Abstract
Purpose
Sexually transmitted infections are a major worldwide concern, and human papillomavirus (HPV) is one of the significant risk factors. Many populations suffer from various diseases caused by HPV, and the overall death toll due to cervical carcinoma is remarkable. Despite vaccine availability, perception about vaccine safety and efficacy, its’ preventive outcome is still inferior among the health professionals and vaccine providers. So, this study aims to assess the knowledge, attitude, and practice level of HPV and its’ vaccination among doctors, dentists, and medical students.
Materials and Methods
This cross-sectional survey was carried out between April to August 2021, where 626 participants from all types of medical institutions of Bangladesh were interviewed using a validated and structured questionnaire that consists of four extensive areas; socio-demographic characteristics, HPV knowledge, attitude, and practices regarding vaccination.
Results
The knowledge and practice standards showed very poor outcomes where 43.29% of the participants showed good knowledge and only 11.82% conveyed good practices. Nevertheless, the attitude towards HPV vaccination was revealed high (75.88%). Female participants showed more positive attitudes than males.
Conclusion
Physicians and dentists play vital roles in raising public knowledge about HPV and awareness regarding HPV vaccination programs. The provision of medical education on HPV must be prioritized, and current training techniques must be re-evaluated. Thus, by implementing this strategy, improvement in national vaccination policy can be expected.
Keywords: Human papillomavirus, Knowledge and attitude, Vaccination, Medical students, Professionals
Introduction
Human papillomavirus (HPV) is the commonest cause of sexually transmitted infections. In 2018, approximately 43 million individuals were infected with HPV; most were in their late 10s and early 20s [1]. HPV comes in a variety of types which causes different diseases, such as genital warts and cancer, that is harmful to one’s health [2]. From benign cutaneous lesions to cervical cancers, it may cause a wide variety of illnesses. Most clinically important lesions produced by HPV are cervical carcinoma and precancerous intraepithelial lesions of the cervix, which afflict approximately 1.4 million women globally [3]. In recent researches, high-risk HPV has been identified as a risk factor for head and neck squamous cell carcinoma (HNSCC), irrespective of the conventional risk variables such as cigarette smoking and alcohol intake [4,5,6]. Recent research in Bangladesh has shown a high prevalence of HPV-associated HNSCC [7].
HPV affects both men and women. According to 2012 data, HPV was linked to 74% of cancer cases in women, where 70% of the cases were cervical cancer [8]. Moreover, HPV DNA has been found in about half of all penile malignancy cases in males, where the most frequent types were HPV 16, HPV 18, and HPV 6/11 [9,10]. Vaccination against HPV is an effective way to reduce the chance of transmission of infection irrespective of genders [11]. The US Food and Drug Administration approved the first HPV vaccination in 2008, with the aim of preventing 70% of the cervical cancers and other illnesses caused by HPV 16 and 18 [12]. A systematic review on cost-effectiveness analysis of HPV vaccine supported the necessity of vaccine coupled with screening tests to prevent the HPV infection [13]. However, in developing countries, the population’s intentions to adopt HPV vaccination remain low [14,15,16]. HPV vaccines were first made accessible and available in 2017, and from then they were made available as a regular immunization for girls in 71 countries [17]. Depending on a person’s age and immunological conditions, two or three doses of HPV vaccination are usually recommended [17]. It is generally advised to females between the ages of 9 and 13 years [18]. In Bangladesh, the HPV vaccine was first introduced in 2016 via establishing a demonstration project in the Gazipur district, overseen by the Ministry of Health and Family Welfare of Bangladesh and funded by the Global Alliance for Vaccines and Immunization (the Vaccine Alliance) [19]. By then, bivalent (Cervarix) and quadrivalent (Gardasil) HPV vaccines are available in Bangladesh, and plan of cost-effectiveness analyses are in the processes to determine if the addition of HPV vaccine to the national immunization program can be beneficial for the country [19]. It is also important to understand people’s views and attitudes towards the disease outcome of HPV and its’ prevention strategies across different sectors of the society to understand about the implementation of an effective national HPV vaccination policy.
According to Islam et al. [20], a cross-sectional study was performed in 2018 among the Bangladeshi women with poor education and low socioeconomic status, where little awareness about the cervical cancer with high desires to get HPV vaccinated were noticed. Another nationally representative, cross-sectional survey was conducted in 2015 among the midlife women of Bangladesh that surprisingly showed a high level of knowledge about cervical cancer (81%) [21]. Several cross-sectional studies among the healthcare professionals in various developed countries have shown substantial lacks of awareness about the HPV vaccination availability [22,23]. These evaluations among health experts are essential since the general people (especially parents of teenagers) obey the advices of vaccine providers and health professionals [24]. So, it is essential to grasp the knowledge and attitude level of HPV infections and vaccination among the medical students and young doctors at first to identify the practice gaps in their professional lives.
Therefore, the primary objective of this study is to evaluate the knowledge level about HPV, attitudes, and practices towards HPV vaccine among the young health professionals and students with the aim to identify areas that require additional attentions and policies, which may increase the acceptability of the vaccine among general population and reduce the disease burden.
