Abstract
Rationale
The effect of COVID-19 lockdowns on mental health is a major concern worldwide. Measuring the impacts, however, is difficult because of a lack of data that tracks and compares outcomes and potential protective social factors before and during lockdowns.
Objective
We aim to quantify the impact of a second lockdown in 2020 in the Australian city of Melbourne on levels of depression, anxiety, and loneliness, and analyse whether social relations in the neighbourhood may buffer against the worst effects of lockdown.
Methods
We draw on quasi-experimental data from a nationally-representative longitudinal survey conducted in Australia. We use a difference-in-difference approach with a number of control variables to estimate changes in mental health among respondents in Melbourne following the imposition of the lockdown. A measure of perceived neighbourhood social relations is included as an explanatory variable to analyse potential protective effects.
Results
Lockdown is estimated to have increased depressive symptoms by approximately 23% and feelings of loneliness by 4%. No effect on anxiety was detected. Levels of neighbourhood social relations were strongly negatively associated with mental health symptoms. A significant interaction between lockdown and neighbourhood social relations suggests that lockdown increased depressive symptoms by 21% for people with average perceived neighbourhood relations, compared with a 9.7% increase for people whose perceived relations is one standard deviation greater than average.
Conclusion
The results add to evidence of the harsh impacts of the COVID-19 pandemic and associated lockdowns on mental health. Importantly, neighbourhood social relations and social cohesion more broadly may be an important source of social support in response to lockdowns. These findings provide important insights for researchers and policy-makers in how to understand and respond to the mental health impacts of COVID-19.
Keywords: COVID-19, Mental health, Lockdown, Neighbourhood social relations, Social cohesion, Natural experiment
1. Introduction
In response to the COVID-19 pandemic, governments have imposed national, state and city-wide lockdowns, severely restricting people's movements and social contact. While protecting the lives and physical health of the population, considerable concern centres on the downstream effects of lockdown restrictions on mental health and well-being (WHO, 2021). Indeed, emerging evidence suggests that infections and lockdowns in the early stages of the pandemic have had a detrimental effect on mental health (Prati and Mancini, 2021). Yet, our understanding of the longer-term effects of lockdowns on mental health is still unfolding and will benefit from increasingly sophisticated efforts to measure their impacts as well as those of protective factors. In view of existing research, social cohesion is likely to be one factor that can play a key role in protecting mental health generally, and in response to the pandemic (Ehsan and De Silva, 2015; Henderson et al., 2016; Chuang et al., 2013). In particular, positive social relations within a neighbourhood may be of critical importance during times of crisis as they facilitate common goals, support, belonging and a united response, particularly when other individuals and social groups are unavailable due to restricted movement.
The aim of this research is twofold. First, we seek to quantify the effect of an extended lockdown on individuals' mental health. Second, we investigate whether positive social relations in one's neighbourhood protects individual mental health during lockdown. The first question is examined using a natural experiment based on a three-wave nation-wide survey conducted in Australia. The survey encompasses the time period before and during a second wave of infections and lockdown in the city of Melbourne (July–December 2020). This timing allows us to examine mental health outcomes before and during lockdown for survey samples who experienced a second, and very strict, lockdown in Melbourne and make comparisons to those who did not experience a second lockdown in Sydney (a comparable Australian city). In so doing, we are uniquely placed to examine how variations in lockdown impact mental health, and how changes in neighbourhood social relations may protect individuals' from experiencing loneliness, depression and anxiety.
1.1. Lockdowns and their burden on mental health
There is great interest and concern in understanding the burden of the COVID-19 pandemic on mental health. For example, a search in APA PsycInfo of mental health (example of keywords: adaptation, anxiety, depression, quality of life) and COVID-19 (example of keywords: COVID-19, SARS-CoV-2, quarantine, lock-down) yielded over 3000 articles. Prati and Mancini (2021), in their meta-analysis, identified 25 longitudinal or quasi-experimental studies conducted in Asia, Europe, North America, and New Zealand during the first waves of the pandemic, where average time spent in lockdown was 22 days. They found a small but significant negative effect of lockdown on aspects of mental health such as depression and anxiety (g = 0.17, SE = 0.05, p = .001). The reviewed studies included longitudinal and cross-sectional designs. The longitudinal studies typically measured the mental health of participants before and during the first wave of COVID-19 (e.g., Niedzwiedz et al., 2021; Pierce et al., 2020), while several of the cross-sectional studies compared the mental health of people living under lockdown/quarantine restrictions or in regions heavily affected by the pandemic to those less or not affected by the pandemic or restrictions (e.g., Guo et al., 2020; Lei et al., 2020; Tull et al., 2020). To date, only one non-peer reviewed study (Biddle et al., 2020) has been identified that compares individual-level changes in mental health before and during the pandemic. Evidence therefore is still emerging that quantifies the precise impacts of lockdown on individual mental health.
Importantly, much of the existing research was conducted early during the global pandemic, when most communities were experiencing or had experienced a single lockdown. Unfortunately, the progression of COVID-19 infections has led many communities to enforce lockdowns several additional times, sometimes for a longer and more sustained period. One example is the Australian city of Melbourne, where a strict second lockdown was enforced from July to October 2020 for a total of 111 days. While this virtually eliminated community transmission in the state and in the country for many months, the burden of a sustained second lockdown on mental health, which was echoed (to different extents) by many communities worldwide (e.g., Canadian provinces of Quebec and Ontario, the Netherlands, several German provinces, Buenos Aires, Brazil), is not well understood. The first goal of the current study therefore is to understand variations in mental health (anxiety, depression, and loneliness) as a function of a long and sustained second lockdown. We hypothesise that experiencing a second lockdown will be associated with worse mental health in terms of greater symptoms and feelings of depression, anxiety and loneliness (H1).
1.2. Collective protective factors: social cohesion and the quality of social relations in the neighbourhood
Research on protective factors emerging during the COVID-19 pandemic has, to date, focused on individual protective factors; that is, characteristics and/or resources an individual possesses that may ward against ill health. One individual factor that has been often studied is social support, or the support available to individuals during COVID-19 lockdowns because of their idiosyncratic social ties to other individuals and groups (Budimir et al., 2021; Nitschke et al., 2021; Ye et al., 2020). Social support allows individuals to access physical and psychological resources when they are needed, in turn mitigating the effect of negative events on individuals' mental health (Turner and Brown, 2010). Although theories of social support acknowledge that support emerges from a broader context, most research usually centres on one's immediate interpersonal social relations (e.g., friends, family, partners, and colleagues).
While the importance of individual protective factors during lockdown is clear, collective protective factors have the potential to impact and protect a wider population. One such collective factor is social cohesion, an “umbrella term” (Delhey and Dragolov, 2016) or “quasi-concept” (Bernard, 2009) that captures the sense of connectedness to a group and its members (Chan et al., 2006). In this research, we focus on the social cohesion dimension that has been most widely studied in the context of health research: the quality of social relations within the group or the extent to which people see others in the community getting along. This quality is reflected and assessed in terms of trust, safety and altruism within the group (Alcalá et al., 2016) and is considered a component of the broader and multidimensional concept of social cohesion, which also includes aspects of societal-level attitudes and behaviours in social and political domains (Bernard, 2009; Chan et al., 2006; Dragolov et al., 2016). Positive social relations, and social cohesion, are important for health outcomes because they offer the collective resources necessary to manage health challenges (Fiori et al., 2016; Thoits, 2010), while also facilitating self-efficacy (Samuel et al., 2014). Being in a group that has positive social relations may also indicate a shared social identity (Haslam et al., 2003) and associated qualities such as belonging, shared purpose and ingroup support, which also support mental health (Cruwys et al., 2014; Jetten et al., 2017).
