Abstract
Purpose:
Total knee arthroplasty (TKA) is one of the most performed procedures. Postoperative pain control is an important factor for the improvement of patient's quality of life. The aim of this study is to report pain control results and functional outcome scores associated with adductor canal blockade (ACB) usage post-TKA.
Methods:
A prospective case series study of patients who underwent TKA for degenerative osteoarthritis with ACB postoperatively from 2018 to 2019 in a single center in Saudi Arabia, Riyadh. Assessment of functional outcome scores and pain level were measured preoperatively and postoperatively respectively using Knee injury and Osteoarthritis Outcome Score (KOOS) and the Visual Analog Scale (VAS).
Results:
Average KOOS score preoperatively for all 5 domains showed a marked improvement at 3 months compared to preoperative values. Pain score postoperatively was measured at 12, 24, and 48 h with an average of 0.7, 1.2, and 0.6 out of 10 on the VAS scale, respectively. The incidence of associated common side effects with the use of analgesic use was included as an add-on in the postoperative questionnaire.
Conclusion:
In conclusion, by comparing preoperative and postoperative pain levels and functional outcome scores, our study showed a significant pain control and improved functional outcome scores following TKA using ACB.
Keywords: Adductor canal block, pain control, Saudi Arabia
Introduction
Adequate postoperative pain control following total knee arthroplasty (TKA) has been a major challenge in orthopedic surgery practice. Efficient and immediate postoperative pain management is important to promote better functional recovery, improve patient satisfaction, and reduce the rate of chronic postoperative pain.[1,2] Despite the evolvement of analgesic modalities, pain control post-TKA remains a challenge for surgeons and patients. There is no standardized protocol for pain management post-TKA. Traditionally, intravenous patient-controlled analgesia (PCA), continuous epidural infusion, and parenteral and oral opioids were used for postoperative pain control.[1,2,3] However, there has been a major move towards multimodal analgesia, using a peripheral nerve blockade and local infiltration analgesia to minimize opioid-related adverse effects following surgery. Femoral nerve block (FNB) and adductor canal catheter block (ACB) are the most frequently used peripheral nerve blockade methods. FNB blocks both the motor and sensory functions of the nerve, it has a disadvantage of weakening the quadriceps muscle strength, resulting in delayed mobilization. Conversely, ACB provides a pure sensory nerve block with preserved quadriceps muscle function, facilitating postoperative rehabilitation.[4,5] Studies comparing the two techniques, reported approximate equivalency between the two used block methods.[4,5,6,7,8] The aim of this study is to assess the efficacy of the ACB with severe knee osteoarthritis and limited mobility following TKA, through assessing the early functional outcome scores and pain levels.
Methodology
Study design, study setting, and participants
A prospective case series was conducted in a single tertiary-care hospital in Riyadh, Saudi Arabia. All patients with severe osteoarthritis who underwent elective unilateral total knee arthroplasty received an adductor canal catheter blockade for analgesia from 2018 to 2019. Exclusion criteria included patients who had other types of arthritis, who were admitted for revision TKA surgery or refused to participate in this study.
Data collection
A prospective assessment of the study sample. The primary outcomes were the assessment of the functional outcome score and pain levels. The functional outcomes were calculated using the Knee injury and Osteoarthritis Outcome Score (KOOS), performed at admission and at 3 months postoperatively. The Visual Analog Score (VAS) was performed to assess postoperative pain by a trained nurse at defined timed intervals (12, 24, 48, and 72 h).[9] The secondary outcomes were early physiotherapy progression, total opioids consumption during admission [calculated in morphine milligram equivalents (MME)], and the prevalence of postoperative side effects associated with analgesic consumption. The range of motion (ROM) was measured by a physiotherapist using a goniometer during the sessions. All the patients received a standard postoperative multimodal analgesic regimen. The anesthesia pain service team managed analgesia when the catheter was in place, which was removed on the 3rd postoperative day. Regular intravenous acetaminophen Q8 hours, oral celecoxib twice a day (for 30 days postoperatively), and IV hydromorphone for breakthrough pain (first 3 days). Tramadol and morphine were used as an alternative or as a concurrent treatment to hydromorphone as required.
