Abstract
Background. Ankle fractures are some of the most common injuries seen in the emergency department. Malunited ankle fractures are uncommon. Patients with malunion frequently present with multiple complaints. Radiographs often show abnormalities in anatomical alignment. Aim. To evaluate the anatomical alignment on radiographic imaging in patients with malunited ankle fractures. Secondary aims were to evaluate patient satisfaction after reconstruction and to investigate the relationships between radiological alignment and functional outcome. Methods. All consecutive patients (n = 25) treated for a fibula malunion between January 1, 2002, and September 1, 2017, were included. The primary outcome was anatomical alignment of the ankle mortise. The talocrural angle (TCA), talar tilt (TT), and medial clear space (MCS) were used to investigate to what extent revision surgery had improved alignment. The patient-related outcome measure consisted of the Olerud and Molander Ankle Score (OMAS). To assess quality of life (QoL) the EQ-5D-5L was used. Results. The median TCA was 78.4° before revision and 79.25° after revision; P = .297. The median TT was 2.95° before revision and 0.70° after; P < .001. The MCS before revision was 5.2 mm and 3.17 mm after; P < .000). The OMAS had a median of 67.5 points. Analysis of the QoL questionnaires yielded a score of 0.84 points. Conclusion. Anatomical alignment improves significantly after revision surgery of malunited ankles. Measurements of the TCA appeared less useful in determining the anatomical alignment. In our series, 60% of patients reported good to excellent results. The QoL scores of our patient were comparable to those in the healthy population in the Netherlands.
Levels of Evidence: Level IV: Case series
Keywords: ankle, fracture, malunion, revision, alignment
“Malunion of the fibula is the most common and the most difficult type of ankle malunion to reconstruct.”
Introduction
Ankle fractures are some of the most common injuries seen in the emergency department. In the Netherlands, the incidence is estimated to be 25 000 ankle fractures a year and has been increasing over the past 25 years. Hospital admission for an ankle fracture increased from 33/100 000 in 1986 to 62/100 000 in 2010, 1 which is comparable with that in other European countries, such as Sweden. 2
Functional recovery has been associated with the restoration of anatomical alignment and joint stability. 3 In the case of an ankle fracture with a nonanatomical position, a reduction (closed or open) is necessary to restore anatomical alignment. If this alignment cannot be maintained in a cast, an open reduction and internal fixation is necessary to ensure stability. During surgery, the typical radiographic landmarks are assessed, including Shenton’s line, dime sign, and Weber’s nose to ensure an anatomical reduction. Consolidation in a nonanatomical position could lead to biomechanical changes and, subsequently, to early posttraumatic ankle arthritis.4-6 Ramsey and Hamilton, 4 for example, described that lateral displacement of the talus resulted in poor functional outcome. However, during surgical treatment, an anatomical reduction is not always achieved, resulting in a malunion of the ankle.
Malunited ankle fractures are uncommon, illustrated by a review of the literature, which shows a limited number of series with an overall small number of patients. 7 Patients with a malunion of the ankle often present with persistent and disabling symptoms of pain, swelling, and stiffness of the ankle. Radiographs often shown abnormalities in anatomical alignment. 8
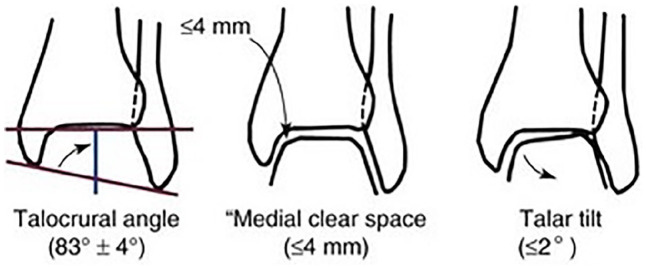
Malunion of the fibula is the most common and the most difficult type of ankle malunion to reconstruct. 9 A malunion of the fibula is typically shortened and usually associated with malrotation. Lengthening of the fibula via a fibular osteotomy, and thereby restoration of anatomical alignment, is the key to solve malunion. Radiographic imaging of the ankle is used to assess this alignment, often using radiographic parameters like medial clear space (MCS), talocrural angle (TCA), and talar tilt (TT).3,10
The aim of this study was to evaluate the anatomical alignment on radiographic imaging before and after revision osteotomy in patients with fibula malunion. Secondary aims were to evaluate patient satisfaction after reconstruction and to investigate the relationships between radiological alignment and functional outcome. We hypothesized that there would be a correlation between the radiological alignment and functional outcome.
