Abstract
Objective
To investigate the association between time to active sitting position and clinical features in people with COVID-19 admitted to intensive care unit (ICU) and referred to physiotherapists.
Method
Prospective study conducted in the largest temporary ICU in Lombardy (Italy) between April 2020 and June 2021. All individuals with COVID-19 who received physiotherapy were included. Multivariable Cox proportional hazard model was fitted to explore the statistical association between active sitting position and characteristics of patients referred to physiotherapists, also accounting for the different multidisciplinary teams responsible for patients.
Results
284 individuals over 478 (59.4%) had access to physiotherapy, which was performed for a median of 8 days, without difference between multidisciplinary teams (P = 0.446). The active sitting position was reached after a median of 18 (IQR: 10.0–32.0) days. Sex was the only characteristic associated with the time to active sitting position, with males showing a reduced hazard by a factor of 0.65 (95% CI: 0.48–0.87; P = 0.0042) compared to females. At ICU discharge, nearly 50% individuals increased Manchester Mobility Score by 3 points. During physiotherapy no major adverse event was recorded.
Conclusion
Individuals with COVID-19 take long time to reach active sitting position in ICU, with males requiring longer rehabilitation than females.
Keywords: Active sitting position, COVID-19, Early mobilization, Sex gap, Physiotherapy
Abbreviations: AEs, Adverse Events; BMI, Body Mass Index; CI, Confidence Interval; FiCOMP, Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico; HR, Hazard Ratio; ICU-AW, Intensive Care Unit- Acquired Weakness; IMV, Invasive Mechanical Ventilation; LOS, Length of Stay; MDTs, Multidisciplinary Teams; MMS, Manchester Mobility Score; PTs, Physiotherapists; SARS-CoV-2, Severe Acute Respiratory Syndrome Coronavirus 2
1. Introduction
People admitted to the intensive care unit (ICU) for Coronavirus disease (COVID-19) frequently required endotracheal intubation and invasive mechanical ventilation (IMV) [1], with males more susceptible than females in terms of disease severity and prevalence [[2], [3], [4]].
Persons with severe COVID-19 under deep sedation, prolonged IMV and ICU length of stay (LOS) are also at high risk of developing ICU-acquired weakness (ICU-AW) and post intensive care syndrome [5]. Therefore, several guidelines and recommendations have been published worldwide to limit the functional sequelae of COVID-19 by including early physiotherapy and rehabilitation interventions [3,6,7]. Increasing levels of mobility in ICU (ranging from in-bed interventions to mobilizing more than 30 m) has been associated with improvements of clinical and functional outcomes and increased odds of discharge home [8]. Most importantly, patients reaching active sitting position (ASP) showed reduced ICU LOS [9], which is associated with better long-term functional outcome [10]. Moreover, gas exchanges and respiratory mechanics are also better after 1 h of ASP and increased tidal volume and oxygen consumption are reported as positive effects of such postural change [11].
Considering the clinical importance of ASP for patients’ recovery, the aim of our study is to describe the time to active sitting position in people with COVID-19 admitted to ICU and its association with clinical features in those referred to the physiotherapy team. Further, we aimed to report the number of adverse events during physiotherapy intervention.
2. Methods
2.1. Study design
This prospective study was conducted at Fiera Milano COVID-19 Intensive Care Hospital, the largest temporary healthcare structure built in Italy, led by our Institution Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico (FiCOMP) during the pandemic between April 2020 and June 2021. All adult patients with Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) infection admitted to ICU were enrolled in this study. The study was approved by the local ethics committee (ethics approval number 827_2021).
2.2. Hospital organization
Italy was the first western country to face the COVID-19 outbreak and to implement extraordinary measures for SARS-CoV-2 containment [12]. To cope with the lack of ICU beds, the Lombardy Region created a temporary hospital, in partnership with Fondazione Fiera Milano [13]. The Fiera Milano COVID-19 Intensive Care Hospital was based on the conversion of two floors of the Milano fair building into a healthcare structure thanks to the installation of fully equipped independent sub-units, distributed across a total surface area of 25,000 m2 and able to accommodate over 200 patients. Our Institution was the head of the general organization and worked synergically with other eight hospitals: each hospital was responsible for one sub-unit with its own team composed by intensivists and nurses. FiCOMP supported the temporary hospital with healthcare assistants, X-ray technicians and physiotherapists (PTs). Per current practice, patients from the FiCOMP sub-unit were routinely assessed by PTs, whereas in other sub-units PTs were called upon request. During the study period, a team of five PTs (composed by one experienced PT in critical care and four PTs with more heterogenous background) worked daily covering the whole week.