Materials and Methods
This cross-sectional study has been conducted among 626 medical and dental students and freshly graduated doctors and dentists. Students in their third, fourth, and fifth years of medical and dental colleges, as well as recent graduates (graduated within last 5 years), were the participants of this research. Participants from medical and dental colleges and hospitals (public, private, and military) from eight divisions of Bangladesh (Dhaka, Mymensingh, Chattogram, Sylhet, Rajshahi, Khulna, Rangpur, and Barisal) were selected via convenient sampling technique. The participants were interviewed physically or over telephone by trained volunteers from different medical and dental colleges. Data was collected over 2 months, from July to August, 2021. The data has been processed and analyzed using the STATA MP ver. 16 software (Stata Corp., College Station, TX, USA). For data analysis, several statistical techniques have been used. A p-value less than 0.05 with a 95% confidence interval (CI) has been considered statistically significant. To evaluate the relationship between outcomes and independent variables, chi-square tests were used. To validate the link, multivariate logistic regression analysis was done.
The questionnaire used in this study was prepared based on previously conducted similar types of studies and was standardized to meet the study’s objectives. The face validity of the questionnaire was verified with the help of five experts in the relevant areas and obtaining their agreement on each item of the list of questions. In order to validate the questionnaire further and to determine whether the questionnaire could be administered successfully or not, a pilot testing was done on 125 participants. Exploratory factor analysis (EFA) was employed to determine the interrelationships between the questions. The principal component technique and varimax rotation were used to divide items into subscales. The loading factor was adjusted at 0.30 and more, with a significance level of <0.001. Following EFA, reliability was determined by calculating Cronbach’s α and item-rest correlations. The data was randomly split into three groups and then examined the inter-class correlation between the datasets; the item rest correlation was higher than 0.3, and Cronbach α values of knowledge and attitude section were greater than 0.6, although it was less in the practice section. Overall calculated α was 0.72. The normality of the distribution, linearity, outliers, and multi-collinearity of the data were all checked. Ethical approval was obtained from the Institutional Review Board (IRB) of North South University (#2021/OR-NSU/IRB/0702). The institutional human ethical commission gave its permission, which was required under regulations. Wherever possible, the ethical criteria outlined in the 1964 Declaration of Helsinki and its subsequent revisions, as well as equivalent ethical norms, were observed. We explicitly explained the detail of the survey to each eligible respondent and informed consent was obtained from all individual participants included in the study. We assured the respondents about the ethical points of view that would disclose any part of the interview to any unauthorized person under no circumstances.
Results
Among the 626 participants, the majority (55.59%) were between 21 and 25 years of age, with females representing 58.95% of the respondents. Among them, 520 participants (83.07%) were Muslims, 76.36% of study participant’s marital status was single, and approximately 95% participants did not have any children. Among the respondents, 64.22% were from government institutions, 35.14% were from private institutions, and 0.64% were from military medical colleges. 30.51% of the participants were MBBS (Bachelor of Medicine, Bachelor of Surgery) students, whereas dental students made up 19.49%, graduated physicians were 26.04%, and dentists made up 23.96%. About 64.22% of the participants were never been sexually exposed, but 26.84% gave the history of sexual exposure, and 8.95% of the respondents refused to talk about this personal issue. Among the participants with sexual exposure, 58.56% said they never used condoms, 27.54% stated occasional use of condoms, and 13.90% gave history of regular condom uses. In terms of household income and others, details have been mentioned in Table 1.
Table 1. Demographic characteristics of the participants (N=626).
| Characteristic | Frequency (%) | |
|---|---|---|
| Age groups (yr) | ||
| 21–25 | 348 (55.59) | |
| 26–30 | 266 (42.49) | |
| 31–35 | 10 (1.60) | |
| >36 | 2 (0.32) | |
| Gender | ||
| Male | 257 (41.05) | |
| Female | 369 (58.95) | |
| Religions | ||
| Islam | 520 (83.07) | |
| Hinduism | 95 (15.18) | |
| Christian | 4 (0.64) | |
| Buddhist | 7 (1.12) | |
| Marital status | ||
| Single | 478 (76.36) | |
| Married | 148 (23.64) | |
| Have children | ||
| No | 595 (95.05) | |
| Yes | 31 (4.95) | |
| Types of institutions | ||
| Government | 402 (64.22) | |
| Private | 220 (35.14) | |
| Others | 4 (0.64) | |
| Educational background | ||
| Medical student | 191 (30.51) | |
| Dental student | 122 (19.49) | |
| MBBS doctor | 163 (26.04) | |
| BDS doctor | 150 (23.96) | |
| History of sexual exposure | ||
| Never exposed | 402 (64.22) | |
| Exposed | 168 (26.84) | |
| Refused to disclose | 56 (8.95) | |
| Family income (BDT) | ||
| <25,000 | 39 (6.23) | |
| 25,000–50,000 | 313 (50.00) | |
| 50,000–1,00,000 | 213 (34.03) | |
| >1,00,000 | 61 (9.74) | |
MBBS, Bachelor of Medicine, Bachelor of Surgery; BDS, Bachelor of Dental Surgery; BDT, Bangladesh taka.
