Abstract
Aims
To test the effectiveness of an intervention, Al-Anon Intensive Referral (AIR), to facilitate participation in Al-Anon Family Groups (Al-Anon).
Design
Multi-site, randomized controlled trial of AIR versus Usual Care (UC) with follow-up assessments at 3, 6, and 12 months. The 12-month follow-up rate was 74%.
Setting
Residential alcohol use disorder (AUD) treatment programs in three US locations.
Participants
Concerned Others (COs) of patients in treatment for AUD. COs were mostly women (77%) who were patients’ spouses (33%) or parents (25%).
Intervention and Comparator
AIR (n=128) consisted of four sessions over 3 months with an Al-Anon Coach. UC (n=151) was the treatment program’s offer of educational sessions for COs.
Measurements
Primary outcome: COs’ self-reports of any Al-Anon attendance (yes or no) at 3 months. Secondary outcomes: number of Al-Anon meetings and the CO-patient relationship (stressors, resources). Potential predictors of outcomes examined in generalized linear mixed models were their baseline value, time, CO-patient relationship type (marital or non-marital), treatment program, and condition.
Findings
There was no effect of condition for the primary outcome (28% in AIR, 21% in UC; Bayes Factor 1.86). Relationship stressors at follow-ups were more severe for COs in a marital relationship with the patient than for COs in a non-marital relationship; Beta (B) (95% confidence interval (CI)): 2.19 (1.07, 3.32). For CO-patient relationship resources at follow-ups, the main effect for condition was significant; B (95% CI): 1.33 (0.04, 2.61). COs assigned to the AIR condition had more resources than COs who were in the UC condition.
Conclusions
Relative to usual care, Al-Anon Intensive Referral was not associated with increases in participation of Concerned Others (COs) in Al-Anon, but was associated with more resources in the CO-patient relationship.
Keywords: Alcohol, Concerned Other, Al-Anon, intensive referral, relationship stressors, relationship resources, treatment
INTRODUCTION
One in five US adults reports having experienced harms in the previous year because of someone else's drinking [1]. Such harms involve social, mental health, and medical difficulties [2-4]. The Al-Anon Family Groups program (known simply as “Al-Anon”) helps Concerned Others (COs, that is, friends and family members concerned about another’s drinking) who may be experiencing such harms. The purpose of this study was to conduct a randomized controlled trial (RCT) of Al-Anon Intensive Referral (AIR) to facilitate COs’ participation in Al-Anon.
Potential benefits of Al-Anon participation
Al-Anon, begun in the 1950s, is a fellowship of family and friends of people with alcohol problems who join together to solve the common difficulties involved in being a CO [5,6]. Al-Anon uses the 12 Steps of Alcoholics Anonymous (AA). A main source of information about Al-Anon is their triennial cross-sectional membership survey; the most recent was in 2018 (n=13,395 Al-Anon members, 51% had at least 10 years of membership). Members reported, on average, an 88% improvement in their mental health, and an 83% improvement in their daily life, from before they began attending Al-Anon meetings to the time of the survey [7].
Empirical studies of Al-Anon, conducted mainly in the 1980s and 1990s, support these findings. Al-Anon members reported improvements in understanding alcohol use disorders (AUDs), as well as in their depression, assertiveness, self-acceptance, and relationships [8]. In RCTs involving people with AUDs who resisted treatment, COs who were referred to therapy based on Al-Anon concepts or to Al-Anon reported reduced personal problems and emotional distress (depression, anxiety, and anger), and increased self-esteem, coping behaviors, and relationship happiness, in comparison to wait-list controls [9-13]. Subsequent to these studies, a 6-month follow-up of people who were newcomers to Al-Anon at baseline found that both sustained attendees and those who terminated attendance reported gains from Al-Anon. However, sustained attendees were more likely than people who discontinued to report benefits in a number of domains, including learning how to handle problems due to their loved one with alcohol problems, general well-being, functioning, and mental health symptoms [14]. Similarly, a study conducted in Iran found that Al-Anon members attending for at least six months’ duration, compared to Al-Anon newcomers, reported better quality of life, fewer role limitations, and improved social functioning [15].
Present study
The present study used a randomized design in which COs of patients newly admitted to residential treatment for AUDs were assigned to usual care (UC) or AIR. AIR procedures were adapted from previous Intensive Referral procedures to facilitate AA attendance [16-19] and addressed previously identified barriers to Al-Anon engagement, including lack of initial referral by health care professionals, and misconceptions about Al-Anon [5,14]. AIR consisted of four sessions with an “Al-Anon Coach.” COs were followed at 3, 6, and 12 months post-baseline. The primary outcome was Al-Anon meeting attendance at 3-month follow-up (yes/no). Although studies have not established patterns of Al-Anon meeting attendance that are linked to benefits over time, they have shown that more immediate Al-Anon attendance is helpful even in the short-term [14,33]. Further, even when Al-Anon participation is less intensive (e.g., infrequent attendance), participation may be beneficial and encourage former attendees to return to Al-Anon later when participation may become sustained [14, 33]. Secondary outcomes were the number of Al-Anon meetings attended and the CO-patient relationship’s stressors and resources. We included the secondary outcomes to determine if AIR alone had benefits relative to UC. That is, receiving AIR may have prompted COs to newly consider their relationship with their patient, independent of any Al-Anon participation [20,21]. The hypothesis was that, compared to COs assigned to UC, COs assigned to AIR would have more Al-Anon attendance and better relationships with their patients.