Methods
Patient Identification and Data Collection
In this retrospective case series, all consecutive patients treated for a malunion of the fibula between January 1, 2002, and September 1, 2017 at our institution were included. Patients were identified by using the surgical code (338611) correlated with the operative treatment of “malleolar ankle or luxation fractures” or “fibula osteotomy,” in the electronic patient database. We included all adult patients older than 17 years at the time of surgery, who underwent subsequent revision osteotomy in case of a malunited ankle fracture. A malunited ankle was defined if a 2-mm shortening of the fibula was seen with an increase of 2 mm of the MCS (cutoff 4 mm) on the plain radiographs. A malunion was often accompanied with a valgus position on weight-bearing radiographs or TT in non–weight-bearing radiographs. Patients were excluded if they objected to the use of their medical records. We invited patients to fill in 2 questionnaires in January 2018. The study was approved by the institution’s Internal Review Board.
Surgical Technique
The patient was in a supine position on a radiolucent table, with a tourniquet in place but not inflated. The fibula was approached via a lateral incision, and if necessary, implants were removed. Under fluoroscopy, the ankle was pushed into the medial gutter. If there was too much widening at the MCS, a small anteromedial incision was made to remove any scar tissue from the medial joint. Depending on whether or not a rotation needed addressing as well, the type of osteotomy was chosen. This could be either an oblique Weber B like osteotomy, or a straight, low Weber C like osteotomy, or a Z-shaped osteotomy. A small distraction device was mounted on the distal tip of the fibula and above the osteotomy. Distraction was provided until the talus shifted back into place. Either a 2.7- or 3.5-mm locking plate was used. Often 1 or 2 syndesmotic positioning screws were used to provide additional stability of the construct (Figures 1 and 2). After the surgery, a below-knee cast was used, with 3 to 4 weeks of non–weight bearing and 3 to 4 weeks of weight bearing.
Figure 1.
Fibula lengthening via Weber B type osteotomy and 2.7-mm plate fixation.
Figure 2.
Z-shaped fibula osteotomy.
Baseline data collected from digital patient records were as follows: patient characteristics (ie, gender, age at the time of surgery and follow-up), fracture characteristics (ie, fracture type according to Weber 11 and number of fractured malleoli according to Potts 12 classification and fracture side), and surgical characteristics (ie, initial treatment, time between initial treatment and revision surgery, wound infections, and type of fibular osteotomy).
Outcome Measurements
The primary outcome was the anatomical alignment of the ankle mortise. Standard radiographs included lateral and mortise views. The TCA ( reference 83° ± 4°), TT (reference ≤ 2°), and MCS (reference ≤ 4 mm) were used to investigate to what extent revision surgery had improved alignment (Figure 3). All measurements were performed using conventional radiographs taken before revision surgery (the last available radiograph before revision surgery was used) and after revision surgery (the first available radiograph after revision surgery was used). Previously, surgery was performed based on conventional imaging, whereas the current treatment protocol from the past few years has included a CT scan and standardized radiographs of both ankles.
Figure 3.
