Abstract
Background
Accurate proxy-report questionnaires, adapted to the child’s developmental stage, are required to monitor 24-h movement behaviors in young children, especially for large samples and low-resource settings.
Objectives
This review aimed to summarize available studies evaluating measurement properties of proxy-report questionnaires assessing physical activity, sedentary behavior and/or sleep in children aged 0–5 years.
Methods
Systematic literature searches were carried out in the PubMed, Embase and SPORTDiscus databases, up to January 2021. For physical activity and sedentary behavior questionnaires this is a review update, whereas for sleep questionnaires we included all relevant studies published up to now. Studies had to evaluate at least one of the measurement properties of a proxy-report questionnaire assessing at least duration and/or frequency of physical activity, sedentary behavior and/or sleep in 0- to 5-year-old children. The COnsensus-based Standards for the selection of health Measurement INstruments (COSMIN) guideline was used to evaluate the quality of evidence.
Results
Thirty-three studies were included, examining a total of 37 questionnaires. Ten questionnaires were designed for infants, two for toddlers, 11 for preschoolers, and 14 for a broader age range targeting multiple of these age groups. Twenty questionnaires assessed constructs of sleep, four assessed constructs of physical activity, two assessed screen behavior, five assessed constructs of both physical activity and sedentary behavior, and six assessed constructs of all 24-h movement behaviors. Content validity was evaluated for six questionnaires, structural validity for two, internal consistency for three, test-retest reliability for 16, measurement error for one, criterion validity for one, and construct validity for 26 questionnaires. None of the questionnaires were considered sufficiently valid and/or reliable for assessing one or more movement behaviors in 0- to 5-year-old children, and the quality of evidence was mostly low or very low.
Conclusions
Valid and/or reliable questionnaires assessing 24-h movement behaviors in 0- to 5-year-olds are lacking. High-quality studies are therefore required, to develop proxy-report questionnaires and evaluate their measurement properties.
PROSPERO registration number
CRD42020169268.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12966-022-01251-x.
Keywords: 24-h movement behaviors, Infants, Toddlers, Preschoolers, Questionnaires, Parent-report, Measurement properties, Validity, Reliability
Background
Establishing healthy movement behaviors in early childhood is necessary to support the growth and development of young children and the maintenance of their long-term health [1–4]. Recent studies indicate the importance of the combination of all 24-h movement behaviors, encompassing physical activity, sedentary behavior, and sleep [5–10]. Valid, reliable, responsive, affordable, and feasible measurement instruments adapted to the child’s developmental stage are required to monitor 24-h movement behaviors in young children. Direct observation is considered a suitable criterion measure of different movement behaviors in children [11, 12]. However, observation can be very time consuming and thus costly, and is thereby not feasible to use on a large scale. Alternatively, physical activity, sedentary behavior and sleep in young children can be measured using accelerometers [3, 12, 13]. Although accelerometers are considered valid and reliable for measuring movement behaviors in children and adolescents [14, 15], its validity is yet to be obtained for the youngest age group (i.e., infants: 0–1 year old) [13]. In addition, accelerometer output is processed by a number of subjective decisions in order to translate acceleration data into time estimates of movement behaviors. Specifically, it is unknown which analyses methods provide the most accurate classification of physical activity, sedentary behavior and sleep in infants. Additionally, current procedures do not take into account that accelerometer output in very young children may reflect movements of others, e.g., that of parents who carry their child or push them in a stroller [16]. Alternative to observation and accelerometry, parent- or caregiver (proxy-) report questionnaires can be used as a measurement instrument for children’s 24-h movement behaviors. Questionnaires can be used to assess movement behaviors on a large scale in a relatively convenient and affordable way, with the additional advantage of obtaining information about the type (e.g., active play, screen time) and context (e.g., outside, alone) of the behavior. Unfortunately, proxy-report questionnaires have their own limitations such as recall and social desirability bias [17]. Furthermore, the intermittent and unstructured pattern of movement behaviors in young children complicates accurate reporting of these behaviors [17].
To date, a number of proxy-report questionnaires have been developed to assess physical activity, sedentary behavior and/or sleep in 0- to 5-year-old children. A few systematic reviews examined the measurement properties of these questionnaires in young children [18–21], searching the literature up to 2014 for questionnaires on sleep [18], up to 2015 for sedentary behavior [20] and up to 2018 for physical activity [19, 21]. However, concerning questionnaires on sleep, questionnaires for the youngest age group were not evaluated (i.e., 0- to 2-year-old children) [18]. Unfortunately, these reviews did not identify any questionnaires that can be considered both reliable and valid for assessing physical activity, sedentary behavior and/or sleep in children aged < 5 years [18–21]. Although a review published in 2011 [22] and updated in 2020 [23] provided an overview of the psychometric analyses performed at the available pediatric sleep questionnaires, including questionnaires for 0- to 5-year-old children, measurement property results were not reported in the review update [23]. In addition, quality of evidence was not considered in both reviews, limiting the conclusions that can be drawn regarding the best available questionnaires [22, 23]. Similarly, a recently published systematic review provided an overview of measurement tools used to assess screen time in 0- to 6-year-old children [22]. Although measurement properties of the available questionnaires were reported, a comprehensive evaluation of the measurement properties, including quality of evidence, was lacking [24]. Furthermore, as the research interest of all 24-h movement behaviors in young children has grown, new questionnaires might have been developed over the last few years. For this reason, an update of previous reviews is required, including physical activity, sedentary behavior and sleep. To be able to select the most appropriate questionnaires to assess 24-h movement behaviors, an overview of the characteristics and measurement properties of the available questionnaires for young children is highly warranted.
Therefore, the purpose of this review was to summarize all studies examining measurement properties (e.g., reliability and validity) of proxy-report questionnaires assessing physical activity, sedentary behavior and/or sleep in children aged 0–5 years. We evaluated the quality of evidence for each measurement property, including a methodological quality assessment of included studies. Additionally, we provided an overview of the characteristics of the evaluated questionnaires (e.g., the target population and format of the questionnaires).
Methods
We registered this review on PROSPERO (international prospective register of systematic reviews; registration number: CRD42020169268) and followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [25].
Literature search
Systematic literature searches were carried out in PubMed, Embase, and SPORTDiscus. For physical activity and sedentary behavior questionnaires this review is an update of previous reviews [19–21], whereas for sleep questionnaires we included all relevant studies published up to now. Therefore, separate searches were carried out, i.e., one for physical activity and sedentary behavior, and one for sleep. The full search strategies can be found in Additional file 1.
For physical activity and sedentary behavior questionnaires, we searched the literature from December 2015 (i.e., last search period for sedentary behavior questionnaires [20]) until December 2019. In PubMed more overlap in time was maintained (search from May 2015), as our previous searches showed that the PubMed time filter can be inaccurate due to incorrect labeling of publication dates. For sleep questionnaires there was no lower limit for publication date, and databases were searched up until January 2020. A combined update search (i.e., physical activity, sedentary behavior and sleep) was completed on 6 January 2021.
Both search strategies focused on terms related to young children (e.g., infant, toddler, preschooler), proxy-report measures (e.g., questionnaire, proxy-report) and measurement properties (e.g., reliability, reproducibility, validity). For the physical activity and sedentary behavior search, these terms were used in AND-combination with terms related to physical activity (e.g., motor activity, exercise) OR sedentary behavior (e.g., stationary behavior, screen-time). For the sleep search, these terms were used in AND-combination with terms related to sleep (e.g., bedtime, nap). In all databases, studies in animals and children with a variety of diseases or disorders (e.g., autism, attention deficit disorder) were excluded using NOT-combinations.
Inclusion and exclusion criteria
Studies were included when: (1) the study evaluated at least one of the measurement properties of a proxy-report questionnaire assessing physical activity, sedentary behavior and/or sleep; (2) the proxy-report questionnaire under study reported at least data on the duration and/or frequency of physical activity, sedentary behavior and/or sleep; (3) the study included apparently healthy children, born term (> 37 weeks), aged < 5 years or a wider age range with the results for 0- to 5-year-old children described separately; (4) the study was published in English in a peer-reviewed journal; and (5) the full-text was available.
Studies were excluded when (1) measurement properties were evaluated in a specific subpopulation or clinical sample (e.g., children with sleep problems); (2) construct validity was only evaluated by examining the relationship between the questionnaire and a non-similar construct (e.g., between physical activity and body mass index (BMI)); (3) structural validity and/or internal consistency were evaluated for questionnaires that represent a formative measurement model as these analysis are not relevant when the items of a scale or subscale form or cause the construct and are therefore not supposed to be correlated (e.g., items assessing different physical activities that together form the construct duration of total physical activity) [26, 27]; (4) responsiveness was evaluated without using a comparison measure to assess a questionnaire’s ability to detect change (e.g., accelerometer).
Selection procedures
Articles were imported in EndNote X9.1, and subsequently duplicate articles were removed. Titles and abstracts of potentially relevant articles were scanned by two independent researchers (JA and TA) using Rayyan. Next, full texts were obtained and independently screened for eligibility by the same two researchers. Additionally, reference lists of all full-text articles were screened for additional studies. Disagreements were resolved through discussion.
Inclusion of studies from previous reviews
To draw definite conclusions regarding the best available questionnaires, we also included studies from the three aforementioned reviews evaluating questionnaires assessing physical activity and sedentary behavior [19–21]. As these reviews were not restricted to questionnaires aimed to assess young children’s behaviors, only the studies that evaluated proxy-report questionnaires for children aged < 5 years were included, in line with our inclusion criteria.
Data extraction
For all eligible studies, two independent reviewers (JA and either JG or AV) extracted data using a structured form. Disagreements were resolved through discussion. The following data was extracted: evaluated measurement properties, study population (i.e., population included in study), target population (i.e., population for which the questionnaire was developed), measurement instrument (i.e., name, construct(s), format), respondent, recall period, comparison method (in case of validity), time interval (in case of test-retest reliability), statistical method used, and results of the examined measurement properties (i.e., reliability, validity, responsiveness).
Methodological quality assessment
Risk of bias was assessed by rating the methodological quality of included studies, using the COnsensus-based Standards for the selection of health Measurement Instruments (COSMIN) checklist [28]. Risk of bias refers to whether results are trustworthy based on the methodological quality of the study. For each examined measurement property, the study design requirements were rated as either very good, adequate, doubtful, or inadequate quality [28]. The lowest score counts method was applied, e.g., if one item was rated inadequate, the final methodological quality was rated as inadequate. For the rating of construct validity studies, the measurement properties of the comparator instrument(s) had to be taken into account. Measurement properties of accelerometers were evaluated using the systematic review of Lettink et al. [29]. An overview of the methodological quality ratings that could be given to different comparator instruments can be found in Additional file 2.
Two independent reviewers (JA and either TA, MC or AL) rated the methodological quality of the included studies. In the case of disagreement, a third researcher was consulted (either TA or MC).
Rating study results
The study results of each measurement property were rated against the criteria for good measurement properties proposed in the COSMIN guideline (i.e., sufficient (+), insufficient (−), inconsistent (±) or intermediate (?)) [30]. Below is indicated for each measurement property which outcomes were considered sufficient (+). Outcomes were considered insufficient (−) when these criteria were not met, and intermediate (?) when not all necessary information was reported. Inconsistent (±) outcomes were only applicable for validity and reliability studies reporting multiple outcomes per questionnaire, and were rated as described below. The COSMIN methodology for evaluating content validity was used to rate the results of content validity studies [31]. For none of the included (versions of) questionnaires multiple studies on a measurement property were available. For this reason, quantitatively pooling or qualitatively summarizing study results was not possible.
Content validity
Content validity is defined as “the degree to which the content of a measurement instrument is an adequate reflection of the construct to be measured” [32]. Content validity consists of three components: relevance (e.g., relevant for construct and target population of interest), comprehensiveness (e.g., all key concepts are included), and comprehensibility (e.g., items, response options, and recall period are understood by the population of interest as intended) [31]. Relevance, comprehensiveness, and comprehensibility were rated using the criteria for good content validity [31]. All three components had to be rated as sufficient, in order to rate the overall content validity as sufficient [31].
Internal structure: structural validity, internal consistency, and cross-cultural validity
Internal structure refers to how the different items in a questionnaire are related, which is important to know for deciding how items might be combined into a scale or subscale [32]. To examine internal structure, three different measurement properties should be evaluated: (1) structural validity, (2) internal consistency and (3) cross-cultural validity. Structural validity and/or internal consistency are only applicable to questionnaires that represent a reflective measurement model, i.e., in which the items of the questionnaire are a reflection of the construct to be measured [27]. In a reflective model, the items are supposed to be correlated and interchangeable [26]. As a reflective measurement model is only applicable to questionnaires assessing sleep quality (i.e., items are a reflection of the construct sleep quality), structural validity and/or internal consistency were only evaluated for questionnaires assessing sleep quality.
Structural validity is defined as “the degree to which the scores of a questionnaire are an adequate reflection of the dimensionality of the construct to be measured” [32], and is usually evaluated by factor analysis. In case of exploratory factor analysis, structural validity outcomes were considered sufficient when factor loadings were ≥ 0.30 [33]. In case of confirmatory factor analyses, structural validity outcomes were considered sufficient when the comparative fit index or Tucker–Lewis index was > 0.95, mean square error of approximation was < 0.06, or standardized root mean residual was < 0.08 [30, 34].
Internal consistency refers to “the degree of the interrelatedness among the items”, and is often evaluated by Cronbach’s alpha [28, 32]. Internal consistency outcomes were considered sufficient if Cronbach’s alpha values were ≥ 0.70 and at least low quality of evidence for sufficient structural validity was provided (as rated by COSMIN guidelines) [30].
Cross-cultural validity or measurement invariance is defined as “the degree to which performance of the items of a translated or culturally adapted questionnaire are an adequate reflection of the performance of the items of an original version of the questionnaire” [32]. Cross-cultural validity is evaluated by group factor analyses or differential item functioning (DIF). When no important differences were found between group factors or DIF for group factors, cross-cultural validity/measurement invariance was considered sufficient [30].
Reliability
Reliability is defined as “the degree to which the measurement is free from measurement error” [32]. Reliability outcomes were considered sufficient if the intraclass correlation coefficients (ICC) or Kappa (K) values were ≥ 0.70 [30]. When Pearson or Spearman correlations were used to assess reliability, correlation coefficients had to be ≥0.80, because these correlations do not take systematic errors into account [26]. Most studies reported multiple correlations per questionnaire for test–retest reliability, e.g., separate correlations for each question or item. For this reason, an overall questionnaire rating was applied, i.e., incorporating all correlations, in order to obtain a final test–retest reliability rating for each questionnaire. When ≥75% of correlations were acceptable, a sufficient (+) rating was received, when ≥50% and < 75% of correlations were acceptable an inconsistent (±) rating was received, and an insufficient (−) rating was received when < 50% of correlations were acceptable.