Supportive social relations exist for different types of groups, including neighbourhoods. Neighbourhoods are a well-studied group, deemed particularly important in daily social interactions and support networks due to their spatial proximity (Unger and Wandersman, 1985). Existing theory and research has theorised and demonstrated that social aspects of the neighbourhood, variously defined as neighbourhood social cohesion, social capital, belonging, collective efficacy, disorder and safety have a beneficial and protective effect on mental health and general wellbeing (e.g., Aminzadeh et al., 2013; Elliot et al. 2014; Fone et al., 2014; Ivory et al., 2011; Kim, 2008; Ruiz et al., 2019). We therefore hypothesise that perceptions of positive social relations in one's neighbourhood will be associated with lower levels of depression, anxiety and loneliness (H2).
Social environments may be of particular importance during collective crises such as global pandemics. Research finds strong but variable positive correlations between community cohesion and resilience to natural disasters (Townshend et al., 2015; Ludin et al., 2019), while cohesion can be beneficial for both disaster preparedness and mental health (Welton-Mitchell et al., 2018). Such evidence suggests that pre-existing levels of social cohesion support communities to manage disasters and mitigate against adverse individual and collective outcomes (e.g., Lalot et al., 2021). While the role of neighbourhoods during the COVID-19 pandemic is still to emerge, their importance is potentially enhanced where wider social networks are impaired by restrictions on people's movements.
The relationship between changes in social relations emerging from crises and mental health, on the other hand, is likely to be more complex. The theory of ‘psychosocial gains from adversity’ posits that crises and adverse events can be beneficial to mental health (Mancini, 2019). A key mechanism through which this improvement occurs is through a strengthening in the social environment. Crises and disasters have been shown to strengthen social bonds, leading to emergent – albeit often temporary – social cohesion (Calo-Blanco et al., 2017; Drury et al., 2016; Fan et al., 2020; Ntontis et al., 2020). Emergent social cohesion then can act as a form of psychosocial support to individuals, including in the context of COVID-19 (Bowe et al., 2021). Nonetheless, where the direct adverse effect of lockdown restrictions are stronger than the protective effects of the social environment, worsening mental health may be observed during lockdown at the same time as perceived social relations improve.
Psychological stress may itself strengthen cohesion, potentially confounding the positive effects of emergent neighbourhood relations on mental health. According to ‘tend and befriend’ theory, stress stimulates a biological response that leads people to strengthen their affiliation with others (Taylor, 2011). In the context of the COVID-19 pandemic, the theory suggests that an adverse mental health response to lockdown may strengthen affiliative links in the neighbourhood and improve perceived relations.
Theory and evidence therefore lead us to hypothesise that the protective effects of established levels of neighbourhood social relations will be enhanced under lockdown restrictions (H3). We do not, however, make the same claim with respect to changes in, or emergent, neighbourhood relations arising from lockdown, given that a positive effect of emergent relations is potentially confounded by endogenous processes including reverse causation.
2. Methods
2.1. Participants and procedure
The data for this study come from a longitudinal three-wave survey of Australian adults in May–October 2020. The sample consisted of 3028 people at Wave 1, of whom 2034 participated at Wave 2 (attrition rate of 32.9%) and 1723 at Wave 3 (attrition rate of 43.1%). Recruitment was conducted by Qualtrics Services, who contacted participants via email or in their online research participation portal, using several double-opt-in market-research panels and blending them to reach individuals across the country, while minimising panel bias. The sample was expected to be 90% representative of Australian residents in terms of age, gender, state and income. Comparisons between the survey sample and the total adult population suggest similar profiles. Of the survey sample, the mean age is 47.8 years (47.7 years for the total adult population [ABS, 2021a]), 52.5% were female (51.0% for the total population [ABS, 2021a]), 72.8% were born in Australia (70.2% for the total population [ABS, 2021b]), 59.3% live in the two most populous states, New South Wales and Victoria (58.1% for the total population [ABS, 2021a]) and 48.7% had personal income of less than $650 per week in Australian dollars (47.1% for the total population [ABS, 2017]).
2.2. Timing of the study and the progression of COVID-19 in Australia
The timing of the survey coincided with a second wave of COVID-19 restrictions and the imposition of a strict lockdown in the Australian city of Melbourne (located in the state of Victoria). During the first wave of COVID-19 in Australia in March–April 2020, the entire population was under lockdown, required to stay at home except for medical reasons, essential shopping or work or a limited period of outdoor exercise (Campbell and Vines, 2021). Infections were successfully contained, with new infections declining from an average of 359 per day in the last week of March 2020 to 21 infections in the first week of May 2020 (John Hopkins University, 2021). By Wave 1 of our study (9–27 May 2020), Australia was emerging from lockdown. Stay-at-home orders were lifted across state jurisdictions by the start of May and further easing to reopen business and community spaces began in mid-May (Storen and Corrigan, 2020). COVID-19 infections were substantially suppressed, with a national average of 12 new infections per day across the Wave 1 survey period (John Hopkins University, 2021).
Wave 2 of the survey (16 June–16 July 2020) was conducted as COVID-19 infections were increasing in Melbourne. The average number of new cases in Victoria increased from five per day in the first week of June to 479 per day in the first week of August (John Hopkins University, 2021). Restrictions were gradually re-imposed, culminating in a second city-wide lockdown commencing on 9 July 2020 (Iorio, 2020). Under these restrictions, people could only leave their home for work, study, exercise, shopping for supplies, medical care and caregiving. Other restrictions included a night-time curfew and limits on how far people could travel from home. In contrast, new COVID-19 infections outside of Victoria remained low (averaging 12 per day in June and July), leading to the re-opening of theatres, cinemas and fitness centres (NSW Government, 2020).
Melbourne residents had experienced 10 weeks of lockdown by the start of Wave 3 (16 September–16 October 2020). Lockdown proved successful in reducing new COVID-19 infections with an average of 12 per day across the state of Victoria over the Wave 3 period (John Hopkins University, 2021). Beginning on 13 September, restrictions were gradually eased with a change in the hours of the curfew, the reopening of playgrounds and somewhat greater allowances for social interaction outside the household (Kinsella and Handley, 2020). Lockdown otherwise remained substantially in place, including through a stay-at-home order, across metropolitan Melbourne for the duration of the survey period. Outside of Victoria, there was an average of 7 new infections per day in Australia over the course of Wave 3 and few restrictions in place.
2.3. Measures
2.3.1. Time and second COVID-19 lockdown
The second COVID-19 lockdown in Melbourne was coded based on the survey wave and the participants' location. The wave of the survey is indicated through two dummy variables, the first for Wave 2 (no = 0; yes = 1) and the second for Wave 3 (no = 0; yes = 1). Wave 1 is the base category, indicated where Wave 2 = 0 and Wave 3 = 0. The participant's city of residence (recorded at Wave 1) is indicated through dummy variables for Melbourne (no = 0; yes = 1) and the Rest of Australia (no = 0; yes = 1). Sydney is the base category, indicated where Melbourne = 0 and Rest of Australia = 0. The COVID-19 lockdown in Melbourne is indicated where Wave 3 = 1 and Melbourne = 1. This interaction between Wave 3 and Melbourne forms a separate variable referred to as COVID-19 lockdown.
