Abstract
Climate change is imposing increasingly severe impacts on public health. Addressing these impacts requires heightened awareness of climate-driven health conditions and appropriate clinical practices to manage these conditions. Within this context, the 2nd Annual Clinical Climate Change Conference, held January 24, 2020 at the New York Academy of Medicine, brought together more than 150 allied health practitioners from across the United States for a one-day conference showcasing the state of the science on the climate and health. Eight platform presentations—including a keynote address from Karenna Gore of the Center for Earth Ethics at Union Theological Seminary—covered a range of environmentally induced, climate-related disease areas as well as topics related to environmental justice. Additionally, key workshops engaged participants in the clinical management of climate-related health conditions. Communicating the existing evidence base for climate change-driven impacts on human health is crucial for preparing practitioners to identify and address these impacts. Further partnership between researchers and practitioners to extend and disseminate this evidence base will yield important advancements toward protecting patients and improving health outcomes in an era of climate crisis.
Keywords: climate change, environmental health, evidence-based medicine, public health
Introduction
The years 2015–2019 were the five warmest years since record-keeping began in 18801. Extreme heat and other severe weather events are increasing in frequency and scale, producing critical threats on human health. Health-related impacts of climate change range from heat-related illnesses to infectious, respiratory, and cardiovascular diseases; nutritional deficiencies and food and water insecurity; and mental health conditions (Figure 1). The World Health Organization highlights climate change as a significant driver of the rapid rises in non-communicable diseases (e.g., respiratory and cardiometabolic diseases) worldwide2. Recognizing and managing these conditions is crucial to protect human health in our changing climate.
Figure 1:
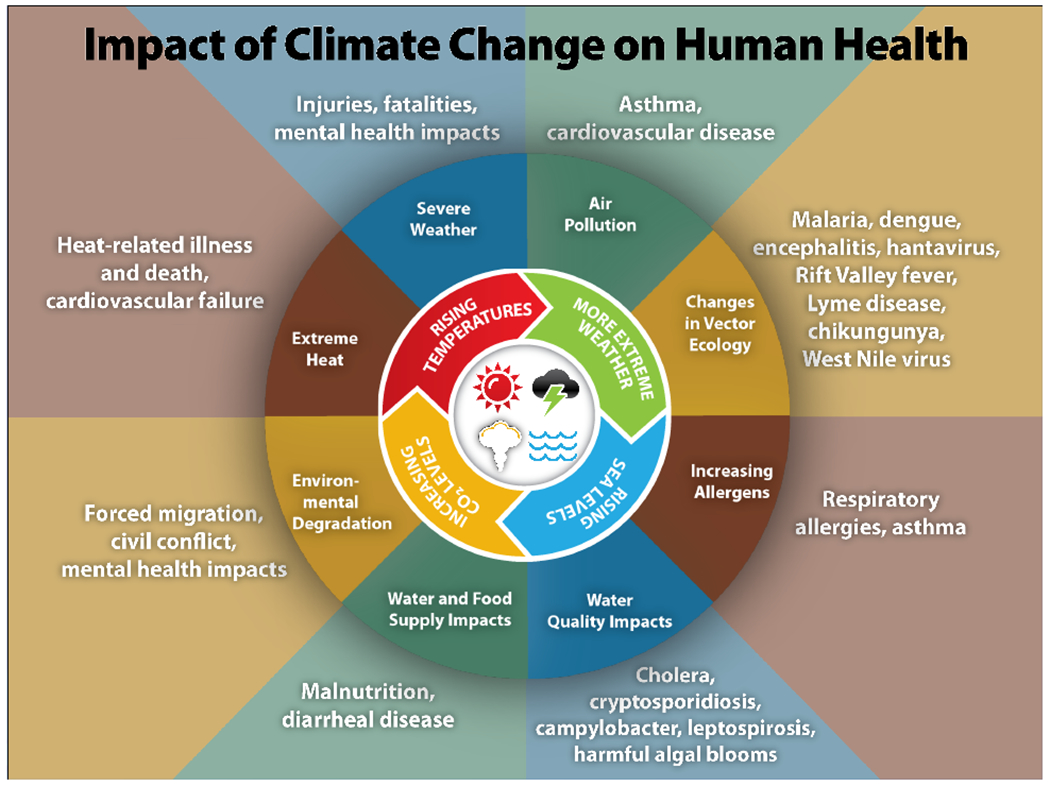
Climate change influences myriad health outcomes through multiple pathways. Rising temperatures, more extreme weather, rising sea levels, and increasing carbon dioxide levels have both direct effects on health and indirect effects through affecting other environmental factors (water and food security and quality, pollution) that affect health. From the U.S. Centers for Disease Control and Prevention32.
