Abstract
A new definition of metabolic dysfunction-associated fatty liver disease (MAFLD) was proposed in 2020. The change from nonalcoholic fatty liver disease (NAFLD) to MAFLD highlights the metabolic abnormalities that accompany fatty liver. The diagnosis of MAFLD does not require exclusion of secondary causes of liver diseases and alcohol consumption. Thus, MAFLD may coexist with other types of liver diseases, such as viral hepatitis, a disease that remains the most common cause of liver disease-related death. With the increasing prevalence of MAFLD, patients with coincidental MAFLD and viral hepatitis are frequently encountered in clinical practice. In this review, we mainly summarize the mutual relationship between hepatitis B/C and systematic metabolism dysfunction related to MAFLD. We discuss the impact of MAFLD on progression of viral hepatitis and the therapies. Some unaddressed clinical problems related to concomitant MAFLD and viral hepatitis are also identified.
Keywords: Metabolic dysfunction-associated fatty liver disease, Chronic hepatitis B, Chronic hepatitis C
Introduction
The term nonalcoholic fatty liver disease (NAFLD) was first coined by Ludwig and colleagues in 1980 to describe fatty liver disease occurring in the absence of significant alcohol intake.1 Currently, NAFLD is arising as the most common chronic liver disease, due to the global obesity epidemic.2 The diagnosis of NAFLD requires evidence of hepatic steatosis and lack of secondary causes of hepatic fat accumulation, such as significant alcohol consumption, hepatitis C (genotype 3), medications, or Wilson’s disease.3,4 Several studies have suggested that NAFLD is commonly associated with metabolic comorbidities, such as obesity, diabetes, and dyslipidemia.3,4 However, experts have raised concerns that the term “NAFLD” is not appropriate for describing fatty liver disease associated with metabolic dysfunction. In this context, an international panel of experts proposed a novel term—metabolic dysfunction-associated fatty liver disease (MAFLD),5,6 which highlights the features of metabolic abnormalities with the acceptance that MAFLD may commonly coexist with other conditions, such as viral hepatitis. As such, some hepatologists argued that the change in terminology from NAFLD to MAFLD is rather premature.7 Viral hepatitis and MAFLD are the two leading causes of chronic liver disease in China and these two conditions likely coexist in many patients. Patients with coincidental MAFLD and viral hepatitis likely have different pathophysiological conditions and show different responses to therapy compared to patients with liver disease caused by a single etiology. Here, we mainly discuss the relationship between MAFLD and hepatitis. We also deliberate how to improve clinical practice for patients with coincidental MAFLD and viral hepatitis.
Hepatitis B and MAFLD
Hepatitis B virus (HBV) infection is a major cause of disease burden in most Asian nations, owing to its high prevalence and high probability of progression to cirrhosis and hepatocellular carcinoma (HCC).8 With the growing prevalence of MAFLD, cases with concomitant hepatitis B and hepatic steatosis are increasingly encountered in clinical practice and several questions remain to be answered.
Negative effects of steatosis on HBV replication
Most HBV infections acquired at birth or perinatally become chronic. Virus-specific T cell responses, which play a major role in HBV clearance, are deeply exhausted in chronic hepatitis B. Besides, the lack of protective T cell memory maturation, impaired natural killer (NK) cell function, and depressed cytokine production contribute to the tolerogenic environment in liver. The overall impairment of T cell responses is likely to be maintained by the persistent exposure to high levels of HBV antigens.9,10 In addition, γδ T cells are involved in HBV-induced immunotolerance by mediating CD8+ T cell exhaustion.11
Most studies have revealed a negative association between liver steatosis and chronic HBV infection.12–16 For example, a retrospective study by Peleg et al.15 found an inverse association between the severity of liver steatosis and HBV viral load in treatment-naïve chronic hepatitis B (CHB) patients. Some studies suggested that liver steatosis affects the immune response during HBV infection. Mak et al.17 analyzed the effect of liver steatosis on HBV surface antigen (HBsAg) seroclearance in treatment-naïve CHB patients over a follow-up period of 3 years; on Cox regression analysis, hepatic steatosis was found to be associated with a 3-fold increase in the probability of HBsAg seroclearance in quiescent CHB. Lee et al.18 explored the factors associated with phase change in patients with CHB in the immune-tolerant phase. Notably, patients who underwent phase change were more likely to have coexisting fatty liver compared to patients who remained in the immune-tolerant phase.18 Further studies are required to clarify whether fatty liver is an important determinant of the immune response in CHB patients.
