Abstract
Background
To compare the immediate effectiveness of low-level laser therapy (LLLT) applied to classical acupoints versus trigger points for patients with cervical myofascial pain syndrome (MPS).
Methods
This was a single-blinded, randomized, placebo-controlled trial. This study was performed in a university-affiliated medical center. One hundred participants with cervical myofascial pain syndrome were randomly allocated to four treatment groups, including (1) acupoint therapy (AcuT), (2) acupoint control (AcuC), (3) trigger point therapy (TriT), and (4) trigger point control (TriC) groups. Low-level laser (810-nm) therapy was used in both therapy groups, while the same procedure was performed without laser in the acupoint control groups. The patients were evaluated based on visual analogue scale (VAS) pain score, pressure pain threshold, and cervical range of motion (ROM) before and after the therapy.
Results
Immediate pain relief was observed in the TriT group (p < 0.01). The TriT group showed improved cervical ROM in ipsilateral bending (p < 0.01), while the AcuT group did not.
Conclusions
LLLT applied to trigger points could significantly relieve myofascial pain and was effective in relieving cervical ROM limitations. Considering the risk of pneumothorax, laser therapy at trigger points for patients with cervical MPS may be a choice when acupuncture therapy is unavailable.
Trial registration
ClinicalTrials.gov ID: NCT01516502.
Keywords: Laser therapy, Low level laser therapy, Myofascial pain syndrome, Acupoint, Trigger point, Range of motion
At a glance commentary.
Scientific background on the subject
Many people continue to suffer from myofascial pain syndrome. Laser therapy with a noninvasive and easy procedure has been used for the treatment of cervical myofascial pain syndrome. The purpose of this study is to compare the immediate effectiveness of laser therapy applying to trigger points and classical acupoints.
What this study adds to the field
This study offers another option to treat cervical myofascial pain syndrome. Considering the risk of pneumothorax, laser therapy at myofascial trigger points of cervical myofascial pain syndrome may be a choice when acupuncture therapy and trigger point needling are unavailable.
Many people continue to suffer from myofascial pain syndrome (MPS) with regional painful muscle spasm as well as particular referred pain pattern. Focal palpable taut bands and tender spots with local twitch responses (called myofascial trigger points (MTrPs)), are the two main clinical signs of MPS [[1], [2], [3]]. Other symptoms of MPS include range of motion (ROM) limitation, rapid exhaustion, and referred pain [4,5]. Patients with MPS begin with one active MTrP (called the primary MTrP) in the affected muscles due to chronic repetitive minor muscle strain, poor posture, systemic diseases, or neuromusculoskeletal lesions. When not treated correctly, expansion of the pain region and additional active MTrPs (called secondary or satellite MTrPs) will develop [3,6]. If they are not treated effectively, the pain often recurs later [7].
Traditional treatments for MPS include medication, stretching therapy, thermal treatment, electrical stimulation, massage, manipulation, and trigger point injection [3,7]. Hsieh et al. [8] have demonstrated the remote effect of MTrP needling on the referred pain and local twitch response elicited in the referred zone of the needling site. Ilbuldu et al. [9] applied He–Ne laser to three MTrPs in the upper trapezius muscles on both sides at 632.8 nm. They reported a significant decrease in pain at rest and with activity, as well as an increase in pain threshold in the laser group compared to dry needling and placebo laser groups.
Low-level laser therapy (LLLT) has the benefit of being a noninvasive, easy, and short-term procedure. LLLT has been used since the 1960s to treat neurological, musculoskeletal, and soft tissue disorders [10]. LLLT has also been used for the treatment of neck pain since 1981 [11], and has demonstrated significant reduction of pain intensity and improvement of cervical ROM in patients with cervical MPS [9,[12], [13], [14]]. However, Chou et al. [15] report that acupuncture needling to distal acupuncture points could also influence the subjective pain intensity and change endplate noise (EPN) amplitude in the MTrP region of the upper trapezius muscle. In addition, some studies suggest that the use of LLLT on acupoints has a similar effect to that induced by needle acupuncture on acupoints [[16], [17], [18]]. In this study, we investigated the immediate effectiveness of LLLT application to the local MTrP and distal classical acupoints in patients with cervical MPS.
Materials and methods
Subjects
We (rehabilitation doctors) enrolled participants who were diagnosed with cervical MPS of the upper trapezius muscles. The sample size was estimated by the software, G-power. We selected the one-way ANOVA test and gave an alpha error = 0.05 and a statistical power = 0.8. The effect size (0.51) was calculated based on a previous article [6] with equal sample size in the treatment and placebo groups (n = 31), mean = 3.11/5.79 and an overall standard deviation = 3.05. The estimated sample size was 22 in each group. Considering the 10% dropout rate, each group would have approximately 25 subjects. The study was conducted from February 2011 to February 2012. The primary diagnosis of cervical MPS was based on the following criteria: (1) complaints of regional pain in the neck, (2) presence of a palpable taut band, (3) presence of a tender spot along the length of the taut band, and (4) reproduction of the clinical symptoms by compression of the active trigger points [3]. Patients with significant clinical conditions other than MPS such as (1) cervical spine lesions, radiculopathy, or myelopathy, (2) fractures or cervical spinal surgery, (3) cervical spinal instability, and (4) cognitive deficits or psychiatric illness were excluded. The study was approved by the Human Studies Research Committee (approval number: 200900569B0D001). The clinical trial was registered on ClinicalTrials.gov (ID number: NCT01516502). Written informed consent was obtained from each participant.
Equipment
An infrared (low-level laser, class IIIb) gallium aluminum arsenide (Ga-Al-As) diode laser device with a wavelength of 810 nm (LaserPen Expert, RJ-LASER; Reimers & Janssen GmbH, Germany) and a maximum power output of 150 mW in the continuous wave mode was used for LLLT in the present study. The diameter of the laser probe is 0.5 cm and its maximum power density is 0.76 W/cm2. The device automatically generates the frequencies and energy of a laser beam according to the pre-determined settings of Reininger Meridian from RL-Laser Pen of Germany (ISO 13485:2012 + AC2012). The probe of the laser device was held perpendicularly to and slightly contacting the skin of participants during the treatment process. The same device and procedure were used for all participants but no laser beam was emitted for the placebo treatment (control groups).