2.3. Physiotherapy interventions
After neuromuscular blocking agent withdrawal, PTs delivered functional mobilization, in-bed sitting positioning and hoist transfer to chair for sedated patients [14]. Due to prolonged invasive mechanical ventilation, respiratory physiotherapy was implemented to favor weaning from mechanical ventilation [15]. Particularly, the rehabilitative program involved posture changes, which are known to modify ventilation/perfusion ratio and to promote lung recruitment, airway clearance techniques and cough assistance [[16], [17]]. At the same time, we focused on muscle recruitment and strengthening exercises for the limbs and dynamic trunk control with the intention of progressing to active transfer from bed to chair, standing, stepping in place and ambulation, with or without assistance [18]. The short-term objective was to reach the ASP, which has been shown to elicit a cardiorespiratory response and increase lung volumes in the critically ill, explained by greater muscle activity during the task [11]. The ASP was performed using the sitting out the edge of the bed position supervised by one physiotherapist and at least one nurse, after having secured the medical devices. We gradually made the task harder using back supports with variable stability in order to challenge the patient to hold the position autonomously, thus stimulating functional recovery [19]. Adverse events (AEs) during physiotherapy were define as an episode during rehabilitation associated with any of the following: stopping or pausing mobilization/rehabilitation, interventions or additional therapy required to address the event (i.e., accidental removal of any medical device, resulting in a new positioning procedure), adverse health consequences not resolved by stopping mobilization/rehabilitation.
All PTs staff used adequate personal protective equipment (including N95 mask, fluid-resistant long-sleeved grown, face shield and gloves) as recommended [6,7].
2.4. Data collection
Patients baseline characteristics, including demographics, days of invasive mechanical ventilation, presence of endotracheal tube and/or tracheostomy, ICU LOS and mortality were retrieved from electronic medical records. Physical function was measured at the beginning of physiotherapy and at ICU discharge using the Manchester Mobility Score (MMS), a seven-point scale used for assessing mobility levels in critical care setting [20].
2.5. Statistical analysis
Variables are summarized as mean and standard deviation (SD) and presented stratified by exposure to physiotherapy treatment. Independent t-test was used to compare continuous variables between individuals who received or not physiotherapy; for categorical variables, we adopted chi-square test statistics or Fisher exact test, as appropriate. Uncertainty of estimates is reported as 95% confidence interval (CI).
In order to investigate the association between time to sitting position and characteristics of patients referred to PTs, we used a multivariable Cox proportional hazard (PH) model accounting for age, sex, body mass index (BMI), level of hypoxemia (PaO2/FiO2 ratio), multidisciplinary teams (MDTs) involved (FiCOMP versus other MDTs), and presence of any comorbidity. Age, BMI and PaO2/FiO2 ratio were fitted as linear functions, based on the Akaike information criterion. Also, a pooled interaction test between MDTs and considered features was performed, taking into account potential different medical practice among teams.
Model's assumptions were checked using smoothed scaled Schoenfeld residuals and formal test, as proposed by Therneau [21]. Model validation and calibration with 300 bootstraps were performed reporting Somers' DXY and mean error, respectively. Model estimates are reported as hazard ratio (HR) and 95%CI. For all analyses, P-values were two-sided, and P < 0.05 was considered to be statistically significant. All the analyses were performed using R Core Team, version 3.6.2, with survminer and rms packages added [22].
3. Results
The first individual was admitted in Fiera Milano COVID-19 Intensive Care Hospital on April 6, 2020. As long as the hub was maintained opened, 284 individuals over 478 (59.4%) were referred to PTs. This hub discharged the last individual on June 05, 2021. Characteristics of individuals observed during the study period are presented in Table 1 .
Table 1.
Patients’ characteristics.
| PT (No), N = 194 | PT (Yes), N = 284 | Difference (95%CI) | p-value | |
|---|---|---|---|---|
| Age, years | 67.4 (7.3) | 62.5 (9.3) | 4.9 (3.4; 6.3) | <0.001 |
| BMI, kg/m2 | 29.1 (4.7) | 29.2 (4.6) | −0.1 (−0.9; 0.8) | 0.842 |
| Sex | 0.592 | |||
| Female | 49/194 (25.3%) | 78/284 (27.5%) | 2.2 (−5.8; 10.2) | |
| Male | 145/194 (74.7%) | 206/284 (72.5%) | −2.2 (−10.2; 5.8) | |
| Presence of any comorbidity | 162/194 (83.5%) | 226/284 (79.6%) | 3.9 (−3.1; 10.9) | 0.280 |
| Comorbidities | ||||
| Pulmonary | 34/194 (17.5%) | 44/284 (15.5%) | 2.0 (−4.8; 8.8) | 0.554 |
| Psychiatric | 11/194 (5.7%) | 18/284 (6.3%) | −0.7 (−5.0; 3.6) | 0.764 |
| Metabolic | 84/194 (43.3%) | 100/284 (35.2%) | 8.1 (−0.8; 17.0) | 0.074 |
| Musculoskeletal | 37/194 (19.1%) | 48/284 (16.9%) | 2.2 (−4.9; 9.2) | 0.542 |
| Cardiovascular | 126/194 (64.9%) | 162/284 (57.0%) | 7.9 (−0.9; 16.8) | 0.082 |
| ICU LOS, days | 15.9 (10.5) | 27.5 (18.8) | −11.6 (−14.3; −8.9) | <0.001 |
| IMV, days | 17.0 (10.7) | 24.1 (17.1) | −7.1 (−9.6; −4.6) | <0.001 |
| Presence of tracheostomy | 21/194 (10.8%) | 79/284 (27.8%) | −17 (−23.8; −10.2) | <0.001 |
| Alive | 63/194 (32.5%) | 261/284 (91.9%) | −59.4 (−66.7; −52.1) | <0.001 |
Data are presented as mean (SD) or counts (percentage). BMI = Body Mass Index; ICU = Intensive Care Unit; LOS = Length Of Stay; IMV = Invasive Mechanical Ventilation.
