Abstract
Objectives:
Given what little is known about the experiences of sexual and gender minority (SGM) caregivers of people with Alzheimer’s disease and related dementias (ADRD), the aim of the current study was to describe psychosocial measures among these caregivers.
Methods:
We used an online survey and social media recruitment strategies.
Results:
Of 286 caregivers, the majority were gay men. Most respondents were white, with a third identifying as Latino American. The plurality of caregivers identified as a spouse/partner and were providing care for someone who identified as a sexual minority; one-fifth cared for someone transgender. Sexual orientation, perceived stress, caregiver stigma, and microaggressions were psychosocial factors associated with family quality of life and depressive symptoms in the caregivers.
Discussion:
This study is the first to provide a focused description of the characteristics and psychosocial needs of SGM caregivers of someone with ADRD, supporting development of targeted interventions for this population.
Keywords: dementia, caregiver, sexual minority, gender minority
Background and Objectives:
The informal caregiving of older adults by sexual and gender minority (SGM; i.e., lesbian, gay, bisexual, and transgender) adults continues to receive limited attention (Muraco & Fredriksen-Goldsen, 2014). Current research rarely examines how caregiving for older adults affects the SGM population (McGovern, 2014). Yet a large proportion of SGM adults are caregivers, with estimates suggesting 27% to over 45% (Fredriksen-Goldsen & Hoy-Ellis, 2007) of SGM adults providing care for someone with a chronic illness. What little is known about SGM caregivers indicates that, compared with heterosexual caregivers, SGM caregivers experience higher levels of depression, disability, victimization, discrimination, and stress (Fredriksen, 1999; Fredriksen-Goldsen & Hoy-Ellis, 2007; Hash, 2001). These factors potentially increase the risk for poor health and quality of life. Additionally, SGM aging-care partnerships are often affected by stigma related to victimization and discrimination, which have a negative impact on health and wellbeing (Hulko, 2009; Jablonski et al., 2013; Price, 2008).
Almost half of all caregivers in the United States (48%) provide care for someone with Alzheimer’s disease and related dementias (ADRD) (Alzheimer’s Association, 2020). Caregivers of people with ADRD face emotional, financial, physical, and social challenges beyond those experienced by caregivers for those with other chronic conditions (Matthews, 2019). Health and quality of life of the general population of caregivers for people with ADRD show individual caregiver characteristics, such as those who experience chronic high stress, high caregiver demand, and have other chronic conditions, including psychiatric morbidities, often lead to poor caregiver health outcomes. Findings from a recent systematic review of factors associated with quality of life outcomes for caregivers of people with ADRD extended this earlier work and found that caregiver-care recipient relationship, living situation, support received, caregiver independence, and caregiver self-efficacy also were associated with quality of life outcomes for caregivers (Farina et al., 2017). However, the experiences and consequences of caring for someone with ADRD may not be the same across caregiving populations. The majority of currently available evidence about the experiences and health of caregivers is largely silent about the experiences of being SGM and caring for a person with ADRD. SGM caregivers of people with ADRD may be especially at risk for poor health and quality of life given the unique experiences of SGM people and how those experiences might intersect with caregiving. It remains unknown how these adverse experiences of the SGM caregiving population are associated with the psychosocial impact of providing care for someone with ADRD.
It is estimated that the number of U.S. adults over the age of 50 years old who self-identify as SGM will increase to 4 to 8 million by 2030 (Zanetos & Skipper, 2020). Compared with heterosexual older adults, SGM older adults ≥50 years old experience a higher prevalence of chronic disease and disability, as well as poorer physical and mental health (Fredriksen-Goldsen, 2016) and increased rates of depression and depressive symptoms (Hughes et al., 2014; Russell & Fish, 2016). SGM older adults (≥50 years old) in particular are more likely to experience mental distress and depression, receive counseling, and take psychiatric medications (Nelson & Andel, 2020). In recent years, this disparity in aging related to SGM identity has become increasingly acknowledged by the National Institutes of Health (National Institutes of Health, 2010), the National Academy of Medicine (NAM; formerly the Institute of Medicine; 2011), and leading organizations such as the Alzheimer’s Association and Services and Advocacy for GLBT Elders (SAGE; 2018).
Our recent analysis of data provided by the National Alliance for Caregiving found that SGM caregivers of older adults represent about 6% of caregivers and are significantly younger and more racially and ethnically diverse than their heterosexual counterparts (Anderson & Flatt, 2018). SGM caregivers are more often friends of their care recipients and more frequently help with medical nursing tasks (e.g., giving medications or injections, wound care, helping with incontinence, or operating medical equipment). We also found evidence of poorer health and psychosocial strain among SGM caregivers compared with heterosexual caregivers. SGM caregivers of older adults more frequently report higher levels of financial strain related to the caregiving role (Anderson & Flatt, 2018).
Within this previous sample (Anderson & Flatt, 2018), only 11% of SGM caregivers (n = 9) identified as providing care for someone with ADRD. While these are valuable preliminary findings, the small number of included respondents providing care for people with ADRD highlights the need for additional, focused research to explore more fully this under-investigated caregiver population given that large-scale, nationally representative studies surveying SGM older adults, such as the National Health, Aging, and Sexuality and Gender Study (NHAS; Fredriksen-Goldsen & Kim, 2017), do not focus on caregivers of people with ADRD, do not include psychosocial measures of the caregiving experience, and are often limited to SGM adults ≥50 years old. Given that a quarter of caregivers for people with ADRD are Millennials (Alzheimer’s Association, 2020) and younger generations are more diverse in terms of sexual orientation and gender identity (GLAAD, 2018), more comprehensive, focused data are critical to document and understand the SGM ADRD caregiving experience. Thus, the goal of the current study was to describe the psychosocial experiences and family quality of life among SGM caregivers of persons with ADRD.
This study was guided by the Health Equity Promotion Model (HEP; Fredriksen-Goldsen & Kim, 2017; Figure 1). This model highlights how the SGM population differs from others in terms of health disparities and is informed by the Stress Process Model (Pearlin et al., 1990), the Minority Stress Model (Meyer, 2003), and the Psychological Mediation Framework (Hatzenbuehler, 2009). Moreover, the HEP model is based on the concept of health equity and includes factors related to resiliency. The model considers inter- and intragroup variability and individual development across the life course, including structural and environmental determinants of health specific to the SGM population (historical and environmental context). As illustrated in Figure 1, social positions influence psychological, social, and behavioral concepts. These concepts (psychological, social, and behavioral) influence each other as well as aspects of health and well-being either directly or by moderating the effects of the historical and environmental context of SGM identity. The HEP model is designed to support the development of culturally responsive interventions by highlighting diversity within groups, such race and ethnicity, age, SGM identity, and geographic location. In so doing, explanatory factors that contribute to these subgroup differences and the intersectionality of identity are considered. Currently, there are no published theoretical models for SGM caregivers. Therefore, the HEP model was used given that it takes into account several stress-related models used to guide previous caregiving research (Hatzenbuehler, 2009; Meyer, 2003; Pearlin et al., 1990) and is specifically designed for use among SGM adults (Fredriksen-Goldsen & Kim, 2017).
Figure 1.