2.3.2. Depressive and anxiety symptoms
Symptoms of depression and anxiety were measured using the 21-item Depression, Anxiety and Stress Scale (DASS-21; Brown et al., 1997). Responses on each of the relevant seven items were aggregated to create separate continuous scores for depression and anxiety. Scores were doubled so as to match the ranges (0–42) of the full DASS-42 sub-scales. Both subscales exhibit good internal consistency with Cronbach's alpha scores of 0.95 for depression and .92 for anxiety across the three waves.
2.3.3. Loneliness
Levels of loneliness were measured using the three-Item Loneliness Scale (Hughes et al., 2004), a previously validated scale appropriate for large surveys. Each item was measured with four-point response categories ranging from 1 (Never) to 4 (Often). A single continuous loneliness score was calculated by aggregating responses across the three items. The loneliness scale also exhibited good internal consistency (α = 0.91).
2.3.4. Neighbourhood social relations
Neighbourhood social relations is conceived as a constituent component of social cohesion (Bernard, 2009; Chan et al., 2006). It is measured using 11 items adapted from Dragolov et al. (2016) and Sampson et al. (1997) (see also Cárdenas et al., 2021). Participants were asked to indicate to what extent they agreed with a series of statements that described whether people in their neighbourhood i) are willing to help each other, ii) trust each other, iii) get along well, iv) form a close knit community, v) feel safe walking alone at night, vi) get along with people from different national or ethnic backgrounds, vii) work together to solve community problems, viii) have civil conversations with people who have different views, ix) respect practices from different national or ethnic groups, x) respect local rules and laws, and xi) usually get what they deserve. Responses were collected using a Likert-scale ranging from 1, Strongly disagree, to 7, Strongly agree. The items of the social relations scale have a high degree of internal consistency (α = 0.90).
The quality of neighbourhood social relations is measured through two components. The first component is the perceived level or stock of neighbourhood relations that have potentially built up over time. This is measured by participants' average scores across waves. The second component is the change in social relations perceived by individuals across waves, measured by taking participants' perceived quality of relations at each wave and subtracting their average scores. Scores for the level of and changes in social relations are standardised by converting them into a z-score with a mean of zero and a standard deviation of one. The first component investigates whether individuals draw on established levels of positive neighbourhood social relations to support their mental health and well-being; the second component investigates whether changes in individuals’ mental health are related to changes in their perceptions of social relations, including in response to the COVID-19 lockdown. The two components allow us to test H3 by isolating levels of perceived relations emerging from lockdown from the potentially confounded changes in perceived relations.
2.3.5. Covariates
Time-invariant covariates are age, sex, employment status (not employed = 0; employed = 1), highest education (a 4-category dummy variable: graduate certificate/degree; diploma/Bachelor's degree; vocational certificate; and high school or less), whether born outside Australia (no = 0; yes = 1), whether has Australian or western European ancestry (no = 0; yes = 1), household composition (a 4-category dummy variable: live alone; couple without children; couple with child (ren); other) and socioeconomic disadvantage of the participant's suburb (measured by the ABS [2018] Index of Relative Socioeconomic Disadvantage). Data on these were collected at Wave 1 and are held constant for individuals across waves. A time-varying covariate is also included, namely whether the participant reported a confirmed case of COVID-19. We also include a continuous variable indicating the length of time since the start of Wave 3. The inclusion of this variable means that the estimated effects of lockdown are weighted to the start of Wave 3 (mid-September 2020) when lockdown restrictions were at their tightest.
2.4. Analytical approach
Multilevel linear mixed effects regression models are used to estimate the associations between COVID-19 lockdown, perceived neighbourhood social relations and the mental health indicators. The three hypotheses are tested by successively introducing explanatory variables through three models. All models are run with Stata 17 (StataCorp, 2021). In Model 1, the effects of lockdown (versus no lockdown) on changes in mental health (H1) are analysed by regressing mental health symptoms on i) the survey wave, ii) the participant's city of residence and iii) an interaction between survey wave and city. The approach therefore takes the form of a difference-in-difference analysis (Wing et al., 2018). In Model 2, mental health is modelled as a function of the variables in Model 1 and the level of, and changes in, neighbourhood social relations, thereby testing H2. In modelling between and within-person differences in perceived social relations as separate parameters, the models take the form of Random Effects Within Between (REWB) models (Bell et al., 2019). In Model 3, interactions between COVID-19 lockdown and the level of, and change in, neighbourhood social relations are added to Model 2. This is intended to address H3, assessing the degree to which neighbourhood social relations have had a differential impact on mental health during lockdown.
Models 1–3 can be expressed through the following equations:
is the natural logarithm of outcome variable for participant at wave ; is an individual-level random intercept; is a vector of two dummy variables indicating whether participants live in Melbourne or the Rest of Australia (Sydney is the base category); is a vector of two dummy variables indicating whether the survey wave is Wave 2 or Wave 3 (Wave 1 is the base category); is a vector of the covariates; is the perceived neighbourhood social relations score for participant at wave , while is the participant's average neighbourhood social relations score across waves. therefore is the within-person deviation in perceived social relations at each wave. The s are the fixed and random effect parameters to be estimated by the model. is the residual between respondent ’s actual and predicted outcome score.
The difference-in-difference and REWB components of the model estimate the within- and between-person associations between lockdown, neighbourhood relations and mental health (Bell et al., 2019; Wing et al., 2018). The individual-level random intercept, , and the random slopes, and on lockdown and social relations respectively, attempt to control for individual time-invariant characteristics such that the models, in effect, regress individual-level changes in mental health across waves on their individual changes in social relations and their lockdown status (a parallel to the fixed effects model). Thus, is a relatively robust and quasi-experimental estimate of the impact of an externally imposed event (COVID-19 lockdown) on individual change in mental health. is an estimate of the association between changes in neighbourhood social relations and mental health. By associating changes over time, controls for unmeasured characteristics to an extent, though is vulnerable to endogeneity and reverse causation as perceived social relations and mental health are measured from the same participant's responses. estimates the between-person association between levels of social relations and mental health. While conceptually important in understanding the role of established stocks of social relations, note that is vulnerable to omitted variable bias (Bell et al., 2019). Finally, and estimate the associations between mental health and the levels of and changes in social relations during lockdown.
The analyses are run on the entire sample, including participants living outside of Sydney and Melbourne; the purpose is to maximise statistical power in estimating the associations between neighbourhood social relations and mental health. People living outside of Sydney and Melbourne are indicated in the models through the dummy variable, Rest of Australia. Doing so allows us to include the full sample in the analyses while isolating the relative effect of lockdown for participants in Melbourne relative to participants in Sydney.
3. Results
3.1. Missing data
Preliminary analyses were performed to assess the extent and potential influence of missing data and participant attrition. Of 9090 potential person-wave records, 3230 (35.5%) contain missing data on one or more variables. The majority (71.3%) of missing data is due to participant attrition; that is, not participating in a survey wave (unit non-response), while 28.7% is due to participants not providing a response to specific questions (item non-response). Random effects logistic regression models were run to predict the probability of a record with missing data as a function of the dependent and independent variables and covariates. Neighbourhood social relations and location were not significantly associated with missing data. Critically though, missing data is positively and significantly associated with Wave 1 depression (odds ratio = 1.02; p < .01), anxiety (odds ratio = 1.04; p < .01) and loneliness (odds ratio = 1.05; p < .05) scores. Thus, missing data are not Missing Completely at Random (MCAR) such that participants with relatively high initial levels of mental health problems are more likely to drop out of the survey and leave questions answered. If left untreated, bias may be created in the results if those with greater mental health problems have a different response to lockdown than those with fewer problems.