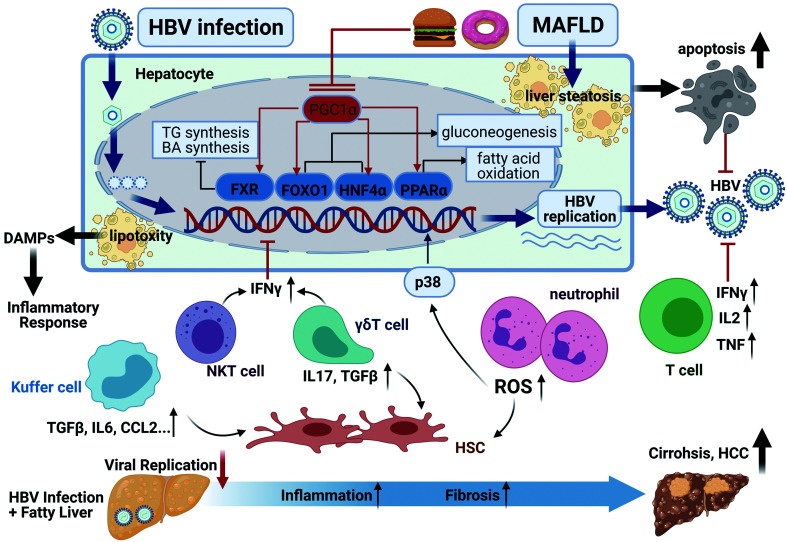
A wide body of published clinical data suggests an inverse association between liver steatosis and HBV replication;12–16 however, the underlying mechanisms are not clear. Some studies have postulated that fat deposition in HBV-infected hepatocytes may inhibit HBV replication.19 Here, we propose some potential mechanisms regarding the impact of liver steatosis on HBV infection and replication (Fig. 1). First, fatty liver is associated with impaired function of peroxisome proliferator activated receptor γ-coactivator 1 alpha (PGC1α),20,21 which is known to activate several transcription factors, such as Farnesoid X receptor (FXR), forkhead Box O1 (FOXO1), hepatocyte nuclear factor 4 alpha (HNF4α), and peroxisome proliferator activated receptor alpha (PPARα).22–25 Interestingly, these transcription factors not only control HBV replication but also regulate the expression of several genes related to fat metabolism in the liver.26 It is plausible that the transcription of fat metabolism genes in fatty liver may interfere with HBV replication by competing for usage of the transcription factors mentioned above. Second, nonalcoholic steatohepatitis (NASH) is accompanied by increased hepatic infiltration of NK T cells, T cells,27 and γδ T cells;28 thus, hepatic fat accumulation may create altered innate and adaptive immune microenvironments that are suboptimal for HBV replication.29 Finally, increased hepatocyte apoptosis induced by NASH may also reduce HBV replication. Despite the several proposed mechanisms, further studies are required to elucidate the precise mechanism by which liver steatosis affects HBV infection.30
Fig. 1. Potential mechanisms underlying the impact of liver steatosis on HBV infection and disease progression.
Liver steatosis suppresses HBV replication via several pathways. Some transcription factors related to lipid metabolism promote HBV replication, such as PGC1α, FXR, FOXO1, HNF4α, and PPARα. Liver steatosis also leads to increased hepatocyte apoptosis. Hepatic infiltrating inflammatory cells, such as NK T cells, T cells, and γδ T cells create an altered immune microenvironment that is suboptimal for HBV replication. On the other hand, increased production of various cytokines and chemokines results in progressive inflammation and activation of hepatic stellate cells (HSCs). The release of damage-associated molecular pattern molecules (DAMPs) also accelerates the inflammatory response. In addition, elevated intracellular levels of ROS may enhance HBV replication via the activation of p38. Figure created in BioRender.com. BA, bile acid; IFNγ, interferon-gamma; TNF, tumor necrosis factor; IL, interleukin; TG, triglyceride; TGFβ, transforming growth factor beta; TNF, tumor necrosis factor.
Effects of HBV on systemic metabolism
Growing evidence has suggested that patients with HBV infection are at a decreased risk of developing NAFLD. For example, in the study by Wong et al.,13 HBV infection was associated with a lower prevalence of fatty liver, hypertriglyceridemia, and metabolic syndrome in the general Chinese population in Hong Kong. Similarly, in a large cohort of Korean adults, HBsAg seropositivity was associated with a lower risk of developing NAFLD.16 Thomopoulos et al.31 studied the prevalence of biopsy-proven liver steatosis in patients with CHB in Greece. Hepatic steatosis was observed in 18% of CHB patients and 73.8% of them presented with grade 1 steatosis. These results suggested an inverse association between HBV infection and MAFLD prevalence.
Interestingly, HBV infection is associated with favorable serum lipid profiles, including lower levels of triglycerides, low-density lipoprotein cholesterol, and higher levels of high-density lipoprotein cholesterol;16 however, there is no conclusive evidence of the association of HBV infection with metabolic syndrome, insulin resistance, and the risk of arteriosclerosis.
The mechanisms underlying the effect of HBV infection on liver steatosis are not well characterized. Some studies have found that HBV-infected patients are associated with increased adiponectin,32,33 which may ameliorate hepatic steatosis.34 Besides, HBV infection may influence cholesterol metabolism by binding of the pre-S1 domain to the cellular receptor sodium-taurocholate cotransporting polypeptide, leading to increased conversion of intracellular cholesterol to bile acids and increased uptake of lipoprotein-associated cholesterol.35 Additional studies are required to better understand the mechanisms involved in glucose and lipid metabolism in HBV-infected patients.
Synergistic effect of MAFLD and CHB on liver disease progression
Liver steatosis itself is a major risk factor for liver- and non-liver-related morbidity and mortality.4 Although liver steatosis is associated with lower HBV viral load15 and increased chances of HBsAg clearance,17 several studies have demonstrated the synergistic role of fatty liver and CHB in promoting liver disease progression.15,36 In a study by Peleg et al.,15 liver steatosis was associated with an increased risk of all-cause mortality and cancer development in CHB patients, regardless of HBV viral load. Other studies have shown that coincidental metabolic syndrome, which is one of the key diagnostic criteria for MAFLD, increases the risk of liver fibrosis progression17,37 and liver cirrhosis38 in CHB patients independent of the viral load and alanine aminotransferase level. Obesity also accelerates hepatitis B-related mortality and HCC.39 Therefore, patients with CHB should be closely monitored for coexisting fatty liver disease irrespective of viral load and HBV seromarkers, as coexisting fatty liver disease may aggravate liver fibrosis, and increase the risk of cirrhosis and HCC.
The mechanisms underlying the synergistic effect of fatty liver on CHB progression remain unclear. Here, we suggest several potential mechanisms regarding the impact of liver steatosis on CHB progression (Fig. 1). Increased hepatocyte damage in steatosis leads to the release of damage-associated molecular pattern molecules, which may enhance the inflammatory response.40 Increased infiltration of neutrophils, monocytes, and γδ T cells28 and other inflammatory cells in NASH accelerates liver inflammation and fibrosis via production of various cytokines and chemokines.40 In addition, elevated intracellular levels of reactive oxygen species (ROS)41 induced by NASH may facilitate HBV replication. Recently, we have found that neutrophil-derived ROS can activate p38 mitogen-activated protein kinase (MAPK), which then promotes the progression of NAFLD.42 P38 MAPK is known to promote HBV replication;43,44 thus, neutrophil-derived ROS may also facilitate HBV replication via the activation of p38 MAPK in NAFLD.