METHODS
Sample and procedure
The sample was 279 COs of patients in treatment for AUDs (Figure 1). All study procedures were Institutional Review Board compliant.
Figure 1.
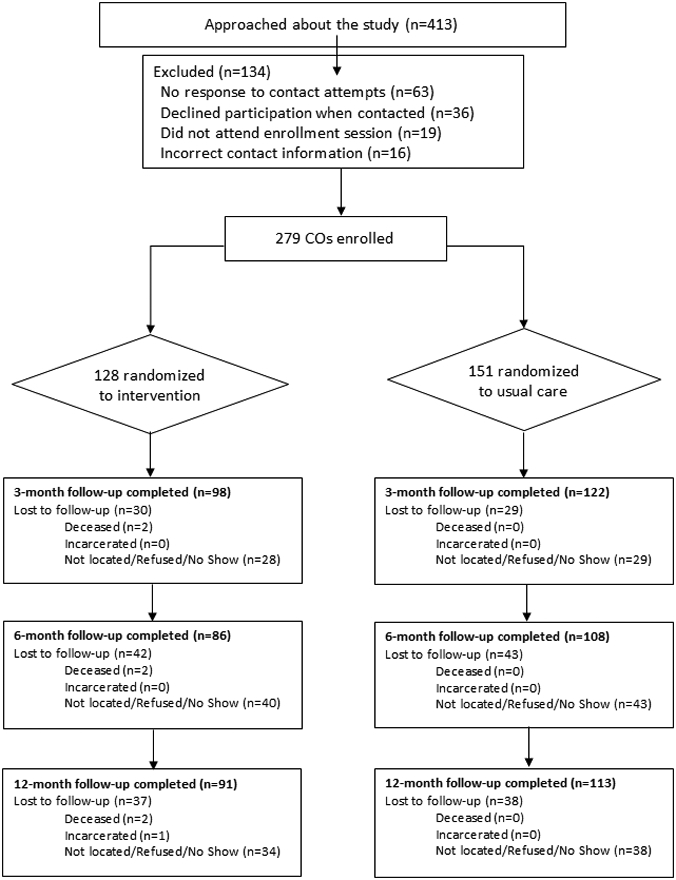
Flow of Concerned Others (COs) through the trial.
Sample size
The sample size was determined by conducting an analysis on primary and secondary outcomes. Specifically, power was based on the expected observation of at least a medium effect size (.50) between the two conditions: (1) addiction treatment patients who received Intensive Referral to AA had, at 1-year follow-up, more AA participation (Cohen’s d=.47) and drinking improvement (d=.50) than UC patients did [19]; and (2) COs of persons with AUDs randomly assigned to 8 weeks of psychotherapy focused on Twelve Step Facilitation to Al-Anon improved from baseline to 1-year follow-up on coping (d=.78) and depression (d=.81) [13]. The projected proportion attending an Al-Anon meeting would be 24% more in the AIR than the UC group. A sample size of 240 COs (120 in each condition) was calculated as allowing an 80% likelihood of detecting a medium effect size at the 5% level of significance (two-tailed test; Proc Power, SAS 9.3).
Recruitment
To accrue the sample, first, patients entering AUD residential treatment were asked for permission by treatment staff to be contacted by the study team. Patients who agreed were contacted in person at the treatment program by study staff, and were screened (if they agreed) for study eligibility (at least 19 years old, could communicate in English, did not have a conservator). Of 453 patients approached about the study by study staff, 94% (n=426) agreed to be screened for eligibility, and of these, 96% (n=409) were eligible for the study (the only reason for ineligibility was having a conservator). Of eligible patients, 402 (98%) were enrolled and completed the study's baseline assessment.
Each patient was asked to provide a signed release naming potential COs (someone at least 19 years old who was important to and supportive of the patient and the current treatment episode) and COs’ contact information. The study team attempted to contact a CO for each patient to obtain informed consent and completion of the study baseline assessment. Of 413 COs approached about the study, 279 were enrolled and completed the study baseline assessment (68%; Figure 1). Reasons for non-enrollment (n=134) were: CO did not respond to repeated contact attempts (47%), CO declined participation when contacted (27%), CO did not attend scheduled enrollment sessions (14%), and CO’s contact information from the drinker was incorrect (12%).
Randomization
After the baseline interview, COs were randomly assigned to condition (AIR or UC). Simple randomization of participants was conducted by the project manager using the website Randomizer.org at each site. Groups were expected to be equal in number.
