Abstract
The COVID-19 pandemic has led to unprecedented levels of uncertainty for people around the world. Research suggests that internet searching resulting in contradictory information can lead to increased levels of distress, particularly for people who have a high intolerance of uncertainty (IU). In the present correlational study, U.S. undergraduate students (N = 317) indicated their IU, the frequency with which they search for COVID-19 related information online, their overall health anxiety, their fear of COVID-19 (FCV-19), and engagement in prevention behaviors. Consistent with previous research, individual differences in IU moderated the relationship between internet searches and FCV-19 such that for people high in IU, more internet searching was associated with greater fear. In turn, we also found that greater FCV-19 predicted more social-distancing behaviors. These findings are important in both future mental health and public health initiatives.
Keywords: Intolerance of uncertainty, Health anxiety, Fear of COVID-19, Internet searching, Social-distancing
The COVID-19 pandemic has brought unprecedented levels of uncertainty and health anxiety worldwide (Asmundson & Taylor, 2020; Clark, 2020; Rajkumar, 2020). Even with, or perhaps, because of overwhelming access to information, there is uncertainty about mortality rates and contagiousness, vaccinations, additional waves and variants, effectiveness of implemented public health policies, and economic and government stability (Altig et al., 2020; Mohammed et al., 2021; Valika et al., 2020). This unpredictability can influence people differently based on their individual levels of Intolerance of Uncertainty (IU; Carleton, 2016); particularly when people are seeking out more information regarding COVID-19 on the internet (Caiata-Zufferey et al., 2010; Fergus, 2013; Starcevic et al., 2021; Tolin et al., 2003; White & Horvitz, 2009). Research shows that IU moderates the relationship between internet searching behaviors and health anxiety generally (e.g., Fergus, 2013); the goal of the present research was to address the role that individual differences in IU play in the fear of COVID-19 specifically.
1. Intolerance of uncertainty
Intolerance of uncertainty (IU) is the difficulty in handling ambiguous information that is associated with uncertainty (Carleton, 2016). It is thought of as an individual, stable, trait-level or dispositional fear of the unknown (Carleton et al., 2012; Dugas et al., 1997; Fergus, 2013). Research has shown that IU is a transdiagnostic variable, meaning that it is present across a range of psychiatric disorders (Freeston et al., 2020; McEvoy & Mahoney, 2012; Talkovsky & Norton, 2016). Specifically, high levels of IU are correlated with anxiety disorders, including, but not limited to, generalized anxiety disorder (Carleton, Collimore, & Asmundson, 2010; McEvoy & Mahoney, 2012; Talkovsky & Norton, 2016), social anxiety disorder and social phobia (McEvoy & Mahoney, 2012; Talkovsky & Norton, 2016), panic disorder and agoraphobia (McEvoy & Mahoney, 2012; Talkovsky & Norton, 2016) and obsessive-compulsive disorder (Carleton, Collimore, & Asmundson, 2010; McEvoy & Mahoney, 2012; Tolin et al., 2003). IU can also lead to impairments of daily life functioning (Ladouceur et al., 1997). Furthermore, research suggests that targeting IU-related biases are related to a decrease in symptoms across multiple disorders including social anxiety, generalized anxiety, and depression (Dugas & Ladouceur, 2000; Mahoney & McEvoy, 2012; McEvoy & Erceg-Hurn, 2016; van der Heiden et al., 2012). This suggests the importance of addressing IU as a strong predictor of various psychiatric disorders.
Additionally, IU is related to health anxiety (Fergus, 2013), which stems from misinterpretations of perceived bodily sensations as being more unhealthy than they actually are (Asmundson & Taylor, 2020; Jungmann & Witthöft, 2020; Warwick & Salkovskis, 1985). When excessive, health anxiety can lead to adverse behaviors (Asmundson & Taylor, 2020) such as overuse or avoidance of medical services, hoarding medical items, and mistrust in public health officials (Asmundson & Taylor, 2020). IU is also associated with poorer safety learning (Morriss, Bennett, et al., 2021; Morriss, Wake, et al., 2021; Morriss, Zuj, & Mertens, 2021); in other words, under uncertain situations, those with high levels of IU tend to remain consistent in their behavior regardless of new information (Morriss, Zuj, & Mertens, 2021) and may generalize threats to safe conditions by expecting the worst outcome (Morriss, Zuj, & Mertens, 2021). In relation to the COVID-19 pandemic, IU might be a factor in people following safety protocols and mandates, but when these protocols (e.g., wearing masks outside when social distancing is possible) are no longer necessary for public safety, people high in IU may struggle in readjusting their behavior.
One way in which people may try to control their health anxiety is by searching for medical information on the internet (e.g., Fergus, 2013). Internet searching for medical information has become widespread in modern daily life (Starcevic, 2017); WebMD, for example, has 75 million unique visitors to their website each month (WebMD, 2018). Internet searching for health information has become a common checking behavior for those high in IU who desire to reduce distress levels (Caiata-Zufferey et al., 2010; Jungmann & Witthöft, 2020; Tolin et al., 2003). In some cases, internet searches can help reassure people that their symptoms do not amount to life-threatening conditions, and can help reduce any uncertainty that surrounds specific symptoms (Fergus, 2013). A recent meta-analysis (McMullan et al., 2019) found that health anxiety predicts both online health information-seeking and cyberchondria (i.e., excessive searching; Starcevic, 2017). The excessive searching cycle of cyberchondria has the potential to be an unhelpful safety strategy and increase uncertainty, which therefore heightens health anxiety for people with high IU (Bottesi et al., 2021; Fergus, 2013; Jungmann & Witthöft, 2020; Morriss & van Reekum, 2019; Starcevic, 2017; Starcevic et al., 2021; White & Horvitz, 2009). One way in which this happens is that people may come to falsely believe that harmless symptoms actually signal grave medical conditions because they misunderstand medical diagnostic information found online (Fergus, 2013; Jungmann & Witthöft, 2020; White & Horvitz, 2009). During the COVID-19 pandemic, this could be particularly likely considering that COVID-19 symptoms often overlap with that of the common cold or allergies (Jungmann & Witthöft, 2020; Ornell et al., 2020). Furthermore, research has shown that people high in IU have increased sensitivity to information about threats and safety (Morriss & van Reekum, 2019). Due to the fact that IU is associated with a decreased ability to tolerate the absence of information, any threat of uncertainty is noted as aversive, even under situations where safety is high (i.e. information about safety is provided) (Freeston et al., 2020; Morriss, Bell, et al., 2021). Another way in which repeated internet searching can increase uncertainty is when the information found online is inconsistent or conflicting (Asmundson & Taylor, 2020; Starcevic et al., 2021). This can lead to an overload of information that can increase, rather than decrease anxiety for those with high IU (Starcevic et al., 2021).
