Abstract
Background
School policies and programs are important in preventing Cannabis use among youth. This study uses an innovative digital citizen science approach to determine the association between Cannabis use and suicidal ideation among youth while investigating how school health policies mediate this association.
Methods
The study engaged 818 youth (aged 13–18 years) and 27 educators as citizen scientists via their own smartphones. Youths responded to time-triggered validated surveys and ecological momentary assessments to report on a complex set of health behaviours and outcomes. Similarly, educators’ reported on substance misuse and mental health school policies and programs. Multivariable logistic regression modeling and mediation analyses were employed.
Results
412 youth provided data on substance misuse and suicidal ideation. Cannabis use and other factors such as bullying, other illicit drug use, and youth who identified as females or other gender were associated with increased suicidal ideation. However, school policies and programs for substance misuse prevention did not mediate the association between Cannabis use and suicidal ideation.
Conclusions
In the digital age, it is critical to reimagine the role of schools in health policy interventions. Digital citizen science not only provides an opportunity to democratize school policymaking and implementation processes, but also provides a voice to vulnerable youth.
Background
Globally, suicide is one of the most common causes of death among young people aged 10–24 years (6% of deaths) [1]. Suicidal behaviours (suicidal thoughts/ideation, suicidal attempts), which have increased among youth (13–18 years) and young adults (18–24 years), are associated with the earlier initiation of cannabis use [2]. This has led researchers to investigate if cannabis use is a risk factor that can trigger suicidal behaviours [3]. Evidence indicates that youth are especially vulnerable to mental health disorders and suicidal ideation associated with cannabis use [4]. Moreover, youth Cannabis use has been linked to an increased risk of depression and suicidal behaviour in young adulthood [5].
Numerous countries have legalized the use of cannabis for nonmedical purposes, including Canada, Georgia, South Africa, Uruguay, and some states in the United States [6]. Recent evidence in the United States showed that 16.4% of youth aged 12–17 years reported cannabis use [7]. Canada is one of the latest jurisdictions to legalize nonmedical use of cannabis, with the government of Canada legalizing the use, possession, purchase, and growth of recreational cannabis on October 17, 2018. According to the National Cannabis Survey (NCS), about 18% (5.3 million) of Canadians aged 15 or older reported using cannabis in the past three months after legalization, which indicated an overall increase in consumption (14% in 2018 Quarter 1 to 17.5% in 2019 Quarter 1) [4].
It is important to understand the mental health impacts of cannabis use among youth and young adults because evidence indicates that physiological development of the brain is not complete until entering adulthood [8–10]. One Canadian study [11] in 1043 young university students (mean age = 20 years) used questionnaires to assess perceptions of risk associated with cannabis use and its associations with anxiety symptoms. The authors observed that males were more likely to perceive minimal risk with the use of cannabis, while cannabis use was more strongly associated with anxiety among females [11].
Consistent evidence also indicates that Cannabis use is a risk factor for developing psychosis and schizophrenia among youth. A systematic review published in the year 2020, which investigated the most recent literature (2009–2019), evaluated studies on the age of initiation of Cannabis use, among other factors [12]. The systematic review showed that early initiation of Cannabis use is associated with an increased risk of psychosis by reiterating that other substance misuse should be factored in when understanding the relationship between Cannabis use and psychosis. Apart from lower age of onset of Cannabis use [13–15], potent varieties of Cannabis use [16, 17], and Cannabis use at higher frequency during adolescence [18] were associated with psychosis. Prospective investigations, such as a 15-year Swedish study among a large cohort of individuals (n = >50,000) [19], also indicate that early use of Cannabis increases the risk of schizophrenia.
The clear evidence of the association of Cannabis use and severe mental illness reiterates the importance of early interventions. Among various interventions and initiatives to address mental health and substance misuse among youth, school policies and programs offer an upstream approach to positively influence youth health behaviours and outcomes [20–23]. However, there is a dearth of evidence that takes into account school policies in understanding the relationship between cannabis use and youth mental health. In particular existing methods do not provide youth or educators a voice to inform and influence school policies [24].
This study uses data from a digital epidemiological and citizen science platform [25] that engaged youth and educators using their own smartphones immediately after the legalization of cannabis in Canada. The study determines not only the association between cannabis use and suicidal ideation among youth, but also the mediation of this association by school mental health and substance misuse policies to explore the potential of digital citizen science to democratize policy and enable youth equity.
Materials and methods
Design
As part of a digital epidemiological and citizen science platform (Smart Platform), [25] a quasi-experimental study called Smart Youth was conducted immediately after the legalization of cannabis in Canada [26] 818 youth (aged 13–18 years) and 27 educators in 5 out of 12 high schools in the provincial capital city of Regina, Saskatchewan, Canada, were engaged as citizen scientists via their own Smartphones. Regina is the second-largest city in the province of Saskatchewan, with a population of 215,106 according to the 2016 Statistics Canada Census [27]. All youth and educators used a custom-built digital epidemiological Smartphone application (app), specifically adapted for the study, which operates on both Android and iOS platforms. Ethics approval was obtained from the Research Ethics Boards of Universities of Regina and Saskatchewan through a synchronized review protocol (REB # 2017–29).
Smart Youth study was embedded in all participating schools’ curricula in collaboration with key stakeholders: Saskatchewan Ministries of Health, Education, and Sport. Smart Youth is informed by a Youth Citizen Scientist Council, which consists of youth from Saskatchewan. The Council engages with the research team to inform the study implementation and knowledge translation efforts.
Recruitment
Twelve high schools in the city of Regina were approached to participate in the study, out of which 5 schools agreed to participate. One week before recruitment, schools shared implied informed consent forms with parents via email. Inclusion criteria deemed that only those youth whose parents did not object to their participation, and youth who confirmed that they did not have any medical condition that prevented them from being physically active will be recruited. Parents were given the option to reach out to the research team to opt their children out of the study.
The Smart Platform research team scheduled school visits in close coordination with schools. During each school visit, the research team conducted separate recruitment presentations to students in each grade (grades 8–12) within a school. Before these presentations were delivered, youth and educators viewed the Smart Platform’s crowdsourcing video [28] that enables the engagement of citizen scientists across the world. After class presentations, youth and educators who decided to participate in the study downloaded the custom-built app onto their own Smartphones. Both youth and educators provided informed consent via the app. The overall participation rate of youth was over 80% across all schools, thus resulting in a representative sample.