Measurement error
Measurement error is “the systematic and random error of a score that is not attributed to true changes in the construct to be measured” [32]. Measurement error outcomes were considered sufficient when the standard error of measurement (SEM), smallest detectable change (SDC) (i.e., defined as “the smallest change that can be detected by the instrument, beyond measurement error” [26]) or limits of agreement (LoA) were smaller than the minimal important change (MIC) (i.e., defined as “the smallest change in score in the construct to be measured that is perceived as important by clinicians or relevant others” [26]) [30]. As the MIC was not defined, we could not give a final rating of the measurement error. Instead, we interpreted the measurement error outcomes per study.
Criterion and construct validity
Criterion validity is defined as “the degree to which the scores of a measurement instrument are an adequate reflection of a gold standard”. Criterion validity was considered sufficient when correlations with the gold standard were ≥ 0.70 [32]. We considered doubly labeled water as a reasonable gold standard for questionnaires aiming to assess physical activity energy expenditure. In addition, we considered polysomnography as a gold standard for questionnaires assessing sleep. Other comparators (e.g., accelerometers, diaries) were considered to reflect construct validity. Construct validity is “the degree to which the scores of a measurement instrument are consistent with (a priori drafted) hypotheses” (e.g., with regard to relationships to scores of other instruments, or differences between relevant groups) [32]. Since a priori drafted hypotheses for construct validity were often lacking, we formulated criteria with regard to the relationships with other instruments (e.g., accelerometers). Table 1 provides an overview of the criteria for evaluating the results of construct validity studies. These criteria were in line with previous reviews [20, 21], and are based on the similarity of the construct that is measured [30]. Additionally, we formulated criteria for studies that evaluated construct validity by comparing subgroups (i.e., children with and without sleep problems). The criteria were subdivided by level of evidence, level 1 indicating strong evidence, level 2 indicating moderate evidence, and level 3 indicating weak evidence. These levels of evidence indicate the confidence in the comparison method to accurately assess the relevant construct. Most studies reported multiple correlations with a comparator instrument, therefore, the same overall rating as used for reliability was applied for each questionnaire (i.e., sufficient (+), inconsistent (±), or insufficient (−)).
Table 1.
A priori drafted hypotheses for the evaluation of construct validity of questionnaires assessinga constructs of physical activity, sedentary behavior and/or sleep, subdivided by level of evidenceb, and criteria for acceptable correlations/relationships with comparator instruments or subgroupscd
| Construct assessed | Level 1 | Level 2 | Level 3 |
|---|---|---|---|
| Physical activity | |||
| Physical activity, all constructs (i.e., including at least indoor and outdoor activities of all intensities) | Acc. cut-point/algorithm for TPA ≥ 0.60 | Acc. cut-point/algorithm for MPA, VPA or MVPA ≥0.40 | Questionnaire or diary, corresponding constructs ≥0.70 |
| Physical activity, not all constructs or timeframes | Acc. cut-point/algorithm for TPA; corresponding timeframe ≥0.60 |
Acc. cut-point/algorithm for TPA; total daytime ≥0.40 Acc. cut-point/algorithm for MPA and VPA ≥ 0.50 |
Questionnaire or diary, corresponding constructs ≥0.70 |
| Physical activity, single constructs (e.g., outdoor play) |
Acc. cut-point/algorithm for TPA ≥ 0.40 Acc. cut-point/algorithm for MPA and VPA ≥ 0.50 |
Questionnaire or diary, corresponding constructs ≥0.70 | |
| Vigorous physical activity | Acc. cut-point/algorithm for VPA ≥ 0.60 | Acc. cut-point/algorithm for TPA ≥ 0.40 | Questionnaire or diary, corresponding constructs ≥0.70 |
| Moderate physical activity | Acc. cut-point/algorithm for MPA ≥ 0.60 | Acc. cut-point/algorithm for TPA ≥ 0.40 | Questionnaire or diary, corresponding constructs ≥0.70 |
| Light physical activity | Acc. cut-point/algorithm for LPA ≥ 0.60 | Acc. cut-point/algorithm for TPA ≥ 0.40 | Questionnaire or diary, corresponding constructs ≥0.70 |
| Moderate-to-vigorous physical activity | Acc. cut-point/algorithm for MVPA ≥0.60 | Acc. cut-point/algorithm for TPA ≥ 0.40 | Questionnaire or diary, corresponding constructs ≥0.70 |
| Sedentary behavior | |||
| Sedentary behavior, all constructs (i.e., including at least screen time and non-screen leisure time activities) | Acc. cut-point/algorithm for SB ≥ 0.60 | Questionnaire or diary, corresponding constructs ≥0.70 | |
| Stationary behavior | Acc. cut-point/algorithm for SB ≥ 0.50 | Questionnaire or diary, corresponding constructs ≥0.70 | |
| Screen time | Diary, logs ≥0.60 | Questionnaire corresponding constructs ≥0.70 | |
| Sedentary behavior, not all constructs or time frames |
Acc. cut-point/algorithm for SB; corresponding timeframe ≥0.60 Acc. cut-point/algorithm for SB; non-corresponding timeframe ≥0.50 |
Questionnaire or diary, corresponding constructs ≥0.70 | |
| Sleep behavior | |||
| Sleep behavior, all constructs (i.e., including at least total sleep duration, sleep latency and night awakenings) | Videosomnography ≥0.60 | Acc. cut-point/algorithm for sleep ≥0.40 |
Questionnaire, log, or diary, corresponding constructs ≥0.70 Acc. or diary not significantly different in the measured sleep construct. Discriminative validity: children without sleep problems score significantly better than children with sleep problems. |
| Sleep behavior, not all constructs or time frames | Videosomnography ≥0.60 | Acc. cut-point/algorithm for sleep ≥0.40 |
Questionnaire, log, or diary, corresponding constructs ≥0.70 Acc. or diary not significantly different in the measured sleep construct. Discriminative validity: children without sleep problems score significantly better than children with sleep problems. |
| Sleep duration | Videosomnography ≥0.60 | Acc. cut-point/algorithm for sleep ≥0.50 |
Questionnaire, log, or diary, corresponding constructs ≥0.70 Acc. or diary not significantly different in the measured sleep duration. Discriminative validity: children without sleep problems score significantly better than children with sleep problems. |
Abbreviations: Acc accelerometer, LPA light physical activity, MPA moderate physical activity, MVPA moderate-to-vigorous physical activity, TPA total physical activity, VPA vigorous physical activity
a Since a priori drafted hypotheses for construct validity were often lacking in included studies, we formulated criteria with regard to the relationships with other instruments (e.g., accelerometers) or subgroups
b Level of evidence: level 1 indicating strong evidence, level 2 indicating moderate evidence, and level 3 indicating weak evidence. These levels of evidence indicate the confidence in the comparison method to accurately assess the relevant construct
b The criteria for acceptable correlations with comparator instruments are based on the similarity of the construct that is measured
d Table adapted from previous reviews by Hidding et al. [20, 21]
Responsiveness
Responsiveness is “the ability of a measurement instrument to detect change over time in the construct to be measured” [32]. As none of the included studies evaluated responsiveness of the questionnaire under study, responsiveness is not reported.
Quality of evidence grading
The quality of evidence was graded using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach, as proposed in the COSMIN guideline [30], indicating the trustworthiness of the measurement property results of questionnaires. The GRADE approach consists of four levels (i.e., high, moderate, low, very low), which depend on the presence of four risk factors: (1) risk of bias (i.e., the methodological quality of the studies), (2) inconsistency (i.e., unexplained inconsistency of results across studies), (3) imprecision (i.e., total sample size of the available studies), and (4) indirectness (i.e., evidence from different populations than the population of interest in this review) [30]. The quality of evidence was subsequently downgraded with one, two or three levels for each factor to moderate, low, or very low when there was risk of bias, inconsistency in results, a low sample size, or indirect results [30]. Because the COSMIN methodology has been updated since publication of the previous reviews, we re-evaluated all included studies from previous reviews on methodological quality and regraded the quality of evidence [30]. The grading of the quality of evidence was done for each measurement property and for each questionnaire separately by one researcher (JA). The ratings of measurement property outcomes (i.e., sufficient, insufficient, inconsistent, intermediate) were only presented in the results section for the measurement properties of questionnaires that received a high or moderate quality of evidence grading, as these results are considered most trustworthy. Consequently, a questionnaire can only be considered as valid/reliable when the quality of evidence is at least moderate, and the reliability/validity results are sufficient.
Results
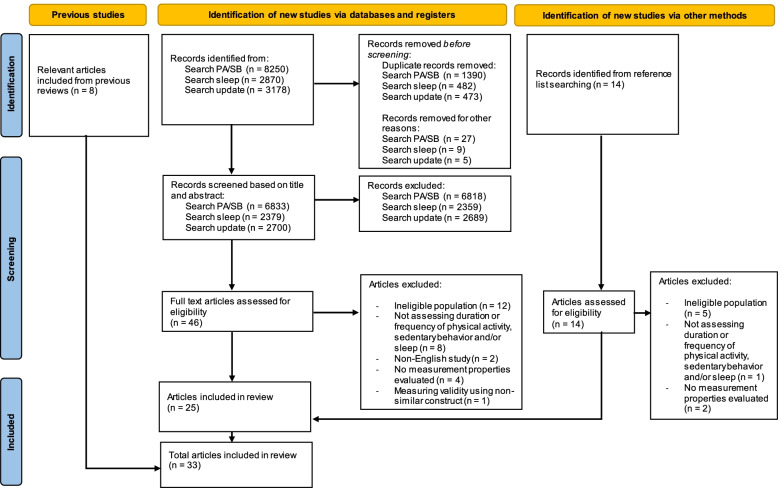
Systematic literature searches using the PubMed, Embase, and SPORTDiscus databases yielded a total of 12,390 unique articles. After title and abstract screening, 46 full-texts were screened. Additionally, 14 articles were found through cross-reference searches. Therefore, a total of 60 full-text articles were assessed for eligibility, of which 25 were included. Additionally, we included 8 relevant articles from previous reviews [19–21], resulting in 33 articles that evaluated a total of 37 different (versions of) questionnaires (see Fig. 1 for the full selection process). Four questionnaires were (translated) versions of the Brief Infant Sleep Questionnaire (BISQ) [35–38], and three questionnaires were versions of the Children’s Sleep Habits Questionnaire (CSHQ) [39–41]. Table 2 presents the characteristics of all included questionnaires. Tables 3-6 summarize the results for content validity, internal consistency and structural validity, reliability, and criterion validity and construct validity.
Fig. 1.
PRISMA flow diagram of study inclusion. Abbreviations: PA physical activity, SB sedentary behavior
Table 2.