Since the onset of the COVID-19 pandemic, the information available online about the symptoms and risks has been ever-changing as new data and sources of information become available. As such, examining how internet searching about COVID-19 and IU interact to predict health anxiety and the fear of COVID-19 is of utmost importance. Bottesi et al. (2021) demonstrated that while IU was correlated with health anxiety pre-pandemic or during the initial COVID-19 lockdown, cyberchondria only played a role in this relationship during the COVID-19 lockdown. This provides initial evidence that how people higher in IU use and respond to internet searching during the COVID-19 pandemic may be different than from pre-pandemic life. Furthermore, Freeston et al. (2020) proposed that individual differences in IU between people begin a cycle of experiencing uncertain situations as aversive, engaging in behaviors that reduce uncertainty, and thus, moderating perceptions of threat and uncertainty. This model of uncertainty distress can be applied to COVID-19, and it is predicted that both the actual and perceived threat and uncertainty, along with situation specific IU, will correlate with variances in the psychological impact of COVID-19 (Freeston et al., 2020).
2. Fear of COVID-19
Recently, a new construct known as Fear of COVID-19 (FCV-19; Ahorsu et al., 2020) was introduced, which assesses the individual differences in psychological fear that people face when exposed to thoughts or information about COVID-19. Some research suggests that one source of FCV-19, as with general health anxiety, is getting information about the virus from social media (Lin et al., 2020). People who have more problematic social media use have higher levels of FCV-19, and this may be caused by the amplification of fear when people are exposed to negative COVID-19 information through social media (Lin et al., 2020).
Additionally, there is already evidence that FCV-19 is predictive of both depression and anxiety symptomatology (Ahorsu et al., 2020; Fitzpatrick et al., 2020; Ornell et al., 2020), health anxiety (Akbari et al., 2021), and overall well-being (Bakioğlu et al., 2020). Satici et al. (2020) found that those with high levels of IU during the COVID-19 pandemic also had higher levels of FCV-19; because IU led to more rumination about COVID-19. In a similar study, researchers found that IU mediated the relationship between FCV-19 and health anxiety (Akbari et al., 2021). Taken together, this suggests that FCV-19 can both be an outcome of IU, and lead to IU.
Notably, research has also found a link between FCV-19 and engagement in COVID-19 prevention behaviors such as staying home, mask wearing, social-distancing, and hand-washing (Breakwell et al., 2021; Melki et al., 2020). Thus, while a FCV-19 is associated with worse mental health outcomes, it is also associated with better adherence to preventive behaviors (CDC, 2020).
3. The present research
The goal of the present research is to examine the relationship between individual differences in IU, health anxiety, FCV-19, and frequency of COVID-19 related health information searches. In a correlational, cross-sectional study, we measured the effect of frequency of COVID-19 related health information searches on both health anxiety and FCV-19 and the moderation effect of IU on this relationship. We also measured the mediation effect of FCV-19 on the relationship between frequency of COVID-19 related health information searches and social-distancing behavior with IU as a moderator. Consistent with previous research (Fergus, 2013), we used negative affect (NA) and exposure to COVID-19 as covariates.
We predicted that greater frequency of COVID-19 related internet searching would positively predict health anxiety and FCV-19. Furthermore, we predicted that IU would moderate this relationship, such that people with a higher intolerance of uncertainty would show a stronger relationship between internet searching and these outcomes. Finally, consistent with other research, we predicted that an increased FCV-19 would mediate the relationship between internet searches, IU, and COVID-19 prevention behaviors.
4. Method
4.1. Participants and design
Undergraduates (N = 317) from a mid-sized Western U.S. private university participated in exchange for partial course credit. Recruitment began in Fall 2020 and concluded in Spring 2021 once the COVID-19 vaccine became available to all participants; we made the a priori decision to recruit as many participants as possible during this time. This study obtained IRB approval (20-08-1492) and all participants provided consent for beginning the study. Participants were on average 19.37 years of age (SD = 2.32), and were predominantly women (68.5%). Participants self-identified their race as white (47.5%), Asian (29.7%), Latinx (16.1%), Black (3.8%), Native Hawaiian or Pacific Islander (3.2%), or other races (3.3%). Only 12.3% of participants had been diagnosed with COVID-19, but 85.2% knew someone who had been diagnosed.
4.2. Materials and procedure
First, participants completed the 12-item Intolerance of Uncertainty Scale (Carleton et al., 2007; α = 0.90 in the current sample). Participants indicated whether they respond with distress to uncertain and ambiguous situations (e.g., “Unforeseen events upset me greatly”; 1 = not at all characteristic of me, 5 = entirely characteristic of me). Scores were averaged to create an aggregate in order to account for missing data; higher scores indicate more IU. Next, participants completed a 10-item Negative Affect scale (Watson et al., 1988; α = 0.87 in the current sample) in which they responded to which word descriptors corresponded to how they felt on a five-point scale (e.g. “scared”, “nervous”; 1 = very slightly or not at all, 5 = extremely). Scores were averaged to create an aggregate; higher scores indicate greater negative affect.
