Abstract
Objective:
To determine the prevalence and severity of impacted permanent mandibular second molars (MdM2s) in the general population of Taiwan as well as to evaluate treatment outcomes with an innovative method for impacted MdM2s.
Materials and Methods:
Dental records of 21,580 patients were retrospectively screened in this study. The impactions of MdM2s were registered. The chosen study population consisted of 96 patients with 125 impacted MdM2s who received orthodontic treatment in our clinics. Standardized periapical radiographs were taken to measure the angles and depths of the impacted MdM2s. In addition, the initial uprighting periods of the impacted MdM2s were recorded.
Results:
The prevalence of MdM2 impaction in the Taiwanese population was 0.65%. Most of the angles and depths of the MdM2s were 31–60° and 9–12 mm, respectively. The mean initial uprighting period of the impacted MdM2 was 3.6 months. There were no significant differences between genders in the initial uprighting period based on patient ages, impacted angles, or impacted depths (P > .05). Correlation analysis revealed that the impacted depth was highly and positively correlated with the initial uprighting period (r > .75).
Conclusions:
The prevalence of MdM2 impaction in this study was low but slightly higher than previous reports investigating whites. Although such impactions are rare, it is recommended to diagnose early for an optimal treatment time and reduction of complications. In addition, the effective molar uprighting appliance used in this study has displayed good treatment outcomes with natural improvement of the adjacent infrabony defects of the first molars.
Keywords: Prevalence, Impacted mandibular second molar, Orthodontic, Uprighting, Pole arm
INTRODUCTION
Impaction is defined as failure of tooth eruption caused by a physical obstacle in the eruption path or the abnormal position of the tooth.1 The most commonly affected are third molars, followed by maxillary canines and mandibular second premolars.2,3 Impaction of a second permanent molar is rare and usually occurs in the mandibular arch with an incidence of 0.06–0.3%.3–5
According to Andreasen et al.,6 three main causes have been distinguished for eruption disturbances: ectopic position, obstacles in the eruption path, and failures in the eruption mechanism. Failure of tooth eruption is associated with various systemic and local factors.7 Heredity is also mentioned as an etiologic factor. Recently, mutations in parathyroid hormone receptor 1 (PTH1R) have been identified in several familial cases of primary failure of eruption.8,9 Local factors related to the failure of eruption include malocclusion disturbances of the deciduous dentition, the position of the adjacent teeth, space deficiency in the dental arch, idiopathic factors, supernumerary teeth, odontomas, or cysts.2,4,5,7
Problems associated with impacted second molars are caries, periodontitis, resorption of adjacent teeth, cyst formation, malocclusion, and pain.5,10,11 Treatment options for an impacted molar include extraction, orthodontic uprighting, surgical uprighting, transplantation, surgical-orthodontic approach, and dental implant replacement.10–14 Many orthodontic appliances and techniques have been suggested for uprighting impacted molars. A bonded attachment with a spring fixed in a vertical lingual sheath, push coil springs, interarch vertical elastics, a removable appliance with an uprighting spring, and miniscrews/miniplates have all been used for the uprighting of impacted molars.2,15–17 Most of the aforementioned methods, however, have limitations in the approach of deeply impacted teeth or in the site of installation.
The aims of this study were to investigate the prevalence and severity of impacted mandibular second molars (MdM2s) in Taiwanese patients and to describe an effective treatment modality for impacted MdM2s. The treatment outcomes using this orthodontic appliance were also analyzed.