Experimental design
The study used a parallel design, in which participants were equally allocated between the four groups. Participants were randomly assigned to one of the four groups: the acupoint therapy (AcuT) group, the acupoint control (AcuC) group, the trigger point therapy (TriT) group, and the trigger point control (TriC) group. We used a sequence generated by a computer randomization program (from another core laboratory) to ensure a balanced group assignment. A single-blinded design was used in which the allocation was blinded to the participant and physician, but not to the therapist and statistician. Allocation concealment was achieved using sealed envelopes. All participants eligible to participate were assessed by the same physician and treated by the same therapist. The physician conducted the processes of participant enrollment, allocation, and assessments. Before the treatment, participants' health information and baseline measurements including demographic data, affected side, and pain characteristics were recorded by the physician. The therapist, licensed to practice acupuncture and operating the low-level laser machine, was responsible for the localization of acupoints in the AcuT and AcuC groups and the application of LLLT in all four groups.
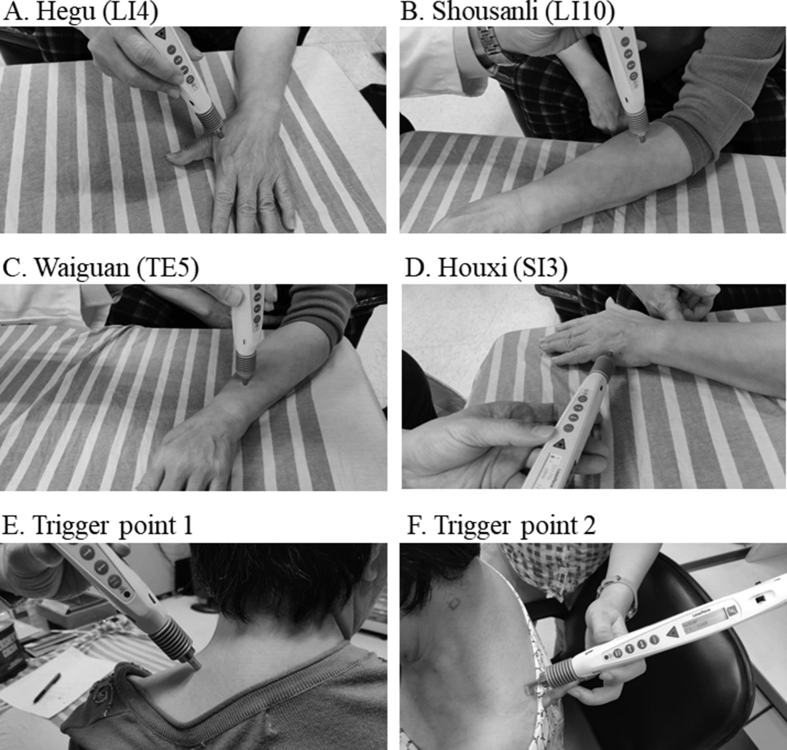
For the AcuT and AcuC groups, we selected the following four acupoints on the affected side: Shousanli (Large Intestine Meridians, LI 10), Hegu (Large Intestine Meridians, LI 4), Waiguan (Sanjiao Meridians, TE 5), and Houxi (Small Intestine Meridians, SI 3), which are commonly used in the treatment of cervical MPS [19,20] [Fig. 1. A, B, C, D]. Note that the four acupoints are distal and distant from the cervical region. In the AcuT group, LLLT was applied to the four aforementioned acupoints ipsilateral to the point of maximal pain. The laser frequencies for each acupoint were 553 Hz in LI Meridians, 791 Hz in SI3 and 731 Hz in TE5. At each acupoint, the laser was applied for 40 s, so that the energy density applied to each acupoint was 2 J/cm2 (the total energy density of the four acupoints: 8 J/cm2).
Fig. 1.
Acupoint and trigger point. The application of low-level laser therapy on acupoints (A, B, C, D) used in acupoint therapy group and proximal (E) or distal (F) trigger points used in trigger point therapy group.
For the TriT and TriC groups, participants were asked to indicate the point of maximal pain in the affected posterior-neck and upper-back regions. The most reliable and the minimal diagnostic criteria for myofascial trigger points of upper trapezius muscles include: (1) spot tenderness; (2) taut band; and (3) pain recognition. Confirmatory criteria include: (1) referred pain; and (2) local twitch response [21]. The physician checked the point according to the diagnostic criteria and then marked it with a pen. The major locations of the trigger point were illustrated in Fig. 1 (E and F). In the TriT group, the laser frequency for the trigger point was 583 Hz (the same frequency to the Gb meridian). LLLT was applied to the trigger point for 160 s so that the total energy density was 8 J/cm2. The study design reflected our attempt to make the total dosages for the AcuT and TriT groups equal (8 J/cm2), even though no evidence yet indicates that the effect of LLLT is proportional to its total energy.
Outcome measurements
We examined the immediate effects of LLLT using a before-after design in which the clinically relevant measurements were evaluated before and 15-min after laser application. The outcome measurements, which included objective pain scores using the visual analogue scale (VAS), pressure pain threshold at the trigger point, and cervical ROM, were performed by the same physician.
We evaluated the pressure pain threshold of the trigger point using an algometer (Wagner Instruments, USA), following the procedure of pressure pain threshold measurement proposed by Fischer [22]. The threshold was determined as the mean of the two last values out of three consecutive measurements, with a 10 s pause in between.
Active cervical ROM for three motion planes, including flexion-extension, bending, and rotation, were measured with the MicroFET3 electrogoniometer (Hoggan Health Industries, USA).