Therapeutic challenges in patients with MAFLD and CHB
There are many unanswered questions regarding the treatment of patients with coincidental MAFLD and CHB. For example, it is not clear whether the absorption and bioavailability of antiviral drugs are affected by hepatic fat accumulation and the commonly associated metabolic abnormalities, such as diabetes and hyperlipidemia. Patients with coincidental MAFLD and CHB may exhibit different responses to antiviral therapies compared to patients with CHB alone. Reports regarding the influence of fatty liver on the antiviral therapies in CHB patients have been inconsistent.45 Since HBV gene expression is closely regulated by nutritional state via the metabolic regulators, further studies are required to explore the effectiveness of lifestyle interventions, such as diet control, physical activity, and weight reduction, in patients with coincidental MAFLD and CHB. Apart from this, treatment of the metabolic abnormalities, such as diabetes, hypertension, and dyslipidemia, should be carefully managed and the impact of these treatments on HBV replication should be cautiously monitored. For example, PPARα has been shown to promote HBV replication;26 thus, PPARα agonists should be cautiously used in patients with coincidental MAFLD and CHB. Besides, antiviral drugs may influence metabolism. For example, tenofovir disoproxil fumarate, which is one of the first-line antiviral treatments for CHB, has been shown to decrease the serum lipid profile in CHB patients.46 Finally, the impact of metabolic treatment on progression of CHB remains to be further explored. Notably, statins, which are commonly administered to patients with hyperlipidemia, have been shown to decrease the risk of decompensation in HBV-related cirrhosis47 and HCC.48,49
Collectively, emerging evidence suggests a negative association between MAFLD and CHB in terms of HBV seromarkers and fatty liver onset; however, MAFLD and CHB synergistically exacerbate liver fibrosis and HCC progression. The mechanisms underlying the interplay between MAFLD and CHB are still poorly understood. Further clinical studies are required to better understand the clinical features and provide more evidence for the management of patients with coincidental MAFLD and CHB.
Hepatitis C and MAFLD
It is well known that chronic HCV infection is associated with liver steatosis, especially in patients infected with HCV genotype 3. The reported prevalence of liver steatosis in patients with HCV infection varies between 40% and 80%; however, this prevalence decreases to approximately 40% when other factors that cause fatty liver, such as alcohol abuse, obesity, and diabetes, have been excluded.50 This suggests that both viral factors and host factors (such as metabolic disorders) contribute to liver steatosis in patients with HCV infection. Therefore, assessment of metabolic risk factors is required for hepatitis C patients, especially in those with concomitant fatty liver.
In the definition of NAFLD, HCV (genotype 3) is considered as a secondary cause of hepatic fat accumulation and is excluded from the criteria of NAFLD. However, in the new definition of MAFLD, patients who have HCV infection and also meet the criteria for the diagnosis of MAFLD are defined as having concomitant MAFLD with HCV infection. Renaming of “NAFLD” to “MAFLD” divided hepatitis C into two categories, i.e. “hepatitis C with MAFLD” and “hepatitis C without MAFLD”. This new classification will help distinguish the causes of liver steatosis and will lead to better management of hepatitis C patients. Notably, patients with concomitant MAFLD and HCV infection and patients with HCV-induced liver steatosis both present with fatty liver. The differential diagnosis of the causes of fatty liver should mainly rely on the presence of metabolic risk factors, viral load and genotype, and the responsiveness to antiviral therapy.51 The differences with respect to the clinical presentations of concomitant MAFLD and HCV infection and viral steatosis are summarized in Table 1.
Table 1. MAFLD vs. HCV-induced fatty liver: Clinical differences.
| MAFLD with HCV infection | HCV-induced fatty liver | |
|---|---|---|
| Criteria for MAFLD* | Yes | No |
| Genotype-dependent | No | Yes |
| Viral load-related | No | Yes |
| Disappears after antiviral therapy | No | Yes |
*Overweight/obesity, type 2 diabetes mellitus, or metabolic dysregulation. HCV, hepatitis C virus; MAFLD, metabolic dysfunction-associated fatty liver disease.
Relationship between HCV infection and metabolism
Lipids are important for HCV replication and virion assembly, and lipoproteins are required for HCV circulation in the blood.52 HCV infection alters lipid metabolism in many ways, including by impairing very low density lipoprotein (VLDL) secretion, increasing lipogenesis, and decreasing lipid oxidation.53 HCV infection is associated with dyslipidemia, through lower levels of total cholesterol and triglycerides, and hypobetalipoproteinaemia.54 The multifaceted interaction between HCV and lipid metabolism has been previously reviewed.50,53
Although there is a paucity of studies on the impact of MAFLD on HCV replication, several studies have suggested the complex effects of fatty acid metabolism on HCV replication. For example, fatty acids, especially polyunsaturated fatty acids, were shown to inhibit HCV replication.55,56 In a study by Yamane et al.,56 lipid peroxidation, which is a feature of NASH, was shown to restrict HCV replication in hepatocytes. On the contrary, Hofmann et al.57 demonstrated that knockdown of fatty acid elongases and desaturases, which are responsible for de novo fatty acid synthesis, can disrupt HCV replication in hepatocytes. These results suggest the existence of a complex network that regulates HCV RNA replication in fatty liver.
Liver steatosis, which is frequently found in patients with chronic hepatitis C, accelerates fibrosis58 and HCC59 progression and is associated with poor response to interferon-alpha (IFN-α)-based therapy.60 In patients with genotype 3 infection, the severity of liver steatosis was shown to correlate with the viral load and was ameliorated following successful antiviral treatment.61 Besides, chronic HCV infection is associated with an increased risk of diabetes62 and higher levels of insulin resistance.63 Insulin resistance and elevated body mass index have been reported to impair sustained response to IFNα-based therapy.64 Although there is no conclusive evidence of the association between HCV and metabolic syndrome,65 based on these published data, we predict that patients with concomitant MAFLD and hepatitis C are likely to have poor clinical outcomes, including accelerated liver fibrosis progression, and increased risk of HCC and atherosclerosis compared to patients with hepatitis C alone.