The 76.9% (90/117) of patients followed by the FiCOMP-MDT had access to physiotherapy whereas we recorded a lower proportion (194/361, 53.7%) in the other large group of patients followed by other heterogenous MDTs. As per clinical practice, enteral nutrition was started early after ICU admission using a high protein liquid formula via nasogastric tube. All individuals except 2 had endotracheal intubation (2/478, 0.4%), and these received physiotherapy. In this group, reintubation proportion was 7.8% points higher (95%CI: 4.2%–11.4%) compared to individuals for those physiotherapy was not requested. On the whole, we recorded more deaths in the group where physiotherapy was not started (131/194, 67.5%).
Physiotherapy was performed for a median of 8 days, and only the 25% of patients received treatments for longer than 14 days, without difference between MDTs (P = 0.446). When evaluated at discharge from physiotherapy using MMS, the 10.7% (28/261) of patients showed no improvement, the 40.2% (105/261) increased MMS by 2 points and the 49.0% (128/261) improved by more than 3 points compared to baseline. In terms of AEs during physiotherapy, we did not record any fall nor occurrence of pneumothorax. In this group, 131/284 (46.1%) had at least one oxygen desaturation episode, 1 accidental decannulation (1/284, 0.4%), 3 accidental feeding tube removals (3/284, 1.1%) and 1 accidental displacement of medical devices (1/284, 0.4%).
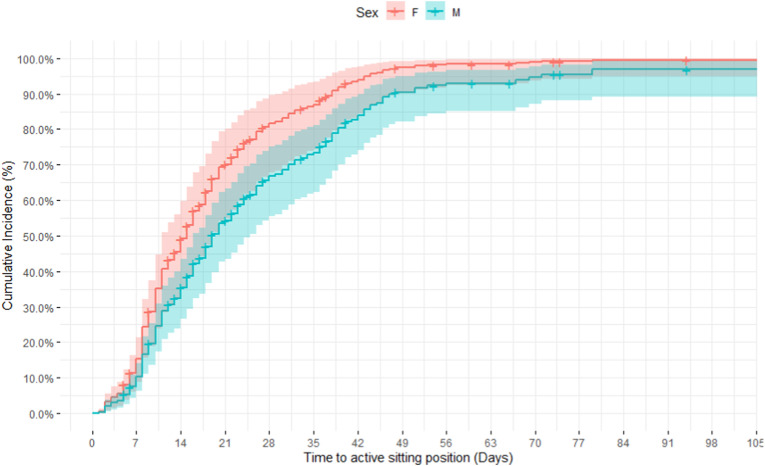
Patients treated by PTs reached the ASP after a median of 18 days since they were hospitalized; particularly, 50% of patients managed by FiCOMP-MDT were positioned sit between the 8th and 37th day after ICU admittance, whereas 50% of patients followed by other MDTs between the 10th and 31st day. Among the clinical characteristics used to fit the Cox PH model, sex was the only feature associated with the hazards of ASP. Particularly, being male reduces the hazards by a factor of 0.65, or 35%. Cumulative incidence for the ASP at any given point in time for males and females is provided in Fig. 1 .
Fig. 1.
Cumulative incidence curves for males and females with any comorbidity and managed by FiCOMP-MDT, with age, BMI and PaO2/FiO2 ratio hold at mean sample values.
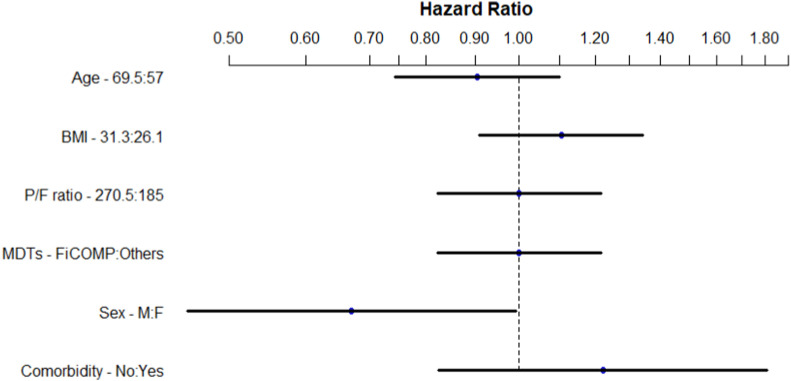
The HR associated with patients managed by MDT at our Institution versus other MDTs is 1.03 (95%CI: 0.79 to 1.36). Fig. 2 presents the point and interval estimates of all considered variables. From the fitted model we did not find evidence of interaction between MDTs and other covariates (P = 0.270).
Fig. 2.
Hazard ratios and 95% confidence bars for the association of covariates in the fitted model, using interquartile range. For example, when age changes from its lower quartile to the upper quartile (57y to 69.5y), the HR decreases (HR 0.88, 95%CI:0.72 to 1.06) Other HRs are: BMI (1.09, 95%CI; 0.93 to 1.27), PaO2/FiO2 ratio (1.05, 95%CI: 0.89 to 1.24), Comorbidity (1.23, 95%CI: 0.88 to 1.72).