Calculation
The statistical analysis was conducted by a statistician using intention-to-treat analysis. The baseline and demographic characteristics were analyzed with the chi-square test for categorical data, and with the Kruskal–Wallis test for non-parametric data. The change ratios were calculated using the following formula: (before treatment value – after treatment value)/before treatment value. The median change ratios among the groups were compared using the Kruskal–Wallis test; post-hoc pair-wise comparisons were performed using the Dunn's test. Statistical significance was defined as p < 0.05.
Results
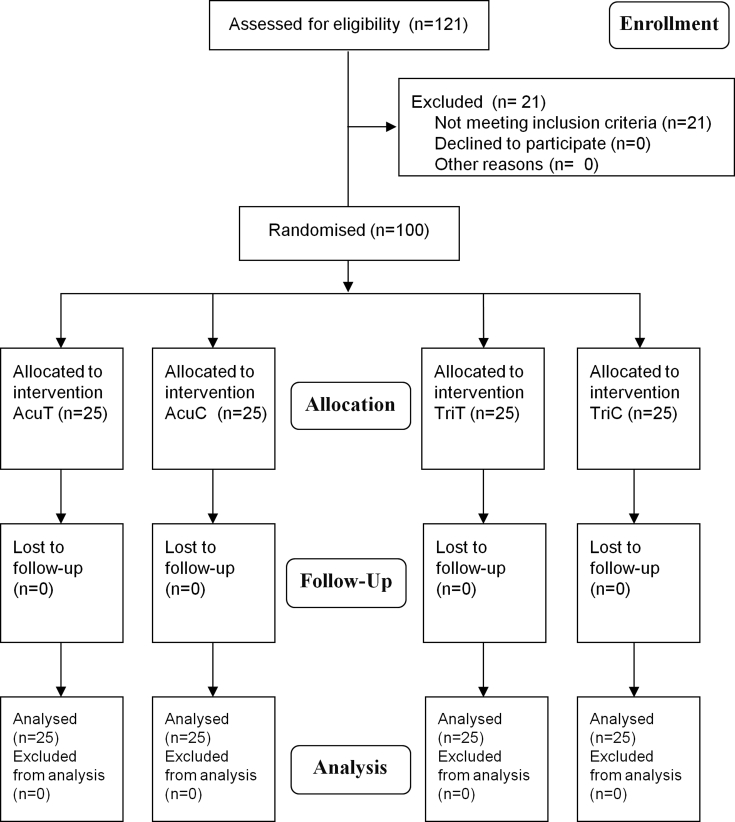
We enrolled 121 participants and twenty-one participants were excluded due to the lack of a palpable taut band despite the tenderness of their upper trapezius muscles. One hundred participants were analyzed in total (25 participants in each group) and all participants completed the entire study [Fig. 2]. (Consolidated Standards for Reporting Trials, CONSORT) Their ages ranged from 20 to 65 years (median, 25th∼75th percentiles: 32.0, 27.3–40.0 years). No adverse side effects were noted in the process of laser therapy. There was no difference between the four groups in terms of their demographic data [Table 1]. Comparisons of the baseline ROM between the four groups showed that ROM was comparable across the groups for most types of contralateral bending, extending, flexing, and bilateral rotating. However, we noticed differences in baseline ROM for ipsilateral bending (p = 0.03) between the four groups, and the post-hoc test showed a significant difference (p = 0.04) between the AcuT (42.0, 37.5–46.0) and TriT (36.0, 29.0–41.5) groups.
Fig. 2.
Flow diagram of this study. Flow diagram for participant enrollment, allocation, follow-up, and analysis (following the CONSORT guideline). Abbreviations used: AcuT: acupoint therapy group; AcuC: acupoint control group; TriT: trigger point therapy group; TriC: trigger point control group.
Table 1.
The demographic data and baseline evaluation〈number or median (25th-75th percentiles)〉for the four groups.
| Data | AcuT (n = 25) | AcuC (n = 25) | TriT (n = 25) | TriC (n = 25) | p value |
|---|---|---|---|---|---|
| Gender (female/male) | 23/2 | 22/3 | 21/4 | 22/3 | 0.59 |
| Age (year) | 31.0 (26.5–40.0) | 35.0 (26.5–40.5) | 33.0 (27.0–42.0) | 32.0 (28.0–35.5) | 0.90 |
| Body height (cm) | 159.0 (156.0–163.0) | 159.0 (157.0–164.0) | 159.0 (156.0–163.5) | 161.0 (153.0–164.0) | 0.75 |
| Body weight (kg) | 56.0 (50.0–63.0) | 56.0 (52.5–66.0) | 57.0 (54.5–68.0) | 55.0 (50.0–61.0) | 0.55 |
| Disease Duration (month) (1/2/>3 months) |
2/2/21 | 5/1/19 | 2/3/20 | 5/3/17 | 0.64 |
| Painful side (right/left/bilateral) | 8/2/15 | 3/7/15 | 4/6/15 | 9/4/12 | 0.25 |
| Pain VAS | 5.8 (3.6–6.8) | 5.0 (3.3–6.7) | 6.0 (4.8–7.2) | 5.7 (3.8–6.9) | 0.72 |
| Pressure pain threshold (kg/cm2) | 1.3 (1.2–2.1) | 1.5 (1.2–2.2) | 1.5 (1.3–2.3) | 1.4 (1.0–2.0) | 0.50 |
| Flexion ROM (°) | 54.0 (40.5–60.0) | 48.0 (39.0–63.5) | 50.0 (38.5–57.5) | 48.0 (43.0–58.5) | 0.95 |
| Extension ROM (°) | 60.0 (48.5–70.0) | 55.0 (48.0–65.0) | 50.0 (43.5–59.0) | 60.0 (50.0–68.0) | 0.14 |
| Ipsilateral bending ROM (°) | 42.0 (37.5–46.0) | 38.0 (31.5–48.0) | 36.0 (29.0–41.5) | 42.0 (37.0–46.0) | 0.03∗ |
| Contralateral bending ROM (°) | 42.0 (36.0–45.0) | 38.0 (30.5–46.5) | 37.0 (28.0–42.0) | 40.0 (36.5–45.5) | 0.13 |
| Ipsilateral rotation ROM (°) | 80.0 (64.5–86.0) | 80.0 (70.0–85.0) | 75.0 (58.5–82.0) | 78.0 (70.5–83.0) | 0.47 |
| Contralateral rotation ROM (°) | 79.0 (66.5–88.5) | 79.0 (71.5–86.0) | 78.0 (62.0–87.5) | 78.0 (69.5–85.5) | 0.98 |
All data are presented as number or median (25th-75th percentiles). Abbreviations: F: female; M: male; AcuT: acupoint therapy group; AcuC: acupoint control group; TriT: trigger point therapy group; TriC: trigger point control group; VAS: visual analogue scale; ROM: range of motion.
