Learning objectives.
By reading this article you should be able to:
-
•
Describe the epidemiology of major burn injuries and the possible mechanisms of injury.
-
•
Recall the structure and function of the skin.
-
•
Use burn depth classification and surface area to assess a patient's burn wound.
-
•
Describe the initial management of a major burn.
Key points.
-
•
An adult with a major burn, defined as >15% of total body surface area burned, will require resuscitation and care at a specialised burns service.
-
•
Depth of burn is assessed by the degree that the dermis has been affected and determines subsequent surgical management.
-
•
Major burns have local tissue and wider systemic effects. In burns >25% total body surface area, a systemic inflammatory response occurs.
-
•
Timely but safe transfer to a specialist centre is often required with attention to airway, invasive catheters, fluids and temperature maintenance.
-
•
Early surgical management with total or near-total burn wound excision in <48 h of injury has been shown to decrease blood loss, burn wound sepsis and length of stay.
A burn injury is the coagulative destruction of the skin and its structures by thermal, chemical, electrical or mechanical energy. A major burn is defined according to the percentage total body surface area (%TBSA) affected by the injury. A burn greater than 15% TBSA is considered major in an adult aged >16 yrs. A recent update on paediatric burns is available.1
Epidemiology
Fire, heat and hot substance injuries caused 8,991,468 injuries and 120,632 deaths worldwide in 2017.2 Ninety percent of these were in low- or middle-income countries.3 Comprehensive up-to-date statistics for the UK are not available for reference, but there are approximately 10,000 hospital admissions and 300 major burns in adults requiring fluid resuscitation in England and Wales per year.4,5 In Scotland there is an incidence of 500 burn injury admissions per year, of which 5% are major burns.6
The most common mechanism of injury requiring admission is scalds; however, the most common cause of major burns are flame injuries.7 Burn injuries have a wide aetiology including thermal (scald, flame, flash, contact, irradiation), electrical (including lightning strikes) and chemical (acid, alkali). Most are accidents in the home or work-related, but intentional injuries from deliberate self-harm, assaults or fires are more likely to result in major burns.8
Risk factors
Risk factors worldwide for suffering a burn injury include: low socioeconomic status; overcrowding; households where young girls have domestic roles; cooking with kerosene; generalised poor health; and poor safety practices.3 Injuries are more common in patients with pre-existing psychiatric diagnoses, substance use problems and those at extremes of age. Children suffer accidental and non-accidental injury. As the population ages, the older and frail individuals with pre-existing medical conditions presenting as collapse, are increasingly represented.9 Burns are a preventable injury and strategies to decrease the incidence focus on awareness, education and health and safety legislation.
Risk prediction
The main scoring system used to predict mortality and length of hospitalisation in adult burns injury is the revised Baux score, which takes into account age, %TBSA burned and the presence of inhalation injury.10 The point of futility (the Baux score at which the predicted mortality approaches 100%) was 100 in Baux's original article. The point of futility with 21st century burn care is now 160 and the Baux50 (the Baux score at which predicted mortality is 50%) is 109.6.11 Other risk prediction models are also in use such as the Belgian Outcome in Burn Injury score and the Abbreviated Burn Severity Index.12,13 As increasing age is strongly associated with mortality from a burn injury, there is a developing need to assess frailty and comorbidities as part of a holistic assessment of the older burns patient, although not yet included in the current scoring systems.14 Clinical frailty scores are increasingly being used in burns services, and the Rockwood clinical frailty scale is used in our unit for burn injuries in older people.15,16
Pathophysiology
Skin physiology
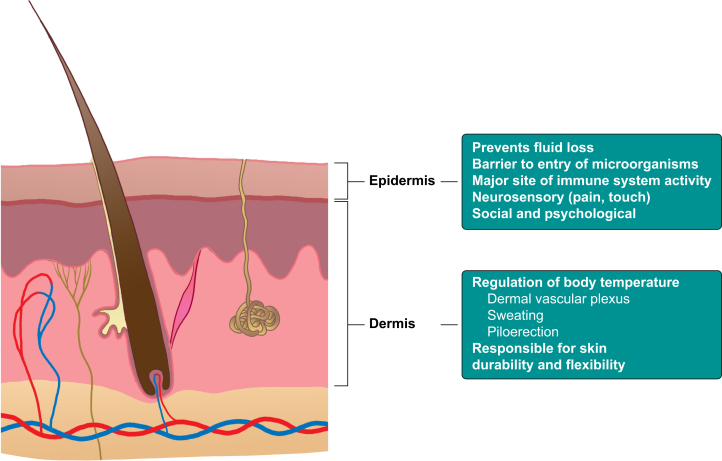
The skin is the largest organ system in the body. It is composed of the five layers of the epidermis and the two layers of the dermis, which sit on subcutaneous fat, connective tissue and the muscle compartments. The deepest layers of the epidermis continually divide and migrate to the surface to regenerate every 2–3 weeks. Melanocytes responsible for the skin's pigmentation are found in the epidermis. The dermis contains nerves, blood vessels, exocrine glands and hair follicles around which regenerating epidermal cells are found. The epidermis cannot regenerate without the presence of dermal tissue. By understanding the multiple functions of the skin and its roles in homeostasis (Fig. 1), it is easy to understand the sequelae of a burns injury, which will be discussed in detail in Part 2 of this series.17
Fig 1.