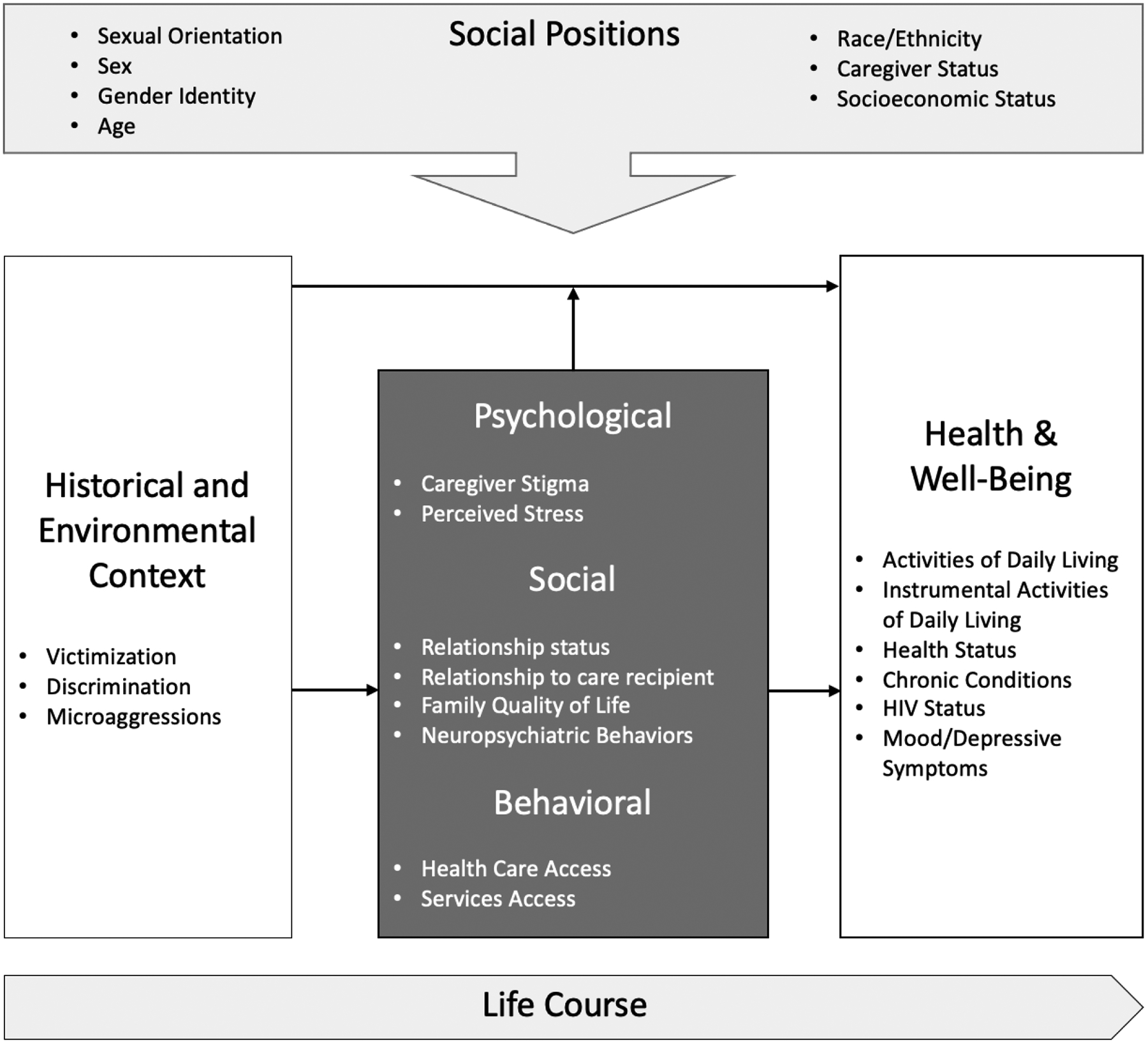
Concepts of the Health Equity Promotion Model (Adapted from Fredriksen-Goldsen et al., 2014).
The Health Equity Promotion model is based on the concept of health equity and includes factors related to resiliency. The model considers inter- and intragroup variability and individual development across the life course, including structural and environmental determinants of health specific to the sexual and gender minority population (historical and environmental context). Characteristics related to social position influence psychological, social, and behavioral concepts. These concepts (psychological, social, and behavioral) affect each other as well as aspects of health and well-being either directly or by moderating the impact of the historical and environmental context of sexual and gender minority identity. Variables and measures assessed in the present study for each concept are delineated in the figure.
Research Design and Methods
Study Sample
SGM adults ≥18 years old who identified as a family caregiver or a caregiving, non-relative for a person with ADRD were eligible to participate in the study. We defined caregivers as those who self-reported assisting and attending to the needs of an adult with ADRD at least 8 hours a week on average. We used the Ascertain Dementia 8-Item Informant Questionnaire (AD8) to confirm self-reported caregiver status. The AD8 is sensitive to detecting cognitive changes related to ADRD (Galvin et al., 2006) and is used in the National Health and Aging Trends Study as a proxy report of ADRD diagnosis (Kasper et al., 2013). The scale consists of eight items assessing changes in cognition (thinking and memory) with responses of yes, no, or don’t know. Scores range from 0 to 8, with a score of ≥2 indicative of likely cognitive impairment. In the present sample, the Cronbach’s α for the AD8 was 0.77. The study design and procedures were approved by the Institutional Review Board.
Data Collection
Potential participants were recruited via social media (i.e., Facebook and Twitter) through posts targeted toward SGM adults, as well as posts targeted to the social media feeds for research and service organizations and groups (e.g., Services and Advocacy for GLBT Elders [SAGE] or the Fenway Institute) specific to SGM adults, a strategy used successfully by the NHAS (Fredriksen-Goldsen & Kim, 2017) and other studies of the SGM population (Glick & Golden, 2014; Martinez et al., 2014). Study information also was posted on the social media accounts of other aging and ADRD researchers known to the research team and in organizational newsletters, including the regional chapters of the Alzheimer’s Association, and the online forums of the Rainbow Research and Family Caregiving Interest Groups of the Gerontological Society of America. Additionally, study information was posted on the research registries of the Family Caregiver Alliance and the Alzheimer’s Association.
Study-related posts included a link to an electronic survey housed on a HIPAA-secured survey platform. When potential participants clicked the link to the survey, they were directed to a landing page describing the study and presenting an alteration of consent (i.e., consent implied by completing the survey). Participants received a $25 electronic Amazon gift card for completing the survey. Items and instruments included in the electronic survey represented concepts of the HEP Model (Figure 1). The survey took roughly 40 minutes (38.8 ± 16.6) to complete based on clickstream data collected by the survey platform. The study landing page was viewed 2554 times. A total of 483 individuals started the survey. We used casewise deletion to address missing data related to incomplete responses (i.e., those individuals who did not complete the full survey). This resulted in a total sample of 286 participants with complete data.
Demographic Items
Demographic characteristics related to social position within the HEP Model included sexual orientation, transgender-inclusive gender identity, age (years), race, ethnicity, highest level of education, income, difficulty in affording the basics, employment status, living location, caregiver status (described above), and number of months in the caregiving role. Respondents’ sexual orientation was assessed with a sexual identity measure where response options were as follows: gay, lesbian, bisexual, or specifying their identity if not listed (referred to as queer in this paper). Gender identity was assessed in response to the question “Which of the following best represents how you currently think of your gender?” (woman, man, not listed [please specify]). Transgender identity was determined in response to the question “Do you consider yourself to be trans/transgender?” (yes, no). Responses to racial identity included White, African American/Black, Native American/Alaska Native, Asian, Pacific Islander/Native Hawaiian, other, don’t know, or refuse to answer. Ethnicity was ascertained by responses to the question “Do you consider yourself to be of Hispanic/Latino American origin, such as Mexican, Puerto Rican, Cuban or other Spanish background?” (yes, no).
Level of education was based on the highest grade or year of school completed. Difficulty in affording basic living essentials was assessed by responses to the question “How hard is it for you to pay for the very basics like food, housing, medical care, and heating?” (not difficult at all, not very difficult, somewhat difficult, very difficult). Living location was captured by zip code and description. Region corresponded to the four U.S. regions recognized by the Census Bureau (Northeast, North Central/Midwest, South, West; National Center for Health Statistics, 2017).
Historical and Environmental Context of SGM Identity
Survey items related to the historical and environmental context of SGM identity within the HEP Model included measures from the NHAS assessing lifetime victimization, lifetime and day-to-day discrimination, and microaggressions, which have established reliability and validity (Fredriksen-Goldsen & Kim, 2017). Lifetime victimization was ascertained using nine questions that asked respondents to indicate how many times in their life they experienced victimization because of their SGM identity using a Likert-type response (never, once, twice, three or more times). Total scores range from 9 to 36, with higher scores indicating more experiences of lifetime victimization. The Cronbach’s α in the present sample for this victimization scale was 0.86. Lifetime (five questions) and day-to-day discrimination (six questions) asked respondents to report how many times in their lifetime and day-to-day life they experienced discrimination because of their SGM identity using a Likert-type response (never, once, twice, three or more times). Total scores for the lifetime discrimination scale range from 5 to 20 and from 6 to 24 for the day-to-day discrimination scale. Higher scores represent more experiences of lifetime and day-to-day discrimination. In the present sample, the Cronbach’s α for the lifetime discrimination measure was 0.79 and 0.86 for the day-to-day discrimination measure. Microaggressions were assessed with eight questions asking respondents to identify how many times in the past 12 months they experienced microaggressions related to their SGM identity using a Likert-type response (never, once, twice, three or more times). Scores range from 8 to 32, with higher scores indicative of experience more frequent microaggressions. The Cronbach’s alpha in the present sample was 0.87.
Psychological Factors
Psychological factors within the HEP Model included caregiver stigma and stress. The Caregiver Stigma Impact Scale includes 24 items representing four aspects of the stigma experience: social rejection, financial insecurity, internalized shame, and social isolation (Burgener & Berger, 2008). Total scores can range from 24 to 120, with higher scores indicating higher levels of caregiver stigma. The Caregiver Stigma Impact Scale has established reliability and validity (Burgener & Berger, 2008). The Cronbach’s α in the present sample was 0.92. The Perceived Stress Scale is a 10-item scale assessing perceived stress by asking persons to rate how often they felt or thought a certain way (described by the item stem) in the past month. Total scores can range from 0 to 40. Higher scores indicate higher levels of perceived stress (low stress = ≤13; moderate stress = 14–26; high stress ≥27). The Perceived Stress Scale has established reliability and validity (Cohen et al., 1983). In the present sample, the Cronbach’s α for the Perceived Stress Scale was 0.79.