To provide allied health practitioners with an evidence base to address climate-driven health impacts, the Mount Sinai Institute for Exposomic Research instituted an annual Clinical Climate Change Conference. The second annual meeting, Clinical Climate Change 2020, held January 24, 2020 at the New York Academy of Medicine, highlighted the latest research and clinical updates on disease areas impacted by climate change (see Table 1 for a summary of presentations; for full meeting details and video recordings, see https://www.clinicalclimatechange.com/2020). More than 150 clinicians and allied health professionals from across the United States (U.S.) attended to learn about the current state of science cardiovascular and respiratory diseases, heat-related illnesses, allergies and asthma, vector-borne and waterborne illness, mental health, and nutrition, as well as policies aimed at protecting workforces and the general population from a wide variety of environmentally induced health conditions. We summarize these contributions to highlight the burgeoning climate-related health issues for incorporation into clinical research and practice.
Table 1:
Clinical Climate Change 2020, Conference Presentations
| Presenter(s) | Presentation Title |
| Karenna Gore, Founder and Director, Center for Earth Ethics, Union Theological Seminary | Health Care in the Time of Climate Crisis: An Earth Ethics Perspective |
| Robert Wright, MD, Chair, Department of Environmental Medicine and Public Health; Co-Director, Mount Sinai Institute for Exposomic Research; Icahn School of Medicine at Mount Sinai (ISMMS) | Exposomics and Climate Change |
| Allan Just, PhD, Assistant Professor, Department of Environmental Medicine and Public Health, ISMMS | Climate Change and Environment Exposures |
| Nick DeFelice, PhD, Assistant Professor, Department of Environmental Medicine and Public Health, ISMMS | Seasonal Cycles of Infectious Diseases |
| Jodi Sherman, MD, Associate Professor, Anesthesiology and Epidemiology; Director of Sustainability; Yale School of Medicine | Balancing Patient Safety and Public Health: The Dilemma of Health Care Pollution |
| Surili Patel, Deputy Director, Center for Public Health Policy, American Public Health Association | Justice in the Era of Climate Crisis |
| Lewis Ziska, PhD, Associate Professor, Columbia University | Role of Rising CO2 on Nutritional Quality |
| Albert Rizzo, MD, Chief Medical Officer, American Lung Association | The “State of the Air” and 50th Anniversary of the Clean Air Act |
|
Albert Rizzo, MD, Chief Medical Officer, American Lung Association Emily Senay, MD, Assistant Professor, Department of Environmental Medicine and Public Health, ISMMS Erin Thanik, MD, Assistant Professor, Department of Environmental Medicine and Public Health, ISMMS |
Workshop A: Managing Respiratory and Cardiovascular Diseases |
|
Roberto Lucchini, MD, Professor, Occupational and Environmental Medicine, School of Public Health, Florida International University Ismail Nabeel, MD, Deputy Medical Director of Employee Health, Safety, and Wellness, Mount Sinai Health System Perry Sheffield, MD, Associate Professor, Department of Pediatrics, ISMMS |
Workshop B: Managing Heat Exposure in Vulnerable Populations |
Exposomics and Climate Change
Environmental factors are increasingly linked to myriad health outcomes, and many of these factors are susceptible to climate change. One approach to uncovering how climate-related exposures affect health over time is through exposomics3, 4. The ‘exposomics’ concept reflects the totality of environmental exposures throughout a lifetime5; such exposures are ubiquitous and dynamic.
