breakfast time is stocked with breakfast foods, etc.). Participants must consume their foods alone and may not use electronic devices. Following their meal, participants must return uneaten food and the original packaging to be processed by the metabolic kitchen staff. (Person in picture is not a study participant.)
Food processing was facilitated by study staff, whereby mealtimes were stamped, and meal content itemized. Macronutrient content (protein, carbohydrates, and fat) and energy intake were calculated with the software by weighing uneaten food. Vending paradigm endpoints have been previously demonstrated to display a high degree of reproducibility (Energy intake (kcal/d) ICC = 0.90 ;PRO (g/d) ICC = 0.74; CHO (g/d) ICC = 0.88; FAT (g/d) ICC = 0.87(15)). Daily value ICCs were calculated for the present study and demonstrated a high to moderate degree of consistency (Energy intake (kcal/d) ICC = 0.73; PRO (g/d) ICC = 0.69; CHO (g/d) ICC = 0.71; FAT (g/d) ICC = 0.66).
2.3. KCAL and Macronutrient Content.
Energy intake (Kcal) and protein, carbohydrates, and fat (in grams) for meals consumed from the vending machine were measured and recorded (see above for Procedure). Macronutrients were lagged by meal (for meal-to-meal analyses) and lagged by day (for daily analyses). The term meal in the present analyses was defined as any instance the participant visited the vending machine and consumed food, which would include meals and snacks.
2.4. Covariates.
Covariates for all models included age (in years), biological sex (women as reference), self-reported race/ethnicity (American Indian as reference), fat free mass index [fat mass (kg)/height2 (m2)], and fat mass index [fat mass (kg)/ height2 (m2)]. Both indices were included based on past research that demonstrated each had unique contributions on energy intake(19). An additional set of sensitivity analyses were performed that included plasma glucose concentrations at fasting and 120 minutes in all analytic models. Time was also included to account for any secular trends in food consumption.
2.5. Statistical Analyses.
All analyses were computed in SAS 9.4 (Cary, NC, USA: SAS Institute Inc, 2013). Proc Mixed was used to estimate the lagged mixed models, using compound symmetry (CS) covariance matrices and restricted maximum likelihood estimation (REML). Models were constructed such that total energy intake and each macronutrient content were separately modeled as dependent variables both in meal and daily analyses. The model outcomes were as follows: meal-to-meal models included meal Kcal, protein, carbohydrate, and fat intake; Daily total models included total daily kcal, protein, carbohydrate, and fat intake. Predictors included lagged macronutrient content (e.g., the effect of a meal on the subsequent meal) and included covariates listed above. All values were analyzed as absolute values, with macronutrients in grams: Energy intake (Kcal) and protein, carbohydrates, and fat (in grams) for meals consumed from the vending machine were measured and recorded (see above for Procedure). Macronutrient was conducted in grams to allow investigation of specific macronutrients in absolute terms. However, models included all macronutrients so relative amount of each were accounted for. All models presented were reanalyzed with fat free mass and fat mass (in place of fat mass and fat free mass indices), with no substantial changes to the models presented. Supplemental results and Tables S1 and S2 present the analyses stratified by sex. Statistical significance was defined as p <.05 (two-sided). Model parameter estimates presented include unstandardized coefficients (B), standard errors (SE), 95% confidence intervals (95% CI), and p-value (p).
3. Results
3.1. Participant Characteristics
The sample was predominately male (67.7 %), American Indian (57.5 %), obese (49.5 %), and approximately 35.8 years old (SD = 10.6). The sample additionally had a fat free mass index of 19.3 (SD = 3.0) and a fat mass index of 12.3 (SD = 6.2). Participant meals averaged 815.8 KCal (SD = 483.5) with 5.2 meals daily (SD = 1.7). See Table 1 for additional descriptive statistics.
Table 1.
Physical and sociodemographic characteristics of study cohort.