Functions of the skin.
Classification of burn injuries
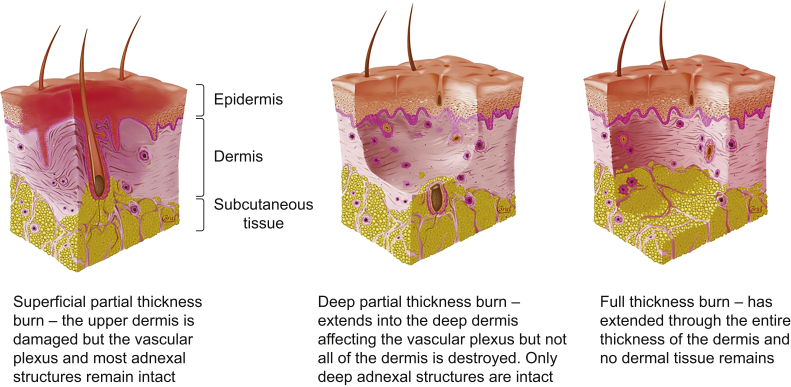
A burns injury is classified according to aetiology, percentage total body surface area involved and depth (Fig. 2).
Fig 2.
Depth of burn injuries are described by how much of the dermis has been destroyed. Adapted with permission from the Nederlandse Brandwonden Stichting, Dutch Burns Foundation.
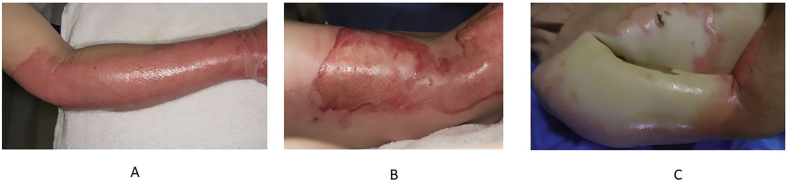
Simple erythema involving damage to the epidermis only is referred to as an epidermal or superficial burn and excluded from the calculation of surface area involved. Clinically significant burns involve the dermis, and are termed partial thickness, either superficial or deep, and full thickness. Worldwide it is more common for burn depth to be described as first degree (epidermal/superficial), second degree (partial thickness) or third degree (full thickness). The characteristics on examination are detailed in Figure 3.
Fig 3.
Clinical characteristics of burn injuries (written consent obtained from patient to publish images). (A) Superficial partial thickness burns are pale, pink and moist. Blisters form from fluid leak because of blood vessel damage. They are very painful because the nerve endings are exposed. (B) Deep partial thickness burns are drier, red and non-blanching as the dermal plexus is coagulated by heat. They are less sensate. (C) Full-thickness burns are waxy and white; they may look charred and are not painful.
The amount of tissue damage caused can be burn related or patient related. Burn-related factors include aetiology, temperature and duration of exposure. For example wet heat (scalds) carries more energy than dry heat (flame), so greater tissue damage is caused by the same temperature. Patient-related factors include skin thickness, age and whether or not first aid was given. The very young and older individuals with thinner, more fragile skin will have a greater injury from the same insult compared with an adult. A superficial partial thickness wound has a good blood supply and sufficient regenerating epidermal cells that, with proper management, can heal without scarring in 1–2 weeks. Deep partial thickness and full thickness burns have lost the dermal vascular plexus and cells to heal. They are generally managed by excision and skin grafting. The burn can also affect tissue deep to the dermis, the fat and muscle. Muscle injury can lead to compartment syndrome and rhabdomyolysis.