Management of hepatitis C and MAFLD
Direct antiviral agents (DAAs), which show improved tolerability and high efficacy for HCV clearance, have now been recommended as the first-line treatment for hepatitis C.66,67 In addition to the high efficacy for HCV eradication, DAA treatment also showed a beneficial impact on systemic metabolism. In a study by Sun et al.,68 DAA therapy led to increased triglyceride-to-cholesterol ratio in VLDL, indicating an improvement in HCV-related unfavorable plasma lipid parameters. Besides, successful treatment with DAAs is associated with improved glycemic control69 and a significant decrease in the risk of cardiovascular disease events.70 The changes in liver steatosis following DAA treatment have not been well studied.
Apart from DAA therapy, HCV patients with concomitant MAFLD should be appropriately managed with lifestyle changes and specific drugs. Since DAAs present an important potential for drug-drug interactions (DDIs), assessment of DDIs prior to initiation of DAA therapy is important in patients with concomitant MAFLD. For example, statins and antihypertensive agents may potentially interact with DAAs.66,67 Thus, due caution should be exercised while selecting a suitable DAA. To date, the effects of diabetes, obesity, and metabolic syndrome on the antiviral efficacy of DAAs have not been carefully evaluated. It will be interesting to compare the efficiency of DAA therapy in hepatitis C patients with or without MAFLD.
Acute viral hepatitis and MAFLD
The association of MAFLD and acute viral hepatitis (such as acute hepatitis A and acute hepatitis E) has not been reported. However, published data from experimental animal models suggest that preexisting liver steatosis may lead to more severe liver damage. Secondary stimuli such as lipopolysaccharide/alcohol71,72 can induce more severe liver injury in mice fed with high-fat diet compared with mice fed with chow diet. Besides, metabolic disorders such as diabetes and obesity may also accelerate liver injury. Zhang et al.73 found that diabetes is an independent risk factor for adverse outcomes, especially mortality, in patients with acute HEV infection. It will be interesting to explore the relationship between MAFLD and acute hepatitis in the future.
Conclusions
The global burden of chronic liver disease has increased over the past decade.74 NAFLD is the most rapidly growing cause of cirrhosis and liver cancer worldwide, while viral hepatitis remains the most common contributor to liver disease-related mortality in China.75 A new definition of “MAFLD”, which emphasizes the metabolic disorders, will help update the clinical practices for liver diseases. There are a series of pertinent questions in the context of patients with concomitant MAFLD and viral hepatitis (Table 2), with some of them remaining unanswered. Management of patients with concomitant MAFLD and viral hepatitis requires close collaboration between hepatologists and endocrinologists. Further clinical trials are required to determine the optimal treatments for these patients.
Table 2. Potential questions in clinical practice for patients with concomitant MAFLD and chronic hepatitis B/C.
| Potential questions in clinical practice | HBV | HCV |
|---|---|---|
| Does hepatitis B/C promote fatty liver? | No | Yes |
| Does HBV/HCV infection increase the risk of diabetes? | Unknown | Yes |
| Does HBV/HCV infection worsen hyperlipidemia? | No | No |
| Does fatty liver promote liver fibrosis in chronic hepatitis? | Yes | Yes |
| Does fatty liver promote HCC in chronic hepatitis? | Yes | Yes |
| Does fatty liver facilitate viral replication? | No | Yes |
| Does fatty liver reduce the therapeutic effects of antiviral therapy? | Unknown | IFN-α—Yes DAA—unknown |
| Do drugs for diabetes, hypertension, and dyslipidemia interact with antiviral therapies? | Unknown | IFN-α—unknown For some DAAs—Yes |
DAAs, direct antiviral agents; HBV, hepatitis B virus; HCV, hepatitis C virus; HCC, hepatocellular carcinoma; IFN-α, interferon-alpha; MAFLD, metabolic dysfunction-associated fatty liver disease.
Acknowledgments
The authors acknowledge the valuable suggestions and careful editing by Dr. Bin Gao, Laboratory of Liver Diseases, NIAAA/NIH.