We have set our knowledge score “19” since we used 19 questions to evaluate the participants’ knowledge about the HPV and its vaccination. Therefore, we classified good knowledge as having at least 60% of the entire score, which is 12 or above, and poor knowledge as having less than 60% of the total score, which is less than 12. The prevalence of good knowledge was 43.29% among the total participants, whereas it was poor among 56.71% of respondents. Table 2 shows the frequency and percentage of knowledge level among the participants and their attitude and practice prevalence. Among them, 75.88% of respondents showed a positive attitude towards HPV vaccination, but only 11.82% of respondents have started or completed their HPV vaccination. In attitude subsection, answers with “agree” to all vaccine related questions were considered positive attitude. Completing or staring vaccination, encouraging others and educating on HPV was labeled as good practice in practice subsection. Expatiated attitudes towards the HPV and its’ vaccination have been illustrated in Table 3.
Table 2. Overall prevalence of knowledge, attitude, and practice.
| Variable | Frequency (%) | |
|---|---|---|
| Knowledge | ||
| Poor knowledge (score <12) | 355 (56.71) | |
| Good knowledge (score ≥12) | 271 (43.29) | |
| Attitude towards vaccine recommendation | ||
| Negative attitude | 151 (24.12) | |
| Positive attitude | 475 (75.88) | |
| Practice of human papillomavirus vaccination | ||
| Poor practice | 552 (88.18) | |
| Good practice | 74 (11.82) | |
Table 3. Medical professionals’ attitude towards HPV and vaccination.
| Attitude | Agree | Disagree | |
|---|---|---|---|
| HPV | |||
| Human papilloma is a deadly virus | 511 (81.63) | 115 (18.37) | |
| Education on HPV is useful | 625 (99.84) | 1 (0.16) | |
| Interested in attending HPV training programs | 595 (95.05) | 31 (4.95) | |
| Anti-HPV vaccine | |||
| Recommend HPV vaccine to patients | 606 (96.81) | 20 (3.19) | |
| Willing to get vaccinated | 531 (84.82) | 95 (15.18) | |
| Intention to children get vaccinated | 601 (96.01) | 25 (3.99) | |
| HPV vaccine is effective | 597 (95.37) | 29 (4.63) | |
| HPV vaccine is safe | 602 (96.17) | 24 (3.83) | |
| HPV vaccine should be mandatory for both boys and girls before sexual exposure | 581 (92.81) | 45 (7.19) | |
Values are presented as number (%).
HPV, human papillomavirus.
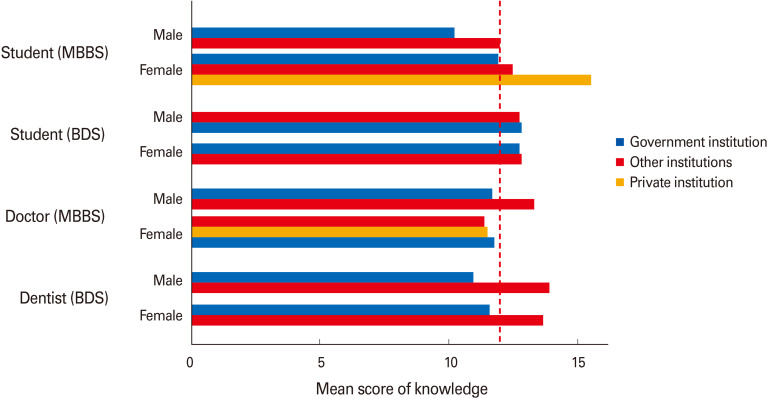
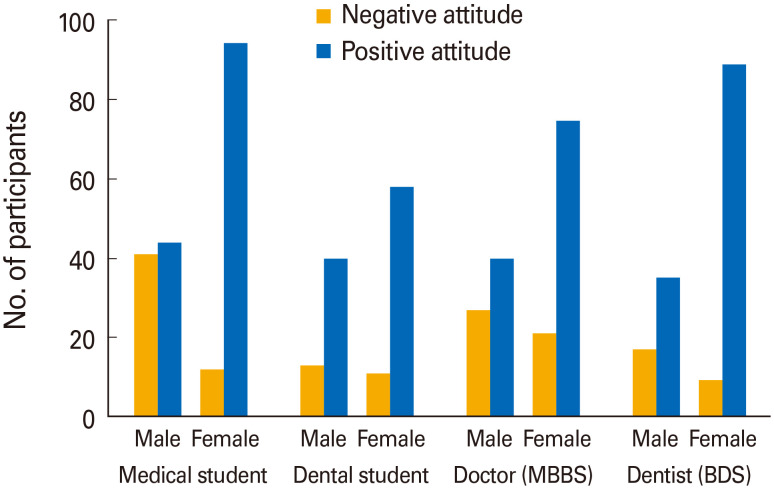
Here, we also performed bi-variate analysis, and the unadjusted result has been presented in Table 4. The result shows that several potential factors are associated with the knowledge, attitude, and practice of HPV and its vaccine. After doing the chi-square test, gender is significantly associated with attitude and practice of HPV and its vaccine (both p<0.001) but not with the knowledge (p-value=0.485). Female participants showed a more positive attitude (85.64%) towards the HPV vaccine than male participants (61.87%). Practices of HPV vaccination was poor in both genders, but it was poorer among male professionals (93.39%). On average, our findings showed that religion was significantly associated (p<0.05) with awareness of HPV and its vaccination as 100% of the participants showed good knowledge who belong to Christianity. Parenthood also showed significant associations with HPV knowledge (p-value=0.038) as knowledge level was comparatively good among those who have kids. Marital status showed good association with HPV