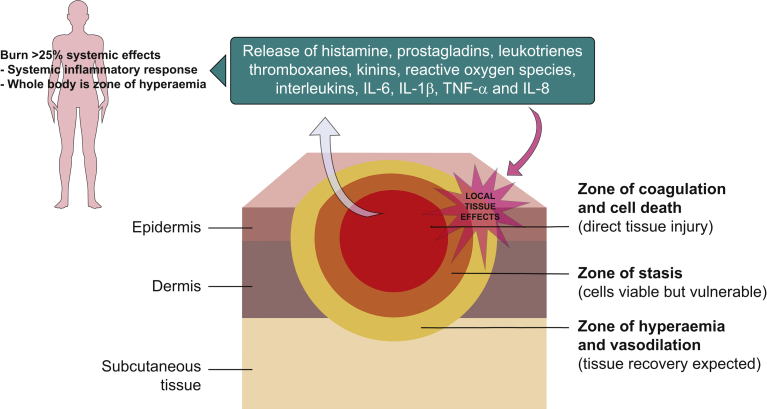
Local and systemic effects of major burns
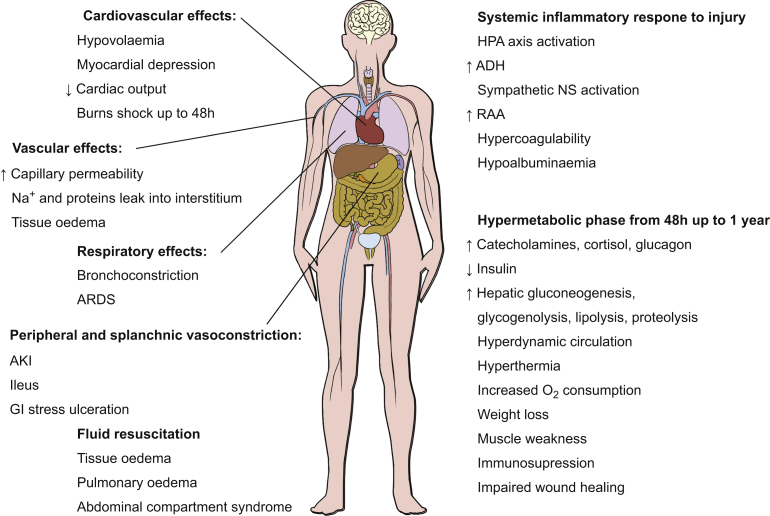
Major burn injuries have local and systemic effects (Fig. 4).
Fig 4.
Pathophysiology of burns. IL, interleukin; TNF-α, tumour necrosis factor-alpha.
The local effects are divided into three zones of tissue injury and blood flow described in Jackson's burn wound model.18 The zone of coagulation contains dead tissue as a result of direct injury. Adjacent to this area in the zone of stasis tissues suffer hypoperfusion owing to the vasoconstriction of vessels in response to the injury, and although not directly damaged, these tissues are vulnerable to ischaemia, infection and necrosis, and initial burn wounds may expand and deepen. Dead tissue prompts the release of inflammatory mediators, which act locally causing vasodilation, increased vascular permeability and oedema in the zone of hyperaemia. In the absence of resuscitation with i.v. fluids, this vasodilation exacerbates hypovolaemia and subsequent tissue hypoperfusion. In burns >25% TBSA, these mediators also cause a systemic inflammatory response with the effects outlined in Figure 5.
Fig 5.
Systemic effects of major burns. ADH, anti-diuretic hormone; AKI, acute kidney injury; ARDS acute respiratory distress syndrome; GI, gastrointestinal; HPA, hypothalamic–pituitary–adrenal; NS, nervous system; RAA, renin–angiotensin–aldosterone.
Early burn wound excision decreases the necrotic load, infection risk and systemic inflammatory effects. Burns dressings help stabilise the wound bed, decrease fluid losses and help prevent infection. Systemic effects consist of an acute phase up to 48 h after injury, in which a combination of peripheral vasodilation, hypovolaemia and myocardial depression result in burns shock and a hypermetabolic phase from approximately 48 h up to 1 yr after injury. The stress response to a burn injury is via the same pro-inflammatory mediators as in other causes of tissue injury, but of greater severity and duration.
Initial management
First aid
First aid at the scene is vitally important in burns and can prevent more severe injury. In particular there is a strong evidence base that a burn should be managed under cool or tepid running water for 20 min even up to 4 h after the injury is sustained. By arresting tissue damage, wounds are not as deep as they otherwise would have been, with subsequent improvement in healing and decreased scar formation.19 The general principles for thermal injuries are to use the SAFE approach (Shout/call for help, Assess the scene, Free from danger, Evaluate the casualty), stop the burning process, cool the burn and then cover in a non-adherent dressing (e.g. cling film).20,21 Although the burn must be cooled, the rest of the patient must be warmed to prevent hypothermia. For chemical burns the patient should be removed from the area of exposure and all contaminated clothing removed. Chemical burns should be irrigated with running water or sterile fluids taking care not to wash chemicals into the eyes. Irrigation is key in such burns as removing the chemicals stops the burning process. It is recommended that acid burns be irrigated for 45 min and alkali burns for 1 h.21 Agent-specific treatments should be given if available according to National Poisons Information Service advice.22 Electrical injuries may be accompanied by a burn, a useful comprehensive review of presentation and specific management is available.23
All major burns are traumatic injuries and should be treated according to the principles of Advanced Trauma Life Support (ATLS).24 The treatment recommendations that follow can be learnt on the Emergency Management of Severe Burns (EMSB) course run by the British Burn Association.25
Airway and breathing
The airway can be threatened via several mechanisms in a patient with major burns. Indications for intubation are: reduced conscious level requiring airway protection (e.g. because of head trauma during escape from a fire also requiring c-spine immobilisation, systemic toxicity from inhalation injury, medical or substance use causing collapse); actual or impending upper airway obstruction owing to deep neck, perioral or intra-oral burns and oedema; respiratory distress from inhalation injury requiring ventilatory support; or to facilitate safe transfer to a burns centre. However, the requirement for intubation is not always clear-cut, and the main concern is that a burned patient may have an associated inhalation injury that will subsequently cause airway oedema and an airway emergency in the hours that follow fluid resuscitation.