Abbreviations
- CHB
chronic hepatitis B
- CHC
chronic hepatitis C
- DAAs
direct antiviral agents
- DDIs
drug-drug interactions
- FOXO1
forkhead Box O1
- FXR
Farnesoid X receptor
- HBsAg
hepatitis B virus surface antigen
- HCC
hepatocellular carcinoma
- HNF4α
hepatocyte nuclear factor 4α
- IFN-α
interferon-alpha
- MAFLD
metabolic dysfunction-associated fatty liver disease
- MAPK
mitogen-activated protein kinase
- NAFLD
nonalcoholic fatty liver disease
- NASH
nonalcoholic hepatitis
- NK
natural killer
- PGC1α
peroxisome proliferator activated receptor γ-coactivator 1 alpha
- PPARα
peroxisome proliferator activated receptor alpha
- ROS
reactive oxygen species
- VLDL
very low density lipoprotein
References
- 1.Ludwig J, Viggiano TR, McGill DB, Oh BJ. Nonalcoholic steatohepatitis: Mayo Clinic experiences with a hitherto unnamed disease. Mayo Clin Proc. 1980;55(7):434–438. [PubMed] [Google Scholar]
- 2.Younossi Z, Anstee QM, Marietti M, Hardy T, Henry L, Eslam M, et al. Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol. 2018;15(1):11–20. doi: 10.1038/nrgastro.2017.109. [DOI] [PubMed] [Google Scholar]
- 3.European Association for the Study of the Liver (EASL) European Association for the Study of Diabetes (EASD) European Association for the Study of Obesity (EASO) EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. J Hepatol. 2016;64(6):1388–1402. doi: 10.1016/j.jhep.2015.11.004. [DOI] [PubMed] [Google Scholar]
- 4.Chalasani N, Younossi Z, Lavine JE, Charlton M, Cusi K, Rinella M, et al. The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67(1):328–357. doi: 10.1002/hep.29367. [DOI] [PubMed] [Google Scholar]
- 5.Eslam M, Newsome PN, Sarin SK, Anstee QM, Targher G, Romero-Gomez M, et al. A new definition for metabolic dysfunction-associated fatty liver disease: An international expert consensus statement. J Hepatol. 2020;73(1):202–209. doi: 10.1016/j.jhep.2020.03.039. [DOI] [PubMed] [Google Scholar]
- 6.Eslam M, Sanyal AJ, George J, International Consensus Panel MAFLD: A Consensus-Driven Proposed Nomenclature for Metabolic Associated Fatty Liver Disease. Gastroenterology. 2020;158(7):1999–2014.e1. doi: 10.1053/j.gastro.2019.11.312. [DOI] [PubMed] [Google Scholar]
- 7.Younossi ZM, Rinella ME, Sanyal AJ, Harrison SA, Brunt EM, Goodman Z, et al. From NAFLD to MAFLD: Implications of a Premature Change in Terminology. Hepatology. 2021;73(3):1194–1198. doi: 10.1002/hep.31420. [DOI] [PubMed] [Google Scholar]
- 8.Wong MCS, Huang JLW, George J, Huang J, Leung C, Eslam M, et al. The changing epidemiology of liver diseases in the Asia-Pacific region. Nat Rev Gastroenterol Hepatol. 2019;16(1):57–73. doi: 10.1038/s41575-018-0055-0. [DOI] [PubMed] [Google Scholar]
- 9.Bertoletti A, Gehring AJ. The immune response during hepatitis B virus infection. J Gen Virol. 2006;87(Pt 6):1439–1449. doi: 10.1099/vir.0.81920-0. [DOI] [PubMed] [Google Scholar]
- 10.Ferrari C. HBV and the immune response. Liver Int. 2015;35(Suppl 1):121–128. doi: 10.1111/liv.12749. [DOI] [PubMed] [Google Scholar]
- 11.Kong X, Sun R, Chen Y, Wei H, Tian Z. gammadeltaT cells drive myeloid-derived suppressor cell-mediated CD8+ T cell exhaustion in hepatitis B virus-induced immunotolerance. J Immunol. 2014;193(4):1645–1653. doi: 10.4049/jimmunol.1303432. [DOI] [PubMed] [Google Scholar]
- 12.Wang MM, Wang GS, Shen F, Chen GY, Pan Q, Fan JG. Hepatic steatosis is highly prevalent in hepatitis B patients and negatively associated with virological factors. Dig Dis Sci. 2014;59(10):2571–2579. doi: 10.1007/s10620-014-3180-9. [DOI] [PubMed] [Google Scholar]
- 13.Wong VW, Wong GL, Chu WC, Chim AM, Ong A, Yeung DK, et al. Hepatitis B virus infection and fatty liver in the general population. J Hepatol. 2012;56(3):533–540. doi: 10.1016/j.jhep.2011.09.013. [DOI] [PubMed] [Google Scholar]
- 14.Cheng YL, Wang YJ, Kao WY, Chen PH, Huo TI, Huang YH, et al. Inverse association between hepatitis B virus infection and fatty liver disease: a large-scale study in populations seeking for check-up. PLoS One. 2013;8(8):e72049. doi: 10.1371/journal.pone.0072049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Peleg N, Issachar A, Sneh Arbib O, Cohen-Naftaly M, Braun M, Leshno M, et al. Liver steatosis is a strong predictor of mortality and cancer in chronic hepatitis B regardless of viral load. JHEP Rep. 2019;1(1):9–16. doi: 10.1016/j.jhepr.2019.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Joo EJ, Chang Y, Yeom JS, Ryu S. Hepatitis B virus infection and decreased risk of nonalcoholic fatty liver disease: A cohort study. Hepatology. 2017;65(3):828–835. doi: 10.1002/hep.28917. [DOI] [PubMed] [Google Scholar]
- 17.Mak LY, Hui RW, Fung J, Liu F, Wong DK, Cheung KS, et al. Diverse effects of hepatic steatosis on fibrosis progression and functional cure in virologically quiescent chronic hepatitis B. J Hepatol. 2020;73(4):800–806. doi: 10.1016/j.jhep.2020.05.040. [DOI] [PubMed] [Google Scholar]
- 18.Lee HA, Lee HW, Kim IH, Park SY, Sinn DH, Yu JH, et al. Extremely low risk of hepatocellular carcinoma development in patients with chronic hepatitis B in immune-tolerant phase. Aliment Pharmacol Ther. 2020;52(1):196–204. doi: 10.1111/apt.15741. [DOI] [PubMed] [Google Scholar]
