Abstract
Objectives:
United States (US) youth consume an average of 10 teaspoons of added sugar from sugar-sweetened beverages (SSB) on any given day. Few population-based studies have examined the association between SSB consumption asthma in children and adolescents. This study aimed to examine the association between SSB consumption and asthma in the US pediatric population.
Design:
Analytical cross-sectional study.
Setting and Participants:
A total of 9,938 children aged 2-to-17 years old who participated in the 2011-2016 National Health and Nutrition Examination Surveys. SSB consumption was categorized into 3 groups based on the caloric intake from 24-hour food recall data as follows: 1) no consumption (0 kcal/day); 2) moderate consumption (1-499 kcal/day); and 3) heavy consumption (≥ 500 kcal/day). The primary outcome of interest was self-reported current asthma condition.
Results:
Asthma prevalence estimates were significantly higher in heavy (16.4%) and moderate (11.0%) SSB consumers versus non-consumers (7.5%) (p < 0.05 for both comparisons). The adjusted odds of asthma were twice that among children with heavy SSB consumption (aOR 2.01, 95% confidence interval [CI] 1.31-3.08) versus non-SSB consumers. The odds of asthma were higher among those who consumed fruit drinks (aOR 2.51, 95% CI 1.55-4.08), non-diet soft drinks (aOR 1.89, 95% CI 1.23-2.89) and sweet tea (aOR 1.87, 95% CI 1.13-3.09) compared to non-drinkers. The effect was independent of obesity status (p-interaction=0.439).
Conclusions:
Findings here suggest a dose-response relationship between SSB intake and asthma diagnosis, therefore controlling SSB consumption may potentially improve pulmonary health risk in the US pediatric population.
Keywords: Sugar-sweetened beverage, childhood asthma, NHANES, national prevalence, childhood nutrition
Introduction
The American Heart Association recommends children ages 2- to-18-years old should consume no more than one 8 ounces of sugar-sweetened beverages (SSB) per week,1 yet nearly two-thirds of children living in the United States (US) consume at least one SSB on any given day.2 Secular trend analysis has reported the prevalence of soft drink consumption is decreasing’ 3 while the consumption of other SSB, such as fruit drinks, sweet tea and nutrition/energy drinks is significantly increasing among US children. 4 Excess SSB consumption is associated with several chronic diseases including obesity, diabetes, dental carries, and cardiovascular diseases. 5-7
Previous study suggests SSB consumption is associated with childhood asthma8-12, one of the most common chronic childhood diseases.13 Park et al. analyzed data from the 2009 Youth Risk Behavior Survey and found US high schoolers who drank non-diet soda frequently were at a higher risk of being asthmatic compared with those who did not drink non-diet soda.8 Similarly, another cross-sectional study found a significant association between asthma and SSB intake, and fruit drinks consumption in particular among 11-year-old children from the Netherlands.9 Data from 2003-2006 National Health and Nutrition Examination Survey (NHANES) also suggests asthma risk among children ages 2-to-9 years old was significantly higher among SSB drinkers than non-drinkers.10 Those previous studies from the US and European countries only included sub-samples with a restricted age range, therefore the results may not be generalizable to US children out of those age ranges included. Moreover, to the best of our knowledge, no previous studies have examined the association between SSB and asthma among US children aged 2-to 17-years old.
A recent meta-analysis14 included 10 observational studies involving children up to 18 years old also indicated a positive association between SSB and asthma. However, the interpretation of findings was limited by the variation in the study population, unmeasured confounders, and lack of objective SSB intake measures.14
Hence, we conducted a large-scale, population-based analytical cross-sectional study to examine the association between SSB consumption (measured by the actual caloric intake from the 24-hour food recall) and asthma among US children and adolescents ages 2-to-17 years old. Based on previous studies, it was hypothesized that children who consumed SSB would have higher prevalence estimates of asthma versus those who do not drink SSB.
Methods
Study population
National Health and Nutrition Examination Surveys (NHANES) from the 2011-2012, 2013-2014, and 2015 to 2016 (Total n = 29,902) cycles were used for this analysis. More than half of the participants were children and adolescents (n=9,956). NHANES is a cross-sectional, publicly accessible and continuous survey conducted in a 2-year cycle by the National Center for Health Statistics (NCHS) of the Centers for Disease Control and Prevention (CDC) to monitor health and nutrition status of the US population.15 For each survey cycle, a complex 3-step weighting method is created to represent the US noninstitutional, civilian population.