Social Factors
Social factors within the HEP Model included the caregiver’s relationship status and their relationship to the person with ADRD. Social factors also included family quality of life and the impact of neuropsychiatric symptoms exhibited by the person with ADRD. The Family Quality of Life in Dementia Scale is a 41-item scale designed to assess family quality of life in families caring for someone with ADRD. Individual items are rated on a 4-point, Likert-type scale generating a total score (range 41 to 205), with higher scores indicating higher levels of family quality of life. The scale has high internal consistency (Cronbach’s α = 0.95) and validity (Rose et al., 2020). The Cronbach’s α in the present sample was 0.96. The Neuropsychiatric Inventory Questionnaire is a caregiver-reported measure providing information on presence and severity of behaviors (agitation, aggression, anxiety, irritability, aberrant motor behaviors, disrupted sleep) in people with ADRD. Caregivers rate each of the 12 behaviors as present or absent in the previous month and, if present, the severity and level of distress experienced by the caregiver. Higher scores indicate increased levels of severity (score range 0 to 36) and distress (score range 0 to 60). Reliability and validity are established (Kaufer et al., 2000). The Cronbach’s α in the present sample was 0.90.
Behavioral Factors
Behavioral factors within the HEP Model included aspects of health care access, including insurance status and distance to and source of emergency care. The use of caregiving services was included among the behavioral factors. The use of these services and resources (financial, respite, transportation, paid care, home modifications) were adapted from the Caregiving in the U.S. survey (National Alliance for Caregiving, 2017).
Health and Well-being
Factors related to health and well-being within the HEP Model included measures related to the caregiver and the person with ADRD. Caregiver health items included health status, HIV status, presence of chronic health conditions, and mood/depressive symptoms. Caregiver health status was ascertained using the PROMIS Global Health Scale. This 10-item scale assesses global health, which is a person’s evaluation of overall health rather than a specific aspect of health. Items include ratings of five primary domains (physical function, fatigue, pain, emotional distress, social health) and general health perceptions (Cella et al., 2010). Raw scores can range from 16 to 68. A score ≥29 on the Global Health Scale represents average or better health (Cella et al., 2010). In the present sample, the Cronbach’s α for the Global Health Scale was 0.86.
Chronic conditions included self-reported diagnosis (yes, no, or prefer not to answer) of each of the following conditions: cardiovascular disease, coronary artery disease, cancer, diabetes, hypertension, pulmonary disease, neurodegenerative disease, autoimmune disease, fibromyalgia, or arthritis. The presence of depressive symptoms was assessed using the Centers for Epidemiological Studies Depression Scale (CES-D). This 20-item, self-administered questionnaire is designed to quantify current depressive symptoms (Radloff, 1977). Each item uses a 4-point, Likert-type scale; total scores can range from 0 to 60. Probable depression is indicated by scores ≥16. The Cronbach’s α in the present sample was 0.85.
For the person with ADRD included Activities of Daily Living (ADLs) and Instrumental Activities of Daily Living (IADLs). The Activities of Daily Living Scale is a 6-item scale that assesses functional ability (Katz et al., 1963). Total counts can range from 0 to 6, with higher counts indicating increased dependence. The Instrumental Activities of Daily Living Scale includes eight items to assess independent living skills considered more complex than ADLs (Lawton & Brody, 1969). Total scores can range from 0 to 8, with higher scores indicating higher levels of independence.
Data Analyses
We used SPSS version 25 for all data analyses. Prior to analysis, data were reviewed for completeness and accuracy, as well as skewness and kurtosis for continuous variables. Continuous variables were normally distributed, except for the number of caregiving months. Caregiving months was log-transformed before entering it into the regression models. The level of significance for statistical tests was set at p < 0.05. Descriptive statistics for the sample were calculated, including means and standard deviations for continuous variables and frequencies and percentages for categorical variables. Analyses of variance and independent t-tests were used to assess differences in scale scores by sexual orientation (LGBQ) and gender identity (cisgender, transgender), respectively.
Hierarchical multiple regression analyses were conducted to examine the associations between environmental, psychological, social, behavioral, and health factors and caregiver measures of family quality of life, neuropsychiatric severity, and mood/depressive symptoms (dependent variables). Independent variables included sexual orientation, transgender identity, caregiver stigma, perceived stress, day-to-day discrimination, and microaggressions. Covariates included age, race, ethnicity, income, living location, presence of chronic conditions among caregivers, relationship to the care recipient, and caregiving time. Ordinary least squares regression models were used for each dependent variable. Variance explained was expressed as Nagelkerke’s R2. There was no evidence of considerable multicollinearity between model parameters. Demographic and caregiving variables of age, race, ethnicity, income, presence of chronic conditions among caregivers, relationship to the care recipient, and caregiving time were entered in block one. To understand the unique impact of sexual orientation and transgender identity, these variables were entered in block two. Psychosocial measures related to caregiver stigma, perceived stress, day-to-day discrimination, and microaggressions were entered in block three.
Results
Demographic characteristics of the sample are reported in Table 1. Caregivers in the sample ranged in age from 21 to 72 years old (mean = 37.4 ± 8.6 years). Millennial caregivers (≤38 years old) made up 58.7% of the sample, with those part of Generation X (39–54 years old) representing 36.4% and Baby Boomers 4.9% (≥55 years old). Gay men made up the majority (43.0%) of the sample; however, the sample consisted of fairly even numbers of those who identified as female (47.9%) and male (51.4%). A little more than one tenth (13.3%) of the sample identified as transgender. The sample mostly identified as White (79.4%), though roughly one-third (36.0%) identified as Latino American. A plurality of the sample was college-educated (45.5%), married or partnered (55.9%), and employed full or part-time (90.9%). Approximately half of the sample (54.9%) reported an income ≥$50,000. Despite the relatively high levels of income, nearly one-third (32.1%) reported difficulty in paying for everyday basics. While most lived in an urban/suburban setting, one-third (32.8%) reported living in a small town or rural area. Respondents living in Western states were the most represented (46.9%). Nearly all (99.3%) respondents had health insurance. The majority of caregivers (81.5%) reported a negative HIV status, though roughly ten percent (9.4%) reported not knowing their HIV status.
Table 1.
Demographic characteristics of the sample
| Characteristic | N = 286 |
|---|---|
| Age (years) | 37.4 ± 8.6 |
| Gender identity (caregiver) | |
| Female | 137 (47.9%) |
| Male | 147 (51.4%) |
| Other | 2 (0.7%) |
| Sexual orientation (caregiver) | |
| Gay | 123 (43.0%) |
| Lesbian | 38 (13.3%) |
| Bisexual | 56 (19.6%) |
| Queer/pansexual/other | 69 (24.1%) |
| Transgender (caregiver) | |
| Yes | 38 (13.3%) |
| No | 248 (86.7%) |
| Race | |
| White | 227 (79.4%) |
| African American | 29 (10.1%) |
| Native American/Alaska Native | 20 (7.0%) |
| Asian/Pacific Islander/Other | 10 (3.5%) |
| Latino American | |
| Yes | 103 (36.0%) |
| No | 183 (64.0%) |
| Years of education | |
| 7–11 years | 3 (1.0%) |
| High school graduate | 73 (25.5%) |
| Some college | 80 (28.0%) |
| College graduate | 106 (37.1%) |
| Post-graduate | 24 (8.4%) |
| Partner status | |
| Never married | 92 (32.2%) |
| Married/partnered | 160 (55.9%) |
| Widowed | 12 (4.2%) |
| Divorced | 8 (2.8%) |
| Separated | 14 (4.9%) |
| Employment status | |
| Employed full time | 190 (66.4%) |
| Employed part time | 70 (24.5%) |
| Homemaker, not currently working for pay | 8 (2.8%) |
| Retired | 8 (2.8%) |
| Unemployed | 10 (3.5%) |
| Insurance coverage type | |
| Public | 138 (48.3%) |
| Private | 136 (47.6%) |
| Military | 10 (3.5%) |
| Uninsured | 2 (0.7%) |
| Emergency care | |
| Type of emergency care | |
| Nurse practitioner | 54 (18.9%) |
| Urgent care | 13 (4.5%) |
| Physician’s office | 25 (8.7%) |
| Hospital | 161 (56.3%) |
| Pharmacy/Minute Clinic | 33 (11.5%) |
| Miles to closest emergency care | 16.9 ± 23.1 |
| Time to closest emergency care (minutes) | 28.6 ± 27.3 |
| Household income | |
| ≤$10,000 | 3 (1.0%) |
| $10,001-$20,000 | 13 (4.5%) |
| $20,001-$30,000 | 32 (11.2%) |
| $30,001-$40,000 | 39 (13.6%) |
| $40,001-$50,000 | 42 (14.7%) |
| $50,001-$60,000 | 32 (11.2%) |
| $60,001-$70,000 | 72 (25.2%) |
| >$70,000 | 53 (18.5%) |
| Difficulty in paying for everyday basics? | |
| Not difficult at all | 86 (30.1%) |
| Not very difficult | 108 (37.8%) |
| Somewhat difficult | 87 (30.4%) |
| Very difficult | 5 (1.7%) |
| Region | |
| Northeast | 31 (10.8%) |
| North Central/Midwest | 41 (14.3%) |
| South | 80 (28.0%) |
| West | 134 (46.9%) |
| Living location | 31 (10.8%) |
| Farm or ranch | 4 (1.4%) |
| Rural area | 22 (7.7%) |
| Small rural town | 23 (8.0%) |
| Small town | 45 (15.7%) |
| Medium-sized city | 47 (16.4%) |
| Large city | 83 (29.0%) |
| Suburban area | 36 (12.6%) |
| Major metropolitan area | 26 (9.1%) |
| HIV status (caregiver) | |
| Negative | 233 (81.5%) |
| Positive | 22 (7.7%) |
| Don’t know | 27 (9.4%) |
| Prefer not to answer | 4 (1.4%) |
| Chronic conditions* | |
| No chronic conditions | 197 (67.2%) |
| At least one chronic condition | 96 (32.8%) |
Note: Chronic conditions included cardiovascular disease, coronary artery disease, cancer, diabetes, hypertension, pulmonary disease, neurodegenerative disease, autoimmune disease, fibromyalgia, and arthritis
Description of Caregiving
Caregiving characteristics of the sample are reported in Table 2. The average time spent providing care was approximately two years (27.4 ± 17.1 months) and ranged from two months to ten years. A plurality of the sample did not live with their care recipient (53.1%) and identified as the spouse or partner (50.0%) of the person with ADRD. However, nearly one in ten (9.8%) was an unrelated friend or neighbor. Most caregivers reported caring for someone who identified as male (54.2%) and one in five (19.9%) reported caring for someone who identified as transgender. Over one-third (37.4%) reported caring for someone who identified as heterosexual/straight. The majority of caregivers reported requesting information about how to get financial help for a person with memory loss (80.4%) or making modifications to the home where the person with memory loss lived (57.3%). Half of the sample reported not using respite services (53.8%) or transportation services (52.8%). The majority reported health care providers asking if they needed help caring for the person with ADRD (66.1%) or taking care of themselves (58.0%).