Inhalation injury
The hot gaseous products of combustion are inhaled particularly when a patient is trapped in an enclosed space with a fire. Hot gas causes direct burn injury to the upper airway, particulate matter and chemicals enter the lower airways causing acute lung injury and carbon monoxide and hydrogen cyanide cause systemic toxicity. Inhalation injury is more common if facial burns are present, but not all patients with facial burns have an inhalation injury. Signs and symptoms include cough, soot in the nose, mouth and sputum and singed eyebrows and nasal hair, but in the absence of a facial burn these are unlikely to signal an airway emergency. Voice changes, hoarseness and stridor, however, are particularly concerning as these signs may not develop until swelling is already obstructing the airway.26 If there is doubt about whether tracheal intubation is needed, discussion with the receiving burns service is advised. When securing the airway, it is vital to plan for a difficult intubation including a surgical airway as the tissues may be erythematous, ulcerated and distorted by oedema. Suxamethonium can be used safely up to 48 h after burn injury.27 A videolaryngoscope should be used if available and an uncut tracheal tube is vital to allow for further soft tissue swelling that might otherwise make a cut tube recede into the mouth. A larger-diameter tracheal tube is preferable to facilitate bronchoscopy and respiratory toilet.
Ventilation
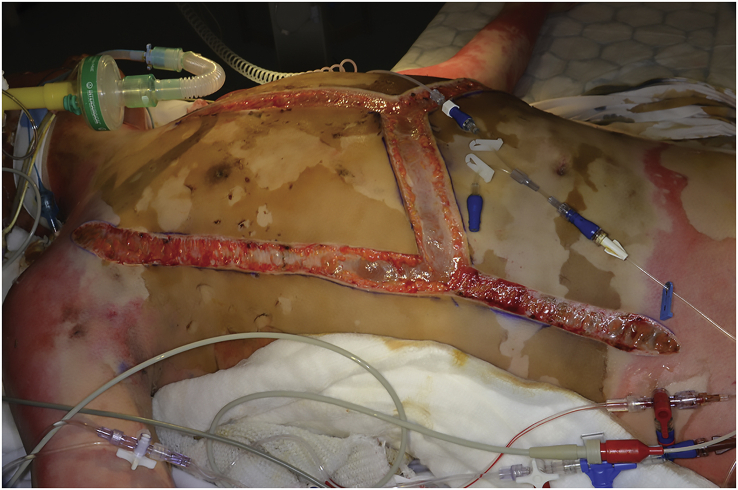
In full thickness burns the dead tissue or ‘eschar’ is non-compliant and may prevent adequate ventilation and adversely affect cardiac pre-load, necessitating escharotomies to the chest before transfer (Fig. 6). Impaired gas exchange may also be the result of inhalation injury and associated carbon monoxide poisoning. Hypoxaemia will persist despite adequate oxygen saturation by pulse oximetry, so it is important to check the co-oximetry results on an arterial blood gas. The time to carbon monoxide washout is reduced by ventilation in 100% oxygen, but hyperbaric oxygen therapy is not currently recommended.22 Patients' lungs should be ventilated with 100% oxygen until the carboxyhaemoglobin level is <3%, taking care to reduce the Fio2 as soon as possible to avoid further lung damage.27 Hydrogen cyanide poisoning should be considered in patients with inhalation injury, cardiovascular instability and increasing blood lactate levels not responding to treatment, and the specific antidote – hydroxycobalamin – should be given. A recent detailed review of inhalation injury is available from BJA Education.26
Fig 6.
Example of escharotomies performed to facilitate ventilation in a major chest burn (published with written consent from the patient).
Circulation
Burns and burn shock are not an immediate cause of hypovolaemia. Any haemodynamic instability must be assessed as possible bleeding in the first instance. Peripheral i.v. access may be difficult with limited sites available. Two large bore cannulas are necessary. Ideally, access is not placed through burned tissue but this may be unavoidable and if unable, intraosseous access must be gained before proceeding to definitive central venous access. The Parkland formula guides resuscitation fluids in the first 24 h for burns of >15% TBSA. The principles are as follows:
| Parkland formula: 2–4 ml × actual body weight (kg) × %TBSA burned |
-
–
From the time burn sustained
-
–
½ in first 8 h, ½ in subsequent 16 h
-
–
Subtract any fluid already given
-
–
Use warm, isotonic balanced crystalloid
The modified Parkland formula of 3 ml × actual body weight (kg) × %TBSA burns is advocated to limit excessive fluids being given. The amount of fluid actually given will need adjustment according to the evolving clinical picture as covered in Part 2 of this series.