Treatment programs
We included Department of Veterans Affairs (VA) and community programs at three US geographically dispersed sites to increase generalizability of findings; 115 COs were recruited in the west, 75 in the midwest, and 89 in the south. VA is the largest health care system and provider of addiction treatment services in the US, provides similar health care to that in non-VA systems, is used by patients who also use community care, provides evidence-based treatment at appropriate levels of care, and has a nationwide electronic medical record that enhances study follow-ups. Due to their high risk, Veterans are a major focus of public health efforts to improve population well-being. Nevertheless, to avoid limiting findings to one health care system, the study included community programs which were selected in part because they provided similar UC and were geographically close to enable project coordination and oversight.
Conditions
Usual care
UC was available to all COs enrolled in the study. UC consisted of the treatment program’s offer of educational sessions for COs of patients residing in the program. These educational sessions covered the causes, effects, and treatment of addictions; recovery phases; and COs’ reactions to the course of addiction and recovery. They were offered weekly or biweekly for 60-90 minute sessions. Of COs assigned to UC, 24% had attended educational sessions at the 3-month follow-up.
Al-Anon Intensive Referral
AIR consisted of four sessions lasting 30-60 minutes each. The first two sessions were held in person or by telephone, one week apart. The third and fourth sessions were held by telephone, one and two months, respectively, after the second session. All sessions were led by AIR Coaches who had master’s degrees and training in working with substance use disorder patients and their COs. Coaches were trained in and delivered, with supervision, AIR. After Coaches were trained together, they delivered AIR at the site at which they were located (west, midwest, or south). Supervision was from a clinician and included review of session content and feedback on adherence using a protocol checklist.
Session 1’s aim was to explain what Al-Anon is and what meeting attendance involves. The Coach told COs how to obtain a schedule of local in-person and virtual Al-Anon meetings, and reviewed handouts on Al-Anon that provided an introduction to its philosophy, structure, and terminology; addressed common concerns about participation; and encouraged COs to set goals (e.g., attend meetings, work the first steps). COs were encouraged to go to at least one Al-Anon meeting during the following week (using the obtained schedule) and keep a journal about Al-Anon meetings attended (or reasons for not attending). At Session 2, the Coach mainly asked about COs’ experiences attending Al-Anon meetings and discussed any doubts COs may have had about Al-Anon participation. The Coach suggested that the CO obtain a temporary sponsor, reviewed how to do so, and discussed any concerns the CO may have about asking for and working with a sponsor. COs were encouraged to attend at least 3-6 Al-Anon meetings before deciding whether to continue. Sessions 3 and 4 were booster sessions to continue to support Al-Anon engagement. During both booster sessions, the Coach asked about Al-Anon attendance and involvement (e.g., sponsorship), problem-solved any barriers COs may have had to Al-Anon participation (e.g., strategies to overcome them, redressing misunderstandings), and supported COs’ continued Al-Anon engagement by highlighting successes. During all sessions, Coaches kept notes on challenges COs reported to attending Al-Anon.
Of 128 COs randomized to AIR, 85.0% completed Session 1; 79.0% completed Sessions 1 and 2; 63.8% completed Sessions 1 through 3; and 57.7% completed Sessions 1 through 4. No adverse events occurred due to AIR participation. We used an intent-to-treat design and followed all participants irrespective of participation in AIR.
Measures
Primary outcome
The primary outcome was Al-Anon attendance at 3-month follow-up. At baseline, COs reported whether they had been to an Al-Anon meeting in the past 6 months (21.0% said yes). At the 3- and 6-month follow-ups, COs reported whether they had attended an Al-Anon meeting in the past 3 months; at the 12-month follow-up, COs reported on the past 6 months.
Secondary outcomes
At baseline, COs reported the number of Al-Anon meetings attended in the past 6 months (M=1.8, SD=7.5). At the 3- and 6-month follow-ups, COs reported the number of Al-Anon meetings they had attended in the past 3 months; at the 12-month follow-up, COs reported on the past 6 months.
The CO-patient relationship at baseline and each follow-up was assessed using the Health and Daily Living Form (HDL) [22]. The HDL has been used extensively and is psychometrically sound [23,24]. COs rated their relationship with their patient on 10 items in the Quality of Significant Relationship index with regard to how often events occurred (0=never, 4=very often). Relationship Stressors was the sum of five items from the index (e.g., patient expected more from you than she or he gave; at baseline, M=11.2, SD=5.9, alpha =.89). Relationship Resources was the sum of five items from the index (e.g., you calmly discussed something with your patient; at baseline, M=13.1, SD=5.7, alpha = .89).
Covariates/predictors
We included the CO-patient relationship type as marital (32.7%) or not marital (67.3%) because this is standard practice in studies of harms due to others’ substance use [32, 34, 35]. The CO’s self-reported relationship to the drinker was current spouse or partner (30.1%), former spouse or partner (2.6%), parent (25.0%), sibling (13.2%), offspring (11.4%), other relative (2.6%), or friend (15.1%). Program was also included as a predictor due to the study design. Time (with values 1-4 to indicate follow-up duration) was included to examine if outcomes varied across timepoints.
