Background:
Emerging evidence suggests sociodemographic disparities in telemedicine access and utilization during the COVID-19 pandemic, especially for older adults. (1) Older adults may benefit most from telemedicine due to a high prevalence of serious illness and functional impairment, which makes travel to healthcare visits challenging. Furthermore, as compared to audio-only visits, video-visits may lead to improved patient-provider communication and physical exam. (2) Yet, little is known about the characteristics of older adults who utilized video-visits during the pandemic.
Objective:
We aim to characterize “telemedicine use,” defined as communicating with your usual healthcare provider using video-visits during the COVID-19 pandemic, among older adults in the United States using data from a nationally representative cohort study of Medicare beneficiaries.
Methods and Findings:
In order to assess prevalence and predictors of telemedicine use among older adults, we used data from the National Health and Aging Trends Study (NHATS), a longitudinal study of Medicare enrollees, wherein respondents are annually surveyed regarding their health, function, and technological environment. Using data from the 2019 NHATS annual survey (weighted response rate 96.0%), which was collected through in-person interviews between May and October 2019, we captured respondent sociodemographic and clinical characteristics (3). From the 2020 NHATS COVID-19 supplement, which was collected via mailed survey between June and October 2020 and returned by respondents through January 2021, we captured self-reported telemedicine use (4). Respondents excluded from the COVID-19 supplement were deceased or using facility questionnaires in 2020. Of the respondents eligible to receive the COVID-19 supplement (3,961), 2,350 (weighted response rate 60.5%) completed the telemedicine use questions.
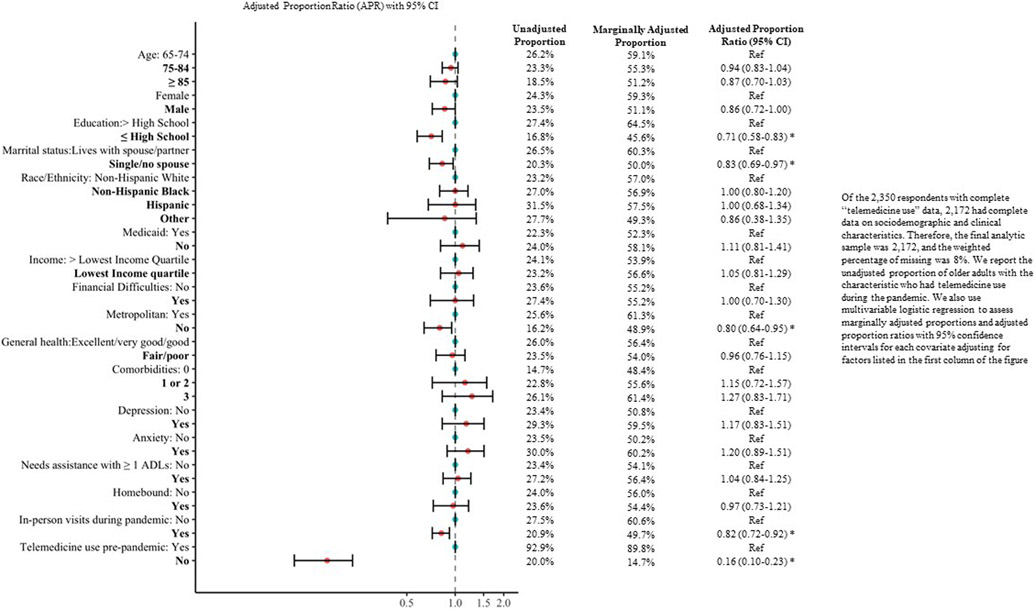
We report sociodemographic and clinical characteristics of older adults who did and did not have telemedicine use during the pandemic as well as the unadjusted proportion of older adults with a given characteristic who had telemedicine use during the pandemic. We used multivariable logistic regression to assess marginally adjusted proportions and adjusted proportion ratios (APR) with 95% confidence intervals for each covariate adjusting for all other covariates. All analyses took into account complex survey design by incorporating survey weight, strata, and primary sampling unit into the survey procedures in SAS (version 9.4TS1m6). Our study used publically available de-identified data.