Table 2.
Caregiving characteristics of the sample
| Characteristic | N = 286 |
|---|---|
| Number of months in the caregiving role | 27.4 ± 17.1 |
| Living with person with memory loss | |
| Yes | 134 (46.9%) |
| No | 152 (53.1%) |
| Relationship to the person with memory loss | |
| Spouse/partner | 143 (50.0%) |
| Daughter | 37 (12.9%) |
| Son | 33 (11.5%) |
| Other relative | 40 (14.0%) |
| Friend/neighbor | 28 (9.8%) |
| Parent | 5 (1.7%) |
| Gender identity (care recipient) | |
| Female | 130 (45.5%) |
| Male | 155 (54.2%) |
| Other | 1 (0.3%) |
| Transgender (care recipient) | |
| Yes | 57 (19.9%) |
| No | 229 (80.1%) |
| Sexual orientation (care recipient) | |
| Gay | 119 (41.6%) |
| Lesbian | 52 (18.2%) |
| Bisexual | 6 (2.1%) |
| Straight/heterosexual | 107 (37.4%) |
| Other | 2 (0.7%) |
| Requested information about how to get financial help for the person with memory loss | |
| Yes | 230 (80.4%) |
| No | 56 (19.6%) |
| Used respite services | |
| Yes | 132 (46.2%) |
| No | 154 (53.8%) |
| Had an outside service provide transportation for the person with memory loss | |
| Yes | 135 (47.2%) |
| No | 151 (52.8%) |
| Had modifications made in the house or apartment where the person with memory loss lives/lived | |
| Yes | 164 (57.3%) |
| No | 122 (42.7%) |
| Had a health care provider ask you about what you need/needed to help care for the person with memory loss | |
| Yes | 189 (66.1%) |
| No | 97 (33.9%) |
| Had a health care provider ask you what you need/needed to take care of yourself | |
| Yes | 166 (58.0%) |
| No | 120 (42.0%) |
Psychosocial Measures
Mean scores of psychosocial measures are reported in Table 3 and correlations are reported in Table 4. The mean score for the sample in terms of the Global Health Scale (30.2 ± 7.2) was equivalent to an average health status; however, a third of the sample (36.4%) reported a below average health status, with lesbian and transgender participants reporting a significantly lower health status (Table 3). In terms of discrimination, victimization, and microaggressions, those caregivers who identified as queer had significantly higher scores on each of these measures, while transgender caregivers reported significantly lower scores (Table 3). The sample mean on the Perceived Stress Scale (17.8 ± 6.5) was indicative of moderate stress, with nearly three-quarters of the sample (73.4%) reporting moderate or high levels of stress and bisexual and queer caregivers reporting significantly higher stress scores (Table 3). Transgender caregivers reported significantly lower stress scores compared with their cisgender counterparts. Neuropsychiatric symptom distress scores were significantly higher among bisexual and queer caregivers and significantly lower among transgender caregivers (Table 3). Gay caregivers reported the highest levels of caregiver stigma, while lesbian and transgender caregivers reported significantly lower scores (Table 3). Queer caregivers reported significantly lower family quality of life scores, while transgender caregivers reported significantly higher scores on this measure. The majority of caregivers (78.0%) scored above the cutoff indicative of probable depression (≥16) on the CES-D, with queer caregivers reporting significantly higher scores and transgender caregivers significantly lower scores (Table 3). There was a significant difference in depression scores by race, with African American/Black SGM caregivers reporting higher levels of depression (27.3 ± 1.8) than White SGM caregivers (22.8 ± 0.6; F = 4.6, p = 0.03).
Table 3.
Mean scale scores (± standard deviations) by sexual orientation and gender identity
| Scale | Sexual orientation | P-value | Gender Identity | P-value | ||||
|---|---|---|---|---|---|---|---|---|
| Gay (n = 123) | Lesbian (n = 38) | Bisexual (n = 56) | Queer (n = 69) | Cisgender | Transgender | |||
| Alzheimer’s Disease Questionnaire | 4.7 ± 2.6a,b,c | 3.7 ± 2.2b | 5.6 ± 2.2c | 4.0 ± 2.1a,b | <0.001 | 4.6 ± 2.3 | 4.3 ± 3.1 | 0.54 |
| Global Health Scale | 30.1 ± 8.0a | 24.7 ± 6.9b | 34.4 ± 5.5c | 30.1 ± 4.7a | <0.001 | 31.2 ± 6.4 | 23.5 ± 8.9 | <0.001 |
| Lifetime Discrimination | 7.6 ± 2.9a | 9.2 ± 3.2b | 9.2 ± 3.6b,c | 11.9 ± 3.4d | <0.001 | 9.3 ± 3.6 | 8.0 ± 3.8 | 0.032 |
| Day-to-Day Discrimination | 13.2 ± 5.7a | 15.0 ± 5.8a | 14.8 ± 6.6a | 18.9 ± 6.4b | <0.001 | 15.5 ± 6.2 | 12.7 ± 7.5 | 0.01 |
| Lifetime Victimization | 14.7 ± 5.2a | 16.8 ± 5.2a | 16.7 ± 6.2a | 20.6 ± 5.6b | <0.001 | 17.2 ± 5.7 | 13.7 ± 6.8 | 0.001 |
| Microaggressions | 17.7 ± 7.3a | 20.0 ± 8.1a,b | 21.8 ± 8.1b | 25.5 ± 6.8c | <0.001 | 21.1 ± 7.6 | 17.4 ± 10.1 | 0.03 |
| Perceived Stress Scale | 15.7 ± 6.3a | 15.2 ± 6.9a | 21.0 ± 4.8b | 20.4 ± 6.0b | <0.001 | 18.4 ± 6.0 | 14.0 ± 8.2 | 0.003 |
| Neuropsychiatric Inventory Questionnaire Distress Score | 15.6 ± 10.0a,b | 12.5 ± 11.9a | 18.2 ± 9.7a,b | 19.0 ± 10.8b | 0.013 | 17.6 ± 9.5 | 9.6 ± 14.2 | 0.002 |
| Activities of Daily Living Scale | 1.3 ± 1.4a | 1.2 ± 1.0a | 1.6 ± 1.6a | 2.4 ± 1.2b | <0.001 | 1.7 ± 1.4 | 0.9 ± 1.7 | 0.001 |
| Instrumental Activities of Daily Living | 5.2 ± 1.7a | 5.1 ± 2.2a | 3.9 ± 1.9b | 3.3 ± 1.6b | <0.001 | 4.3 ± 1.9 | 5.7 ± 1.9 | <0.001 |
| Caregiver Stigma Impact Scale | 56.8 ± 16.7a | 39.6 ± 17.8b | 50.4 ± 13.8c | 48.4 ± 13.5d | <0.001 | 52.8 ± 15.4 | 41.0 ± 20.6 | 0.002 |
| Family Quality of Life in Dementia Scale | 156.1 ± 24.5a | 146.1 ± 32.9a | 153.3 ± 26.5a | 129.5 ± 21.7b | <0.001 | 146.3 ± 27.6 | 157.6 ± 25.9 | 0.02 |
| Center for Epidemiological Studies Depression Scale | 21.5 ± 9.4a | 21.4 ± 7.3a | 21.5 ± 11.1a | 29.1 ±8.0b | <0.001 | 23.7 ± 9.3 | 20.8 ± 12.1 | 0.17 |
For sexual orientation, values not sharing a superscript are significantly different.
