Abstract
Background and Aim:
The third leading preventable cause of death in the United States is excessive alcohol consumption. Our study sought to assess the impact of the coronavirus disease 2019 (COVID-19) on hospitalizations for alcohol-related hepatitis at a community hospital system. We hypothesized an increase in cases of alcohol-related hepatitis requiring inpatient management, mirroring the strain on economic and societal norms imposed by the COVID-19 pandemic.
Approach/Results:
We performed a retrospective chart review to study the incidence of alcohol-related hepatitis in patients presenting to 3 community hospitals in Fresno, California, before and during the COVID-19. Data including patient demographics, markers of disease severity, and clinical course were extracted from electronic medical records for 329 patients included in the study. There was a 51% increase in the overall incidence of alcohol-related hepatitis requiring hospitalization between 2019 and 2020 (P=0.003) and 69% increase (P<0.001) after implementation of the stay-at-home orders. In addition, 94% (P=0.028) increase in rehospitalizations was noted in 2020 (P=0.028), a 100% increase in patients under the age of 40 (P=0.0028), as well as a trend towards a 125% increase (P=0.06) of female patients admitted with this diagnosis during the COVID-19 pandemic.
Conclusions:
Our study revealed drastic increases in severe alcohol-related hepatitis requiring inpatient management, specifically in patients under the age of 40 and in women during the COVID-19 pandemic. Given the high morbidity and mortality associated with severe alcohol-related hepatitis, these findings have far-reaching and lasting implications for our already strained health care system extending beyond the COVID-19 pandemic timeframe. Urgent public health interventions are needed to combat the rising misuse of alcohol and its consequences.
Key Words: alcohol misuse, alcoholic hepatitis, COVID-19, coronavirus, alcohol
The third leading preventable cause of death in the United States is excessive alcohol consumption.1 The link between alcohol intake and alcoholic liver disease is well documented,2 as are the risk factors for alcohol misuse disorder such as socioeconomic and environmental factors, genetics, age, and mental health conditions.3 We observed an unprecedented increase in severe cases of alcohol-related hepatitis requiring inpatient management; this paralleled the strain on the economic and societal norms imposed by the coronavirus disease 2019 (COVID-19) pandemic.
Alcohol-related hepatitis ranges in severity from mild to severe. Mild presentations resolve with supportive treatment, while severe alcohol-related hepatitis may require admission to the intensive care unit (ICU) and is associated with high mortality.4 Alcohol-related hepatitis can lead to sequelae of portal hypertension such as ascites and variceal bleeding.4 In-hospital mortality rates are high in these patients, especially those with coagulopathy, encephalopathy, acute renal failure requiring continuous renal replacement therapy, and those who suffer infectious complications.5 Given the high morbidity and mortality associated with alcohol-related hepatitis, clinicians need to be acutely aware of the increase in both hospitalizations and severity of illness associated with alcohol-related hepatitis during the COVID-19 pandemic.
The COVID-19 pandemic has led to an implementation of social distancing interventions such as stay-at-home orders in an effort to curb the spread of the virus. Based on a nationwide study using an internet-based platform (Amazon’s Mechanical Turk), a significant association between the impact of COVID-19 on daily life and subsequent psychological outcomes including greater health anxiety, financial worry, and loneliness, was noted.6 We postulate that these factors are instrumental in the rise of alcohol sales and consumption that has been seen during the COVID-19 pandemic.7 One study comparing the number of days of any alcohol use, heavy drinking, and average number of drinks consumed over the past 30 days before and during the COVID-19 pandemic revealed a 14% increase in alcohol consumption.8 Although the impact of COVID-19 on mental health, societal and economic stressors, and increased alcohol use has been documented, there is a lack of published data regarding the consequences of these effects on major health outcomes such as hospitalizations for alcohol-related liver disease. Our study explored the impact of the COVID-19 pandemic on hospitalizations for alcohol-related hepatitis in 3 hospitals in Fresno, California, the fifth largest city in California with a total population of 522,000.
METHODS
This retrospective study was approved by the Institutional Review Board and is compliant with the Health Insurance Portability and Accountability Act (HIPAA). Data was collected from the Electronic Medical Records of the Community Medical Center system that consists of 3 hospitals in Fresno, California (Community Regional Medical Center, Clovis Community Medical Center, and Fresno Heart and Surgical Hospital).