Characteristics of questionnaires assessing physical activity, sedentary behavior and/or sleep in 0- to 5-year-old children, sorted by behavior and target population
| Questionnaire Name | Behavior (PA, SB, ScT, S) b | Sub-constructs | Target population (age) c | Respondent | Recall period | Format: Dimensions (F, D, I) d | Format: Number of items | Format: Scores |
|---|---|---|---|---|---|---|---|---|
| Sleep diary (nn) [38] | S | Night awakenings, wake after sleep onset (WASO), sleep latency, sleep onset, sleep duration | Infants (nr) | Parent | Current day | F, D | 4 items | Continuous: time, duration (h/min), frequency (times per night) |
| Sleep diary by phone (nn) [42] | S | Sleep onset time, rise time, sleep period, number of night awakenings | Infants (nr) | Mother | Day | F, D | Unclear | Questions answered by phone |
| Electronic-diary (nn) [43] | S | Sleep during day (08-20 h), sleep during night (20-08 h), sleep over 24 h | Infants (nr) | Parent | Current day | D | Unclear | Unclear |
| Paper-diary (nn) [43] | S | Sleep during day (08-20 h), sleep during night (20-08 h), sleep over 24 h | Infants (nr) | Parent | Current day (5 min epochs) | D | Logline | Continuous: duration (h/min), derived from sleep state every 5 min |
| Sleep diary (nn) [44] | S | Night sleep duration, longest nighttime sleep, daytime sleep duration, night awakenings, sleep onset time, and sleep offset time | Infants (nr) | Parent | Current day (5 min epochs) | F, D | Logline | Continuous: time, duration (h/min), frequency (times per night), derived from sleep state every 5 min |
| Sleep survey (including items from the BISQ and CSHQ) [44] | S | Night sleep duration, longest nighttime sleep, daytime sleep duration, night awakenings, sleep onset time, and sleep offset time | Infants (nr) | Parent | Typical day | F, D | 6 items | Continuous: time, duration (h/min), frequency (times per night) |
| Sleep and Settle Questionnaire (SSQ) [45] | S |
Sleep patterns (number and duration of sleeps, night awakenings), time to settle to sleep, duration of crying Additionally: Temperament awake, confidence parent to get baby to sleep, attribution of unsettled infant behavior, whether parents are bothered by this |
Infants (nr) | Primary caregivers | Last week | F, D |
12 items Total questionnaire: 34 items |
Continuous: duration (h/min), frequency (sleeps per day/times per night) Ordinal: 5-point Likert scale ranging from 1 ‘Didn’t bother me at all’ to 5 ‘Bothered me extremely’ |
| Children’s Sleep Habits Questionnaire - Infant version (CSHQ-I) [39] | S | Bedtime resistance, sleep anxiety, daytime sleepiness, and positive sleep habitse | Infants (0–1 year old) | Mother | Typical week | F, D, I | 31 items across 4 subscales: Bedtime resistance (11 items), Sleep anxiety (10 items), Positive sleep habits (6 items), and Daytime sleepiness (5 items)e |
Continuous: time, duration (h/min) Ordinal: 3-point scale: “usually” (5–7 times per week); “sometimes” (2–4 times per week;) and “rarely” (0–1 time per week) (+not applicable) |
| Brief Infant Sleep Questionnaire (BISQ) [38] | S | Night awakenings, wake after sleep onset (WASO), sleep latency, sleep onset | Infants (nr) | Parent | Typical day | F, D | Unclear (other studies: 13 items) | Continuous: time, duration (h/min), frequency (times per night) |
| Expanded version of the Brief Infant Sleep Questionnaire (BISQ), Turkish version [37] | S |
Nocturnal sleep duration (7 pm-7 am), daytime sleep durations (7 am-7 pm), number of night awakenings, duration of wakefulness during night, settling time Additionally:Method falling asleep, location of sleep, preferred body position, perception of sleep problems |
Infants (nr) | Parent | Typical day | F, D | 13 items (including 4 demographic) | Continuous: time, duration (h/min), frequency (times per night) |
| BISQ Spanisch version (BISQ-E) [35] | S |
Time of sleep onset, duration of night-time sleep, duration of daytime sleep, total sleep duration, night-time awakenings, duration of night-time awakenings Additionally: Method falling asleep, location of sleep, preferred body position, perception of sleep problems |
Infants and toddlers (3–30 months old) | Parent | Typical day | F, D | 14 items (4 demographic, 10 sleep habits) | Continuous: time, duration (h/min), frequency (times per night) |
| BISQ (Nepali version) [36] | S |
Nocturnal and daytime sleep duration, night awakenings, duration night wakefulness, sleep onset time, sleep settling time Additionally: Method falling asleep, location of sleep, preferred body position, perception of sleep problems |
Infants and toddlers (0–3 years old) | Parent | Typical day | F, D | Unclear (other studies: 13 items) | Continuous: time, duration (h/min), frequency (times per night) |
| Sleep diary (nn) [46] | S | Sleep onset time, sleep offset time, nocturnal sleep time duration, number of night awakenings (> 5 min), wake minutes during nocturnal sleeping | Infants and toddlers (nr) | Mother | Current day (30 min epochs) | F, D | Unclear |
Nominal: general questions per day Continuous: duration (h/min), derived from sleep state every 30 min |
| Sleep diary (nn) [47] | S | Sleep duration, sleep efficiency | Toddlers (2 years old) | Mother | Current day (30 min epochs) | D | Unclear | Continuous: duration (h/min), derived from sleep state every 30 min |
| Own questionnaire (nn) [48] | S | Get up time, bedtime, sleeping hours | Preschoolers (3–4 years old) | Parent | Current day | D | 3 items | Continuous: time, duration (h/min) |
| Parent log (nn) [49] | S | Afternoon naps, bedtime, sleep latency, awakenings, sleep end time morning. Sleep onset time was calculated by adding sleep latency to the bedtime | Preschoolers (3–5 years old) | Parent (with input day care workers) | Current day | F, D | 10 items (4 just before going to bed, and 6 first thing in the morning) |
Continuous: time, duration (min) Ordinal: frequency of awakenings giving 4 options: 0, 1, 2, 3 or more |
| Children’s Sleep Habits Questionnaire (CSHQ) [41] | S |
Quantitative: bedtime, wake-up time, daily sleep time, number and duration of night- awakenings Qualitative: Bedtime resistance, sleep onset delay, sleep duration, sleep anxiety, night-awakenings, parasomnias, obstructive sleep apnea, and daytime sleepinesse |
Preschoolers (3–6 years old) | Parent | Typical week, typical weekday and weekend day | F, D, I | 33 items across 8 subscalese |
Continuous: time, duration (h/min), frequency (times per night) Ordinal: 3-point scale: “usually” (5–7 times per week); “sometimes” (2–4 times per week;) and “rarely” (0–1 time per week) (+not applicable) |
| Children’s Sleep Habits Questionnaire - Chinese version (CSHQ) [40] | S | Bedtime resistance, sleep onset delay, sleep duration, sleep anxiety, night-time awakenings, parasomnias, sleep disordered breathing, daytime sleepinesse | Preschoolers (3–6 years old) | Parent/Caregiver | Typical week | F, D, I | 33 items across 8 subscales: Bedtime resistance (6 items), Sleep-onset delay (1 item), Sleep duration (3 items), Sleep anxiety (4 items), Night-time awakenings (3 items), Parasomnias (7 items), Sleep disordered breathing (3 items), and Daytime sleepiness (8 items)e |
Continuous: time, duration (h/min) Ordinal: 3-point scale: “usually” (5–7 times per week); “sometimes” (2–4 times per week;) and “rarely” (0–1 time per week) (+not applicable) |
| Children’s ChronoType Questionnaire (CCTQ) - Japanese version [50] | S | Sleep-wake parameters, chronotype and morningness/eveningness (M/E) | Preschoolers (3–6 years old) | Parent | Typical weekday and weekend day | F, D | 27 items across 3 subscales: Sleep–wake parameters (16 items), M/E (10 items), and Chronotype (1 item) |
Continuous: time, duration (min), frequency (days per week) Nominal: yes/no Ordinal: different 5-point scales (e.g., ranging from Very difficult to Not at all a problem) |
| Children’s Sleep-Wake Scale (CSWS) [51] | S | Going to bed, falling asleep, arousing and awakening during the night, returning to sleep after waking during the night, waking in the morning | Children (2–8 years old) | Parent | Typical day | F, D, I | 25 items across 5 subscales: Going to bed (5 items), falling asleep (5 items), arousing and awakening during the night (5 items), returning to sleep after waking during the night (5 items), waking in the morning (5 items) | Ordinal: 6-point scale (Never, Once in a while, Sometimes, Quite Often, Frequently - if not Always, and Always) |
| Technology Use Questionnaire (TechU-Q) [52] | ScT | Frequency, duration and purpose of use of multiple technology devices (television, computers, tablet computers, mobile phones, and electronic games) | Infants, toddlers, preschoolers (0–5 years old) | Parent/Caregiver | Typical weekday and weekend day | F, D | Unclear | Continuous: duration (h/min), frequency (times per week) |
| PREPS questionnaire [53] | ScT |
Screen time Additionally: Children’s cognitions/personal attributes, parental cognitions, home and neighborhood environment |
Toddlers (1–3 years old) | Parent | Typical weekday and weekend day | D |
4 items Total questionnaire:83 items |
Continuous: duration (h/min) |
| Outdoor time checklist [54]a | PA | Time playing outdoors | Toddlers and preschoolers (2–5 years old) | Parent | 24 h (wake-up to bedtime) | D | 2 items | Ordinal: 5-point scale with the following responses: 0 min; 1–15 min; 16–30 min; 31–60 min; and over 60 min |
| Parental report – outdoor time recall questionnaire [54]a | PA | Time playing outdoors | Toddlers and preschoolers (2–5 years old) | Parent | Typical week/weekend day in the last month | D | 2 items | Continuous: time spent (min) |
| Modified Burdette proxy report [55]a | PA | Indoor and outdoor active play at family child care homes | Toddlers and preschoolers (2–5 years old) | Family Child Care Home Providers | Arrival until lunch time and lunch time until departure | D | 1 item (2 times) | Ordinal: 5-point scale with the following responses: 0 min; 1–15 min; 16–30 min; 31–60 min; and over 60 min |
| Modified Harro proxy report [55]a | PA | Sitting, low-to moderate intensity indoor activities, low-to-moderate intensity outdoor activities, moderate-to-vigorous intensity indoor activities, and moderate-to-vigorous outdoor activities | Toddlers and preschoolers (2–5 years old) | Family Child Care Home Providers | Arrival until lunch and lunch until departure | D | 5 items (2 times) | Continuous: time spent (min) |
| KidActive-Q [56]a | PA, ScT | Method of transportation to and from daycare, time spent outdoors, time spent watching television and/or playing computer games, and athletic activities performed on a regular basis | Toddlers and preschoolers (2–6 years old) | Parent | Usual, past few months | F, D | 10–12 items |
Nominal: yes/no Ordinal: different options for frequency and/or duration |
| Early Years Physical Activity Questionnaire (EY-PAQ) [57] | PA, SB | Various indoor and outdoor activities, which were grouped according to PA intensity (moderate-to-vigorous physical activity or sedentary time) | Toddlers and preschoolers (2–5 years old) | Parent | Typical week in previous month | F, D | 16 items (MVPA: 10, ST: 6) | Ordinal: number of days per week, and duration giving 4 options: 1) up to 15 min/day; 2) 16–30 min/day; 3) 31–60 min/day; or 4) free-text for > 60 min/day |
| Preschool-aged Children’s Physical Activity Questionnaire (Pre-PAQ) [58]a | PA, SB | Time spent in car, time spent walking, activity, eating in front of television, attend organized physical activity, use of facilities to play or be physically active | Preschoolers (3–5 years old) | Parent/Guardian | Last week, yesterday, last weekend | F, D |
Total questionnaire = 37 questions divided into 4 sections Number of items differs depending on answers |
Continuous: duration (h/min) Nominal: yes/no Ordinal: 6-poimt scale ranging from daily to rarely |
| Children’s Physical Activity Questionnaire (CPAQ) [59]a | PA, SB | Various physical activity and sedentary activities, which were grouped in: sports, leisure time activities, and activities at school | Preschoolers (4–5 year old) | Parent | Last week | F, D |
PA: 34 items SB: 15 items |
Continuous: duration (h/min), frequency (times Mon-Fri/times Sat-Sun) |
| Healthy Kids [60, 61] | PA, ScT, S |
TV and computer behavior, playing outside, and sleep Additionally: Diet and parenting practices |
Toddlers and preschoolers of low income families (2–5 years old) | Parent/Caregiver | Typical week and day | F, D |
Development study: PA: 4 items, ScT: 5 items, S: 1 item Total questionnaire: 45 items Selected in following study: PA: 1 item, ScT: 2 items, S: 1 item Total questionnaire: 19 items |
Continuous: time, duration (h) Ordinal: 4-point scale ranging from no to every day |
| Physical activity questionnaire for parents of preschoolers in Mexico [62]a | PA, SB, S | Sleep and various indoor and outdoor activities, which were grouped according to PA intensity (sedentary, moderate, and vigorous) | Preschoolers (3–5 years old) | Parent | Typical week and day | F, D |
PA: 3 items SB: 1 item S: 2 items Total questionnaire: 6 items |
Continuous: duration (h/min), frequency (times per day/days per week) Ordinal: 5 categories ranging from 15 min. to more than 1 h |
| Energy balance-related behaviors (ERBs) selfadministered primary caregivers questionnaire (PCQ), from the ToyBox study [63]a | PA, SB, S |
PA: duration sport, transport, playing outside; SB: watching TV/DVD/video, playing games on a computer or game console, quiet play; Sleep: night sleep duration, duration naps. Additionally: Sociodemographic and perinatal factors, water and beverages consumption, snacking |
Preschoolers (nr) | Parent |
PA: Yesterday/last weekday, last weekend day, usually. SB/S: Typical weekday and weekend day |
D |
PA: 27 items SB: 38 items S: 4 items Total questionnaire: 229 items |
Continuous: duration (h/min) Ordinal: 10 categories ranging from Never to I don’t know (30 min and 1 h intervals) |
| Physical activity and sedentary behavior questionnaire (based on Canadian Health Measures Survey) [64]a | PA, SB, ScT |
PA: time outside, time in a gymnasium, recess, unstructured free play; organized physical activities; SB: TV viewing, videos/DVD viewing, computer playing, game console playing, playing handheld devices, stroller time, traveling in motor vehicle |
Infants, toddlers and preschoolers (0–6 years old) | Parent | Typical weekday and weekend day | D |
PA: 5 items SB: 12 items |
Continuous: time spent (min) |
| Surveillance of digital Media hAbits in earLy chiLdhood Questionnaire (SMALLQ™) [65] | PA, SB, ScT, S |
Digital media use outside of pre-school/kindergarten; Non-digital behavior outside of pre-school/kindergarten: indoor and outdoor play, non-screen reading, and drawing; Day time naps, night-time sleep. Additionally: Digital media environment at home, parent digital media habits, perception, concern, awareness and practice of guidelines, demographic information |
Toddlers and preschoolers (2–6 years old) | Parent | Typical weekday and weekend day | Digital media use: F,D; Non-digital behavior: D, Sleep: D, I |
PA/SB/S: 4 items ScT: 4 items Total questionnaire: 25 items across 3 subscales: Digital media use (9 items), Non-digital behavior (3 items), Child and Parent information (13 items) |
Continuous: duration (h/min), and percentage of time spent Ordinal: 6 point-scale ranging from never to 9 or more times a week |
| Family Health Survey (consists a.o. of Outdoor Playtime Recall, InFANT, POI.nz) [66] | PA, SB, ScT, S |
Outdoor play, duration watching TV/DVD, using computer, using smartphone/tablet, playing videogame, sleep duration Additionally: Child parent interactions in relation to physical activity, screen time, and sleep |
Preschoolers (3–6 years old) | Parent | Typical weekday and weekend day | D |
PA: 1 item ScT: 4 items S: 2 items Total questionnaire: number of items differs depending on answers (max. 55 questions) |
Continuous: time, duration (h/min) |
| Healthy Active Preschool Years (HAPPY) parent proxy report survey [67] | PA, SB, ScT, S |
Participation in active transport, non-organized activities, participation in organized activities, attendance at playgroup, usual participation in screen behaviors, quiet play & imaginary games, time spent playing outdoors, night & day sleep time Additionally: Demographic and family profile; child personality, preferences and constraints; parental influence; rules and boundaries, social interaction and support; modeling of physical activity; home physical environment; neighborhood physical environment |
Preschoolers (3–5 years old) | Parent | Typical week, typical weekday and weekend day | F, D |
PA/SB/ScT: 28 items S: 2 items Total questionnaire: 230 items |
Continuous: duration (h) and frequency (times per week) Ordinal: never-daily Nominal: yes/no |
Abbreviations: BISQ Brief Infant Sleep Questionnaire, D duration, F frequency, h hour, I intensity, nn no name, nr not reported, M/E morningness/eveningness, MVPA moderate-to-vigorous activity, PA physical activity, PREPS Parents’ Role in Establishing healthy Physical activity and Sedentary behaviour habits, S sleep, SB sedentary behavior, ScT screen time, ST sedentary time, TV television
a Questionnaire included from previous review
b Behaviors: physical activity (PA), sedentary behavior (SB), screen time (ScT) and/or sleep (S)
c Infants: 0–1 year old, Toddlers: 1–3 years old, Preschoolers: 3–5 years old
d Dimensions: frequency (F), duration (D), and/or intensity (I) of physical activity, sedentary behavior and/or sleep. Quality of sleep is also considered as an intensity
e Note that some of the items included in this questionnaire might reflect indicators of sleep disorders, rather than sleep quality or duration/frequency of sleep
Table 3.