MATERIALS AND METHODS
Dental records of 21,580 patients (10,668 males and 10,912 females) from three large dental clinics in the City of Kaohsiung, Taiwan, were retrospectively analyzed in this study. The selection criteria were as follows:
Ethnic Taiwanese and older than 10 years
No history of orthodontic treatment
No hereditary diseases or systemic syndrome
One or both MdM2s were impacted
Good-quality panoramic or periapical radiographs of MdM2s were taken
The number, position, and severity of the impacted MdM2s were registered according to present definitions.1 Among the identified subjects, 96 patients with 125 impacted MdM2s were orthodontically treated with an innovative appliance during 1999–2010. For all 96 patients, standardized periapical radiographs of MdM2s were taken before orthodontic treatment. To calibrate magnification, a segmental stainless-steel wire 4 mm in length was attached to each periapical radiograph before exposure. The following landmarks were identified on each periapical film: distal marginal ridge of the first molar (DMR6), mesial marginal ridge of the impacted MdM2 (MMR7), occlusal plane of the first molar (OP6), occlusal plane of the impacted MdM2 (OP7), and stainless-steel wire (SSW). The impacted angle (Ang) defined in this study was the included angle between OP6 and OP7. The impacted depth (Dep) was measured as the vertical distance from DMR6 to MMR7 (Figure 1). The angles were measured with a cephalometric protractor in degrees, whereas the depths were measured with a digital caliper in millimeters. All measurements were surveyed four times, and the means of the measurements were taken as the Ang and Dep. Patient approval was received for this study.
Figure 1.
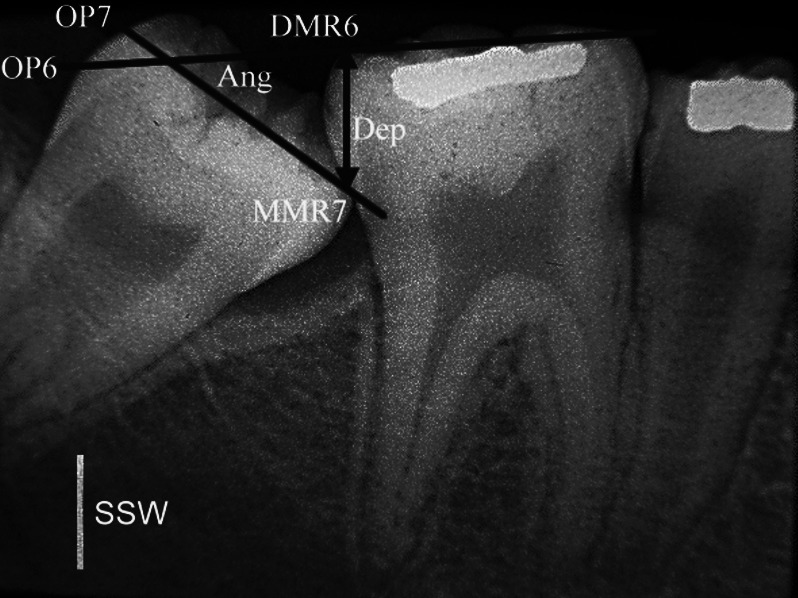
Landmarks and measurements in this study. DMR6, distal marginal ridge of the first molar. MMR7, mesial marginal ridge of the impacted second molar. OP6, occlusal plane of the first molar. OP7, occlusal plane of the impacted second molar. Ang, the included angle between OP6 and OP7. Dep, the vertical distance from DMR6 to MMR7. SSW, stainless-steel wire (4-mm length) that was used to calibrate magnification.
The 96 subjects who had at least one impacted MdM2 were treated with a new molar uprighting spring. This appliance, which we have termed the pole arm, has biomechanics similar to the pole vault. The pole arm was constructed of 0.016 × 0.022 inch titanium molybdenum alloy (TMA) wire (Figure 2). Periapical radiographs were taken of the impacted MdM2 before and after applying the technique to confirm the severity of the impaction and the position of the inserted pole arm. Before insertion of the pole arm appliance, we recommend applying local anesthesia to the buccal and lingual gingivae, which are between the impacted molar and the adjacent tooth. The buccal arm (D) is inserted from the lingual side, passing beneath the contact area between the adjacent tooth and the impacted molar and is pulled out buccally. Activation of the uprighting spring is accomplished by bending the distal contact between the first molar tube and buccal arm (D), when the buccal arm is ligated by wire to the anchor teeth. As the contact works toward restoring its original form, it produces a distal uprighting force against the mesial surface of the impacted molar (Figure 3). Finally, a lingual rest (A) is fixed with glass-ionomer or composite resin on the occlusal surface close to the lingual groove of the first molar to prevent it from sliding out of position. Moving the pole arm gingivally activates the appliance. The pole arm can be reactivated in the mouth by lifting, gently squeezing the buccal arm occlusally, and ligating the buccal arm again. After the initial adjustment at 3 to 4 weeks, adjustments every 6 weeks seem to be adequate. The pole arm uprighting spring acts on impacted MdM2s as depicted in Figure 4. When the impacted MdM2s were uprighted with their mesial marginal ridges above the distal contours of the first molars, the pole arm uprighting springs were removed, and the activation periods were recorded as the initial uprighting periods.