Participants then completed the 18-item Short Health Anxiety Inventory (SHAI; Alberts et al., 2011; Salkovskis et al., 2002; α = 0.85 in the current sample). Consistent with previous research (Alberts et al., 2011; Fergus, 2013), only the first 14 items of the 18-item SHAI were used because they directly assess health anxiety (Alberts et al., 2011). Participants responded to statements assessing their health anxiety independent of actual physical health status over the past six months (e.g. “I spend most of my time thinking I have a serious illness”; 0 = I do not, 3 = I spend most of my time). Scores were averaged to create an aggregate; higher scores indicate increased levels of health anxiety.
Then, participants responded to a single item question and indicated how frequently they search for online COVID-19 health information (0 = Never, 6 = Several times a day; adapted from Baumgartner & Hartmann, 2011; Fergus, 2013; Muse et al., 2012). Participants completed the 7-item Fear of COVID-19 Scale (Ahorsu et al., 2020; α = 0.89 in the current sample). Participants indicated their agreement with several items about fears about COVID-19 (e.g. “I am afraid of losing my life because of COVID-19”; 1 = strongly disagree, 5 = strongly agree). Scores were averaged to create an aggregate; higher scores indicate a greater FCV-19. Participants then completed several other measures including a measure of financial anxiety, as well as several exploratory questions, but these analyses will not be reported here.
Finally, participants responded to two different mitigation behaviors. They indicated whether they or someone they know personally had been diagnosed with COVID-19, and indicated whether they practice prevention behaviors such as social-distancing or wearing masks in public (1 = yes, 2 = no). Following this, participants were thanked and debriefed.
5. Results
Descriptive statistics and correlations for the study variables are displayed in Table 1 . As seen in the table, frequency of internet searching is correlated with FCV-19 and health anxiety. Similarly, IU is correlated with FCV-19 and health anxiety. Furthermore, there is a correlation between FCV-19 and social-distancing practices.
Table 1.
Descriptive statistics and zero order correlations.
| Variable | Possible | Mean (SD) | N | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Internet searching frequency | 1–7 | 3.30 (1.30) | 315 | – | |||||||
| 2. Intolerance of Uncertainty Scale | 1–5 | 2.84 (0.78) | 316 | 0.10 | – | ||||||
| 3. Short Health Anxiety Inventory | 1–4 | 2.04 (0.48) | 314 | 0.31⁎⁎ | 0.28⁎⁎ | – | |||||
| 4. Fear of COVID-19 Scale | 1–5 | 2.40 (0.95) | 315 | 0.40⁎⁎ | 0.31⁎⁎ | 0.54⁎⁎ | – | ||||
| 5. Social Distancing Practices | 1–2 | 1.10 (0.31) | 315 | −0.05 | 0.01 | −0.01 | −0.15⁎⁎ | – | |||
| 6. Mask Wearing Practices | 1–2 | 1.00 (0.06) | 315 | −0.06 | 0.08 | −0.04 | −0.08 | 0.17⁎⁎ | – | ||
| 7. Negative Affect (NA) | 1–5 | 2.79 (0.77) | 315 | 0.15⁎⁎ | 0.44⁎⁎ | 0.47⁎⁎ | 0.43⁎⁎ | 0.02 | −0.10 | – | |
| 8. COVID-19 myself diagnosed | 1–2 | 1.88 (0.33) | 316 | −0.01 | 0.07 | 0.06 | 0.10 | −0.12⁎ | 0.02 | 0.02 | – |
| 9. COVID-19 personally know diagnosed | 1–2 | 1.14 (0.35) | 315 | −0.09 | 0.10 | −0.06 | 0.07 | −0.05 | 0.14⁎ | 0.01 | 0.13⁎ |
All r values significant at p < .01 (2-tailed).
All r values significant at p < .05 (2-tailed).
5.1. Primary analyses
We conducted a series of centered-regression analyses using the PROCESS macro for SPSS, Model 1 (Hayes, 2017) to test the moderation effects with 5000 bootstrap samples. The predictor variable (x) was internet searches, the outcome variables (y) were SHAI and FCV-19 and the moderating variable (w) was IU.1
5.1.1. Short health anxiety inventory
The overall model was significant for the Short Health Anxiety Inventory, R 2 = 0.16, F(3,310) = 19.34, p < .001. There was a significant main effect of frequency of internet searches for COVID-19 health information on SHAI (β = 0.10, SE = 0.02, t = 5.34, p < .001, 95% CI = [0.06, 0.14]) such that more searching predicted greater health anxiety. There was also a significant main effect of IU on SHAI (β = 0.16, SE = 0.03, t = 4.83, p < .001, 95% CI = [0.09, 0.22]) such that greater IU predicted greater health anxiety. The frequency of internet searches for COVID-19 health information x IU interaction was not significant (β = 0.00, SE = 0.02, t = 0.17, p = .86, 95% CI = [−0.44, 0.52]).