The dietary data from the NHANES is obtained through 24-hour food recalls which asks detailed information about all food and beverage intake of respondents in the past 24 hours using USDA's dietary data collection instrument (http://www.ars.usda.gov/nea/bhnrc/fsrg). Children aged 12 years and above completed the survey on their own. Proxy respondents reported for children <5 years. Proxy-assisted interview are conducted among children 5-to-11 years old. In the 2011-2016 cycle, two nonconsecutive 24-hour recall questionnaires were administered on two separate days to the same respondent in order to establish the dietary pattern of each individual.16 The reliability of two non-consecutive 24-hour dietary recalls was assessed using dietary recall status variables provided by NHANES: DR1DRSTZ variable for the Day 1 interview and DR2DRSTZ variable for the Day 2 interview. Non-reliable responses that did not complete the first 4 steps of the 5-step data collection instrument or did not identify eating occasion were excluded in the final analysis (n = 18).
Hence, the final analytical sample included children aged 2- to 17- year old who completed two 24-hour recalls with reliable responses (n = 9,938). We included 3,888 (37.5%, 95% confidence interval [CI] 35.5-39.6%) participants who had no sugar-sweetened beverage (SSB) consumption (0 kcal/day) in two 24-hour recalls; and 4,968 (51.0%, 95% CI 48.9-52.8%) moderate drinkers (defined as 1-499 kcal/day in SSB consumption). Heavy SSB drinkers, defined as consumption of ≥ 500 kcal/day in SSB in any two 24-hour recalls were the primary independent variable of interest and comprised 1082 (11.5%, 95% CI 10.6-12.5%) children in this sample. The primary dependent variable was self-reported current asthma diagnosis (yes or no).
Measures
Sugar-sweetened beverage consumption.
In the 24-hour recalls, each consumed food or beverage item is assigned with a unique 8-digit food code based on the Food and Nutrient Database for Dietary Studies (FNDDS) of the US Department of Agriculture.17 The first 3 or 4 digits can be used to identify a specific food subgroup. For example, the first 3 digit of “924” represents carbonated soft drinks, and the last 5 digits indicate the specific types and brand of soda beverages. In this current study, SSB included fruit drinks, non-diet soft drinks, sweet tea, energy drinks and flavored water.
SSB consumption among US children were classified into 3 categories according to the daily calorie intake from SSB: 1) no SSB consumption: participants reported zero calorie intake from SSB in both 24-hour recalls; 2) moderate consumption: participants reported 1-499 kcal in SSB consumption over a 24-hour period; and 3) heavy consumption: participants consumed 500 kcal or more from SSB over 24 hours. The cut-off of 500 kcal was chosen based on a previous study4 which reported this caloric intake is equivalent to drinking 1.2 liter of regular soda over 24 hours. Using the 24-hour food recall questionnaire to establish an individual dietary pattern is widely accepted and validated in multiple studies.18-20
Asthma.
Childhood asthma diagnosis is reported by the child or parent based on children’s age and ability to answer the following two question: 1) “Has a doctor or other health professional ever told {you/SP} that {you have/s/he/SP has} asthma?” 2) “{Do you/Does SP} still have asthma?” 1,090 (10.5%, 95% CI 9.8-11.4%) children in this sample answered “yes” to both questions and were subsequently categorized as having a current asthma condition, which was the primary dependent variable of interest. Current asthma was chosen to be the primary dependent variable because CDC utilizes current asthma when reporting prevalence estimates.21
Covariates
Based on previous studies,8-12 selected covariates included the following descriptives; child age, sex, race/ethnicity (Non-Hispanic White, Non-Hispanic Black, Hispanic, and Other) and ratio of family income to poverty. Body mass index (BMI) percentile was also included as a covariate because overweight/obesity is a well-established risk factor for the childhood asthma22 and SSB consumption is associated with weight gain.5
Statistical analysis
Demographic characteristics of participants were generated by the three SSB consumption categories (heavy, moderate and no consumption), respectively. One-way analysis of variance (ANOVA) and chi-square analysis was used to compare SSB consumption percentage for continuous dependent variables and categorical dependent variables, respectively. Univariable logistic regression models generated crude odds ratios (ORs) to examine SSB consumption by current asthma (Y/N). The first multivariable logistic regression model adjusted for age, sex, race, and family income and generated adjusted odds ratios (aORs) of asthma history by SSB consumption. A second multivariable logistic regression model was created with the adjustment of above covariates and BMI percentile. Additional sub-group analyses were conducted to determine the odds of asthma diagnosis by SSB product types, including fruit drinks, soft drinks, sweet tea, and other SSB (nutrition/energy drinks and flavored water). Interaction between weight status (obese vs. non-obese) and SSB to predict asthma diagnosis was also examined in the multivariate logistic regression model using the following interaction term: weight status*SSB consumption.