Figure 2.
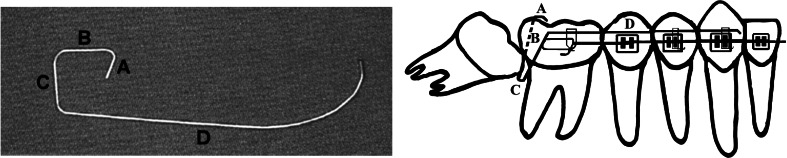
The pole arm uprighting spring. A, lingual rest bending; B, occlusogingival bending with length according to the impacted depth; C, buccolingual bending with length according to the buccolingual width of the impacted molar; D, mesial extension following the buccal curve of anterior anchor teeth.
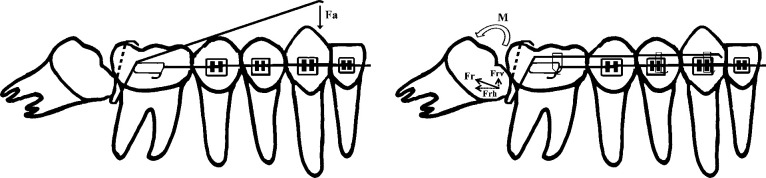
Figure 3.
Force delivered to the pole arm and force as well as moment acting on the impacted molar. Fa, active force acting on the pole arm; Fr, reciprocal force acting on the impacted molar; Frv, vertical (extrusive) component of Fr; Frh, horizontal (distal) component of Fr; and M, moment acting on the impacted molar.
Figure 4.

Intraoral photograph and periapical radiograph at insertion of the pole arm.
The orthodontically treated impacted MdM2s were assigned to different groups according to patient age, impacted angles, and impacted depths (Tables 1–3). The chi-square test, one-way analysis of variance (ANOVA), Tukey-Kramer HSD, and pairwise correlations were performed to test statistical significance of differences (P < .05) and correlations.
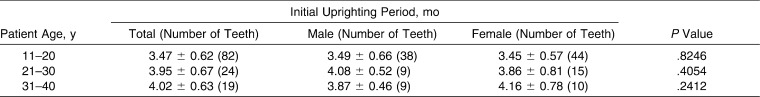
Table 1.
Patient Ages and Initial Uprighting Periods of the Impacted Second Molars
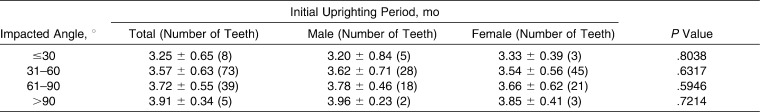
Table 2.
Impacted Angles and Initial Uprighting Periods of the Impacted Second Molars
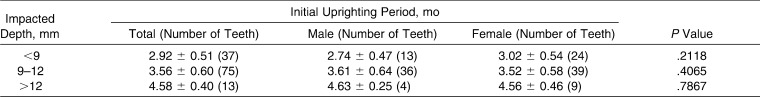
Table 3.