5.1.2. Fear of COVID-19 Scale
The overall model was significant for the Fear of COVID-19 Scale, R 2 = 0.50, F(3, 310) = 34.20, p < .001. There was a significant main effect of frequency of internet searches for COVID-19 health information on FCV-19 (β = 0.27, SE = 0.04, t = 7.52, p < .001, 95% CI = [0.20, 0.34]). There was also a significant main effect of IU on FCV-19, (β = 0.33, SE = 0.06, t = 5.46, p < .001, 95% CI = [0.21, 0.45]). Additionally, as predicted, the frequency of internet searches for COVID-19 health information x IU interaction was significant (β = 0.10, SE = 0.05, t = 2.28, p = .02, 95% CI = [0.01, 0.19]). See Fig. 1 . Simple slopes analysis revealed that for participants high in IU, a higher frequency of internet searches for COVID-19 health information was strongly associated with a greater fear of COVID-19 (β = 0.35, SE = 0.05, t = 6.86, p < .001, 95% CI = [0.25, 0.45]). For participants low in IU, a greater frequency of internet searches for COVID-19 health information was also associated with greater fear of COVID-19 (β = 0.18, SE = 0.05, t = 3.45, p < .001, 95% CI = [0.08, 0.28]). In other words, higher frequency of internet searches is associated with higher fear for everyone; but the magnitude of the effect is greater for people higher in IU.
Fig. 1.
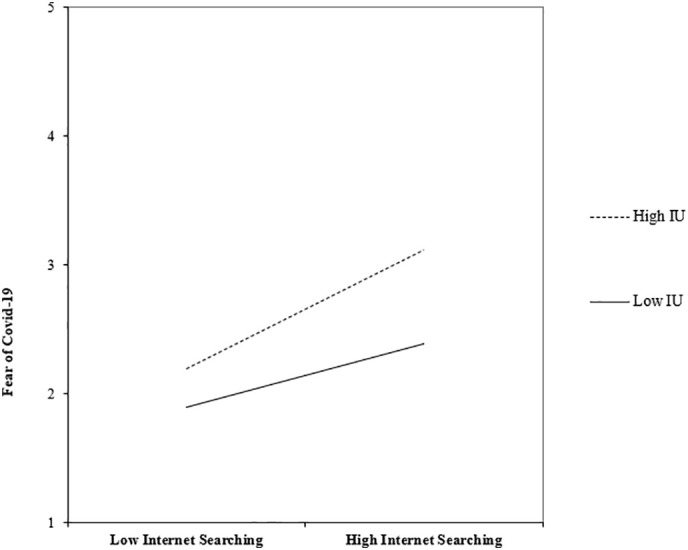
Moderating effect of intolerance of uncertainty (IU = Intolerance of Uncertainty Scale-12-item version) on the relation between frequency of Internet searches for COVID-19 health information and fear of COVID-19 (FCV-19S = Fear of COVID-19 Scale).
**Note: Please position this caption under the figure so it is consistent with the formatting of Fig. 2.
5.1.3. Moderated mediation
To test whether FCV-19 mediated the relationship between the above described interaction and COVID-19 prevention behaviors, we used PROCESS (Hayes, 2017) model 8 to run a moderated mediation in SPSS. The predictor variable (x) was frequency of internet searches, the outcome variable (y) was social-distancing,2 the moderating variable (w) was IU, and the mediating variable (M) was FCV-19. See Fig. 2 . Moderated mediation would be determined if IU moderated the link between frequency of internet searching and either FCV-19 or social-distancing.
Fig. 2.
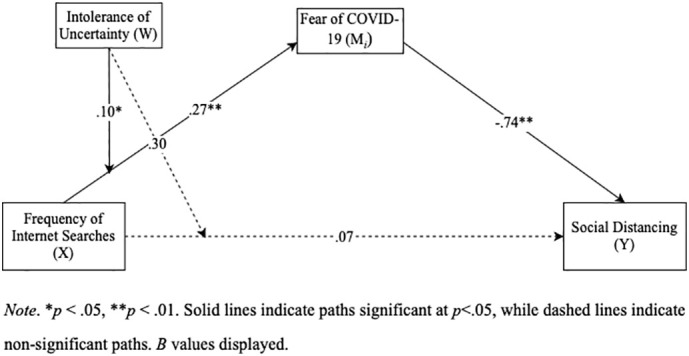
Moderated Mediation Model: Social Distancing (IV), Fear of COVID-19 (Mediator), Frequency of Internet Searches (DV), Intolerance of Uncertainty (Moderator)
Note. *p < .05, **p < .01. Solid lines indicate paths significant at p < .05, while dashed lines indicate non-significant paths. B values displayed.
The index of moderated mediation was significant (0.08, SE = 0.05, 95% CI = [0.01, 0.19]). As described above, there was a significant effect of frequency of internet searches for COVID-19 health information on levels of fear of COVID-19 and, the interaction between frequency of internet searches for COVID-19 health information and IU was significant. Furthermore, Fear of COVID-19 significantly predicted social-distancing (b path), β = 0.74, SE = 0.26, Z = 2.79, p < .001.
The conditional direct effect of frequency of internet searching for COVID-19 health information on social-distancing behavior was not significant (c path), β = −0.07, SE = 0.15, Z = −0.49, p = .62, 95% CI = [−0.37, 0.22]. Furthermore, IU did not moderate the effect of frequency of internet searches for COVID-19 health information and social-distancing behavior, β = −0.02, SE = 0.17, Z = −0.11, p = .91. The conditional indirect effect was greater in people with high IU (0.26, SE = 0.11, 95% CI = [0.07, 0.52]) and weaker in people with low IU (0.13, SE = 0.06, 95% CI = [0.04, 0.28]). In other words, people with high levels of IU that engage in more internet searching about COVID-19 are more likely to have increased FCV-19, and therefore engage in more social-distancing behavior.