Analysis plan
The study’s hypotheses were that, compared to UC, AIR would increase Al-Anon attendance (primary outcome: any attendance; secondary outcome: number of meetings) and improve CO-patient relationships (secondary outcomes: fewer stressors, more resources). To test these hypotheses, analyses used generalized linear mixed models (GLMM) appropriate for the distribution of the outcome variable and error term, under the assumption that data were missing at random. The main effect of interest was condition (UC, AIR). Also included as predictors in the models were: the baseline value of the dependent variable; time (treated as categorical with 3 months as the referent), CO-patient relationship type (marital or not marital), and treatment program (southern US, VA or community program; midwestern US, VA or community program; or western US, VA program). Also included was the interaction of condition by time, and condition by program; when the interaction was not significant, it was dropped from the model. For the binary primary outcome, binomial distribution with logit link was specified. For the secondary outcome of number of Al-Anon meetings, negative binomial distribution with log link was specified given its nature of being a count variable. For the secondary CO-patient relationship outcomes, normal distribution with identity link was specified as they were approximately normally distributed. SAS 9.4 was used for the analysis.
RESULTS
Participant characteristics
COs’ and their patients’ demographic characteristics are provided in Table 1. COs assigned to the two different conditions did not differ on any of their own characteristics (including type of relationship with the patient) or on any of their patients’ baseline characteristics.
Table 1.
Baseline demographic characteristics of Concerned Other and patient members of dyads (n=279 dyads).
| CO AIR | CO UC | COs | Patients CO AIR |
Patients CO UC |
Patients | |
|---|---|---|---|---|---|---|
| Women (%, n) | 78.9 (101) | 75.5 (114) | 77.3 (215) | 23.4 (30) | 24.2 (36) | 23.8 (66) |
| Age (M, SD) | 52.6 (14.4) | 51.3 (15.0) | 51.9 (14.8) | 42.3 (11.6) | 44.2 (13.1) | 43.3 (12.5) |
| White (%, n) | 69.9 (89) | 66.9 (101) | 68.3 (190) | 68.9 (88) | 69.2 (104) | 69.0 (192) |
| Black (%, n) | 19.5 (25) | 23.2 (35) | 21.2 (59) | 21.3 (27) | 24.7 (37) | 23.1 (64) |
| Hispanic (%, n) | 8.6 (11) | 10.7 (16) | 9.9 (27) | 11.0 (14) | 11.0 (17) | 11.0 (31) |
| Not married (%, n) | 58.6 (75) | 58.0 (88) | 58.5 (163) | 84.3 (108) | 79.1 (119) | 81.5 (227) |
| Yrs. of education (M, SD) | 13.8 (2.1) | 13.8 (2.0) | 13.8 (2.0) | 13.1 (1.9) | 13.0 (2.2) | 13.1 (2.1) |
| Employed (%, n) | 55.5 (71) | 60.0 (90) | 57.5 (161) | 16.5 (21) | 20.4 (31) | 18.6 (52) |
| Annual income (M, SD) | $40,186 ($37,277) | $43,483 ($44,007) | $42,300 ($41,100) | $25,300 ($25,679) | $25,091 ($26,261) | $25,187 ($25,948) |
Notes: CO AIR: COs assigned to AIR (n=128); CO UC: COs assigned to UC (n=151); Patients CO AIR: Patients whose CO was assigned to AIR (n=128); Patients CO UC: Patients whose CO was assigned to UC (n=151); M=Mean; SD=Standard Deviation.
Follow-ups
Research assistants, blinded to patients’ condition assignment, attempted to follow all COs who participated at baseline for follow-ups 3, 6, and 12 months later by telephone. Of the 279 COs, two had died by the 3-month follow-up, and one was incarcerated at the 12-month follow-up. The trial was stopped when follow-up procedures for all enrolled participants were completed (April 3, 2020). The 12-month follow-up rate was 74% among COs who were not deceased or incarcerated. There were no differences on baseline characteristics (gender, marital or employment status, race or ethnicity, age, education, income, and relationship to patient) or by condition between COs who were followed or not followed at 3, 6, or 12 months.
Modeling of primary and secondary outcomes
Table 2 presents descriptive statistics for the primary (Al-Anon attendance at 3 months) and secondary (all other) outcomes. Tables 3 and 4 present results for modeling of the outcomes. For the dichotomous outcome of having attended an Al-Anon meeting or not, time (but not relationship type, program, or condition) had a significant effect. Regarding condition, at 3-month follow-up, 28.1% of COs assigned to AIR had attended an Al-Anon meeting, compared to 21.1% of COs assigned to UC. The Bayes Factor was calculated as 1.86 indicating that the findings were inconclusive as to whether or not an association was present between condition assignment and the primary outcome. Regarding time, compared to the 3-month follow-up when 24.6% of COs had attended an Al-Anon meeting, a lower proportion had done so at the 6-month (17.8%) or the 12-month (16.2) follow-up. For the dependent variable of number of Al-Anon meetings attended, time, relationship type, program, and condition did not have a significant effect.
Table 2.