Knee injury and osteoarthritis outcome score (KOOS)
KOOS is a comprehensive patient-reported outcome measurement instrument developed in 1990, validated, and translated to multiple languages, including Arabic. It consists of 5 subscales: (1) Pain experienced during daily activities, (2) Other symptoms experienced 1 week beore surgery, such as swelling, clicking, and a limited range of motion, (3) Difficulties faced during daily activities such as standing, going shopping, and performing domestic duties, (4) Difficulties faced during recreational activities and sports, and finally (5) Knee-related changes in the quality of life (QOL) such as awareness and lifestyle change.[10] The reliability of the Arabic cross-cultural adaptation of the instrument was one of the reasons the authors chose to proceed with implementation.[11]
Administration of the ACB
An ACB was performed immediately after the surgery in the operating room by the attending anesthesiologist. A high-frequency linear ultrasound transducer was placed horizontally on the medial side of the thigh mid-way between the anterior superior iliac spine and the patella. A 22-gauge needle was placed under real-time visualization. An initial dose of 15 mL bupivacaine (0.5%) was administered at a rate of 10 mL/h. On the 3rd day postoperatively, the catheter was removed.
Data management and analysis
Data analysis was done using the STATA14 software package (StataCorp. 2015. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP). The KOOS questionnaire was analyzed using the referenced manual.[12] Pre- and postoperative comparisons of the KOOS scores were done using a paired Students't-test. The descriptive analysis of the numerical data was reported as mean and standard deviation (SD). Frequency and percentage wre used to describe the categorical variables. The severity of the pain, in the immediate postoperative period, and at the 3-months follow-up visit was assessed using VAS. The results were compared using a paired Students’ t-test. Patients were divided into two groups, a positive pain group and a negative pain group for analysis purposes. The mean immediate postoperative VAS is reported in the positive pain group only to avoid data skewness as most patients were expected to report no pain. The Shapiro-Wilk test of normality was used to test the distribution of the positive pain group and is reported as mean and SD.
Ethical approval
The ethical approval was obtained from the Institutional Review Board of our institution under protocol number RC18/293/R.
Results
A total of 114 patients (122 Knees) met the inclusion criteria for the study. The mean age was 64 ± 8.6 years, and females represented the majority (76%) of the sample size. The highest proportion of patients were morbidly obese (44%). The average length of hospital stay was 8 ± 3.6 days [Table 1].
Table 1.
Baseline characteristics of respondents
| Variable | Category | n | % |
|---|---|---|---|
| Gender | Male | 30 | 24 |
| Female | 94 | 76 | |
| Age | Mean 64 | SD 8.6 | |
| BMI group | 18.5-24.9 | 2 | 1.6 |
| 25-29.9 | 29 | 23 | |
| 30-34.9 | 37 | 29 | |
| >35 | 55 | 44 | |
| Smoker | Yes | 2 | 1.6 |
| No | 122 | 98 | |
| Previous surgery on the same side | Yes | 15 | 12 |
| No | 109 | 88 | |
| Length of stay at the hospital | Mean 8 | SD 3.6 | |
| Affected knee | Right | 61 | 49 |
| Left | 63 | 51 |
The KOOS indicated pronounced improvement in all five subscales, 3 months post-surgery, compared to the baseline (P > 0.01). The mean preoperative score was 31, which increased significantly to 72 postoperatively [Graph 1]. The quality-of-life scores had the highest improvement, with a marked progression from 6 preoperatively to 61, at 3-months, postoperatively.
Graph 1.
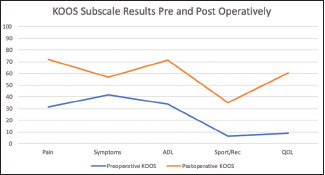
Pre- and post-operative functional recovery results assessed using Knee Injury and Osteoarthritis Outcome Scores (KOOS)
The mean level of preoperative pain at rest was 8, which significantly decreased to 4, at 3-months postoperatively (P > 0.01). In the immediate postoperative period, 85%, 76%, 87%, and 92% of patients in the study reported no pain at 12, 24, 48, and 72 h post-operatively, respectively. The group that reported pain in the same period, had a mean VAS of 4.8 ± 1.7 at 12 h, 5 ± 1.9 at 24 h, 4.8 ± 1.6 at 48 h, and 4.5 ± 1.9 at 72 h, respectively [Graph 2]. The majority (90%) of the patients in the study required additional narcotics to control their breakthrough pain. The average total opioids consumption from day 0 to day 3 was 2, 9, 10, and 9 (unit), respectively [Graph 3]. The reported side effects were relevant in 40 patients. Nausea was the most frequent side effect (23%) followed by constipation (18%) and dizziness (14%) [Table 2]. The postoperative physiotherapy progression showed that most patients were able to mobilize during the first 2 days (mean 1.7 days) with a gradually increasing range of motion (ROM) [Table 3].
Graph 2.
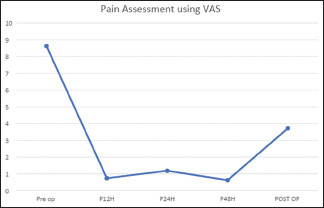
Visual analog scale pain scores of patients
Graph 3.