6. Discussion
The results of this study suggest that individual differences in intolerance of uncertainty is an important factor to consider when examining people's fear of COVID-19. Consistent with previous research, our data suggest that on its own, greater IU predicted more health anxiety, a greater FCV-19, and more social-distancing behaviors. As predicted, IU also moderated the relationship between searching for COVID-19 related information on the internet and FCV-19. That is, frequent internet searches about COVID-19 led to greater FCV-19, especially for people higher in IU. Notably, IU did not moderate the relationship between internet searching about COVID-19 and general health anxiety. Furthermore, these findings were consistent when controlling for NA and direct or second hand experience with COVID-19, which illustrates the impact of IU specifically. This strengthens the study as these results cannot be contributed to other confounding variables.
Interestingly, we also found that FCV-19 mediated the relationship between frequency of internet searches for COVID-19 health information and IU, and social-distancing. That is, the increased FCV-19 that was predicted by frequent internet searching and higher IU, in turn predicted more social-distancing behaviors. While variables like IU and FCV-19 are normally associated with negative mental health outcomes (Carleton, Collimore, & Asmundson, 2010; Fitzpatrick et al., 2020; Ornell et al., 2020; Tolin et al., 2003), this study provides evidence that they might be beneficial for public health during the COVID-19 pandemic. Our data suggests that people with higher levels of IU and FCV-19 are more likely to engage in social-distancing behaviors, which may help slow the transmission of COVID-19. Future research should test how to achieve improvements in public health initiatives through these variables, but with close attention to mental health outcomes.
While IU is not generally targeted in anxiety interventions (Freeston et al., 2020), research has shown methods that are effective in reducing IU, and therefore anxiety in general (Fergus, 2013). For example, in looking at cognitive strategies, clinicians can teach clients that definite explanations are not always possible, thus increasing their tolerance for uncertainty (Abramowitz & Braddock, 2008). Behavioral strategies could also be used by clinicians to increase a client's tolerance for uncertainty, such as exposure to an uncertain situation without the means to engage in checking behaviors (Einstein, 2014; Knowles & Olatunji, 2019; Morriss et al., 2020; Tolin et al., 2003). Exercises like this could help clients familiarize themselves with the anxiety of uncertain situations and help increase future tolerance of situations which they cannot control (Einstein, 2014; Knowles & Olatunji, 2019; Morriss et al., 2020; Tolin et al., 2003). Clinicians can also use models of uncertainty distress in order to understand the interactions among threat, uncertainty, and distress reactions in relation to real world situations, like COVID-19 (Freeston et al., 2020).
In applying this to our research, people who have high levels of IU should be cognizant of the amount of information they are exposed to regarding COVID-19. For example, people high in IU could set aside a specific amount of time per day that they allow themselves to search COVID-19 related health information. It is important to stay up to date with public health mandates, but not become inundated and obsessed with the information available on the internet. Furthermore, individuals should fact check the information they are being exposed to as misinformation and misunderstanding is associated with psychological distress (Lin et al., 2020). Public health officials should create campaigns that promote COVID-19 awareness, but not initiate fear of COVID-19 for individuals.
6.1. Limitations
The findings of the present study should be considered with various limitations. First, our sample was undergraduate students in the Western U.S. This constricted age range is particularly important for COVID-19, as age is considered one of the biggest risk factors of the disease (CDC, 2020). With greater demographic variability, including individuals from outside of the U.S., this research could have broader implications for the public. For example, our undergraduate pool of students was predominately white. National data shows that Black and Latinx people are more affected by COVID-19 in the U.S.; they are almost three times more likely than whites to be hospitalized and twice as likely to die from COVID-19 (CDC, 2021). Additionally, research has shown that non-Hispanic Black adults have had an increase in experiences of anxiety or depression disorders in relation to the pandemic (Fitzpatrick et al., 2020; Panchal et al., 2021). With a broader demographic sample, this could be looked at more closely. Furthermore, since the onset of the pandemic, young adults (18–24) have had an increase in symptoms of anxiety, depression, substance abuse, and suicidal thoughts (Panchal et al., 2021). Since our population was undergraduate students within this age range, our results might have been more extreme than results with a greater age range. Finally, the majority of our sample were women who in previous research, have been shown to have higher levels of anxiety in general compared to men (Bahrami & Yousefi, 2011; Craske, 2003); this could have affected our results. Researchers should take into account these demographic limitations when conducting future research. Additionally, our sample came from a university in a U.S. state with incredibly strict COVID-19 policies relative to other U.S. states, regarding things like masking in indoor public spaces. This limited our ability to test whether variables like IU or FCV-19 actually influence these behaviors. Moreover, preventative measure variables (social-distancing and mask wearing) were measured on a binary scale, with response options as either yes or no. This limited the nuance of possibilities from participants. For example, it may be possible that some participants wear masks, but only when required. Similarly, specifically with the undergraduate student population, participants may only practice social distancing when in classrooms, but not when off campus. Therefore, the response options constrict the variety of possible responses. Future research should include more items with likelihood scales (versus just “yes, no” responses), as well as ask additional questions related to preventative behaviors relating to frequency, duration, and environment to increase the reliability of these findings. Finally, it is important to note that this study is limited due to its correlational design. One alternative hypothesis is that perhaps FCV-19 actually causes more checking behaviors and information seeking (and not the other way around). Similarly to how information seeking is used as a coping mechanism, but can also contribute to greater IU (Fergus, 2013; Jungmann & Witthöft, 2020; Starcevic, 2017; Tolin et al., 2003; White & Horvitz, 2009). Future research should include a longitudinal study to establish temporal precedence, or an experimental study in which people are given more or less information about a new strain to mimic online searching before measuring FCV-19 as an outcome.
6.2. Conclusion
The COVID-19 pandemic for many people has led to an increase in adverse mental health disorders, substance use, and suicidal ideation (Czeisler et al., 2020). With so much unknown surrounding the pandemic, individual differences in IU are important to address so that clinicians can better understand mental health outcomes. Furthermore, this research is important for public health as it sheds light on the relationship between individual differences in IU, frequency of internet searches for COVID-19 health information, FCV-19 and social-distancing behavior. While there are negative mental health outcomes associated with high levels of IU and FCV-19, there may be positive public health outcomes that could be used in public health initiatives addressing the transmission of COVID-19.