Table 4.
Pearson’s correlations between psychosocial scale scores
| Scale | GHS | LD | DTDD | LV | MA | PSS | NPI-Q | CSIS | FQOLD | CES-D |
|---|---|---|---|---|---|---|---|---|---|---|
| Global Health Scale (GHS) | 1 | −0.12* | −0.15** | −0.15* | −0.12* | 0.28** | 0.14* | 0.03 | 0.14* | −0.33** |
| Lifetime Discrimination (LD) | 1 | 0.75** | 0.80** | 0.72** | 0.44** | 0.26** | 0.14* | −0.44** | 0.58** | |
| Day-to-Day Discrimination (DTDD) | 1 | 0.82** | 0.89** | 0.50** | 0.40** | 0.30** | −0.40** | 0.71** | ||
| Lifetime Victimization (LV) | 1 | 0.80** | 0.45** | 0.38** | 0.28** | −0.39** | 0.68** | |||
| Microaggressions (MA) | 1 | 0.53** | 0.38** | 0.31** | −0.43** | 0.75** | ||||
| Perceived Stress Scale (PSS) | 1 | 0.29** | 0.23** | 0.07 | 0.23** | |||||
| Neuropsychiatric Inventory Questionnaire Distress Score (NPI-Q) | 1 | 0.31** | −0.23** | 0.42** | ||||||
| Caregiver Stigma Impact Scale (CSIS) | 1 | 0.14** | 0.47** | |||||||
| Family Quality of Life in Dementia Scale (FQOLD) | 1 | −0.49** | ||||||||
| Center for Epidemiological Studies Depression Scale (CES-D) | 1 |
p < 0.05;
p < 0.01
Psychosocial Characteristics and Family Quality of Life in Dementia
The overall regression model was significant (p < 0.001) and explained 62.7% of the variance in family quality of life (Table 5). Compared with White SGM caregivers, African American/Black SGM caregivers (p = 0.002) and racial minority (Asian, Native American, Pacific Islander, other race) SGM caregivers (p = 0.031) had significantly lower family quality of life. Those with incomes over $50,000 had significantly higher levels of family quality of life (p < 0.001), as did those with at least a college degree (p < 0.001). Those caregivers with at least one chronic condition reported lower levels of family quality of life (p = 0.002). Those who identified as queer had significantly lower family quality of life scores compared with gay respondents (p = 0.006). However, those who identified as transgender reported significantly higher family quality of life than their cisgender counterparts (p = 0.005). As caregiver stigma scores increased by one point, family quality of life scores increased by 0.49 points (p < 0.001). As perceived stress increased by one point, family quality of life increased by 1.16 points (p < 0.001). Those who reported higher levels of microaggressions on average reported lower family quality of life (p = 0.002). No other predictors were significant in terms of family quality of life (Table 5).
Table 5.
Demographic and psychosocial factors associated with family quality of life
| Predictor | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| Age (years) | −0.02 | −0.01 | −0.06 |
| Black/African Americana | −0.15** | −0.14** | −0.13** |
| Asian/AIAN/PIHN/Other racea | −0.08 | −0.07 | −0.09* |
| Latinx/Hispanic | −0.10* | −0.13** | −0.07 |
| Income (≥$50,000) | 0.23** | 0.18** | 0.16** |
| Education (≥College) | 0.37** | 0.38** | 0.30** |
| Married/Partneredb | 0.04 | 0.06 | 0.08 |
| Separated/Divorced/Widowedb | −0.01 | 0.04 | 0.06 |
| At least one chronic condition | −0.15** | −0.16** | −0.13** |
| Child caregiverc | −0.21** | −0.17** | −0.06 |
| Other relative/Friend caregiverc | −0.17** | −0.11 | −0.01 |
| Months caregiving | −0.10* | −0.06 | −0.06 |
| Lesbiand | −0.06 | 0.04 | |
| Bisexuald | 0.05 | 0.06 | |
| Queerd | −0.25** | −0.14** | |
| Transgender | 0.07 | 0.12** | |
| Caregiver stigma | 0.29** | ||
| Perceived stress | 0.27** | ||
| Day-to-day discrimination | −0.13 | ||
| Microagressions | −0.30** |
White referent;
Single/never married referent;
Spousal caregiver referent;
Gay referent; AIAN = American Indian/Alaska Native; PIHN = Pacific Islander/Hawaiian Native;
p < 0.05;
p < 0.01
Psychosocial Characteristics and Neuropsychiatric Inventory and Depressive Symptoms
Multivariable models describing associations between psychosocial characteristics and neuropsychiatric symptom distress are summarized in Table 6. The overall regression model was significant (p < 0.001) and explained 21.3% of the variance in neuropsychiatric symptom distress score. Compared with White SGM caregivers, racial minority (Asian, Native American, Pacific Islander, other race) SGM caregivers reported lower levels of neuropsychiatric symptom distress (p = 0.045). Higher income was associated with higher levels of symptom distress (p = 0.019), while higher levels of formal education were associated with lower levels (p = 0.004). Compared with those caregivers who were single, caregivers who were married/partnered (p = 0.043) and those who were separated, divorced, or widowed (p = 0.040) reported significantly lower levels of symptom distress. Caregivers with at least one chronic condition reported significantly higher levels of symptom distress (p = 0.019). Increased caregiver stigma was associated with increased neuropsychiatric symptom distress (p = 0.02). No other predictors were significant in terms of neuropsychiatric symptom distress (Table 6).
Table 6.
Demographic and psychosocial factors associated with neuropsychiatric symptom severity
| Predictor | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| Age (years) | −0.07 | −0.08 | −0.09 |
| Black/African Americana | 0.004 | −0.001 | −0.02 |
| Asian/AIAN/PIHN/Other racea | −0.11 | −0.12* | −0.12* |
| Latinx/Hispanic | −0.07 | −0.02 | 0.03 |
| Income (≥$50,000) | 0.12 | 0.14* | 0.15* |
| Education (≥College) | −0.25** | −0.24** | −0.20** |
| Married/Partneredb | −0.15* | −0.19** | −0.15* |
| Separated/Divorced/Widowedb | −0.13 | −0.17* | −0.14* |
| At least one chronic condition | 0.11 | 0.13* | 0.15* |
| Child caregiverc | 0.02 | 0.01 | 0.04 |
| Other relative/Friend caregiverc | −0.13 | −0.11 | −0.07 |
| Months caregiving | 0.08 | 0.03 | 0.02 |
| Lesbiand | −0.15* | −0.11 | |
| Bisexuald | −0.04 | −0.03 | |
| Queerd | 0.10 | 0.10 | |
| Transgender | −0.08 | −0.04 | |
| Caregiver stigma | 0.19* | ||
| Perceived stress | 0.04 | ||
| Day-to-day discrimination | 0.14 | ||
| Microagressions | −0.10 |
White referent;
Single/never married referent;
Spousal caregiver referent;
Gay referent; AIAN = American Indian/Alaska Native; PIHN = Pacific Islander/Hawaiian Native;
p < 0.05;
p < 0.01
Psychosocial characteristics associated with depressive symptoms are shown in Table 7. The overall regression model was significant (p < 0.001) and explained 74.8% of the variance in depression scores. Depression scores were higher on average with increasing age (p = 0.008). Compared with spousal caregivers, caregivers who were the child of the person with ADRD had significantly higher depression scores (p < 0.001). Those who identified as queer had significantly higher depression scores compared with gay respondents (p < 0.001). Increased caregiver stigma (p < 0.001), day-to-day discrimination (p = 0.007), and microaggressions (p < 0.001) were all positively associated with depression scores. However, there was an inverse relationship between perceived stress (p < 0.001) and depression scores. In this sample, on average, as perceived stress increased, depression scores decreased. No other psychosocial characteristics were associated with depression scores (Table 7).
Table 7.