| Full Sample (n = 287) | |
|---|---|
| Sex, % (n) | |
| Male | 67.7 (177) |
| Female | 38.3 (110) |
| Race/Ethnicity, % (n) | |
| Native American | 57.5 (165) |
| White | 22.0 (63) |
| Black | 5.2 (15) |
| Other | 9.8 (28) |
| Age (Years), M (SD) | 35.8 (10.6) |
| Body Mass Index, kg/m2, M (SD) | 31.6 (7.9) |
| Normal/Underweight, % (n) | 17.4 (50) |
| Overweight, % (n) | 33.1 (95) |
| Obese, % (n) | 49.5 (142) |
| Body Fat (%), M (SD) | 36.9 (10.9) |
| Fat Mass (kg), M (SD) | 34.7 (16.5) |
| Fat Free Mass (kg), M (SD) | 55.8 (12.1) |
| Fat Mass Index, M (SD) | 12.3 (6.2) |
| Fat Free Mass Index, M (SD) | 19.3 (3.0) |
| Meal Kcal | 815.8 (483.5) |
| Carbohydrates (g) | 103.2 (59.6) |
| Fat (g) | 34.3 (27.5) |
| Protein (g) | 24.4 (18.9) |
| Vend Meals | 5.2 (1.7) |
Note: Descriptives for kcal, macronutrients, and vend meals across sample and repeated measures. SD, standard deviation
3.2. Meal-to-Meal KCAL Lagged Models
Mean calorie content of each meal did not differ across the three days of ad libitum intake. [Type III Fixed Effect F(2, 856) = 2.33, p = 0.10]. Table 2 presents the results from the multilevel lagged model predicting meal-to-meal energy intake (KCAL). Protein intake was associated with lower energy intake at the following meal (B = −1.67 kcal, 95%CI = −2.84, −0.51, p = 0.0048), when controlling for sociodemographics and physical characteristics. There were no significant associations between carbohydrate (B = 0.20 kcal, 95%CI = −0.18, 0.58, p = 0.30) and fat macronutrient content (B = 0.10 kcal, 95%CI = −0.80, 0.99, p = 0.83) and energy intake at the subsequent meal. An exploratory model was constructed to test whether there was a three-way interaction between protein, carbohydrates, and fat (lower-order two-way interactions were included as covariates). There was no significant three-way interaction between the macronutrients in the meal-to-meal KCAL model (B = −1.8e-4, 95% CI = −4.9e-4, 1.25e-4, p = 0.24).
Table 2. Increased protein meal intake predicted lowered caloric intake from the subsequent meal in multilevel lagged models.
Macronutrient meal content (protein, carbohydrates, and fat) were lagged such that the macronutrient content of the meal prior predicted the next meal’s caloric intake. Results from the multilevel models found a negative association, suggesting that prior meals with higher levels of protein intake predict that subsequent meals will be lower in kilocalories. There were no significant effects of carbohydrates and fat.
| Meal-to-Meal KCAL | ||||
|---|---|---|---|---|
| B | SE | 95% CI | p | |
| −2.47 | ||||
| Age | 0.87 | −4.17, −0.77 | 0.0044 | |
| Male | 117.05 | 32.19 | 53.86, 180.23 | 0.0003 |
| Female | Ref | |||
| Black | −157.70 | 39.73 | −235.67, −79.73 | <.0001 |
| Caucasian | −121.53 | 23.73 | −168.10, −74.96 | <.0001 |
| Hispanic | −117.60 | 30.98 | −178.41, −56.79 | 0.0002 |
| Other | −128.96 | 29.24 | −186.35, −71.57 | <.0001 |
| American Indian | Ref | |||
| Fat Free Mass Index | 28.39 | 5.25 | 18.09, 38.68 | <.0001 |
| Fat Mass Index | −0.33 | 2.64 | −5.51, 4.85 | 0.90 |
| Protein Lag (g) | −1.67 | 0.59 | −2.84, −0.51 | 0.0048 |
| Carbohydrates Lag (g) | 0.20 | 0.19 | −0.18, 0.58 | 0.30 |
| Fat Lag (g) | 0.10 | 0.46 | −0.80, 0.99 | 0.83 |
Bolded coefficients are statistically significant (p <.05)
3.3. Meal-to-Meal Macronutrient Content Lagged Models
Table 3 presents the results from the multilevel lagged models predicting meal-to-meal macronutrient content.
Table 3. Multilevel lag models found that increased protein meal intake predicted decreased carbohydrate and protein intake from the subsequent meal.
Meal macronutrient content (protein, carbohydrates, fat) were lagged such that the content from the meal prior were used as predictors for subsequent macronutrient content. Three separate multilevel models were calculated for each subsequent meal macronutrient. Regarding subsequent meal protein intake, increased protein intake from the meal prior predicted a drop in subsequent protein consumption. The same was found for carbohydrates – an increase in protein consumption predicted a decrease in subsequent carbohydrate intake. There were no significant lagged macronutrient predictors for subsequent fat meal intake.