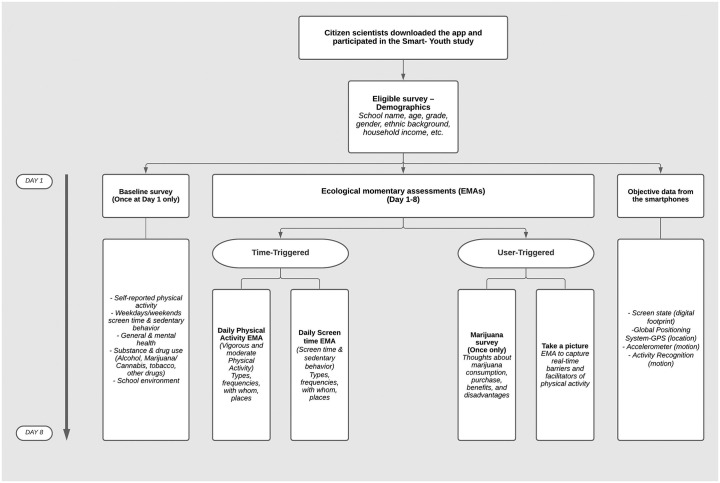
As soon as youth and educators joined the study via the app, eligibility, and baseline surveys were triggered (Smart Youth and Educator Surveys), which were completed in the presence of our team on day 1 of the study. The Smart Youth Survey (Fig 1) utilized a combination of validated questionnaires to capture a complex set of health behaviours and outcomes, including physical activity, sedentary behaviour, sleep, mental health (including anxiety and depression symptoms), and addictions.
Fig 1. Smart youth survey deployment.
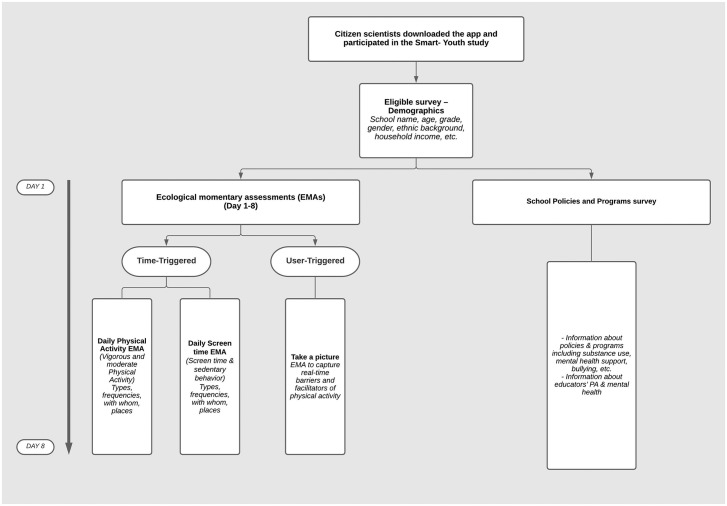
The Smart Educator Survey (Fig 2) was comprised of educators’ input regarding school policies and programs, and perceptions of how youth health outcomes could be improved. Thereafter, for the next 7 days, youth and educator citizen scientists engaged with the Smart Platform team via time-triggered ecological momentary assessments to report their perceptions on health behaviours and outcomes in real-time [29, 30].
Fig 2. Smart educator survey deployment.
Measures
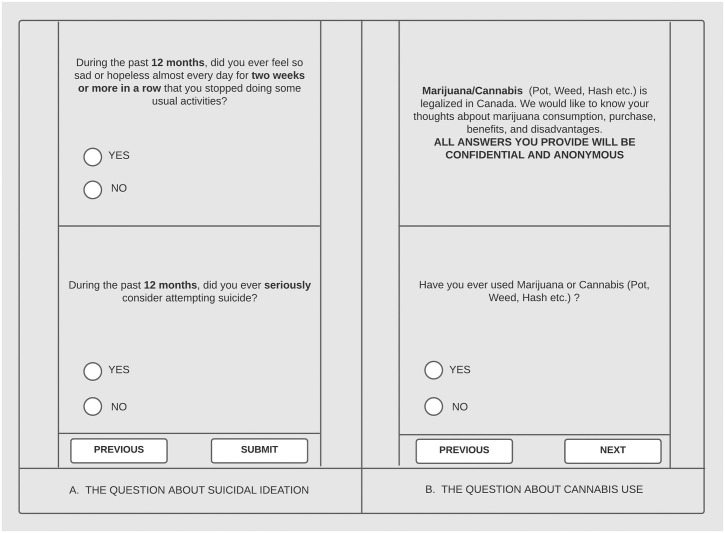
The primary outcome of interest is suicidal ideation measured using the following question: “During the last 12 months, did you ever seriously consider attempting suicide? (Yes/No)” This question has been used previously in the Global School-based Student Health Survey, which was developed by the World Health Organization in collaboration with the Centers for Disease Control [31]. The primary independent variable is cannabis use measured by the question: “Have you ever used Marijuana or Cannabis (Pot, Weed, Hash, etc.)” (Yes/No). This question has been used in multiple surveys in Canada [32]. Screenshot replicas of these two questions as they appeared on the app were shown in Fig 3A & 3B.
Fig 3. Screenshot replicas of suicidal ideation and cannabis questions.
Covariates included to reduce potential confounding are as follows: Gender (male, female, and others, including Transgender individuals); Grades (Grade 9, 10, 11, 12); Tobacco use (Have you ever used any tobacco related products?—Yes/No); Alcohol use (Have you ever consumed alcohol in your life?—Yes/No); Other illicit drug use (Have you ever used any of the following drugs: Cocaine, Methamphetamines, Ectasy, hallucinogenic, synthetic marijuana, steroid, prescription pain medicine without a doctor’s prescription or differently than how a doctor told you to use it—Yes/No); bullying at schools (-Yes/No) (Any affirmative responses to any questions related to bullying at schools such as being shoved/hit/ made fun of or teased by other students in a hurtful way, etc.); household income (less than $70000, $70,000-80000k, more than $80,000; ethnicity (Canadian, First Nations, and Other [Asian, South Asian etc.])); parental education (Less or equal to secondary/high school vs. post-secondary education (university or college)); age first used marijuana or Cannabis; frequency of using Cannabis (a joint, pot, weed, hash) in the last 30 days (Once, 2–3 times, once a week, 2–3 times a week, 4–6 times a week, every day, and did not use); youth perceptions of access to Cannabis (difficult, easy, do not know); youth perceptions of the legalization of nonmedical use of Cannabis (agree, disagree, do not know).
Educator citizen scientists provided their perception of mental health and substance misuse school policy and program availability. Information regarding the availability of school policies and programs at each school was based on a consensus of educator responses within each school. Educators responded to two specific questions: “Are there any mental health supports for youth in your school?” (Yes/No); and “Does your school provide any marijuana, or drug use (cocaine, heroin, etc.) prevention programs?” (Yes/No).