Content validity of physical activity, sedentary behavior and/or sleep questionnaires, including methodological quality, result rating and quality of evidence
| Questionnaire | Study population | Methodological quality a | Results (rating) b | Overall rating c & evidence grading d | ||
|---|---|---|---|---|---|---|
| Relevance | Comprehensiveness | Comprehensibility | ||||
| Children’s Sleep-Wake Scale (CSWS) [51] |
n = 9 pediatric sleep experts n = 30 primary caregivers of 2- to 5-year-old children |
Doubtful | Pediatric sleep experts quantitatively evaluated the content relevance of each item. Items of low content validity were removed which resulted in a CVI of 0.93 for the entire instrument. (+) | Pediatric sleep experts quantitatively evaluated the comprehensiveness of the entire scale as a measure of children’s behavioral sleep quality. Items of low content validity were removed which resulted in a CVI of 0.93 for the entire instrument. (+) |
Primary caregivers provided qualitative feedback on the clarity of directions and items, suitability of the scaling method, and approximate time to complete administration. Following scale revisions, pediatric sleep experts quantitatively evaluated the clarity and conciseness of the administration directions and items. Items of low content validity were removed which resulted in a CVI of 0.93 for the entire instrument. (?) |
?dLow |
| BISQ (Nepali version) [36] | n = 15 parents with child aged < 3 years old | Doubtful | na | na | The respondents had no difficulties in understanding the questionnaire, their answers were appropriate and none of the parents returned the questionnaire for any clarification. (?) | ?Low |
| Surveillance of digital Media hAbits in earLy chiLdhood Questionnaire (SMALLQ™) [65] |
n = 4 experts n = 137 teachers, parents, and school leaders of preschool centers and kindergartens in Singapore |
Doubtful | Experts, including parents, independently reviewed early versions of the questionnaire and guided the development of new questions that were contextually relevant, of concern and interest, and useful. (+) | na | Cognitive load and the ease of understanding of the questionnaire items were tested using a focus group, and, where necessary, the questionnaire items were refined and reorganized. When pilot-testing, average time taken to complete the questionnaire was 20–30 min. Based on qualitative feedback, amendments were made to the questionnaire to enhance its utility and ease of response for participants of the survey. (+) | ?Low |
| Healthy Kids [60] | n = 77 ethnically diverse low-income parents | Doubtful | Relevant items for this tool were identified from results of comprehensive literature reviews for the broad determinants of obesity, corresponding behaviors and survey items. (+) | na | Cognitive interviews provided contextual rich qualitative data for instrument development, including how respondents interpreted text and photographs and their recommendations for changes to improve understanding, consistency of interpretation, and appeal by limited literacy readers. Researchers agreed the message was consistent with the original intent for each item. (+) | ?Low |
| Family Health Survey (consists a.o. of Outdoor Playtime Recall, InFANT, POI.nz) [66] | n = 24 parents of children in ECE (from urban and rural North-eastern Brazil) | Doubtful | na | na | In the cognitive interviews, parents understood most items, but requested modifications to the formatting of the questionnaire, recall period, and the wording of a small number of items. The process of translation and cognitive interviews conducted in Brazilian families resulted in an appropriate cultural adaptation of scales measuring children’s movement behaviors and parenting practices. (+) | ? Low |
| Technology Use Questionnaire (TechU-Q) [52] |
n = 94 parents n = 10 experts (in research of technology use by children, measurement and activity and task behaviors, and childcare professionals) |
Doubtful | na |
Experts were asked if any common technology devices were not included. Overall, experts agreed with the measured constructs and questions. (+) |
Parents found the questions appropriate and no major changes were suggested based on parent feedback. Experts commented on the content validity and made suggestions to wording and question structure. Questions were modified based on substantial and consensus comments. (+) |
?Low |
Abbreviations : BISQ Brief Infant Sleep Questionnaire, COSMIN COnsensus-based Standards for the selection of health Measurement Instruments, CVI content validity index, na not assessed
a Methodological quality based on the COSMIN risk of bias checklist
b Result rating for relevance, comprehensiveness, comprehensibility based on the COSMIN methodology for content validity
c Overall rating of content validity results based on the COSMIN methodology for content validity. If not all ratings of content validity (i.e., relevance, comprehensiveness, comprehensibility) were available, an intermediate (?) score was given
d Quality of evidence grading based on the COSMIN methodology for content validity
Table 6.
Criterion/construct validity of physical activity, sedentary behavior and/or sleep questionnaires, sorted by quality of evidence, level of evidence, result rating and methodological quality
| Questionnaire | Study population b | Comparison measure | Methodological quality c | Results | Rating d , level of evidence e & evidence grading f |
|---|---|---|---|---|---|
| Early Years Physical Activity Questionnaire (EY-PAQ) [57] |
n = 196 Age = 3.2 ± 0.8 years Sex = 49.5% girls |
Accelerometer (Actigraph, GT3X+, right hip, 5 s (Costa)/15 s (Pate) epoch, Costa (SB) / Pate (PA) cut-points [68, 69]) | Doubtful (PA) / Adequate (SB) |
MVPA: MD = 7.1 min/day (LoA = 85.9 ± 200.1); r = 0.03 (no boundaries); r = 0 .30 (boundaries applied) ST: MD = 87.5 min/day (LoA = 376.6 ± 192.7); r = 0.02 (no boundaries); r = 0.19 (boundaries applied) |
PA: – (Level 1) Low SB: – (Level 2) Moderate |
| Sleep diary by phone (nn) [42] |
n = 90 Age: = 3.61 months (range 2.67–5.17 months) Sex = 43% girls |
- Videosomnography (four infrared, high-definition, color Hikvision cameras with internal microphones) - Accelerometer (Actiwatch-2, left ankle, 15 s epoch, default wake threshold value = .888 * average activity count) |
Adequate (Vid) / Doubtful (Acc) |
Videosomnography correlations: Sleep onset time (r = 0.84), rise time (r = 0.74), sleep period (r = 0.81), night awakenings (r = 0.37); Videosomnography MD (min): Sleep onset time = − 0:23:51, rise time = 0:13:19, sleep period = 31.99, night awakenings = − 1.38; Accelerometer correlations: Sleep onset time (r = 0.91), rise time (r = 0.84), sleep period (r = 0.90), night awakenings (r = 0.51) Accelerometer MD (min): Sleep onset time = 0:06:17, rise time = 0:15:08, sleep period = 8.41, night awakenings = −.26; |
Vid: + (Level 1) Low Acc: + (Level 2) Very low |
| Preschool-aged Children’s Physical Activity Questionnaire (Pre-PAQ) [58]a |
n = 67 Age = 3–5 years Sex = 38% girls |
Accelerometer (Actigraph, uni-axial MTI 7164, right hip, 15 s epoch, Sirard/Reilly cut-points [70, 71]) | Adequateg (both PA and SB) |
Level 1–2 Pre-PAQ vs Stationary: MD = 7.6, LoA = [− 141.3, 156.4], r = 0.25; Level 1–2 Pre-PAQ vs Sedentary (Reilly): MD = − 208.6, LoA = [− 349.8, − 67.5], r = 0.28; Level 1–2 Pre-PAQ vs Sedentary (Sirard): MD = − 235.4, LoA = [− 383.1, − 87.7], r = 0.19; Level 3 Pre-PAQ vs LPA (Sirard): MD = − 4.8, LoA = [− 105.4, 96.0], r = − 0.07; Level 4 Pre-PAQ vs MPA (Sirard): MD = 48.2, LoA = [− 24.9, 121.3], r = 0.13; Level 5 Pre PAQ vs VPA (Sirard): MD = 1.9, LoA = [− 37.5, 41.3], r = 0.17; Level 4–5 Pre-PAQ vs MVPA (Sirard): MD = 50.1, LoA = [− 42.9, 143.1], r = 0.17; Level 3–5 Pre-PAQ vs LMVPA (Sirard): MD = 45.2, LoA = [− 103.6, 194.1], r = 0.05; Level 3–5 Pre-PAQ vs Non-sedentary (Reilly): MD = 20.9, LoA = [− 121.9, 163.7], r = 0.16 |
PA: – (Level 1) Low SB: – (Level 2) Low |
| Modified Burdette proxy report [55]a |
n = 107 Age = 3.4 ± 1.2 years Sex = unknown |
Accelerometer (Actigraph, GTM1, right hip, 15 s epoch, Pate cut-points [72]) | Doubtful | PA: vs. total PA min/day: r = 0.30; vs. MVPA min/day: r = 0.34 | – (Level 1) Low |
| Modified Harro proxy report [55]a |
n = 131 Age = 3.8 ± 1.3 years Sex = unknown |
Accelerometer (Actigraph, GTM1, right hip, 15 s epoch, Pate cut-points [72]) | Doubtful | MVPA: vs. MVPA min/day: r = 0.10; vs. total PA min/day: r = 0.09 | – (Level 1) Low |
| Electronic-diary (nn) [43] |
n = 90 Age = 5.0 ± 2.0 months (range 1–9) Sex = 50% girls |
Accelerometer (MicroMini Motionlogger Actigraph, ankle, 60s epoch, Sadeh algorithm [73]) | Adequate | Sleep percentage over 24 h (r = 0.41), sleep percentage during the day (r = 0.65), sleep percentage at night (r = 0.64) | + (Level 2) Low |
| Paper-diary (nn) [43] |
n = 95 Age = 5.0 ± 2.0 months (range 1–9) Sex = 47% girls |
Accelerometer (MicroMini Motionlogger Actigraph, ankle, 60s epoch, Sadeh algorithm [73]) | Adequate | Sleep percentage over 24 h (r = 0.57), Sleep percentage during the day (r = 0.47), Sleep percentage at night (r = 0.70) | + (Level 2) Low |
| Sleep diary (nn) [44] |
n = 314 Age = 6.4 ± 0.6 months Sex = 51% girls |
- Accelerometer (Philips Actiwatch 2, left ankle, 30s epoch, wake threshold value = 80 [74]) - Questionnaire (Sleep survey) |
Doubtful (both methods) |
Accelerometer ICC: Total night sleep duration = 0.51, longest night sleep = 0.40, total day sleep duration = 0.53; Accelerometer MD (95% CI): Total night sleep duration = − 42.9 (− 50.6 – − 35.2), longest night sleep = 58.2 (43.4–73.0), total day sleep duration = − 30.8 (− 35.9 – − 25.6); Questionnaire ICC: Total night sleep duration = 0.44, longest night sleep = 0.55, total day sleep duration = 0.33, sleep onset time = 0.31, sleep offset time = 0.10; Questionnaire MD (95% CI): Total night sleep duration = 22.9 (14.0–31.7), longest night sleep = 1.8 (− 17.2–13.6), total day sleep duration = − 1.0 (− 10.3–8.3), sleep onset time = 0.2 (0.0, 0.5), sleep offset time = − 0.4 (− 0.6 – − 0.1) |
Acc: + (Level 2) Low QA: – (Level 3) Low |
| Sleep diary (nn) [38] | Data were collected at 3 (n = 226, girls = 49.5%), 6 (n = 191), 12 (n = 172), and 18 months (n = 150) postpartum. |
- Accelerometer (micromotion logger sleep watch, 60s epoch, Sadeh algorithm [75]) - Questionnaire (BISQ) |
Doubtful (both methods) |
Accelerometer correlations at 3, 6, 12 and 18 months: Night awakenings: 0.58, 0.56, 0.40, 0.27; WASO = 0.72, 0.69, 0.63, 0.61; Sleep duration = 0.87, 0.94, 0.61, 0.78; Sleep onset = 0.88, 0.89, 0.89, 0.84; BISQ correlations at 3, 6, 12 and 18 months: Night awakenings: 0.70, 0.76, 0.68, 0.59; WASO = 0.33, 0.34, 0.54, 0.69; Sleep latency = 0.40, 0.43, 0.59, 0.63; Sleep onset = 0.82, 0.82, 0.81, 0.78 |
Acc: + (Level 2) Low QA: – (Level 3) Low |
| Brief Infant Sleep Questionnaire (BISQ) [38] | Data were collected at 3 (n = 226, girls = 49.5%), 6 (n = 191), 12 (n = 172), and 18 months (n = 150) postpartum. |
- Accelerometer (micromotion logger sleep watch, 60s epoch, Sadeh algorithm [75]) - Sleep diary |
Doubtful (both methods) |
Accelerometer correlations at 3, 6, 12 and 18 months: Night awakenings: 0.53, 0.48, 0.27, 0.06; WASO = 0.22, 0.15, 0.31, 0.39; Sleep onset = 0.74, 0.75, 0.78, 0.72 Diary correlations at 3, 6, 12 and 18 months: Night awakenings: 0.70, 0.76, 0.68, 0.59; WASO = 0.33, 0.34, 0.54, 0.69; Sleep latency = 0.40, 0.43, 0.59, 0.63; Sleep onset = 0.82, 0.82, 0.81, 0.78 |
Acc: ± (Level 2) Low Diary: – (Level 3) Low |
| Sleep survey (including items from the BISQ and CSHQ) [44] |
n = 314 Age = 6.4 ± 0.6 months Sex = 51% girls |
- Accelerometer (Philips Actiwatch 2, left ankle, 30s epoch, wake threshold value = 80 [74]) - Sleep diary |
Doubtful (both methods) |
Accelerometer ICC: Total night sleep duration = 0.34, longest night sleep = 0.17, total day sleep duration = 0.25, sleep onset time = 0.23, sleep offset time = 0.08; Accelerometer MD (95% CI): Total night sleep duration = − 67.1 (− 76.3 – − 57.9); longest night sleep = 58.2 (39.9–76.4), total day sleep duration = − 28.9 (− 38.1 – − 19.7), sleep onset time = − 0.3 (− 0.6 – − 0.1), sleep offset time = 0.4 (0.1–0.6); Sleep diary ICC: Total night sleep duration = 0.44, longest night sleep = 0.55, total day sleep duration = 0.33, sleep onset time = 0.31, sleep offset time = 0.10; Sleep diary MD (95% CI): Total night sleep duration = 22.9 (14.0–31.7), longest night sleep = 1.8 (− 17.2–13.6), total day sleep duration = − 1.0 (− 10.3–8.3), sleep onset time = 0.2 (0.0–0.5), sleep offset time = − 0.4 (− 0.6 – − 0.1) |
Acc: – (Level 2) Low Diary: – (Level 3) Low |
| Parental report – outdoor time checklist [54]a |
n = 250 Age: 44 months (29–52 months) Sex: 43% girls |
- Accelerometer (RT3 tri-axial research tracker, waist worn, 60s epoch) - Questionnaire (Outdoor time recall questionnaire) |
Doubtful (both methods) |
Accelerometer: r = 0.33; Recall questionnaire: r = 0.57 |
Acc: – (Level 2) Low QA: – (Level 3) Low |
| Parental report – outdoor time recall questionnaire [54]a |
n = 250 Age: 44 months (29–52 months) Sex: 43% girls |
- Accelerometer (RT3 tri-axial research tracker, waist worn, 60s epoch) - Questionnaire (Outdoor time checklist) |
Doubtful (both methods) |
Accelerometer: r = 0.20; Checklist questionnaire: r = 0.57 |
Acc: – (Level 2) Low QA: – (Level 3) Low |
| Healthy Kids [61] |
n = 176 Age = 3.3 ± 1.6 years Sex = 42% girls |
Parent reported physical, screen, and sleep activity using 3 days of 36-h activity logs | Doubtful | Television: r = − 0.53; Computer games: r = − 0.50; Play: r = 0.21, Bedtime: r = 0.22 | – (Level 3) Low |
| Children’s Sleep Habits Questionnaire - Infant version (CSHQ-I) [39] |
n = 299 Age = 2–12 months Sex = 46.8% girls |
Sleep diary (Infant Sleep Chronogram) | Doubtful | Sleep hours (r = − 0.36), awake hours (r = 0.26), night-time awakenings (r = 0.04), latency to sleep (r = 0.14), longest sleep period (r = − 0.36) | – (Level 3) Low |
| Children’s Physical Activity Questionnaire (CPAQ) [59]a |
n = 27 Age: 4.9 ± 0.7 years (range 4–5) Sex: 38% girls |
- Doubly labeled water (DLW) - Accelerometer (Actigraph, model 7165, hip left/right randomized, 60s epoch, Treuth/Freedson cut-points [76, 77]) |
Very good (DLW) / Doubtfulg (Acc) |
DLW: PAEE: r = 0.22; Accelerometer (both cut-points): MVPA: r = 0.42 |
DLW: – (Level 1) Low Acc: – (Level 1) Very low |