Demographic and psychosocial factors associated with depressive symptoms
| Predictor | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| Age (years) | 0.10 | 0.81 | 0.10** |
| Black/African Americana | 0.09 | 0.08 | 0.02 |
| Asian/AIAN/PIHN/Other racea | −0.09 | −0.10 | −0.07 |
| Latinx/Hispanic | −0.11 | −0.07 | 0.06 |
| Income (≥$50,000) | −0.16** | −0.11 | −0.05 |
| Education (≥College) | −0.28** | −0.30** | −0.02 |
| Married/Partneredb | −0.15* | −0.18** | −0.03 |
| Separated/Divorced/Widowedb | −0.06 | −0.12 | −0.04 |
| At least one chronic condition | 0.01 | 0.02 | 0.05 |
| Child caregiverc | 0.24** | 0.19** | 0.17** |
| Other relative/Friend caregiverc | 0.08 | 0.02 | 0.06 |
| Months caregiving | 0.05 | −0.01 | −0.04 |
| Lesbiand | 0.02 | 0.05 | |
| Bisexuald | −0.01 | 0.001 | |
| Queerd | 0.29** | 0.19** | |
| Transgender | −0.04 | 0.03 | |
| Caregiver stigma | 0.40** | ||
| Perceived stress | −0.24** | ||
| Day-to-day discrimination | 0.19** | ||
| Microagressions | 0.46** |
White referent;
Single/never married referent;
Spousal caregiver referent;
Gay referent; AIAN = American Indian/Alaska Native; PIHN = Pacific Islander/Hawaiian Native;
p < 0.05
p < 0.01
Discussion and Implications
To our knowledge, this is the first study to investigate and describe the psychosocial experiences of SGM people who provide care for someone with ADRD. Our study addresses the gaps and limitations presented by currently available data on SGM caregivers (Anderson & Flatt, 2018), builds upon the broader data from the NHAS (Fredriksen-Goldsen & Kim, 2017), and is guided by the HEP Model (Figure 1). The current sample of SGM caregivers of people with ADRD was diverse in terms of age, race, and ethnicity. The age range of participants (21 to 72 years old; mean 37.4 ± 8.6 years) skewed toward Millennial caregivers (i.e., ≤38 years old; Pew Research Center, 2019a). This is in line with current demographics as younger individuals take on caregiving roles (National Alliance for Caregiving, 2017; U.S. Census Bureau, 2015), particularly among SGM caregiver populations (Anderson & Flatt, 2018). Additionally, younger populations in the U.S. are more racially and ethnically diverse (U.S. Census Bureau, 2015), as well as more diverse in terms of sexual orientation and gender identity (GLAAD, 2018).
Caregiver Health
A third of SGM caregivers in the sample reported a below average health status. Health disparities among SGM people exist across the life course (Fredriksen-Goldsen et al., 2013; Gonzales & Henning-Smith, 2017), including an increased risk of illnesses with a high health burden or multiple chronic health problems (Gonzalez & Henning-Smith, 2017). Additionally, SGM adults have an increased likelihood of reporting their health as fair or poor (Potter & Patterson, 2019), which could result in greater strain for these caregivers. Nearly a third of SGM caregiver participants reported some level of difficulty in paying for everyday basics, despite the relatively high incomes reported. Half were caregiving at a distance and most reported making modifications to the home where their care recipient lived. These findings are congruent with those of SGM caregivers of older adults overall (Anderson & Flatt, 2018). In terms of caregiving services, the majority reported not using respite or transportation services. Though speculative, this may be related to the SGM identity of the caregiver and/or person with ADRD. The heteronormative nature of the majority of caregiver support services may create interpersonal and structural barriers in accessing these services (Fredriksen-Goldsen et al., 2016).
Family Quality of Life
Quality of life measures acknowledge the subjective dimensions of health beyond the presence or absence of a specific disease or condition (Dwyer-Lindgren et al., 2017; Moriarty et al., 2003; Potter & Patterson, 2019). SGM caregivers in our sample who identified as queer reported on average poorer family quality of life compared with those who identified as gay. Racial minority SGM caregivers also reported poorer family quality of life, as did those with chronic conditions. The Stress Process Model highlights how primary (e.g., directly related to caregiving) and secondary (other factors outside of caregiving) stressors related to the caregiver’s background and the context of caregiving can predict wellbeing among caregivers (Pearlin et al., 1990). SGM caregivers experiencing secondary stressors, such racial identity or having a chronic condition, may be at increased risk for caregiver strain and reduced quality of life (Goode, Haley, Roth, & Ford, 1998). Additionally, individuals who, on average, had higher scores related to microaggressions also had poorer quality of life. This is consonant with the existing literature that indicates that experiencing microaggressions diminishes many aspects of people’s lived experiences (Sue, 2010), including quality of life. It is likely that SGM people who are experiencing microaggressions while providing care for a person with ADRD experience diminished quality of life, as well as poorer mental health. This finding also is in line with the HEP Model (Figure 1) in that the historical and environmental context of the SGM lived experience provides a backdrop for and influences psychological, social, and behavioral outcomes such as family quality of life.
Depressive symptoms
The majority (78%) of our sample of SGM caregivers reported elevated depressive symptoms. Among the general population of caregivers of people with ADRD, the prevalence of depression was found to be 34% (Sallim et al., 2015). The scores within our sample were on average 22% (transgender) to 45% (queer) higher than the cut off for probable depression using the CES-D (Radloff, 1977). Additionally, individuals who identified as queer were the most likely to report elevated depressive symptoms, even in fully adjusted multivariable models. African American/Black SGM caregivers in our sample reported significantly higher levels of depressive symptoms than White SGM caregivers. It may be that the historical and environmental context of stigma associated with overlapping identities of SGM status and race increase the risk of depression among this group of caregivers. These findings are not just statistically significant, but also represent clinically relevant differences in depression scores and could point to an important intervention target for SGM people providing care for people with ADRD, particularly among racial minority SGM caregivers.
Microaggressions and day-to-day discrimination were associated with higher levels of depressive symptoms among SGM caregivers. SGM people experience minority stressors in the form of microaggressions and discrimination related to a non-heterosexual sexual orientation. These minority stressors are cumulative, exist beyond individual control, and are in addition to the daily hassles and stressful life events experienced by all people (Meyer, 2003), including caregiving stress, and are taken into account by the HEP Model. Health disparities experienced by the SGM population include increased rates of depression and depressive symptoms (Hughes et al., 2014; Russell & Fish, 2016) and reports of more poor mental health days (Potter & Patterson, 2019). These mental health disparities increase the risk of physical health issues, including cardiovascular disease (Caceres et al., 2019) and cognitive impairment (Hsieh et al., 2020). Minority stress also is associated with risky health behaviors and poor physical health outcomes (Flenar et al., 2017). These risky health behaviors, such as smoking, excessive drinking, and poor diet, are more common among SGM adults (Potter & Patterson, 2019) and can contribute to and increase the risk of chronic disease. The mechanisms driving these health disparities and accompanying sequelae among the SGM caregiver population warrant further study because experiences with discrimination, victimization, and microaggressions vary among SGM adults and because these experiences can influence both physical and mental health (Hatzenbuehler et al., 2014). This is particularly salient given that the more global Caregiver Stigma Impact Scale was not as strongly associated with depressive symptoms as the more SGM-specific measures related to minority stigma and stress.
Child caregivers in our sample experienced higher levels of depressive symptoms. For SGM caregivers of older adults, being the child of the care recipient was associated with greater emotional strain (Anderson & Flatt, 2018). Role strain has been identified as a potential mechanism that may link caregiving to stress (Pearlin et al., 1990). SGM child caregivers of people with ADRD may experience more emotional strain in providing care to a parent who at one time may not have been supportive of their sexual orientation and/or gender identity, or who may be providing care for someone to whom they are not “out.” However, without additional data related to the relationship between SGM child caregivers and the person for whom they are caring, we can only speculate and further research is warranted.
Transgender caregivers
Transgender caregivers reported better scores on the psychosocial outcomes included in the study compared with cisgender caregivers, despite a lower-than-average health status among transgender caregivers. These findings could be viewed through a resilience lens that allows for both risk and protective factors in relation to physical and mental health (Fredriksen-Goldsen et al., 2015). Resilience offers a multidimensional perspective to account for a broader sociocultural context and personal and social resources often experienced by hidden populations. The potential buffering effects of crisis competency gained as part of the “coming out” process (Kimmel, 1978), the creation of families of choice, and the increasing visibility of the transgender population may offer a protective effect to balance minority stress.
Families of choice are more common among SGM caregivers (Anderson & Flatt, 2018; Fredriksen-Goldsen & Kim, 2017) and have arisen as an adaptation to historical discrimination and stigma. According to the NHAS (Shiu, Muraco, & Fredriksen-Goldsen, 2016), 44% of SGM caregivers overall provided care to a friend and experienced lower levels of social support, elevating the risk for caregiver strain and negative health outcomes. A quarter of SGM caregivers for someone with ADRD identified as a friend or other relative in the present sample. This has significant research, practice, and policy implications given the majority of research regarding caregivers of older adults and interventions and services designed to relieve strain for caregivers focuses on spousal or child caregivers. Greater attention to caregiving provided by friends and other relatives among SGM caregivers is needed in the development of future research and health policy.
The HEP Model (Fredriksen-Goldsen et al., 2014) provided the framework for the present study in terms of data collection (Figure 1) and analysis. Currently, there are no published theoretical models specific to SGM caregivers. Given that it takes into account several stress-related models used to guide previous caregiving research (Hatzenbuehler, 2009; Meyer, 2003; Pearlin et al., 1990) and is specifically designed for use among SGM adults (Fredriksen-Goldsen & Kim, 2017), the HEP model was used. Our findings further extend the model by illustrating the reciprocal relationships among psychological, social, and behavioral factors in terms of family quality of life and neuropsychiatric behaviors. Future research to understand the directionality of the relationships of variables via path analysis and the moderating effects of psychological, social, and behavioral factors and measures related to health and well-being are warranted. Such information would further elucidate targets for intervention, service allocation, and policy solutions for this population of caregivers.