vaccination practices (p<0.001) and good knowledge level was found among those who gave a history of sexual exposure and always use condoms. Furthermore, institutional type and graduation status showed strong associations with knowledge and attitude regarding HPV and vaccination. Good knowledge about the outcome of HPV infection and its’ vaccination was higher among the participants who are currently studying or graduated from private institutions (55.45%) than the participants who are studying or graduated from government institutions (36.32%). Although, it was highest (75%) among the participants who graduated from armed forces medical schools. Positive attitude was also found more among the participants from private institutions (85.45%) than the government institutions (70.9%). In both cases, the p-value was 0.000. Interestingly, the educational background also showed an important association with attitudes regarding HPV and vaccination (p<0.05) where dentists and who are currently studying dentistry showed more positive attitude (82.67% and 80.33%, respectively) than the MBBS doctors and students (70.55% and 72.25%, respectively). Both the comparisons have been illustrated in a bar chart (Fig. 1).
Table 4. Associations between demographic characteristics and HPV, HPV vaccine knowledge, attitude, and practices.
| Variable | Knowledge | Attitude towards vaccine | Practice | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Poor | Good | p-value | Negative | Positive | p-value | Poor | Good | p-value | ||
| Gender | 0.485 | 0.000 | 0.000 | |||||||
| Male | 58.37 | 41.63 | 38.13 | 61.87 | 93.39 | 6.61 | ||||
| Female | 55.56 | 44.44 | 14.36 | 85.64 | 84.55 | 15.45 | ||||
| Religion | 0.040 | 0.462 | 0.472 | |||||||
| Islam | 55.58 | 44.42 | 24.81 | 75.19 | 88.46 | 11.54 | ||||
| Hinduism | 64.21 | 35.79 | 22.11 | 77.89 | 87.37 | 12.63 | ||||
| Buddhist | 71.43 | 28.57 | 0 | 100.00 | 71.43 | 28.57 | ||||
| Christian | 0 | 100.00 | 25.00 | 75.00 | 100.00 | 0 | ||||
| Marital status | 0.188 | 0.774 | 0.000 | |||||||
| Single | 58.16 | 41.84 | 23.85 | 76.15 | 91.21 | 8.79 | ||||
| Married | 52.03 | 47.97 | 25.00 | 75.00 | 78.38 | 21.62 | ||||
| Sexual exposure | 0.000 | 0.197 | 0.000 | |||||||
| No | 62.19 | 37.81 | 25.12 | 74.88 | 91.54 | 8.46 | ||||
| Yes | 52.38 | 47.62 | 25.00 | 75.00 | 79.17 | 20.83 | ||||
| Prefer not to say | 30.36 | 69.64 | 14.29 | 85.71 | 91.07 | 8.93 | ||||
| Condom use | 0.014 | 0.141 | 0.090 | |||||||
| Never | 65.75 | 34.25 | 32.88 | 67.12 | 89.50 | 10.50 | ||||
| Sometimes | 54.37 | 45.63 | 22.33 | 77.67 | 80.58 | 19.42 | ||||
| Always | 46.15 | 53.85 | 26.92 | 73.08 | 86.54 | 13.46 | ||||
| Child | 0.038 | 0.524 | 0.057 | |||||||
| Yes | 38.71 | 61.29 | 19.35 | 80.65 | 77.41 | 22.58 | ||||
| No | 57.65 | 42.35 | 24.37 | 75.63 | 88.74 | 11.26 | ||||
| Type of institution | 0.000 | 0.000 | 0.728 | |||||||
| Government | 63.68 | 36.32 | 29.10 | 70.90 | 87.81 | 12.19 | ||||
| Private | 44.55 | 55.45 | 14.55 | 85.45 | 88.64 | 11.36 | ||||
| Other | 25.00 | 75.00 | 50.00 | 50.00 | 100.00 | 0 | ||||
| Educational background | 0.075 | 0.029 | 0.813 | |||||||
| Student (MBBS) | 57.59 | 42.40 | 27.75 | 72.25 | 90.05 | 9.95 | ||||
| Student (BDS) | 54.92 | 45.08 | 19.67 | 80.33 | 87.70 | 12.30 | ||||
| Doctor (MBBS) | 63.80 | 36.20 | 29.45 | 70.55 | 87.12 | 12.88 | ||||
| Dentist (BDS) | 49.33 | 50.67 | 17.33 | 82.67 | 87.33 | 12.66 | ||||
Values are presented as %. The bold type is considered statistically significant.