Impacted Depths and Initial Uprighting Periods of the Impacted Second Molars
RESULTS
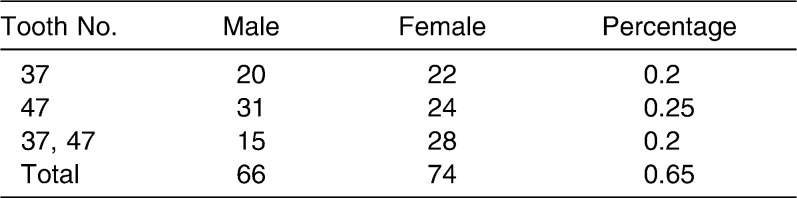
The prevalence of the impacted MdM2s in 21,580 patients is shown in Table 4. There were a total of 140 subjects (66 males and 74 females; mean age 26.5 ± 8.4 years, ranging from 11 to 67 years of age) with one or two impacted MdM2s. Overall, 183 impacted MdM2s were found in the survey group, and the resulting prevalence was 0.65%. The male-to-female ratio was 1∶1.12, which showed no significant difference. In 97 cases, the impaction was unilateral: 42 on the left side and 55 on the right side. In the remaining 43 subjects, the impaction was bilateral.
Table 4.
Overall Prevalence of the Impacted Mandibular Second Molars in 21,580 Patients
Among the 140 subjects with 183 impacted MdM2s, 96 patients (42 males, 54 females) with 125 impacted MdM2s were orthodontically treated using the pole arm appliance, and the remaining 44 subjects were not treated or had undergone tooth extraction due to personal considerations or poor prognosis of the MdM2s.
Following activation of the pole arm spring, rapid uprighting of the impacted molar occurred in 2 to 4 months in most cases. The mean initial uprighting period of the impacted MdM2 was 3.6 months and ranged from 2 months to 5 months. The major impacted angles of MdM2s were between 31° and 60°, with a mean initial uprighting period of 3.62 ± 0.71 months in males and 3.54 ± 0.56 months in females. Most of the impacted depths were between 9 and 12 mm, with a mean initial uprighting period of 3.61 ± 0.64 months in males and 3.52 ± 0.58 months in females (Tables 1–3).
There were no significant differences between genders in the initial uprighting period based on patient age, impacted angles, or impacted depths (P > .05). No significant differences in the initial uprighting period were found for patients of different ages or for patients with different degrees of impaction (P > .05). However, significant differences in the initial uprighting period existed when comparing the three groups of patients with different impacted depths (P < .05). A positive correlation was found between the impacted angle and the initial uprighting period (.5 < r < .75), whereas the impacted depth showed a highly positive correlation with the initial uprighting period (r > .75).
One female subject aged 18 who had presented with bilaterally impacted MdM2s and who was successfully treated using the pole arm appliance is shown in Figures 5 and 6. Healing of the adjacent infrabony defects of the first molars was observed.
Figure 5.
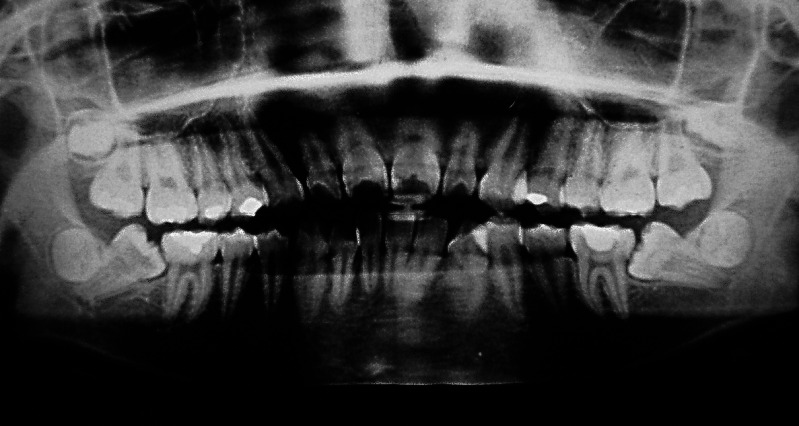
Pretreatment panoramic radiograph showing bilaterally impacted mandibular second molars.
Figure 6.

Posttreatment panoramic radiograph showing corrected inclination of mandibular second molars.