Limitations and strengths
The present study has several limitations. The cross-sectional nature of these data precludes our ability to assess causality. However, this study has provided a much needed, first investigation into the experiences of SGM caregivers for people with ADRD. We did not ask if the SGM caregiver was “out” or disclosed their sexual orientation or gender identity to the person for whom they provided care or about the quality of that relationship. Being “out” has been shown to reduce distress and depression (Riggle et al., 2017) among SGM individuals. Alternatively, it is also possible that being out to care recipients could elevate risk for SGM caregivers to be the target of microaggressions if care recipients hold negative attitudes about SGM people. The study survey did not include questions about the age of the person with ADRD, where the person with ADRD lived if they did not reside with the caregiver, or questions about the type of caregiving tasks performed. Future studies should consider the difficulty and type of caregiving activities performed by SGM caregivers and the relationship with psychosocial measures of caregiving. The survey also did not include questions regarding risky health behaviors for the caregivers, which would help broaden our understanding of the health of this caregiving population. Finally, although the digital divide is not as prevalent as in the past (Smith & Anderson, 2018) and most SGM people have access to the Internet (Jabson et al., 2017), there are caregivers without regular Internet access, potentially limiting the generalizability of the findings from the current analysis given the sample included only those caregivers who have Internet access.
Despite these limitations, our study has important strengths. No study to date has assessed or described the associations between psychosocial factors and quality of life outcomes among SGM adults providing care for people with ADRD. Effective interventions and services tailored specifically for this population cannot be developed or delivered effectively to improve quality of life and psychosocial health outcomes for this population of caregivers without such information. Our results provide much-needed evidence to support the design, testing, and implementation of interventions and services for SGM caregivers, answering calls from the National Institutes of Health to examine health disparities among SGM individuals (National Institutes of Health, 2020).
We also found it was feasible to use digital methods, specifically social media, to recruit populations considered hard to reach or “hidden” successfully, such as SGM individuals (Fredriksen-Goldsen & Kim, 2017). SGM people increasingly use social media and networking sites (Pew Research Center, 2013) like Facebook and YouTube (Seidenberg et al., 2017; Jabson et al., 2017) and use the Internet to seek health information more frequently than their heterosexual counterparts (Jabson et al., 2017). Additionally, digital recruitment and data collection methods increase accessibility and reduce exclusion of rural caregivers or caregivers with fear of discrimination, thereby broadening the understanding of the SGM caregiver experience. Finally, given that social media platforms are used by a diverse population in terms of age, race, and ethnicity (Pew Research Center, 2019b), this enhanced our ability to recruit a diverse sample.
Conclusion
This study is the first to provide a focused description of the characteristics and psychosocial needs of SGM caregivers of someone with ADRD, as well as differences in those outcomes across sexual orientations and gender identities. These findings support the development of targeted interventions to enhance quality of life and psychosocial health for this caregiving population. Additionally, our results can inform future research to understand the impact of overlapping identities among caregivers (e.g., racial and sexual minority caregivers) and the influence of resilience on the caregiving experiences of minoritized caregivers.
Funding
Research reported in this publication was supported by an intramural award from the Office of Research Services in the College of Nursing at the University of Tennessee-Knoxville (JGA) and by the National Institute on Aging of the National Institutes of Health under award number 1R03AG058528-01A1 (JGA). Dr. Gross was supported by K01AG050699 from the National Institute on Aging. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflicts of Interest
The Authors declare that there are no conflicts of interest.
Contributor Information
Joel G. Anderson, College of Nursing, University of Tennessee-Knoxville, 1200 Volunteer Boulevard, Knoxville TN 37996.
Jason D. Flatt, School of Public Health, University of Nevada-Las Vegas.
Jennifer M. Jabson Tree, Department of Public Health, University of Tennessee-Knoxville.
Alden L. Gross, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD 21231.
Karen M. Rose, Center for Healthy Aging, Self-Management and Complex Care, College of Nursing, The Ohio State University.
References
- Alzheimer’s Association. (2020). Alzheimer’s Disease Facts and Figures.
- Anderson JG, & Flatt JD (2018). Characteristics of LGBT caregivers of older adults: Results from the national Caregiving in the U.S. 2015 Survey. Journal of Gay and Lesbian Social Services, 30(2), 103–116. [Google Scholar]
- Burgener SC, & Berger B (2008). Measuring perceived stigma in persons with progressive neurologic disease: Alzheimer’s dementia and Parkinson’s disease. Dementia, 7, 31–53. [Google Scholar]
- Caceres BA, Brody A, Luscombe RE, Primiano JE, Marusca P, Sitts EM, & Chyun D (2017). A systematic review of cardiovascular disease in sexual minorities. American Journal of Public Health, 107(4), e13–e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cella D, Riley W, Stone A, Rothrock N, Reeve B, Yount S, …, Hays R (2010). Initial adult health item banks and first wave testing of the Patient-Reported Outcomes Measurement Information System (PROMIS™) network: 2005–2008. Journal of Clinical Epidemiology, 63, 1179–1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, & Mermelstein R (1983). A global measure of perceived stress. Journal of Health & Social Behavior, 24(4), 385–396. [PubMed] [Google Scholar]
- Dwyer-Lindgren L, Mackenbach JP, van Lenthe FJ, & Mokdad AH (2017). Self-reported general health, physical distress, mental distress, and activity limitation by US county, 1995–2012. Population Health Metrics, 15, 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farina N, Page TE, Daley S, Brown A, Bowling A, Basset T, … & Banerjee S (2017). Factors associated with the quality of life of family carers of people with dementia: A systematic review. Alzheimer’s & Dementia, 13(5), 572–581. [DOI] [PubMed] [Google Scholar]
- Flenar DJ, Tucker CM, & Williams JL (2017). Sexual minority stress, coping, and physical health indicators. Journal of Clinical Psychology in Medical Settings, 24(3–4), 223–233. [DOI] [PubMed] [Google Scholar]
- Fredriksen KI (1999). Family caregiving responsibilities among lesbians and gay men. Social Work, 44(2), 142–155. [DOI] [PubMed] [Google Scholar]
- Fredriksen-Goldsen KI (2016). Equity: A powerful force for the future of aging. 2016 Elder Friendly Futures Conference, Seattle, WA. [Google Scholar]
- Fredriksen-Goldsen KI (2011). Resilience and disparities among lesbian, gay, bisexual, and transgender older adults. Public Policy and Aging Report, 21(3):3–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen KI, & Hoy-Ellis CP (2007). Caregiving with pride: An introduction. Journal of Gay & Lesbian Social Services, 18(3–4), 1–13. [Google Scholar]
- Fredriksen-Goldsen KI, & Kim HJ (2017). The science of conducting research with LGBT older adults: An introduction to Aging with Pride: National Health, Aging, and Sexuality/Gender Study (NHAS). The Gerontologist, 51, S1–S14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen KI, & Kim HJ (2014). Count me in: Response to sexual orientation measures among older adults. Research on Aging, 1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen KI, Jen S, Bryan AE, Goldsen J (2016) Cognitive Impairment, Alzheimer’s Disease, and Other Dementias in the Lives of Lesbian, Gay, Bisexual and Transgender (LGBT) Older Adults and Their Caregivers. Journal of Applied Gerontology, 37(5), 545–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen KI, Kim HJ, Shiu C, Goldsen J, & Emlet CA (2015). Successful aging among LGBT older adults: Physical and mental health-related quality of life by age group. The Gerontologist, 55, 154–168. 10.1093/geront/gnu081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen KI, Simoni JM, Kim HJ, Lehavot K, Walters KL, Yang J, …, Muraco A (2014). The Health Equity Promotion Model: Reconceptualization of lesbian, gay, bisexual, and transgender (LGBT) health disparities. The American Journal of Orthopsychiatry, 84, 653–663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen KI, Kim HJ, Barken SE, et al. (2013). Health disparities among lesbian, gay, and bisexual older adults: Results from a population-based study. American Journal of Public Health, 103, 1802–1809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galvin JE, Roe CM, Xiong C, & Morris JC (2006). Validity and reliability of the AD8 informant interview in dementia. Neurology, 67(11), 1942–1948. [DOI] [PubMed] [Google Scholar]
- Gay and Lesbian Alliance Against Defamation. (2018). Accelerating acceptance 2018. Retrieved from https://www.glaad.org/publications/accelerating-acceptance-2018.