Exposomics leverages numerous technologies to capture these exposures: from laboratory assays of biological samples like blood, urine, and hair to capture the ‘internal exposome’, to estimates based on satellite and remote sensing, geospatial mapping, and wearable devices to measure population- and individual-level ‘external exposomes’. Such studies can be either targeted (measuring pre-specified types of exposures) or untargeted (measuring all potential exposures) to reveal how various climate-related factors influence health. Untargeted exposomics analyses are increasingly important given that exposures are complex and that climate change exerts a combination of direct effects along with more indirect, or ‘butterfly’, effects.
For example, heat waves produce direct effects on injury and mortality, particularly for populations experiencing poverty or living in urban areas. On the other hand, chronic kidney disease of unknown origin is increasingly common among certain agricultural communities, likely as a butterfly effect of environmental exposures. Applying exposomics approaches to longitudinal and geospatial data on temperature variation (hot weather) and pesticide exposures may help to identify the combinations of these factors that are propagating chronic kidney disease6. For these and many other conditions, leveraging the power of exposomics to assess both direct and indirect effects of climate change may help to pinpoint problems for both the environment and human health.
Highlights:
Exposomics provides a powerful approach to generate critical insights on how climate-related environmental exposures influence public health over time.
While direct effects are closely studied, the more complex indirect, or ‘butterfly,’ effects from climate change could have important adverse effects on both the environment and health.
Climate Change and Environmental Exposures
The changing climate produces three major phenomena that affect environmental exposures: an increased frequency of extreme heat events exacerbated in cities by the urban heat island effect7; an increased frequency of air inversion and stagnation events8; and an increased frequency, severity, and duration of wildfires9. Each of these phenomena promotes worsened air quality; in the case of wildfires, poor air quality can be experienced thousands of miles from the wildfires themselves10. Air pollutants, especially fine particulate matter (PM2.5), are a known toxicant associated with cardiovascular disease11, kidney disease12, and poor birth outcomes13, along with mortality14, 15.
Linking air pollution to health outcomes was previously limited by the sparsity of ground monitors used to measure pollutants and associate those measures to the health of people who lived or worked near those monitors16, 17. Advances in satellite remote sensing systems and modeling now enable accurate reconstructions of both fine particulate matter (PM2.5) air pollution and temperature variation at fine scales over large areas18, 19. These models generate billions of predictions that can then be linked to health outcome measures to uncover the dynamic effects of these environmental exposures impacted by climate change on population health.
Highlights:
Advanced methods for detecting climate-related changes in air pollution and temperature enable linkage to health outcomes among populations, as well as forecasting to predict climate-related health threats.
Seasonal Cycles of Infectious Disease
Forecasting is also crucial for interrupting infectious disease transmission. Changes in the climate alter the habitat range and transmission cycles for vector-borne pathogens20, introducing disease to new or expanded areas. For example, as the northeastern U.S. has experienced a warming climate over recent decades, the tick-borne illness Lyme disease has become more widespread and prevalent21. Similarly, West Nile virus, transmitted by mosquitos where birds are the reservoir host, first emerged in the U.S. in 199922, and has since expanded in range, with multiple severe outbreaks over this time.
Preventing such outbreaks requires information on where and when transmissions are most likely to occur. Forecasting models offer critical insights by incorporating multiple climate-related aspects, such as temperature and humidity variations4. Synthesizing surveillance data (e.g., mosquito monitoring), reported cases, climatology, and a mathematical model representing the transmission dynamics of WNV among mosquitoes and birds, as well as spillover to humans23–25 enables predictions of when transmission is most likely to occur. Such information can inform interventions (e.g., alert the public to future periods of elevated WNV spillover transmission risk, and identify when to intensify blood donor screening) and other measures to avert outbreaks.