| Physical activity questionnaire for parents of preschoolers in Mexico [62]a |
n = 35 Age = 4.4 ± 0.7 years Sex = 51% girls |
Accelerometer (Actigraph, GT1M, right hip, 15 s epoch, Sirard/Pate cut-points [70, 72]) | Adequateg (both PA and SB) |
Sirard cut-points: SB vs. % of time in SB: 0.35; MPA vs. % of time in MPA: r = − 0.23; VPA vs. % of time in VPA: r = 0.53; MVPA vs. % of time in MVPA: 0.49 Pate cut-points: SB vs. % of time in SB: 0.34; MPA vs. % of time in MPA: r = − 0.07; VPA vs. % of time in VPA: r = 0.41; MVPA vs. % of time in MVPA: r = 0.34 |
PA: – (Level 1) Very low SB: – (Level 2) Very low |
| Children’s ChronoType Questionnaire (CCTQ) - Japanese version [50] |
n = 72 Age = 4.8 ± 0.8 years Sex = 51% girls |
- Accelerometer (Actiwatch-2, non-dominant wrist, 60s epoch, threshold automatic sensitivity) - Sleep diary |
Doubtful (both methods) |
Accelerometer correlations (week/weekend): Sleep onset (r = 0.78/0.61), wake-up time (r = 0.82/0.71), midsleep point (r = 0.84/0.79), sleep period (r = 0.74/0.49), sleep latency (r = 0.51/0.38) Diary correlations (week/weekend): Bedtime (r = 0.77/0.64), get-up time (r = 0.83/0.71,) time in bed (r = 0.74/0.56) |
Acc: + (Level 2) Very low Diary: + (Level 3) Very low |
| Physical activity and sedentary behavior questionnaire (based on Canadian Health Measures Survey) [64]a |
n = 87 Age = 4–70 months Sex = 54% girls |
Accelerometer (Actical, right hip, Wong/Adolph cut-points [78, 79]) | Doubtfulg (both PA and SB) |
Total PA vs. total PA min/day: MD = 131 min/day*, LoA = [− 80, 290], r = 0.39 (95% CI 0.19–0.56) Outdoor unstructured free play aside from school daycare setting vs. total PA min/day: r = 0.30 (95% CI 0.09–0.49) Unstructured play in school/daycare setting vs. total PA min/day: r = 0.42 (95% CI 0.23–0.58) Structured PA vs. total PA min/day: r = 0.26 (95% CI 0.05–0.46) Total SB: MD = 306 min/day*, LoA = [125, 460], r = 0.10 (95% CI − 0.12–0.33) Screen time: r = − 0.05 (95% CI − 0.27–0.18) Stroller time: r = 0.31 (95% CI 0.09–0.50) Motor vehicle time: r = − 0.09 (95% CI − 0.30–0.13) |
PA: – (Level 1) Very low SB: – (Level 2) Very low |
| Sleep diary (nn) [46] |
n = 52 Age = 13.7 ± 6.7 months (< 1 year old = 28, > 1 year old = 21) Sex = 56% girls |
Accelerometer (Actigraph, Micro-mini RC, ankle, 60s epoch, Sadeh algorithm [80]) | Doubtful | Sleep onset time (r = 0.89), sleep offset time (r = 0.91), nocturnal sleep duration (r = 0.75), the number of night awakenings (r = 0.46), WASO (r = 0.34) | + (Level 2) Very low |
| Children’s Sleep Habits Questionnaire (CSHQ) [41] |
n = 46 Age = 58 ± 10.25 months (range = 3–6 years) Sex = 50% girls |
Accelerometer (Actiwatch 2, non-dominant wrist, 60s epoch, wake threshold value = 40) | Doubtful |
Bedtime (week/weekend): r = 0.75/0.57, wake-up (week/weekend): r = 0.86/0.64, total sleep: r = − 0.08; Interval in hours/min (LoA): Bedtime (week/weekend) = ± 0:52 [− 1:31, 0:12]/± 1:20 [− 1:37, 1:02], wake-up (week/weekend) = ± 0:38 [− 0:45, 0:31]/± 0:32 [− 1:04, 2:00], total sleep = ± 2:39 [− 0:06, 5:12], WASO = ± 1:02 [− 2:17, − 0:14] |
+ (Level 2) Very low |
| Own questionnaire (nn) [48] |
n = 21 Age = 3.81 ± 0.28 years Sex = 43% girls |
Accelerometer (Actiwatch, non-dominant ankle, 60s epochs, threshold automatic sensitivity) | Doubtful | Reported vs assumed sleeping hours (r = 0.90); Reported vs actual sleeping hours (r = 0.90); assumed vs actual sleeping hours (r = 0.99) | + (Level 2) Very low |
| Sleep diary (nn) [47] |
n = 80 Age = 25.34 ± 1.04 months Sex = 40% girls |
Accelerometer (Mini-Mitter Actiwatch Actigraph, wrist/ankle, 60s epoch, high sensitivity automatic scoring algorithm/Sitnick “smooting” algorithm to detect night awakenings [81]) | Doubtful |
Sleep duration: r = 0.30, sleep efficiency: r = 0.02. Based on the a priori agreement criteria in this study, agreement was satisfactory for 70.0% of children with respect to sleep duration (≤90 min) and for 71.3% of children with respect to sleep efficiency (≤15%) |
– (Level 2) Very low |
| Parent log (nn) [49] |
n = 59 Age = 4.34 ± 0.75 years Sex = 53% girls |
Accelerometer (Minimitter Motionlogger Actiwatch, non-dominant wrist, 60s epoch, Sadeh algorithm [80]) | Doubtful | Weekday naps (t = 0.19), weekend naps (t = − 1.48), total napping (t = 0.004), weekday night sleep (t = − 5.33*), weekend night sleep (t = − 2.96*), total nights (t = − 5.01*), total sleep (t = − 5.07*) | – (Level 2) Very low |
| BISQ Spanisch version (BISQ-E) [35] |
n = 27 Age = 3–30 months Sex = unknown |
Sleep diary | Doubtful | Bedtime during weekdays (Mon-day through Friday) (r = 0.73), hours of night-time sleep (between 8 pm and 7 am) (r = 0.73), hours of daytime sleep (between 7 am and 8 pm) (r = 0.87) and number of night-time awakenings (r = 0.89), bedtime on weekend days (r = 0.69) | + (Level 3) Very low |
| Sleep and Settle Questionnaire (SSQ) [45] |
n = 34–36 mothers of infants Age = unknown Sex = unknown |
Mothers attending a community class on sleep and settling difficulties with infants | Doubtful |
Discriminant validity (mothers who report their babies sleep well vs. mothers attending a sleep and settle class): Time the infant sleeps (min): mornings (η2 = 0.03*), afternoons (NS), during night (η2 = 0.12*); How long to settle the baby to sleep (min): daytime (η2 = 0.17*), evening (η2 = 0.18*), night-time (η2 = 0.07*); Number of daytime sleeps (NS), number night awakenings (η2 = 0.17*). |
+ (Level 3) Very low |
Abbreviations: Acc accelerometer, BISQ Brief Infant Sleep Questionnaire, CI confidence interval, COSMIN COnsensus-based Standards for the selection of health Measurement Instruments, CSHQ Children’s Sleep Habits Questionnaire, DLW doubly labeled water, h hour, ICC intraclass correlation, LoA limits of agreement, MD mean difference, min minute, MPA moderate physical activity, MVPA moderate-to-vigorous physical activity, nn no name, NS not significant, PA physical activity, PAEE physical activity energy expenditure, QA Questionnaire, r correlation coefficient (Pearson or Spearman), s second, SB sedentary behavior, ST sedentary time, VPA vigorous physical activity, Vid videosomnography, WASO wake after sleep onset, * significant
a Questionnaire included from previous review
b Age presented as mean age ± SD (range)
c Methodological quality based on the COSMIN risk of bias checklist
d Result rating based on Table 1: + indicates ≥75% in accordance with hypotheses; ± indicates ≥50 to < 75% in accordance with hypotheses; − indicates < 50% accordance with hypotheses
e Level of evidence based on criteria listed in Table 1
f Quality of evidence grading based on the COSMIN guidelines
g When multiple methods (e.g., cut-points) were used to analyze accelerometer data, the methodological quality rating was based on the method with the highest quality
Description of questionnaires
Of the included questionnaires, 10 were designed for infants specifically (0–1 year old). These questionnaires all assessed constructs of sleep [37–39, 42–45]. Two questionnaires were designed for toddlers (1–3 years old), of which one assessed sleep [47], and one screen behavior [53]. Eleven questionnaires were designed for preschoolers (3–5 years old). Five of these questionnaires assessed constructs of sleep [40, 41, 48–50], two physical activity and sedentary behavior [58, 59], and four assessed constructs of all 24-h movement behaviors [62, 63, 66, 67]. Fourteen questionnaires were designed for multiple of the aforementioned age groups. Three questionnaires assessed sleep behavior in infants and toddlers [35, 36, 46]. Two questionnaires targeted both infants, toddlers, and preschoolers, of which one assessed screen behavior [52], and one physical activity and sedentary behavior [64]. Nine questionnaires targeted toddlers and preschoolers, of which one assessed sleep behavior [51], four assessed physical activity [54, 55], two assessed constructs of both physical activity and sedentary behavior [56, 57], and two assessed constructs of all 24-h movement behaviors [60, 61, 65].
Respondents of the questionnaires were parents or caregivers, except for two questionnaires that were completed by family child care providers, i.e., the modified Burdette proxy report and the modified Harro proxy report [55]. Recall periods varied across questionnaires, ranging from current day (n = 9) to a typical week (n = 3), with a typical (week or weekend) day being used most frequently (n = 13). Four questionnaires used ordinal response options (e.g., Likert scale), 17 continuous (e.g., duration in hours and/or minutes), one nominal and 14 questionnaires used a combination of these response options.
Content validity
Six studies reported data on the comprehensiveness, comprehensibility and/or relevance of the items of the questionnaire under study (Table 3). Two of the examined questionnaires assessed constructs of sleep behavior, i.e., the Children Sleep Wake Scale (CSWS) [51] and Nepali version of the BISQ [36]. One questionnaire assessed screen behavior in children aged 0–5, i.e., the Technology Use Questionnaire (TechQ-U) [52]. The other three questionnaires, i.e., the Healthy Kids [60], the Family Health Survey [66], and the Surveillance of digital Media habits in early childhood Questionnaire (SMALLQ™) [65], assessed constructs of all 24-h movement behaviors in toddlers and/or preschoolers. Questionnaire development was reported in five studies [51, 52, 60, 65, 66]. These studies used cognitive interviews [60, 65, 66], semi-structured interviews [52], focus groups [65], and/or expert opinions [51, 52, 65] to evaluate content validity of the questionnaire. Two of these questionnaires were additionally pilot-tested in a small sample of caregivers to provide information on, for example, readability or time to complete the questionnaire [51, 65]. Overall, we graded the quality of evidence for the content validity of these questionnaires as low. Unfortunately, none of the questionnaires were evaluated on all aspects of content validity (i.e., relevance, comprehensiveness, and comprehensibility). For this reason, we could not rate the overall content validity of these questionnaires.
Internal structure: structural validity, internal consistency, and cross-cultural validity
Internal consistency was evaluated for three questionnaires (Table 4), all assessing sleep behavior: the CSWS, Children’s Sleep Habits Questionnaire (CSHQ) and Children’s Sleep Habits Questionnaire for infants (CSQH-I) [39, 40, 51]. Internal consistency was evaluated by calculating Cronbach’s alpha of each subscale for all three questionnaires. The quality of evidence for the internal consistency was high for all three questionnaires. The internal consistency outcomes for the CSWS were rated as sufficient [51], whereas outcomes for the CSHQ and CSQH-I were rated as insufficient [39, 40]. The CSHQ and CSQH-I were also evaluated on structural validity by performing confirmatory factor analysis [40] and/or exploratory factor analysis [39, 40], both receiving a moderate evidence grading (Table 4). Structural validity outcomes of both questionnaires were considered sufficient. None of the translated or culturally adapted questionnaires were evaluated on cross-cultural validity or measurement invariance [35–37, 39, 40, 66].
Table 4.
Internal consistency and structural validity of sleep questionnaires, including methodological quality, result rating and quality of evidence
| Questionnaire | Study population a | Internal consistency | Structural validity | ||||
|---|---|---|---|---|---|---|---|
| Methodological quality b | Results | Rating & Evidence grading c | Methodological quality b | Results | Rating & Evidence grading c | ||
| Children’s Sleep-Wake Scale (CSWS) [51] |
n = 543 Age = 4.9 ± 2.0 years (range 2–8) Sex = unknown |
Very good | Cronbach’s α for the total scale was 0 .89. Cronbach’s α for the subscales were: Going to Bed (α = 0.88), Falling Asleep (α = 0.83), Maintaining Sleep (α = 0.81), Reinitiating Sleep (α = 0.81), and Returning to Wakefulness (α = 0.91) | + High | |||
| Children’s Sleep Habits Questionnaire - Chinese version (CSHQ) [40] |
n = 2816 Age = 4.82 ± 1.06 years Sex = 46.9% girls |
Very good |
Cronbach’s α for the total scale was 0.72. Cronbach’s α for the subscales were: Sleep duration (α = 0.46), Sleep disordered breathing (α = 0.54), Sleep anxiety (α = 0.57); Parasomnias (α = 0.58, and Daytime sleepiness (α = 0.63) |
– High | Adequate |
EFA: model was adjusted to acceptable eight-factor structure; CFA: comparative fit index = 0.91, Tucker–Lewis index = 0.90, and standardized root mean residual = 0.03 |
+Moderate |
| Children’s Sleep Habits Questionnaire - Infant version (CSHQ-I) [39] |
n = 299 Age = 2–12 months Sex = 46.8% girls |
Very good |
Cronbach’s α for the total scale was 0.78. Cronbach’s α for the subscales were: Bed-time Resistance (α = 0.77), Sleep Anxiety (α = 0.66), Positive Sleep Habits (α = 0.58), and Daytime Sleepiness (α = 0.52) |
– High | Adequate | EFA: after removing items with factor loadings < 0.30, 33 items remained | +Moderate |
Abbreviations: COSMIN COnsensus-based Standards for the selection of health Measurement, CFA confirmatory factor analysis, EFA exploratory factor analysis
a Age presented as mean age ± SD (range)
b Methodological quality based on the COSMIN risk of bias checklist
c Result rating and quality of evidence grading based on the COSMIN guidelines
Reliability
Sixteen questionnaires were assessed on reliability (Table 5). Six of these questionnaires assessed constructs of sleep [35, 37, 39, 40, 45, 51], six assessed constructs of physical activity and/or sedentary behavior [52, 53, 56–59], and four assessed constructs of all 24-h movement behaviors [61–63, 67]. Reliability of nine questionnaires was evaluated by calculating ICC [40, 52, 53, 56–59, 63, 67], whereas Pearson or Spearman correlations were calculated for seven questionnaires [35, 37, 39, 45, 51, 61, 62]. Time interval between test and retest ranged between 7 days [53, 57] and 3 months [39]. Two questionnaires received a moderate quality of evidence grading for reliability, i.e., the Early Years Physical Activity Questionnaire (EY-PAQ) [57] and Preschool-age Children’s Physical Activity Questionnaire (Pre-PAQ) [58]. Reliability outcomes were considered insufficient for both questionnaires. Five questionnaires received a low quality of evidence grading, and nine questionnaires received a very low evidence grading.