We collected data for quarterly hospitalizations of patients with a diagnosis of alcohol-related hepatitis (K70.10, K70.11) and alcoholic hepatic failure (K70.40 and K70.41) between January 1, 2019, and December 15, 2020. A total of 420 patients were identified. A total of 420 patients were identified. A diagnosis of alcohol-related hepatitis was made per the following criteria for inclusion in the study: recent alcohol abuse within the last 3 months of presentation, elevated white blood cell count>10, aspartate transaminase/alanine transaminase ratio of >2:1, and elevated total bilirubin >1.2 mg/dL. Patients below 18 years of age and pregnant patients were excluded from the study. A total of 329 patients were included in the study.
The following data were collected: quarterly number of hospitalizations of patients with the diagnosis of alcohol-related hepatitis and alcoholic hepatic failure from January 1, 2019, to December 15, 2020, with emphasis on the timing of stay-at-home orders in California (last 3 quarters of 2020). Each quarter (defined as a 3 mo period) from 2019 was compared with the same quarter in 2020.
In addition, data on age, gender, race, hazardous drinking patterns (defined as 5 or more drinks for men and 4 or more drinks for women), comorbidities, and rehospitalization rates was collected and compared between 2019 and 2020. The laboratory values white blood cell count, alanine transaminase, aspartate transaminase, creatinine, international normalized ratio were also collected and were used to calculate Maddrey Discriminant Function (MDF) scores and Model for end-stage Liver Disease-Sodium (MELD-Na) scores.
We also compared the number of patients who required endoscopic procedures, steroids, ICU admission, and intubation, as well as the incidence of complications such as acute kidney injury and initiation of hemodialysis between 2019 and 2020 was studied.
Differences in prolonged length of hospitalization, which was defined as >15 days, rehospitalization within 3 months, number of deaths during admission, or within 3 months between 2019 and 2020, were also studied.
IBMM SPSS Statistic, Version 27 was used for analysis. To study the above-mentioned points, basic frequencies were run to calculate means and SDs. Associations and correlations were tested using χ2 and Pearson correlation testing. For continuous variables, independent-sample t tests were run to calculate P-values to assess differences.
RESULTS
Demographics
In 2019, the mean age of patients with alcohol-related hepatitis was 48.4 (±1.9), while in 2020 mean age was 47.4 (±1.7). There was a 50% increase in patients admitted with alcohol-related hepatitis under the age of 40 between 2019 and 2020 (P=0.0028). In 2019, men (n=107) accounted for 81.7% of the cases, with women (n=24) comprising only 18.3% of the cases (Fig. 1). In 2020, women (n=54) accounted for 27.3% of cases, while men (n=144) accounted for 72.7% of total cases. There was a 125% increase in the number of women admitted for alcoholic hepatitis during the pandemic (P=0.06). In 2019, Hispanics (n=71) accounted for 55% of the cases of alcohol-related hepatitis (Table 1), while non-Hispanics (n=58) accounted for 45% of the cases. In 2020, Hispanics (n=95) accounted for 48.2% cases, while non-Hispanics accounted for 51.8% of cases of alcohol-related hepatitis (Fig. 1).
FIGURE 1.
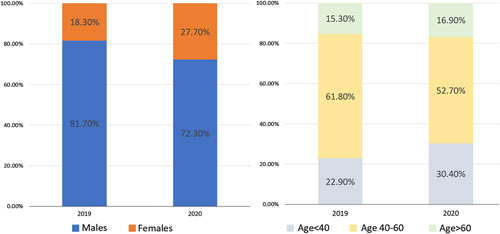
Age and gender distribution in patients presenting with alcoholic hepatitis in 2019 and 2020. As compared with 2019, there has been an increase in the proportion of females and young patients admitted with the diagnosis of alcoholic hepatitis in 2020.
TABLE 1.