Descriptive statistics for the primary and secondary outcomes at each follow-up.
| Outcome | Follow-up | AIR M (SD) |
UC M (SD) |
Total M (SD) |
|---|---|---|---|---|
| Primary | ||||
| Attended Al-Anon | 3-month | 28.1 (44.1) | 21.1 (42.1) | 24.6 (42.9) |
| 6-month | 17.4 (37.3) | 18.1 (38.3) | 17.8 (39.3) | |
| 12-month | 15.9 (35.0) | 16.4 (38.4) | 16.2 (36.9) | |
| Secondary | ||||
| Number of meetings | 3-month | 4.3 (6.03) | 5.3 (10.7) | 4.86 (8.9) |
| 6-month | 4.67 (1.3) | 4.6 (1.21) | 4.63 (7.9) | |
| 12-month | 7.01 (15.1) | 6.9 (15.1) | 6.98 (15.0) | |
| Relationship Stressors | 3-month | 6.92 (5.5) | 6.91 (5.8) | 6.92 (5.7) |
| 6-month | 7.19 (5.9) | 7.71 (5.9) | 7.47 (5.9) | |
| 12-month | 6.90 (5.8) | 7.17 (5.9) | 7.05 (5.9) | |
| Relationship Resources | 3-month | 15.77 (5.7) | 15.13 (5.9) | 15.42 (5.8) |
| 6-month | 15.21 (6.5) | 12.78 (6.3) | 14.87 (6.5) | |
| 12-month | 16.00 (6.4) | 13.96 (6.3) | 14.73 (6.4) |
Table 3.
Longitudinal modeling of outcomes: attended Al-Anon (primary) and number of Al-Anon meetings (secondary).
| Attended Al-Anon OR (95% CI) |
Number of meetings Ratio of expected values (95% CI) |
|
|---|---|---|
| Baseline value | 302.20 (29.30, 3116.00) | 1.19 (1.10, 1.29) |
| Time | ||
| 3 months | 1 | 1 |
| 6 months | 0.36 (0.14, 0.88) | 0.62 (0.36, 1.05) |
| 12 months | 0.26 (0.10, 0.65) | 0.74 (0.44, 1.23) |
| Relationship type | ||
| Non-spousal | 1 | 1 |
| Spousal | 0.78 (0.19, 3.26) | 1.68 (0.44, 6.37) |
| Program | ||
| West VA | 1 | 1 |
| Midwest VA | 13.92 (0.76, 253.6) | 5.00 (0.32, 78.87) |
| South VA | 0.41 (0.01, 11.80) | 0.35 (0.02, 7.42) |
| Midwest Community | 7.19 (1.28, 40.28) | 2.49 (0.48, 12.80) |
| South Community | 0.87 (0.15, 5.06) | 4.50 (0.96, 21.21) |
| Condition | ||
| Usual care | 1 | 1 |
| AIR | 0.40, 5.52) | 1.07 (0.31, 3.67) |
| Fit statistics | Pearson X2/df=0.23 | Pearson X2/df=0.19 |
| Baseline | 3.16 (<.0001) | 18.99 (<.0001) |
| Time | 4.56 (0.011) | 1.62 (0.199) |
| Relationship type | 0.11 (0.736) | 0.59 (0.444) |
| Program | 2.27 (0.062) | 1.39 (0.237) |
| Condition | 0.34 (0.560) | 0.01 (0.912) |
Table 4.
Longitudinal modeling of outcomes: relationship stressors and resources (secondary).
| Relationship Stressors B (95% CI) |
Relationship Resources B (95% CI) |
|
|---|---|---|
| Baseline value | 0.47 (0.38, 0.56) | 0.34 (0.23,0.45) |
| Time | ||
| 3 months | (referent) | (referent) |
| 6 months | 0.44 (−0.32, 1.20) | −1.72 (−.2.59, −0.85) |
| 12 months | 0.13 (−0.62, 0.89) | −0.63 (−1.49, 0.23) |
| Relationship type | ||
| Non-spousal | (referent) | (referent) |
| Spousal | 2.19 (1.07, 3.32) | 1.08 (−0.31,2.47) |
| Program | ||
| West VA | (referent) | (referent) |
| Midwest VA | 1.36 (−0.93, 3.65) | −1.78 (−4.64, 1.08) |
| South VA | 2.40 (0.34, 4.45) | −2.29 (−4.87, 0.30) |
| Midwest Community | 0.11 (−1.30, 1.52) | 0.45 (−1.29, 2.20) |
| South Community | 0.77 (−0.52, 2.06) | −0.79 (−2.38, 0.80) |
| Condition | ||
| Usual care | (referent) | (referent) |
| AIR | 0.12 (−1.14, 0.91) | 1.33 (0.04. 2.61) |
| Fit statistics | Gener. X2/df=14.11 | Gener. X2/df=18.15 |
| Type III F (p) | ||
| Baseline | 105.13 (<.0001) | 35.09 (<.0001) |
| Time | 0.66 (0.519) | 7.65 (0.0006) |
| Relationship type | 14.70 (0.0001) | 2.32 (0.128) |
| Program | 1.69 (0.153) | 1.45 (0.218) |
| Condition | 0.05 (0.824) | 4.55 (0.033) |
For the secondary outcome of CO-patient relationship stressors, the main effect for relationship type (but not time, program, or condition) was significant. Stressors were more severe for COs in a marital relationship with the patient than for COs in a non-marital relationship. Means (SDs) at 3, 6, and 12 months, respectively, for COs in a marital relationship with the patient were 8.7 (5.2), 9.3 (5.5), and 9.9 (5.5). In contrast, means (SDs) at 3, 6, and 12 months, respectively, for COs in a non-spousal relationship with the patient were 5.9 (5.6), 6.4 (5.8), and 5.7 (5.5).