HPV, human papillomavirus; MBBS, Bachelor of Medicine, Bachelor of Surgery; BDS, Bachelor of Dental Surgery.
Fig. 1. A bar chart showing the status of knowledge based on the types of institutions and educational backgrounds of the participants. MBBS, Bachelor of Medicine, Bachelor of Surgery; BDS, Bachelor of Dental Surgery.
In multivariate logistic regression model, we included all the potential variables from the bivariate analysis. With this analysis, we incorporated the adjusted results and showed them in Table 5. Multiple logistic regression also showed that in case of type of institution, participants who studied in private institutions have more knowledge (odds ratio [OR], 2.04) than who studied in government institutions (95% CI, 1.23–3.36; p=0.005). Also, participants aged between 26 to 30 years had more knowledge (OR, 1.75) about HPV and its vaccination than other age groups (95% CI, 1.015–3.018; p=0.044). Here in terms of attitude, females showed more positivity towards HPV vaccination (OR, 2.89) than males (95% CI, 1.68–4.97; p=0.000), and additionally, students from private institutions had more positive attitude than students from government institutions (95% CI, 2.13–8.88; p=0.000). The associations have been shown in the following bar chart (Fig. 2). In vaccination history and practice, married female participants had higher tendencies for good practice (OR, 2.47) than males, with a 95% CI (1.14–11.70; p=0.029 and 1.18–5.18; p=0.016, respectively).
Table 5. Multivariate logistic regression of HPV and HPV vaccine knowledge, attitude, and practices.
| Variable | Adjusted OR (95% CI) | p-value | |
|---|---|---|---|
| HPV and HPV vaccine knowledge | |||
| Age (yr) | |||
| <25 | Ref | ||
| 26–30 | 1.724 (1.003–2.965) | 0.049 | |
| 31–35 | 2.406 (0.394–14.697) | 0.342 | |
| >36 | 0.767 (0.025–23.419) | 0.879 | |
| Gender | |||
| Male | Ref | ||
| Female | 0.904 (0.56–1.46) | 0.681 | |
| Institutions | |||
| Government | Ref | ||
| Private institution | 1.959 (1.196–3.208) | 0.008 | |
| Other institutions | 2.156 (0.08–58.136) | 0.648 | |
| Attitude towards HPV vaccination | |||
| Gender | |||
| Male | Ref | ||
| Female | 2.895 (1.684–4.978) | 0.00 | |
| Marital status | |||
| No | Ref | ||
| Yes | 0.655 (0.262–1.638) | 0.366 | |
| Institution type | |||
| Government | Ref | ||
| Private institution | 4.361 (2.14–8.888) | 0.00 | |
| Educational background | |||
| Student (MBBS) | Ref | ||
| Dental (Student) | 2.121 (0.955–4.711) | 0.065 | |
| Doctor (MBBS) | 0.959 (0.41–2.245) | 0.924 | |
| Dentist (BDS) | 1.312 (0.562–3.06) | 0.53 | |
| Practice of HPV and its vaccination | |||
| Gender | |||
| Male | Ref | ||
| Female | 2.533 (1.22–5.258) | 0.013 | |
| Marital status | |||
| Single | Ref | ||
| Married | 3.536 (1.112–11.244) | 0.032 | |
| Institution type | |||
| Government | Ref | ||
| Private | 1.037 (0.524–2.053) | 0.917 | |
The old type is considered statistically significant.
HPV, human papillomavirus; OR, odds ratio; CI, confidence interval; Ref, reference; MBBS, Bachelor of Medicine, Bachelor of Surgery; BDS, Bachelor of Dental Surgery.
Fig. 2. Participants’ attitude towards human papillomavirus vaccination, based on the gender and their educational backgrounds.
Discussion
To our best knowledge, this is the first and only study that took place in Bangladesh to evaluate the knowledge level about HPV and anti-HPV vaccine among the medical students and graduates, to understand the nature of their attitudes towards vaccine, and to corelate the knowledge and attitude levels to their intentions and practices. Bangladesh is a low-middle income country with 18 million school-going children, where 50.9% are female, belong to the 6–13 years age group [25]. A step was initially taken to introduce the HPV vaccine to the nationwide immunization program and mandate it for the school going girls between 9 to 13 years of age to prevent the risk of cervical cancer among women in the future [19]. However, the introduction and implementation of the HPV vaccination program raised multiple ethical concerns. Social stigma and conservativeness about the route of transmission of HPV, lack of knowledge about cervical cancer in the general population, and lack of proper information providers (such as teachers, healthcare providers) were the main reasons for HPV vaccination program being oversighted. Moreover, lack of knowledge about the vaccine efficacy among the vaccine providers and medical professionals was also a significant point [19].