| Meal-to-Meal Protein |
Meal-to-Meal Carbohydrates |
Meal-to-Meal Fat | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | 95% CI | p | B | SE | 95% CI | p | B | SE | 95% CI | p | |
| Age | −0.03 | 0.03 | −0.09, 0.04 | 0.39 | −0.23 | 0.11 | −0.44, −0.02 | 0.0359 | −0.14 | 0.05 | −0.24, −0.05 | 0.0026 |
| Male | 3.08 | 1.23 | 0.67, 5.50 | 0.0125 | 15.82 | 4.06 | 7.84, 23.79 | 0.0001 | 4.19 | 1.79 | 0.68, 7.70 | 0.0194 |
| Female | Ref | Ref | Ref | |||||||||
| Black | −2.39 | 1.74 | −5.80, 1.02 | 0.17 | −24.17 | 5.20 | −34.37, −13.97 | <.0001 | −7.68 | 2.34 | −12.27, −3.08 | 0.0011 |
| Caucasian | −1.67 | 0.85 | −3.33, 0.00 | 0.05 | −20.20 | 2.94 | −25.98, −14.42 | <.0001 | −4.52 | 1.35 | −7.18, −1.86 | 0.0009 |
| Hispanic | −2.48 | 1.18 | −4.79, −0.16 | 0.04 | −10.22 | 4.06 | −18.19, −2.25 | 0.012 | −8.20 | 1.87 | −11.86, −4.54 | <.0001 |
| Other | −0.79 | 1.31 | −3.37, 1.78 | 0.55 | −23.11 | 3.45 | −29.88, −16.34 | <.0001 | −4.15 | 1.63 | −7.35, −0.95 | 0.01 |
| American Indian | Ref | Ref | Ref | |||||||||
| Fat Free Mass Index | 0.97 | 0.19 | 0.60, 1.34 | <.0001 | 2.89 | 0.68 | 1.55, 4.22 | <.0001 | 1.38 | 0.28 | 0.83, 1.94 | <.0001 |
| Fat Mass Index | −0.02 | 0.10 | −0.21, 0.18 | 0.86 | −0.29 | 0.34 | −0.95, 0.37 | 0.39 | 0.10 | 0.15 | −0.20, 0.39 | 0.51 |
| Protein Lag (g) | −0.08 | 0.02 | −0.13, −0.04 | 0.0006 | −0.21 | 0.07 | −0.35, −0.07 | 0.0032 | −0.05 | 0.03 | −0.12, 0.02 | 0.17 |
| Carbohydrates Lag (g) | 0.01 | 0.01 | 0.00, 0.03 | 0.08 | 0.01 | 0.02 | −0.04, 0.06 | 0.75 | 0.01 | 0.01 | −0.01, 0.03 | 0.21 |
| Fat Lag (g) | 0.00 | 0.02 | −0.03, 0.04 | 0.80 | 0.09 | 0.06 | −0.02, 0.20 | 0.10 | −0.01 | 0.03 | −0.06, 0.04 | 0.63 |
Bolded coefficients are statistically significant (p <.05)
3.3.1. Protein Intake.
Higher protein intake of the prior meal was associated with less protein consumption at subsequent meals (B = −0.08 grams, 95%CI = −0.13, −0.04, p = 0.0006). Conversely, carbohydrates (B = 0.01 grams, 95%CI = 0.00, 0.03, p = 0.08) and fats (B = 0.00 grams, 95%CI = −0.03, 0.04, p = 0.80) did not predict subsequent protein intake.
3.3.2. Carbohydrate Intake.
Higher protein intake was associated with decreased carbohydrate consumption (B = −0.21 grams, 95%CI = −0.35, −0.07, p = 0.0032; Table 3). Neither carbohydrates (B = 0.01 grams, 95%CI = −0.04, 0.06, p = 0.75) nor fat (B = 0.09 grams, 95%CI = −0.02, 0.20, p = 0.10) predicted subsequent carbohydrate intake.
3.3.3. Fat Intake.
There were no significant lagged associations between prior macronutrient meal content and subsequent meal fat content (Table 3).
3.4. Daily Total KCAL
Exploration of total daily energy intake revealed a marginally significant difference by day [Type III Fixed Effect F(2, 570) = 3.11, p = 0.05]. Total energy intake was significantly higher on day one (LS Mean = 4041.43, 95% CI =3860.85, 4222.00), compared to day three (LS Mean = 3877.02, 95% CI =3696.91, 4057.14) [Tukey adjusted p = .02]. There were no differences between day 1 and day 2 (Tukey adjusted p = .06) or between day 2 and day 3 (Tukey adjusted p = 0.50). Table 4 presents parameter estimates for total energy intake across the three-day vend period. Each specific macronutrient intake was associated with increased energy intake the following day [Protein B = 4.31 kcal, 95%CI = 1.40, 7.22, p = 0.0039; Carbohydrates B = 3.24 kcal, 95%CI = 2.49, 3.99, p<.0001; Fat B = 5.46 kcal, 95%CI = 3.51, 7.41, p <.0001].
Table 4. Daily total caloric intake was predicted by protein, carbohydrate, and fat intake from the subsequent day (multilevel lag model).