- 19.Hu D, Wang H, Wang H, Wang Y, Wan X, Yan W, et al. Non-alcoholic hepatic steatosis attenuates hepatitis B virus replication in an HBV-immunocompetent mouse model. Hepatol Int. 2018;12(5):438–446. doi: 10.1007/s12072-018-9877-7. [DOI] [PubMed] [Google Scholar]
- 20.Aharoni-Simon M, Hann-Obercyger M, Pen S, Madar Z, Tirosh O. Fatty liver is associated with impaired activity of PPARgamma-coactivator 1alpha (PGC1alpha) and mitochondrial biogenesis in mice. Lab Invest. 2011;91(7):1018–1028. doi: 10.1038/labinvest.2011.55. [DOI] [PubMed] [Google Scholar]
- 21.Wan X, Zhu X, Wang H, Feng Y, Zhou W, Liu P, et al. PGC1alpha protects against hepatic steatosis and insulin resistance via enhancing IL10-mediated anti-inflammatory response. FASEB J. 2020;34(8):10751–10761. doi: 10.1096/fj.201902476R. [DOI] [PubMed] [Google Scholar]
- 22.Zhang Y, Castellani LW, Sinal CJ, Gonzalez FJ, Edwards PA. Peroxisome proliferator-activated receptor-gamma coactivator 1alpha (PGC-1alpha) regulates triglyceride metabolism by activation of the nuclear receptor FXR. Genes Dev. 2004;18(2):157–169. doi: 10.1101/gad.1138104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rhee J, Inoue Y, Yoon JC, Puigserver P, Fan M, Gonzalez FJ, et al. Regulation of hepatic fasting response by PPARgamma coactivator-1alpha (PGC-1): requirement for hepatocyte nuclear factor 4alpha in gluconeogenesis. Proc Natl Acad Sci U S A. 2003;100(7):4012–4017. doi: 10.1073/pnas.0730870100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vega RB, Huss JM, Kelly DP. The coactivator PGC-1 cooperates with peroxisome proliferator-activated receptor alpha in transcriptional control of nuclear genes encoding mitochondrial fatty acid oxidation enzymes. Mol Cell Biol. 2000;20(5):1868–1876. doi: 10.1128/mcb.20.5.1868-1876.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Puigserver P, Rhee J, Donovan J, Walkey CJ, Yoon JC, Oriente F, et al. Insulin-regulated hepatic gluconeogenesis through FOXO1-PGC-1alpha interaction. Nature. 2003;423(6939):550–555. doi: 10.1038/nature01667. [DOI] [PubMed] [Google Scholar]
- 26.Bar-Yishay I, Shaul Y, Shlomai A. Hepatocyte metabolic signalling pathways and regulation of hepatitis B virus expression. Liver Int. 2011;31(3):282–290. doi: 10.1111/j.1478-3231.2010.02423.x. [DOI] [PubMed] [Google Scholar]
- 27.Bhattacharjee J, Kirby M, Softic S, Miles L, Salazar-Gonzalez RM, Shivakumar P, et al. Hepatic Natural Killer T-cell and CD8+ T-cell Signatures in Mice with Nonalcoholic Steatohepatitis. Hepatol Commun. 2017;1(4):299–310. doi: 10.1002/hep4.1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Torres-Hernandez A, Wang W, Nikiforov Y, Tejada K, Torres L, Kalabin A, et al. gammadelta T Cells Promote Steatohepatitis by Orchestrating Innate and Adaptive Immune Programming. Hepatology. 2020;71(2):477–494. doi: 10.1002/hep.30952. [DOI] [PubMed] [Google Scholar]
- 29.Jung MC, Pape GR. Immunology of hepatitis B infection. Lancet Infect Dis. 2002;2(1):43–50. doi: 10.1016/s1473-3099(01)00172-4. [DOI] [PubMed] [Google Scholar]
- 30.Feldstein AE, Canbay A, Angulo P, Taniai M, Burgart LJ, Lindor KD, et al. Hepatocyte apoptosis and fas expression are prominent features of human nonalcoholic steatohepatitis. Gastroenterology. 2003;125(2):437–443. doi: 10.1016/s0016-5085(03)00907-7. [DOI] [PubMed] [Google Scholar]
- 31.Thomopoulos KC, Arvaniti V, Tsamantas AC, Dimitropoulou D, Gogos CA, Siagris D, et al. Prevalence of liver steatosis in patients with chronic hepatitis B: a study of associated factors and of relationship with fibrosis. Eur J Gastroenterol Hepatol. 2006;18(3):233–237. doi: 10.1097/00042737-200603000-00002. [DOI] [PubMed] [Google Scholar]
- 32.Hsu CS, Liu WL, Chao YC, Lin HH, Tseng TC, Wang CC, et al. Adipocytokines and liver fibrosis stages in patients with chronic hepatitis B virus infection. Hepatol Int. 2015;9(2):231–242. doi: 10.1007/s12072-015-9616-2. [DOI] [PubMed] [Google Scholar]
- 33.Chiang CH, Lai JS, Hung SH, Lee LT, Sheu JC, Huang KC. Serum adiponectin levels are associated with hepatitis B viral load in overweight to obese hepatitis B virus carriers. Obesity (Silver Spring) 2013;21(2):291–296. doi: 10.1002/oby.20000. [DOI] [PubMed] [Google Scholar]
- 34.Matsuzawa Y. Adiponectin: a key player in obesity related disorders. Curr Pharm Des. 2010;16(17):1896–1901. doi: 10.2174/138161210791208893. [DOI] [PubMed] [Google Scholar]
- 35.Oehler N, Volz T, Bhadra OD, Kah J, Allweiss L, Giersch K, et al. Binding of hepatitis B virus to its cellular receptor alters the expression profile of genes of bile acid metabolism. Hepatology. 2014;60(5):1483–1493. doi: 10.1002/hep.27159. [DOI] [PubMed] [Google Scholar]
- 36.Choi HSJ, Brouwer WP, Zanjir WMR, de Man RA, Feld JJ, Hansen BE, et al. Nonalcoholic Steatohepatitis Is Associated With Liver-Related Outcomes and All-Cause Mortality in Chronic Hepatitis B. Hepatology. 2020;71(2):539–548. doi: 10.1002/hep.30857. [DOI] [PubMed] [Google Scholar]