All analyses in this study applied sampling methods, including the appropriate sample weight, stratum variable, and cluster variable, provided by the NHANES and were performed in SAS v 9.4 (SAS Institute Inc, Cary, North Carolina). A two-sided p-value of 0.05 was used to decide the statistical significance. Data were analyzed from November 15, 2019, to September 1, 2020.
Results
During 2011-2016, among US children aged 2-to-17 years old, heavy SSB drinkers were more likely to be male (60.2%), non-Hispanic white (53.0%), in 1-5th grade levels (30.4%), and have family income between 0-99% federal poverty level (FPL) (29.2%). Conversely, the majority of non-SSB drinkers in the sample were female (51.0%), non-Hispanic white (53.4%), and from high school (35.5%). The weighted demographic information of moderate SSB drinkers is also demonstrated in Table 1. The mean BMI percentile was significantly higher among heavy SSB drinkers (75.3% vs 70.7% among moderate drinkers and 69.7% among non-drinkers, p = 0.029). During two-day food recall interviews, the average total amount of sugar consumed among heavy drinkers (mean = 246.9, standard error [SE] = 11.4g) was significantly higher than the average total sugar amount ingested by non-drinkers (mean = 150.9g, SE = 5.3g) and moderate drinkers (mean = 184.8g, SE = 4.4g). Mean caloric intake attributed to SSB was 783.9 (SE=31.3) kcal among the heavy consumption group, roughly equivalent to two 400kcal/liters of regular soda.4 (Table 1)
Table 1.
Demographic characteristics of children ages 2-to-17 years old by sugar-sweetened beverage consumption, NHANES 2011-2016 (n=9,938).
| No sugar- sweetened beverage consumptiona (n = 3888) |
Moderate sugar- sweetened beverage consumptionb (n = 4968) |
Heavy sugar- sweetened beverage consumptionc (n = 1082) |
p-value | |
|---|---|---|---|---|
| Age, weighted mean (SE) | 8.1 (0.2) | 9.8 (0.1) | 11.5 (0.2) | <0.001 |
| 2-6 years, N (weighted %) | 1742 (41.2) | 1612 (26.7) | 179 (12.4) | |
| 7-11 years, N (weighted %) | 1224 (29.4) | 1707 (31.6) | 374 (29.8) | |
| 12-17 years, N (weighted %) | 922 (29.4) | 1649 (41.7) | 529 (57.8) | |
| Sex, N (weighted %) | <0.001 | |||
| Male | 1947 (49.0) | 2487 (50.0) | 628 (60.2) | |
| Female | 1941 (51.0) | 2481 (50.0) | 454 (39.8) | |
| Race/Ethnicity, N (weighted %) | <0.001 | |||
| Non-Hispanic White | 1013 (53.4) | 1210 (51.8) | 286 (53.0) | |
| Non-Hispanic Black | 871 (12.3) | 1357 (14.8) | 358 (18.3) | |
| Hispanic | 1126 (21.2) | 1749 (25.7) | 326 (21.5) | |
| Other | 878 (13.1) | 652 (7.7) | 112 (7.1) | |
| Education level, N (weighted %) | <0.001 | |||
| Kindergarten | 313 (7.3) | 421 (7.2) | 64 (5.5) | |
| 1-5th grade | 1230 (29.7) | 1739 (33.0) | 378 (30.4) | |
| 6-8th grade | 500 (15.9) | 869 (21.4) | 276 (30.0) | |
| 9-11th grade | 362 (11.6) | 660 (17.2) | 224 (24.6) | |
| High school graduate | 1483 (35.5) | 1279 (21.2) | 140 (9.5) | |
| Family income, N (weighted %) | 0.020 | |||
| ≥400% FPL | 695 (25.0) | 652 (20.7) | 149 (20.2) | |
| 200-399% FPL | 779 (23.6) | 1056 (27.6) | 208 (25.2) | |
| 100-199%FPL | 865 (21.3) | 1324 (23.5) | 296 (25.4) | |
| 0-99% FPL | 1549 (30.1) | 1936 (28.2) | 429 (29.2) | |
| BMI percentile, weighted mean (SE) | 69.7 (1.2) | 70.7 (0.8) | 75.3 (1.5) | 0.029 |
| Sugar amount (g), weighted mean (SE) d | 150.9 (5.3) | 184.8 (4.4) | 246.9 (11.4) | <0.001 |
| Calories intake from SSB (kcal), weighted mean (SE) e | 0 (0) | 135.3 (3.9) | 783.9 (31.3) | <0.001 |
Note.