Declaration of competing interest
The authors have no conflict of interest to report.
Acknowledgements
This work was funded by the Santa Clara University Real Experience Applied Learning (REAL) Award.
Footnotes
All analyses were also run with NA and direct or second hand experience with COVID-19 as covariates; the pattern of results held true so the results are reported without covariates; see Supplementary Materials for full analyses including these covariates.
We had initially planned to aggregate social-distancing with mask wearing, however, 99% of our sample reported engaging in mask wearing, likely because of strict local masking laws, so the two variables were not strongly related (r = 0.11).
Supplementary data to this article can be found online at https://doi.org/10.1016/j.actpsy.2022.103534.
Appendix A. Supplementary data
Analyses including covariates.
References
- Abramowitz J.S., Braddock A.E. Hogrefe & Huber; Cambridge, MA: 2008. Psychological treatments of health anxiety and hypochondriasis: A biopsychosocial approach. [Google Scholar]
- Ahorsu D.K., Lin C.Y., Imani V., Saffari M., Griffiths M.D., Pakpour A.H. The fear of COVID-19 scale: Development and initial validation. International Journal of Mental Health and Addiction. 2020 doi: 10.1007/s11469-020-00270-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akbari M., Spada M.M., Nikčević A.V., Zamani E. The relationship between fear of COVID-19 and health anxiety among families with COVID-19 infected: The mediating role of metacognitions, intolerance of uncertainty, and emotion regulation. Clinical Psychology & Psychotherapy. 2021;28(6):1354–1366. doi: 10.1002/cpp.2628. [DOI] [PubMed] [Google Scholar]
- Alberts N.M., Sharpe D.S., Kehler M.D., et al. Health anxiety: Comparison of the latent structure in medical and non-medical samples. Journal of Anxiety Disorders. 2011;25:612–614. doi: 10.1016/j.janxdis.2011.01.011. [DOI] [PubMed] [Google Scholar]
- Altig D., Baker S.R., Barrero J.M., Bloom N., Bunn P., Chen S., Mizen P. National Bureau of Economic Research; 2020. Economic uncertainty before and during the COVID-19 pandemic (no. w27418) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asmundson G.J., Taylor S. How health anxiety influences responses to viral outbreaks like COVID-19: What all decision-makers, health authorities, and health care professionals need to know. Journal of Anxiety Disorders. 2020;71 doi: 10.1016/j.janxdis.2020.102211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bahrami F., Yousefi N. Females are more anxious than males: A metacognitive perspective. Iranian Journal of Psychiatry and Behavioral Sciences. 2011;5(2):83. [PMC free article] [PubMed] [Google Scholar]
- Bakioğlu F., Korkmaz O., Ercan H. Fear of COVID-19 and positivity: Mediating role of intolerance of uncertainty, depression, anxiety, and stress. International Journal of Mental Health and Addiction. 2020:1–14. doi: 10.1007/s11469-020-00331-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumgartner S.E., Hartmann T. The role of health anxiety in online health information search. CyberPsychology, Behavior, & Social Networking. 2011;14:613–618. doi: 10.1089/cyber.2010.0425. [DOI] [PubMed] [Google Scholar]
- Bottesi G., Marino C., Vieno A., Ghisi M., Spada M.M. Psychological distress in the context of the COVID-19 pandemic: The joint contribution of intolerance of uncertainty and cyberchondria. Psychology & Health. 2021:1–18. doi: 10.1080/08870446.2021.1952584. [DOI] [PubMed] [Google Scholar]
- Breakwell G.M., Fino E., Jaspal R. The COVID-19 preventive behaviors index: Development and validation in two samples from the United Kingdom. Evaluation & the Health Professions. 2021;44(1):77–86. doi: 10.1177/0163278720983416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caiata-Zufferey M., Abraham A., Sommerhalder K., et al. Online health information seeking in the context of the medical consultation in Switzerland. Qualitative Health Research. 2010;20:1050–1061. doi: 10.1177/1049732310368404. [DOI] [PubMed] [Google Scholar]
- Carleton R.N. Into the unknown: A review and synthesis of contemporary models involving uncertainty. Journal of Anxiety Disorders. 2016;39:30–43. doi: 10.1016/j.janxdis.2016.02.007. [DOI] [PubMed] [Google Scholar]
- Carleton R.N., Collimore K.C., Asmundson G.J. “It’s not just the judgements—It’s that I don’t know”: Intolerance of uncertainty as a predictor of social anxiety. Journal of Anxiety Disorders. 2010;24(2):189–195. doi: 10.1016/j.janxdis.2009.10.007. [DOI] [PubMed] [Google Scholar]
- Carleton R.N., Mulvogue M.K., Thibodeau M.A., McCabeb R.E., Antony M.M., Asmundsona G.J. Increasingly certain about uncertainty: Intolerance of uncertainty across anxiety and depression. Journal of Anxiety Disorders. 2012;26(3):468–479. doi: 10.1016/j.janxdis.2012.01.011. [DOI] [PubMed] [Google Scholar]
- Carleton R.N., Norton P.J., Asmundson G.J.G. Fearing the un-known: A short version of the intolerance of uncertainty scale. Journal of Anxiety Disorders. 2007;21:105–117. doi: 10.1016/j.janxdis.2006.03.014. [DOI] [PubMed] [Google Scholar]
- Clark D. Living with uncertainty during COVID-19. Psychology Today. 2020. https://www.psychologytoday.com/us/blog/the-runaway-mind/202003/living-uncertainty-during-covid-19
- <collab>Risk for COVID-19 Infection H., and Death By Race/Ethnicity</collab> Centers for Disease Control and Prevention (CDC) 2021. https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html