Many studies conducted in developed countries revealed that general people, especially the parents of teenagers, believe lack of guidance and vaccine recommendations from the healthcare providers are the main reasons for being ignorant to vaccinate their children against HPV [26]. To overcome this situation, priority should be given to the healthcare facilitators to train and educate them about HPV and its vaccine. So, before appraising this target it is mandatory to evaluate the knowledge, attitude, and practice standards among the healthcare providers first.
Our study represents the status of knowledge, attitude, and practices regarding HPV and its’ vaccination among the young doctors, dentists, and medical students of Bangladesh, where only 43.29% of the respondents were knowledgeable enough about the HPV infections and its’ vaccination. Comparing to other similar researches conducted in Malaysia and South West Nigeria, our study showed quite low knowledge level, as 62.9% and 67.1% of medical students in both the mentioned countries were well-versed about the HPV and its vaccine, respectively [27,28]. Previously two cross-sectional surveys were performed in our country that evaluated the HPV knowledge among the midlife women of rural and urban areas, and the knowledge outcomes were really poor. They considered these findings as the barrier to cervical cancer screening and HPV vaccine acceptance [20,21]. So, the HPV vaccination programs can be hampered in our country due to the knowledge gap that has been discovered in our study and also in previous researches. The study participants’ (such as doctors, dentists, medical students) knowledge of HPV is crucial, influencing their recommendations to the general public, thus impeding the acceptance of the HPV vaccination. Educational initiatives are highly recommended here to enhance their understanding of HPV infection and vaccinations.
Attitude towards HPV vaccination is very remarkable as it indicates medical personnel’s points of view during their practices and recommendations of the vaccine to the healthcare receivers. The young and future professionals’ positive attitudes and good practices can increase awareness and vaccine acceptance among the general population. In our study, the percentage of the participants with positive attitudes was higher than their knowledge and practice standards. More than 70% of the respondents showed a positive attitude, with 96.81% of them were willing to recommend the vaccine to the patients. Approximately 80% of the participants consider HPV a deadly one, and almost all of them accepted that education on HPV can be beneficial to minimize the negligence about its outcome and preventive vaccine measures. Additionally, most of the answerers mentioned their interests in participating in HPV training programs. One significant finding of the vaccine recommendation in our study was that more than 90% of the respondents think vaccination should be mandatory for teenagers irrespective of gender. This indicates that young health professionals are well informed about the vaccination plan for males along with the females. They also believe the anti-HPV vaccine is well effective and safe. From the bivariate analysis that we have done in our study, female participants showed more positive attitudes than males. This was expected because most of the female physicians are usually concerned about cervical cancer and previous studies showed almost similar outcomes [29]. An important finding from our bi-variate analysis was that the prevalence of positive attitude was highest among dentists and dental students. The possible reason might be the additional importance of the relationship between the HPV and oropharyngeal carcinoma in their educational curriculum and medical practices [30]. Therefore, students and graduates from private institutions appeared to be more positive towards the HPV vaccine than other institutions.
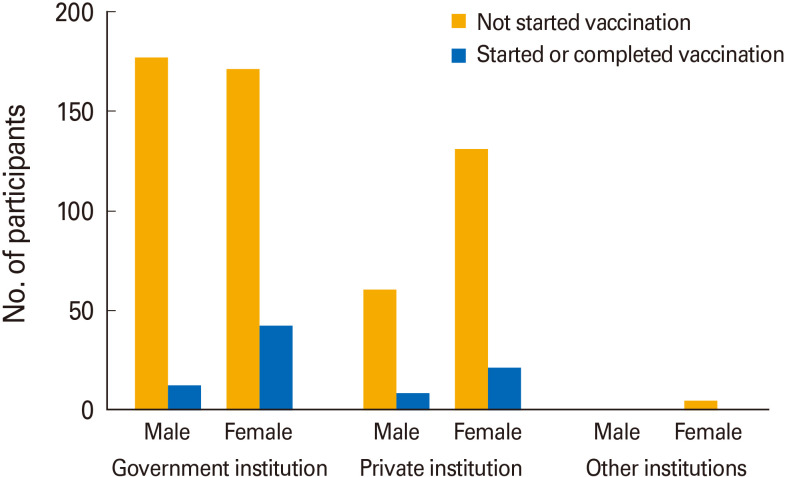
Poor practices of HPV vaccine were observed in our study (nearly 90%) as only 83 participants have taken the vaccine or started the vaccine course. Moreover, most of the vaccinated participants are female (Fig. 3). According to our study findings, 80% of respondents generally encourage patients to take the anti-HPV vaccine. This finding is significantly higher than the other studies conducted in Turkey and Ghana [31,32]. Lastly, only around 10% of our study respondents had the opportunity to participate in training sessions on HPV, which is substandard.
Fig. 3. The bar chart showing vaccination status among male, female and based on the types of institutions they belong.
