As the coronavirus disease 2019 (COVID-19) pandemic ensues and mass vaccination efforts continue, we learn more about the potential, yet rare, side effects of the vaccine. Along with other worldwide reports regarding postvaccination-associated myocarditis,1 we recently published a case series of 8 patients with this potential complication (young males with a benign disease course).2
On July 30th, a third vaccination dose, a booster shot of the Pfizer vaccine was approved in Israel for adults aged >60 years with promising results.3 Shortly after, mass vaccination of Israelis aged >18 years began. Throughout August 2021, 11 905 people received the booster shot at the Tel Aviv Sourasky Medical Center. Since September 1, 2021, 4 patients presented to our hospital with a clinical picture of myocarditis after receiving the third dose of the Pfizer vaccine. Participants were identified after approaching the emergency department at our center where they were evaluated due to complaints of chest pain, dyspnea, fatigue, and elevated troponin levels. The study was approved by our Institutional Review Board. The data that support the findings of this study are available from the corresponding author upon reasonable request.
All cases involved young patients (aged 21–38 years), all of male gender. Acute COVID-19 infection was ruled out in all patients based on negative polymerase chain reaction swabs and normal chest X-Rays. Three out of 4 patients also tested negative for COVID-19 anti N antibodies, and all 4 patients tested positive for COVID-19 anti-S antibodies, confirming recent vaccination. Common alternative causes of myocarditis (eg, infectious, autoimmune, and toxic) were excluded using serological tests and blood cultures. Eosinophil count was normal and the patients denied recent exposure to new medications/drugs. None of the patients received other vaccinations during that time period.
Previous medical history was notable in 3 out of 4 patients. One had untreated hyperlipidemia. The second had 2 prior episodes of peri-myocarditis from 2014 to 2015 for which he was hospitalized at our institution. Both episodes were presumed to be associated with acute viral gastroenteritis. His baseline echocardiogram was normal. Following his admission in 2015, he underwent a cardiac magnetic resonance (CMR) which showed slightly reduced left ventricular ejection fraction. Late gadolinium enhancement was minimal (comparing to his current CMR). A follow-up stress echocardiogram was described as normal (the patient did not have a follow-up CMR). The third patient had a history of bilateral feet hyperkeratosis. A genetic screening revealed a mutation in keratin 16 gene-(NM_005557.4):c.374A>G; p.Asn125SerKRT16 (not involved in cardiomyopathy but close to KRT9 gene involved in Naxos syndrome). During childhood, he was also followed for a prolonged QT interval which later shortened.
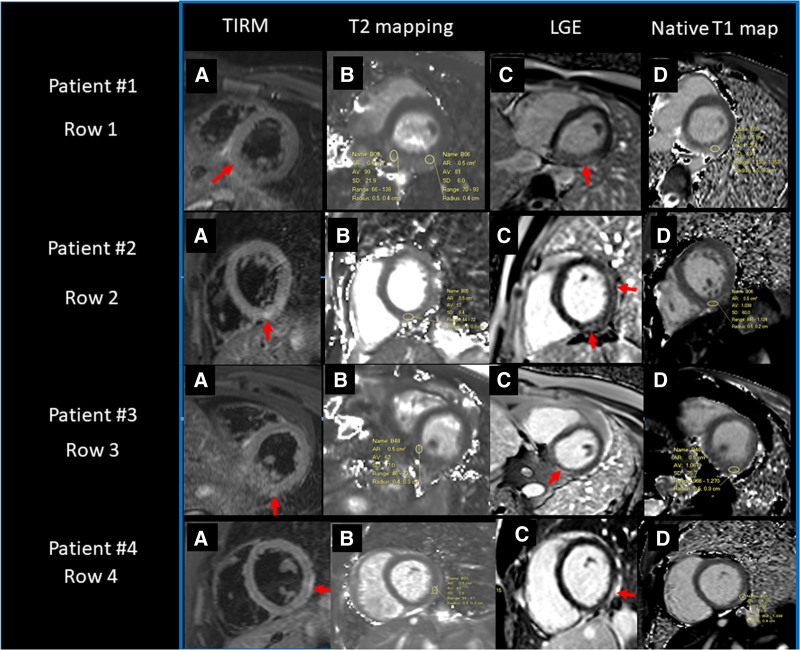
Three out of 4 patients had an uneventful course after the first 2 vaccinations. The fourth developed a short flu-like reaction after the second dose but denied chest pain. All patients presented to our emergency department 2 to 11 days after receiving the third vaccination, all with complaints of fever and weakness, which then developed into chest pain. Upon admission, 2 out of 4 had abnormal ECG with ST-segment elevation in II, III, and AVF or V1 to V2, along with elevated troponin levels (median 2880 ng/L, normal <2.5 ng/L) in all patients. The fluctuating pattern of troponin, evident in our previous report,2 was not seen here. Echocardiogram showed slightly reduced left ventricular ejection fraction (50%–55%) in 2 out of 4 patients. All patients underwent CMR (MAGNETOM Aera 1.5T, Siemens) confirming accepted criteria for myocardial inflammation,4 including late gadolinium enhancement and edema on T2 imaging. According to our institutional local clinical policy, the patients underwent cardiac computed tomography (Spectral CT 7500 Philips, iodine dose 1.3 mL/kg, radiation dose 5–7 mSv) which ruled out obstructive coronary artery disease, but demonstrated on delayed scan (6 minutes postinjection) late iodine enhancement in a distribution typical of myocarditis. Figure shows the CMR of all patients. Symptoms resolution, along with a consistent decrease in troponin levels, occurred in all patients. None suffered from complications (eg, hemodynamic instability, arrhythmias) and all were discharged after several days.