Highlights:
Climate-related factors like rising temperature, changes in precipitation, and increased humidity alter the habitats, life cycles, and disease transmission rates of vectors like ticks and mosquitos.
Infectious disease forecasting can provide public health professionals with up-to-date information to recognize, treat, and plan for the rapidly changing infectious disease landscape.
Role of Rising Carbon Dioxide on Nutritional Quality
A key link between climate and health relates to the changing climate’s effects on nutrition sources26. Plants require different nutrient balances to support growth; all plants derive carbon from the air, but pull other nutrients from the soil. As atmospheric CO2 continues to rise rapidly, soil nutrients are not increasing in parallel. Some plants—for example, poison ivy—thrive under higher CO2 levels; other plants, however, respond poorly to this increased CO2. In particular, rice is an important human food source that is exhibiting a significantly altered nutritional profile from the skewed carbon to nitrogen availability. Such changes have nutritional and health consequences not only for humans consuming plants, but also for livestock and pollinators27.
Importantly, changing CO2 affects plant biology in other ways that can impact human health. For example, altered plant growth may affect plant combustibility, which may further exacerbate threats from wildfires. Some plants will produce altered compounds and protein contents, which can have important implications for irritants or allergens that affect humans28. Further research into the impact of excess atmospheric CO2 is needed to determine ways to mitigate or harness its effects on plants, particularly to ensure food security and ecosystem balance.
Highlights:
Rising atmospheric CO2 alters plant nutrient quality, including among human and livestock food sources, which poses a threat to food security and nutrition.
Changes in atmospheric CO2 may alter the growth and combustibility of plants associated with fire outbreaks, leading to increased potential to burn during dry, hot conditions associated with climate change.
Balancing Patient Safety and Public Health: The Dilemma of Healthcare Pollution
Given the widespread and increasing effects of climate on human health, climate change is now considered a medical emergency. Yet, the healthcare sector itself produces substantial amounts of pollution, including greenhouse gas emissions. Despite the highest per-capita spend on healthcare, and the highest per-capita healthcare greenhouse gas emissions, the U.S. does not have the highest life expectancy or maternal-fetal outcomes, suggesting that changes in the industry are necessary to improve healthcare quality. Engaging healthcare professionals around healthcare pollution is key for public policy and societal transformation and aligns with practitioners’ mandate to ‘do no harm’29.
The environmental impacts of healthcare stem from the industry’s position as a major resource consumer: hospitals are energy-intensive, safety regulations require unique protocols (e.g., for infection prevention), business models drive a wasteful and unnecessary utilization of resources, and there is a culture of disposability. For example, facilities and practitioners implement single-use medical devices and equipment under the aegis of improved safety/infection prevention and lower costs; yet, these disposable resources do not significantly prevent infection and, in fact, drive up costs30. Further, medical supplies undergo an entire life cycle from manufacture to use, and the environmental impacts of each of these stages must be considered to inform the selection of products and processes with lower impacts. Beyond waste related to disposable healthcare materials, hospitals produce major emissions in their use of inhaled anesthetics and energy and resources needed to support high-tech diagnostic and intervention approaches. Importantly, portions of the healthcare sector have instituted sustainability practices around pollution prevention and are making strides toward reducing their environmental impacts.
Highlights:
Patient safety and public safety are one in the same, and public health is directly damaged by healthcare emissions and wastes. Pollution prevention is the new patient safety movement.
Clinicians have an important responsibility to consider healthcare waste and emissions; undertaking sustainability practices can reduce these impacts as well as improve patient and population outcomes.
Healthcare in the Time of Climate Crisis: An Earth Ethics Perspective
Addressing the climate crisis and its impacts on population health requires diverse approaches. As one example, an ethical framework presents a unique and important perspective in addressing the climate crisis. This perspective centers around the concept that morality can serve as a driving and organizing principle that motivates people to take action. For example, faith-based organizations frequently mobilize quickly to provide aid in environmental disasters. Religion and morality drive behaviors and shared values that can be used to promote positive change, particularly for the benefit of vulnerable populations—those most likely to be harmed but least likely to have a voice. Within such a framework, public health experts and health practitioners must take action to promote healing of the planet and its people without doing further harm.