So, our study was well structured and nationally representative as we took the information of both students and fresh graduates from all types of medical and dental institutions of the country. Lack of representativeness of different groups can be considered our limitations as the number of female participants was higher than the male participants, and participation from military schools was very few. Finally, we can conclude that HPV knowledge was poor to average among the population we studied and poor practices were observed regarding vaccination. Although, positive attitudes towards HPV education, training programs and vaccine recommendations have been spotted as exceptional. Our recommendation is to initiate major educational and training programs on HPV in all over country’s medical institutions to increase awareness against HPV and vaccine acceptance. Young and future healthcare providers’ good knowledge, positive attitudes, and intentions concerning HPV and its vaccines may be useful in guiding the general population and making the vaccine delivery programs nationwide successful.
Footnotes
No potential conflict of interest relevant to this article was reported.
We would like to thank Dr. Anannya Roy, Nirupoma Das, Mahzabeen Islam, Md. Shahidur Rahman, Chowdhury Mohammad Omar, Dipa Dev for their tremendous efforts in data collection. A short technical support was provided by the Public Health Professional Development Society (PPDS) to conduct this survey.
References
- 1.Centers for Disease Control and Prevention. Human papillomavirus (HPV) is the most common sexually transmitted infection (STI) in the United States: HPV vaccines can prevent some of the health effects HPV causes [Internet] Atlanta (GA): Centers for Disease Control and Prevention; 2021. [cited 2021 Sep 10]. Available from: https://www.cdc.gov/std/hpv/stdfact-hpv.htm . [Google Scholar]
- 2.Centers for Disease Control and Prevention. Genital HPV infection: CDC Fact Sheet [Internet] Atlanta (GA): Centers for Disease Control and Prevention; 2017. [cited 2021 Sep 10]. Available from: https://www.cdc.gov/std/hpv/hpv-Fs-July-2017.pdf . [Google Scholar]
- 3.Akhtar M. Human papillomavirus: the disease and prevention strategies. Ann Saudi Med. 2004;24:2–5. doi: 10.5144/0256-4947.2004.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.D’Souza G, Kreimer AR, Viscidi R, et al. Case-control study of human papillomavirus and oropharyngeal cancer. N Engl J Med. 2007;356:1944–1956. doi: 10.1056/NEJMoa065497. [DOI] [PubMed] [Google Scholar]
- 5.Gillison ML, Koch WM, Capone RB, et al. Evidence for a causal association between human papillomavirus and a subset of head and neck cancers. J Natl Cancer Inst. 2000;92:709–720. doi: 10.1093/jnci/92.9.709. [DOI] [PubMed] [Google Scholar]
- 6.Gillison ML, Shah KV. Human papillomavirus-associated head and neck squamous cell carcinoma: mounting evidence for an etiologic role for human papillomavirus in a subset of head and neck cancers. Curr Opin Oncol. 2001;13:183–188. doi: 10.1097/00001622-200105000-00009. [DOI] [PubMed] [Google Scholar]
- 7.Shaikh MH, Khan AI, Sadat A, et al. Prevalence and types of high-risk human papillomaviruses in head and neck cancers from Bangladesh. BMC Cancer. 2017;17:792. doi: 10.1186/s12885-017-3789-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bruni L, Albero G, Serrano B, et al. Human papillomavirus and related diseases in the world: summary report. Barcelona: ICO/IARC Information Centre on HPV and Cancer; 2019. [Google Scholar]
- 9.Miralles-Guri C, Bruni L, Cubilla AL, Castellsague X, Bosch FX, de Sanjose S. Human papillomavirus prevalence and type distribution in penile carcinoma. J Clin Pathol. 2009;62:870–878. doi: 10.1136/jcp.2008.063149. [DOI] [PubMed] [Google Scholar]
- 10.de Martel C, Ferlay J, Franceschi S, et al. Global burden of cancers attributable to infections in 2008: a review and synthetic analysis. Lancet Oncol. 2012;13:607–615. doi: 10.1016/S1470-2045(12)70137-7. [DOI] [PubMed] [Google Scholar]
- 11.Quinn S, Goldman RD. Human papillomavirus vaccination for boys. Can Fam Physician. 2015;61:43–46. [PMC free article] [PubMed] [Google Scholar]
- 12.Stewart J. Gardasil 9 FDA approval history [Internet] Auckland: Drugs.com; 2020. [cited 2021 Sep 10]. Available from: https://www.drugs.com/history/gardasil-9.html . [Google Scholar]