- 37.Wong GL, Chan HL, Yu Z, Chan AW, Choi PC, Chim AM, et al. Coincidental metabolic syndrome increases the risk of liver fibrosis progression in patients with chronic hepatitis B—a prospective cohort study with paired transient elastography examinations. Aliment Pharmacol Ther. 2014;39(8):883–893. doi: 10.1111/apt.12658. [DOI] [PubMed] [Google Scholar]
- 38.Wong GL, Wong VW, Choi PC, Chan AW, Chim AM, Yiu KK, et al. Metabolic syndrome increases the risk of liver cirrhosis in chronic hepatitis B. Gut. 2009;58(1):111–117. doi: 10.1136/gut.2008.157735. [DOI] [PubMed] [Google Scholar]
- 39.Yu MW, Shih WL, Lin CL, Liu CJ, Jian JW, Tsai KS, et al. Body-mass index and progression of hepatitis B: a population-based cohort study in men. J Clin Oncol. 2008;26(34):5576–5582. doi: 10.1200/JCO.2008.16.1075. [DOI] [PubMed] [Google Scholar]
- 40.Magee N, Zou A, Zhang Y. Pathogenesis of Nonalcoholic Steatohepatitis: Interactions between Liver Parenchymal and Nonparenchymal Cells. Biomed Res Int. 2016;2016:5170402. doi: 10.1155/2016/5170402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hwang S, He Y, Xiang X, Seo W, Kim SJ, Ma J, et al. Interleukin-22 Ameliorates Neutrophil-Driven Nonalcoholic Steatohepatitis Through Multiple Targets. Hepatology. 2020;72(2):412–429. doi: 10.1002/hep.31031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hwang S, Wang X, Rodrigues RM, Ma J, He Y, Seo W, et al. Protective and Detrimental Roles of p38alpha Mitogen-Activated Protein Kinase in Different Stages of Nonalcoholic Fatty Liver Disease. Hepatology. 2020;72(3):873–891. doi: 10.1002/hep.31390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chang WW, Su IJ, Chang WT, Huang W, Lei HY. Suppression of p38 mitogen-activated protein kinase inhibits hepatitis B virus replication in human hepatoma cell: the antiviral role of nitric oxide. J Viral Hepat. 2008;15(7):490–497. doi: 10.1111/j.1365-2893.2007.00968.x. [DOI] [PubMed] [Google Scholar]
- 44.Yang Q, Zhang Q, Zhang X, You L, Wang W, Liu W, et al. HoxA10 Facilitates SHP-1-Catalyzed Dephosphorylation of p38 MAPK/STAT3 To Repress Hepatitis B Virus Replication by a Feedback Regulatory Mechanism. J Virol. 2019;93(7):e01607-18. doi: 10.1128/JVI.01607-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhang J, Lin S, Jiang D, Li M, Chen Y, Li J, et al. Chronic hepatitis B and non-alcoholic fatty liver disease: Conspirators or competitors? Liver Int. 2020;40(3):496–508. doi: 10.1111/liv.14369. [DOI] [PubMed] [Google Scholar]
- 46.Shaheen AA, AlMattooq M, Yazdanfar S, Burak KW, Swain MG, Congly SE, et al. Tenofovir disoproxil fumarate significantly decreases serum lipoprotein levels compared with entecavir nucleos(t)ide analogue therapy in chronic hepatitis B carriers. Aliment Pharmacol Ther. 2017;46(6):599–604. doi: 10.1111/apt.14218. [DOI] [PubMed] [Google Scholar]
- 47.Chang FM, Wang YP, Lang HC, Tsai CF, Hou MC, Lee FY, et al. Statins decrease the risk of decompensation in hepatitis B virus- and hepatitis C virus-related cirrhosis: A population-based study. Hepatology. 2017;66(3):896–907. doi: 10.1002/hep.29172. [DOI] [PubMed] [Google Scholar]
- 48.Goh MJ, Sinn DH, Kim S, Woo SY, Cho H, Kang W, et al. Statin Use and the Risk of Hepatocellular Carcinoma in Patients With Chronic Hepatitis B. Hepatology. 2020;71(6):2023–2032. doi: 10.1002/hep.30973. [DOI] [PubMed] [Google Scholar]
- 49.Simon TG, Duberg AS, Aleman S, Hagstrom H, Nguyen LH, Khalili H, et al. Lipophilic Statins and Risk for Hepatocellular Carcinoma and Death in Patients With Chronic Viral Hepatitis: Results From a Nationwide Swedish Population. Ann Intern Med. 2019;171(5):318–327. doi: 10.7326/M18-2753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bugianesi E, Salamone F, Negro F. The interaction of metabolic factors with HCV infection: does it matter? J Hepatol. 2012;56(Suppl 1):S56–65. doi: 10.1016/S0168-8278(12)60007-5. [DOI] [PubMed] [Google Scholar]
- 51.Negro F. Facts and fictions of HCV and comorbidities: steatosis, diabetes mellitus, and cardiovascular diseases. J Hepatol. 2014;61(1 Suppl):S69–78. doi: 10.1016/j.jhep.2014.08.003. [DOI] [PubMed] [Google Scholar]
- 52.Negro F. HCV infection and metabolic syndrome: which is the chicken and which is the egg? Gastroenterology. 2012;142(6):1288–1292. doi: 10.1053/j.gastro.2011.12.063. [DOI] [PubMed] [Google Scholar]
- 53.Negro F. Abnormalities of lipid metabolism in hepatitis C virus infection. Gut. 2010;59(9):1279–1287. doi: 10.1136/gut.2009.192732. [DOI] [PubMed] [Google Scholar]
- 54.Schaefer EA, Chung RT. HCV and host lipids: an intimate connection. Semin Liver Dis. 2013;33(4):358–368. doi: 10.1055/s-0033-1358524. [DOI] [PubMed] [Google Scholar]
- 55.Kapadia SB, Chisari FV. Hepatitis C virus RNA replication is regulated by host geranylgeranylation and fatty acids. Proc Natl Acad Sci U S A. 2005;102(7):2561–2566. doi: 10.1073/pnas.0409834102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Yamane D, McGivern DR, Wauthier E, Yi M, Madden VJ, Welsch C, et al. Regulation of the hepatitis C virus RNA replicase by endogenous lipid peroxidation. Nat Med. 2014;20(8):927–935. doi: 10.1038/nm.3610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hofmann S, Krajewski M, Scherer C, Scholz V, Mordhorst V, Truschow P, et al. Complex lipid metabolic remodeling is required for efficient hepatitis C virus replication. Biochim Biophys Acta Mol Cell Biol Lipids. 2018;1863(9):1041–1056. doi: 10.1016/j.bbalip.2018.06.002. [DOI] [PubMed] [Google Scholar]