The planet is currently experiencing a ‘health crisis’ that affects the health of all its inhabitants. Practitioners are increasingly noting that the many adverse health outcomes promulgated by climate change include mental health concerns. For example, ‘eco-anxiety’ and climate grief are psychological manifestations associated with fear, resignation, empathy for those suffering the traumatic events associated with climate change, and even a failure to act to resolve climate change. These phenomena highlight the need to promote psychological resiliency in parallel with fostering better connections and reciprocity with nature. Public health campaigns that embrace an Earth ethics perspective can be crucial to call for healing of the planet and its population, while also fulfilling a ‘duty to warn’ of the dangers of this continued crisis.
Highlights:
The health of the planet is closely tied with human health, and the largest impacts of climate change will fall on populations least likely to have a voice.
An ethical framework for resolving climate change can leverage organizing power and shared values that transcend politics.
Decisions and actions taken today to address climate change must be considered for their impact on future generations.
Justice in the Era of Climate Change
As the healthcare community considers how best to prepare for the increase in adverse health outcomes related to climate change, it must also consider redressing environmental injustice via diverse perspectives and multi-pronged solutions. Climate change exerts impacts on all populations, independent of age, race/ethnicity, income, and myriad other factors. Yet, many of these factors influence whether some populations will be more resilient to the effects of climate change. Promoting climate justice requires the consideration of vulnerable populations including giving a voice to the needs and welfare of children, aging individuals, and communities of color7.
Crucially, solutions to climate injustice must incorporate approaches for psychosocial resilience. Mental health disorders are an ‘invisible’ outcome promulgated by acute, gradual, and indirect effects of climate change. Further, roughly 80% of what people need to be healthy is not addressed in the clinic; these are social and structural determinants of health such as job, food, and housing stability and security, and access to health insurance and health care. Health practitioners should promote the depoliticization around climate change by centering equity around a critical issue that affects all people: health. Medical and public health practitioners can serve as key messengers to the public by influencing practice and leading on actions that can ultimately promote climate-related health equity.
Highlights:
Climate change and related events infringe on basic human rights and civil rights.
A health equity framework that incorporates procedural, distributive, and contextual equity can be central to promoting climate justice and psychosocial resilience.
The “State of the Air” and 50th Anniversary of the Clean Air Act
The worsening of air quality via climate change represents an increasing threat to human health. Each April, the American Lung Association (ALA) publishes a State of the Air report to translate and contextualize for a wide audience the U.S. Environmental Protection Agency’s three-year air monitoring data. The 2019 report, capturing data for 2015–2017, highlighted that ozone and air pollution measures have worsened in many locations31. These trends reflect that recent years have been the warmest on record and have had increased wildfire activity. Importantly, 141 million people in the U.S. reside in areas in which air quality receives a failing grade in at least one measure; 20 million reside in areas receiving failing grades across all measures.
These findings underscore a crucial need to address both climate change and air pollution. U.S. air quality standards and regulations established in 1970 by the Clean Air Act produced significant reductions in some harmful emissions (Figure 2); while this progress is encouraging, much work remains to be done. The need is particularly poignant given the risks to vulnerable populations including children, older individuals, those with chronic lung conditions, and those who work outside and/or live in socioeconomically depressed areas. The ALA’s 2019 report identified seven key concerns: removal of limits to methane emissions from oil and gas industries; repeal of plans to reduce carbon emissions from power plants; waivers for clean air and fuel; cuts to expertise around clean air; denial of scientific evidence; weakening of Clear Air Act implementation/enforcement; and weakening of the Clean Air Act. To promote advocacy and engagement around these issues, which pose direct threats to human health, the ALA has assembled a new community: Health Professionals for Clean Air and Climate Action. By advocating for clean air, health professionals have a key opportunity to impact the lives and health of millions.