Figure.
Cardiac magnetic resonance imaging findings. Patients 1-4 (A–D, rows 1-4). Local normal T1 values are 945+/-35 ms, T2 46+/-3 ms. A, Short axis oblique view (SAO) T2 weighted dark blood (turbo inversion recovery magnitude [TIRM]) image showing regional edema (arrows), (B) T2 mapping, showing high signal intensity/values corresponding to edema as marked by the region of interest (ROI for patients number 1–4: 99, 57, 62, 63 ms, respectively). C, SAO phase-sensitive inversion recovery showing late gadolinium enhancement (LGE) (arrows) (D) SAO, showing increased value on native T1 (ROI for patients number 1–4: 1254, 1038, 1067, 1168 ms, respectively).
To our knowledge, this is the first report of a suspected booster-associated myocarditis. Similar to previous reports on the association between the COVID-19 vaccine and myocarditis,1 it presents as a rare phenomenon with an estimated prevalence of ≈0.03% and a benign course. Several mechanisms have been proposed to explain this uncommon potential side effect of the vaccine, including a genetic predisposition5; therefore, it is noteworthy that 2 patients, one in this series and another in our previous one, had 2 episodes of peri-myocarditis in the past. Accordingly, a closer postvaccination follow-up might be suggested in patients with similar history. To conclude, we present here a cluster of 4 young males who developed myocarditis following the booster COVID-19 vaccination and had a benign course of disease. Given the time course following mass administration of the booster shot, with few patients presenting with this side effect, we think that myocarditis following the booster shot is a rare complication of the vaccine.
Article Information
Sources of Funding
None.
Disclosures
None.
Nonstandard Abbreviations and Acronyms
- CMR
- cardiac magnetic resonance
- COVID-19
- coronavirus disease 2019
G. Aviram and D. Viskin contributed equally.
For Sources of Funding and Disclosures, see page 124.
Contributor Information
Galit Aviram, Email: galita@tlvmc.gov.il.
Dana Viskin, Email: danaviskin@gmail.com.
Yan Topilsky, Email: topilskyyan@gmail.com.
Sapir Sadon, Email: Sapirsadon8@gmail.com.
Tamar Shalmon, Email: tamarshalmon@gmail.com.
Philippe Taieb, Email: taieb.phil@gmail.com.
Eihab Ghantous, Email: ehab.1988@yahoo.com.
Nir Flint, Email: flintn@gmail.com.
Shmuel Banai, Email: banais@netvision.net.il.
Ofer Havakuk, Email: havakukofer@gmail.com.
References
- 1.Bozkurt B, Kamat I, Hotez PJ. Myocarditis with COVID-19 mRNA vaccines. Circulation. 2021;144:471–484. doi: 10.1161/CIRCULATIONAHA.121.056135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Viskin D, Topilsky Y, Aviram G, Mann T, Sadon S, Hadad Y, Flint N, Shmilovich H, Banai S, Havakuk O. Myocarditis associated with COVID-19 vaccination: echocardiography, cardiac tomography, and magnetic resonance imaging findings. Circ Cardiovasc Imaging. 2021;14:e013236. doi: 10.1161/CIRCIMAGING.121.013236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bar-On YM, Goldberg Y, Mandel M, Bodenheimer O, Freedman L, Kalkstein N, Mizrahi B, Alroy-Preis S, Ash N, Milo R, Huppert A. Protection of BNT162b2 vaccine booster against Covid-19 in Israel. N Engl J Med. 2021;385:1393–1400. doi: 10.1056/NEJMoa2114255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ferreira VM, Schulz-Menger J, Holmvang G, Kramer CM, Carbone I, Sechtem U, Kindermann I, Gutberlet M, Cooper LT, Liu P, et al. Cardiovascular magnetic resonance in nonischemic myocardial inflammation: expert recommendations. J Am Coll Cardiol. 2018;72:3158–3176. doi: 10.1016/j.jacc.2018.09.072 [DOI] [PubMed] [Google Scholar]
- 5.Caso F, Costa L, Ruscitti P, Navarini L, Del Puente A, Giacomelli R, Scarpa R. Could Sars-coronavirus-2 trigger autoimmune and/or autoinflammatory mechanisms in genetically predisposed subjects? Autoimmun Rev. 2020;19:102524. doi: 10.1016/j.autrev.2020.102524 [DOI] [PMC free article] [PubMed] [Google Scholar]