Disability
Reduced Glasgow Coma Scale at presentation in major burns is not caused by the burn itself and must lead to a search for the cause and appropriate management. As described previously, these include poisoning by inhaled toxins (carbon monoxide and hydrogen cyanide); overdose; trauma including head injury and medical comorbidities leading to collapse.
Exposure and estimation of % TBSA burned
All clothing and jewellery must be removed; however, exposure of the patient must be kept to a minimum as almost all major burns patients become hypothermic. Erythema alone is not counted in the estimation of burn surface area. All areas of superficial partial thickness burn or deeper are included. Many management decisions including transfer decisions and prognosis are based on %TBSA burned, and overestimation of burned surface area leads to fluid overload. Traditional methods include the Lund and Browder chart or the Wallace Rule of Nines, but more recently the Mersey Burns app has gained popularity for ease of use and accuracy.28 Example output from the app can be seen in the recent BJA Education article on burns in paediatrics.1
Indications for escharotomy
Initial surgical management at the referring centre should be either life or limb saving. Escharotomies are surgical incisions through non-compliant full thickness burn, which restricts ventilation on the chest and abdomen or causes significantly reduced perfusion in circumferential burns to the limbs. Escharotomies to produce decompression should be performed as soon as they are required for ventilation or perfusion; the incision is longitudinal from unburned skin to unburned skin if possible, and deep enough to reach subcutaneous fat and release the eschar.29 Anaesthesia will be required, diathermy is usually used so blood loss should be minimal and prophylactic antibiotics should be given. Fasciotomy incisions are deeper than for escharotomies, through the subcutaneous tissue and the fascial layers surrounding the muscle compartments. They are most commonly indicated in high-voltage electrical burns where tissue necrosis of muscle causes compartment syndrome.
Secondary survey