Demographics of Patients Presenting With Alcohol-related Hepatitis Between 2019 and 2020
| n (%) | |||
|---|---|---|---|
| Age, Sex, Race and Hazardous Drinking | 2019 | 2020 | P |
| Mean age (y) | 48.4 | 47.4 | 0.472 |
| Age<40 | 30 (22.9) | 60 (30.5) | 0.0028 |
| 40-60 | 81 (61.8) | 104 (52.8) | 0.0849 |
| Age>60 | 20 (15.3) | 33 (16.8) | 0.0951 |
| Males | 107 (81.7) | 144 (72.7) | 0.06 |
| Females | 24 (18.3) | 54 (27.3) | 0.06 |
| Hispanics | 71 (55) | 95 (48) | 0.229 |
| Non-Hispanics | 58 (45) | 102 (51.8) | 0.229 |
| Males>14 drinks/wk | 81 (75) | 98 (68) | 0.212 |
| Females>7 drinks/wk | 15 (62.5) | 40 (74.07) | 1 |
Bold value is statistically significant.
A statistically significant increase was noted in patients under the age of 40 years.
Comorbidities
In 2019, alcohol-related hepatitis was diagnosed in 4.5% (n=6) of patients with hepatitis B, while in 2020, there was an increase to 7.5% (n=15) of patients with hepatitis B (Table 2). In 2019, 15% (n=20) of patients with underlying hepatitis C had alcohol-related hepatitis, while in 2020, 13% (n=26) patients had alcohol-related hepatitis. Overall, 44% (n=57) of patients in 2019 had a prior admission for alcohol-related hepatitis as compared with 49% (n=98) patients in 2020. In our study, 25.5% (n=84) had underlying chronic liver disease, including nonalcoholic fatty liver disease, nonalcoholic steatohepatitis, autoimmune liver disease, hepatitis C and B.
TABLE 2.
Comorbidities of Patients Admitted With Alcoholic-related Hepatitis
| Past Medical History | 2019 | 2020 | P |
|---|---|---|---|
| Hepatitis B | 6 | 15 | 0.310 |
| Hepatitis C | 20 | 26 | 0.511 |
| Prior alcohol-related hepatitis | 57 | 98 | 0.428 |
| Nonalcoholic fatty liver | 4 | 9 | 0.496 |
| Nonalcoholic steatohepatitis | 11 | 14 | 0.65 |
| Chronic liver conditions | 31 | 55 | 0.40 |
This table revealed almost double the number of patients had a prior episode of alcohol-related hepatitis.
Case Numbers
A total of 329 patients who met our inclusion criteria were admitted to the hospital between January 1, 2019, and December 15, 2020 (Fig. 2). The overall incidence of alcohol-related hepatitis increased by 51% (P=0.003) between 2019 and 2020 (Fig. 2). In the first quarter of 2019 and 2020, the number of cases were identical at 34 (Table 3). After the stay-at-home orders in March 2020, we saw an increase in the number of cases from 32 in the second quarter of 2019 to 40 in the second quarter of 2020. Comparing the third quarters of 2019 and 2020, the number of cases increased from 31 to 69 reaching statistical significance (P=0.001). Incomplete data for the fourth quarters (limited to December 15, 2020) showed an increase in cases from 34 in 2019 to 55 in 2020 (P=0.026). Comparison between combined cases after implementation of the stay-at-home orders in the second through the fourth quarters of 2019 versus 2020 revealed a 69% increase in cases (P<0.001).
FIGURE 2.
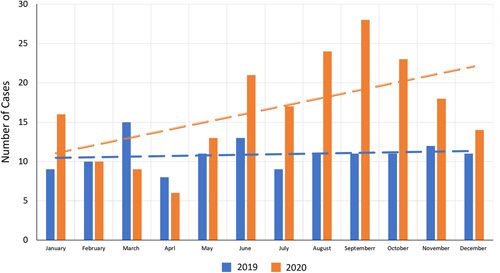
Monthly distribution of patients presenting with alcoholic hepatitis in 2019 and 2020. As compared with 2019, we see a significant increase in the number of cases admitted to the hospitals after the stay-at-home orders in March.
TABLE 3.