Multiple imputation is used to address potential bias arising from missing data. Missing data are imputed both for item and unit non-response. Imputing unit non-response allows us to adjust for non-random rates of attrition. Imputation is performed by chained equations in which linear, binary logistic and multinomial logistic regression models are sequentially run on each variable containing missing data. All variables are included in the imputation model, including the interaction terms (von Hippel, 2009). A set of auxiliary variables are also included, namely a measure of self-rated health, the participant's average depression, anxiety and loneliness scores across waves and the individual items on the depression, anxiety and loneliness scales. This allows us to maximise the use of available information in imputing data and is particularly beneficial where participants provide responses on some but not all items of the DASS and loneliness scales. We impute 20 datasets and use von Hippel's (2020) quadratic rule to confirm that this is a sufficient number. An important assumption of our imputation approach is that attrition resulting from unobserved deterioration in mental health is random or can be predicted by pre-existing levels of mental health or the other imputation variables.
3.2. Descriptive statistics
The socio-demographic profiles of Melbourne and Sydney provide a strong basis for comparison. Pre-pandemic results from the National Health Survey, 2017–18 (ABS, 2019) indicate that the proportion of the population in Melbourne and Sydney who experience moderate (21.4% and 24.0% respectively), high (9.1% and 9.1% respectively) and very high (4.2% and 4.3% respectively) levels of psychological distress (using the Kessler-10 scale) are very similar. Likewise, in this study, survey participants in Melbourne and Sydney have similar sociodemographic characteristics (see Table 1 ). Differences in average age (F = 1.65; p = .20), sex (χ2 = 0.00; p = .99), employment (χ2 = 0.00; p = .97) and household type (χ2 = 1.21; p = .75) are small and not statistically significant. Sydney and Melbourne participants also have similar rates of item (χ2 = 0.47; p = .49) and unit (χ2 = 0.15; p = .70) non-response. Compared with Sydney, participants in Melbourne are somewhat and significantly less likely to be born outside of Australia (χ2 = 8.17; p < .01), live in less disadvantaged suburbs on average (F = 4.70; p < .03) and marginally more likely to have been diagnosed with COVID-19 (χ2 = 3.19; p = .07). Differences in post-school qualification (χ2 = 1.62; p = .20) and non-western European ancestry (χ2 = 1.85; p = .17) are not significant. Bivariate associations between all variables are provided in the supplementary material.
Table 1.
Descriptive statistics of survey sample by location.
| Location |
||||
|---|---|---|---|---|
| Melbourne | Sydney | Rest of Australia | Australia | |
| Average age at wave 1 | 43.1 | 44.4 | 50.0 | 47.8 |
| % female | 50.5 | 50.4 | 54.0 | 52.7 |
| % Australian born | 27.8 | 35.9 | 24.5 | 27.2 |
| % no western European ancestry | 20.2 | 23.6 | 7.3 | 12.5 |
| % employed at wave 1 | 58.4 | 58.6 | 46.9 | 51.1 |
| % diagnosed with COVID-19 at wave 1 | 4.9 | 2.8 | 1.3 | 2.2 |
| Average neighbourhood socioeconomic decile | 6.7 | 6.3 | 5.3 | 5.7 |
| Highest education at wave 1 (% of total) | ||||
| High school or less | 20.8 | 24.0 | 30.3 | 27.5 |
| Trade qualification | 14.3 | 14.7 | 22.0 | 19.3 |
| Diploma or degree | 41.5 | 37.7 | 32.7 | 35.2 |
| Postgraduate qualification | 23.4 | 23.6 | 14.9 | 18.0 |
| Household type at wave 1 (% of total) | ||||
| Live alone | 15.8 | 13.5 | 19.6 | 17.8 |
| Couple (no children) | 28.1 | 28.5 | 37.3 | 34.1 |
| Couple with child (ren) | 31.9 | 32.4 | 25.7 | 28.0 |
| Other | 24.1 | 25.6 | 17.4 | 20.1 |
| Missing data (% of total) | ||||
| Attrition (unit non-response) rate | 24.8 | 24.2 | 25.8 | 25.3 |
| Person-waves with item non-response | 10.7 | 10.1 | 10.1 | 10.2 |
| Total sample, N | 527 | 563 | 1940 | 3030 |
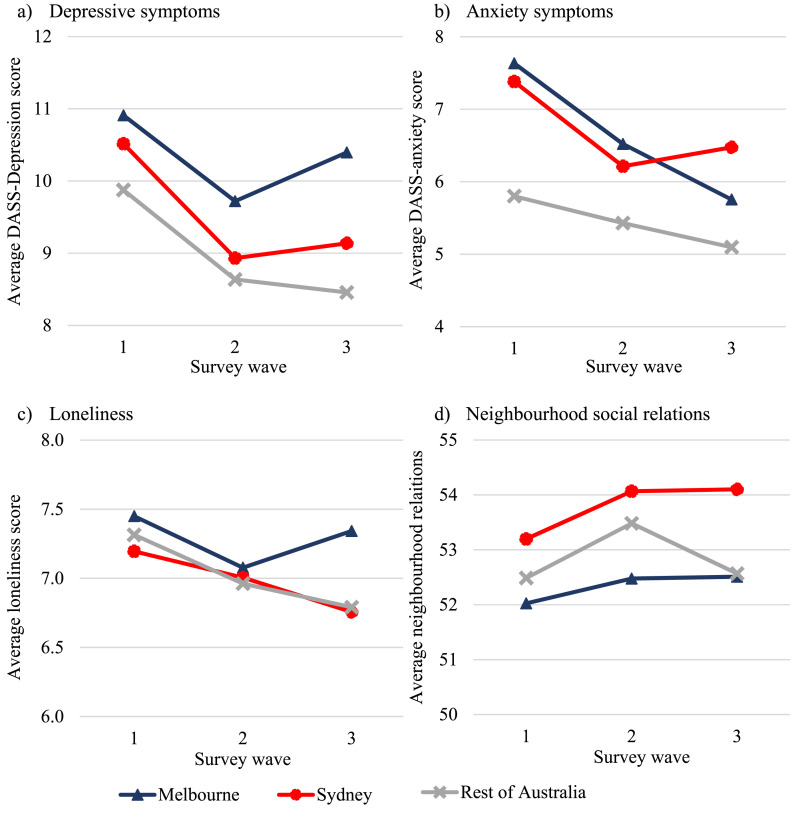
Average participant mental health and neighbourhood social relations scores are presented in Fig. 1 by location. Mental health scores generally declined across survey waves, indicating an aggregate-level improvement in mental health over time. This aligns with population-level trajectories recorded in the United Kingdom (Fancourt et al., 2021), suggesting that anxiety and depression levels peaked during the initial stages of the pandemic in early 2020. In Melbourne, however, average depression and loneliness scores increased between Wave 2 and Wave 3, coinciding with the imposition of lockdown restrictions. Average anxiety scores in Melbourne declined across all three waves and increased in Sydney between Waves 2 and 3. Perceived neighbourhood social relations scores increased over time in Sydney and Melbourne and decreased in the rest of Australia (on average) between Waves 2 and 3.
Fig. 1.
Mental health and perceived neighbourhood social relations trajectories by location.
3.3. Main analyses
The key regression results shown in Table 2 test the four hypotheses, illustrating the associations between mental health, the second COVID-19 lockdown in Melbourne and neighbourhood social relations. The full set of regression results are provided in the supplementary material. F statistics indicate that all models are statistically significant at the 99% confidence level. Unless otherwise stated, the results presented here and in the supplementary material are based on the 20 imputed datasets.
Table 2.