Other common areas of injury in major burns include corneal damage and examination with fluorescein stain is required. Electrical burns are at risk of rhabdomyolysis, and a creatine kinase level should be measured. All major burn injuries should receive tetanus toxoid treatment. Pain relief using intravenous opioid titrated to effect should be given (if the patient is not already anaesthetised). Gastric decompression with a nasogastric tube should occur. Routine use of antibiotics is not required.
Criteria for referral to a specialist unit and initial management
The referral criteria to specialist burns services are available.30 All major burns will need referral and transfer to specialist services. Severe burns thought to be non-survivable should also be discussed as accurate estimation of burn size, site of donor areas, age and comorbidities are essential in making this decision, which is best done using the expertise of the burns centre.
Goals of transfer
Patients should be transferred as soon as they are resuscitated and stable, and with a secure airway noting that fluid resuscitation will cause burn oedema, which may worsen en route. If the patient's trachea is intubated, a nasogastric tube should also be inserted to decompress the stomach.27 If tracheal intubation is not indicated, the patient should be sat up as much as possible to offset the effects of developing oedema. Invasive monitoring is usually required, and lines must be secured with stitches. Provision for continuation of possible large volume fluid resuscitation during transfer together with consideration of vasopressor support is necessary. Active warming is required as patients will continue to lose heat and may become severely hypothermic and acidotic. Delaying transfer to try to warm an already hypothermic patient is often not effective, but decisions should be made on a case-by-case basis in conjunction with the specialist centre. Burn wounds should be dressed with cling film for transfer taking care to avoid circumferential application that might impair blood flow.27
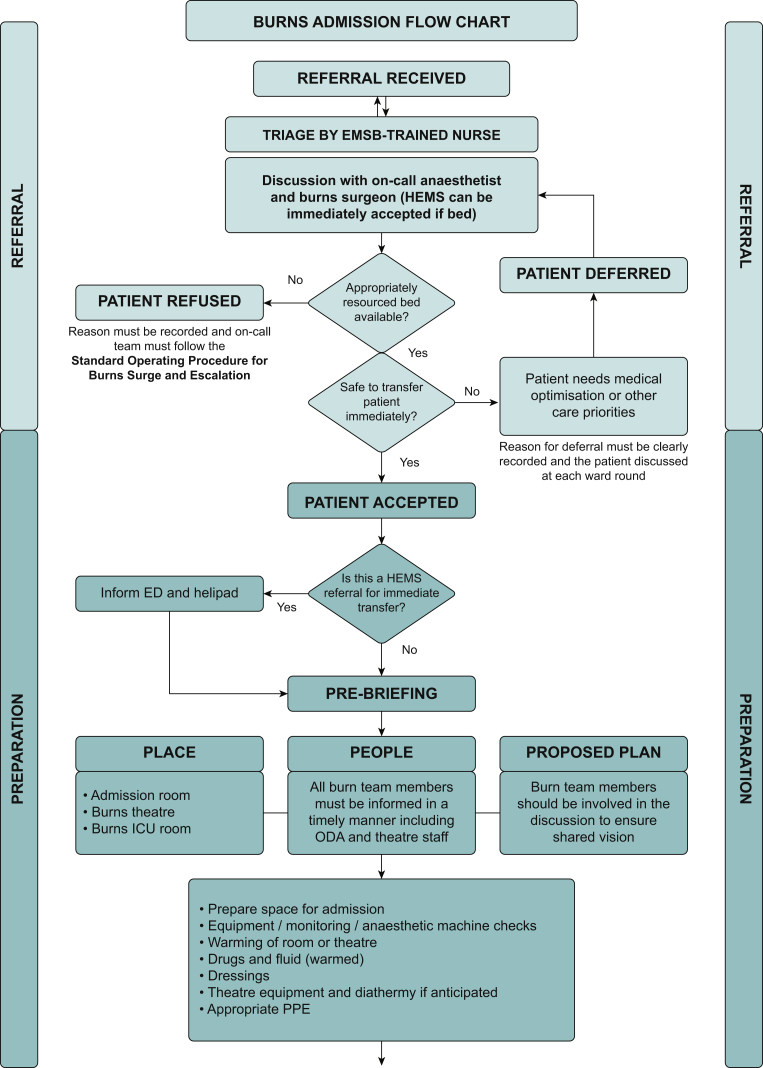
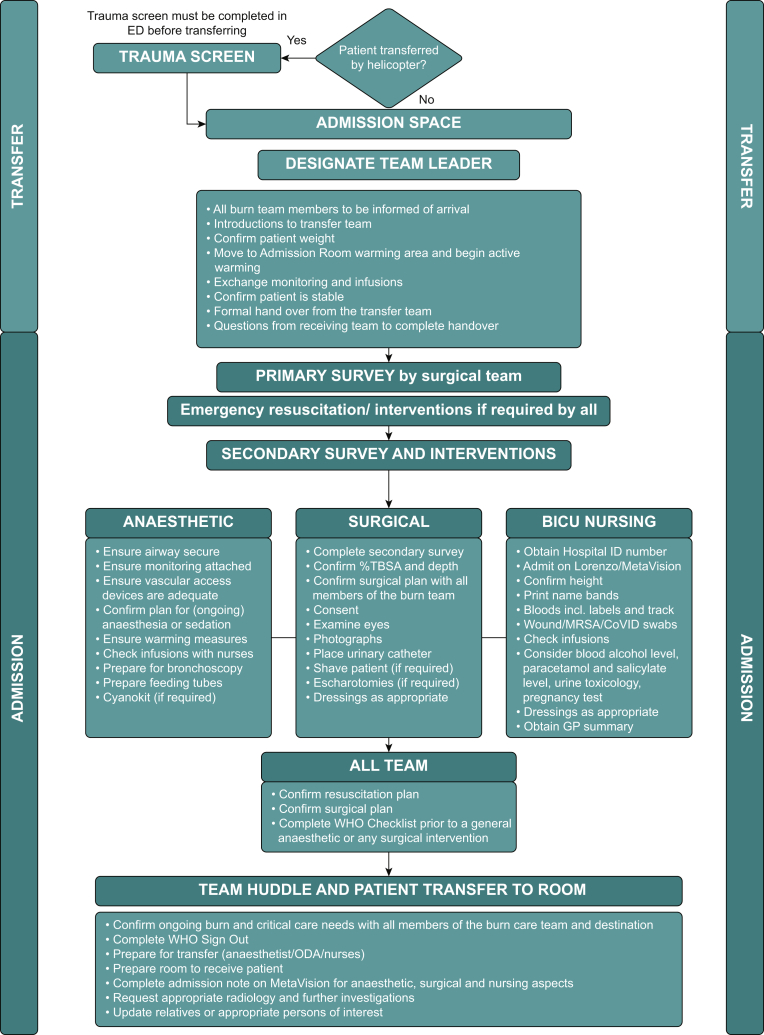
The admission protocol for major burns on arrival in our unit is outlined in Figure 7.
Fig 7.
Example admission room protocol in use at our institution. ED, emergency department; EMSB, emergency management of severe burns course; HEMS, helicopter emergency medical service; MRSA, methicillin-resistant Staphylococcus aureus; ODA, operating department assitant; PPE, personal protective equipment.