- Glick SN, & Golden MR (2014). Early male partnership patterns, social support, and sexual risk behavior among young men who have sex with men. AIDS Behavior, 18, 1466–1475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzales G, & Henning-Smith C (2017). Health disparities by sexual orientation: Results and implications from the Behavioral Risk Factor Surveillance System. Journal of Community Health, 42, 1163–1172. [DOI] [PubMed] [Google Scholar]
- Goode KT, Haley WE, Roth DL, & Ford GR (1998). Predicting longitudinal changes in caregiver physical and mental health: A stress process model. Health Psychology, 17(2), 190–198. doi: 10.1037/0278-6133.17.2.190 [DOI] [PubMed] [Google Scholar]
- Hash KM (2001). Preliminary study of caregiving and post-caregiving experiences of older gay men and lesbians. Journal of Gay & Lesbian Social Services, 13(4), 87–94. [Google Scholar]
- Hatzenbuehler ML (2009). How does sexual minority stigma “get under the skin”? A psychological mediation framework. Psychological Bulletin, 135, 707–730. 10.1037/a0016441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Slopen N, & McLaughlin KA (2014). Stressful life events, sexual orientation, and cardiometabolic risk among young adults in the United States. Health Psychology, 33, 1185–1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsieh N, Liu H, & Lai WH (2020). Elevated risk of cognitive impairment among older sexual minorities: Do health conditions, health behaviors, and social connections matter?. The Gerontologist, gnaa136. 10.1093/geront/gnaa136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes M (2008). Imagined futures and communities: Older lesbian and gay people’s narratives on health and aged care. Journal of Gay and Lesbian Social Services, 20, 167–186. 10.1080/10538720802179211 [DOI] [Google Scholar]
- Hulko W (2009). The time- and context-contingent nature of intersectionality and interlocking oppressions. Affilia, 24, 44–55. [Google Scholar]
- Institute of Medicine. (2011). The health of lesbian, gay, bisexual, and transgender people: Building a foundation for better understanding. Washington, DC: The National Academies Press. [PubMed] [Google Scholar]
- Jablonski RA, Vance DE, & Beattie E (2013). The invisible elderly: Lesbian, gay, bisexual, and transgender older adults. Journal of Gerontological Nursing, 39, 46–52. [DOI] [PubMed] [Google Scholar]
- Jabson JM, Patterson JG, & Kamen C (2017). Understanding health information seeking on the Internet among sexual minority people: Cross-sectional analysis from the Health Information National Trends Survey. Journal of Medical Internet Research: Public Health Surveillance, 19, e39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasper JD, Freedman VA, & Spillman B (2013). Classification of persons by dementia status in the National Health and Aging Trends Study. Technical Paper #5. Baltimore: Johns Hopkins University School of Public Health. Retrieved from www.NHATS.org. [Google Scholar]
- Katz S, Ford AB, Moskowitz RW, Jackson BA, & Jaffe MW (1963). Studies of illness in the aged: The index of ADL: A standardized measure of biological and psychosocial function. JAMA, 185, 914–919. [DOI] [PubMed] [Google Scholar]
- Kaufer DI, Cummings JL, Ketchel P, Smith V, MacMillan A, Shelley T, … & DeKosky ST (2000). Validation of the NPI-Q, a brief clinical form of the Neuropsychiatric Inventory. Journal of Neuropsychiatry and Clinical Neurosciences, 12(2), 233–239. [DOI] [PubMed] [Google Scholar]
- Kimmel D (1978). Adult development and aging: A gay perspective. Journal of Social Issues, 34, 113–130. [Google Scholar]
- Lawton MP, & Brody EM (1969). Assessment of older people: Self-maintaining and instrumental activities of daily living. The Gerontologist, 9(3), 179–186. [PubMed] [Google Scholar]
- Martinez O, Wu E, Shultz AZ, Capote J, Lopez Rios J, Sandfort T, …, & Rhodes SD (2014). Still a hard-to-reach population? Using social media to recruit Latino gay couples for and HIV intervention adaptation study. Journal of Medical Internet Research, 16, e113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews KA, Xu W, Gaglioti AH, Holt JB, Croft JB, Mack D, & McGuire LC (2019). Racial and ethnic estimates of Alzheimer’s disease and related dementias in the United States (2015–2060) in adults aged >65 years. Alzheimer’s Dementia, 15(1), 17–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGovern J (2014). The forgotten: Dementia and the aging LGBT community. Journal of Gerontological Social Work, 1–13. [DOI] [PubMed] [Google Scholar]
- Meyer IH (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin, 129, 674–697. 10.1037/0033-2909.129.5.674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moriarty DG, Zack MM, & Kobau R (2003). The Centers for Disease Control and Prevention’s Healthy Days Measures—Population tracking of perceived physical and mental health over time. Health Quality of Life Outcomes, 1, 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muraco A, & Fredriksen-Goldsen KI (2014). The highs and lows of caregiving for chronically ill lesbian, gay, and bisexual elders. Journal of Gerontological Social Work, 57, 251–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Alliance for Caregiving. (2017). Caregiving in the U.S. 2015. Retrieved from http://www.caregiving.org/caregiving2015/.
- National Center for Health Statistics. (2017). National Health Interview Survey (NHIS) Geocodes. Retrieved from: https://www.cdc.gov/rdc/geocodes/geowt_nhis.htm.
- National Institutes of Health. (2020). Strategic plan to advance research on the health and well-being of sexual & gender minorities, Fiscal Years 2021–2025. Washington, DC: U.S. Government Printing Office. [Google Scholar]
- National Institutes of Health. (2010). Biennial report of the Director, National Institutes of Health, Fiscal Years 2008 & 2009 (Vol. 1). Washington, DC: U.S. Government Printing Office. [Google Scholar]
- Nelson CL, & Andel R (2020). Does Sexual Orientation Relate to Health and Well-Being? Analysis of Adults 50+ Years of Age. The Gerontologist. [DOI] [PubMed] [Google Scholar]
- Pearlin LI, Mullan JT, Semple SJ, & Skaff MM (1990). Caregiving and the stress process: An overview of concepts and their measures. The Gerontologist, 30(5), 583–594. [DOI] [PubMed] [Google Scholar]
- Pew Research Center. (2019a). Defining generations: Where Millennials end and Generation Z begins. Accessed from https://www.pewresearch.org/fact-tank/2019/01/17/where-millennials-end-and-generation-z-begins/.
- Pew Research Center. (2019b). Social Media Fact Sheet. Accessed from https://www.pewresearch.org/internet/fact-sheet/social-media/.
- Pew Research Center. (2013). A Survey of LGBT Americans. Washington, DC: Pew Research Center. [Google Scholar]
- Potter EC, & Patterson CJ (2019). Health-related quality of life among lesbian, gay, and bisexual adults: The burden of health disparities in 2016 Behavioral Risk Factor Surveillance System data. LGBT Health, 6(7), 357–369. [DOI] [PubMed] [Google Scholar]
- Price E (2008). Pride or prejudice? Gay men, lesbians and dementia. British Journal of Social Work, 38, 1337–1352. [Google Scholar]
- Radloff LS (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385. [Google Scholar]
- Riggle ED, Rostosky SS, Black WW, & Rosenkrantz DE (2017). Outness, concealment, and authenticity: Associations with LGB individuals’ psychological distress and well-being. Psychology of Sexual Orientation and Gender Diversity, 4(1), 54. [Google Scholar]
- Rose KM, Williams IC, Anderson JG, & Geldmacher DS (2020). Development and validation of the Family Quality of Life in Dementia Scale. The Gerontologist, gnaa022. [DOI] [PubMed] [Google Scholar]
- Russell ST, & Fish JN (2016). Mental health in lesbian, gay, bisexual, and transgender (LGBT) youth. Annual Reviews in Clinical Psychology, 12, 465–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sallim AB, Sayampanathan AA, Cuttilan A, & Ho R (2015). Prevalence of mental health disorders among caregivers of patients with Alzheimer’s disease. Journal of the American Medical Directors Association, 16(12), 1034–1041. [DOI] [PubMed] [Google Scholar]
- Seidenberg AB, Jo CL, Ribisl KM, Lee JGL, Buchting FO, Kim Y, & Emery SL (2017). A national study of social media, television, radio, and internet usage of adults by sexual orientation and smoking status: Implications for campaign design. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Services and Advocacy for GLBT Elders (SAGE). (2018). Issues Brief: LGBT and Dementia. Retrieved from: https://www.sageusa.org/resource-posts/issues-brief-lgbt-and-dementia/.
- Shiu C, Muraco A, & Fredriksen-Goldsen K (2016). Invisible care: Friend and partner care among older lesbian, gay, bisexual, and transgender (LGBT) adults. Journal of the Society for Social Work and Research, 7, 527–545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith A, & Anderson M (2018). Social media use in 2018. Pew Research Center. Retrieved from http://www.pewinternet.org/2018/03/01/socialmedia-use-in-2018/ [Google Scholar]
- Stewart AL, & Kamberg C (1992). Physical functioning. In: Stewart AL, & Ware JE (Eds.), Measuring functioning and well-being: The medical outcomes study approach. Durham, NC: Duke University Press. p. 86–142. [Google Scholar]
- Sue DW (2010). Microaggressions in everyday life: Race, gender, and sexual orientation. John Wiley & Sons. [Google Scholar]
- U.S. Census Bureau. (2015). Millennials outnumber baby boomers and are far more diverse, Census Bureau reports. Retrieved from https://www.census.gov/newsroom/pressreleases/2015/cb15-113.html.
- Zanetos JM, & Skipper AW (2020). The effects of health care policies: LGBTQ aging adults. Journal of Gerontological Nursing 46(3), 9–13. [DOI] [PubMed] [Google Scholar]