Key regression results predicting associations between mental health, COVID-19 lockdown and neighbourhood social relations.
| Model |
|||
|---|---|---|---|
| 1 | 2 | 3 | |
| Predicted % increase in scores [95% confidence interval] | |||
| Depression | |||
| COVID-19 lockdown | 23 [9.9, 37]** | 22 [9.0, 36]** | 21 [8.2, 36]** |
| Neighbourhood social relations | |||
| Level | −23 [-26, −19]** | −13 [-21, −3.2]* | |
| Change | -.25 [-1.7, 1.3] | −4.5 [-11, 2.2] | |
| Neighbourhood social relations × lockdown | |||
| Level × lockdown | −9.4 [-17, −1.3]* | ||
| Change × lockdown | 12 [-.44, 25]† | ||
| Model F statistic | 27** | 27** | 18** |
| Anxiety | |||
| COVID-19 lockdown | .71 [-9.2, 12] | -.46 [-10, 11] | −1.1 [-11, 10] |
| Neighbourhood social relations | |||
| Level | −14 [-17, −10]** | −6.9 [-16, 2.7] | |
| Change | .45 [-1.0, 1.9] | −2.3 [-8.1, 3.9] | |
| Neighbourhood social relations × lockdown | |||
| Level × lockdown | −2.4 [-9.7, 5.4] | ||
| Change × lockdown | 11 [.25, 23]* | ||
| Model F statistic | 26** | 27** | 18** |
| Loneliness | |||
| COVID-19 lockdown | 4.1 [.96, 7.4]* | 4.1 [.97, 7.4]* | 4.2 [1.0, 7.4]** |
| Neighbourhood social relations | |||
| Level | −5.4 [-6.5, −4.4]** | −2.2 [-5.0, .64] | |
| Change | -.29 [-.74, .16] | −1.2 [-3.1, .71] | |
| Neighbourhood social relations × lockdown | |||
| Level × lockdown | −1.4 [-3.7, 1.0] | ||
| Change × lockdown | 2.0 [-1.2, 5.2] | ||
| Model F statistic | 18** | 21** | 14** |
Note. All results based on 20 imputed datasets. **p < .01; *p < .05; †p < .1.
The second lockdown in Melbourne appears to have increased depressive symptoms and, to a lesser extent, feelings of loneliness. Experiencing a second COVID-19 lockdown predicts greater depression scores (23% before and 22% after accounting for neighbourhood social relations), indicating that lockdown had a substantial and significant adverse effect on depressive symptoms. The lockdown had a smaller yet significant effect on loneliness (4.0% before and after accounting for social relations). By contrast, lockdown did not predict anxiety symptoms. Therefore, H1 is partially supported, as lockdown predicts greater depression and loneliness but not anxiety.
The level of perceived neighbourhood social relations is strongly associated with depression, anxiety, and loneliness. A one standard deviation increase in the level of social relations is associated with a −23% difference in depression scores, a −14% difference in anxiety and a −5.4% difference in loneliness scores (see Table 2). Within-person changes in perceived relations, on the other hand, are not associated with depression, anxiety, or loneliness. Overall, there is support for H2, that levels but not changes in perceived neighbourhood relations strongly predict better mental health.
The interaction between social relations levels and lockdown is significantly negatively associated with depressive symptoms (p < .05), but not with anxiety or loneliness. A one standard deviation increase in perceived relations is associated with a 9.4% reduction in depressive symptoms under lockdown. As a result, the Melbourne lockdown is predicted to have increased depressive symptoms by 21% for people with average perceived neighbourhood relations, compared with a 9.7% increase for people whose perceived relations is one standard deviation greater than average. Thus, there is some evidence that the buffering effect of neighbourhood social relations on depression was strengthened during the second lockdown in Melbourne (supporting H3).
Individual-level increases in neighbourhood social relations, on the other hand, are moderately associated with increasing depression and anxiety during lockdown. As seen in Model 3 (Table 2), the interaction between lockdown and a one standard deviation increase in neighbourhood social relations increases depressive symptoms by 12% (p < .1) and anxiety symptoms by 11% (p < .05).
3.4. Robustness analyses
The models are run without multiple imputation to test the robustness of the model to the missing data treatment. The direction and significance of the regression coefficients are unchanged. The measured effects of lockdown and neighbourhood social relations on depression and loneliness scores are somewhat smaller in the imputed data. For example, in Model 3, lockdown is estimated to increase depression scores by 26% and loneliness scores by 6.4% without multiple imputation (compared with 21% for depression and 4.0%, p < .05, for loneliness in datasets with imputation). Similar differences are found for neighbourhood social relations between the imputed and non-imputed datasets. Therefore, there is no evidence of bias due to treatment of missing data.
Analyses are undertaken to explain why individual-level increases in neighbourhood relations are associated with worsening mental health. The full set of analyses are provided in the supplementary material. We find that the positive associations are modest in size and robust to different model specifications. We perform tests to determine the potential direction of causation and look for evidence in support of the ‘psychosocial gains to adversity’ and ‘tend and befriend’ theories. No evidence is found that establishes a temporal order for a potential causal relationship. Yet, as the study only contains one wave of data during the Melbourne lockdown (Wave 3), we are not able to test the effects of changes in mental health during lockdown on subsequent changes in perceived neighbourhood relations and vice versa. Thus, we have not been able to disentangle the direction of the relationship between emergent social relations and mental health during lockdown.
4. Discussion
Countries and societies around the world have experienced multiple lockdowns in response to the COVID-19 pandemic. Despite their effectiveness in suppressing infections, emerging evidence suggests that lockdowns are detrimental to mental health. The results of this study build on existing research in demonstrating that the second COVID-19 lockdown in Melbourne adversely impacted levels of depression and loneliness. Although other research also finds that lockdowns adversely impact anxiety levels, our findings generally fit with existing literature (Prati and Mancini, 2021) and support our first hypothesis (H1). The present study adds to the statistical rigour of the current body of work through our ability to track the mental health of participants before and during a second severe lockdown (i.e., in Melbourne), and compare them to the mental health trajectories of people who did not experience lockdown (i.e., in Sydney).
In support of H2, levels of perceived neighbourhood social relations are strongly related to mental health (anxiety, depression, and loneliness) controlling for a range of other key predictors such as age, gender, socio-economic status, and education levels. A one standard deviation increase in perceived relations is predicted to offset or buffer the adverse impact of COVID-19 lockdown on depression, anxiety, and loneliness. These results support existing theory and evidence on the hypothesised effects of social environments and social identities on mental health (Ehsan et al., 2019; Jetten et al., 2017; Mair et al., 2008).
We were not able to establish a clear link between changes in individual-level neighbourhood relations over time and mental health. Note that perceived neighbourhood relations are likely to gradually accumulate over time as relationships and connections develop, and the survey timespan in this study may not be sufficient to assess the effects of change. Nevertheless, the magnitude, significance, and robustness of the associations between the level of neighbourhood relations and mental health supports the view that investment in social cohesion at local levels benefits individual mental health (Lalot et al., 2021). Programs and interventions that promote mental health would therefore benefit from strengthening social connections and resources within communities (Cruwys et al., 2014; Fong et al., 2021; Haslam et al., 2018).
Findings were mixed with respect to the hypothesised protective effect of neighbourhood social relations during lockdown. On the one hand, we find some evidence that the level of neighbourhood social relations had a stronger protective effect on depression during lockdown (supporting H3) but we did not find evidence of a similar effect on anxiety or loneliness. We also find that positive changes in perceptions of social relations are associated with worse symptoms of depression and anxiety. This provides circumstantial evidence in support of theories positing that social environments and perceived affiliative links strengthen in response to collective crises and psychological stress (Mancini, 2019; Taylor, 2011). Other factors may also underpin such findings such as real and perceived gaps between expectations regarding the quality of neighbourhoods and the lack of psychosocial support actually experienced by individual members. Thus, understanding the interactions between individual well-being and the social environment during the pandemic is an area for further research.