Table 5.
Reliability of physical activity, sedentary behavior and/or sleep questionnaires, sorted by quality of evidence, result rating and methodological quality
| Questionnaire | Reliability | ||||
|---|---|---|---|---|---|
| Study population b | Time interval | Methodological quality c | Results | Rating d & evidence grading e | |
| Preschool-aged Children’s Physical Activity Questionnaire (Pre-PAQ) [58]a |
n = 103 Age = 3.80 ± 0.74 years Sex = 48% girls |
1–2 weeks | Adequate |
Pre-PAQ level 1–2: ICC = 0.44; Pre-PAQ level 3: ICC = 0.53; Pre-PAQ level 4: ICC = 0.44; Pre-PAQ level 5: ICC = 0.64; Time child spent in car: ICC = 0.31–0.63; Child’s activity nature: ICC = 0.87–0.93; Involvement in organized activities: K = 0.95, Time spent in organized activities: ICC = 0.96–0.99; Use of neighborhood facilities for activity: K = 0.70–0.80 |
– Moderate |
| Early Years Physical Activity Questionnaire (EY-PAQ) [57] |
n = 109 Age = 3.3 ± 0.8 years Sex = 53% girls |
7.2 days (5–12 days) | Adequate |
MVPA: ICC = 0.35 (95% CI 0.17–0.50); ST: ICC = 0.47 (95% CI 0.30–0.61) |
–Moderate |
| PREPS questionnaire [53] |
n = 118 Age = 19.3 ± 2.7 months Sex = 48% female |
7 days | Doubtful | Screen time: ICC = 0.82 | +Low |
|
Energy balance-related behaviors (ERBs) selfadministered primary caregivers questionnaire (PCQ), from the ToyBox study [63]a |
n = 93 preschooler Age = unknown Sex = unknown |
2 weeks | Adequate |
ICC (95% CI) = Sports: time per week = 0.93 (0.85–0.97), type of sport = 0.71 (0.46–0.86); Active/passive transport: travel forth = 0.91 (0.87–0.94), time = 0.82 (0.73–0.88), travel home = 0.88 (0.82–0.92), time = 0.89 (0.83–0.93); Computer use: weekdays = 0.72 (0.60–0.80), weekend days = 0.81 (0.73–0.87); TV viewing: weekdays = 0.67 (0.54–0.77), weekend days = 0.67 (0.53–0.77); Quiet play: weekdays = 0.42 (0.24–0.58), weekend days = 0.50 (0.33–0.64); Night sleep duration: weekdays = 0.68 (0.55–0.78), weekend days = 0.69 (0.56–0.78); Naps: weekdays = 0.62 (0.48–0.73), weekend days = 0.70 (0.58–0.79) |
±Low |
| Children’s Sleep Habits Questionnaire - Chinese version (CSHQ) [40] |
n = 82 Age = unknown Sex = unknown |
2 weeks | Adequate | ICC = Full-scale = 0.77, Sleep duration = 0.38, Bedtime resistance = 0.78, Night-time awakenings = 0.54, Parasomnias = 0.56, Sleep onset delay = 0.57, Daytime sleepiness = 0.60, Sleep disordered breathing = 0.67, Sleep anxiety = 0.76 | –Low |
| Children’s Sleep Habits Questionnaire - Infant version (CSHQ-I) [39] |
n = 98 (completing all 3 times points) Age = 2–12 months Sex = unknown |
3 months (2 times) | Doubtful |
CSHQ-I total scale scores: between 0 and 3 months and 3–6 months (r = 0.64), between 3 and 6 months and 6–12 months (r = 0.73); The subscales Bedtime Resistance, Sleep Anxiety, and Positive Sleep Habits: between 0 and 3 months and 3–6 months (r range = 0.48–0.56), between 3 and 6 months and 6–12 months (r range = 0.43–0.73); The subscale Daytime Sleepiness: between 0 and 3 months and 3–6 months (r = 0.08), between 3 and 6 months and 6–12 months (r = 0.23) |
–Low |
| Healthy Kids [61] |
Year 1: n = 133; Year 2: n = 98 Sex = unknown |
12 weeks | Doubtful |
Television: r = 0.44, CV = 24%; Computer games: r = 0.34, CV = 15%; Play: r = 0.32, CV = 31%; Bedtime: CV = 38% |
–Low |
| KidActive-Q [56]a |
n = 20 Age = 4.2 ± 1.3 years (range: 2–6) Sex = 50% girls |
3 weeks | Adequate |
ICC (95% CI): Watching TV = 0.85 (0.72–0.97); Overall PA level = 0.66 (0.41–0.91); Time spent outdoors = 0.60 (0.31–0.88) |
+ Very low |
| BISQ Spanisch version (BISQ-E) [35] |
n = 60 Age = 3–30 months Sex = unknown |
10 days (8–22 days) | Doubtful |
Inter-observer reliability: K = 0.94 (95% CI 0.85–1.00); Test - retest reliability: bed-time (r = 0.74), hours of night-time sleep (r = 0.88), hours of daytime sleep (r = 0.90) and number of awakenings (r = 0.88) |
+ Very low |
| Physical activity questionnaire for parents of preschoolers in Mexico [62]a |
n = 21 Age = 3–5 years old Sex = unknown |
1 week | Doubtful |
Duration low activity: r = 0.86; Duration moderate activity: r = 0.79; Duration vigorous activity: r = 0.94; Overall activity: r = 0.97 |
+ Very low |
| Technology Use Questionnaire (TechU-Q) [52] |
n = 22–27 Age = unknown Sex = unknown |
2 weeks | Adequate |
ICC for weekday, weekend day and total: TV = 0.58, 0.64, 0.72; Desktop = 0.91, 0.96, 0.92; Laptop = 0.20, 0.35, 0.25; Tablet = 0.50, 0.93, 0.75; Mobile = 0.92, 0.88, 0.90; Total tech = 0.70, 0.70, 0.71 |
±Very low |
| Healthy Active Preschool Years (HAPPY) parent proxy report survey [67] |
n = 43 Age = unknown Sex = unknown |
24 days (14–50 days) | Adequate |
ICC for summed items/continuous variables: Child’s sleep: individual variables = 0.75–0.78, combined sum = 0.72; Active transport = 0.75; Non-organized activities = 0.63: Total organized activities = 0.70; Usual participation in screen behaviors: Individual items = 0.31–0.84 (week days); 0.05–0.75 (weekend days). Summed items: weekly TV = 0.69, weekly e-games = 0.55, weekly computer = 0.51, weekly Wii/Eye Toy = 0.23, total weekly SBE time = 0.68, total week day SBE time = 0.44, total weekend SBE time = 0.70; Quiet play/imaginary games: 0.30–0.50 (weekday), 0.34–0.40 (weekend day), 0.37–0.63 (total weekly); Summed items: weekly quiet play = 0.63, weekly imaginary games = 0.37 K (% agreement) for categorical variables: Child’s PA & SB = − 0.02 to 0.90 (50.07–95.84); Organized activities: participation = 0.66–0.84 (91.49–100.0), frequency = 0.38–0.70 (88.9–93.62); Playgroup attendance: participation = 0.91 (95.74); frequency = 0.77 (93.33); Screen behaviors: participation = 0.52–1.00 (82.22–100.0) |
±Very low |
| Children’s Physical Activity Questionnaire (CPAQ) [59]a |
n = 27 Age: 4.9 ± 0.7 years (range: 4–5 years) Sex: 38% girls |
7 days | Adequate |
MVPA: ICC = 0.39; PAEE: ICC = 0.25 |
–Very low |
| Expanded version of the Brief Infant Sleep Questionnaire (BISQ), Turkish version [37] |
n = 30 Age = 9 months Sex = unknown |
3 weeks | Doubtful | Nocturnal sleep duration (r = 0.71), daytime sleep duration (r = 0.73), number of night awakenings (r = 0.82), duration of nocturnal wakefulness (r = 0.77), nocturnal sleep onset time (r = 0.81), and settling time (r = 0.63) | –Very low |
| Children’s Sleep-Wake Scale (CSWS) [51] |
n = 36 Age = 4.4 ± 2.1 years Sex = unknown |
1 month | Doubtful | CSWS total (r = 0.85), going to bed (r = 0.84), falling asleep (r = 0.78), maintaining Sleep (r = 0.75), reinitiating Sleep (r = 0.67), and returning to wakefulness (r = 0.70) | –Very low |
| Sleep and Settle Questionnaire (SSQ) [45] |
n = 20 Age = unknown Sex = unknown |
7–14 days | Doubtful | Morning sleeps (r = 0.38), afternoon sleeps (r = 0.34), night sleeps (r = 0.14), number of daytime naps (r = 0.40), number awakenings at night (r = 0.43), how long to settle in the day (r = 0.01), how long to settle in evening (r = 0.26), how long to settle at night (r = 0.52) | –Very low |
Abbreviations: BISQ Brief Infant Sleep Questionnaire, CI confidence interval, COSMIN COnsensus-based Standards for the selection of health Measurement Instruments, ICC intraclass correlation name, K kappa, M mean, MVPA moderate-to-vigorous physical activity, PA physical activity, PREPS Parents’ Role in Establishing healthy Physical activity and Sedentary behavior, r correlation coefficient (Pearson or Spearman), SB sedentary behavior, SBE screen behavior entertainment, ST sedentary time
a Questionnaire included from previous review
b Age presented as mean age ± SD (range)
c Methodological quality based on the COSMIN risk of bias checklist
d Result rating: + indicates ≥75% acceptable correlations; +/− indicates ≥50 to < 75% acceptable correlations; − indicates < 50% acceptable correlations
e Quality of evidence grading based on the COSMIN guidelines
Measurement error
Measurement error was evaluated for one questionnaire, i.e., the Pre-PAQ [58]. The quality of evidence for the measurement error of this questionnaire was graded as moderate. This questionnaire demonstrated a measurement error ranging from 1.0–1.1 min for time spent in organized physical activities. Unfortunately, as the MIC for interpreting the measurement error outcomes was not defined, we could not give a final rating for measurement error. However, a measurement error of 1.0–1.1 min seems acceptable.
Criterion and construct validity
Criterion validity was evaluated for one questionnaire (Table 6), i.e., the Children’s Physical Activity Questionnaire (CPAQ) [59]. The CPAQ was used to assess energy expenditure in 4- to 5-year-olds. This questionnaire received a low quality of evidence grading for criterion validity, and outcomes were considered insufficient.
Twenty-one studies evaluated the construct validity of a total of 26 different questionnaires (Table 6). Sixteen of these questionnaires assessed constructs of sleep [35, 38–50], eight assessed constructs of physical activity and/or sedentary behavior [54, 55, 57–59, 64], and two assessed constructs of all three movement behaviors [61, 62]. Thirteen studies evaluated construct validity using an objective comparator instrument (e.g., accelerometer) [41–43, 47–49, 55, 57–59, 62, 64], three used a subjective comparator instrument (e.g., diary) [35, 39, 61], and four studies used both [38, 44, 50, 54]. Nineteen studies used Pearson or Spearman correlations to evaluate construct validity, of which 10 studies also presented Bland-Altman plots [38, 41–44, 47, 54, 57–59, 64]. One study evaluated construct validity by comparing subgroups (i.e., discriminative validity) [45]. The quality of evidence for construct validity was graded as moderate for one questionnaire, i.e., the EY-PAQ [57], showing outcomes that were considered insufficient. Fifteen of the questionnaires received a low quality of evidence grading, and 10 questionnaires received a very low evidence grading.
Discussion
This review summarizes studies that evaluated the measurement properties of proxy-report questionnaires for assessing physical activity, sedentary behavior, and/or sleep in 0- to 5-year-old children. The questionnaires varied in constructs, format, target population, and evaluated measurement properties. Unfortunately, while we identified 37 relevant questionnaires, none were considered valid and/or reliable for assessing one or more movement behaviors in children aged 0–5 years.
Proxy-report questionnaires for assessing all 24-h movement behaviors in this young age group are scarce. The majority of included questionnaires assessed one type of behavior, of which sleep behavior was assessed most frequently. Only six questionnaires assessed duration and/or frequency of all three behaviors (physical activity, sedentary behavior, and sleep) [60–63, 65, 67]. Unfortunately, these six questionnaires mostly used very few items per movement behavior, which questions the comprehensiveness of the items (e.g., a single item to assess sedentary behavior). Overall, 21 out of 37 questionnaires targeted children above 2 years old (e.g., preschoolers). Questionnaires that targeted solely infants all assessed sleep behavior (n = 10). Only one questionnaire (i.e., based on the Canadian Health Measures Survey) assessed physical activity and sedentary behavior in infants, next to toddlers and preschoolers (i.e., 0- to 6-year-old children) [64]. In addition, one questionnaire assessed screen use in 0- to 5-year-old children (i.e., TechU-Q) [52]. There were only two questionnaires that specifically targeted toddlers: a questionnaire assessing screen use (i.e., PREPS questionnaire) [53] and a sleep diary [47]. This further indicates the urgent need for developing questionnaires assessing 24-h movement behaviors in infants and toddlers. Notably is the large number of questionnaires (n = 14) that were designed for multiple age groups (e.g., toddlers and preschoolers). However, since infants, toddlers and preschoolers each have their own form and context of physical activity, sedentary behavior and sleep [9], tailored questionnaires are needed that fit the specific behavior of the target group.