Although validating data for prospective use was not necessary, the model showed a predictive discrimination of 0.10, with a slope shrinkage of 0.76 indicating some overfitting. The absolute calibration error is 0.01 for 7-day prediction.
4. Discussion
When the Fiera Milano COVID-19 Intensive Care Hospital admitted the first patient (April 6, 2020), the Lombardy region reported 1343 people already hospitalized in ICU and 9202 were the people dead counted so far [23]. Over one year, the temporary hospital admitted nearly 500 patients, and more than 50% were referred to the physiotherapy team, that worked homogenously across the different MDTs. On average, patients reached the active sitting position in 18 days, and the only factor negatively associated with time to ASP was being male.
Literature is scanty about teamworking in the ICU. In the temporary hospital in Milan, the organizational context provided the same group of PTs delivering physiotherapy under two difference circumstances: PTs as part on an established MDT in the FiCOMP sub-unit and PT interventions started upon medical request in all other sub-units. Nevertheless, no evidence of difference was found.
We may assume that the context did not influence the performance of the PT team, and therefore short-term rehabilitation outcomes. Although in the FiCOMP sub-unit PTs typically oversee the provision of mechanical ventilation and early mobilization, which are two crucial points for patients experiencing respiratory failure and among the most common ICU treatments [[24], [25], [26]], this may provide a framework for highlighting that a strong PT team could minimize disparities among different attitudes towards rehabilitation [27,28].
Recently, we illustrated how the combined efforts of experienced physiotherapists and nurses made pronation of patients mechanically ventilated and deeply sedated safe and feasible, without affecting their mobility and muscle strength at ICU discharge [29]. A structured intervention with appropriate supervision and support by PTs with previous clinical experience in treating critically ill patients could play a crucial role to manage an emergency situation [28], improving independent physical status at hospital discharge [30,31]. When PTs are integrated in the ICU team, greater functional goals can be expected, favoring a rapid discharge from ICU [27,32].
In the present study, ASP was reached after two weeks from ICU admission, in line with the results obtained by another group from United Kingdom [5]. Previous works on acutely hospitalized patients managed by trained ICU staff found that median time to sitting position was below 9 days [32,33]. This discrepancy can be explained by the different care of patients with COVID-19 requiring prolonged IMV and deep sedation. ASP reached within 5 days from ICU admission was found associated with a shorter LOS in ICU in a group of critically ill individuals [9]. To the best of our knowledge, this is the only study specifically focusing on ASP and its relevance towards clinically relevant outcomes such as ICU LOS. Usually, ASP is presented as a component of an articulated mobility algorithm to promote early mobilization [18,32,[34], [35], [36]]. Since the introduction of early mobilization in ‘70s, a growing body of evidence demonstrated that it is safe and feasible for the severe individuals admitted in ICU [37]. Among the described short-term benefits, we list shorter delirium duration, more ventilator-free days and increased level of autonomy at hospital discharge [31], together with decreased ICU and hospital LOS [33].
It is important mentioning that we are describing for the first time an association between sex and a rehabilitative milestone such as ASP. Biological sex was already reported as a determinant of COVID-19 disease prevalence and severity [2]. However, anatomical and hormonal features were recently reported as significant differences between biological males and females [38]. Literature on sex-related differences is contradicting. Female sex showed an advantage for long-term physical function recovery in one study on acute respiratory failure survivors [39]. On the contrary, other findings have described females at higher risk of ICU-AW than males [40,41]. If confirmed by larger studies, such difference between males and females may have a direct impact on clinical practice and sex-specific assessments should be considered.
Among the characteristics of patients referred to physiotherapy team, we are reporting a higher rate of tracheostomy, a longer LOS in ICU and length of IMV, as expected. These differences can be due to the referral criteria for physiotherapy intervention. Usually, patients were referred to PTs when cardiovascular and neurological conditions were stable, therefore a higher death rate is also reported when physiotherapy intervention was not deemed feasible. In addition, the higher number of tracheostomy procedures in patients who have performed physiotherapy could be explained by the need to support weaning and rehabilitation. Consistently, patients who were not referred to PTs were 5-years older. As reported elsewhere [2], age was shown to be a key factor for COVID-19 survival.
It is interesting to compare our results with previous findings on people undergoing physiotherapy during ICU stay. On average, ICU LOS and IMV duration were higher in our study compared to other reports [5,42]; Stutz et al. enrolled a population of less severe patients with COVID-19, where only 40% of subjects were intubated, as compared to 99.6% of our work. Moreover, we counted less tracheostomy procedures as opposed to McWilliams et al. (27.8% versus 77%), investigating a population of severe patients with COVID-19 from United Kingdom. It is worth mentioning that tracheostomy was inserted mainly for inadequate cough strength, difficult weaning and extubation failure in our study. With regard to previous findings from our group collected on severe patients with COVID-19 and managed in the ICU of our Institution [29], we are reporting higher IMV duration and ICU stay. These differences could also be due to several organizational issues. The study of Binda et al. is restricted to the very first pandemic wave [29], when emergency levels and ICU-bed demands were high, thus requiring a rapid weaning from ventilators and a quick ICU discharge. Also, the lack of sub-intensive units inside the Fiera Milano COVID-19 Intensive Care Hospital was a barrier to fast ICU-discharge of patients. Moreover, in the present study we observed a smaller proportion of people with MMS score <3 at ICU discharge (42% versus 85%), suggesting that patients showed better functional recovery despite longer ICU stay.