Figure 2:
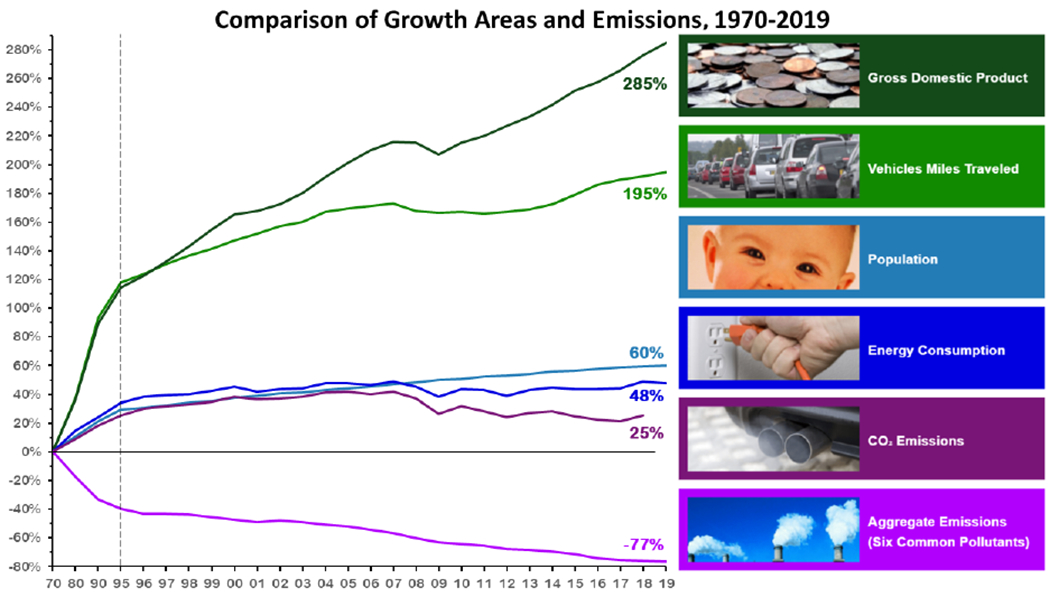
The U.S. has achieved some progress in emission reduction for six common pollutants, but work remains to be done for reducing CO2 emissions. From the U.S. Environmental Protection Agency33.
Highlights:
Poor air quality exerts health risks related to chronic lung illness, lung cancers, heart disease, and prenatal development and birth outcomes.
Many millions of Americans, including vulnerable populations, continue to be exposed to poor air quality, particularly during extreme heat events.
The Clean Air Act is under threat due to rollbacks in regulations and weak enforcement. Health professionals should engage in advocacy for clean air as a crucial factor in ensuring population health.
Bringing Awareness to Climate-related Disease and Vulnerable Populations
The conference included 18 poster presentations covering the latest evidence on a variety of topics related to climate change and health. Many discussed the link between heat and/or temperature variability and adverse health events like stroke, sepsis, allergy, asthma, and cardiac events. Others focused on identifying neighborhoods and individuals with the greatest need for intervention in climate-related events like hurricanes, and the impact of these events on population health. Several posters described the need for hospitals to lead the way in looking toward the future and mandating sustainability, as well as the need to educate and prepare future practitioners to manage the increasing burden of climate changed-related health issues.
Workshops
Two concurrent workshops gave attendees the opportunity to learn how climate change is already negatively affecting their patients’ health and to give providers practical clinical information on how to manage and protect vulnerable populations in a changing climate. The workshops began with brief didactics followed by interactive case studies and discussion. The goal of Workshop A, “Managing Respiratory and Cardiovascular Diseases,” was to help attendees make the link between climate change, air quality, and specific health outcomes such as asthma and heart disease and how to help patients use air quality information in clinical management. Workshop B, “Managing Heat Exposure in Vulnerable Populations,” aimed to provide practical guidance on the clinical detection, prevention, and management of heat and hot weather-associated illness in a changing climate and how to utilize heat wave warning systems in the clinical management of vulnerable patients. Case studies looked at occupational exposure to heat and the risk of chronic kidney disease. Together, these workshops equipped attendees with practical information for managing climate-related conditions.