Number of Patients Admitted to the Hospital With Alcohol-related Hepatitis Divided into 4 Quarters in 2019 and 2020
| Quarter | No. Patients in 2019 | No. Patients in 2020 | P |
|---|---|---|---|
| Q1 | 34 | 34 | 1.000 |
| Q2 | 32 | 40 | 0.7484 |
| Q3 | 31 | 69 | 0.001 |
| Q4 | 34 | 55 | 0.026 |
| Total | 131 | 198 | 0.003 |
Bold values are statistically significant.
A statistically significant increase in a total number of cases between 2019 and 2020 was noted.
Severity and Complications
In 2019, the mean MDF score was 47.82 (±48), while in 2020 it was 41.1 (±40.54) (P=0.212) (Table 4). In 2019, the mean MELD-Na score was 20.73 (±10.76) as compared with the mean MELD-Na score of 19.62 (±9.44), in 2020. In 2019, 15% (n=20) of patients died during hospitalization, while in 2020, 13% (n=26) patients died during hospitalization (P=0.528). In 2019, 25% (n=33) patients required ICU admission/transfer with 16% (n=21) requiring intubations. In 2020, 28% (n=55) patients required ICU admission/transfer with 20% (n=40) of patients requiring intubation. In 2019, 20% (n=26) of patients received steroids for alcohol-related hepatitis, while in 2020, 17% (n=34) of patients received steroids (P=0.488). In 2019, 36% (n=47) of patients developed acute kidney injury, while in 2020, 33% (n=66) of patients had acute renal failure (P=0.518). Of the 36% of patients in 2019 with acute kidney injury, 34% (n=16) were initiated on hemodialysis, while in 2020, of the 33% with acute kidney injury, 21% were started on hemodialysis (P=0.110). In 2020, 27% (n=35) of patients underwent endoscopy, while in 2019, 21% (n=41) of patients underwent endoscopy during the hospitalization. In 2019, 29% (n=38) of patients had a length of stay >15 days, while in 2020, 23% (n=45) of patients had a similar prolonged stay. There was a 94% increase in rehospitalization rates between 2019 and 2020 (P=0.028).
TABLE 4.
Mean Laboratory Values Along With SD, Complications, and Outcomes of Patients Admitted With Alcohol-related Hepatitis Between 2019 and 2020
| Laboratory Values, Complications and Interventions | 2019 | 2020 | P |
|---|---|---|---|
| Mean Maddrey Discriminant Function Score | 47.82 (±48) | 41.1 (±40) | 0.212 |
| Mean MELD score | 20.73 (±10.76) | 19.62 (±9.441) | 0.378 |
| Mean albumin | 3.248 (±0.847) | 3.173 (±0.80) | 0.418 |
| Mean bilirubin | 8.905 (±11.4) | 7.497 (±9) | 0.249 |
| Mean INR | 1.813 (±1.1) | 1.69 (±1.02) | 0.367 |
| Mean creatinine | 3.6 (±2.5) | 1.2 (±1.3) | 0.287 |
| Endoscopy | 41 | 35 | 0.003 |
| Steroid use | 26 | 34 | 0.488 |
| ICU admission | 33 | 55 | 0.672 |
| Intubation | 21 | 40 | 0.379 |
| Acute kidney injury | 47 | 66 | 0.518 |
| Hemodialysis | 16 | 14 | 0.110 |
| Death during admission | 20 | 26 | 0.528 |
| Rehospitalised within 3 mo | 18 | 35 | 0.028 |
Bold values are statistically significant.
There was a significant decrease in the number of endoscopic procedures performed in 2020. A significant increase in rehospitalizations was also seen in 2020.
ICU indicates intensive care unit; INR, international normalized ratio; MELD, Model for End-stage Liver Disease.
DISCUSSION
While there has been published literature examining the risks associated with contracting COVID-19 in patients with liver disease,9 to our knowledge, this is one of the first few studies to demonstrates the increase in the number of hospitalizations for alcohol-related hepatitis during the COVID-19 pandemic. Alcoholic liver disease is on the rise, especially in younger populations, and studies such as ours demonstrate an unprecedented further increase in hospitalizations for a major alcohol-related consequence during the time of the COVID-19 pandemic. The observed increase in alcohol-related hepatitis has far-reaching consequences on a patient’s health and outcomes, as well as a significant impact on the capacity and cost of an already strained health care system. The burden of increased alcoholic hepatitis-related hospitalizations was especially challenging during the times of the COVID-19 surge as many hospitals were already beyond capacity.