Weighted percentage and means. One-way ANOVA test for continuous variables. Chi-square test for categorical variables.
BMI, body mass index; FPL, federal poverty level.
No sugar-sweetened beverage consumption: participants who did not report any sugar-sweetened beverages consumption (0 kcal/day) in two 24-hour food recalls.
Moderate sugar-sweetened beverage consumption: participants who consumed 1- 499 kcal/day sugar-sweetened beverages.
Heavy sugar-sweetened beverage consumption: participants who consumed ≥ 500 kcal/day sugar-sweetened beverages.
Total amount of sugar consumed per day.
Average calories consumed per day from sugar-sweetened beverage.
Self-reported current asthma prevalence estimates were significantly higher in heavy drinkers compared with non-drinkers. Specifically, 16.4% (95% CI 12.8-20.1%) of heavy drinkers and 11.0% (95% CI 9.4-12.6%) of moderate drinkers self-reported a current asthma condition, respectively, while 7.5% (95% CI 5.8-9.2%) of non-drinkers reported a current asthma (p < 0.001 for heavy vs. non-drinkers, and p = 0.006 for moderate vs. non-drinkers, respectively). (Figure 1) Age-group specific findings showed asthma was most prevalent among heavy SSB consumers ages 12-to-17 years old. Specifically, approximately 1 in every 5 teenagers who consumed ≥500 kcal per day in SSB reported having asthma (19.7%, 95% CI 14.4-25.1%), followed by children aged 2-to 6 years old (17.7%, 95% CI 7.2-28.2%) and 7-to-11 years old (10.2%, 95% CI 6.2-14.2%). (Data not shown)
Figure 1.
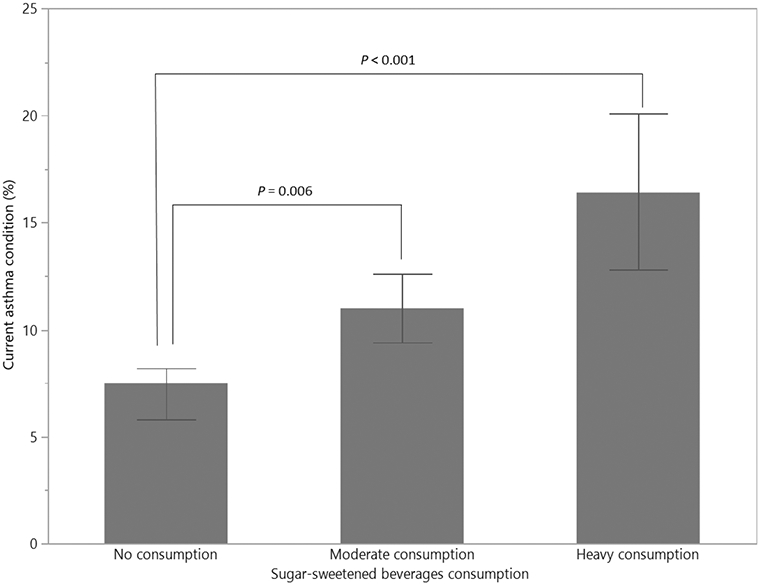
Weighted current asthma prevalence by sugar-sweetened beverage consumption, NHANES 2011-2016.
Note.
No consumption: participants who did not report any sugar-sweetened beverage consumption (0 kcal/day) in two 24-hour recalls; Moderate consumption: participants who consumed 1- 499 kcal/day in sugar-sweetened beverages; Heavy consumption: participants who consumed ≥ 500 kcal/day in sugar-sweetened beverages.
Table 2 illustrates the odds of current asthma by SSB consumption categories in 3 logistic regression models. First, the crude model showed that compared to children who did not consume SSB, any SSB consumption regardless of the amount (in other words, moderate and heavy SSB consumption combined) was significantly associated with current asthma (OR 1.70, 95% CI 1.25-2.32), and odds were highest among heavy drinkers (OR 2.43, 95% 1.64-3.60). The second model adjusted for age, sex, race/ethnicity, and family income found the odds of having current asthma continued to be highest among heavy drinkers (adjusted OR [aOR] 2.02, 95% CI 1.33-3.05). In a final, fully adjusted model that also included BMI percentile as a covariate, the odds of having current asthma were significantly higher among heavy drinkers (aOR 2.01, 95% CI 1.31-3.08) and moderate drinkers (aOR 1.40, 95% CI 1.01-1.95) versus non-drinkers. Notably, there was no BMI interaction effect on the association between asthma and SSB consumption (p-interaction = 0.439).