Conclusions
Public health and allied health practitioners have key roles to play in recognizing and addressing the health impacts of climate change. These roles include not only clinical management of climate-related conditions from respiratory disease to mental health disorders, but also communicating to the public the needs for climate awareness and action. To adequately fulfill these roles, clinicians and public health representatives need accurate information on these growing threats as well as the changing needs of patients and populations.
Footnotes
Conflict of Interests: None
Ethical considerations: None
References
- 1.NOAA National Centers for Environmental Information. State of the Climate: Global Climate Report for Annual 2019. Type.: Institution; 2020 Date. Contract No.: Document Number. https://www.ncdc.noaa.gov/sotc/global/201913 [Google Scholar]
- 2.Campell-Lendrum D, Pruss-Ustun A. Climate change, air pollution and noncommunicable diseases. Bulletin of the World Health Organization. 2019;97:160–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chiu YH, Bellinger DC, Coull BA, et al. Associations between traffic-related black carbon exposure and attention in a prospective birth cohort of urban children. Environ Health Perspect. 2013;121(7):859–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wright RO. Environment, susceptibility windows, development, and child health. Curr Opin Pediatr. 2017;29(2):211–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wild CP. Complementing the genome with an “exposome”: the outstanding challenge of environmental exposure measurement in molecular epidemiology. Cancer Epidemiol Biomarkers Prev. 2005;14(8):1847–50. [DOI] [PubMed] [Google Scholar]
- 6.Zheng LY, Sanders AP, Saland JM, Wright RO, Arora M. Environmental exposures and pediatric kidney function and disease: A systematic review. Environ Res. 2017;158:625–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.New York City Panel on Climate Change. Advancing Tools and Methods for Flexible Adaptation Pathways and Science Policy Integration. Type. New York, NY: Institution, Office NYCMs/Division; 2019 Date. Contract No.: Document Number. https://www.nyas.org/annals/special-issue-advancing-tools-and-methods-for-flexible-adaptation-pathways-and-science-policy-integration-new-york-city-panel-on-climate-change-2019-report-vol-1439/
- 8.Hou P, Wu S. Long-term Changes in Extreme Air Pollution Meteorology and the Implications for Air Quality. Sci Rep. 2016;6:23792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Abatzoglou JT, Williams AP. Impact of anthropogenic climate change on wildfire across western US forests. Proc Natl Acad Sci U S A. 2016;113(42):11770–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dreessen J, Sullivan J, Delgado R. Observations and impacts of transported Canadian wildfire smoke on ozone and aerosol air quality in the Maryland region on June 9-12, 2015. J Air Waste Manag Assoc. 2016;66(9):842–62. [DOI] [PubMed] [Google Scholar]
- 11.Brook RD, Rajagopalan S, Pope CA 3rd, et al. Particulate matter air pollution and cardiovascular disease: An update to the scientific statement from the American Heart Association. Circulation. 2010;121(21):2331–78. [DOI] [PubMed] [Google Scholar]
- 12.Bowe B, Xie Y, Li T, Yan Y, Xian H, Al-Aly Z. Particulate Matter Air Pollution and the Risk of Incident CKD and Progression to ESRD. J Am Soc Nephrol. 2018;29(1):218–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Paranjpe I, Chaudhary K, Paranjpe M, et al. Association of APOL1 Risk Genotype and Air Pollution for Kidney Disease. Clin J Am Soc Nephrol. 2020;15(3):401–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kloog I, Melly SJ, Ridgway WL, Coull BA, Schwartz J. Using new satellite based exposure methods to study the association between pregnancy PM(2).(5) exposure, premature birth and birth weight in Massachusetts. Environ Health. 