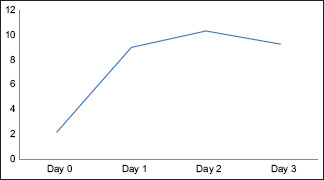
Total opioids consumption
Table 2.
Common postoperative side effects associated with pain medication usage
| Type of symptoms | Percentage of sample |
|---|---|
| Nausea | 23% |
| Constipation | 18% |
| Dizziness | 14% |
| Vomiting | 6% |
| Difficulty Breathing | 5% |
| Urinary retention | 4% |
| Sedation | 2% |
| Heartburn | 1.6% |
| Abdominal Pain | 1% |
Table 3.
Postoperative physiotherapy progression
| Day 1 | Day 2 | Day 3 | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Extension | Flexion | Extension | Flexion | Extension | Flexion | |
| Range of Motion | 2.1 | 88 | 2.3 | 92 | 2 | 97 |
| Mobilization | ||||||
| Mean | 1.7 Days | Standard deviation: 1 | ||||
Discussion
Analgesia post-TKA remains a challenge with continuing efforts to improve the currently available modalities. The patient's age and preoperative functional activity level have an effect on the recovery time and postoperative pain significantly[13] This encourages individual optimization of postoperative pain control. In many clinical trials, ACB has been found equivalent in the adequacy of pain control to FNB. This prompted the authors to investigate the effectiveness of this modality in the elderly population with low preoperative functional activity and high preoperative pain levels.
The pain control was adequate while the catheter was in place for the first 3 days, as evidenced by the majority of the patients, who reported either no postoperative pain and low pain level. An interesting observation was an increase in patients reporting pain at 24 h postoperatively, which may be attributed to the initiation of physiotherapy. It is expected that the level of pain would increase after the catheter removal on day 3, despite that it has remained comparatively low compared with the preoperative pain. In this study, opioids consumption was negligibly low compared to the literature as the three-day total opioid consumption amounted to 28MME only. Roof et al. in a recent study reviewed 4038 TKAs across multiple institutions and multiple surgeons. They reported an average of 46.24 ±0.75 MME/day/patient encounter and a lack of consistency between institutions.[14] Roof et al.'s study highlights the necessity of continued innovation to reach a standardized pain control regimen.
Early mobilization is the hallmark of ACB with catheter use. This modality blocks the sensory branch of the femoral and the saphenous nerve, thus encouraging early mobilization in the postoperative period.[8] Severe muscle weakness may interfere with adequate mobilization post-TKA, the reason that discourages the use of FNB. Our current study presents a challenge for physiotherapy, as most of the patients were unable to walk more than a few steps before surgery. This may explain the delay in mobilization postoperatively with most patients mobilizing on day 2, as well as the increase in opioid consumption starting at day 1 postoperatively.
The KOOS functional scores were reported after 3 months to evaluate any delay in patient's progression with physiotherapy due to their severely limited preoperative scores. All patients on average progressed as expected and showed statistically significant improvement.
Future research will focus on the efficacy of eliminating posterior knee pain as patients who reported knee pain in this study, reported mainly posterior pain. Infiltration between the popliteal artery and capsule of the knee (IPACK) block presents an interesting adjuvant to ACB catheter infiltration.[15] In addition, periarticular injection (PIA) with long-acting agents such as bupivacaine presents an interesting alternative to ACB catheter as a whole, as recent randomized control trials (RCTs) showed promising results.[16,17,18]
Conclusion
ACB catheter block continues to show efficacy, even in a low mobility population with a high preoperative level of pain, for early postoperative pain control.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Turnbull ZA, Sastow D, Giambrone GP, Tedore T. Anesthesia for the patient undergoing total knee replacement: Current status and future prospects. Local Reg Anesth. 2017;10:1–7. doi: 10.2147/LRA.S101373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Song SJ. Pain management and anesthesia in total knee arthroplasty. Knee Surg Relat Res. 2017;29:77–9. doi: 10.5792/ksrr.17.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kukreja P, Feinstein J, Kalagara HK, Huntley SR, Lee SR, Naranje S, et al. A Summary of the anatomy and current regional anesthesia practices for postoperative pain management in total knee arthroplasty. Cureus. 