There are two important issues that complicate drawing definite conclusions regarding the best available questionnaires. First, there is a lack of studies comprehensively evaluating measurement properties of proxy-report questionnaires. These findings are consistent with previous reviews [20, 21, 24]. For example, only one study reported information on the measurement error of a questionnaire [58]. Measurement error is an important characteristic of reliability, as it gives an indication of the systematic and random error expressed in units of measurement (e.g., minutes per day), which facilitates the interpretation of measurements [26]. Unfortunately, our systematic review confirms that measurement error is still largely underreported in studies evaluating measurement instruments [26]. Consequently, we are unable to correctly interpreted the results of research using these questionnaires to assess time spent in physical activity, sedentary behavior and/or sleep. Likewise, criterion validity was evaluated for only one questionnaire [59]. As in many of the included studies the comparison instrument was not considered a gold standard, these studies were considered to reflect construct validity. Additionally, none of the included studies evaluated the responsiveness of the questionnaire. However, for the purpose of longitudinally monitoring one or more movement behaviors, questionnaires should be able to detect changes over time [26, 30]. Furthermore, none of the translated or adapted questionnaires were evaluated on cross-cultural validity (measurement invariance). Without evaluating this type of validity, it remains unsure if the performance of the translated items are an adequate reflection of the performance of the items of the original questionnaire [30]. Moreover, there is a lack of studies describing the development or content validity of the questionnaire [20, 21]. Only six studies reported information that contributed to the content validity of the questionnaire [36, 51, 52, 60, 65, 66]. Consequently, it remains unclear if the respondents (e.g., parents, youth health care providers) consider the content of the questionnaire as relevant, comprehensive and comprehensible [32]. Without evaluating content validity, there is no certainty that the questionnaire measures what it intends to measure [26, 31]. It can be argued that it is difficult to proxy-report young children’s sporadic and intermittent behaviors [17], and therefore it would be unrealistic to expect that questionnaires can be used to assess 24-h movement behaviors very accurately in this target population. However, a more comprehensive development and evaluation of questionnaires (while including the target population and professionals in the process) would improve the quality of questionnaires. As appropriate measurement instruments are lacking, current evidence on young children’s 24-h movement behaviors and the effects on their growth and development is limited [82]. Therefore, improving the quality of questionnaires and alternative (device-based) measures would strongly benefit research in this field, and thereby future public health recommendations.
Second, the quality of evidence was graded as low or very low for the majority of evaluated measurement properties of included questionnaires (i.e., 40 out of 49 evaluated measurement properties across all questionnaires), which makes it even more difficult to draw conclusions about the most appropriate available questionnaires. Although there are a number of questionnaires of which reliability (test-retest reliability: n = 4, internal consistency: n = 1) and/or validity (construct validity: n = 11, structural validity: n = 2) outcomes were considered sufficient, only three of these questionnaires received at least a moderate quality of evidence grading for one of the evaluated measurement properties. This concerns the internal consistency of the CSWS [30] and the structural validity of the CSHQ [40] and CSHQ-I [39]. Unfortunately, other measurement properties of these questionnaires received a low or very low quality of evidence grading (e.g., reliability), or were not included in our review since these were not assessed in 0- to 5-year-old children (e.g., construct validity and structural validity of the CSWS [51]). Hence, no definite conclusions about the appropriateness of these questionnaires to assess sleep behavior in young children can be drawn.
There are a few reasons that contributed to the low quality of evidence of questionnaires. First, quality of evidence was often downgraded because of the small sample sizes (< 100 participants) included in studies (i.e., risk of imprecision) [30]. If multiple studies on the same measurement property of a questionnaire would have been available, pooling of study results would be possible, thereby solving this sample size issue [30].
Second, quality of evidence was often downgraded because of the doubtful methodology quality of studies (i.e., risk of bias) [30]. The lack of high-quality studies is consistent with findings from previous reviews by Hidding et al. [20, 21]. Common methodological limitations varied by evaluated measurement property. Concerning test-retest reliability, Pearson or Spearman correlations were often used without providing evidence that no systematic changes had occurred [30]. Furthermore, some reliability studies used inappropriate long time intervals between test and retest, e.g., 3 months, reducing the probability that children have remained stable in the interim period on the construct to be measured [30, 83]. The low methodological quality of construct validity studies was predominantly due to using comparator instruments with unknown or insufficient measurement properties. Most studies used, for example, non-validated diaries, or accelerometers without providing validated analyses methods (e.g., cut-points) in young children. Unfortunately, adequate comparator instruments with validated analyses methods are generally lacking in this young age group, making it difficult to ensure that comparator instruments measure the same constructs [13, 16, 29]. The doubtful methodological quality of content validity studies was predominantly due to the limited information reported on the methods used for the development of the questionnaire or the content validity evaluation. In particular, details on procedures of interviews or group meetings were lacking. For example, it was unclear whether interviewers were trained, whether data was coded independently, or whether data saturation was reached [31]. Moreover, not all aspects of content validity (i.e., relevance, comprehensiveness, and comprehensibility) were evaluated or the respondents (e.g., parents) were not included where appropriate.
It should be noted that some of the included questionnaires were not specifically aimed at assessing movement behaviors [53, 60, 61, 63, 65–67]. Consequently, frequency and/or duration of physical activity, sedentary behavior and/or sleep were only one of the many sub-constructs in these questionnaires. The Healthy Kids [60, 61], for example, is intended to assess obesity risk. This questionnaire included items related to children’s physical activity, sedentary behavior and sleep, as part of a larger questionnaire. Studies evaluating the content validity of such questionnaires considered the questionnaire as a whole, instead of each sub-construct separately [60, 65, 66]. Consequently, it was unclear whether all included items for physical activity, sedentary behavior and/or sleep were relevant and whether all key concepts were included (i.e., comprehensiveness). Future studies evaluating the content validity of questionnaires assessing multiple behaviors should evaluate each subscale or sub-construct separately to ensure an adequate evaluation of all included constructs [31].
Strengths and limitations
A strength of this review is the standardized quality assessment of included studies, using the COSMIN guidelines [28, 30, 31]. Another strength is that we included questionnaires for assessing all 24-h movement behaviors (i.e., physical activity, sedentary behavior and sleep). There is growing evidence that all 24-h movement behaviors should be targeted when aiming for optimal health [5–10]. The current review gives a clear overview of the available proxy-report questionnaires to monitor these behaviors in young children. Additionally, screening, data extraction and methodological quality assessment have each been done by at least two independent researchers, minimizing the chance of bias. However, our review also has some limitations. We only included studies published in English, disregarding studies published in other languages. Consequently, our review might not be representative for questionnaires available in non-English speaking countries, although we only excluded a limited number of studies based on language. Furthermore, we rated the methodological quality of studies based on the information reported in each of the articles. When details on the methodology were lacking, studies received lower quality of evidence grades. We did not contact authors for additional information other than requesting the questionnaires that were used. Consequently, the quality of evidence of some studies might have been underestimated.
Recommendations for future studies
Given the lack of questionnaires for assessing movement behaviors in young children, we recommend future studies to develop proxy-report questionnaires targeted specifically at children aged 0–5 years, including all 24-h movement behaviors. These questionnaires should preferably be tailored to fit the specific behavior of the subgroup (i.e., infants, toddlers or preschoolers), as movement behaviors quickly change during this period of rapid development.
When developing questionnaires, we strongly recommend future studies to evaluate the content validity of proxy-report questionnaires in a sample representing the target population (e.g., parents), including all components of content validity (i.e., relevance, comprehensiveness, and comprehensibility). We recommend these studies to use appropriate qualitative data collection methods, such as focus groups, interviews or concept mapping [31], and to evaluate the content validity of each subscale or sub-construct separately [31].
Next, high quality research on all other relevant measurement properties (both reliability and validity) of developed questionnaires is necessary. Future studies evaluating measurement properties of questionnaires are recommended to use standardized tools to increase study quality. We recommend the use of the COSMIN methodology for the design and reporting of these studies [84]. Specifically, high quality studies on measurement error, responsiveness, and cross-cultural validity of questionnaires are needed.
First, we recommend future studies that examine test-retest reliability to additionally report the measurement error, as both measurement properties can be calculated based on the same data and study design [84]. These studies should use at least two independent measurements with similar test conditions and an appropriate time interval, according to previous recommendations for youth physical activity questionnaires: > 1 day and < 1 week for questionnaires recalling the previous day, > 1 day and < 2 weeks for questionnaires recalling the recalling the previous week [19]. The preferred statistical method to assess the measurement error of continuous scores is the calculation of the standard error of measurement (SEM) [30]. For categorical scores we recommend calculating the percentage positive and negative agreement [84].
Second, more studies examining responsiveness of questionnaires are needed, reflecting longitudinal validity. Similar to construct validity, it is important to define hypotheses in advance when assessing responsiveness of a questionnaire, to enable drawing unbiased conclusions [84].
Third, we recommend future studies evaluating translated or culturally adapted questionnaires to examine cross-cultural validity. These studies are recommended to provide a clear description of the characteristics that should be similar in the different subgroups (e.g., demographics such as age) and provide clear information on the performance of the analysis (e.g. software program used, criteria for model fit) [84].
Last, as current studies evaluating the criterion and construct validity of questionnaires are limited due to a lack of comparators with sufficient measurement properties, we recommend future studies to improve comparator instruments and analysis methods to assess 24-h movement behaviors (e.g., accelerometer data analyses). Subsequently, improving the quality of questionnaires and alternative measurement methods would strongly benefit research in this field.
Conclusion
None of the 37 proxy-report questionnaires included in this review were considered valid and/or reliable for assessing one or more movement behaviors in children aged 0–5 years. The lack of high-quality methodological studies that evaluate all relevant measurement properties of developed questionnaires hampers our ability to draw definite conclusions about the best available questionnaires. In addition, questionnaires for assessing 24-h movement behaviors in 0- to 5-year-olds are scarce. Thus, high-quality studies are required aimed to develop proxy-report questionnaires for this age group and to evaluate their measurement properties, starting with content validity. When sufficient content validity is established, the remaining relevant measurement properties (i.e., reliability, validity, responsiveness) should be evaluated [31, 84]. Until valid and reliable proxy-report questionnaires are available, caution is needed when interpreting results of research using proxy-reported physical activity, sedentary behavior and sleep in this young age group.
Supplementary Information
Acknowledgements
Not applicable.
Authors’ contributions
JA, TA, JG, AV and MC conceived the study. JA and TA screened all articles for eligibility. JA, JG and AV extracted the data. JA, TA, MC and AL rated the methodological quality of studies. JA completed data analysis. JA drafted the manuscript. TA, JG, AV and MC revised and edited significant sections of the manuscript. All authors reviewed and approved the final manuscript.
Funding
This review is part of the ‘My Little Moves’ project that is funded by ZonMw (546003008) and the Bernard van Leer foundation. The funding bodies had no role in the design of the study; in the collection, analysis, and interpretation of data; or in the writing of the manuscript.
Availability of data and materials
The data that support the findings of this review are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hills AP, King NA, Armstrong TP. The contribution of physical activity and sedentary Behaviours to the growth and development of children and adolescents. Sports Med. 2007;37(6):533–545. doi: 10.2165/00007256-200737060-00006. [DOI] [PubMed] [Google Scholar]
- 2.Jones RA, et al. Tracking physical activity and sedentary behavior in childhood: a systematic review. Am J Prev Med. 2013;44(6):651–658. doi: 10.1016/j.amepre.2013.03.001. [DOI] [PubMed] [Google Scholar]
- 3.Timmons BW, et al. Systematic review of physical activity and health in the early years (aged 0-4 years) Appl Physiol Nutr Metab. 2012;37(4):773–792. doi: 10.1139/h2012-070. [DOI] [PubMed] [Google Scholar]
- 4.Chaput JP, et al. Systematic review of the relationships between sleep duration and health indicators in the early years (0-4 years) BMC Public Health. 2017;17(Suppl 5):855. doi: 10.1186/s12889-017-4850-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chaput JP, et al. Importance of all movement behaviors in a 24 hour period for overall health. Int J Environ Res Public Health. 2014;11(12):12575–12581. doi: 10.3390/ijerph111212575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kuzik N, et al. Systematic review of the relationships between combinations of movement behaviours and health indicators in the early years (0-4 years) BMC Public Health. 2017;17(5):849. doi: 10.1186/s12889-017-4851-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tremblay MS, et al. Canadian 24-hour movement guidelines for children and youth: an integration of physical activity, sedentary behaviour, and sleep. Appl Physiol Nutr Metab. 2016;41(6 Suppl 3):S311–S327. doi: 10.1139/apnm-2016-0151. [DOI] [PubMed] [Google Scholar]
- 8.Tremblay MS, et al. Canadian 24-hour movement guidelines for the early years (0-4 years): an integration of physical activity, sedentary behaviour, and sleep. BMC Public Health. 2017;17(Suppl 5):874. doi: 10.1186/s12889-017-4859-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization. Guidelines on physical activity, sedentary behaviour and sleep for children under 5 years of age. Geneva: World Health Organization; 2019. https://apps.who.int/iris/handle/10665/311664. License: CC BY-NC-SA 3.0 IGO. [PubMed]
- 10.Rollo S, Antsygina O, Tremblay MS. The whole day matters: understanding 24-hour movement guideline adherence and relationships with health indicators across the lifespan. J Sport Health Sci. 2020;9(6):493–510. [DOI] [PMC free article] [PubMed]
- 11.Sirard JR, Pate RR. Physical activity assessment in children and adolescents. Sports Med. 2001;31(6):439–454. doi: 10.2165/00007256-200131060-00004. [DOI] [PubMed] [Google Scholar]
- 12.Sadeh A, Iii. Sleep assessment methods. Monogr Soc Res Child Dev. 2015;80(1):33–48. doi: 10.1111/mono.12143. [DOI] [PubMed] [Google Scholar]
- 13.Bruijns BA, et al. Infants' and toddlers' physical activity and sedentary time as measured by accelerometry: a systematic review and meta-analysis. Int J Behav Nutr Phys Act. 2020;17(1):14. doi: 10.1186/s12966-020-0912-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Trost SG. State of the art reviews: measurement of physical activity in children and adolescents. Am J Lifestyle Med. 2007;1(4):299–314. [Google Scholar]
- 15.Trost SG, McIver KL, Pate RR. Conducting accelerometer-based activity assessments in field-based research. Med Sci Sports Exerc. 2005;37(11 Suppl):S531–S543. doi: 10.1249/01.mss.0000185657.86065.98. [DOI] [PubMed] [Google Scholar]
- 16.Cliff DP, Reilly JJ, Okely AD. Methodological considerations in using accelerometers to assess habitual physical activity in children aged 0–5 years. J Sci Med Sport. 2009;12(5):557–567. doi: 10.1016/j.jsams.2008.10.008. [DOI] [PubMed] [Google Scholar]
- 17.Kohl HW, Fulton JE, Caspersen CJ. Assessment of physical activity among children and adolescents: a review and synthesis. Prev Med. 2000;31(2):S54–S76. [Google Scholar]
- 18.Nascimento-Ferreira MV, et al. Validity and reliability of sleep time questionnaires in children and adolescents: a systematic review and meta-analysis. Sleep Med Rev. 2016;30:85–96. doi: 10.1016/j.smrv.2015.11.006. [DOI] [PubMed] [Google Scholar]
- 19.Chinapaw MJ, et al. Physical activity questionnaires for youth: a systematic review of measurement properties. Sports Med. 2010;40(7):539–563. doi: 10.2165/11530770-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 20.Hidding LM, et al. Systematic review of childhood sedentary behavior questionnaires: what do we know and what is next? Sports Med. 2017;47(4):677–699. doi: 10.1007/s40279-016-0610-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hidding LM, et al. An updated systematic review of childhood physical activity questionnaires. Sports Med. 2018;48(12):2797–2842. doi: 10.1007/s40279-018-0987-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Spruyt K, Gozal D. Pediatric sleep questionnaires as diagnostic or epidemiological tools: a review of currently available instruments. Sleep Med Rev. 2011;15(1):19–32. doi: 10.1016/j.smrv.2010.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sen T, Spruyt K. Pediatric sleep tools: an updated literature review. Front Psychiatry. 2020;11:317. doi: 10.3389/fpsyt.2020.00317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Byrne R, Terranova CO, Trost SG. Measurement of screen time among young children aged 0–6 years: a systematic review. Obes Rev. 2021;22(8):e13260. 10.1111/obr.13260. [DOI] [PMC free article] [PubMed]
- 25.Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372:1–36. 10.1136/bmj.n160. [DOI] [PMC free article] [PubMed]
- 26.De Vet H, et al. Measurement in medicine: A practical guide. Measurement in Medicine: A Practical Guide. 2011. pp. 1–338. [Google Scholar]
- 27.Edwards JR, Bagozzi RP. On the nature and direction of relationships between constructs and measures. Psychol Methods. 2000;5(2):155. doi: 10.1037/1082-989x.5.2.155. [DOI] [PubMed] [Google Scholar]
- 28.Mokkink LB, et al. COSMIN risk of Bias checklist for systematic reviews of patient-reported outcome measures. Qual Life Res. 2018;27(5):1171–1179. doi: 10.1007/s11136-017-1765-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lettink, A., et al., Systematic review of accelerometer-based methods for 24-hour physical behavior assessment in young children (0–5-years-old). Article in preparation. [DOI] [PMC free article] [PubMed]
- 30.Prinsen CAC, et al. COSMIN guideline for systematic reviews of patient-reported outcome measures. Qual Life Res. 2018;27(5):1147–1157. doi: 10.1007/s11136-018-1798-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Terwee CB, et al. COSMIN methodology for evaluating the content validity of patient-reported outcome measures: a Delphi study. Qual Life Res. 2018;27(5):1159–1170. doi: 10.1007/s11136-018-1829-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mokkink LB, et al. The COSMIN study reached international consensus on taxonomy, terminology, and definitions of measurement properties for health-related patient-reported outcomes. J Clin Epidemiol. 2010;63(7):737–745. doi: 10.1016/j.jclinepi.2010.02.006. [DOI] [PubMed] [Google Scholar]
- 33.Field A. Discovering statistics using IBM SPSS statistics. London: SAGE Publications; 2013. ISBN: 9781446249185. https://books.google.nl/books?hl=nl&lr=&id=c0Wk9IuBmAoC&oi=fnd&pg=PP2&dq=reference+Field+A.+Discovering+statistics+using+IBM+SPSS+statistics:+sage%3B+2013.&ots=LcDlJO2w_F&sig=UzPuSLsTGv9BQuM42Ha0fwcnfc&redir_esc=y#v=onepage&q=reference%20Field%20A.%20Discovering%20statistics%20using%20IBM%20SPSS%20statistics%3A%20sage%3B%202013.&f=false.