DISCUSSION
The prevalence of impacted MdM2s in this study population was 0.65%. There is probable reason to believe that 0.65% is an underestimate due to some deeply impacted MdM2s being neglected during clinical examination along with radiographs not being routinely taken from all subjects. Besides, impacted MdM2s are often ignored by asymptomatic patients and are incidentally discovered during routine dental visits. Notwithstanding the aforementioned possible causes, the prevalence of impacted MdM2s in this study was slightly higher than previously reported.3–5 Larger tooth sizes among Chinese compared with whites may partly explain the higher prevalence.18,19 Patients with impacted MdM2s have been reported to have a more frequent occurrence of morphological tooth anomalies, such as root deflections, invaginations, and taurodontism.20,21 In a recent study, Shapira et al.22 investigated genetic traits in MdM2 impaction and found that the Chinese-American population had a higher prevalence (2.3%) of MdM2 impaction compared with the Israeli population (1.4%).
In the present study, there are more females than males with impacted MdM2s, but no significant difference was detected. This is contrary to the report by Varpio and Wellfelt,4 who found that boys had more eruption disturbances of the MdM2s than girls did. On the other hand, several studies have revealed no gender differences concerning the prevalence of impacted MdM2s.5,21,23 Therefore, no conclusion can be made as to whether any correlation exists between sex and impacted MdM2s. The different outcomes in this study and other previous reports may have resulted from the methodology, sample size, age, and racial differences.
Impacted MdM2s may incite various pathologic conditions such as caries, periodontitis, pericoronitis, and resorption of first molar roots. Thus, it is suggested that these teeth be diagnosed and treated at an early age.2,5,10 The best time to treat impacted MdM2s was reported to be between 11 and 14 years of age, when root formation of the MdM2s is incomplete.2 Our findings indicated that although the age of the patient affected the initial uprighting period, it seemed to have little impact on the performance and outcome of the technique. Despite this, it is crucial to make an early diagnosis for an optimal treatment time and reduction of complications.
The impacted angle and impacted depth played more important roles than patient age in determining the difficulty and initial uprighting period of the impacted MdM2. There was a tendency toward a longer initial uprighting period when the MdM2 was more deeply, horizontally, or distally impacted.
Tooth extraction, orthodontic uprighting, surgical uprighting, transplantation, surgical-orthodontic approach, and dental implant replacement have been proposed to treat impacted molars.10–17 Each modality has its indications, contraindications, advantages, and disadvantages. For example, many subjects in this study were younger than 20 years, implying the potential growth of the craniofacial skeleton and dental implant replacement of an impacted MdM2 was not feasible.24
The innovation of the pole arm appliance eliminates the need for application of an early bonding or banding apparatus to impacted molars.14 Compared with many tip-back cantilevers, the pole arm uprighting spring seldom causes occlusal interference. Furthermore, the nonrequirement of surgical exposure of adequate crown surface for the bonding/banding apparatus or surgical installation of miniscrews/miniplates has greatly increased the acceptance of this device by the patients.
Before uprighting the impacted second molar, the need for third molar extraction must be well evaluated. Usually, the third molar can hinder the distal movement of the impacted second molar, implying the need for extraction. Nevertheless, if the root formation of the impacted second molar is incomplete and the degree of impaction is mild, extraction of the third molar is not so urgent, until otherwise deemed necessary.2,10,14
Healing or improvement of infrabony periodontal defects on the distal surfaces of the first molars was noticed in this study. The uprighting of impacted MdM2s may well raise the alveolar bone coronally and repair the infrabony defects on the distal roots of the first molars, an effect that is beneficial for the long-term periodontal health of these teeth.2,14,25
This uprighting appliance is effective and had been used for the past 12 years in the treatment of 96 patients with 125 impacted MdM2s. It has also been used to upright first and third molars. Occasionally, the technique has also been applied to the maxillary teeth. Various initial uprighting periods for impacted second molars were observed in patients of different age groups and with different impacted angles and depths. The analyzed data can be regarded as references for the prediction of treatment time but should not be interpreted as absolute values when consulting with patients due to individual variations.