Table 2.
Crude and adjusted odds of current asthma by sugar-sweetened beverage drinker consumption level.
| Current asthma diagnosis | |||
|---|---|---|---|
| Odds ratio | 95% CI | p-value | |
| Model 1 a | |||
| Moderate consumption (1-499 kcal/day) | 1.53 | 1.12-2.09 | 0.008 |
| Heavy consumption (≥ 500kcal/day) | 2.43 | 1.64-3.60 | <0.001 |
| Combined Moderate and Heavy Consumption (≥ 1 kcal/day) | 1.70 | 1.25-2.32 | 0.001 |
| Model 2 b | |||
| Moderate consumption (1-499 kcal/day) | 1.41 | 1.01-1.96 | 0.044 |
| Heavy consumption (≥ 500kcal/day) | 2.02 | 1.33-3.05 | 0.001 |
| Combined Moderate and Heavy Consumption (≥ 1 kcal/day) | 1.52 | 1.09-2.11 | 0.014 |
| Model 3 c | |||
| Moderate consumption (1-499 kcal/day) | 1.40 | 1.01-1.95 | 0.047 |
| Heavy consumption (≥ 500kcal/day) | 2.01 | 1.31-3.08 | 0.002 |
| Combined Moderate and Heavy Consumption (≥ 1 kcal/day) | 1.51 | 1.08-2.11 | 0.017 |
Note.
No sugar-sweetened beverage consumption is the reference group.
Model 1: crude model.
Model 2: Adjusted for age, sex, race/ethnicity and family income.
Model 3: Adjusted for age, sex, race/ethnicity, family income and body mass index percentile.
Figure 2 shows the adjusted odds of having an asthma diagnosis by SSB types. Among 9938 participants, nearly one-third (30.3%) reported consuming non-diet soft drinks, while 16.6% reported consuming fruit drinks and 11.8% sweet tea. A small proportion (3.8%) of children reported consuming other types of SSB such as nutrition/energy drinks and flavored water. Fruit drink consumption was associated with the highest odds of reporting a current asthma condition (aOR 2.51, 95% CI 1.55-4.08). Subsequently, the consumption of non-diet soft drinks (aOR 1.89, 95% CI 1.23-2.89) and sweet tea (aOR 1.87, 95% CI 1.13-3.09) was associated with approximately 2 times higher odds of current asthma condition. Other SSBs were not significantly associated with an increased odds of a self-reported asthma condition.
Figure 2.
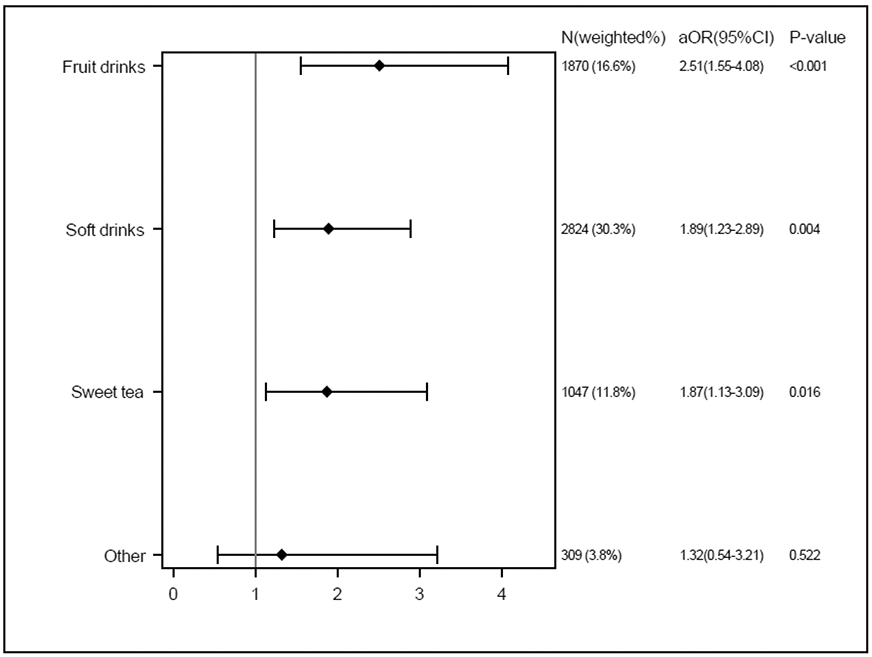
Adjusted odds of current asthma by sugar-sweetened beverage product type.
Note.