- 34.Field AP. Discovering statistics using SPSS : (and sex and drugs and rock 'n' roll). 3rd ed. ed. Introducing statistical methods. Los Angeles [i.e. Thousand Oaks, Calif.]: SAGE Publications; 2009. [Google Scholar]
- 35.Cassanello P, et al. Adaptation and study of the measurement properties of a sleep questionnaire for infants and pre-school children. Anales de Pediatria. 2018;89(4):230–237. doi: 10.1016/j.anpedi.2017.12.003. [DOI] [PubMed] [Google Scholar]
- 36.Dhakal AK, et al. A Nepali translation of brief infant sleep questionnaire (BISQ) for assessment of sleep in infants and toddlers: a preliminary report. J Kathmandu Med Coll. 2014;3(3):102–106. [Google Scholar]
- 37.Boran P, et al. Translation into Turkish of the expanded version of the “brief infant sleep questionnaire” and its application to infants. 2014. [Google Scholar]
- 38.Tikotzky L, Volkovich E. Infant nocturnal wakefulness: a longitudinal study comparing three sleep assessment methods. Sleep. 2019;42(1):zsy191. doi: 10.1093/sleep/zsy191. [DOI] [PubMed] [Google Scholar]
- 39.Dias CC, Figueiredo B, Pinto TM. Children's sleep habits questionnaire – infant version. J Pediatr. 2018;94(2):146–154. doi: 10.1016/j.jped.2017.05.012. [DOI] [PubMed] [Google Scholar]
- 40.Liu Z, et al. Reliability and validity of the children’s sleep habits questionnaire in preschool-aged Chinese children. Sleep Biol Rhythms. 2014;12(3):187–193. [Google Scholar]
- 41.Perpétuo C, Fernandes M, Veríssimo M. Comparison between actigraphy records and parental reports of Child's sleep. Front Pediatr. 2020;8(567390):1–8. 10.3389/fped.2020.567390. [DOI] [PMC free article] [PubMed]
- 42.Camerota M, Tully KP, Grimes M, Gueron-Sela N, Propper CB. Assessment of infant sleep: how well do multiple methods compare? Sleep. 2018;41(10):1–12. 10.1093/sleep/zsy146. [DOI] [PMC free article] [PubMed]
- 43.Muller S, et al. Parental report of infant sleep behavior by electronic versus paper-and-pencil diaries, and their relationship to actigraphic sleep measurement. J Sleep Res. 2011;20(4):598–605. doi: 10.1111/j.1365-2869.2011.00926.x. [DOI] [PubMed] [Google Scholar]
- 44.Quante M, Hong B, von Ash T, Yu X, Kaplan ER, Rueschman M, Jackson CL, Haneuse S, Davison K, Taveras EM, Redline S. Associations between parentreported and objectively measured sleep duration and timing in infants at age 6 months. Sleep. 2021;44(4):1–10. 10.1093/sleep/zsaa217. [DOI] [PMC free article] [PubMed]
- 45.Matthey S. The sleep and settle questionnaire for parents of infants: psychometric properties. J Paediatr Child Health. 2001;37(5):470–475. doi: 10.1046/j.1440-1754.2001.00703.x. [DOI] [PubMed] [Google Scholar]
- 46.Asaka Y, Takada S. Comparing sleep measures of infants derived from parental reports in sleep diaries and acceleration sensors. Acta Paediatr. 2011;100(8):1158–1163. doi: 10.1111/j.1651-2227.2011.02204.x. [DOI] [PubMed] [Google Scholar]
- 47.Bélanger M-È, et al. Investigating the convergence between actigraphy, maternal sleep diaries, and the child behavior checklist as measures of sleep in toddlers. Front psychiatry. 2014;5:158. doi: 10.3389/fpsyt.2014.00158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sekine M, et al. The validity of sleeping hours of healthy young children as reported by their parents. J Epidemiol. 2002;12(3):237–242. doi: 10.2188/jea.12.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lam JC, et al. Defining the roles of actigraphy and parent logs for assessing sleep variables in preschool children. Behav Sleep Med. 2011;9(3):184–193. doi: 10.1080/15402002.2011.583906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ishihara K, Doi Y, Uchiyama M. The reliability and validity of the Japanese version of the Children's ChronoType questionnaire (CCTQ) in preschool children. Chronobiol Int. 2014;31(9):947–953. doi: 10.3109/07420528.2014.933841. [DOI] [PubMed] [Google Scholar]
- 51.LeBourgeois MK, Harsh JR. Development and psychometric evaluation of the Children's sleep-wake scale. Sleep Health. 2016;2(3):198–204. doi: 10.1016/j.sleh.2016.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Howie EK, McNally S, Straker LM. Exploring the reliability and validity of the TechU-Q to evaluate device and purpose specific screen use in preschool children and parents. J Child Fam Stud. 2020;29(10):2879–2889. doi: 10.1007/s10826-020-01787-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Carson V, et al. Psychometric properties of a parental questionnaire for assessing correlates of toddlers’ physical activity and sedentary behavior. Meas Phys Educ Exerc Sci. 2017;21(4):190–200. [Google Scholar]
- 54.Burdette HL, Whitaker RC, Daniels SR. Parental report of outdoor playtime as a measure of physical activity in preschool-aged children. Arch Pediatr Adolesc Med. 2004;158(4):353–357. doi: 10.1001/archpedi.158.4.353. [DOI] [PubMed] [Google Scholar]
- 55.Rice KR, Joschtel B, Trost SG. Validity of family child care providers' proxy reports on children's physical activity. Child Obes. 2013;9(5):393–398. doi: 10.1089/chi.2013.0035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bonn SE, et al. Feasibility of a novel web-based physical activity questionnaire for young children. Pediatr Rep. 2012;4(4):e37–7. [DOI] [PMC free article] [PubMed]
- 57.Bingham DD, et al. Reliability and validity of the early years physical activity questionnaire (EY-PAQ) Sports. 2016;4(2):30. doi: 10.3390/sports4020030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Dwyer GM, et al. The validity and reliability of a home environment preschool-age physical activity questionnaire (pre-PAQ) Int J Behav Nutr Phys Act. 2011;8(1):86. doi: 10.1186/1479-5868-8-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Corder K, et al. Is it possible to assess free-living physical activity and energy expenditure in young people by self-report? Am J Clin Nutr. 2009;89(3):862–870. doi: 10.3945/ajcn.2008.26739. [DOI] [PubMed] [Google Scholar]
- 60.Townsend MS, et al. Obesity risk for young children: development and initial validation of an assessment tool for participants of federal nutrition programs. 2014. [Google Scholar]
- 61.Townsend MS, et al. An obesity risk assessment tool for young children: validity with BMI and nutrient values. J Nutr Educ Behav. 2018;50(7):705–717. doi: 10.1016/j.jneb.2018.01.022. [DOI] [PubMed] [Google Scholar]
- 62.Bacardi-Gascón M, et al. Assessing the validity of a physical activity questionnaire developed for parents of preschool children in Mexico. J Health Popul Nutr. 2012;30(4):439. doi: 10.3329/jhpn.v30i4.13327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.González-Gil E, et al. Reliability of primary caregivers reports on lifestyle behaviours of E uropean pre-school children: the T oy B ox-study. Obes Rev. 2014;15:61–66. doi: 10.1111/obr.12184. [DOI] [PubMed] [Google Scholar]
- 64.Sarker H, et al. Validation of parent-reported physical activity and sedentary time by accelerometry in young children. BMC Res Nnotes. 2015;8(1):735. doi: 10.1186/s13104-015-1648-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Chia M, Tay LY, Chua TBK. The development of an online surveillance of digital media use in early childhood questionnaire-SMALLQ™-for Singapore. 2019. [Google Scholar]
- 66.Goncalves W, et al. Cross-cultural adaptation of instruments measuring Children’s movement behaviors and parenting practices in Brazilian families. Int J Environ Res Public Health. 2021;18(1):239. doi: 10.3390/ijerph18010239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hinkley T, et al. The HAPPY study: development and reliability of a parent survey to assess correlates of preschool children's physical activity. J Sci Med Sport. 2012;15(5):407–417. doi: 10.1016/j.jsams.2011.12.009. [DOI] [PubMed] [Google Scholar]
- 68.Costa S, et al. Calibration and validation of the ActiGraph GT3X+ in 2-3 year olds. J Sci Med Sport. 2014;17(6):617–622. doi: 10.1016/j.jsams.2013.11.005. [DOI] [PubMed] [Google Scholar]
- 69.Pate RR, et al. Validation and calibration of an accelerometer in preschool children. Obesity (Silver Spring) 2006;14(11):2000–2006. doi: 10.1038/oby.2006.234. [DOI] [PubMed] [Google Scholar]
- 70.Sirard JR, et al. Calibration and evaluation of an objective measure of physical activity in preschool children. J Phys Act Health. 2005;2(3):345–357. [Google Scholar]
- 71.Reilly JJ, et al. An objective method for measurement of sedentary behavior in 3- to 4-year olds. Obes Res. 2003;11(10):1155–1158. doi: 10.1038/oby.2003.158. [DOI] [PubMed] [Google Scholar]
- 72.Pate RR, O'Neill JR, Mitchell J. Measurement of physical activity in preschool children. Med Sci Sports Exerc. 2010;42(3):508–512. doi: 10.1249/MSS.0b013e3181cea116. [DOI] [PubMed] [Google Scholar]
- 73.Sadeh A, et al. Actigraphically based automatic bedtime sleep-wake scoring: validity and clinical applications. J Ambul Monit. 1989;2(3):209–216. [Google Scholar]
- 74.So K, et al. Actigraphy correctly predicts sleep behavior in infants who are younger than six months, when compared with polysomnography. Pediatr Res. 2005;58(4):761–765. doi: 10.1203/01.PDR.0000180568.97221.56. [DOI] [PubMed] [Google Scholar]
- 75.Sadeh A, et al. Activity-based assessment of sleep-wake patterns during the 1st year of life. Infant Behav Dev. 1995;18(3):329–337. [Google Scholar]
- 76.Treuth MS, et al. Defining accelerometer thresholds for activity intensities in adolescent girls. Med Sci Sports Exerc. 2004;36(7):1259–1266. [PMC free article] [PubMed] [Google Scholar]
- 77.Freedson PS, Melanson E, Sirard J. Calibration of the computer science and applications. Inc accelerometer Med Sci Sports Exerc. 1998;30(5):777–781. doi: 10.1097/00005768-199805000-00021. [DOI] [PubMed] [Google Scholar]
- 78.Wong SL, et al. Actical accelerometer sedentary activity thresholds for adults. J Phys Act Health. 2011;8(4):587–591. doi: 10.1123/jpah.8.4.587. [DOI] [PubMed] [Google Scholar]
- 79.Adolph AL, et al. Validation of uniaxial and triaxial accelerometers for the assessment of physical activity in preschool children. J Phys Act Health. 2012;9(7):944–953. doi: 10.1123/jpah.9.7.944. [DOI] [PubMed] [Google Scholar]
- 80.Sadeh A, Sharkey M, Carskadon MA. Activity-based sleep-wake identification: an empirical test of methodological issues. Sleep. 1994;17(3):201–207. doi: 10.1093/sleep/17.3.201. [DOI] [PubMed] [Google Scholar]
- 81.Sitnick SL, Goodlin-Jones BL, Anders TF. The use of actigraphy to study sleep disorders in preschoolers: some concerns about detection of nighttime awakenings. Sleep. 2008;31(3):395. doi: 10.1093/sleep/31.3.395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Veldman SL, Paw MJCA, Altenburg TM. Physical activity and prospective associations with indicators of health and development in children aged< 5 years: a systematic review. Int J Behav Nutr Phys Act. 2021;18(1):1–11. doi: 10.1186/s12966-020-01072-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Streiner DL, Norman GR, Cairney J. Health measurement scales: a practical guide to their development and use. USA: Oxford University Press; 2015. [Google Scholar]
- 84.Mokkink LB, et al. COSMIN study design checklist for patient-reported outcome measurement instruments. Department of Epidemiology and Biostatistics. 2019. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this review are available from the corresponding author upon reasonable request.