Data and risk management
To ensure confidentiality, data were encrypted before being stored on the smartphones and streamed to servers when devices established Wi-Fi connection. Any identifiable artefacts (e.g., photos) were removed or deidentified before data analysis. Permissions built into the app are restricted so that the app cannot access personally identifiable information that is present on the smartphones (e.g., contact list or network sites visited). MAC address anonymization was used to protect citizen scientists’ data based on a simple hash algorithm. Risks and privacy management options were made clear to citizen scientists while obtaining informed consent. All citizen scientists had the option to drop out of the study or pause data gathering anytime they wished via the app. Moreover, they also had the option in the settings of the app to upload data only when they had WI-FI access and/or when they were charging their phones [30]. Clear instructions were provided regarding study withdrawal within the app.
Data analysis
Statistical analysis was conducted using IBM SPSS Statistics version 26 (IBM Corporation, Armonk, New York). Chi-square tests were applied to test the univariate association between suicidal ideation, Cannabis use and covariates. Potential risk factors, confounders, and interactive effects were determined. Variables with p-value < 0.20 and/or known risk/protective factors and/or with clinical significance in the univariate analysis were selected for the final multivariable logistic regression model. The variables retained in the final multivariable model included those that were statistically significant (i.e., p < 0.05) as well as clinically important variables. Mediation analyses were conducted to assess whether school policies and program availability mediate the association between Cannabis use and suicidal ideation. The potential mediation effect of each variable was assessed by: ([ORfull model without mediator − ORfull model]/ ORfull model)*100. For mediation to occur, a statistically significant association between the primary exposure and the outcome must be smaller and no longer statistically significant when the mediator is included. A 5% change in the association is a meaningful difference. The Hosmer Lemeshow statistic was used to assess the goodness of fit of the final multivariable logistic regression model. The Hosmer Lemeshow statistic was greater than 0.05 in our final model, which is considered a good fit. The strength of associations was presented by odds ratios (OR) and their 95% confidence intervals (CI).
Results
818 youth (aged 13–18 years) and 27 educators from 5 schools participated as citizen scientists in this study. 412 youth provided valid data on both the primary outcome (suicidal ideation), and the primary independent variable (cannabis use) (Table 1). The mean age of the youth citizen scientists was 15.9 years (SE = 0.07), out of which, 36.9% (n = 152) were male; and 53.9% (n = 222) were female, and 5.56% (n = 22) selected “other” as an option for gender. 25.5% (n = 105) of participants reported using cannabis at least once in their lifetime. 23.06% (n = 95) of participants reported that they seriously considered attempting suicide during the last 12 months. Youth also reported other substance use, including alcohol (61.27%), tobacco (21.65%), and other illicit drugs, such as Cocaine, Methamphetamines, Ecstasy, hallucinogenics (7.32%).
Table 1. Characteristics of study population (n = 412).
| N* | % | ||
|---|---|---|---|
| Age, mean (SE) | 15.9 (0.08) | ||
| Gender | Male | 152 | 38.38 |
| Female | 222 | 56.06 | |
| Other | 22 | 5.56 | |
| Ethnicity | First Nations | 20 | 5.06 |
| Canadian | 159 | 40.25 | |
| Other | 216 | 54.68 | |
| Cannabis use | Yes | 105 | 25.49 |
| No | 307 | 74.51 | |
| Suicide ideation | Yes | 95 | 23.06 |
| No | 317 | 76.94 | |
| Alcohol use | Yes | 250 | 61.27 |
| No | 158 | 38.73 | |
| Tobacco use | Yes | 89 | 21.65 |
| No | 322 | 78.35 | |
| Other drugs use | Yes | 30 | 7.32 |
| No | 380 | 92.68 | |
| Grade | 9 | 114 | 28.57 |
| 10 | 83 | 20.8 | |
| 11 | 58 | 14.54 | |
| 12 | 144 | 36.09 | |
| Parental education | Less or equal than secondary/high school | 101 | 27.45 |
| Some post-secondary (university or college) or more | 267 | 72.55 | |
| Age first used marijuana or Cannabis? (mean, SE) | 100 | 14.01 (0.18) | |
| Frequency of using marijuana or Cannabis (a joint, pot, weed, hash) in the last 30 days | Once | 19 | 18.63 |
| 2–3 times | 8 | 7.84 | |
| Once a week | 4 | 3.92 | |
| 2–3 times a week | 6 | 5.88 | |
| 4–6 times a week | 6 | 5.88 | |
| Every day | 16 | 15.69 | |
| I did not use marijuana in the last 30 days | 43 | 42.16 | |
| Perceptions of getting access to marijuana | Difficult | 41 | 10.46 |
| Easy | 214 | 54.59 | |
| I do not know | 137 | 34.95 | |
| Perceptions of the legalization of recreational marijuana | Agree | 145 | 37.18 |
| Disagree | 123 | 31.54 | |
| I do not know | 122 | 31.28 | |
Table 2 shows the characteristics of youth stratified by suicidal ideation reporting (Yes/No). Females were significantly more likely to report suicidal ideation compared to males (26.6% vs.12.5%; p = 0.008). 45.5% of respondents who selected “Other” gender category reported suicidal ideation which is significantly higher than that of males (12.5%) and females (26.6%). Youth who reported cannabis use were more likely to have suicidal thoughts compared to those who did not (40.0% vs. 17.3%, respectively; p<0.001). Similar trends of suicidal ideation were observed in those who reported other substance use: alcohol (27.6% vs. 15.8%; p = 0.006); tobacco (41.6% vs. 18.0%; p<0.001); other illicit drugs (53.3% vs. 20.8%; p<0.001). Youth who experienced bullying were significantly more likely to report suicidal ideation compared to those who did not experience bullying (34.4% vs. 13.2%; p<0.001). Youth who agreed with the policy of cannabis legalization in Canada reported a higher proportion of suicidal ideation compared to those who did not agree or had a neutral opinion (33.1% vs. 19.5% vs. 16.4%, respectively; p <0.001).