In the cohort described in the present study, features related with severe COVID-19 (i.e., BMI, PaO2/FiO2 ratio) and presence of comorbidity were not found associated with time to ASP, eventually suggesting that these may be not considered as barriers of early mobilization. Similar results were obtained by McWilliams et al., except for BMI: patients with a BMI >40 experienced a significant delay in time to first mobilization compared to patients with BMI of 20–24 (18 versus 10 days) [5]. Previous work already reported early mobilization as feasible also in patients receiving invasive support and deep sedation [43]. Finally, very few serious AEs occurred during physiotherapy. Despite oxygen desaturation, which is described as a common finding during physiotherapy [44] and prone positioning [45] in patients with COVID-19, accidental device removals were reported in five individuals only (1.8%, 5/284), adding to literature that early mobilization is generally safe and within expected frequency [46].
4.1. Strength and limitations
Our study has several limitations. Because of COVID-19 pandemic emergency and infectious-related restrictions, most of instrumental information was not available, especially during the first wave. The absence of safe cleaning and disinfection procedures during early months of the pandemic restrained us from using any device to measure functional outcomes in patients with COVID-19. Indeed, different studies recommended early physiotherapy to improve physical outcomes at hospital discharge, however we were able to record only mobility scores as functional data at ICU discharge. Second, referral to PTs was not homogenous between MDTs thus leading to potential biased associations in the group receiving physiotherapy. However, pooled interaction test between MDTs and selected covariates was not significant, thus indicating the lack of evidence of association between specific features among individuals with COVID-19 managed by different MDTs. Due to this unprecedented health emergency, information about exposure to systemic steroids were not collected, which may play a role in functional outcomes of individuals with COVID-19 [47].
It is worth noting that that our work represents a unique experience in the emergency setting, also considering the large number of patients treated by PTs and managed by different MDTs, thus giving to the present findings a satisfactory external validity.
5. Conclusion
Individuals with COVID-19 take more than two weeks to reach ASP in ICU, with males requiring longer rehabilitation than females. Overall, early mobilization was safe and practical, even when performed by one PTs team across many MDTs with heterogenous backgrounds towards early rehabilitation. The impact of biological sex on physical function recovery in ICU needs to be further addressed and sex-specific issues in rehabilitation should be considered.
Declaration of competing interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: Francesco Blasi reports financial support was provided by Pfizer Inc. Francesco Blasi reports financial support was provided by AstraZeneca Pharmaceuticals LP. Francesco Blasi reports financial support was provided by Chiesi Pharmaceuticals Inc. Francesco Blasi reports financial support was provided by Insmed Inc. Francesco Blasi reports financial support was provided by Menarini Research. Francesco Blasi reports financial support was provided by GSK. Francesco Blasi reports financial support was provided by Guidotti Laboratories. Francesco Blasi reports financial support was provided by Novartis. Francesco Blasi reports financial support was provided by Viatris Inc. Francesco Blasi reports financial support was provided by Vertex Pharmaceuticals. Francesco Blasi reports financial support was provided by Zambon Pharmaceutical Laboratories.
CRediT authorship contribution statement
Veronica Rossi: Conceptualization, Investigation, Data curation, Writing – original draft. Cesare Del Monaco: Conceptualization, Investigation, Data curation, Writing – original draft. Simone Gambazza: Methodology, Formal analysis, Writing – original draft. Martina Santambrogio: Investigation, Data curation, Writing – original draft. Filippo Binda: Investigation, Data curation, Writing – original draft. Mariangela Retucci: Investigation, Data curation, Writing – original draft. Emilia Privitera: Conceptualization, Investigation, Writing – review & editing. Marco Mantero: Resources, Writing – review & editing. Nicola Bottino: Resources, Writing – review & editing, Writing – review & editing, Supervision. Dario Laquintana: Writing – review & editing, Supervision, Project administration, All authors read and approved the final manuscript.