- 13.Gervais F, Dunton K, Jiang Y, Largeron N. Systematic review of cost-effectiveness analyses for combinations of prevention strategies against human papillomavirus (HPV) infection: a general trend. BMC Public Health. 2017;17:283. doi: 10.1186/s12889-017-4076-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vu LT, Bui D, Le HT. Prevalence of cervical infection with HPV type 16 and 18 in Vietnam: implications for vaccine campaign. BMC Cancer. 2013;13:53. doi: 10.1186/1471-2407-13-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Juntasopeepun P, Davidson PM, Srisomboon J. Issues and challenges in implementing cervical cancer screenings in the emergence of HPV vaccination in Thailand. Collegian. 2012;19:45–50. doi: 10.1016/j.colegn.2011.08.002. [DOI] [PubMed] [Google Scholar]
- 16.Chow SN, Soon R, Park JS, et al. Knowledge, attitudes, and communication around human papillomavirus (HPV) vaccination amongst urban Asian mothers and physicians. Vaccine. 2010;28:3809–3817. doi: 10.1016/j.vaccine.2010.03.027. [DOI] [PubMed] [Google Scholar]
- 17.Human papillomavirus vaccines: WHO position paper, May 2017. Wkly Epidemiol Rec. 2017;92:241–268. [PubMed] [Google Scholar]
- 18.World Health Organization. Vaccines and immunization: what is vaccination? [Internet] Geneva: World Health Organization; 2021. [cited 2021 Sep 10]. Available from: https://www.who.int/news-room/q-a-detail/vaccines-and-immunization-what-is-vaccination . [Google Scholar]
- 19.Salwa M, Abdullah Al-Munim T. Ethical issues related to human papillomavirus vaccination programs: an example from Bangladesh. BMC Med Ethics. 2018;19(Suppl 1):39. doi: 10.1186/s12910-018-0287-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Islam JY, Khatun F, Alam A, et al. Knowledge of cervical cancer and HPV vaccine in Bangladeshi women: a population based, cross-sectional study. BMC Womens Health. 2018;18:15. doi: 10.1186/s12905-018-0510-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Islam RM, Bell RJ, Billah B, Hossain MB, Davis SR. Lack of understanding of cervical cancer and screening is the leading barrier to screening uptake in women at midlife in Bangladesh: population-based cross-sectional survey. Oncologist. 2015;20:1386–1392. doi: 10.1634/theoncologist.2015-0235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Alsous MM, Ali A, Al-Azzam S, Karasneh R, Amawi H. Knowledge about cervical cancer and awareness about human papillomavirus vaccination among medical students in Jordan. Peer J. 2021;9:e11611. doi: 10.7717/peerj.11611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Villar LM, Rabello AD, de Paula VS. Evaluating knowledge about human papillomavirus infection among Brazilian health professionals. Asian Pac J Cancer Prev. 2011;12:3251–3256. [PubMed] [Google Scholar]
- 24.Kim HW. Awareness of human papillomavirus and factors associated with intention to obtain HPV vaccination among Korean youth: quasi experimental study. BMC Int Health Hum Rights. 2015;15:4. doi: 10.1186/s12914-015-0042-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.United States Agency for International Development. Female education in Bangladesh [Internet] Washington (DC): United States Agency for International Development; 2021. [cited 2021 Sep 10]. Available from: https://www.usaid.gov/bangladesh/education . [Google Scholar]
- 26.Lindley MC, Jeyarajah J, Yankey D, Curtis CR, Markowitz LE, Stokley S. Comparing human papillomavirus vaccine knowledge and intentions among parents of boys and girls. Hum Vaccin Immunother. 2016;12:1519–1527. doi: 10.1080/21645515.2016.1157673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rashwan HH, Saat NZ, Abd Manan DN. Knowledge, attitude and practice of Malaysian medical and pharmacy students towards human papillomavirus vaccination. Asian Pac J Cancer Prev. 2012;13:2279–2283. doi: 10.7314/apjcp.2012.13.5.2279. [DOI] [PubMed] [Google Scholar]
- 28.Adejuyigbe FF, Balogun MR, Sekoni AO, Adegbola AA. Cervical cancer and human papilloma virus knowledge and acceptance of vaccination among medical students in Southwest Nigeria. Afr J Reprod Health. 2015;19:140–148. [PubMed] [Google Scholar]
- 29.Riedesel JM, Rosenthal SL, Zimet GD, et al. Attitudes about human papillomavirus vaccine among family physicians. J Pediatr Adolesc Gynecol. 2005;18:391–398. doi: 10.1016/j.jpag.2005.09.004. [DOI] [PubMed] [Google Scholar]
- 30.Ozdede M, Bagci N, Gunduz T, Peker I. Evaluation of knowledge and awareness of dentists and dental students about human papillomavirus vaccination and oropharyngeal cancer relationship. Clin Exp Health Sci. 2020;10:309–315. [Google Scholar]
- 31.Kurtoglu E, Arpaci H, Temur M. Family physicians’ knowledge and attitudes about human Papillomavirus vaccine. J Clin Anal Med. 2013;4:132–135. [Google Scholar]
- 32.Agyei-Baffour P, Asare M, Lanning B, et al. Human Papillomavirus vaccination practices and perceptions among Ghanaian healthcare providers: a qualitative study based on multi-theory model. PLoS One. 2020;15:e0240657. doi: 10.1371/journal.pone.0240657. [DOI] [PMC free article] [PubMed] [Google Scholar]