Table 2. Suicidal ideation difference (yes/no) across different characteristics (n = 412)*.
| Self- report of Suicidal ideation | |||||
|---|---|---|---|---|---|
| Yes (n = 95) | No (n = 317) | ||||
| N | % | N | % | ||
| Gender | Male | 29 | 12.5** | 133 | 87.5 |
| Female | 59 | 26.6 | 163 | 73.4 | |
| Others | 10 | 45.5 | 12 | 54.5 | |
| Grade | 9 | 29 | 25.4¥ | 85 | 74.6 |
| 10 | 27 | 32.5 | 56 | 67.5 | |
| 11 | 5 | 8.6 | 53 | 91.4 | |
| 12 | 30 | 20.8 | 114 | 79.2 | |
| Cannabis use | Yes | 42 | 40.0** | 63 | 60.0 |
| No | 53 | 17.3 | 254 | 82.7 | |
| Alcohol use | Yes | 69 | 27.6¥ | 181 | 72.4 |
| No | 25 | 15.8 | 133 | 84.2 | |
| Other drugs use | Yes | 16 | 53.3** | 14 | 46.7 |
| No | 79 | 20.8 | 301 | 79.2 | |
| Tobacco use | Yes | 37 | 41.6** | 52 | 58.4 |
| No | 58 | 18.0 | 264 | 82.0 | |
| Ever bullied | Yes | 66 | 34.4** | 126 | 65.6 |
| No | 29 | 13.2 | 191 | 86.8 | |
| Household income | Less than 70k | 16 | 31.4 | 35 | 68.6 |
| 70- <80k | 3 | 11.5 | 23 | 88.5 | |
| >=80k | 15 | 23.8 | 48 | 76.2 | |
| Ethnicity | First Nations | 5 | 25.0 | 15 | 75.0 |
| Canadian | 33 | 20.8 | 126 | 79.2 | |
| Others | 50 | 23.1 | 166 | 76.9 | |
| Parental education | Less or equal than secondary/high school | 27 | 26.7 | 74 | 73.3 |
| Some post-secondary (university or college) or more | 52 | 19.5 | 215 | 80.5 | |
| Perceptions of the legalization of recreational marijuana | Agree | 48 | 33.1** | 97 | 66.9 |
| Disagree | 24 | 19.5 | 99 | 80.5 | |
| I do not know | 20 | 16.4 | 102 | 83.6 | |
| Perceptions of getting access to marijuana | Difficult | 7 | 17.1 | 34 | 82.9 |
| Easy | 58 | 27.1 | 156 | 72.9 | |
| I do not know | 27 | 19.7 | 110 | 80.3 | |
** p <0.001 based on chi-square tests comparing proportions of suicidal ideation difference (Yes/No) across different characteristics.
¥ p <0.05 based on chi-square tests comparing proportions of suicidal ideation difference (Yes/No) across different characteristics.
Among 27 educators from 5 schools who participated as citizen scientists, even though 92.6% (25/27) reported existing mental health supports for youth in their schools, a majority also reported issues with student mental health 77.8% (21/27), as well as substance use behaviours such as alcohol 70.4% (19/27), tobacco 77.8% (21/27), and other illicit drug use 70.4% (19/27).
Educator citizen scientists also reported that prevention programs were rare, with 18.5% (5/27), 33.3% (9/27), and 11.1% (3/27) reporting knowledge of alcohol, cannabis, and tobacco, prevention programs, respectively. 48.1% (13/27) of educators reported bullying to be an issue in their schools, with the main cause of concern being online bullying 37% (10/27) followed by verbal 25.9% (7/27) and physical bullying 22.2% (6/27). Nevertheless, 77.8% (21/27) of educators also reported that their schools had policies to both prevent bullying and provide support to bullying victims.
In the multivariable analyses (Table 3), youth cannabis use was associated with an increased risk of suicidal ideation (adjusted OR (aOR) = 3.09 [95%CI = 1.21–7.89]). Other illicit drug use (aOR = 5.41 [95%CI = 1.63–17.94]) and being bullied (aOR = 3.34 [95%CI = 1.63–6.43]) were also associated with an increased risk of suicidal ideation. In terms of gender, youth who identified themselves as females (aOR = 3.73 [95%CI = 1.84–7.55]) or other gender (aOR = 5.38 [95%CI = 1.40–20.73]) were associated with an increased risk of suicidal ideation in comparison with males.
Table 3. Univariate and multivariate logistic regression examining the associations between cannabis and suicidal ideation in youth (n = 412).
| Unadjusted OR (95% CI) | Adjusted OR (95% CI) | |
|---|---|---|
| Cannabis use (ref.: No) | 3.19 (1.95–5.21) | 3.09 (1.21–7.89) |
| Sex (ref.: Male) | ||
| Female | 2.53 (1.43–4.46) | 3.73 (1.84–7.55) |
| Others | 5.83 (2.21–15.34) | 5.38 (1.40–20.73) |
| Grade (ref: Grade 9) | ||
| Grade 10 | 1.41 (0.75–2.63) | 1.40 (0.64–3.09) |
| Grade 11 | 0.27 (0.10–0.75) | 0.11 (0.02–0.50) |
| Grade 12 | 0.77 (0.43–1.38) | 0.54 (0.24–1.20) |
| Alcohol use (ref.: No) | 2.02 (1.21–3.37) | - |
| Tobacco use (ref.: No) | 3.23 (1.94–5.38) | 1.60 (0.62–4.11) |
| Other drugs use (ref.: No) | 4.35 (2.03–9.30) | 5.41 (1.63–17.94) |
| Being bullied (ref.: No) | 3.44 (2.11–5.63) | 3.34 (1.63–6.43) |
| Paternal education (ref.: Some post-secondary (university or college) or more) | ||
| Less or equal than secondary/high school | 0.66 (0.38–1.13) | 1.31 (0.67–2.57) |
| Ethnicity (ref.: First Nations) | - | |
| Canadian | 0.78 (0.26–2.31) | |
| Others | 0.90 (0.31–2.60) | |
| Cannabis policy (ref.: No) | 0.76 (0.48–1.22) | 1.34 (0.71–2.52) |
In the mediation analyses, educator reporting of school policies and programs for mental health supports and substance misuse prevention did not statistically mediate the association between cannabis use and suicidal ideation among youth.
Discussion
Using data from a digital epidemiological and citizen science platform that engaged youth and educators as citizen scientists via their own smartphones, this study aimed to determine the association between cannabis use and suicidal ideation among youth, and the mediation of this association by school public health prevention policies and programs. We found that cannabis use was associated with an increased risk of suicidal ideation among youth, with those who identified as females and other gender showing a greater association with suicidal ideation. Other factors such as other illicit drug use (Cocaine, Methamphetamines, Ecstasy, hallucinogenics) and being bullied were also associated with increased risk of suicidal ideation. School mental health supports, and cannabis use prevention policies and programs, as reported by educator citizen scientists did not mediate the association between cannabis use and suicidal ideation among youth.
The positive association between cannabis use and suicidal thoughts has been supported by previous research [5, 8, 33]. For example, a recent systematic review and meta-analysis conducted in 2019 concluded that cannabis use during adolescence is associated with subsequent suicidal ideation within adolescence and in young adulthood with the pooled OR of 1.50 (95% CI, 1.11–2.03). The National Longitudinal Survey of Children and Youth in Canada showed that among 6,788 youth aged 14–15 that substance use increased the risk of suicidal behaviors [32]. A 30-year longitudinal study of a birth cohort of 1265 children in New Zealand showed that frequent cannabis use (at least several times a week) predicts later suicidal ideation in susceptible males [34].