Alcohol sales increased by 55% at the beginning of stay-at-home orders as compared with the previous years. This was attributed to increased alcohol availability, increased stress, and boredom as per a cross-sectional survey.10 Economic dislocation, job loss, fear of loneliness, and death were further triggers for alcohol use.11
The COVID-19 pandemic has impacted not only physical health but also mental and social health. This, coupled with the economic recession, has had major impacts on the overall health of our population. Our study revealed a 51% statistically significant increase in the number of hospitalizations for alcohol-related hepatitis in 2020 compared with 2019 (P=0.003) at 3 hospitals in Fresno, California. Using our data, we can extrapolate doubling the incidence of alcohol-related hepatitis cases in our national health care system. A particularly marked increase of 69% (P<0.001) was noted during a three quarter timeframe after the stay-at-home orders were issued in California. This data is consistent with a rise in alcohol use during the COVID-19 pandemic as compared with the year prior.12
The typical age of presentation for alcohol-related hepatitis ranges between 40 to 60 years of age.13 A finding of concern is a 100% increase in hospitalizations for alcohol-related hepatitis in patients under 40 years of age. Younger populations have been found to be especially vulnerable to increased consumption of alcohol in the past several years, and this was exacerbated further by stressors of the pandemic. This increase may be attributable to aspects such as college campus closures, transitions to online-only education, lack of opportunities for socializing with peers in addition to stressors related to economic insecurity.
A trend toward 125% increase in cases of women diagnosed with alcohol-related hepatitis was seen, while only a 34% increase was noted in the number of men. A study by Brooks et al14 suggests that women have experienced more psychological stress from the pandemic and are motivated more as compared with their male counterparts to drink excessively. In our study, the increase in the cases of alcohol-related hepatitis among women did not reach statistical significance (P=0.06), however, this trend is of great concern as at any level of alcohol consumption, women have a higher likelihood of developing alcoholic liver disease.15
There was not a statistically significant difference between mean MDF scores, MELD-Na scores, ICU admission, intubation, acute kidney injury, or the initiation of hemodialysis. However, we saw a 94% increase in the rehospitalization rates between 2019 and 2020, suggestive of more severe/unresolving disease. While our study clearly demonstrated an increase in hospitalizations and rehospitalizations for alcohol-related hepatitis, we did not appreciate an overall increase in the severity of alcohol-related hepatitis cases. There are several potential explanations for these findings. During the pandemic, there was an increase in alcohol consumption in baseline among both chronic drinkers and new drinkers. In addition, patients with underlying chronic liver disease may have had an acute exacerbation of the alcohol-related liver disease. Patients may have delayed seeking medical care due to the fear of contracting COVID-19 in a hospital setting, thus potentially delaying presentations requiring prolonged hospital courses or the need for rehospitalization. With many hospitals beyond capacity and a limited workforce with medical staff reallocation, access to care may have been limited in realms such as alcohol-cessation counseling and prevention of relapse or increased alcohol consumption. Services such as community alcoholics anonymous face-to-face meetings and overall community support were significantly reduced as a result of the pandemic, and this may have contributed to the rise in alcohol consumption, hospitalizations, and rehospitalizations for alcohol-related hepatitis in these vulnerable positions. It is important for clinicians to closely monitor and screen patients, especially those with underlying liver disease, for alcohol use disorder. During the current COVID-19 pandemic, it is crucial for the medical community to raise attention and awareness to the growing pandemic of alcohol use disorder and to promote alternative methods for alcohol-cessation support group meetings and community education outreach.
There was a statistically significant decrease noted in the number of patients undergoing endoscopy in 2020 as compared with 2019. This can be attributed to hospital COVID-19 infection control procedures as well as provider and staff hesitancy for doing endoscopic procedures in potentially COVID-19-positive patients.
Limitations of our study included its retrospective nature, small sample size, and limited geographical reach. Future studies in additional cities and hospital systems are needed to further assess the nationwide impact of the COVID-19 pandemic on alcohol misuse disorder and alcoholic liver disease.