∗ p < 0.05.
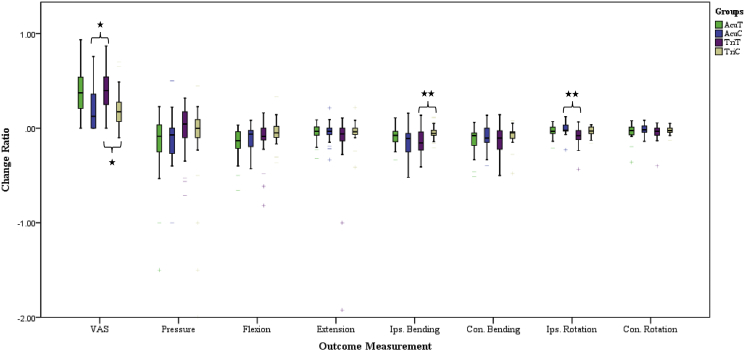
The Kruskal–Wallis test showed that the relative change in VAS (p < 0.01) and ROM (p < 0.01) scores for ipsilateral bending and ipsilateral rotation induced by LLLT differed significantly across the four groups, while changes in the other measurements, including pressure pain threshold, ROM in cervical flexion, extension, contralateral bending and contralateral rotation, did not differ significantly among the four groups (p > 0.05) [Table 2]. We then performed post-hoc analysis to compare the relative change in VAS between groups using the Dunn's test [Fig. 3]. For pain relief after LLLT of acupoint and trigger point, results showed that the change in VAS differed significantly between the TriT (0.40, 0.25–0.56) and the AcuC (0.13, 0.00–0.38) groups (p = 0.03), as well as between the TriT (0.40, 0.25–0.56) and TriC (0.17, 0.06–0.32) groups (p = 0.04) [Table 2]. There was a possible trend toward significance in the change in VAS between AcuT and AcuC groups (p = 0.08). There was no significant difference in VAS between AcuT and TriT group pairs (p > 0.05), indicating the comparable effectiveness of pain relief from applying LLLT to trigger points.
Table 2.
Comparison of treatment results〈change ratios, median (25th-75th percentile)〉between the four groups.
| AcuT |
AcuC |
TriT |
TriC |
p value | post hoc | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| After treatment | Change ratioa | After treatment | Change ratioa | After treatment | Change ratioa | After treatment | Change ratioa | |||
| Pain scale | ||||||||||
| VAS | 3.1 (1.7–5.4) | 0.38 (0.20–0.56) | 3.3 (2.5–5.6) | 0.13 (0.00–0.38) | 3.3 (2.4–4.6) | 0.40 (0.25–0.56) | 4.7 (2.6–6.2) | 0.17 (0.06–0.32) | <0.01∗∗ | bc∗,cd∗ |
| Pressure pain threshold | 1.5 (1.2–2.0) | −0.08 (−0.26–0.05) | 1.6 (1.3–2.3) | −0.07 (−0.28–0.03) | 1.5 (1.2–2.3) | 0.05 (−0.13–0.19) | 1.4 (1.1–1.7) | 0.00 (−0.15–0.10) | 0.19 | |
| ROM | ||||||||||
| Flexion | 57.0 (54.0–66.0) | −0.13 (−0.23–0.03) | 50.0 (45.5–68.0) | −0.06 (−0.20–0.02) | 52.0 (42.5–61.0) | −0.09 (−0.13–0.00) | 52.0 (45.5–60.0) | −0.05 (−0.11–0.03) | 0.19 | |
| Extension | 62.0 (53.0–69.0) | −0.03 (−0.01–0.02) | 62.0 (49.0–65.0) | −0.03 (−0.10–0.01) | 53.0 (47.0–65.5) | −0.06 (−0.14–0.01) | 62.0 (52.0–70.0) | −0.04 (−0.07–0.00) | 0.76 | |
| Ipsilateral bending | 44.0 (41.0–50.0) | −0.08 (−0.15–0.03) | 40.0 (36.5–48.5) | −0.11 (−0.25–0.02) | 40.0 (34.5–44.5) | −0.16 (−0.25–0.04) | 44.0 (38.0–48.0) | −0.05 (−0.08–0.01) | <0.01∗∗ | cd∗∗ |
| Contralateral bending | 46.0 (41.5–51.0) | −0.08 (−0.20–0.05) | 42.0 (36.5–49.0) | −0.11 (−0.21–0.00) | 38.0 (34.5–43.5) | −0.11 (−0.24–0.03) | 44.0 (38.0–48.0) | −0.05 (−0.11–0.02) | 0.37 | |
| Ipsilateral rotation | 78.0 (74.5–86.5) | −0.03 (−0.06–0.01) | 80.0 (70.0–84.5) | −0.02 (−0.04–0.04) | 80.0 (67.5–85.0) | −0.08 (−0.12–0.03) | 80.0 (74.5–86.0) | −0.03 (−0.07–0.01) | <0.01∗∗ | bc∗∗ |
| Contralateral rotation | 81.0 (69.0–90.5) | −0.03 (−0.07–0.02) | 77.0 (74.0–85.5) | −0.02 (−0.04–0.02) | 82.0 (66.0–92.0) | −0.03 (−0.08–0.00) | 80.0 (72.5–85.0) | −0.02 (−0.04–0.01) | 0.39 | |
∗ p < 0.05; ∗∗ p < 0.01.