We also found that the use of the other illicit drugs such as Cocaine, Methamphetamines, Ecstasy, and hallucinogenics, was associated with increased the risk of suicidal ideation, a finding that is consistent with current evidence [35–37]. This suggests that cannabis use should be targeted as part of a multicomponent substance misuse prevention plan to support youth during a vulnerable phase in their life course.
Another risk factor of youth suicidal ideation in our study was bullying, which is supported by existing evidence [38–40]. Both cross-sectional and longitudinal findings indicate that there is an increased risk of suicidal ideation among youth who are bullied [37]. This is indicative of the need for school bullying policies and programs that also take into consideration the association between substance misuse and suicidal ideation [40, 41].
Gender played a significant role in youth’s association with suicidal ideation, a finding that is consistent with previous studies [40, 42]. Youth who identified themselves as females were at higher risk of having suicidal ideation than males. Perhaps more significantly, almost half the youth who identified as belonging to a gender other than male or female reported suicidal ideation. This finding was substantiated in adjusted multivariable analyses, where the risk of association with suicidal ideation among other gender category was significantly higher in comparison with male youth.
These findings corroborate emerging evidence of suicidal ideation among youth who identify as transgender [43, 44]. Gender differences in suicidal thoughts should be taken into consideration when designing school prevention and/or support policies to reduce the risk of suicidal ideation among youth. Our findings also indicate the need for consistent use of sex and gender-based data collection processes and analyses to inform population health policies [45].
School policies and programs are known to have a direct impact on youth health [46–48]. Given the long-term consequences of cannabis use in adolescence, [49] we set out to understand the influence of school policies and programs from an educator perspective. Current evidence indicates that school-based programs can be effective in preventing and reducing the use of cannabis among youth [50–52] Such programs also increase youth awareness of the consequences of cannabis use and benefits related to non-use. Although educators citizen scientists reported school policies related to mental health and substance misuse, we weren’t able to establish that these policies mediated the relationship between cannabis use and suicidal ideation among youth.
Apart from the possibility that current school policies are not adequate to address cannabis use among youth, our innovative citizen science approach points towards several implications. There is a difference between policy presence and policy implementation. Our approach differed from existing methods of obtaining policy information from a single source to understand implementation [46–48]. We engaged a randomly selected cohort of educators from across all schools to obtain their perception of school policies, which provides us an estimate of the dispersion of school policies.
This digital citizen science approach is not only a democratic way of understanding school policy from the perception of educators (i.e., better data), but also provides a pathway for democratizing policymaking—educators and youth citizen scientists influencing school policies [24]. With respect to cannabis use, it is important to not only understand the success of school policies, but also to obtain a perception of youth about cannabis access and legalization—data which are critical for the success of policy development and implementation. Citizen science provides a voice to youth, which in itself could address mental health [24].
As understanding implementation and uptake of school policies is an essential component of policy effectiveness and efficacy, digital citizen science can also facilitate the evaluation of school policies. Perhaps more importantly, digital citizen science opens up the possibility of machine learning-informed behavioural interventions that can identify risk in real-time and provide virtual care services [53, 54]. However, to ethically engage citizens it is important to provide anonymity, privacy and data sovereignty [24].
Apart from adding to the current evidence that Cannabis use among youth is associated with increased risk of suicidal ideation [5], this study reiterates that the relationship between substance misuse and mental health is complex, where use of multiple drugs and negative experiences such as bullying play a key role [55]. This indicates the need for holistic school policy development, where silos are avoided in addressing substance misuse, mental health, and bullying. However, holistic school policies should not equate to one-size-fits-all approach, as this study showed that youth who identified as females or other gender were at a much higher risk of suicidal ideation. In practical terms of providing support at the school-level, it is important to develop targeted interventions that prioritize at-risk youth.
Nevertheless, we live in a digital world, where youth are especially susceptible to negative consequences of technology and social media [56] There is only so much we can do in physical school places when youth are literally in virtual spaces for significant portions of the day. The most significant implication of this study is the digital citizen science approach, which allows real-time engagement with youth and educators to ensure consistent engagement and prospective measurement of health behaviours and outcomes. The critical element is in providing a voice to both youth and educators, which in itself can be a positive force in mitigating the risk of substance misuse and mental illness.
The digital citizen science approach also provides a pathway for obtaining longitudinal as well as qualitative data that will not only enable effective implementation of school policies, but also facilitate the evaluation of the implementation and efficacy of school policies. The engagement of youth and educators using digital citizen science approaches goes beyond participatory action as advanced machine learning and artificial intelligence algorithms can be used to address the risk of suicidal ideation in real-time [57]. With mental health being a significant challenge among youth globally [58], the risks of not innovating are far greater and schools need to leverage the technology at hand to use it for promoting school health.
This is the first cannabis use study to engage with both youth and educators as citizen scientists to obtain both individual-level and school-level data in real-time. Our digital citizen science approach provides a pathway for obtaining longitudinal as well as qualitative data that will not only enable effective implementation of school policies, but also facilitate the evaluation of the implementation and efficacy of school policies [24]. More importantly, with the risk of suicide being the highest among youth [59, 60], it is important to look beyond existing measures that are not working and explore digital citizen science approaches using big data and machine learning to address mental health in real-time [61, 62].
Strengths and limitations
Citizen scientist perspectives obtained through smartphone reporting are prone to recall and social desirability bias. Youth may have under- or over-reported cannabis use due to peer pressure. However, we believe the self-reported use of cannabis is relatively accurate (79.9% sensitivity and 80.0% specificity), and the smartphone engagement provides anonymity that reduces misreporting [46]. Nevertheless, objective measurement of behaviours by ethically engaging citizens using their own mobile devices would provide an opportunity to validate these findings [30, 63].
The exposures and outcomes that we examined were cross-sectional, raising issues of temporality and reverse causality. However, the direction of causality between mental health problems and cannabis use remains unclear, and our findings were supported by literature [64]. Our study does not take into account youth who may have dropped out of school, and these data should be collected in future studies. Although we engaged youth to obtain comprehensive information, residual confounders may not have been accounted for in our analysis (e.g., information about peer pressure)–another area of focus for future data collection. The lack of qualitative data about the process of school policy is a limitation that reduces our ability to understand the impact of school policies. Another key aspect that is usually not measured is the variation of behaviours across seasons in children and youth, an important factor that needs to accounted in future studies [65, 66].
Finally, Internet inequity could be an issue in obtaining a representative sample from participants, and potentially widen the gap of existing inequities [24]. Nevertheless, the primary strength of our study is that it provides insight into both big data collection and policy interventions using digital citizen science. With over 3 billion smartphones in global usage currently [67], the ability to engage as citizen scientists change the landscape of population health research [68] In fact, all youth and educators who agreed to participate in our study owned smartphones with data plans. As part of the digital citizen science-based Smart Platform [28], to address potential Internet inequity, we work with schools to ensure that all youth and educators who participate as citizen scientists receive access to mobile phones and data plans [24].