References
- 1.Yang X., Yu Y., Xu J., Shu H., Xia J., Liu H., Wu Y., Zhang L., Yu Z., Fang M., Yu T., Wang Y., Pan S., Zou X., Yuan S., Shang Y. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir. Med. 2020;8:475–481. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Márquez E.J., Trowbridge J., Kuchel G.A., Banchereau J., Ucar D. The lethal sex gap: COVID-19. Immun. Ageing. 2020;17:1–8. doi: 10.1186/s12979-020-00183-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., Zhang L., Fan G., Xu J., Gu X., Cheng Z., Yu T., Xia J., Wei Y., Wu W., Xie X., Yin W., Li H., Liu M., Xiao Y., Gao H., Guo L., Xie J., Wang G., Jiang R., Gao Z., Jin Q., Wang J., Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ishigami J. Risk factors for severe COVID-19 in a large medical records linkage system in the United States. Mayo Clin. Proc. 2021;96:2508–2510. doi: 10.1016/j.mayocp.2021.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McWilliams D., Weblin J., Hodson J., Veenith T., Whitehouse T., Snelson C. Rehabilitation levels in patients with COVID-19 admitted to intensive care requiring invasive ventilation an observational study. Ann. Am. Thorac. Soc. 2021;18:122–129. doi: 10.1513/AnnalsATS.202005-560OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lazzeri M., Lanza A., Bellini R., Bellofiore A., Cecchetto S., Colombo A., D'Abrosca F., Del Monaco C., Gaudellio G., Paneroni M., Privitera E., Retucci M., Rossi V., Santambrogio M., Sommariva M., Frigerio P. Respiratory physiotherapy in patients with COVID-19 infection in acute setting: a position paper of the Italian association of respiratory physiotherapists (ARIR) Monaldi Arch. Chest Dis. 2020;90 doi: 10.4081/monaldi.2020.1285. [DOI] [PubMed] [Google Scholar]
- 7.Thomas P., Baldwin C., Bissett B., Boden I., Gosselink R., Granger C.L., Hodgson C., Jones A.Y.M., Kho M.E., Moses R., Ntoumenopoulos G., Parry S.M., Patman S., van der Lee L. Physiotherapy management for COVID-19 in the acute hospital setting: recommendations to guide clinical practice. Pneumonology. 2020;33:32–35. doi: 10.1016/j.jphys.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim R.Y., Murphy T.E., Doyle M., Pulaski C., Singh M., Tsang S., Wicker D., Pisani M.A., Connors G.R., Ferrante L.E. Factors associated with discharge home among medical ICU patients in an early mobilization program. Crit. Care Explor. 2019;1 doi: 10.1097/CCE.0000000000000060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McWilliams D., Pantelides K. Does physiotherapy led early mobilisation affect length of stay on ICU? Assoc. Chart. Physiother. Respir. Care. 2008;40:5–11. https://www.researchgate.net/publication/285704470 [Google Scholar]
- 10.Gil S., Jacob Filho W., Shinjo S.K., Ferriolli E., Busse A.L., Avelino-Silva T.J., Longobardi I., de Oliveira Júnior G.N., Swinton P., Gualano B., Roschel H., Bonfá E., Utiyama E., Segurado A., Perondi B., Morais A.M., Montal A., Letaif L., Fusco S., Rodrigues da Silva M.F., Rocha M., Marcilio I., Rios I.C., Kawano F.Y.O., de Jesus M.A., Kallas É.G., Carmo C., Tanaka C., de Souza H.P., Marchini J.F.M., Carvalho C., Ferreira J.C., Levin A.S.S., de Oliveira M.S., Guimarães T., dos Santos Lázari C., da Silva Duarte A.J., Sabino E., Chaves Magri M.M., Barros-Filho T.E.P., Braido Francisco M.C.P. Muscle strength and muscle mass as predictors of hospital length of stay in patients with moderate to severe COVID-19: a prospective observational study. J. Cachexia. Sarcopenia Muscle. 2021 doi: 10.1002/jcsm.12789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Collings N., Cusack R. A repeated measures, randomised cross-over trial, comparing the acute exercise response between passive and active sitting in critically ill patients. BMC Anesthesiol. 2015;15:1. doi: 10.1186/1471-2253-15-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grasselli G., Pesenti A., Cecconi M. Critical care utilization for the COVID-19 outbreak in Lombardy, Italy: early experience and forecast during an emergency response. JAMA. 2020;323:1545–1546. doi: 10.1001/jama.2020.4031. [DOI] [PubMed] [Google Scholar]
- 13.Rezoagli E., Magliocca A., Bellani G., Pesenti A., Grasselli G. Development of a critical care response - experiences from Italy during the coronavirus disease 2019 pandemic. Anesthesiol. Clin. 2021;39:265–284. doi: 10.1016/j.anclin.2021.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lewis M. Intensive care unit rehabilitation within the United Kingdom: Review. Physiotherapy. 2003;89 doi: 10.1016/S0031-9406(05)60179-4. [DOI] [Google Scholar]
- 15.Battaglini D., Robba C., Caiffa S., Ball L., Brunetti I., Loconte M., Giacobbe D.R., Vena A., Patroniti N., Bassetti M., Torres A., Rocco P.R., Pelosi P. Chest physiotherapy: an important adjuvant in critically ill mechanically ventilated patients with COVID-19. Respir. Physiol. Neurobiol. 2020;282:103529. doi: 10.1016/j.resp.2020.103529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fink J.B. Positioning versus postural drainage. Respir. Care. 2002;47:769–777. http://www.ncbi.nlm.nih.gov/pubmed/12088547 [PubMed] [Google Scholar]
- 17.Rossi V., Santambrogio M., Del Monaco C., Retucci M., Tammaro S., Ceruti C., Saderi L., Aliberti S., Privitera E., Grasselli G., Sotgiu G., Blasi F. Safety and feasibility of physiotherapy in ICU-admitted severe COVID-19 patients: an observational study. Monaldi Arch. Chest Dis. 2022 doi: 10.4081/monaldi.2022.2087. [DOI] [PubMed] [Google Scholar]
- 18.Gosselink R., Clerckx B., Robbeets C., Vanhullebusch T., Vanpee G., Segers J. Physiotherapy in the intensive care unit. Netherlands J. Crit. Care. 2011;15:1–10. [Google Scholar]
- 19.Sommers J., Engelbert R.H., Dettling-Ihnenfeldt D., Gosselink R., Spronk P.E., Nollet F., van der Schaaf M. Physiotherapy in the intensive care unit: an evidence-based, expert driven, practical statement and rehabilitation recommendations. Clin. Rehabil. 2015;29:1051–1063. doi: 10.1177/0269215514567156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mcwilliams D., Atkins G., Hodson J., Boyers M., Lea T., Snelson C. Is the manchester mobility score a valid and reliable measure of physical function within the intensive care unit. Intensive Care Med. Exp. 2015;3:A553. doi: 10.1186/2197-425X-3-S1-A553. [DOI] [Google Scholar]
- 21.Grambsch P., Therneau T. Proportional hazards tests and diagnostics based on weighted residuals. Biometrika. 1994;81:515–526. [Google Scholar]
- 22.R Core Team . 2019. R: A Language and Environment for Statistical Computing. [Google Scholar]
- 23.Dipartimento della Protezione Civile-Presidenza del Consiglio dei Ministri, Italian COVID-19 Data, ((n.d.)).