2012;11:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rosa MJ, Pajak A, Just AC, et al. Prenatal exposure to PM2.5 and birth weight: A pooled analysis from three North American longitudinal pregnancy cohort studies. Environ Int. 2017;107:173–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Di Q, Dai L, Wang Y, et al. Association of Short-term Exposure to Air Pollution With Mortality in Older Adults. JAMA. 2017;318(24):2446–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wu X, Braun D, Schwartz J, Kioumourtzoglou MA, Dominici F. Evaluating the impact of long-term exposure to fine particulate matter on mortality among the elderly. Sci Adv. 2020;6(29):eaba5692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sorek-Hamer M, Just AC, Kloog I. Satellite remote sensing in epidemiological studies. Curr Opin Pediatr. 2016;28(2):228–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Just AC, Arfer KB, Rush J, et al. Advancing methodologies for applying machine learning and evaluation spatiotemporal models of fine particulate matter (PM2.5) using satellite data over large regions. Atmospheric Environment. 2020;239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Molaei G, Little EA, Williams SC, Stafford KC. Bracing for the worst—Range expansion of the lone star tick in the northeastern United States. New England Journal of Medicine. 2019;381(23):2189–92. [DOI] [PubMed] [Google Scholar]
- 21.Shapiro ED, Wormser GP. Lyme disease in 2018: what is new (and what is not). Jama. 2018;320(7):635–6. [DOI] [PubMed] [Google Scholar]
- 22.Lanciotti R, Roehrig J, Deubel V, et al. Origin of the West Nile virus responsible for an outbreak of encephalitis in the northeastern United States. Science. 1999;286(5448):2333–7. [DOI] [PubMed] [Google Scholar]
- 23.DeFelice NB, Little E, Campbell SR, Shaman J. Ensemble forecast of human West Nile virus cases and mosquito infection rates. Nature Communications. 2017;8:14592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.DeFelice NB, Birger R, DeFelice N, et al. Modeling and surveillance of reporting delays of mosquitoes and humans infected with West Nile Virus and associations with accuracy of West Nile Virus forecasts,. JAMA network open. 2019;2(2(4):e193175):e193175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.DeFelice NB, Schneider Z, Little E, et al. Use of temperature to improve West Nile virus forecasts. Plos Computational Biology. 2018;14(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Beach RH, Sulser TB, Crimmins A, et al. Combining the effects of increased atmospheric carbon dioxide on protein, iron, and zinc availability and projected climate change on global diets: a modelling study. Lancet Planet Health. 2019;3(7):e307–e17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ziska LH, Pettis JS, Edwards J, et al. Rising atmospheric CO2 is reducing the protein concentration of a floral pollen source essential for North American bees. Proc Biol Sci. 2016;283(1828). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ziska LH, Makra L, Harry SK, et al. Temperature-related changes in airborne allergenic pollen abundance and seasonality across the northern hemisphere: a retrospective data analysis. Lancet Planet Health. 2019;3(3):e124–e31. [DOI] [PubMed] [Google Scholar]
- 29.Sherman JD, MacNeill A, Thiel C. Reducing Pollution From the Health Care Industry. JAMA. 2019. [DOI] [PubMed] [Google Scholar]
- 30.Sherman JD, Hopf HW. Balancing Infection Control and Environmental Protection as a Matter of Patient Safety: The Case of Laryngoscope Handles. Anesth Analg. 2018;127(2):576–9. [DOI] [PubMed] [Google Scholar]
- 31.American Lung Association. State of the Air, 2019. 2019. https://www.stateoftheair.org/assets/SOTA-2020.pdf [Google Scholar]
- 32.U.S. Centers for Disease Control and Prevention. Climate and Health: Climate Change Effects on Health. Type.: Institution; 2020 Date. Contract No.: Document Number. https://www.cdc.gov/climateandhealth/effects/default.htm
- 33.U.S. Environmental Protection Agency. Air Quality National Summary. Type.: Institution; 2020 Date. Contract No.: Document Number. https://www.epa.gov/air-trends/air-quality-national-summary