Early surgical management
Burns are a surgical disease; the wound must be debrided and deep partial thickness and full thickness burns require tissue excision and wound closure with skin grafts. Guidance suggests surgical removal of full thickness burns within 5 days.31 However the preferred practice at our institution is to perform total or near-total early burn wound excision in <48 h of injury with the aim of reducing the necrotic load of the burn wound that drives the systemic inflammatory response. Early wound excision has been shown to decrease blood loss, burn wound sepsis and length of stay. There is also a positive association with aesthetic and functional outcomes compared with the alternative treatment of serial excision or conservative management; however, available evidence is not yet conclusive on whether this technique offers improved survival outcomes.32, 33, 34 Once the burned tissue is excised, wound closure must be achieved to decrease fluid loss, prevent further wound desiccation and infection and reduce hypermetabolism. This can be either temporary covering with allograft (skin from organ donors) or synthetic skin substitutes, or permanent, with autologous split skin grafts. In general, autologous split skin grafts are the gold standard for treating burn wounds. The ability to cover all wounds permanently depends on the size of area requiring grafting and the availability of donor sites. Patients with a major burn undergo repeated operations and dressing changes and require multidisciplinary specialist care in ICU, which will be discussed in detail in a forthcoming article in this journal.17
Declaration of interests
The authors declare that they have no conflicts of interest.
Acknowledgements
The authors thank the London and South East Burn Network and the Dutch Burns Foundation for their kind permission in allowing the adaptation of illustrations for Fig. 2, Nederlandse Brandwonden Stichting.
MCQs
The associated MCQs (to support CME/CPD activity) will be accessible at www.bjaed.org/cme/home by subscribers to BJA Education.
Biographies
Claire McCannBMedSci MRCP FRCA FFICM is a speciality registrar in anaesthetics and clinical fellow in burns anaesthesia and intensive care at St Andrew's Centre for Burns and Plastic Surgery.
Agnes WatsonFRCA FFICM is a consultant in adult and paediatric burns and plastics anaesthesia and intensive care, St Andrew's Centre for Burns and Plastic Surgery. She is the outgoing college tutor for burns and plastics anaesthesia and has a special interest in anaesthesia for cleft lip and palate surgery.
David BarnesBMSc MSc FRCS Plast (Edin) is consultant and clinical lead for adult and paediatric burns surgery, St Andrew's Centre for Burns and Plastic Surgery. He is a previous chair of the London South East Burns Network and a member of the 2018 British Burn Care Standards panel.
Matrix codes: 1A01, 2A02, 3H00
References
- 1.Suman A., Owen J. Update on the management of burns in paediatrics. BJA Educ. 2020;20:103–110. doi: 10.1016/j.bjae.2019.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.James S.L., Lucchesi L.R., Bisignano C., et al. Epidemiology of injuries from fire, heat and hot substances: global, regional and national morbidity and mortality estimates from the Global Burden of Disease 2017 study. Inj Prev. 2020;26:i36–45. doi: 10.1136/injuryprev-2019-043299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organisation. Burns factsheets 2018. https://www.who.int/news-room/fact-sheets/detail/burns Available from:
- 4.National Health Service. Hospital episode statistics 2004 to 2009. England and Wales.
- 5.British Burn Association . National Burn Care Review Committee Report; 2001. Standards and strategy for burn care: a review of burn care in the British isles. [Google Scholar]
- 6.Gilhooly C.J., Kinsella J. Care of burns in Scotland: 3-year data from the managed clinical Network national registry. Crit Care. 2014;18:76. [Google Scholar]
- 7.International Burn Injury Database . Ad hoc report request; England: 2020. Adult resuscitation burns 2019/20 and causation covering 2019 to 2020 inclusive. [Google Scholar]
- 8.Peck M.D. Epidemiology of burns throughout the World: Part II. Intentional burns in adults. Burns. 2012;38:630–637. doi: 10.1016/j.burns.2011.12.028. [DOI] [PubMed] [Google Scholar]
- 9.Brusselaers N., Juhász I., Erdei I., et al. Evaluation of mortality following severe burns injury in Hungary: external validation of a prediction model developed on Belgian burn data. Burns. 2009;35:1009–1014. doi: 10.1016/j.burns.2008.12.017. [DOI] [PubMed] [Google Scholar]
- 10.Osler T., Glance L.G., Hosmer D.W. Simplified estimates of the probability of death after burn injuries: extending and updating the Baux score. J Trauma. 2010;68:690–697. doi: 10.1097/TA.0b013e3181c453b3. [DOI] [PubMed] [Google Scholar]