Of the 2,350 respondents who completed the telemedicine use questions, the majority were female (53.4%) and lived in metropolitan areas (81.8%). Overall, 23.9% of respondents reported telemedicine use during the pandemic up from 5.4% pre-pandemic, and 59.9% reported in-person visits during the pandemic. (Table 1) Living in non-metropolitan areas (APR 0.80; 95% CI 0.64-0.95), ≤ high school education (APR 0.71; 95% CI 0.58-0.83), no spouse/partner (APR 0.83; 95% CI 0.69-0.97), no pre-pandemic telemedicine use (APR 0.16; 95% CI 0.10-0.23), and in-person visits during the pandemic (APR 0.82; 95% CI 0.72-0.92) were associated with lower pandemic telemedicine use. (Figure 1)
Table 1.
Sociodemographic and clinical characteristics of NHATS respondents who did and did not report telemedicine use
| All Respondentsa n = 2,350 Weighted n = 19,771,970 |
Telemedicine use during the COVID-19 pandemicb | ||
|---|---|---|---|
| No n = 1834 Weighted n = 15,039,201 (76.1%) |
Yes n = 516 Weighted n = 4,732,769 (23.9%) |
||
| Age | |||
| 65-74 | 42.8% | 41.5% | 46.9% |
| 75-84 | 44.0% | 44.3% | 42.8% |
| ≥ 85 | 13.3% | 14.2% | 10.3% |
| Male | 46.6% | 46.8% | 45.8% |
| Race/Ethnicityc | |||
| Non-Hispanic White | 86.8% | 87.7% | 84.1% |
| Non-Hispanic Black | 5.4% | 5.2% | 6.1% |
| Hispanic | 4.8% | 4.3% | 6.3% |
| Otherd | 3.0% | 2.8% | 3.5% |
| Lives with Spouse/Partner | 58.8% | 58.9% | 65.0% |
| Lives in Metropolitan area | 81.8% | 80.0% | 87.7% |
| ≤ High School Education | 33.9% | 37.0% | 24.0% |
| Lowest Income Quartilee | 14.2% | 14.3% | 13.8% |
| Medicaid coverage | 9.2% | 9.4% | 8.6% |
| Financial Difficultiesf | 5.5% | 5.2% | 6.4% |
| Fair/poor self-rated health | 18.3% | 17.8% | 19.9% |
| Self-reported comorbiditiesg | |||
| 0 | 5.7% | 6.4% | 3.5% |
| 1 or 2 | 46.4% | 47.1% | 44.2% |
| ≥ 3 | 47.9% | 46.5% | 52.3% |
| Depressionh | 8.0% | 7.5% | 9.8% |
| Anxietyi | 6.6% | 6.1% | 8.3% |
| Needs Assistance with ≥ 1 ADLj | 13.4% | 12.8% | 15.2% |
| Homeboundk | 3.9% | 3.9% | 3.9% |
| Telemedicine use pre-pandemicl | 5.4% | 0.5% | 21.0% |
| In-person visits during the pandemicb | 59.9% | 62.0% | 53.3% |
Data is presented as percentages, weighted to account for complex survey design.. < 3% of each variable was found to be missing.
Telemedicine use and in-person visits during the pandemic were defined by the following question on the NHATS 2020 COVID-19 supplement: “DURING the COVID-19 outbreak, how did you communicate with your usual health care provider? a) Phone Calls Yes/No, b) Emails or texts or portal messages Yes/No, c) Video calls (also called “telehealth”) Yes/No, d) In-person visits Yes/No”
Data were collected by self-report.
Categories included American Indian, Asian, Native Hawaiian, Pacific Islander, other, do not know, or more than 2 reported race/ethnicity categories.