4.1. Limitations
The context in which the survey took place is critical to the interpretation of the findings. The entirety of the survey was conducted during the period of the global pandemic, and mental health and well-being was likely strained across all waves and locations. Indeed, mental health symptoms were highest in the earlier stages of the pandemic when Australia was emerging from an initial nation-wide lockdown. Further, the fact that the lockdown in Melbourne was imposed in response to a spike in COVID-19 infections makes it difficult to distinguish the effects of lockdown restrictions from infections and the pandemic itself. In saying that, the third wave of the survey occurred after the peak in infections, and while lockdown restrictions were still in place, the number of new infections were low. Thus, concern and anxiety around infections and the spread of the virus may have peaked and receded before the start of Wave 3. This may also help to explain the lack of association between lockdown and anxiety, but also suggests the short-term impacts of lockdown may be disguised by the timing of the survey.
The broader government response to the pandemic should be also kept in mind. The Australian national government responded to the pandemic by funding a nation-wide wage scheme and enhanced income support for those out of work (Phillips et al., 2020), which may have weakened the potential financial mechanisms through which lockdown affects mental health. The long-term effects of lockdown restrictions and supporting policies on mental health remains an important question, particularly when successful in curbing COVID-19 infections and returning life to normalcy.
Further caveats and limitations relate to the design of the study. Firstly, we focus on average mental health effects, rather than assessing the diversity of trajectories (Bonanno et al., 2011). Secondly, while our imputation strategy helps address problems of missing data and attrition, the underpinning assumption of ignorability (Sidi and Harel, 2018) is potentially violated and the results biased by hidden relationships between the variables and missingness. Thirdly, neighbourhood social relations is measured by the participants' subjective perceptions, rather than an external, ‘objective’ measure. The subjective experience of neighbourhoods is likely critical to individual mental health and is in line with research on subjective well-being, which suggests that the way individuals experience their lives is both different from objective indicators of well-being (e.g., income), and a unique predictor of life outcomes (Diener et al., 2020). Yet, the use of participants' perceptions in our analyses impairs our ability to fully understand the relationship between objective neighbourhood relations and mental health, because a) a person's mental health may shape their perceptions of their neighbourhood, and b) other unmeasured subjective factors may explain both neighbourhood perceptions and mental health. Future research ought to consider how perceived social relations and cohesion relate to, and interact with, objective and externally measured indicators (e.g., rates of volunteering) to buffer mental health during and after crises.
5. Conclusion
This study provides robust evidence on the short-term mental health impacts of COVID-19 lockdowns. While lockdowns appear to be detrimental to mental health, particularly in terms of depression, strong associations between established levels of neighbourhood relations and mental health offset the effects of lockdown. This underscores the importance of the social environment to mental health, providing new evidence on its role during COVID-19. The pattern of findings also points to the need for future research on how changes in social relations and cohesion impact individuals. Altogether, these results illustrate the importance of the social environment on individuals’ mental health and the need for future research and interventions in this area.
Credit author statement
James O'Donnell: Conceptualisation, Methodology, Software, Validation, Formal analysis, Writing – original draft, Writing – review & editing, Diana Cárdenas: Conceptualisation, Methodology, Validation, Investigation, Data curation, Writing – original draft, Writing – review & editing, Nima Orazani: Conceptualisation, Methodology, Validation, Writing – original draft, Writing – review & editing, Ann Evans: Conceptualisation, Methodology, Writing – review & editing, Supervision, Project administration, Funding acquisition, Katherine J. Reynolds: Conceptualisation, Methodology, Writing – review & editing, Supervision, Project administration, Funding acquisition.
Acknowledgements
This research was supported by the ANU College of Health and Medicine Crisis Seed Funding Grant and the Australian Social Cohesion: Exploring New Directions Grand Challenge Scheme.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.socscimed.2022.114821.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- ABS . 2017. Census of Population and Housing.https://www.abs.gov.au/census/find-census-data [Google Scholar]
- ABS . 2018. Census of Population and Housing: Socio-Economic Indexes for Areas (SEIFA), Australia 2016.https://www.abs.gov.au/ausstats/abs@.nsf/mf/2033.0.55.001 [Google Scholar]
- ABS . 2019. Microdata: National Health Survey, 2017-18.https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/4324.0.55.001main+features12017-18 [Google Scholar]
- ABS . 2021. National, State and Territory Population.https://www.abs.gov.au/statistics/people/population/national-state-and-territory-population [Google Scholar]
- ABS . 2021. Migration, Australia.https://www.abs.gov.au/statistics/people/population/migration-australia/2019-20 [Google Scholar]
- Alcalá H.E., Sharif M.Z., Albert S.L. Social cohesion and the smoking behaviors of adults living with children. Addict. Behav. 2016;53:201–205. doi: 10.1016/j.addbeh.2015.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aminzadeh K., Denny S., Utter J., Milfont T.L., Ameratunga S., Teevale T., Clark T. Neighbourhood social capital and adolescent self-reported wellbeing in New Zealand: a multilevel analysis. Soc. Sci. Med. 2013;84:13–21. doi: 10.1016/j.socscimed.2013.02.012. [DOI] [PubMed] [Google Scholar]
- Bell A., Fairbrother M., Jones K. Fixed and random effects models: making an informed choice. Qual. Quantity. 2019;53:1051–1074. doi: 10.1007/s11135-018-0802-x. [DOI] [Google Scholar]
- Bernard P. Social cohesion: a dialectical critique of a quasi-concept. Lien Soc. Politiques. 2009;41:47–59. doi: 10.7202/005057ar. [DOI] [Google Scholar]
- Biddle N., Edwards B., Gray M., Solis K. Centre for Social Research & Methods, ANU; 2020. Tracking Outcomes during the COVID-19 Pandemic (August 2020) – Divergence with Australia.https://csrm.cass.anu.edu.au/research/publications/tracking-outcomes-during-covid-19-pandemic-august-2020-divergence-within [Google Scholar]
- Bonanno G.A., Westphal M., Mancini A.D. Resilience to loss and potential trauma. Annu. Rev. Clin. Psychol. 2011;7:511–535. doi: 10.1146/annurev-clinpsy-032210-104526. [DOI] [PubMed] [Google Scholar]