To date, no clear standard therapy has been established for treating impacted MdM2s. Many factors such as age, occlusion, the presence of the third molar, the degree of crowding, pathological conditions, the position and degree of root dilacerations of the impacted MdM2, and patient cooperation and expectations should be considered before making a final treatment decision.2,10,11,14,21,24 Most importantly, the potential risks and possible benefits of treatment alternatives should be informed and discussed before intervention, which should be evaluated on an individual case basis.
CONCLUSIONS
The prevalence of impacted MdM2s was low but slightly higher than previous reports. Although the impaction is rare, it is crucial to diagnose early for an optimal treatment time and reduction of complications.
Orthodontic treatment of the impacted MdM2s with the pole arm appliance seemed to be effective and success predictable.
Natural improvement of the adjacent infrabony defects of the first molars through orthodontic uprighting of impacted MdM2s contributed to the healthy periodontium.
REFERENCES
- 1.Raghoebar G. M, Boering G, Vissink A, Stegenga B. Eruption disturbances of permanent molars: a review. J Oral Pathol Med. 1991;20:159–166. doi: 10.1111/j.1600-0714.1991.tb00913.x. [DOI] [PubMed] [Google Scholar]
- 2.Sawicka M, Racka-Pilszak B, Rosnowska-Mazurkiewicz A. Uprighting partially impacted permanent second molars. Angle Orthod. 2007;77:148–154. doi: 10.2319/010206-461R.1. [DOI] [PubMed] [Google Scholar]
- 3.Grover P. S, Lorton L. The incidence of unerupted permanent teeth and related clinical cases. Oral Surg Oral Med Oral Pathol. 1985;59:420–425. doi: 10.1016/0030-4220(85)90070-2. [DOI] [PubMed] [Google Scholar]
- 4.Varpio M, Wellfelt B. Disturbed eruption of the lower second molar: clinical appearance, prevalence, and etiology. ASDC J Dent Child. 1988;55:114–118. [PubMed] [Google Scholar]
- 5.Bondemark L, Tsiopa J. Prevalence of ectopic eruption, impaction, retention and agenesis of the permanent second molar. Angle Orthod. 2007;77:773–778. doi: 10.2319/072506-306.1. [DOI] [PubMed] [Google Scholar]
- 6.Andreasen J. O, Petersen J. K, Laskin D. M. Textbook and Color Atlas of Tooth Impactions. Copenhagen, Denmark: Munksgaard; 1997. pp. 199–208. [Google Scholar]
- 7.Suri L, Gagari E, Vastardis H. Delayed tooth eruption: pathogenesis, diagnosis, and treatment. A literature review. Am J Orthod Dentofacial Orthop. 2004;126:432–445. doi: 10.1016/j.ajodo.2003.10.031. [DOI] [PubMed] [Google Scholar]
- 8.Frazier-Bowers S. A, Simmons D, Koehler K, Zhou J. Genetic analysis of familial non-syndromic primary failure of eruption. Orthod Craniofac Res. 2009;12:74–81. doi: 10.1111/j.1601-6343.2009.01440.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Frazier-Bowers S. A, Simmons D, Wright J. T, Proffit W. R, Ackerman J. L. Primary failure of eruption and PTH1R: the importance of a genetic diagnosis for orthodontic treatment planning. Am J Orthod Dentofacial Orthop. 2010;137:160.e1–7. doi: 10.1016/j.ajodo.2009.10.019. [DOI] [PubMed] [Google Scholar]
- 10.Kurol J. Impacted and ankylosed teeth: why, when, and how to intervene. Am J Orthod Dentofacial Orthop. 2006;129:86–90. doi: 10.1016/j.ajodo.2005.11.008. [DOI] [PubMed] [Google Scholar]