- <collab>WebMD facts SHEET m.s., and audience information</collab> WebMD. 2018. https://www.webmd.com/corporate/press-center-fact-sheet#1
- COVID-19 Overview and Infection Prevention and Control Priorities in non-US Healthcare Settings Centers for Disease Control and Prevention (CDC) 2020. https://www.cdc.gov/coronavirus
- Craske M.G. Elsevier; 2003. Origins of phobias and anxiety disorders: Why more women than men? [Google Scholar]
- Czeisler M.É., Lane R.I., Petrosky E., Wiley J.F., Christensen A., Njai R., Rajaratnam S.M. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic—United States, June 24–30, 2020. Morbidity and Mortality Weekly Report. 2020;69(32):1049. doi: 10.15585/mmwr.mm6932a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dugas M.J., Freeston M.H., Ladouceur R. Intolerance of uncertainty and problem orientation in worry. Cognitive Therapy and Research. 1997;21(6):593–606. [Google Scholar]
- Dugas M.J., Ladouceur R. Treatment of GAD: Targeting intolerance of uncertainty in two types of worry. Behavior Modification. 2000;24(5):635–657. doi: 10.1177/0145445500245002. [DOI] [PubMed] [Google Scholar]
- Einstein D.A. Extension of the transdiagnostic model to focus on intolerance of uncertainty: A review of the literature and implications for treatment. Clinical Psychology: Science and Practice. 2014;21(3):280. doi: 10.1111/cpsp.12077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fergus T.A. Cyberchondria and intolerance of uncertainty: Examining when individuals experience health anxiety in response to internet searches for medical information. Cyberpsychology, Behavior, and Social Networking. 2013;16(10):735–739. doi: 10.1089/cyber.2012.0671. [DOI] [PubMed] [Google Scholar]
- Fitzpatrick K.M., Harris C., Drawve G. Fear of COVID-19 and the mental health consequences in America. Psychological trauma: theory, research, practice, and policy. 2020;12(S1):S17–S21. doi: 10.1037/tra0000924. [DOI] [PubMed] [Google Scholar]
- Freeston M., Tiplady A., Mawn L., Bottesi G., Thwaites S. Towards a model of uncertainty distress in the context of coronavirus (COVID-19) Cognitive behaviour therapist. 2020;13 doi: 10.1017/S1754470X2000029X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes A.F. 2nd ed. Guilford Press; NY, NY: 2017. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. [Google Scholar]
- Jungmann S.M., Witthöft M. Health anxiety, cyberchondria, and coping in the current COVID-19 pandemic: Which factors are related to coronavirus anxiety? Journal of Anxiety Disorders. 2020;73 doi: 10.1016/j.janxdis.2020.102239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knowles K.A., Olatunji B.O. Enhancing inhibitory learning: The utility of variability in exposure. Cognitive and Behavioral Practice. 2019;26(1):186–200. doi: 10.1016/j.cbpra.2017.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ladouceur R., Talbot F., Dugas M.J. Behavioral expressions of intolerance of uncertainty in worry: Experimental findings. Behavior Modification. 1997;21(3):355–371. doi: 10.1177/01454455970213006. [DOI] [PubMed] [Google Scholar]
- Lin C.Y., Broström A., Griffiths M.D., Pakpour A.H. Investigating mediated effects of fear of COVID-19 and COVID-19 misunderstanding in the association between problematic social media use, psychological distress, and insomnia. Internet Interventions. 2020;21 doi: 10.1016/j.invent.2020.100345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahoney A.E., McEvoy P.M. Changes in intolerance of uncertainty during cognitive behavior group therapy for social phobia. Journal of Behavior Therapy and Experimental Psychiatry. 2012;43(2):849–854. doi: 10.1016/j.jbtep.2011.12.004. [DOI] [PubMed] [Google Scholar]
- McEvoy P.M., Erceg-Hurn D.M. The search for universal transdiagnostic and trans-therapy change processes: Evidence for intolerance of uncertainty. Journal of Anxiety Disorders. 2016;41:96–107. doi: 10.1016/j.janxdis.2016.02.002. [DOI] [PubMed] [Google Scholar]
- McEvoy P.M., Mahoney A.E. To be sure, to be sure: Intolerance of uncertainty mediates symptoms of various anxiety disorders and depression. Behavior Therapy. 2012;43(3):533–545. doi: 10.1016/j.beth.2011.02.007. [DOI] [PubMed] [Google Scholar]
- McMullan R.D., Berle D., Arnáez S., Starcevic V. The relationships between health anxiety, online health information seeking, and cyberchondria: Systematic review and meta-analysis. Journal of Affective Disorders. 2019;245:270–278. doi: 10.1016/j.jad.2018.11.037. [DOI] [PubMed] [Google Scholar]
- Melki J., Tamim H., Hadid D., Farhat S., Makki M., Ghandour L., Hitti E. Media exposure and health behavior during pandemics: The mediating effect of perceived knowledge and fear on compliance with COVID-19 prevention measures. Health Communication. 2020:1–11. doi: 10.1080/10410236.2020.1858564. [DOI] [PubMed] [Google Scholar]
- Mohammed M., Sha'aban A., Jatau A.I., Yunusa I., Isa A.M., Wada A.S., Obamiro K., Zainal H., Ibrahim B. Assessment of COVID-19 Information Overload Among the General Public. Journal of Racial and Ethnic Health Disparities. 2021:1–9. doi: 10.1007/s40615-020-00942-0. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morriss J., Bell T., Biagi N., Johnstone T., Van Reekum C.M. Intolerance of uncertainty is associated with heightened responding in the prefrontal cortex during cue-signalled uncertainty of threat. Cognitive, Affective, & Behavioral Neuroscience. 2021:1–11. doi: 10.3758/s13415-021-00932-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morriss J., Bennett K.P., Larson C.L. I told you it was safe: Associations between intolerance of uncertainty and different parameters of uncertainty during instructed threat of shock. Journal of Behavior Therapy and Experimental Psychiatry. 2021;70 doi: 10.1016/j.jbtep.2020.101620. [DOI] [PubMed] [Google Scholar]