- 24.Netzer G., Liu X., Shanholtz C., Harris A., Verceles A., Iwashyna T.J. Decreased mortality resulting from a multicomponent intervention in a tertiary care medical intensive care unit. Crit. Care Med. 2011;39:284–293. doi: 10.1097/CCM.0b013e3181ffdd2f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stamm T. Head & Face Medicine - a new journal for “intra-interdisciplinary” science. Why? When? Where? Head Face Med. 2005;1:1. doi: 10.1186/1746-160x-1-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vitacca M., Carone M., Clini E.M., Paneroni M., Lazzeri M., Lanza A., Privitera E., Pasqua F., Gigliotti F., Castellana G., Banfi P., Guffanti E., Santus P., Ambrosino N. Joint statement on the role of respiratory rehabilitation in the COVID-19 crisis: the Italian position paper. Respiration. 2020;99:493–499. doi: 10.1159/000508399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Watanabe S., Liu K., Morita Y., Kanaya T., Naito Y., Arakawa R., Suzuki S., Katsukawa H., Lefor A.K., Hasegawa Y., Kotani T. Changes in barriers to implementing early mobilization in the intensive care unit: a single center retrospective cohort study. Nagoya J. Med. Sci. 2021;83:443–464. doi: 10.18999/nagjms.83.3.443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hodgson C.L., Schaller S.J., Nydahl P., Timenetsky K.T., Needham D.M. Ten strategies to optimize early mobilization and rehabilitation in intensive care. Crit. Care. 2021;25:324. doi: 10.1186/s13054-021-03741-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Binda F., Rossi V., Gambazza S., Privitera E., Galazzi A., Marelli F., Santambrogio M., Adamini I., Grasselli G., Laquintana D. Muscle strength and functional outcome after prone positioning in COVID-19 ICU survivors. Intensive Crit. Care Nurs. 2021:103160. doi: 10.1016/j.iccn.2021.103160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schaller S.J., Anstey M., Blobner M., Edrich T., Grabitz S.D., Gradwohl-Matis I., Heim M., Houle T., Kurth T., Latronico N., Lee J., Meyer M.J., Peponis T., Talmor D., Velmahos G.C., Waak K., Walz J.M., Zafonte R., Eikermann M. Early, goal-directed mobilisation in the surgical intensive care unit: a randomised controlled trial. Lancet. 2016;388 doi: 10.1016/S0140-6736(16)31637-3. [DOI] [PubMed] [Google Scholar]
- 31.Chen S., Su C.-L., Wu Y.-T., Wang L.-Y., Wu C.-P., Wu H.-D., Chiang L.-L. Physical training is beneficial to functional status and survival in patients with prolonged mechanical ventilation. J. Formos. Med. Assoc. 2011;110:572–579. doi: 10.1016/j.jfma.2011.07.008. [DOI] [PubMed] [Google Scholar]
- 32.Morris P.E., Goad A., Thompson C., Taylor K., Harry B., Passmore L., Ross A., Anderson L., Baker S., Sanchez M., Penley L., Howard A., Dixon L., Leach S., Small R., Hite R.D., Haponik E. Early intensive care unit mobility therapy in the treatment of acute respiratory failure. Crit. Care Med. 2008;36:2238–2243. doi: 10.1097/CCM.0b013e318180b90e. [DOI] [PubMed] [Google Scholar]
- 33.McWilliams D., Weblin J., Atkins G., Bion J., Williams J., Elliott C., Whitehouse T., Snelson C. Enhancing rehabilitation of mechanically ventilated patients in the intensive care unit: a quality improvement project. J. Crit. Care. 2015;30:13. doi: 10.1016/j.jcrc.2014.09.018. 8. [DOI] [PubMed] [Google Scholar]
- 34.Liu K., Ogura T., Takahashi K., Nakamura M., Ohtake H., Fujiduka K., Abe E., Oosaki H., Miyazaki D., Suzuki H., Nishikimi M., Lefor A.K., Mato T. The safety of a novel early mobilization protocol conducted by ICU physicians: a prospective observational study. J. Intensive Care. 2018;6:10. doi: 10.1186/s40560-018-0281-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schweickert W.D., Pohlman M.C., Pohlman A.S., Nigos C., Pawlik A.J., Esbrook C.L., Spears L., Miller M., Franczyk M., Deprizio D., Schmidt G.A., Bowman A., Barr R., McCallister K.E., Hall J.B., Kress J.P. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet. 2009;373:1874–1882. doi: 10.1016/S0140-6736(09)60658-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Corner E.J., Wood H., Englebretsen C., Thomas A., Grant R.L., Nikoletou D., Soni N. The Chelsea Critical Care Physical Assessment Tool (CPAx): validation of an innovative new tool to measure physical morbidity in the general adult critical care population; an observational proof-of-concept pilot study. Physiotherapy. 2013;99:33–41. doi: 10.1016/j.physio.2012.01.003. [DOI] [PubMed] [Google Scholar]