No sugar-sweetened beverage consumption is the reference group (n=3888, 37.5%).
Multivariable logistic regression adjusted for age, sex, race/ethnicity, family income, body mass index percentile, and SSB consumption status (non-drinker vs. heavy drinker and non-drinker vs. moderate drinker).
Discussion
We report here the national prevalence of self-reported asthma diagnosis among children aged 2-to-17-years old by SSB consumption level based on caloric intake using the 2011-2016 NHANES datasets. Overall, results support our hypothesis that the weighted prevalence estimates of current asthma among US children were about nine percentage points higher in heavy SSB drinkers (16.4%) versus non-drinkers (7.5%). After model adjustment for key demographic variables and BMI percentile, the odds of current asthma were about 2 times higher in children who consumed ≥ 500 kcal/day in SSB over 24 hours compared to those who reported no SSB consumption. Moreover, after controlling for covariates and the amount of consumption, fruit drinks, non-diet soft drinks and sweet tea were associated with higher odds of current asthma condition compared to no consumption.
Similar to the present study, several previous studies8-12,14 suggest the intake of sugary drinks is associated with an asthma diagnosis in pediatric populations worldwide. For example, a recent meta-analysis14 included 468,836 participants with >50,000 asthma cases from 19 eligible publications suggested soft drink consumption was significantly associated with childhood asthma (OR = 1.14; 95% CI, 1.06 - 1.21) compared with non-soft drink consumers. Our study found the association between asthma and SSB consumption was independent of obesity status. This finding was consistent with the results of a prior cross-sectional study8, which also found that participants’ weight status did not mediate the association between SSB consumption and asthma diagnosis among US adolescents.
Furthermore, Park et al. 8 suggested a dose-response relationship between regular soda intake and asthma prevalence. Specifically, the more frequent intake of regular soda, the higher odds of asthma diagnosis (≥ 3 times/day vs. none: aOR 1.64, 95% CI 1.25- 2.16; 1 time/day vs. none: aOR 1.28, 95% CI 0.99 – 1.66). The present study also found the odds of being asthmatic increased as SSB-attributed caloric intake increased. Compared with non-drinkers, heavy SSB drinkers had 2 times higher odds of asthma (aOR 2.01, 95% CI 1.31-3.08), while moderate drinkers had 1.4 times higher odds (aOR 1.40, 95% 1.01-1.95).
This analysis found that the consumption of fruit drink, non-diet soft drinks, and sweet tea was associated with current asthma, whilst such an association did not emerge among children who had other SSB. Given a relatively small sample size of other SSB consumers (n=309), in the future, it should be confirmed by a larger study with more statistical power.
Two possible biochemical mechanisms explaining the association between asthma and sugary drinks have been previously proposed. First, most SSB use sodium benzoate or potassium benzoate as a preservative, which has been shown to cause wheezing and exacerbate asthma symptoms,8,23,24 However, a recent longitudinal birth cohort study that enrolled 60,466 participants from Denmark found asthma was only positively associated with artificially sweetened soft drinks (ASB) consumption, and not with SSB consumption.12 Hence, the association between SSB and asthma may be due to other components other than preservatives because both ASB and SSB contain preservatives. Second, sugar-sweetened fruit drinks in particular contain large amounts of fructose corn syrup that might promote inflammation, cause chronic airway mucus hypersecretion, and eventually trigger asthmatic episodes.10,25,26 A more recent longitudinal research suggested the excess consumption of SSB was associated with 2 ~ 3.5 times higher asthma incidence among the US toddlers.27
Some interesting, and perhaps counterintuitive characteristics of heavy SSB consumers should be noted. According to the CDC, SSB intake is higher among non-Hispanic Black adolescents from low-income backgrounds versus other ethnic groups.2 Yet here the analysis showed that the weighted proportion of non-Hispanic White SSB heavy consumers (53.0%), was more than twice that of non-Hispanic black (18.3%) and Hispanic (21.5%) regular consumers. Also, those of elementary age were most likely to be heavy SSB consumers (30.4%) versus middle schoolers (30.0%), high schoolers (24.6%) and high school graduates (9.5%). Most importantly, the BMI percentile significantly along with the amount of consuming SSB suggesting that SSB consumption is one of the most important dietary factors driving the current childhood obesity epidemic.28 Therefore, public health initiatives targeting non-Hispanic whites, children/adolescents of all weight categories, and those who are preschool age might help control excess SSB consumption in the US pediatric population.