The daily total macronutrient intake was calculated and lagged such that the macronutrients were predictors for next day total kilocalorie intake. Results from the multilevel model find that increased protein, carbohydrate, and fat intake from the day prior predicted increased daily total kilocalorie from the following day.
| Daily Total KCAL | ||||
|---|---|---|---|---|
| B | SE | 95% CI | p | |
| Age | −3.06 | 3.36 | −9.68, 3.56 | 0.36 |
| Male | −47.85 | 131.90 | −307.49, 211.80 | 0.72 |
| Female | Ref | |||
| Black | -322.69 | 124.69 | −568.15, −77.22 | 0.0102 |
| Caucasian | −105.79 | 94.30 | −291.42, 79.85 | 0.26 |
| Hispanic | −158.80 | 158.67 | −471.15, 153.54 | 0.32 |
| Other | −62.25 | 116.32 | −291.22, 66.72 | 0.59 |
| American Indian | Ref | |||
| Fat Free Mass Index | 62.30 | 21.69 | 19.60, 104.99 | 0.0044 |
| Fat Mass Index | −11.35 | 10.30 | −31.62, 8.91 | 0.27 |
| Total Protein Lag (g) | 4.31 | 1.48 | 1.40, 7.22 | 0.0039 |
| Total Carbohydrates Lag (g) | 3.24 | 0.38 | 2.49, 3.99 | <.0001 |
| Total Fat Lag (g) | 5.46 | 0.99 | 3.51, 7.41 | <.0001 |
Bolded coefficients are statistically significant (p <.05)
3.5. Daily Macronutrient Content
3.5.1. Total Protein Intake.
Total daily protein intake was positively associated with next-day protein intake (Table 4; B = 0.72 grams, 95%CI = 0.59, 0.84, p <.0001) but not with next day carbohydrate or fat intake.
3.5.2. Total Carbohydrate Intake.
Total carbohydrate intake was positively associated with carbohydrate intake the following day (Table 4; B = 0.71 grams, 95% CI = 0.62, 0.81, p <.0001) but not with next day protein or fat intake.
3.5.3. Total Fat Intake.
Carbohydrates and fat intake were positively associated with next day total fat intake [Table 4; Carbohydrates B = 0.05 grams, 95% CI = 0.01, 0.09, p = 0.0163; Fat B = 0.53, 95% CI = 0.43, 0.64, p < .0001].
3.6. Sensitivity Analyses
3.6.1. Glucose Values.
Additional sensitivity analyses were performed that accounted for plasma glucose values at fasting and 120 minutes. Inclusion of both glucose covariates in the model did not alter the patterning of the results.
3.6.2. Secular trends in food consumption.
Inclusion of admission date (as a way to control for secular trends) with and without the glucose covariates, did not alter the patterning of the results of the meal-to-meal and daily models.
4. Discussion
Analyzing meal to meal data from our ad libitum vending machine paradigm, we found that protein consumption, but not carbohydrate or fat intake from the meal prior was associated with less total calorie consumption at the next meal, while accounting for key confounders such as adiposity (fat and fat free mass indices). Higher protein consumption was also associated with less protein and carbohydrate intake at subsequent meals. There was no meal-to-meal effect of protein on fat intake. Conversely, between-day analyses demonstrated that macronutrient patterns remain consistent daily. Protein, carbohydrate, and fat intake were associated with specific macronutrient intake on the following day. These results indicate that during ad libitum periods of intake, meal protein content affects subsequent meal calorie and protein content resulting in overall stable day-to-day intake.
Homeostatic models of energy intake posit that food consumption should be tightly regulated and previous meal composition should modify timing, macronutrient content, and size of subsequent meal. However, the regulatory effect of calorie or macronutrient content from meal-to-meal or day to day may not be very strong. (20). Nevertheless, there is evidence of negative associations between day-to-day macronutrient intake and macronutrient-specific regulatory effects (20, 21). The duration of these effects remains in doubt although previous authors have concluded that these regulatory effects may last as long as a week, although with substantial variability. Using our ad libitum paradigm, we were able to identify an association of protein intake on subsequent meal calorie, protein, and carbohydrate intake, such that higher meal protein content was associated with reduced calorie, protein and carbohydrate intake at the next meal. However, this apparent negative regulatory effect did not translate to the day-to-day intake. The differences in previous findings versus our own may be attributed to the varying study design (20). Other studies that have found contrasting results to ours have relied on a self-report on composition and amount of food consumed (21). Other studies which have investigated meal to meal macronutrient intake found that (1) variability of protein consumption (i.e., standard deviation), relative to other macronutrients is small compared to fat and carbohydrate and consistent with our findings (7, 22), (2) meal protein intake reduces subsequent meal carbohydrate and energy intake and/or (23, 24, 25), (3) meal protein also reduces subsequent meal protein intake(8). Our results confirm the meal-to-meal observations but in a less controlled ad libitum condition. Because participants ate over several days, we were able to dissect out meal to meal versus day-to-day associations demonstrating that these effects appear to be very short term and enable more daily consistency in macronutrient intake.