CONCLUSIONS
We observed drastic increases in severe alcohol-related hepatitis requiring inpatient management, especially in patients under the age of 40 and in women, as well as an increase in readmission rates during the COVID-19 pandemic. These increases in the number and severity of cases of alcohol-related hepatitis corresponded to an increased burden of alcohol misuse in our communities that experienced unparalleled levels of social disruption. Our community is likely a reflection of the nationwide pandemic of alcohol misuse disorder spurred on by the COVID-19 pandemic. The long-term impacts of the increase in alcohol use on our national health system will be seen in years to come unless urgent public health interventions are implemented to combat the rising misuse of alcohol and its consequences.
Footnotes
The authors declare that they have nothing to disclose.
Contributor Information
Aalam Sohal, Email: aalamsohal@gmail.com.
Sameeha Khalid, Email: sameeha.khalid@ucsf.edu.
Victoria Green, Email: v.a.green149@gmail.com.
Alakh Gulati, Email: alakh.gulati@ucsf.edu.
Marina Roytman, Email: marina.roytman@ucsf.edu.
REFERENCES
- 1.Centers for Disease Control and Prevention. Alcohol-attributable deaths and years of potential life lost—United States, 2001. MMWR Morb Mortal Wkly Rep. 2004;53:866–870. [PubMed] [Google Scholar]
- 2.Zakhari S, Li TK. Determinants of alcohol use and abuse: impact of quantity and frequency patterns on liver disease. Hepatology. 2007;46:2032–2039. [DOI] [PubMed] [Google Scholar]
- 3.Gilbertson R, Prather R, Nixon SJ. The role of selected factors in the development and consequences of alcohol dependence. Alcohol Res Health. 2009;31:389–399. [PMC free article] [PubMed] [Google Scholar]
- 4.Sersté T, Cornillie A, Njimi H, et al. The prognostic value of acute-on-chronic liver failure during the course of severe alcoholic hepatitis. J Hepatol. 2018;69:318–324. [DOI] [PubMed] [Google Scholar]
- 5.Liangpunsakul S. Clinical characteristics and mortality of hospitalized alcoholic hepatitis patients in the United States. J Clin Gastroenterol. 2011;45:714–719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tull MT, Edmonds KA, Scamaldo KM, et al. Psychological outcomes associated with stay-at-home orders and the perceived impact of COVID-19 on daily life. Psychiatry Res. 2020;289:113098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.The Nielsen Company. Rebalancing the ‘COVID-19 Effect’ on alcohol sales; 2020. Available at: www.nielsen.com/us/en/insights/article/2020/rebalancing-the-covid-19-effect-on-alcohol-sales/. Accessed August 27, 2020.
- 8.Pollard MS, Tucker JS, Green HD. Changes in adult alcohol use and consequences during the COVID-19 pandemic in the US. JAMA Netw Open. 2020;3:e2022942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang Q, Davis PB, Xu R. COVID-19 risk, disparities and outcomes in patients with chronic liver disease in the United States. EClinicalMedicine. 2021;31:100688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grossman ER, Benjamin-Neelon SE, Sonnenschein S. Alcohol consumption during the COVID-19 pandemic: a cross-sectional survey of US adults. Int J Environ Res Public Health. 2020;17:9189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Polakovic G. COVID-19 drives alcohol sales, raises concerns about substance abuse. USC News; April 15, 2020. Available at: http://news.usc.edu/168549/covid-19-alcohol-sales-abuse-stress-relapse-usc-experts. Accessed March 1, 2021.
- 12.Lee BP, Dodge JL, Leventhal A, et al. Retail alcohol and tobacco sales during COVID-19. Ann Intern Med Ther. 2021;174:1027–1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cohen SM, Ahn J. Review article: the diagnosis and management of alcohol-related hepatitis. Aliment Pharmacol Ther. 2009;30:3–13. [DOI] [PubMed] [Google Scholar]
- 14.Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Becker U, Deis A, Sorensen TI, et al. Prediction of risk of liver disease by alcohol intake, sex, and age: a prospective population study. Hepatology. 1996;23:1025–1029. [DOI] [PubMed] [Google Scholar]