This study had some limitations. Because the asthma outcome variable was self-reported, differential misclassification of asthma diagnosis may occur and bias the effect estimates towards or away from the null, potentially causing either a type I or type II error. While analysis comprehensively controlled for key sociodemographic factors, BMI percentile and the amount consumed, there may be other potential confounders that have not been rigorously controlled that could impact the findings reported here. It also should be noted that the 24-hour food recalls only provide a snapshot of an individual’s diet. Although we used the actual calories intake to measure the SSB consumption, inter-individual variation may exist, resulting in residual confounding. Finally, a temporal or causal relationship between SSB intake and asthma cannot be established because of the cross-sectional nature of our study.
Conclusions
Analysis here suggests a dose-response relationship between SSB intake and asthma diagnosis. Specifically, the adjusted odds of current asthma were about 2 times higher in children who consumed > 500 kcal/day in SSB, and 40% higher in children who consumed 1-499 kcal/day in SSB over 24 hours compared to those who reported no SSB consumption. Children who consumed fruit drinks reported the highest odds of asthma diagnosis. Longitudinal studies that can establish a temporal relationship between asthma diagnosis and SSB consumption should be conducted that can in turn inform pediatric clinical care, particularly among those caring for children and adolescents with asthma.
Acknowledgments:
We thank the participants who generously shared their time for answering the National Health and Nutrition Examination Survey (NHANES) in 2011-2016.
Footnotes
Transparency Declaration: The lead author LX and senior author SM affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Ethics: 2011-2016 NHANES is approved by NCHS Research Ethics Review Board, Protocol #2011-17, can be accessed at https://www.cdc.gov/nchs/nhanes/irba98.htm.
Conflict of Interests: All authors declare no competing interests.
Dissemination Declaration: We plan to disseminate the results to study participants and the public.
Data Sharing Statement: The data that support the findings of this study are available in National Center for Health Statistics at https://www.cdc.gov/nchs/nhanes/index.htm. These data were derived from the following resources available in the public domain: https://wwwn.cdc.gov/nchs/nhanes/Default.aspx.
References
- 1.Miller PE, McKinnon RA, Krebs-Smith SM, et al. Sugar-sweetened beverage consumption in the U.S.:Novel assessment methodology. Am J Prev Med. 2013;45(4):416–421. [DOI] [PubMed] [Google Scholar]
- 2.CDC. Get the Facts: Sugar-Sweetened Beverages and Consumption. 2017. https://www.cdc.gov/nutrition/data-statistics/sugar-sweetened-beverages-intake.html. Accessed February 14, 2020. [Google Scholar]
- 3.Miller G, Merlo C, Demissie Z, Sliwa S, Park S. Trends in Beverage Consumption Among High School Students — United States, 2007–2015. MMWR Morb Mortal Wkly Rep 2017;66:112–116. doi: 10.15585/mmwr.mm6604a5External [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Han and Powell. Consumption Patterns of Sugar-Sweetened Beverages in the United States J Acad Nutr Diet. 2013;113:43–53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Malik V, Popkin B, Bray G, Desprs J-P, Hu F. Sugar-sweetened beverages, obesity, type 2 diabetes mellitus, and cardiovascular disease risk. Circulation. 2010;121(11):1356–1364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bernabe E, Vehkalahti MM, Sheiham A, Aromaa A, Suominen AL. Sugar-sweetened beverages and dental caries in adults: a 4-year prospective study. J Dent. 2014;42(8):952–958. [DOI] [PubMed] [Google Scholar]
- 7.Eny KM, Jeyakumar N, Dai DWH, et al. Sugar-containing beverage consumption and cardiometabolic risk in preschool children. Prev Med Rep. 2020;17:101054. Published 2020. Jan 14. doi: 10.1016/j.pmedr.2020.101054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Park S, Blanck HM, Sherry B, Jones SE, Pan L. Regular-soda intake independent of weight status is associated with asthma among US high school students. J Acad Nutr Diet. 2013;113(1):106–111. doi: 10.1016/j.jand.2012.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Berentzen NE, van Stokkom VL, Gehring U, et al. Associations of sugar-containing beverages with asthma prevalence in 11-year-old children: the PIAMA birth cohort. Eur J Clin Nutr. 2015;69(3):303–308. doi: 10.1038/ejcn.2014.153. [DOI] [PubMed] [Google Scholar]
- 10.DeChristopher LR, Uribarri J, Tucker KL. Intakes of apple juice, fruit drinks and soda are associated with prevalent asthma in US children aged 2-9 years. Public Health Nutr. 2016;19(1):123–130. doi: 10.1017/S1368980015000865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wickens K, Barry D, Friezema A, Rhodius R, Bone N, Purdie G et al. Fast foods — are they a risk factor for asthma? Allergy 2005;60: 1537–1541 [DOI] [PubMed] [Google Scholar]
- 12.Maslova E, Strøm M, Olsen SF, Halldorsson TI. Consumption of artificially-sweetened soft drinks in pregnancy and risk of child asthma and allergic rhinitis. PLoS One. 2013;8(2):e57261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.CDC (Centers for Disease Control and Prevention). Most Recent Asthma Data. 2019. https://www.cdc.gov/asthma/most_recent_data.htm. Accessed February 25, 2019.