Protein is essential for health, growth, and somatic maintenance (26). Daily protein turnover can reach as high as 300 g (27), requiring an obligate daily protein requirement of ~ 1 g/kg of body weight to replenish loss (28).The importance of protein in somatic effort and upkeep suggests that physiological mechanisms must be set in place to regulate intake. Regulation of protein intake and macronutrient balance may be driven by secretion of fibroblast growth factor 21 (FGF21)(29). FGF21 is a hormone produced by the liver and communicates with the brain. Human and non-human animal research suggests that diets characterized by low protein intake may increase levels of circulating FGF21, signaling to the organism the need adjust energy intake to compensate for restricted consumption of protein (30, 31, 32, 33). Cholecystokinin (CCK) is another possible important regulator of protein, as it may mediate the association between protein consumption and satiety (34). Following high protein preloads, overweight participants increase CCK secretion and consume smaller meals compared to consumption of glucose preloads (35). CCK is a plausible hormone to explain meal to meal variation because of the short duration if its effect. Meal protein content also alters satiety hormones. In a cross-over design of 25 men (12 overweight/obese, 13 normal weight), participants were fed three meals in randomized order of varying levels of protein (14%, 25%, 50%), with 4-week washout between meals and tests(36). A fasting blood draw and a subsequent series of postprandial blood tests revealed a protein dose-response increase in satiety- and appetite-related hormones, GLP-1, PPY, and glucagon.
Lower protein content might be a longer-term driver for increased calorie consumption if the available overall food is low in protein at most meals (37, 38). Quality foods with greater protein content tend to be more expensive (39) and may not be widely available in food swamps (i.e., environments characterized by an abundance of low quality or ultra-processed food choices). Instead, ultra-processed foods high in carbohydrate and fat content may be driving excess energy intake to compensate for diluted levels of protein present in the meals (40, 41). A two-week randomized crossover trial comparing the effects of ultra-processed foods to whole un-processed foods found that participants consumed over 400 more calories – mainly from carbs and fats – when given access to processed food choices, in comparison to unprocessed foods (42). Interestingly, there was no significant difference in protein intake between the whole un-processed foods (15.6% of intake) and ultra-processed foods (14% of intake) groups. The authors hypothesize that protein regulation may be fueling this finding.
We acknowledge that despite the use of a validated ad libitum model, our findings may be limited to experimentally controlled conditions and we are uncertain if they apply to food choices of free-living humans outside of the laboratory. The food selections available to participants via the preliminary food preference scores of the ad libitum model are not necessarily low in protein, which limits the interpretation of the findings as protein leverage. It is also important to acknowledge that a formal test of protein leverage (as oppose to protein regulation) mechanisms in an ad libitum setting would require experimentally constraining macronutrient content (i.e., limit food choices) and measure total energy intake to achieve a target intake of protein. Additionally, ad libitum food consumption was assessed over a 3-day period, which may be a limited amount of time to assess any long-term regulatory effects. However, a strength of the study is that this is a true ad libitum paradigm with directly measured energy intake. Sensory specific satiety is the concept that highly preferred foods will decrease in preference following consumption. It is possible that this phenomenon may alter the patterns of consumptive behavior. The order of consumed foods might represent sensory specific satiety, but we are not able to assess this within this paradigm. Finally, we did not have meal to meal hormonal measures so are unable to confirm the physiological mechanisms that underpin these findings.
Conclusion
To summarize, we found evidence that regulation of meal-to-meal energy intake and macronutrient content is associated with prior ingestion levels of protein, at least in the short term. Conversely, daily-level analyses did not provide evidence of such regulation, implying that in the setting of immediately available ad libitum food of varying protein content, protein regulation plays a role over meals rather than days. These results indicate that mechanisms that regulate macronutrient content may vary based on temporal length of assessment and food availability. Shorter temporal lengths may be more tightly regulated by protein ingestion, while longer temporal lengths are regulated by habitual patterning of macronutrient ingestion. If this is the case, then increasing availability of high protein foods in settings of low-quality low protein choices might offset overconsumption.
Supplementary Material
Table 5. Multilevel lag models predicting increased macronutrient consumption from macronutrient intake from the day prior.