Change ratio = (before – after)/before. Abbreviations: AcuT: acupoint therapy group; AcuC: acupoint control group; TriT: trigger point therapy group; TriC: trigger point control group; VAS: visual analogue scale; ROM: range of motion; bc: AcuC vs. TriT; cd: TriT vs. TriC.
Fig. 3.
Boxplot. The boxplots of change ratios between different groups for each outcome measurement. The median, 25th and 75th percentiles, and the significance of the post-hoc analysis in outcome measurement is shown for each of the four groups. Abbreviations used: AcuT: acupoint therapy group; AcuC: acupoint control group; TriT: trigger point therapy group; TriC: trigger point control group. ∗ p < 0.05; ∗∗ p < 0.01.
Post-hoc analysis for ROM in ipsilateral bending showed significant differences (p < 0.01) between the TriT (−0.16, −0.25∼−0.04) and TriC (−0.05, −0.08–0.01) groups, indicating that only LLLT to trigger points improved ipsilateral bending. Post-hoc analysis for ROM in ipsilateral rotation showed significant differences (p < 0.01) between the TriT (−0.08, −0.12∼−0.03) and AcuC (−0.02, −0.04–0.04) groups, implying that LLLT to trigger points was possible superior for improving ipsilateral rotation.
Discussion
In this randomized, single-blind, placebo-controlled study, we evaluated the use of LLLT (using an 810-nm, 150-mW laser) applied to acupoints and trigger points for the management of cervical MPS. The pain VAS and some types of cervical ROM immediately improved in the trigger point group. Moreover, trigger point therapy was also effective for improving ipsilateral cervical bending ROM and rotation ROM. In most of the studies on LLLT and cervical MPS, trigger points were chosen as the application area for LLLT [13,14,23]. Some studies evaluated the application of laser therapy to acupoints [24] or to both trigger points and acupoints [25] for cervical MPS. To the best of our knowledge, there is no existing work that compares the effectiveness of LLLT on trigger points and traditional acupoints. This study is the first to compare the effects between LLLT application to trigger points and to acupoints with the same total laser dosage. The rationales for choosing distal acupoints rather than local acupoints are as follows: (1) The distal acupuncture has been proven effective for relieving cervical myofascial pain [15,26,27]. (2) Local acupoints such as SI15 and GB21 may be near to the trigger points of the posterior-neck and upper-back regions, which may confound the comparison of the treatment outcome between acupoint and trigger point groups.
The efficacy of LLLT for pain reduction had been demonstrated by meta-analysis and systemic reviews [28,29]. The systemic effects of laser, including altering the endogenous analgesic mediators [30,31] and reducing afferent nociceptive input to the central nervous system (CNS) [16,17], have been reported. The systemic analgesic effect of LLLT does not fully account for the effect of specific distal acupoint on pain relief for MPS. Laser acupuncture is assumed to share similar effects with needle acupuncture [32], as proven by some studies reporting that laser acupuncture generates comparable effects in modulation of CNS activation to needle acupuncture [18,33]. Moreover, Litscher et al. found that laser irradiation of four visual-associated acupoints on limbs (LI4, ST36, Bl60 and Bl67) induced an increase signal in the visual cortex when visualized with functional magnetic resonance imaging [18]; Lorenzini et al. revealed that laser irradiation to acupoints associated to pain and inflammation (ST36 and TE5) reduced edema, hyperalgesia and spontaneous pain [34]; Erthal et al. reported that laser irradiation to ST36 elicited the antinociceptive effect mediated by activation of the opioidergic and serotonergic systems [35] and produced an anti-inflammatory effect by reduction of inflammatory mediators [36]. LLLT may actually stimulate the acupoints and thus induce the therapeutic effects of the specific acupoints. Taken together, these studies suggest the possible mechanism of LLLT on distal acupoints for treatment of MPS.
Many studies have demonstrated positive effects from LLLT application to trigger points in terms of reduction of pain intensity, alleviation of muscle stiffness, and improvement of disability scale [9,[12], [13], [14]]. Moreover, a double-blind placebo-controlled trial in which a pulsed infrared beam was applied to the four most painful muscular trigger points and five bilateral homometameric acupoints for treatment of cervical MPS showed significant pain attenuation in the treated group both at the end of therapy and in the 3-month follow-up examination [25]. According to our results, the effect of LLLT trigger point application seemed similar to acupoint application for pain reduction and improvement of cervical ROM in patients with cervical MPS, but only LLLT trigger point application significantly improved pain and cervical ROM compared to the control group. Local effects on the affected muscle might account for the superiority of LLLT trigger point application. A study for chronic myofascial pain syndrome stated that LLLT inhibited vasodilation and thus improved local circulation and reduced edema [13]. Another possible mechanism of LLLT on local muscle tissue is the reduction of oxidative stress and skeletal muscle fatigue. Studies have shown that laser irradiation before exercise can delay the onset of muscle fatigue and accelerate muscle recovery because LLLT inhibited the exercise-induced increase in creatine kinase and accelerated the removal of lactate [37,38]. The local effects of LLLT, including the improvement of local circulation and reduction of muscle fatigue, may enhance the flexibility and contraction of the affected upper trapezius muscle. These mechanisms could explain the improvement of cervical ROM in patient with trigger point LLLT.
Numerous articles have reported conflicting results for LLLT application to acupoints to reduce pain in treatment of temporomandibular joint disorder, lateral epicondylitis, low back pain, knee osteoarthritis, and MPS [[39], [40], [41], [42], [43], [44], [45], [46], [47]]. The inconsistent effectiveness may be caused by variation in patient groups, treatment protocols, laser therapy parameters, and duration of follow-up [48,49]. Among these studies, only one article actually applied LLLT to acupoints to treat MPS and compare the effectiveness between treatment and placebo [24]. The researchers found no significant difference between groups. The result seemed to be analogous to our study but further studies are needed to determine the effectiveness of LLLT on acupoints for pain reduction in MPS.