- 14.Al-Zalabani AH, Noor Elahi I, Katib A, et al. Association between soft drinks consumption and asthma: a systematic review and meta-analysis. BMJ Open. 2019;9(10):e029046. Published 2019 Oct 14. doi: 10.1136/bmjopen-2019-029046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.CDC. National Health and Nutrition Examination Survey. 2018. https://wwwn.cdc.gov/nchs/nhanes/tutorials/module3.aspx. Accessed February 14, 2020. [Google Scholar]
- 16.CDC. Task 2: Key Concepts About NHANES Dietary Data Collection. 2020. https://www.cdc.gov/nchs/tutorials/dietary/surveyorientation/dietarydataoverview/info2.htm. Accessed February 14, 2020. [Google Scholar]
- 17.U.S. Department of Agriculture, Agricultural Research Service. 2020. USDA Food and Nutrient Database for Dietary Studies 2011-2016. Food Surveys Research Group Home Page, http://www.ars.usda.gov/nea/bhnrc/fsrg [Google Scholar]
- 18.Mertens E, Kuijsten A, Geleijnse JM, Boshuizen HC, Feskens EJM, Van't Veer P. FFQ versus repeated 24-h recalls for estimating diet-related environmental impact. Nutr J. 2019;18(1):2. Published 2019 Jan 8. doi: 10.1186/s12937-018-0425-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Frankenfeld CL, Poudrier JK, Waters NM, Gillevet PM, Xu Y. Dietary intake measured from a self-administered, online 24-hour recall system compared with 4-day diet records in an adult US population. J Acad Nutr Diet. 2012;112(10):1642–1647. doi: 10.1016/j.jand.2012.06.003 [DOI] [PubMed] [Google Scholar]
- 20.Zheng M, Campbell KJ, Scanlan E, McNaughton SA. Development and evaluation of a food frequency questionnaire for use among young children. PLoS One. 2020;15(3):e0230669. Published 2020 Mar 25. doi: 10.1371/journal.pone.0230669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.CDC. Asthma Surveillance data. https://www.cdc.gov/asthma/national-surveillance-data/default.htm. Accessed July 27, 2020. [Google Scholar]
- 22.Peters U, Dixon AE, Forno E. Obesity and asthma. J Allergy Clin Immunol. 2018;141(4):1169–1179. doi: 10.1016/j.jaci.2018.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Freedman BJ. Sulphur dioxide in foods and beverages: Its use as a preservative and its effect on asthma. Br J Dis Chest. 1980;74(2):128–134. [DOI] [PubMed] [Google Scholar]
- 24.Steinman HA, Weinberg EG. The effects of soft-drink preservatives on asthmatic children. S Afr Med J 1986;70: 404–406. [PubMed] [Google Scholar]
- 25.DeChristopher LR, Uribarri J, Tucker KL. The link between soda intake and asthma: science points to the high-fructose corn syrup, not the preservatives: a commentary. Nutr Diabetes. 2016;6(11):e234. Published 2016 Nov 28. doi: 10.1038/nutd.2016.46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Aeberli I, Gerber PA, Hochuli M, Kohler S, Haile SR, Gouni-Berthold I et al. Low to moderate sugar-sweetened beverage consumption impairs glucose and lipid metabolism and promotes inflammation in healthy young men: a randomized controlled trial. Am J Clin Nutr 2011;94: 479–485. [DOI] [PubMed] [Google Scholar]
- 27.DeChristopher LR, Tucker KL. Excess free fructose, apple juice, high fructose corn syrup and childhood asthma risk - the National Children's Study. Nutr J. 2020;19(1):60. Published 2020 Jun 23. doi: 10.1186/s12937-020-00578-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Keller A, Bucher Della Torre S. Sugar-Sweetened Beverages and Obesity among Children and Adolescents: A Review of Systematic Literature Reviews. Child Obes. 2015;11(4):338–346. doi: 10.1089/chi.2014.0117 [DOI] [PMC free article] [PubMed] [Google Scholar]