For the secondary outcome of CO-patient relationship resources, the main effect for condition and for time (but not for relationship type or program) was significant. COs assigned to the AIR condition had more resources than COs who were in the UC condition; see Table 2. In addition, resources declined from 3 months to 6 months and to 12 months; see Table 2.
DISCUSSION
In this randomized trial of COs of patients in treatment for AUDs, a referral intervention, AIR, was not associated with increases in COs’ participation in Al-Anon, relative to the usual care condition. The lack of advantage for AIR on Al-Anon attendance occurred despite having successfully delivered the intervention (i.e., 85% of COs assigned to AIR received at least one session, and 58% received all four sessions). However, AIR was associated with more resources in the CO-patient relationship. In addition, stressors in the CO-patient relationship were more severe among COs who were married to the patient than COs who had a different type of family relationship or were friends with the patient. In the following sections, we describe the context and implications of the findings along with the study’s limitations and conclusions.
Context and implications
The study’s finding that the referral intervention, AIR, did not increase Al-Anon attendance stands in contrast to findings that referral interventions to increase AA attendance have been shown to be effective [25]. For example, in a series of studies, Timko and colleagues demonstrated that Intensive Referral for patients in detoxification or substance use disorder treatment, including those with co-occurring mental health diagnoses, increased AA participation and improved outcomes. Specifically, patients assigned to Intensive Referral were more likely to attend and be involved with 12-step groups, and improved more on alcohol and drug use outcomes, at 6-month and 1- and 2-year follow-ups, than patients assigned to standard referral [17,19,26,27].
Possibly, AIR’s lack of efficacy with COs was due in part to the lesser availability of Al-Anon meetings relative to AA meetings. Prior to the COVID pandemic, there were 14,213 Al-Anon groups compared to 115,326 AA groups around the world. In addition, AIR Coaches’ notes reported reasons besides meeting unavailability that COs did not attend Al-Anon, including a lack of need (their well-being was not affected by the patient, or the patient’s difficulties would resolve now that treatment had been initiated), and a lack of willingness to do any more to help the patient than they already had (despite explanations that Al-Anon is intended to help the CO, not the patient). These Coach reports are consistent with findings that COs often withdraw emotionally from loved ones with years of active addiction, that COs’ care of others with chronic and relapsing substance use disorders is challenging to maintain over time, and that COs who do maintain a relationship with the patient may also maintain a self-identity as well-functioning to meet external expectations [6,28,29]. Additional studies using mixed methods are needed to more fully understand some COs’ reluctance to attend Al-Anon meetings.
Despite AIR’s ineffectiveness for increasing Al-Anon attendance, AIR was effective relative to UC in terms of increasing CO-patient resources as seen by the CO. Relationship resources, which declined over follow-ups, consisted of the CO and patient having calm discussions, showing consideration for and interest in each other, and cooperating with things asked of them by the other. Again, more qualitative and quantitative research is needed to fully understand these results for relationship resources. Although the finding for the effect of condition may be spurious, it suggests that a brief intervention presenting options for help for COs alone may foster a more positive view of the relationship. In turn, a more positive view may open the door to the COs’ continued support of the patient, which has been shown to contribute to patients’ recovery [30]. McCrady et al. [30] found that during Alcohol Behavioral Couple Therapy (ABCT), couples talked less about drinking and increased their positive behaviors, and that contemptuousness between partners predicted poorer drinking outcomes for the patient. Possibly, AIR’s focus on a care option for the CO, rather than on the patient’s drinking, inadvertently helped the CO to consider the positive aspects of continuing to invest in a relationship with the patient.
As suggested by the study of treatments such as ABCT that focus on married partners, the negative effects of a patient’s AUD on a spouse, including depression and anxiety, the experience of violence, and financial and legal difficulties, are well known [31]. Accordingly, ABCT has been tested mainly among heterosexual romantic partners and spouses. The present study found that CO-patient stressors were more severe for COs who were spouses than for other COs. Regarding the type of CO-patient relationship, other approaches to studying dyads of COs and people with addictions (sometimes referred to as the Identified Patients) did not find different effects based on type of relationship. For example, a recent systematic review of CRAFT (i.e., Community Reinforcement Approach and Family Training) found that the type of CO-Identified Patient relationship (e.g., child, spouse or partner) was not a determining factor of the intervention’s effects [32]. The determinants and outcomes of CO-patient relationship stressors and resources need to be evaluated in all types of CO-drinker pairs, including dyads of friends, parents, and offspring; these composed the majority of CO-patient relationship types in the present sample.