Income quartiles for respondents were defined in relation to all Medicare beneficiaries.
Data were collected by self-report regarding financial difficulties specifically during the COVID-19 pandemic.
NHATS questions regarding self-reported comorbidities include heart disease (such as myocardial infarction, angina, or congestive heart failure), high blood pressure or hypertension, arthritis (including osteoarthritis or rheumatoid arthritis), osteoporosis or thinning of the bones, diabetes, lung disease (such as emphysema, asthma, or chronic bronchitis), a stroke, dementia or Alzheimer’s disease, and cancer
Probable depression if scored ≥3 on the PHQ-2 scale (range: 0–6).
Probably anxiety if scored ≥3 on the GAD-2 scale (range: 0–6).
ADLs: activities of daily living (eating, bathing, getting dressed, mobility, continence, and toileting).
Homebound is defined as leaving home never or rarely (1 time per week).
Telemedicine use pre-pandemic is defined by the following question on the NHATS 2020 COVID-19 supplement: “BEFORE the COVID-19 outbreak, how did you communicate with your usual health care provider? a) Phone Calls Yes/No, b) Emails or texts or portal messages Yes/No, c) Video calls (also called “telehealth”) Yes/No, d) In-person visits Yes/No”
Figure 1:
Association of respondent characteristics and telemedicine use during the COVID-19 pandemic
Discussion:
Our study is the first to describe the prevalence and predictors of telemedicine use by older adults during the first peak of the COVID-19 pandemic. Although video-visits for older adults increased five-fold, our findings suggest that the vast majority of older adults did not use video-visits during the first surge of the pandemic. Despite the burdens of travel to in-person visits and the high risk for severe COVID-19 before access to vaccination, twice as many older adults presented for in-person as compared to video-visits. Furthermore, we found less telemedicine use among respondents who had lower educational attainment, no spouse/partner, and lived in non-metropolitan areas.
Our study is limited by the response rate to the COVID-19 supplement and telemedicine use questions. In addition, the COVID-19 supplement was mailed to participants rather than conducted in-person, potentially impacting its validity. Generalizability may be further limited as this supplement only accounts for the first wave of the pandemic during which older adults living in metropolitan areas were disproportionately impacted.
Future work should examine telemedicine uptake during subsequent waves and after the health crisis. Because telemedicine has become a novel complement to in-person visits, our findings suggest a need to understand whether low telemedicine uptake is driven by barriers for older adults, their preferences for accessing care in-person, or a combination of these factors. Promoting telemedicine uptake will likely require addressing the digital divide, improving the usability of telemedicine platforms, and providing community-based technical support (5).
References:
- 1.Rivera V, Aldridge MD, Ornstein K, Moody KA, Chun A. Racial and Socioeconomic Disparities in Access to Telehealth. J Am Geriatr Soc. 2021;69(1):44–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lally K, Kematick BS, Gorman D, Tulsky J. Rapid Conversion of a Palliative Care Outpatient Clinic to Telehealth. JCO Oncology Practice. 2021;17(1):e62–e67. doi: 10.1200/OP.20.00557 [DOI] [PubMed] [Google Scholar]
- 3.National Health and Aging Trends Study: User Guide Rounds 1-10; Final Release July 2021. Accessed September 9, 2021. https://www.nhats.org/sites/default/files/2021-07/NHATS_User_Guide_R10_Final_Release.pdf
- 4.COVID-19 Supplement to the National Health and Aging Trends Study: User Guide; Final Release June 2021. Accessed September 7, 2021. https://www.nhats.org/sites/default/files/2021-06/NHATS%20COVID-19%20User%20Guide%20Final.pdf
- 5.Roberts ET, Mehrotra A. Assessment of Disparities in Digital Access Among Medicare Beneficiaries and Implications for Telemedicine. JAMA Intern Med. 2020;180(10):1386–1389. [DOI] [PMC free article] [PubMed] [Google Scholar]