Acupuncture therapy has been widely used to treat patients for more than 2500 years. In addition to classical and extraordinary acupoints, Ashi point was described by an ancient Chinese physician, Dr. SM Sun (AC 584–682). When patients feel a strong withdrawal response (the jump sign) to palpation of such a hyperirritable point, they respond by saying “Ashi yes, this is the trigger point.” Ashi points have the extremely similar characteristics and locations that as the trigger points associated with myofascial pain syndrome (MTrP) [6,50,51], but were discovered independently and labeled differently [6,52]. Kawakita & Okada [53] found that polymodal receptors are the key to pain control when acupuncture and moxibustion are applied to the acupoint/trigger points.
Our study has some limitations. We excluded participants with cervical spine lesions, radiculopathy, or myelopathy. Imaging data was not obtained to confirm the diagnosis. The present study did not focus on the long-term effects of LLLT and therefore the results can only be applied to the immediate effects of LLLT. Also, the dosage effect of LLLT to distal acupoints needs to be addressed in future researches.
Conclusion
This study demonstrates that the Ga-Al-As laser (with a wavelength of 810 nm and a maximum power output of 150 mW) is an effective therapeutic option for immediately relief from cervical MPS, while the sham laser did not have this effect. Significant pain improvement was noted only after LLLT was applied to MTrP. Pain relief occurred 15 min after a single treatment and relieved cervical ROM limitations for ipsilateral bending. Considering the risk of pneumothorax, laser therapy at MTrP for patients with cervical MPS may be a choice when acupuncture therapy is unavailable.
Formatting of funding sources
This research was supported in part by the Chang Gung Medical Foundation (Grant Numbers CMRPG5E0081∼83), and by Healthy Aging Research Center and the Taiwan Ministry of Education's Higher Education Deep Plowing Program (Grant Numbers EMRPD1K0391 and EMRPD1K0481). Grants provide personnel and consumables and the support for data analysis. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflicts of interest
We certify that no party having a direct interest in the results of the research supporting this article has or will confer a benefit on us or on any organization with which we are associated and, if applicable, we certify that all financial and material support for this research (eg, NIH or NHS grants) and work are clearly identified in the title page of the manuscript.
Acknowledgements
The protocol is also funded by the corresponding author, Alice MK Wong.
Footnotes
Peer review under responsibility of Chang Gung University.
References
- 1.Melzack R. Myofascial trigger points: relation to acupuncture and mechanisms of pain. Arch Phys Med Rehabil. 1981;62:114–117. [PubMed] [Google Scholar]
- 2.Baldry P. Superficial dry needling at myofascial trigger point sites. J Musculoskel Pain. 1995;3:117–126. [Google Scholar]
- 3.Simons D.G., Travell J.G., Simons L.S. 2. vol. 1. Lippincott Williams & Wilkins; Baltimore: 1999. (Travell & Simons' myofascial pain and dysfunction: the trigger point manual). [Google Scholar]
- 4.Rachlin E.S. Mosby; St. Louis: 1994. History and physical examination for regional myofascial pain syndrome. Myofascial pain and fibromyalgia: trigger point management; pp. 159–172. [Google Scholar]
- 5.Simons D.G. Mosby; St. Louis: 1988. Myofascial pain syndrome due to trigger points. [Google Scholar]
- 6.Hong C.Z. Myofascial trigger points: pathophysiology and correlation with acupuncture points. Acupunct Med. 2000;18:41–47. [Google Scholar]
- 7.Hong C.Z. Treatment of myofascial pain syndrome. Curr Pain Headache Rep. 2006;10:345–349. doi: 10.1007/s11916-006-0058-3. [DOI] [PubMed] [Google Scholar]
- 8.Hsieh Y.L., Kao M.J., Kuan T.S., Chen S.M., Chen J.T., Hong C.Z. Dry needling to a key myofascial trigger point may reduce the irritability of satellite MTrPs. Am J Phys Med Rehabil. 2007;86:397–403. doi: 10.1097/PHM.0b013e31804a554d. [DOI] [PubMed] [Google Scholar]
- 9.Ilbuldu E., Cakmak A., Disci R., Aydin R. Comparison of laser, dry needling, and placebo laser treatments in myofascial pain syndrome. Photomed Laser Ther. 2004;22:306–311. doi: 10.1089/pho.2004.22.306. [DOI] [PubMed] [Google Scholar]
- 10.Basford J.R. Low-energy laser therapy: controversies and new research findings. Laser Surg Med. 1989;9:1–5. doi: 10.1002/lsm.1900090103. [DOI] [PubMed] [Google Scholar]
- 11.Chow R.T., Barnsley L. Systematic Review of the literature of low-level laser therapy (LLLT) in the management of neck pain. Laser Surg Med. 2005;37:46–52. doi: 10.1002/lsm.20193. [DOI] [PubMed] [Google Scholar]
- 12.Simunovic Z. Low level laser therapy with trigger points technique: a clinical study on 243 patients. J Clin Laser Med Surg. 1996;14:163–167. doi: 10.1089/clm.1996.14.163. [DOI] [PubMed] [Google Scholar]
- 13.Gur A., Sarac A.J., Cevik R., Altindag O., Sarac S. Efficacy of 904 nm gallium arsenide low level laser therapy in the management of chronic myofascial pain in the neck: a double-blind and randomize-controlled trial. Laser Surg Med. 2004;35:229–235. doi: 10.1002/lsm.20082. [DOI] [PubMed] [Google Scholar]