Daily macronutrient content (protein, carbohydrates, and fat) were calculated and lagged. Three separate multilevel models were calculated predicting subsequent daily macronutrient intake. Increased protein intake from the day prior predicted increased protein intake the subsequent day. The same patterning was found with carbohydrates. Subsequent daily fat intake was predicted by prior carbohydrate and fat intake
| Daily Protein |
Daily Carbohydrates |
Daily Fat |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | 95% CI | p | B | SE | 95% CI | p | B | SE | 95% CI | p | |
| Age | 0.03 | 0.09 | −0.15, 0.22 | 0.74 | −0.12 | 0.43 | −0.96, 0.72 | 0.78 | −0.28 | 0.19 | −0.66, 0.10 | 0.14 |
| Male | −2.13 | 3.88 | −9.77, 5.52 | 0.58 | 3.58 | 16.60 | −29.09, 36.25 | 0.83 | −4.50 | 7.89 | −20.04, 11.05 | 0.57 |
| Female | Ref | Ref | Ref | |||||||||
| Black | −3.09 | 5.29 | −13.50, 7.32 | 0.56 | −44.22 | 15.94 | −75.59, −12.84 | 0.0059 | −15.40 | 8.64 | −32.40, 1.61 | 0.08 |
| Caucasian | −1.43 | 2.96 | −7.26, 4.39 | 0.63 | −16.46 | 10.84 | −37.80, 4.89 | 0.13 | −5.03 | 5.88 | −16.62, 6.55 | 0.39 |
| Hispanic | −4.84 | 3.72 | −12.17, 2.50 | 0.20 | −2.69 | 26.04 | −53.95, 48.57 | 0.92 | −15.70 | 7.96 | −31.37, −0.03 | 0.05 |
| Other | 7.84 | 4.56 | −1.13, 16.82 | 0.09 | −23.51 | 15.09 | −53.21, 6.19 | 0.12 | −1.00 | 6.81 | −14.40, 12.41 | 0.88 |
| American Indian | Ref | Ref | Ref | |||||||||
| Fat Free Mass Index | 2.22 | 0.63 | 0.98, 3.45 | 0.0005 | 5.26 | 2.73 | −0.12, 10.64 | 0.06 | 3.52 | 1.25 | 1.06, 5.98 | 0.0052 |
| Fat Mass Index | −0.44 | 0.32 | −1.07, 0.19 | 0.17 | −1.34 | 1.34 | −3.98, 1.31 | 0.32 | −0.33 | 0.60 | −1.50, 0.84 | 0.58 |
| Total Protein Lag (g) | 0.72 | 0.06 | 0.59, 0.84 | <.0001 | 0.11 | 0.19 | −0.27, 0.49 | 0.58 | 0.10 | 0.08 | −0.06, 0.26 | 0.20 |
| Total Carbohydrates Lag (g) | 0.01 | 0.01 | −0.01, 0.04 | 0.23 | 0.71 | 0.05 | 0.62, 0.81 | <.0001 | 0.05 | 0.02 | 0.01, 0.09 | 0.0163 |
| Total Fat Lag (g) | 0.00 | 0.04 | −0.07, 0.07 | 0.91 | 0.12 | 0.13 | −0.13, 0.38 | 0.35 | 0.53 | 0.06 | 0.43, 0.64 | <.0001 |
Bolded coefficients are statistically significant (p <.05)
Acknowledgments
This study was funded by the Intramural Research Program of the NIH and the NIDDK. The funders had no role in study design, data collection and analysis, the decision to publish, or preparation of the manuscript.
Data described in the article will be made available upon request pending application and approval by the Institutional Review Board of the NIDDK
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Competing Interests: The authors declare no competing financial interests
Clinical Trial Registry: ClinicalTrials.gov identifier NCT00342732
Ethics Statement
A subset of participants (n = 287) from The Food Intake Phenotype study (ClinicalTrials.gov identifier NCT00342732) was used for the present set of analyses. The Food Intake study was a 10-day clinical trial designed to examine and classify eating patterns and behavior in a sample of healthy participants without diabetes (see (11, 12, 13, 14, 15) for additional background and findings derived from this cohort). The trial began in November 1999 and is ongoing. Procedures for the clinical trial (described below) were approved by the NIDDK Institutional Review Board (OH99-DKN019). Participants enrolled in the study provided written informed consent.