- Morriss J., van Reekum C.M. I feel safe when I know: Contingency instruction promotes threat extinction in high intolerance of uncertainty individuals. Behaviour Research and Therapy. 2019;116:111–118. doi: 10.1016/j.brat.2019.03.004. [DOI] [PubMed] [Google Scholar]
- Morriss J., Wake S., Elizabeth C., van Reekum C.M. I doubt it is safe: A meta-analysis of self-reported intolerance of uncertainty and threat extinction training. Biological Psychiatry Global Open Science. 2021;1(3):171–179. doi: 10.1016/j.bpsgos.2021.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morriss J., Wake S., Lindner M., McSorley E., Dodd H. How many times do I need to see to believe? The impact of intolerance of uncertainty and exposure experience on safety-learning and retention in young adults. International Journal of Psychophysiology. 2020;153:8–17. doi: 10.1016/j.ijpsycho.2020.04.012. [DOI] [PubMed] [Google Scholar]
- Morriss J., Zuj D.V., Mertens G. The role of intolerance of uncertainty in classical threat conditioning: Recent developments and directions for future research. International Journal of Psychophysiology. 2021;166:116–126. doi: 10.1016/j.ijpsycho.2021.05.011. [DOI] [PubMed] [Google Scholar]
- Muse K., McManus F., Leung C., et al. Cyberchondrias: Factor or fiction? A preliminary examination of the relationship between health anxiety and searching for health information on the internet. Journal of Anxiety Disorders. 2012;26:189–196. doi: 10.1016/j.janxdis.2011.11.005. [DOI] [PubMed] [Google Scholar]
- Ornell F., Schuch J.B., Sordi A.O., Kessler F.H.P. “Pandemic fear” and COVID-19: Mental health burden and strategies. Brazilian Journal of Psychiatry. 2020;42(3):232–235. doi: 10.1590/1516-4446-2020-0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panchal N., Kamal R., Cox C., Garfield R. The implications of Covid-19 for mental health and substance use. KFF. 2021. https://www.kff.org/coronavirus-covid-19/issue-brief/the-implications-of-covid-19-for-mental-health-and-substance-use/ Retrieved September 11, 2021, from.
- Rajkumar R.P. COVID-19 and mental health: A review of the existing literature. Asian Journal of Psychiatry. 2020;102066 doi: 10.1016/j.ajp.2020.102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salkovskis P.M., Rimes K.A., Warwick H.M., et al. The health anxiety inventory: Development and validation of scales for the measurement of health anxiety and hypochondriasis. Psychological Medicine. 2002;32:843–853. doi: 10.1017/s0033291702005822. [DOI] [PubMed] [Google Scholar]
- Satici B., Saricali M., Satici S.A., Griffiths M.D. Intolerance of uncertainty and mental wellbeing: Serial mediation by rumination and fear of COVID-19. International Journal of Mental Health and Addiction. 2020;Advance Online Publication:1–12. doi: 10.1007/s11469-020-00305-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starcevic V. Cyberchondria: Challenges of problematic online searches for health-related information. Psychotherapy and Psychosomatics. 2017;86(3):129–133. doi: 10.1159/000465525. [DOI] [PubMed] [Google Scholar]
- Starcevic V., Schimmenti A., Billieux J., Berle D. Cyberchondria in the time of the COVID-19 pandemic. Human Behavior and Emerging Technologies. 2021;3(1):53–62. doi: 10.1002/hbe2.233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talkovsky A.M., Norton P.J. Intolerance of uncertainty and transdiagnostic group cognitive behavioral therapy for anxiety. Journal of Anxiety Disorders. 2016;41:108–114. doi: 10.1016/j.janxdis.2016.05.002. [DOI] [PubMed] [Google Scholar]
- Tolin D.F., Abramowitz J.S., Brigidi B.D., et al. Intolerance of uncertainty in obsessive-compulsive disorder. Journal of Anxiety Disorders. 2003;17:233–242. doi: 10.1016/s0887-6185(02)00182-2. [DOI] [PubMed] [Google Scholar]
- Valika T.S., Maurrasse S.E., Reichert L. A second pandemic? Perspective on information overload in the COVID-19 era. Otolaryngology-Head and Neck Surgery. 2020;163(5):931–933. doi: 10.1177/0194599820935850. [DOI] [PubMed] [Google Scholar]
- van der Heiden C., Muris P., van der Molen H.T. Randomized controlled trial on the effectiveness of metacognitive therapy and intolerance-of-uncertainty therapy for generalized anxiety disorder. Behaviour Research and Therapy. 2012;50(2):100–109. doi: 10.1016/j.brat.2011.12.005. [DOI] [PubMed] [Google Scholar]
- Warwick H.M., Salkovskis P.M. Hypochondriasis: An acceptable diagnosis- reassurance. British Medical Journal (Clinical Research Education) 1985;290(6474):1028. doi: 10.1136/bmj.290.6474.1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D., Clark L.A., Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality & Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- White R.W., Horvitz E. Cyberchondria: Studies of the escalation of medical concerns in web search. ACM Transactions on Information Systems (TOIS) 2009;27(4):1–37. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Analyses including covariates.