- 14.Chow R.T., Heller G.Z., Barnsley L. The effect of 300mW, 830nm laser on chronic neck pain: a double-blind, randomized, placebo-controlled study. Pain. 2006;124:201–210. doi: 10.1016/j.pain.2006.05.018. [DOI] [PubMed] [Google Scholar]
- 15.Chou L.W., Hsieh Y.L., Kao M.J., Hong C.Z. Remote influences of acupuncture on the pain intensity and the amplitude changes of endplate noise in the myofascial trigger point of the upper trapezius muscle. Arch Phys Med Rehabil. 2009;90:905–912. doi: 10.1016/j.apmr.2008.12.020. [DOI] [PubMed] [Google Scholar]
- 16.Tsuchiya K., Kawatani M., Takeshige C., Matsumoto I. Laser irradiation abates neuronal responses to nociceptive stimulation of rat-paw skin. Brain Res Bull. 1994;34:369–374. doi: 10.1016/0361-9230(94)90031-0. [DOI] [PubMed] [Google Scholar]
- 17.Tsuchiya K., Kawatani M., Takeshige C., Sato T., Matsumoto I. Diode laser irradiation selectively diminishes slow component of axonal volleys to dorsal roots from the saphenous nerve in the rat. Neurosci Lett. 1993;161:65–68. doi: 10.1016/0304-3940(93)90141-7. [DOI] [PubMed] [Google Scholar]
- 18.Litscher G., Rachbauer D., Ropele S., Wang L., Schikora D., Fazekas F., et al. Acupuncture using laser needles modulates brain function: first evidence from functional transcranial Doppler sonography and functional magnetic resonance imaging. Laser Med Sci. 2004;19:6–11. doi: 10.1007/s10103-004-0291-0. [DOI] [PubMed] [Google Scholar]
- 19.Kreisel V., Weber M. Fuchtenbusch; 2012. A practical handbook: laser acupuncture - successful treatment concepts. [Google Scholar]
- 20.Chung C. Taiwan: Chen Kwan Book Co.; 1985. Handbook of acupuncture prescription. Chinese. [Google Scholar]
- 21.Hong C.Z., Simons D.G. Pathophysiologic and electrophysiologic mechanisms of myofascial trigger points. Arch Phys Med Rehabil. 1998;79:863–872. doi: 10.1016/s0003-9993(98)90371-9. [DOI] [PubMed] [Google Scholar]
- 22.Fischer A.A. Pressure algometry over normal muscles. Standard values, validity and reproducibility of pressure threshold. Pain. 1987;30:115–126. doi: 10.1016/0304-3959(87)90089-3. [DOI] [PubMed] [Google Scholar]
- 23.Dundar U., Evcik D., Samli F., Pusak H., Kavuncu V. The effect of gallium arsenide aluminum laser therapy in the management of cervical myofascial pain syndrome: a double blind, placebo-controlled study. Clin Rheumatol. 2007;26:930–934. doi: 10.1007/s10067-006-0438-4. [DOI] [PubMed] [Google Scholar]
- 24.Waylonis G., Wilke S., O’toole D., Waylonis D., Waylonis D. Chronic myofascial pain: management by low-output helium-neon laser therapy. Arch Phys Med Rehabil. 1988;69:1017–1020. [PubMed] [Google Scholar]
- 25.Ceccherelli F., AltafiniL L., Castro G.L., Avila A., Ambrosio F., Giron G. Diode laser in cervical myofascial pain: a double-blind study versus placebo. Clin J Pain. 1989;5:301–304. doi: 10.1097/00002508-198912000-00005. [DOI] [PubMed] [Google Scholar]
- 26.Chou L.W., Kao M.J., Lin J.G. Probable mechanisms of needling therapies for myofascial pain control. Evid base Compl Alternative Med. 2012;2012:705327. doi: 10.1155/2012/705327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Irnich D., Behrens N., Gleditsch J.M., Stör W., Schreiber M.A., Schöps P., et al. Immediate effects of dry needling and acupuncture at distant points in chronic neck pain: results of a randomized, double-blind, sham-controlled crossover trial. Pain. 2002;99:83–89. doi: 10.1016/s0304-3959(02)00062-3. [DOI] [PubMed] [Google Scholar]
- 28.Enwemeka C.S., Parker J.C., Dowdy D.S., Harkness E.E., Harkness L.E., Woodruff L.D. The efficacy of low-power lasers in tissue repair and pain control: a meta-analysis study. Photomed Laser Ther. 2004;22:323–329. doi: 10.1089/pho.2004.22.323. [DOI] [PubMed] [Google Scholar]
- 29.Bjordal J.M., Couppé C., Chow R.T., Tunér J., Ljunggren E.A. A systematic review of low level laser therapy with location-specific doses for pain from chronic joint disorders. Aust J Physiother. 2003;49:107–116. doi: 10.1016/s0004-9514(14)60127-6. [DOI] [PubMed] [Google Scholar]
- 30.Hagiwara S., Iwasaka H., Hasegawa A., Noguchi T. Pre-irradiation of blood by gallium aluminum arsenide (830 nm) low-level laser enhances peripheral endogenous opioid analgesia in rats. Anesth Analg. 2008;107:1058–1063. doi: 10.1213/ane.0b013e31817ee43e. [DOI] [PubMed] [Google Scholar]
- 31.Ceylan Y., Hizmetli S., Siliğ Y. The effects of infrared laser and medical treatments on pain and serotonin degradation products in patients with myofascial pain syndrome. A controlled trial. Rheumatol Int. 2004;24:260–263. doi: 10.1007/s00296-003-0348-6. [DOI] [PubMed] [Google Scholar]
- 32.Whittaker P. Laser acupuncture: past, present, and future. Laser Med Sci. 2004;19:69–80. doi: 10.1007/s10103-004-0296-8. [DOI] [PubMed] [Google Scholar]
- 33.Siedentopf C.M., Koppelstaetter F., Haala I.A., Haid V., Rhomberg P., Ischebeck A., et al. Laser acupuncture induced specific cerebral cortical and subcortical activations in humans. Laser Med Sci. 2005;20:68–73. doi: 10.1007/s10103-005-0340-3. [DOI] [PubMed] [Google Scholar]