References
- 1.Flatt JP. The difference in the storage capacities for carbohydrate and for fat, and its implications in the regulation of body weight. Ann N Y Acad Sci 1987;499: 104–123. [DOI] [PubMed] [Google Scholar]
- 2.Flatt JP. Dietary fat, carbohydrate balance, and weight maintenance. Ann N Y Acad Sci 1993;683: 122–140. [DOI] [PubMed] [Google Scholar]
- 3.Flatt JP. Use and storage of carbohydrate and fat. Am J Clin Nutr 1995;61: 952S–959S. [DOI] [PubMed] [Google Scholar]
- 4.Simpson SJ, Raubenheimer D. Obesity: the protein leverage hypothesis. Obes Rev 2005;6: 133–142. [DOI] [PubMed] [Google Scholar]
- 5.Raubenheimer D, Simpson SJ. Protein Leverage: Theoretical Foundations and Ten Points of Clarification. Obesity (Silver Spring) 2019;27: 1225–1238. [DOI] [PubMed] [Google Scholar]
- 6.Martinez-Cordero C, Kuzawa CW, Sloboda DM, Stewart J, Simpson SJ, Raubenheimer D. Testing the Protein Leverage Hypothesis in a free-living human population. Appetite 2012;59: 312–315. [DOI] [PubMed] [Google Scholar]
- 7.Lieberman HR, Fulgoni VL, Agarwal S, Pasiakos SM, Berryman CE. Protein intake is more stable than carbohydrate or fat intake across various US demographic groups and international populations. Am J Clin Nutr 2020;112: 180–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.de Castro JM, Elmore DK. Subjective hunger relationships with meal patterns in the spontaneous feeding behavior of humans: Evidence for a causal connection. Physiology & Behavior 1988;43: 159–165. [DOI] [PubMed] [Google Scholar]
- 9.Martens EA, Lemmens SG, Westerterp-Plantenga MS. Protein leverage affects energy intake of high-protein diets in humans. Am J Clin Nutr 2013;97: 86–93. [DOI] [PubMed] [Google Scholar]
- 10.Bluher M Obesity: global epidemiology and pathogenesis. Nat Rev Endocrinol 2019;15: 288–298. [DOI] [PubMed] [Google Scholar]
- 11.Stinson EJ, Piaggi P, Ibrahim M, Venti C, Krakoff J, Votruba SB. High Fat and Sugar Consumption During Ad Libitum Intake Predicts Weight Gain. Obesity (Silver Spring) 2018;26: 689–695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bundrick SC, Thearle MS, Venti CA, Krakoff J, Votruba SB. Soda consumption during ad libitum food intake predicts weight change. J Acad Nutr Diet 2014;114: 444–449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gluck ME, Venti CA, Salbe AD, Krakoff J. Nighttime eating: commonly observed and related to weight gain in an inpatient food intake study. Am J Clin Nutr 2008;88: 900–905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Salbe AD, Tschop MH, DelParigi A, Venti CA, Tataranni PA. Negative relationship between fasting plasma ghrelin concentrations and ad libitum food intake. J Clin Endocrinol Metab 2004;89: 2951–2956. [DOI] [PubMed] [Google Scholar]
- 15.Venti CA, Votruba SB, Franks PW, Krakoff J, Salbe AD. Reproducibility of ad libitum energy intake with the use of a computerized vending machine system. Am J Clin Nutr 2010;91: 343–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ferraro R, Boyce VL, Swinburn B, De Gregorio M, Ravussin E. Energy cost of physical activity on a metabolic ward in relationship to obesity. Am J Clin Nutr 1991;53: 1368–1371. [DOI] [PubMed] [Google Scholar]
- 17.American Diabetes A Diagnosis and classification of diabetes mellitus. Diabetes Care 2007;30 Suppl 1: S42–47. [DOI] [PubMed] [Google Scholar]
- 18.Geiselman PJ, Anderson AM, Dowdy ML, West DB, Redmann SM, Smith SR. Reliability and Validity of a Macronutrient Self-Selection Paradigm and a Food Preference Questionnaire 11P. J. G. and M. L. D. are also affiliated with the Department of Psychology, Louisiana State University, Baton Rouge, LA. Physiology & Behavior 1998;63: 919–928. [DOI] [PubMed] [Google Scholar]
- 19.Weise CM, Hohenadel MG, Krakoff J, Votruba SB. Body composition and energy expenditure predict ad-libitum food and macronutrient intake in humans. Int J Obes (Lond) 2014;38: 243–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.de Castro JM. The Control of Eating Behavior in Free-Living Humans. 2004;14: 469–504. [Google Scholar]
- 21.de Castro JM. Prior day’s intake has macronutrient-specific delayed negative feedback effects on the spontaneous food intake of free-living humans. J Nutr 1998;128: 61–67. [DOI] [PubMed] [Google Scholar]