- 11.Roberts G., Lloyd M., Parker M., et al. The Baux score is dead. Long live the Baux score: a 27-year retrospective cohort study of mortality at a regional burns service. J Trauma Acute Care Surg. 2012;72:251–256. doi: 10.1097/TA.0b013e31824052bb. [DOI] [PubMed] [Google Scholar]
- 12.Belgian Outcome in Burn Injury Study Group Development and validation of a model for prediction of mortality in patients with acute burn injury. Br J Surg. 2009;96:111–117. doi: 10.1002/bjs.6329. [DOI] [PubMed] [Google Scholar]
- 13.Tobiasen J., Hiebert J.M., Edlich R.F. The abbreviated burn severity index. Ann Emerg Med. 1982;11:260–262. doi: 10.1016/s0196-0644(82)80096-6. [DOI] [PubMed] [Google Scholar]
- 14.Bloemsma G.C., Dokter J., Boxma H., et al. Mortality and causes of death in a burn centre. Burns. 2008;34:1103–1107. doi: 10.1016/j.burns.2008.02.010. [DOI] [PubMed] [Google Scholar]
- 15.Rockwood K., Theou O. Using the Clinical Frailty Scale in allocating scarce health care resources. Can Geriatr J. 2020;23:210–215. doi: 10.5770/cgj.23.463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Masud D., Norton S., Smailes S., et al. The use of a frailty scoring system for burns in the elderly. Burns. 2013;39:30–36. doi: 10.1016/j.burns.2012.03.002. [DOI] [PubMed] [Google Scholar]
- 17.McGovern C., Puxty K., Paton L. Major burns: Part 2. Anaesthesia, intensive care and pain management. BJA Educ. 2022 doi: 10.1016/j.bjae.2022.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jackson D.M. The diagnosis of the depth of burning. Br J Surg. 1953;40:588–596. doi: 10.1002/bjs.18004016413. [DOI] [PubMed] [Google Scholar]
- 19.Cuttle L., Kempf M., Liu P.Y., et al. The optimal duration and delay of first aid treatment for deep partial thickness burn injuries. Burns. 2010;36:673–679. doi: 10.1016/j.burns.2009.08.002. [DOI] [PubMed] [Google Scholar]
- 20.Greaves I., Porter K.M. CRC Press; Boca Raton, FL: 1999. Pre-hospital medicine: the principles and practice of immediate care. [Google Scholar]
- 21.British Burn Association . 2018. First aid clinical practice guidelines.https://www.britishburnassociation.org/wp-content/uploads/2017/06/BBA-First-Aid-Guideline-24.7.18.pdf Available from: [Google Scholar]
- 22.TOXBASE The primary clinical toxicology database of the National Poisons Information Service. https://www.toxbase.org/ Available from:
- 23.Waldmann V., Narayanan K., Combes N., et al. Electrical injury. Br Med J. 2017;357:j1418. doi: 10.1136/bmj.j1418. [DOI] [PubMed] [Google Scholar]
- 24.American College of Surgeons . 10th edition. 2018. Advanced trauma life support student course manual.https://viaaerearcp.files.wordpress.com/2018/02/atls-2018.pdf Available from: [Google Scholar]
- 25.British Burn Association. Emergency Management of the Severe Burn Course. Available from: https://www.britishburnassociation.org/emsb-courses/ (accessed 3 January 2021).
- 26.Gill P., Martin R.V. Smoke inhalation injury. BJA Educ. 2015;15:143–148. [Google Scholar]
- 27.Care of Burns in Scotland. Management of adult major burns: initial burns management standard operating procedure 2021. Available from: https://www.cobis.scot.nhs.uk/wp-content/uploads/2021/01/Initial-Burns-Management-SOP-1.png (7 accessed May 2021).
- 28.Barnes J., Duffy A., Hamnett N., et al. The Mersey Burns App: evolving a model of validation. Emerg Med J. 2015;32:637–641. doi: 10.1136/emermed-2013-203416. [DOI] [PubMed] [Google Scholar]
- 29.Butts C.C., Holmes J.H., IV, Carter J.E. Surgical escharotomy and decompressive therapies in burns. J Burn Care Res. 2019;41:263–269. doi: 10.1093/jbcr/irz152. [DOI] [PubMed] [Google Scholar]
- 30.British Burn Association . 2012. National burn care referral guidance.https://www.britishburnassociation.org/wp-content/uploads/2018/02/National-Burn-Care-Referral-Guidance-2012.pdf Available from: [Google Scholar]
- 31.British Burn Association . 1st edition. Burn Standards Review Group; London: 2018. National standards for provision and outcomes in adult and paediatric burn care. [Google Scholar]
- 32.Herndon D.N., Parks D.H. Comparison of serial debridement and autografting and early massive excision with cadaver skin overlay in the treatment of large burns in children. J Trauma. 1986;26:149–152. doi: 10.1097/00005373-198602000-00009. [DOI] [PubMed] [Google Scholar]
- 33.Herndon D.N., Barrow R.E., Rutan R.L., et al. A comparison of conservative versus early excision. Therapies in severely burned patients. Ann Surg. 1989;209:547–553. doi: 10.1097/00000658-198905000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dziewulski P. Annual scientific meeting Australian & New Zealand burn association; Perth. 2017. Total burn wound excision in major burn injury; two decades experience at St Andrew’s. [Google Scholar]