Limitations and conclusions
Despite this study’s strengths (e.g., good retention rates among this difficult-to-follow CO sample), there were also limitations. A main limitation was that the sample consisted of COs in a dyad with people who had entered residential treatment. Results may not generalize to dyads that include people unable or unwilling to access such treatment. In particular, AIR or a similar intervention may be more efficacious in a less severely impacted population of patients and their COs, such as in outpatient treatment settings. In addition, the sample consisted of COs who were not necessarily seeking help or experiencing mental health symptoms or lack of social support, and were identified by patients as supportive of their recovery, possibly limiting generalizability of the findings. Screening for those with a reason to attend Al-Anon may have set the stage for improved AIR outcomes.
In conclusion, the COs in this study participated in the year following a family member or friend’s entry into an AUD treatment episode. The findings, together with those from a formative evaluation of AIR [36], suggest avenues for future research including that these COs may need a more intensive intervention to engage in the 12-step program of Al-Anon, that AIR should be delivered by peers who share the lived experience of being harmed by another’s drinking [35], or that Al-Anon’s availability is too limited to be a feasible option for many COs. They also suggest that COs may be most open to intervention soon after the patient enters treatment, given that both Al-Anon participation and relationship resources were highest during the 3-month follow-up period. Unknown is whether the shift to online meetings during the current pandemic may facilitate Al-Anon participation among COs. This study also observed that the AIR intervention was associated with COs’ perceptions of having more resources within their relationship with their patient. Gaining a better understanding of how COs, especially those who are married to patients in treatment, may benefit from talking with an Al-Anon Coach may be helpful to their well-being. It is important to continue to develop and test novel methods to improve outcomes among COs to benefit both COs and patients.
Acknowledgements
We gratefully acknowledge these contributors to the study: Cynthia Beaumont, LaKiesha Kemp, Kristina Kennedy, Rebecca Losh, Camille Mack, Rakshitha Mohankumar, Amia Nash, Alexandra Shelley, Emmeline Taylor, and KaSheena Winston; and consultants Barbara McCrady and Gregory Stuart.
This research was supported by NIH/NIAAA (R01 AA024136 01A1 to Drs. Timko and Cucciare; ClinicalTrials.gov Identifier: NCT04018560) and the Department of Veterans Affairs (VA), Health Services Research and Development (HSR&D) Service (RCS 00-001 to Dr. Timko). The views expressed are the authors’. No conflicts of interest are reported by any of the authors listed on this manuscript.
REFERENCES
- 1.Nayak MB, Patterson C, Wilsnack S Alcohol's secondhand harms in the United States: New data on prevalence and risk factors. J Stud Alcohol Drugs 2019; 80: 273–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Karriker-Jaffe KJ, Greenfield TK, Kaplan LM Distress and alcohol-related harms from intimates, friends, and strangers. J Subst Use 2017; 22: 434–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Laslett A-M, Jiang H, Kuntsche S, Stanesby O, Wilsnack S, Sundin E et al. Cross-sectional surveys of financial harm associated with others' drinking in 15 countries: unequal effects on women? Drug Alcohol Depend 2020; 211: 107949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Timko C, Cronkite R, Laudet A, Kaskutas LA, Roth J, Moos RH Al-Anon Family Groups' newcomers and members: Concerns about the drinkers in their lives. Am J Addict 2014; 23: 329–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Timko C, Young LB, Moos RH Al-Anon Family Groups for relatives and friends. J Groups Addict Recover 2012; 7: 279–296. [Google Scholar]
- 6.Young LB, Timko C Benefits and costs of alcoholic relationships and recovery through Al-Anon. Subst Use Misuse 2015; 50: 62–71. [DOI] [PubMed] [Google Scholar]
- 7.Al-Anon Family Groups. Triennial 2018 membership survey. Virginia Beach, VA: Al-Anon Family Groups Headquarters; 2018. [Google Scholar]
- 8.Cutter CG, Cutter HS Experience and change in Al-Anon Family groups: Adult children of alcoholics. J Stud Alcohol Drugs 1987; 48: 29–32. [DOI] [PubMed] [Google Scholar]
- 9.Barber JG, Gilbertson R An experimental study of brief unilateral intervention for the partners of heavy drinkers. Res Soc Work Pract 1996; 6: 325–336. [Google Scholar]
- 10.Dittrich JE, Trapold MA A treatment program for wives of alcoholics: An evaluation. Addict Behav 1984; 3: 91–102. [Google Scholar]
- 11.Miller RM, Meyers RJ, Tonigan JS Engaging the unmotivated in treatment for alcohol problems: A comparison of three strategies for intervention through family members. J Consult Clin Psychol 1999; 67: 688–697. [DOI] [PubMed] [Google Scholar]
- 12.Nowinski J Self-help groups for addictions. In: McCrady BS, Epstein EE, eds. Addictions: A comprehensive guidebook. New York, NY, US: Oxford University Press; 1999: 328–346. [Google Scholar]