2018;10:e2755. doi: 10.7759/cureus.2755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Koh IJ, Choi YJ, Kim MS, Koh HJ, Kang MS, In Y. Femoral nerve block versus adductor canal block for analgesia after total knee arthroplasty. Knee Surg Relat Res. 2017;29:87–95. doi: 10.5792/ksrr.16.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lim YC, Quek HYK, Phoo WHJ, Mah CL, Tan S. A randomised controlled trial comparing adductor canal block and femoral nerve block for knee arthroplasty. Singapore Med J. 2019;60:145–9. doi: 10.11622/smedj.2018082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li D, Yang Z, Xie X, Zhao J, Kang P. Adductor canal block provides better performance after total knee arthroplasty compared with femoral nerve block: A systematic review and meta-analysis. Int Orthop. 2016;40:925–33. doi: 10.1007/s00264-015-2998-x. [DOI] [PubMed] [Google Scholar]
- 7.Jæger P, Zaric D, Fomsgaard JS, Hilsted KL, Bjerregaard J, Gyrn J, et al. Adductor canal block versus femoral nerve block for analgesia after total knee arthroplasty: A randomized, double-blind study. Reg Anesth Pain Med. 2013;38:526–32. doi: 10.1097/AAP.0000000000000015. [DOI] [PubMed] [Google Scholar]
- 8.Gao F, Ma J, Sun W, Guo W, Li Z, Wang W. Adductor canal block versus femoral nerve block for analgesia after total knee arthroplasty: A systematic review and meta-analysis. Clin J Pain. 2017;33:356–68. doi: 10.1097/AJP.0000000000000402. [DOI] [PubMed] [Google Scholar]
- 9.Heller GZ, Manuguerra M, Chow R. How to analyze the visual analogue scale: Myths, truths and clinical relevance. Scand JPain. 2016;13:67–75. doi: 10.1016/j.sjpain.2016.06.012. [DOI] [PubMed] [Google Scholar]
- 10.Collins NJ, Misra D, Felson DT, Crossley KM, Roos EM. Measures of knee function: International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form, Knee Injury and Osteoarthritis Outcome Score (KOOS), Knee Injury and Osteoarthritis Outcome Score Physical Function Short Form (KOOS-PS), Knee Outcome Survey Activities of Daily Living Scale (KOS-ADL), Lysholm Knee Scoring Scale, Oxford Knee Score (OKS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Activity Rating Scale (ARS), and Tegner Activity Score (TAS) Arthritis Care Res. 2011;63(Suppl 11):S208–28. doi: 10.1002/acr.20632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alfadhel SA, Vennu V, Alnahdi AH, Omar MT, Alasmari SH, AlJafri Z, et al. Cross-cultural adaptation and validation of the Saudi Arabic version of the Knee Injury and Osteoarthritis Outcome Score (KOOS) Rheumatol Int. 2018;38:1547–55. doi: 10.1007/s00296-018-4072-7. [DOI] [PubMed] [Google Scholar]
- 12.Roos EM, Lohmander LS. The Knee injury and Osteoarthritis Outcome Score (KOOS): From joint injury to osteoarthritis. Health Qual Life Outcomes. 2003;1:64. doi: 10.1186/1477-7525-1-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Harato K, Kobayashi S, Kojima I, Sakurai A, Tanikawa H, Niki Y. Factors affecting one-leg standing time in patients with end-stage knee osteoarthritis and the age-related recovery process following total knee arthroplasty. J Orthop Surg Res. 2017;12:21. doi: 10.1186/s13018-017-0522-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Roof MA, Sullivan CW, Feng JE, Anoushiravani AA, Waren D, Friedlander S, et al. Inpatient opioid consumption variability following total knee arthroplasty: Analysis of 4,038 procedures. J Knee Surg. 2020 doi: 10.1055/s-0040-1702183. doi: 10.1055/s-0040-1702183. [DOI] [PubMed] [Google Scholar]
- 15.Thobhani S, Scalercio L, Elliott CE, Nossaman BD, Thomas LC, Yuratich D, et al. Novel regional techniques for total knee arthroplasty promote reduced hospital length of stay: An analysis of 106 patients. Ochsner J. 2017;17:233–8. [PMC free article] [PubMed] [Google Scholar]
- 16.Sardana V, Burzynski JM, Scuderi GR. Adductor canal block or local infiltrate analgesia for pain control after total knee arthroplasty. A systematic review and meta-analysis of randomized controlled trials? J Arthroplasty. 2019;34:183–9. doi: 10.1016/j.arth.2018.09.083. [DOI] [PubMed] [Google Scholar]
- 17.Uesugi K, Kitano N, Kikuchi T, Sekiguchi M, Konno S. Comparison of peripheral nerve block with periarticular injection analgesia after total knee arthroplasty: A randomized, controlled study. Knee. 2014;21:848–52. doi: 10.1016/j.knee.2014.04.008. [DOI] [PubMed] [Google Scholar]
- 18.Chung AS, Spangehl MJ. Peripheral nerve blocks vs periarticular injections in total knee arthroplasty. J Arthroplasty. 2018;33:3383–8. doi: 10.1016/j.arth.2018.08.006. [DOI] [PubMed] [Google Scholar]