- 11.Magnusson C, Kjellberg H. Impaction and retention of second molars: diagnosis, treatment and outcome. Angle Orthod. 2009;79:422–427. doi: 10.2319/021908-97.1. [DOI] [PubMed] [Google Scholar]
- 12.McAboy C. P, Grumet J. T, Siegel E. B, Iacopino A. M. Surgical uprighting and repositioning of severely impacted mandibular second molars. J Am Dent Assoc. 2003;134:1459–1462. doi: 10.14219/jada.archive.2003.0074. [DOI] [PubMed] [Google Scholar]
- 13.Motamedi M. H, Shafeie H. A. Technique to manage simultaneously impacted mandibular second and third molars in adolescent patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:464–466. doi: 10.1016/j.tripleo.2006.05.030. [DOI] [PubMed] [Google Scholar]
- 14.Fu P. S, Lai C. H, Wu Y. M, et al. Uprighting impacted mandibular permanent second molars with the tip-back cantilever technique. J Den Sci. 2008;3:174–180. [Google Scholar]
- 15.Majourau A, Norton L. A. Uprighting impacted second molars with segmented springs. Am J Orthod Dentofacial Orthop. 1995;107:235–238. doi: 10.1016/s0889-5406(95)70137-0. [DOI] [PubMed] [Google Scholar]
- 16.Giancotti A, Muzzi F, Santini F, Arcuri C. Miniscrew treatment of ectopic mandibular molars. J Clin Orthod. 2003;37:380–383. [PubMed] [Google Scholar]
- 17.Giancotti A, Arcuri C, Barlattani A. Treatment of ectopic mandibular second molar with titanium miniscrews. Am J Orthod Dentofacial Orthop. 2004;126:113–117. doi: 10.1016/j.ajodo.2003.08.025. [DOI] [PubMed] [Google Scholar]
- 18.Ling J. Y, Wong R. W. Tanaka-Johnston mixed dentition analysis for southern Chinese in Hong Kong. Angle Orthod. 2006;76:632–636. doi: 10.1043/0003-3219(2006)076[0632:TMDAFS]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 19.Cho S. Y, Ki Y, Chu V, Chan J. Impaction of permanent mandibular second molars in ethnic Chinese schoolchildren. J Can Dent Assoc. 2008;74:521e. [PubMed] [Google Scholar]
- 20.Vedtofte H, Andreasen J. O, Kjaer I. Arrested eruption of the permanent lower second molar. Eur J Orthod. 1999;21:31–40. doi: 10.1093/ejo/21.1.31. [DOI] [PubMed] [Google Scholar]
- 21.Kenrad J, Vedtofte H, Andreasen J. O, Kvetny M. J, Kjær I. A retrospective overview of treatment choice and outcome in 126 cases with arrested eruption of mandibular second molars. Clin Oral Invest. 2011;15:81–87. doi: 10.1007/s00784-009-0364-3. [DOI] [PubMed] [Google Scholar]
- 22.Shapira Y, Finkelstein T, Shpack N, Lai Y. H, Kuftinec M. M, Vardimon A. Mandibular second molar impaction. Part I: genetic traits and characteristics. Am J Orthod Dentofacial Orthop. 2011;140:32–37. doi: 10.1016/j.ajodo.2009.08.034. [DOI] [PubMed] [Google Scholar]
- 23.Baccetti T. Tooth anomalies associated with failure of eruption of first and second permanent molars. Am J Orthod Dentofacial Orthop. 2000;118:608–610. doi: 10.1067/mod.2000.97938. [DOI] [PubMed] [Google Scholar]
- 24.Fudalej P, Kokich V. G, Leroux B. Determining the cessation of vertical growth of the craniofacial structures to facilitate placement of single-tooth implants. Am J Orthod Dentofacial Orthop. 2007;131:59–67. doi: 10.1016/j.ajodo.2006.07.022. [DOI] [PubMed] [Google Scholar]
- 25.Alessandri Bonetti G, Pelliccioni G. A, Checchi L. Management of bilaterally impacted mandibular second and third molars. J Am Dent Assoc. 1999;130:1190–1194. doi: 10.14219/jada.archive.1999.0373. [DOI] [PubMed] [Google Scholar]