Conclusions
Irrespective of the variation of cannabis legalization across global jurisdictions, cannabis access and use among youth is an important public health issue. With the risk of suicide being very high among youth, and with cannabis use being associated with the risk of suicidal ideation, it is critical to reimagine the role of schools in health policy interventions. Digital citizen science not only provides an opportunity to democratize school policymaking and implementation processes, but also provides a voice to vulnerable youth, which in itself could improve mental health and facilitate equity in the 21st century.
Data Availability
Data cannot be shared publicly because citizen scientists have co-ownership. Data are available from the University of Regina’s Institutional Data Access / Ethics Committee (research.ethics@uregina.ca) for researchers who meet the criteria for access to confidential data.
Funding Statement
This study is funded by the Saskatchewan Health Research Foundation’s Establishment Grant #3779, and the Saskatchewan Health Research Foundation-Saskatchewan Centre for Patient-Oriented Research’s Patient Oriented Research Leader Award, which were awarded to TRK. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Patton GC, Coffey C, Sawyer SM, Viner RM, Haller DM, Bose K, et al. Global patterns of mortality in young people: a systematic analysis of population health data. Lancet. 2009;374: 881–892. doi: 10.1016/S0140-6736(09)60741-8 [DOI] [PubMed] [Google Scholar]
- 2.Serafini G, Pompili M, Innamorati M, Temple EC, Amore M, Borgwardt S, et al. The Association between Cannabis Use, Mental Illness, and Suicidal Behavior: What is the Role of Hopelessness? Front Psychiatry. 2013;4. doi: 10.3389/fpsyt.2013.00125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Maharajh HD, Konings M. Cannabis and Suicidal Behaviour Among Adolescents: A Pilot Study from Trinidad. Sci World J. 2005;5: 576–585. doi: 10.1100/tsw.2005.79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rotermann M. Analysis of trends in the prevalence of cannabis use and related metrics in Canada. Heal reports. 2019;30: 3–13. doi: 10.25318/82-003-x201900600001-eng [DOI] [PubMed] [Google Scholar]
- 5.Gobbi G, Atkin T, Zytynski T, Wang S, Askari S, Boruff J, et al. Association of Cannabis Use in Adolescence and Risk of Depression, Anxiety, and Suicidality in Young Adulthood. JAMA Psychiatry. 2019;76: 426. doi: 10.1001/jamapsychiatry.2018.4500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.CDC. Marijuana and Public Health. 2021 [cited 24 Sep 2021]. https://www.cdc.gov/marijuana/index.htm
- 7.Yu B, Chen X, Chen X, Yan H. Marijuana legalization and historical trends in marijuana use among US residents aged 12–25: results from the 1979–2016 National Survey on drug use and health. BMC Public Health. 2020;20: 156. doi: 10.1186/s12889-020-8253-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moore TH, Zammit S, Lingford-Hughes A, Barnes TR, Jones PB, Burke M, et al. Cannabis use and risk of psychotic or affective mental health outcomes: a systematic review. Lancet. 2007;370: 319–328. doi: 10.1016/S0140-6736(07)61162-3 [DOI] [PubMed] [Google Scholar]
- 9.Degenhardt L, Hall W, Lynskey M. Exploring the association between cannabis use and depression. Addiction. 2003;98: 1493–1504. doi: 10.1046/j.1360-0443.2003.00437.x [DOI] [PubMed] [Google Scholar]
- 10.Copeland J, Rooke S, Swift W. Changes in cannabis use among young people. Curr Opin Psychiatry. 2013;26: 325–329. doi: 10.1097/YCO.0b013e328361eae5 [DOI] [PubMed] [Google Scholar]
- 11.Hellemans KGC, Wilcox J, Nino JN, Young M, McQuaid RJ. Cannabis Use, Anxiety, and Perceptions of Risk among Canadian Undergraduates: The Moderating Role of Gender. Can J Addict. 2019;10: 22–29. doi: 10.1097/CXA.0000000000000059 [DOI] [Google Scholar]
- 12.van der Steur SJ, Batalla A, Bossong MG. Factors Moderating the Association between Cannabis Use and Psychosis Risk: A Systematic Review. Brain Sci. 2020, 10(2), 97. doi: 10.3390/brainsci10020097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arseneault L, Cannon M, Poulton R, Murray R, Caspi A, Moffitt TE. Cannabis use in adolescence and risk for adult psychosis: Longitudinal prospective study. BMJ 2002, 325, 1212–1213. doi: 10.1136/bmj.325.7374.1212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zammit S, Allebeck P, Andreasson S, Lundberg I, Lewis G. Self reported cannabis use as a risk factor for schizophrenia in Swedish conscripts of 1969: Historical cohort study. BMJ 2002, 325, 1199. doi: 10.1136/bmj.325.7374.1199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Henquet C, Krabbendam L, Spauwen J, Kaplan C, Lieb R, Wittchen HU, et al. Prospective cohort study of cannabis use, predisposition for psychosis, and psychotic symptoms in young people. BMJ 2005, 330, 11. doi: 10.1136/bmj.38267.664086.63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Di Forti M, Morgan C, Dazzan P, Pariante C, Mondelli V, Marques TR, et al. High-potency cannabis and the risk of psychosis. Br J Psychiatry. 2009. Dec;195(6):488–91. doi: 10.1192/bjp.bp.109.064220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Murray RM, Quigley H, Quattrone D, Englund A, Di Forti M. Traditional marijuana, high-potency cannabis and synthetic cannabinoids: Increasing risk for psychosis. World Psychiatry 2016, 15, 195–204. doi: 10.1002/wps.20341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Leadbeater BJ, Ames ME, Linden-Carmichael AN. Age-varying effects of cannabis use frequency and disorder on symptoms of psychosis, depression and anxiety in adolescents and adults. Addiction 2019, 114, 278–293. doi: 10.1111/add.14459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Andreasson S, Engstrom A, Allebeck P, Rydberg U. Cannabis and schizophrenia: a longitudinal study of Swedish conscripts. Lancet 1987;2:1483–6. doi: 10.1016/s0140-6736(87)92620-1 [DOI] [PubMed] [Google Scholar]
- 20.Durlak JA, Taylor RD, Kawashima K, Pachan MK, DuPre EP, Celio CI, et al. Effects of positive youth development programs on school, family, and community systems. Am J Community Psychol. 2007;39: 269–286. doi: 10.1007/s10464-007-9112-5 [DOI] [PubMed] [Google Scholar]