- 13.Rychtarik RG, McGillicuddy NB Coping skills training and 12-step facilitation for women whose partner has alcoholism: Effects on depression, the partner’s drinking, and partner physical violence. J Consult Clin Psychol 2005; 73: 249–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Timko C, Laudet A, Moos RH Al-Anon newcomers: Benefits of continuing attendance for six months. Am J Drug Alcohol Abuse, 2016; 42, 441–449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Etemadi A, Zarebahramabadi M, Mirkazemi R Effect of Al-Anon attendance on family function and quality of life in women in Mashhad, Iran. Drug Alcohol Abuse 2015; 41: 442–448. [DOI] [PubMed] [Google Scholar]
- 16.Grant KM, Young LB, Tyler KA, Simpson JL, Pulido RD, Timko C Intensive referral to mutual-help groups: A field trial of adaptations for rural veterans. Patient Educ Couns 2018;101: 79–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Timko C, Sutkowi A, Cronkite RC, Makin-Byrd K, Moos RH Intensive referral to 12-step dual-focused mutual-help groups. Drug Alcohol Depend 2011; 118: 194–201. [DOI] [PubMed] [Google Scholar]
- 18.Timko C, Below M, Vittorio L, Taylor E, Chang G, Lash S, et al. , Brief, D. Randomized controlled trial of enhanced telephone monitoring with detoxification patients: 3- and 6-month outcomes. J Subst Abuse Treat 2019; 99: 24–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Timko C, DeBenedetti A A randomized controlled trial of intensive referral to 12-step self-help groups: One-year outcomes. Drug Alcohol Depend 2007; 90: 270–279. [DOI] [PubMed] [Google Scholar]
- 20.McCambridge J, Kypri K, Elbourne D Research participation effects: A skeleton in the methodological cupboard. J Clin Epidemiol 2014; 67: 845–849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McCambridge J, Witton J, Elbourne D Systematic review of the Hawthorne effect: New concepts are needed to study research participation effects. J Clin Epidemiol 2014; 67: 267–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moos RH, Cronkite RC, & Finney JW Health and daily living form manual (2nd ed.). Menlo Park, CA: Mind Garden; 1992. [Google Scholar]
- 23.Bi X, Moos RH, Timko C, Cronkite RC Family conflict and somatic symptoms over 10 years: A growth mixture model analysis. J Psychosom Res 2015; 78: 459–465. [DOI] [PubMed] [Google Scholar]
- 24.Holahan CJ, Brennan PL, Schutte KK, Holahan CK, Hixon JG, Moos RH Drinking level versus drinking pattern and cigarette smoking among older adults. Alcohol Clin Exp Res 2018; 42: 795–802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kelly JF, Abry A, Ferri M, Humphreys K Alcoholics Anonymous and 12-step facilitation treatments for alcohol use disorder: A distillation of a 2020 Cochrane Review for clinicians and policy makers. Alcohol 2020; 55: 641–651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Timko C, DeBenedetti A, Billow R Intensive referral to 12-Step self-help groups and 6-month substance use disorder outcomes. Addiction 2006;101: 678–688. [DOI] [PubMed] [Google Scholar]
- 27.Vederhus JK, Timko C, Kristensen O, Hjemdahl B, Clausen T Motivational intervention to enhance post-detoxification 12-Step group affiliation: A randomized controlled trial. Addiction 2014; 109: 766–773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McKay JR Making the hard work of recovery more attractive for those with substance use disorders. Addiction 2017; 112: 751–757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tambling RR, Russell B, D’Aniello C Where is the family in young adult substance use treatment? The case for Systemic Family Therapy for young adults with substance use disorders. Int J Ment Health Addict 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McCrady BS, Tonigan JS, Ladd BO, Hallgren KA, Pearson MR, Owens MD, Epstein EE Alcohol Behavioral Couple Therapy: In-session behavior, active ingredients and mechanisms of behavior change. J Subst Abuse Treat 2019; 99: 139–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dostanic N, Djikanovic B, Jovanovic B, Stamenkovic Z, Deric A The association between family violence, depression and anxiety among women whose partners have been treated for alcohol dependence. J Fam Violence 2021; 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Archer M, Harwood H, Stevelink S, Rafferty L, Greenberg N Community reinforcement and family training and rates of treatment entry: A systematic review. Addiction 2020; 115: 1024–1037. [DOI] [PubMed] [Google Scholar]
- 33.Roozen HG, Waart R, van der Kroft P Community reinforcement and family training: an effective option to engage treatment-resistant substance-abusing individuals in treatment. Addiction 2010; 105: 1729–38. [DOI] [PubMed] [Google Scholar]
- 34.Karriker-Jaffe K, Li L, Greenfield TK Estimating mental health impacts of alcohol's harms from other drinkers: using propensity scoring methods with national cross-sectional data from the United States. Addiction 2018; 113:1826–1839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Timko C, Cucciare MA, Grant KM, Young LB, Rossi FS, Lor MC, Woodhead E Patients with alcohol use disorders and their concerned others: Concordance of lived experience as a moderator of treatment outcomes. Journal of Studies on Alcohol Studies in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Baloh J, Curran GM, Timko C, Grant KM, & Cucciare MA Al-Anon Intensive Referral (AIR): A qualitative formative evaluation for implementation. Journal of Substance Abuse Treatment in press. [DOI] [PMC free article] [PubMed] [Google Scholar]