- 58.Fartoux L, Chazouilleres O, Wendum D, Poupon R, Serfaty L. Impact of steatosis on progression of fibrosis in patients with mild hepatitis C. Hepatology. 2005;41(1):82–87. doi: 10.1002/hep.20519. [DOI] [PubMed] [Google Scholar]
- 59.Ohata K, Hamasaki K, Toriyama K, Matsumoto K, Saeki A, Yanagi K, et al. Hepatic steatosis is a risk factor for hepatocellular carcinoma in patients with chronic hepatitis C virus infection. Cancer. 2003;97(12):3036–3043. doi: 10.1002/cncr.11427. [DOI] [PubMed] [Google Scholar]
- 60.Poynard T, Ratziu V, McHutchison J, Manns M, Goodman Z, Zeuzem S, et al. Effect of treatment with peginterferon or interferon alfa-2b and ribavirin on steatosis in patients infected with hepatitis C. Hepatology. 2003;38(1):75–85. doi: 10.1053/jhep.2003.50267. [DOI] [PubMed] [Google Scholar]
- 61.Rubbia-Brandt L, Giostra E, Mentha G, Quadri R, Negro F. Expression of liver steatosis in hepatitis C virus infection and pattern of response to alpha-interferon. J Hepatol. 2001;35(2):307. doi: 10.1016/s0168-8278(01)00087-3. [DOI] [PubMed] [Google Scholar]
- 62.White DL, Ratziu V, El-Serag HB. Hepatitis C infection and risk of diabetes: a systematic review and meta-analysis. J Hepatol. 2008;49(5):831–844. doi: 10.1016/j.jhep.2008.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hui JM, Sud A, Farrell GC, Bandara P, Byth K, Kench JG, et al. Insulin resistance is associated with chronic hepatitis C virus infection and fibrosis progression [corrected] Gastroenterology. 2003;125(6):1695–1704. doi: 10.1053/j.gastro.2003.08.032. [DOI] [PubMed] [Google Scholar]
- 64.Romero-Gomez M, Del Mar Viloria M, Andrade RJ, Salmeron J, Diago M, Fernandez-Rodriguez CM, et al. Insulin resistance impairs sustained response rate to peginterferon plus ribavirin in chronic hepatitis C patients. Gastroenterology. 2005;128(3):636–641. doi: 10.1053/j.gastro.2004.12.049. [DOI] [PubMed] [Google Scholar]
- 65.Wang CC, Cheng PN, Kao JH. Systematic review: chronic viral hepatitis and metabolic derangement. Aliment Pharmacol Ther. 2020;51(2):216–230. doi: 10.1111/apt.15575. [DOI] [PubMed] [Google Scholar]
- 66.Ghany MG, Morgan TR, AASLD-IDSA Hepatitis C Guidance Panel Hepatitis C Guidance 2019 Update: American Association for the Study of Liver Diseases-Infectious Diseases Society of America Recommendations for Testing, Managing, and Treating Hepatitis C Virus Infection. Hepatology. 2020;71(2):686–721. doi: 10.1002/hep.31060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.European Association for the Study of the Liver EASL recommendations on treatment of hepatitis C: Final update of the series. J Hepatol. 2020;73(5):1170–1218. doi: 10.1016/j.jhep.2020.08.018. [DOI] [PubMed] [Google Scholar]
- 68.Sun HY, Cheng PN, Tseng CY, Tsai WJ, Chiu YC, Young KC. Favouring modulation of circulating lipoproteins and lipid loading capacity by direct antiviral agents grazoprevir/elbasvir or ledipasvir/sofosbuvir treatment against chronic HCV infection. Gut. 2018;67(7):1342–1350. doi: 10.1136/gutjnl-2017-313832. [DOI] [PubMed] [Google Scholar]
- 69.Hum J, Jou JH, Green PK, Berry K, Lundblad J, Hettinger BD, et al. Improvement in Glycemic Control of Type 2 Diabetes After Successful Treatment of Hepatitis C Virus. Diabetes Care. 2017;40(9):1173–1180. doi: 10.2337/dc17-0485. [DOI] [PubMed] [Google Scholar]
- 70.Butt AA, Yan P, Shuaib A, Abou-Samra AB, Shaikh OS, Freiberg MS. Direct-Acting Antiviral Therapy for HCV Infection Is Associated With a Reduced Risk of Cardiovascular Disease Events. Gastroenterology. 2019;156(4):987–996.e988. doi: 10.1053/j.gastro.2018.11.022. [DOI] [PubMed] [Google Scholar]
- 71.Ma X, Hua J, Mohamood AR, Hamad AR, Ravi R, Li Z. A high-fat diet and regulatory T cells influence susceptibility to endotoxin-induced liver injury. Hepatology. 2007;46(5):1519–1529. doi: 10.1002/hep.21823. [DOI] [PubMed] [Google Scholar]
- 72.Chang B, Xu MJ, Zhou Z, Cai Y, Li M, Wang W, et al. Short- or long-term high-fat diet feeding plus acute ethanol binge synergistically induce acute liver injury in mice: an important role for CXCL1. Hepatology. 2015;62(4):1070–1085. doi: 10.1002/hep.27921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Zhang S, Chen C, Peng J, Li X, Zhang D, Yan J, et al. Investigation of underlying comorbidities as risk factors for symptomatic human hepatitis E virus infection. Aliment Pharmacol Ther. 2017;45(5):701–713. doi: 10.1111/apt.13938. [DOI] [PubMed] [Google Scholar]
- 74.Asrani SK, Devarbhavi H, Eaton J, Kamath PS. Burden of liver diseases in the world. J Hepatol. 2019;70(1):151–171. doi: 10.1016/j.jhep.2018.09.014. [DOI] [PubMed] [Google Scholar]
- 75.Paik JM, Golabi P, Younossi Y, Mishra A, Younossi ZM. Changes in the Global Burden of Chronic Liver Diseases From 2012 to 2017: The Growing Impact of NAFLD. Hepatology. 2020;72(5):1605–1616. doi: 10.1002/hep.31173. [DOI] [PubMed] [Google Scholar]