- 21.Murray NG, Low BJ, Hollis C, Cross AW, Davis SM. Coordinated School Health Programs and Academic Achievement: A Systematic Review of the Literature. J Sch Health. 2007;77: 589–600. doi: 10.1111/j.1746-1561.2007.00238.x [DOI] [PubMed] [Google Scholar]
- 22.Morton KL, Atkin AJ, Corder K, Suhrcke M, Sluijs EMF. The school environment and adolescent physical activity and sedentary behaviour: a mixed-studies systematic review. Obes Rev. 2016;17: 142–158. doi: 10.1111/obr.12352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sylva K. School Influences on Children’s Development. J Child Psychol Psychiatry. 1994;35: 135–170. doi: 10.1111/j.1469-7610.1994.tb01135.x [DOI] [PubMed] [Google Scholar]
- 24.Katapally TR. Smart Indigenous Youth: The Smart Platform Policy Solution for Systems Integration to Address Indigenous Youth Mental Health. JMIR Pediatr Parent. 2020;3: e21155. doi: 10.2196/21155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Katapally T. A Digital Epidemiological and Citizen Science Initiative. 2020 [cited 24 Sep 2021]. https://tarunkatapally.com/smart-indigenous-youth/
- 26.Government of Canada. Cannabis laws and regulations. 2020 [cited 24 Sep 2021]. https://www.canada.ca/en/health-canada/services/drugs-medication/cannabis/laws-regulations.html
- 27.Statistics Canada. Population of census metropolitan areas. 2020 [cited 24 Sep 2021]. https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1710007801
- 28.Katapally T. The Smart Platform. 2020 [cited 24 Sep 2021]. https://tarunkatapally.com/the-smart-platform/
- 29.Katapally TR, Chu LM. Digital epidemiological and citizen science methodology to capture prospective physical activity in free-living conditions: a SMART Platform study. BMJ Open. 2020;10: e036787. doi: 10.1136/bmjopen-2020-036787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Katapally TR, Bhawra J, Leatherdale ST, Ferguson L, Longo J, Rainham D, et al. The SMART Study, a Mobile Health and Citizen Science Methodological Platform for Active Living Surveillance, Integrated Knowledge Translation, and Policy Interventions: Longitudinal Study. JMIR Public Heal Surveill. 2018;4: e31. doi: 10.2196/publichealth.8953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McKinnon B, Gariépy G, Sentenac M, Elgar FJ. Adolescent suicidal behaviours in 32 low- and middle-income countries. Bull World Health Organ. 2016;94: 340–350F. doi: 10.2471/BLT.15.163295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Statistics Canada. Survey questions related to cannabis/marijuana, by survey, 1985 through 2015. 2018 [cited 24 Sep 2021]. https://www150.statcan.gc.ca/n1/pub/82-003-x/2018002/article/54908/tbl/tbla-eng.htm
- 33.Weeks M, Colman I. Predictors of Suicidal Behaviors in Canadian Adolescents with No Recent History of Depression. Arch Suicide Res. 2017;21: 354–364. doi: 10.1080/13811118.2016.1193076 [DOI] [PubMed] [Google Scholar]
- 34.van Ours JC, Williams J, Fergusson D, Horwood LJ. Cannabis use and suicidal ideation. J Health Econ. 2013;32: 524–537. doi: 10.1016/j.jhealeco.2013.02.002 [DOI] [PubMed] [Google Scholar]
- 35.Wilcox HC. Epidemiological evidence on the link between drug use and suicidal behaviors among adolescents. Can Child Adolesc Psychiatr Rev. 2004;13: 27–30. Available: http://www.ncbi.nlm.nih.gov/pubmed/19030482 [PMC free article] [PubMed] [Google Scholar]
- 36.Poorolajal J, Haghtalab T, Farhadi M, Darvishi N. Substance use disorder and risk of suicidal ideation, suicide attempt and suicide death: a meta-analysis. J Public Health (Bangkok). 2016;38: e282–e291. doi: 10.1093/pubmed/fdv148 [DOI] [PubMed] [Google Scholar]
- 37.Klomek AB, Sourander A, Gould M. The Association of Suicide and Bullying in Childhood to Young Adulthood: A Review of Cross-Sectional and Longitudinal Research Findings. Can J Psychiatry. 2010;55: 282–288. doi: 10.1177/070674371005500503 [DOI] [PubMed] [Google Scholar]
- 38.Alavi N, Reshetukha T, Prost E, Antoniak K, Patel C, Sajid S, et al. Relationship between Bullying and Suicidal Behaviour in Youth presenting to the Emergency Department. J Can Acad Child Adolesc Psychiatry. 2017;26: 70–77. Available: http://www.ncbi.nlm.nih.gov/pubmed/28747929 [PMC free article] [PubMed] [Google Scholar]
- 39.Espelage DL, Holt MK. Suicidal Ideation and School Bullying Experiences After Controlling for Depression and Delinquency. J Adolesc Heal. 2013;53: S27–S31. doi: 10.1016/j.jadohealth.2012.09.017 [DOI] [PubMed] [Google Scholar]
- 40.Tang JJ, Yu Y, Wilcox HC, Kang C, Wang K, Wang C, et al. Global risks of suicidal behaviours and being bullied and their association in adolescents: School-based health survey in 83 countries. EClinicalMedicine. 2020;19: 100253. doi: 10.1016/j.eclinm.2019.100253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Radliff KM, Wheaton JE, Robinson K, Morris J. Illuminating the relationship between bullying and substance use among middle and high school youth. Addict Behav. 2012;37: 569–572. doi: 10.1016/j.addbeh.2012.01.001 [DOI] [PubMed] [Google Scholar]
- 42.Zhang Y-Y, Lei Y-T, Song Y, Lu R-R, Duan J-L, Prochaska JJ. Gender differences in suicidal ideation and health-risk behaviors among high school students in Beijing, China. J Glob Health. 2019;9: 010604. doi: 10.7189/jogh.09.010604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Peter T, Edkins T, Watson R, Adjei J, Homma Y, Saewyc E. Trends in suicidality among sexual minority and heterosexual students in a canadian population-based cohort study. Psychol Sex Orientat Gend Divers. 2017;4: 115–123. doi: 10.1037/sgd0000211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Saewyc EM, Skay CL, Hynds P, Pettingell S, Bearinger LH, Resnick MD, et al. Suicidal Ideation and Attempts in North American School-Based Surveys: Are Bisexual Youth at Increasing Risk? J LGBT Health Res. 2007;3: 25–36. doi: 10.1300/J463v03n02_04 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gogovor A, Mollayeva T, Etherington N, Colantonio A, Légaré F, Adisso L, et al. Sex and gender analysis in knowledge translation interventions: challenges and solutions. Heal Res Policy Syst. 2020;18: 108. doi: 10.1186/s12961-020-00625-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zuckermann AME, Gohari MR, de Groh M, Jiang Y, Leatherdale ST. The role of school characteristics in pre-legalization cannabis use change among Canadian youth: implications for policy and harm reduction. Health Educ Res. 2020;35: 297–305. doi: 10.1093/her/cyaa018 [DOI] [PubMed] [Google Scholar]