- Bowe M., Wakefield J.R., Kellezi B., Stevenson C., McNamara N., Jones B.A., Sumich A., Heym N. The mental health benefits of community helping during crisis: coordinated helping, community identification and sense of unity during the COVID‐19 pandemic. J. Community Appl. Soc. Psychol. 2021 doi: 10.1002/casp.2520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown T.A., Chorpita B.F., Korotitsch W., Barlow D.H. Psychometric properties of the depression anxiety stress scales (DASS) in clinical samples. Behav. Res. Ther. 1997;35(1):79–89. doi: 10.1016/S0005-7967(96)00068-X. [DOI] [PubMed] [Google Scholar]
- Budimir S., Probst T., Pieh C. Coping strategies and mental health during COVID-19 lockdown. J. Ment. Health. 2021;30(2):1–8. doi: 10.1080/09638237.2021.1875412. [DOI] [PubMed] [Google Scholar]
- Calo-Blanco A., Kovářík J., Mengel F., Romero J.G. Natural disasters and indicators of social cohesion. PLoS One. 2017;12(6):1–13. doi: 10.1371/journal.pone.0176885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell K., Vines E. COVID-19: a chronology of Australian Government announcements (up until 30 June 2020) Depart. Parliament Serv. 2021 https://www.aph.gov.au/About_Parliament/Parliamentary_Departments/Parliamentary_Library/pubs/rp/rp2021/Chronologies/COVID-19StateTerritoryGovernmentAnnouncements [Google Scholar]
- Cárdenas D., Orazani N., Stevens M., Cruwys T., Platow M., Zekulin M., Reynolds K.J. United we stand, divided we fall: socio-political predictors of physical distancing and hand hygiene during the covid-19 pandemic. Polit. Psychol. 2021;42(5):845–861. doi: 10.1111/pops.12772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan J., To H., Chan E. Reconsidering social cohesion: developing a definition and analytical framework for empirical research. Soc. Indicat. Res. 2006;75(2):273–302. doi: 10.1007/s11205-005-2118-1. [DOI] [Google Scholar]
- Chuang Y.C., Chuang K.Y., Yang T.H. Social cohesion matters in health. Int. J. Equity Health. 2013;12 doi: 10.1186/1475-9276-12-87. Article 87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cruwys T., Haslam S.A., Dingle G.A., Haslam C., Jetten J. Depression and social identity: an integrative review. Personal. Soc. Psychol. Rev. 2014;18(3):215–238. doi: 10.1177/1088868314523839. [DOI] [PubMed] [Google Scholar]
- Delhey J., Dragolov G. Happier together. Social cohesion and subjective well-being in Europe. Int. J. Psychol. 2016;51(3):163–176. doi: 10.1002/ijop.12149. [DOI] [PubMed] [Google Scholar]
- Diener E., Thapa S., Tay L. Positive emotions at work. Ann. Rev. Org. Psychol. Org. Behav. 2020;7:45–477. doi: 10.1146/annurev-orgpsych-012119-044908. [DOI] [Google Scholar]
- Dragolov G., Ignácz Z.S., Lorenz J., Delhey J., Boehnke K., Unzicker K. What Holds Societies Together: Insights from the Social Cohesion Radar. Springer International; 2016. Social cohesion in the Western world. [DOI] [Google Scholar]
- Drury J., Brown R., González R., Miranda D. Emergent social identity and observing social support predict social support provided by survivors in a disaster: solidarity in the 2010 Chile earthquake. Eur. J. Soc. Psychol. 2016;46(2):209–223. doi: 10.1002/ejsp.2146. [DOI] [Google Scholar]
- Ehsan A., De Silva M.J. Social capital and common mental disorder: a systematic review. J. Epidemol. Commun. Health. 2015;69(10):1021–1028. doi: 10.1136/jech-2015-205868. [DOI] [PubMed] [Google Scholar]
- Ehsan A., Klaas H.S., Bastianenm A., Spini D. Social capital and health: a systematic review of systematic reviews. SSM – Population Health. 2019;8:1–18. doi: 10.1016/j.ssmph.2019.100425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fan C., Jiang Y., Mostafavi A. Emergent social cohesion for coping with community disruptions in disasters. J. R. Soc. Interface. 2020;17 doi: 10.1098/rsif.2019.0778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fancourt D., Steptoe A., Bu F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: a longitudinal observational study. Lancet Psychiatr. 2021;8(2):141–149. doi: 10.1016/S2215-0366(20)30482-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiori K.L., Antonucci T.C., Cortina K.S. Social network typologies and mental health among older adults. J. Geol. B. 2016;61(1):P25–P32. doi: 10.1093/geronb/61.1.P25. [DOI] [PubMed] [Google Scholar]
- Fone D., White J., Farewell D., Kelly M., John G., Lloyd K., Williams G., Dunstan F. Effect of neighbourhood deprivation and social cohesion on mental health inequality: a multilevel population-based longitudinal study. Psychol. Med. 2014;44(11):2449–2460. doi: 10.1017/S0033291713003255. [DOI] [PubMed] [Google Scholar]
- Fong P., Cruwys T., Robinson S.L., Haslam S.A., Haslam C., Mance P.L., Fisher C.L. Evidence the loneliness can be reduced by a whole-of-community intervention to increase neighbourhood identification. Soc. Sci. Med. 2021;277 doi: 10.1016/j.socscimed.2021.113909. Article 113909. [DOI] [PubMed] [Google Scholar]
- Guo J., Feng X.L., Wang X.H., van Ijzendoorn M.H. Coping with COVID-19: exposure to COVID-19 and negative impact on livelihood predict elevated mental health problems in Chinese adults. Int. J. Environ. Res. Publ. Health. 2020;17(11) doi: 10.3390/ijerph17113857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haslam S.A., Postmes T., Ellemers N. More than a metaphor: organizational identity makes organizational life possible. Br. J. Manag. 2003;14(4):357–369. doi: 10.1111/j.1467-8551.2003.00384.x. [DOI] [Google Scholar]
- Haslam C., Jetten J., Cruwys T., Dingle G.A., Haslam S.A. Routledge; 2018. The New Psychology of Health: Unlocking the Social Cure. [DOI] [Google Scholar]
- Henderson H., Child S., Moore S., Moore J.B., Kaczynski A.T. The influence of neighborhood aesthetics, safety, and social cohesion on perceived stress in disadvantaged communities. Am. J. Community Psychol. 2016;58(1–2):80–88. doi: 10.1002/ajcp.12081. [DOI] [PubMed] [Google Scholar]
- Hopkins University John. COVID-19 data repository [data set] GitHub. 2021 https://github.com/CSSEGISandData/COVID-19 [Google Scholar]
- Hughes M.E., Waite L.J., Hawkley L.C., Cacioppo J.T. A short scale for measuring loneliness in large surveys: results from two population-based studies. Res. Aging. 2004;26(6):655–672. doi: 10.1177/0164027504268574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iorio K. ABC News; 2020. Melbourne Enters New Coronavirus Lockdown. Here Are the Key Points from Premier Daniel Andrews.https://www.abc.net.au/news/2020-07-07/melbourne-lockdown-daniel-andrews-key-points/12431708 July 7. [Google Scholar]
- Ivory V.C., Collings S.C., Blakely T., Dew K. When does neighbourhood matter? Multilevel relationships between neighbourhood social fragmentation and mental health. Soc. Sci. Med. 2011;72:1993. doi: 10.1016/j.socscimed.2011.04.015. 2002. [DOI] [PubMed] [Google Scholar]
- Jetten J., Haslam S.A., Cruwys T., Greenaway K.H., Haslam C., Steffens N.K. Advancing the social identity approach to health and well‐being: progressing the social cure research agenda. Eur. J. Soc. Psychol. 2017;47(7):789–802. doi: 10.1002/ejsp.2333. [DOI] [Google Scholar]
- Kinsella E., Handley E. ABC News; 2020. Melbourne's Coronavirus Restrictions Roadmap: the Five Steps from Stage 4 Lockdown to ‘COVID Normal’.https://www.abc.net.au/news/2020-09-06/coronavirus-explainer-melbourne-roadmap-easing-restrictions/12634506 September 6. [Google Scholar]