- 37.Paton M., Lane R., Hodgson C.L. Early mobilization in the intensive care unit to improve long-term recovery. Crit. Care Clin. 2018;34:557–571. doi: 10.1016/j.ccc.2018.06.005. [DOI] [PubMed] [Google Scholar]
- 38.LoMauro A., Aliverti A. Sex and gender in respiratory physiology. Eur. Respir. Rev. 2021;30:210038. doi: 10.1183/16000617.0038-2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gandotra S., Lovato J., Case D., Bakhru R.N., Gibbs K., Berry M., Files D.C., Morris P.E. Physical function trajectories in survivors of acute respiratory failure. Ann. Am. Thorac. Soc. 2019;16:471–477. doi: 10.1513/AnnalsATS.201806-375OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.De Jonghe B., Sharshar T., Lefaucheur J.-P., Authier F.-J., Durand-Zaleski I., Boussarsar M., Cerf C., Renaud E., Mesrati F., Carlet J., Raphaël J.-C., Outin H., Bastuji-Garin S. Groupe de Réflexion et d'Etude des Neuromyopathies en Réanimation, Paresis acquired in the intensive care unit: a prospective multicenter study. JAMA. 2002;288:2859–2867. doi: 10.1001/jama.288.22.2859. [DOI] [PubMed] [Google Scholar]
- 41.De Jonghe B., Bastuji-Garin S., Sharshar T., Outin H., Brochard L. Does ICU-acquired paresis lengthen weaning from mechanical ventilation? Intensive Care Med. 2004;30:1117–1121. doi: 10.1007/s00134-004-2174-z. [DOI] [PubMed] [Google Scholar]
- 42.Stutz M.R., Leonhard A.G., Ward C.M., Pearson S.D., Osorio P.L., Herbst P.R., Wolfe K.S., Pohlman A.S., Hall J.B., Kress J.P., Patel B.K. Early rehabilitation feasibility in a COVID-19 intensive care unit. Chest. 2021:55–57. doi: 10.1016/j.chest.2021.05.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Devlin J.W., O'Neal H.R., Thomas C., Barnes Daly M.A., Stollings J.L., Janz D.R., Ely E.W., Lin J.C. Strategies to optimize ICU liberation (A to F) bundle performance in critically ill adults with coronavirus disease 2019. Crit. Care Explor. 2020;2 doi: 10.1097/CCE.0000000000000139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lee A.J.Y., Chung C.L.H., Young B.E., Ling L.M., Ho B.C.H., Puah S.H., Iqbal S.R., Tan G.P. Clinical course and physiotherapy intervention in 9 patients with COVID-19. Physiotherapy. 2020;109:1–3. doi: 10.1016/j.physio.2020.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Binda F., Galazzi A., Marelli F., Gambazza S., Villa L., Vinci E., Adamini I., Laquintana D. Complications of prone positioning in patients with COVID-19: a cross-sectional study. Intensive Crit. Care Nurs. 2021;67:103088. doi: 10.1016/j.iccn.2021.103088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nydahl P., Sricharoenchai T., Chandra S., Kundt F.S., Huang M., Fischill M., Needham D.M. Safety of patient mobilization and rehabilitation in the intensive care unit. Systematic review with meta-analysis. Ann. Am. Thorac. Soc. 2017;14:766–777. doi: 10.1513/AnnalsATS.201611-843SR. [DOI] [PubMed] [Google Scholar]
- 47.Wu C., Hou D., Du C., Cai Y., Zheng J., Xu J., Chen X., Chen C., Hu X., Zhang Y., Song J., Wang L., Chao Y., Feng Y., Xiong W., Chen D., Zhong M., Hu J., Jiang J., Bai C., Zhou X., Xu J., Song Y., Gong F. Corticosteroid therapy for coronavirus disease 2019-related acute respiratory distress syndrome: a cohort study with propensity score analysis. Crit. Care. 2020;24:643. doi: 10.1186/s13054-020-03340-4. [DOI] [PMC free article] [PubMed] [Google Scholar]