- 47.Probst C, Elton-Marshall T, Imtiaz S, Patte KA, Rehm J, Sornpaisarn B, et al. A supportive school environment may reduce the risk of non-medical prescription opioid use due to impaired mental health among students. Eur Child Adolesc Psychiatry. 2021;30: 293–301. doi: 10.1007/s00787-020-01518-3 [DOI] [PubMed] [Google Scholar]
- 48.Gohari MR, Cook RJ, Dubin JA, Leatherdale ST. The impact of an alcohol policy change on developmental trajectories of youth alcohol use: examination of a natural experiment in Canada. Can J Public Heal. 2021;112: 210–218. doi: 10.17269/s41997-020-00366-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Silins E, Horwood LJ, Patton GC, Fergusson DM, Olsson CA, Hutchinson DM, et al. Young adult sequelae of adolescent cannabis use: an integrative analysis. The Lancet Psychiatry. 2014;1: 286–293. doi: 10.1016/S2215-0366(14)70307-4 [DOI] [PubMed] [Google Scholar]
- 50.Tobler NS, Stratton HH. Effectiveness of School-Based Drug Prevention Programs: A Meta-Analysis of the Research. J Prim Prev 1997. 181. 1997;18: 71–128. doi: 10.1023/A:1024630205999 [DOI] [Google Scholar]
- 51.Tobler NS, Roona MR, Ochshorn P, Marshall DG, Streke A V., Stackpole KM. School-Based Adolescent Drug Prevention Programs: 1998 Meta-Analysis. J Prim Prev 2000. 204. 2000;20: 275–336. doi: 10.1023/A:1021314704811 [DOI] [Google Scholar]
- 52.Porath-Waller AJ, Beasley E, Beirness DJ. A Meta-Analytic Review of School-Based Prevention for Cannabis Use. Heal Educ Behav. 2010;37: 709–723. doi: 10.1177/1090198110361315 [DOI] [PubMed] [Google Scholar]
- 53.Ceccaroni L, Bibby J, Roger E, Flemons P, Michael K, Fagan L, et al. Opportunities and Risks for Citizen Science in the Age of Artificial Intelligence. Citiz Sci Theory Pract. 2019;4. doi: 10.5334/cstp.241 [DOI] [Google Scholar]
- 54.World Health Organization. WHO guideline: recommendations on digital interventions for health system strengthening Web Supplement 2: Summary of findings and GRADE tables. 2019. http://apps.who.int/bookorders. [PubMed]
- 55.Mackie CJ, O’Leary-Barrett M, Al-Khudhairy N, Castellanos-Ryan N, Struve M, Topper L, et al. Adolescent bullying, cannabis use and emerging psychotic experiences: a longitudinal general population study. Psychol Med. 2013;43: 1033–1044. doi: 10.1017/S003329171200205X [DOI] [PubMed] [Google Scholar]
- 56.Joshi S V., Stubbe D, Li S-TT, Hilty DM. The Use of Technology by Youth: Implications for Psychiatric Educators. Acad Psychiatry. 2019;43: 101–109. doi: 10.1007/s40596-018-1007-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Fonseka TM, Bhat V, Kennedy SH. The utility of artificial intelligence in suicide risk prediction and the management of suicidal behaviors. Aust New Zeal J Psychiatry. 2019;53: 954–964. doi: 10.1177/0004867419864428 [DOI] [PubMed] [Google Scholar]
- 58.Wainberg ML, Scorza P, Shultz JM, Helpman L, Mootz JJ, Johnson KA, et al. Challenges and Opportunities in Global Mental Health: a Research-to-Practice Perspective. Curr Psychiatry Rep. 2017;19: 28. doi: 10.1007/s11920-017-0780-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cash SJ, Bridge JA. Epidemiology of youth suicide and suicidal behavior. Curr Opin Pediatr. 2009;21: 613–9. doi: 10.1097/MOP.0b013e32833063e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ivey-Stephenson AZ, Demissie Z, Crosby AE, Stone DM, Gaylor E, Wilkins N, et al. Suicidal Ideation and Behaviors Among High School Students—Youth Risk Behavior Survey, United States, 2019. MMWR Suppl. 2020;69: 47–55. doi: 10.15585/mmwr.su6901a6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Garcia-Ceja E, Riegler M, Nordgreen T, Jakobsen P, Oedegaard KJ, Tørresen J. Mental health monitoring with multimodal sensing and machine learning: A survey. Pervasive Mob Comput. 2018;51: 1–26. doi: 10.1016/j.pmcj.2018.09.003 [DOI] [Google Scholar]
- 62.Uhlhaas P, Torous J. Digital tools for youth mental health. npj Digit Med. 2019;2: 104. doi: 10.1038/s41746-019-0181-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Katapally T.R.; Chu L.M. Methodology to Derive Objective Screen-State from Smartphones: A SMART Platform Study. Int. J. Environ. Res. Public Health 2019, 16, 2275. doi: 10.3390/ijerph16132275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zielinski L, Bhatt M, Sanger N, Plater C, Worster A, Varenbut M, et al. Association between cannabis use and methadone maintenance treatment outcomes: an investigation into sex differences. Biol Sex Differ. 2017;8: 8. doi: 10.1186/s13293-017-0130-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Katapally T.R.; Rainham D.; Muhajarine N. Factoring in weather variation to capture the influence of urban design and built environment on globally recommended levels of moderate to vigorous physical activity in children. BMJ Open 2015, 5, e009045. doi: 10.1136/bmjopen-2015-009045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Katapally T.R.; Rainham D.; Muhajarine N. The Influence of Weather Variation, Urban Design and Built Environment on Objectively Measured Sedentary Behaviour in Children. AIMS Public Health 2016, 3, 663–681. doi: 10.3934/publichealth.2016.4.663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Statista. Number of smartphone users worldwide from 2016 to 2021. 2021 [cited 24 Sep 2021]. https://www.statista.com/statistics/330695/number-of-smartphone-users-worldwide/
- 68.Katapally TR. A Global Digital Citizen Science Policy to Tackle Pandemics Like COVID-19. J Med Internet Res. 2020;22: e19357. doi: 10.2196/19357 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data cannot be shared publicly because citizen scientists have co-ownership. Data are available from the University of Regina’s Institutional Data Access / Ethics Committee (research.ethics@uregina.ca) for researchers who meet the criteria for access to confidential data.