- Lalot F., Abrams D., Broadwood J., Hayon K.D., Platts-Dunn I. The social cohesion investment: communities that invested in integration programmes are showing greater social cohesion in the midst of the COVID-19 pandemic. J. Community Appl. Soc. Psychol. 2021 doi: 10.1002/casp.2522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lei L., Huang X., Zhang S., Yang J., Yang L., Xu M. Comparison of prevalence and associated factors of anxiety and depression among people affected by versus people unaffected by quarantine during the COVID-9 epidemic in Southwestern China. Med. Sci. Mon. Int. Med. J. Exp. Clin. Res. 2020;26 doi: 10.12659/MSM.924609. e924609–e924609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ludin S.M., Rohaizat M., Arbon P. The association between social cohesion and community disaster resilience: a cross-sectional study. Health Soc. Care. 2019;27(3):621–631. doi: 10.1111/hsc.12674. [DOI] [PubMed] [Google Scholar]
- Mair C., Roux A.V.D., Galea S. Are neighbourhood characteristics associated with depressive symptoms? A review of evidence. J. Epidemol. Commun. Health. 2008;62(11):940–946. doi: 10.1136/jech.2007.066605. [DOI] [PubMed] [Google Scholar]
- Mancini A. When acute adversity improves psychological health: a social-contextual framework. Psychol. Rev. 2019;126(4):486–505. doi: 10.1037/rev0000144. [DOI] [PubMed] [Google Scholar]
- Niedzwiedz C.L., Green M.J., Benzeval M., Campbell D., Craig P., Demou E., Leyland A., Pearce A., Thomson R., Whitley E., Katikireddi S.V. Mental health and health behaviours before and during the initial phase of the COVID-19 lockdown: longitudinal analyses of the UK Household Longitudinal Study. J. Epidemiol. Community Health. 2021;75(3):224–231. doi: 10.1136/jech-2020-215060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nitschke J.P., Forbes P.A.G., Ali N., Cutler J., Apps M.A.J., Lockwood P.L., Lamm C. Resilience during uncertainty? greater social connectedness during COVID‐19 lockdown is associated with reduced distress and fatigue. Br. J. Health Psychol. 2021;26(2):553–569. doi: 10.1111/bjhp.12485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NSW Government . 2020. Gyms and Kids Sports to Reopen across NSW.https://www.nsw.gov.au/news/gyms-and-kids-sports-to-reopen-across-nsw June 2. [Press Release] [Google Scholar]
- Ntontis E., Drury J., Amlôt R., Rubin G.J., Williams R. Endurance or decline of emergent groups following a flood disaster: implications for community resilience. Int. J. Disaster Risk Reduc. 2020;45 doi: 10.1016/j.ijdrr.2020.101493. Article 101493. [DOI] [Google Scholar]
- Phillips B., Gray M., Biddle N. COVID-19 JobKeeper and JobSeeker impacts on poverty and housing stress under current and alternative economic and policy scenarios. ANU Centre Soc. Res. Method. 2020 https://csrm.cass.anu.edu.au/research/publications/covid-19-jobkeeper-and-jobseeker-impacts-poverty-and-housing-stress-under [Google Scholar]
- Pierce M., Hope H., Ford T., Hatch S., Hotopf M., John A., Kontopantelis E., Webb R., Wessely S., McManus S., Abel K.M. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatr. 2020;7(10):883–892. doi: 10.1016/S2215-0366(20)30308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prati G., Mancini A.D. The psychological impact of COVID-19 pandemic lockdowns: a review and meta-analysis of longitudinal studies and natural experiments. Psychol. Med. 2021;51:201–211. doi: 10.1017/S0033291721000015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruiz M., Malyutina S., Pajak A., Kozela M., Kubinova R., Bobak M. Congruent relations between perceived neighbourhood social cohesion and depressive symptoms among older European adults: an East-West analysis. Soc. Sci. Med. 2019;237:1–9. doi: 10.1016/j.socscimed.2019.112454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sampson R.J., Raudenbush S.W., Earls F. Neighborhoods and violent crime: a multilevel study of collective efficacy. Science. 1997;277(5328):918–924. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- Samuel L.J., Commodore-Mensah Y., Himmelfarb C.R. Developing behavioral theory with the systematic integration of community social capital concepts. Health Educ. Behav.: Off. Publ. Soc. Public. Health Edu. 2014;41(4):359–375. doi: 10.1177/1090198113504412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sidi Y., Harel O. The treatment of incomplete data: reporting analysis, reproducibility, and replicability. Soc. Sci. Med. 2018;209:169–173. doi: 10.1016/j.socscimed.2018.05.037. [DOI] [PubMed] [Google Scholar]
- StataCorp . StataCorp LLC; 2021. Stata Statistical Software: Release 17. [Google Scholar]
- Storen R., Corrigan N. Department of Parliamentary Services; 2020. COVID-19: a Chronology of State and Territory Government Announcements (Up until 30 June 2020)https://www.aph.gov.au/About_Parliament/Parliamentary_Departments/Parliamentary_Library/pubs/rp/rp2021/Chronologies/COVID-19StateTerritoryGovernmentAnnouncements [Google Scholar]
- Taylor S.E. In: Van Lange P.A.M., Kruglanski A.W., Higgins E.T., editors. ume 1. SAGE Publications Ltd; 2011. Tend and befriend theory; pp. 32–49. (Handbook of Theories of Social Psychology). [DOI] [Google Scholar]
- Thoits P.A. Stress and health: major findings and policy implications. J. Health Soc. Behav. 2010;51:S41. doi: 10.1177/0022146510383499. –S53. [DOI] [PubMed] [Google Scholar]
- Townshend I., Awosoga O., Kulig J., Fan H.Y. Social cohesion and resilience across communities that have experienced a disaster. Nat. Hazards. 2015;76:913–938. doi: 10.1007/s11069-014-1526-4. [DOI] [Google Scholar]
- Tull M.T., Edmonds K.A., Scamaldo K.M., Richmond J.R., Rose J.P., Gratz K.L. Psychological outcomes associated with stay-at-home orders and the perceived impact of COVID-19 on daily life. Psychiatr. Res. 2020;289 doi: 10.1016/j.psychres.2020.113098. 113098–113098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner J.C., Brown R.L. In: A Handbook for the Study of Mental Health: Social Contexts, Theories and Systems. Scheid T.L., Brown T.N., editors. Cambridge University Press; 2010. Social support and mental health. [DOI] [Google Scholar]
- Unger D.G., Wandersman A. The importance of neighbors: the social, cognitive, and affective components of neighboring. Am. J. Community Psychol. 1985;13(2):139–169. doi: 10.1007/BF00905726. [DOI] [Google Scholar]
- von Hippel P.T. How to impute interactions, squares, and other transformed variables. Socio. Methodol. 2009;39(1):265–291. doi: 10.1111/j.1467-9531.2009.01215.x. [DOI] [Google Scholar]
- von Hippel P.T. How many imputations do you need? A two-stage calculation using a quadratic rule. Socio. Methods Res. 2020;49(3):699–718. doi: 10.1177/0049124117747303. [DOI] [Google Scholar]
- Welton-Mitchell C., James L.E., Khanal S.N., James A.S. An integrated approach to mental health and disaster preparedness: a cluster comparison with earthquake affected communities in Nepal. BMC Psychiatr. 2018;18(1) doi: 10.1186/s12888-018-1863-z. 296–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . 2021. Mental Health & COVID-19.https://www.who.int/teams/mental-health-and-substance-use/covid-19 [Google Scholar]
- Wing C., Simon K., Bello-Gomez R.A. Designing difference in difference studies: best practices for public health policy research. Annu. Rev. Publ. Health. 2018;39:453–469. doi: 10.1146/annurev-publhealth-040617-013507. [DOI] [PubMed] [Google Scholar]
- Ye Z., Yang X., Zeng C., Wang Y., Shen Z., Li X., Lin D. Resilience, social support, and coping as mediators between COVID‐19‐related stressful experiences and acute stress disorder among college students in China. Appl. Psychol.: Health and Well-being. 2020;12(4):1074–1094. doi: 10.1111/aphw.12211. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.