- 34.Lorenzini L., Giuliani A., Giardino L., Calza L. Laser acupuncture for acute inflammatory, visceral and neuropathic pain relief: an experimental study in the laboratory rat. Res Vet Sci. 2010;88:159–165. doi: 10.1016/j.rvsc.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 35.Erthal V., Da Silva M.D., Cidral-Filho F.J., Santos A.R.S., Nohama P. ST36 laser acupuncture reduces pain-related behavior in rats: involvement of the opioidergic and serotonergic systems. Laser Med Sci. 2013;28:1345–1351. doi: 10.1007/s10103-012-1260-7. [DOI] [PubMed] [Google Scholar]
- 36.Erthal V., Maria-Ferreira D., de Paula Werner M.F., Baggio C.H., Nohama P. Anti-inflammatory effect of laser acupuncture in ST36 (Zusanli) acupoint in mouse paw edema. Laser Med Sci. 2016;31:315–322. doi: 10.1007/s10103-015-1845-z. [DOI] [PubMed] [Google Scholar]
- 37.Junior E.C.P.L., Lopes-Martins R.Á.B., Vanin A.A., Baroni B.M., Grosselli D., De Marchi T., et al. Effect of 830 nm low-level laser therapy in exercise-induced skeletal muscle fatigue in humans. Laser Med Sci. 2009;24:425–431. doi: 10.1007/s10103-008-0592-9. [DOI] [PubMed] [Google Scholar]
- 38.Junior E.C.P.L., Lopes-Martins R.Á.B., Baroni B.M., De Marchi T., Taufer D., Manfro D.S., et al. Effect of 830 nm low-level laser therapy applied before high-intensity exercises on skeletal muscle recovery in athletes. Laser Med Sci. 2009;24:857–863. doi: 10.1007/s10103-008-0633-4. [DOI] [PubMed] [Google Scholar]
- 39.Acosta-Olivo C., Siller-Adame A., Tamez-Mata Y., Vilchez-Cavazos F., Peña-Martinez V. Laser treatment on acupuncture points improves pain and wrist functionality in patients undergoing rehabilitation therapy after wrist bone fracture. A randomized, controlled, blinded study. Acupunct Electro-Therapeut Res. 2017;42:11–25. doi: 10.3727/036012917x14908026365007. [DOI] [PubMed] [Google Scholar]
- 40.Helianthi D.R., Simadibrata C., Srilestari A., Wahyudi E.R., Hidayat R. Pain reduction after laser acupuncture treatment in geriatric patients with knee osteoarthritis: a randomized controlled trial. Acta Med Indones. 2016;48:114–121. [PubMed] [Google Scholar]
- 41.Shin J.Y., Ku B., Kim J.U., Lee Y.J., Kang J.H., Heo H., et al. Short-term effect of laser acupuncture on lower back pain: a randomized, placebo-controlled, double-blind trial. Evid base Compl Alternative Med. 2015;2015:808425. doi: 10.1155/2015/808425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Huang Y.F., Lin J.C., Yang H.W., Lee Y.H., Yu C.H. Clinical effectiveness of laser acupuncture in the treatment of temporomandibular joint disorder. J Formos Med Assoc. 2014;113:535–539. doi: 10.1016/j.jfma.2012.07.039. [DOI] [PubMed] [Google Scholar]
- 43.Glazov G., Yelland M., Emery J. Low-dose laser acupuncture for non-specific chronic low back pain: a double-blind randomised controlled trial. Acupunct Med. 2014;32:116–123. doi: 10.1136/acupmed-2013-010456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ferreira L.A., de Oliveira R.G., Guimarães J.P., Carvalho A.C.P., De Paula M.V.Q. Laser acupuncture in patients with temporomandibular dysfunction: a randomized controlled trial. Laser Med Sci. 2013;28:1549–1558. doi: 10.1007/s10103-013-1273-x. [DOI] [PubMed] [Google Scholar]
- 45.Glazov G., Schattner P., Lopez D., Shandley K. Laser acupuncture for chronic non-specific low back pain: a controlled clinical trial. Acupunct Med. 2009;27:94–100. doi: 10.1136/aim.2009.000521. [DOI] [PubMed] [Google Scholar]
- 46.Haker E., Lundeberg T. Laser treatment applied to acupuncture points in lateral humeral epicondylalgia. A double-blind study. Pain. 1990;43:243–247. doi: 10.1016/0304-3959(90)91078-W. [DOI] [PubMed] [Google Scholar]
- 47.Haker E.H., Lundeberg T.C. Lateral epicondylalgia: report of noneffective midlaser treatment. Arch Phys Med Rehabil. 1991;72:984–988. [PubMed] [Google Scholar]
- 48.Chon T.Y., Mallory M.J., Yang J., Bublitz S.E., Do A., Dorsher P.T. Laser acupuncture: a concise review. Med Acupunct. 2019;31:164–168. doi: 10.1089/acu.2019.1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Law D., McDonough S., Bleakley C., Baxter G.D., Tumilty S. Laser acupuncture for treating musculoskeletal pain: a systematic review with meta-analysis. J Acupunct Meridian Stud. 2015;8:2–16. doi: 10.1016/j.jams.2014.06.015. [DOI] [PubMed] [Google Scholar]
- 50.Dorsher P.T., Fleckenstein J. Trigger points and classical acupuncture points: part 1: qualitative and quantitative anatomic correspondences. Dtsch Z Akupunkt. 2008;51:15–24. [Google Scholar]
- 51.Liu L., Skinner M.A., McDonough S.M., Baxter G.D. Traditional Chinese Medicine acupuncture and myofascial trigger needling: the same stimulation points? Compl Ther Med. 2016;26:28–32. doi: 10.1016/j.ctim.2016.02.013. [DOI] [PubMed] [Google Scholar]
- 52.Hsu T.H., Chou S.W., Leong C.P., Wong P.Y., Wang C.M., Wong A.M. The immediate effects of oblique acupuncture in myofascial pain syndrome: evidence of improvement in physical parameters and of size change in the trapezius muscle. Taiwan J Phys Med Rehabil. 2003;31:13–20. [Google Scholar]
- 53.Kawakita K., Okada K. Mechanisms of action of acupuncture for chronic pain relief–polymodal receptors are the key candidates. Acupunct Med. 2006;24:58–66. [Google Scholar]