- 22.Gosby AK, Conigrave AD, Raubenheimer D, Simpson SJ. Protein leverage and energy intake. Obes Rev 2014;15: 183–191. [DOI] [PubMed] [Google Scholar]
- 23.Booth DA, Chase A, Campbell AT. Relative effectiveness of protein in the late stages of appetite suppression in man. Physiology & Behavior 1970;5: 1299–1302. [DOI] [PubMed] [Google Scholar]
- 24.Anderson GH, Moore SE. Dietary proteins in the regulation of food intake and body weight in humans. J Nutr 2004;134: 974S–979S. [DOI] [PubMed] [Google Scholar]
- 25.Latner JD, Schwartz M. The effects of a high-carbohydrate, high-protein or balanced lunch upon later food intake and hunger ratings. Appetite 1999;33: 119–128. [DOI] [PubMed] [Google Scholar]
- 26.Morrison CD, Laeger T. Protein-dependent regulation of feeding and metabolism. Trends Endocrinol Metab 2015;26: 256–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tome D Protein: what’s on in research on clinical nutrition. Eur J Clin Nutr 2018;72: 1215–1220. [DOI] [PubMed] [Google Scholar]
- 28.Elango R, Humayun MA, Ball RO, Pencharz PB. Evidence that protein requirements have been significantly underestimated. Curr Opin Clin Nutr Metab Care 2010;13: 52–57. [DOI] [PubMed] [Google Scholar]
- 29.Hill CM, Qualls-Creekmore E, Berthoud HR, Soto P, Yu S, McDougal DH, et al. FGF21 and the Physiological Regulation of Macronutrient Preference. Endocrinology 2020;161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Laeger T, Henagan TM, Albarado DC, Redman LM, Bray GA, Noland RC, et al. FGF21 is an endocrine signal of protein restriction. J Clin Invest 2014;124: 3913–3922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Basolo A, Begaye B, Hollstein T, Vinales KL, Walter M, Santini F, et al. Effects of Short-Term Fasting and Different Overfeeding Diets on Thyroid Hormones in Healthy Humans. Thyroid 2019;29: 1209–1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hill CM, Laeger T, Dehner M, Albarado DC, Clarke B, Wanders D, et al. FGF21 Signals Protein Status to the Brain and Adaptively Regulates Food Choice and Metabolism. Cell Rep 2019;27: 2934–2947 e2933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vinales KL, Begaye B, Bogardus C, Walter M, Krakoff J, Piaggi P. FGF21 Is a Hormonal Mediator of the Human “Thrifty” Metabolic Phenotype. Diabetes 2019;68: 318–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Brennan IM, Luscombe-Marsh ND, Seimon RV, Otto B, Horowitz M, Wishart JM, et al. Effects of fat, protein, and carbohydrate and protein load on appetite, plasma cholecystokinin, peptide YY, and ghrelin, and energy intake in lean and obese men. Am J Physiol Gastrointest Liver Physiol 2012;303: G129–140. [DOI] [PubMed] [Google Scholar]
- 35.Bowen J, Noakes M, Trenerry C, Clifton PM. Energy intake, ghrelin, and cholecystokinin after different carbohydrate and protein preloads in overweight men. J Clin Endocrinol Metab 2006;91: 1477–1483. [DOI] [PubMed] [Google Scholar]
- 36.Belza A, Ritz C, Sorensen MQ, Holst JJ, Rehfeld JF, Astrup A. Contribution of gastroenteropancreatic appetite hormones to protein-induced satiety. Am J Clin Nutr 2013;97: 980–989. [DOI] [PubMed] [Google Scholar]
- 37.Cabeza de Baca T, Durazo EM, Rodriguez F. Achieving Optimal Cardiovascular Health: a Social Epidemiological Approach. Current Epidemiology Reports 2018;5: 262–271. [Google Scholar]
- 38.Raubenheimer D, Simpson SJ. Nutritional Ecology and Human Health. Annu Rev Nutr 2016;36: 603–626. [DOI] [PubMed] [Google Scholar]
- 39.Brooks RC, Simpson SJ, Raubenheimer D. The price of protein: combining evolutionary and economic analysis to understand excessive energy consumption. Obes Rev 2010;11: 887–894. [DOI] [PubMed] [Google Scholar]
- 40.Martinez Steele E, Raubenheimer D, Simpson SJ, Baraldi LG, Monteiro CA. Ultra-processed foods, protein leverage and energy intake in the USA. Public Health Nutr 2018;21: 114–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rolls BJ, Cunningham PM, Diktas HE. Properties of Ultraprocessed Foods That Can Drive Excess Intake. Nutrition Today 2020;55: 109–115. [Google Scholar]
- 42.Hall KD, Ayuketah A, Brychta R, Cai H, Cassimatis T, Chen KY, et al. Ultra-Processed Diets Cause Excess Calorie Intake and Weight Gain: An Inpatient Randomized Controlled Trial of Ad Libitum Food Intake. Cell Metab 2019;30: 67–77 e63. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