Radiographic measurements. 28
Our secondary aim was to investigate patient functional outcome, satisfaction, and general quality of life (QoL). The patient-related outcome measure consisted of the Olerud and Molander Ankle Score (OMAS) for functional outcome. 13 The response scales vary from binary to 5 points, with clinical scoring that reflects the level of disability for individual items. Item responses are added up to form a score from 0 to 100, with higher scores representing the best possible scenario. For the QoL assessment, the EQ-5D-5L was used. 14 Both scoring systems have been validated previously.15,16
Statistical Analysis
Statistical analysis was performed using IBM SPSS Statistics for Windows, Version 24.0 (IBM Corp, Armonk, NY). Descriptive statistics were used to describe baseline characteristics, radiological measurements, OMAS, and QoL. The radiological measurements were evaluated for normality using the Shapiro-Wilk test and Q-Q plots. If normally distributed, these measurements were analyzed by a paired-samples t-test. If not normally distributed, these measurements were compared, before and after revision surgery, using a Wilcoxon signed-rank test for paired values. A level of significance of P <.05 was selected.
Results
In total, 25 patients were included, with a male to female ratio of 3:2 and a median age of 41 years (interquartile range [IQR] = 27.5-48). Prerevision and postrevision radiographs were available in 24 patients. The Weber type C fracture was most commonly revised (88%). The median time between initial treatment and revision surgery was 82 days (IQR = 43-292; Table 1). Twelve patients returned the functional outcome and QoL questionnaire. The radiological measurements to assess anatomical alignment prerevision and postrevision for each patient are shown in Table 2.
Table 1.
Patient and management characteristics.
| Patient | Gender | Age | Follow-up (years) | Time to Revision (days) | Side | Weber Classification | Potts Classification | Initial Tx | Wound Infection | Revision L/R | Revision T/O/Z | Lenghtening (mm) | OMAS | EQ-5D-5L |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 46 | 82 | Left | Weber C | Unimalleolar | ORIF | No infection | L | T | — | |||
| 2 | M | 22 | 8 | 12 | Left | Weber C | Unimalleolar | ORIF | No infection | L | — a | — | 60 | 0.7 |
| 3 | M | 25 | 73 | Left | Weber C | Unimalleolar | ORIF | No infection | L | O | — | |||
| 4 | F | 28 | 51 | Right | Weber C | Bimalleolar | ORIF | No infection | L | O | — | |||
| 5 | F | 27 | 6 | 21 | Right | Weber C | Trimalleolar | ORIF | No infection | L and R | O | — | 25 | 0.322 |
| 6 | M | 40 | 6 | 36 | Left | Weber C | Bimalleolar | ORIF | No infection | L | O | 4 | 60 | 0.805 |
| 7 | M | 26 | 16 | Right | Weber B | Unimalleolar | ORIF | POWI after revision | L and R | O | 1 | |||
| 8 | M | 18 | 5 | 157 | Right | Weber C | Unimalleolar | ORIF | No infection | L | O | 4 | 90 | 1 |
| 9 | F | 46 | 14 | 193 | Right | Weber C | Bimalleolar | ORIF | No infection | L and R | O | 10 | 40 | 0.677 |
| 10 | M | 46 | 7 | 342 | Left | Weber C | Unimalleolar | ORIF | No infection | L and R | T | — | 80 | 1 |
| 11 | F | 58 | 5 | Left | Weber C | Bimalleolar | ORIF | No infection | L and R | — a | — | |||
| 12 | M | 49 | 4 | 273 | Left | Weber C | Unimalleolar | ORIF | POWI after revision | L | Z | 6 | 80 | 0.874 |
| 13 | M | 63 | 14 | 3 | Left | Weber C | Bimalleolar | ORIF | No infection | L | — a | — | 65 | 0.798 |
| 14 | M | 41 | 64 | Left | Weber C | Unimalleolar | ORIF | No infection | L and R | O | — | |||
| 15 | F | 47 | 12 | 82 | Right | Weber C | Unimalleolar | ORIF | No infection | L | O | — | 25 | 0.733 |
| 16 | F | 46 | 15 | 78 | Left | Weber C | Unimalleolar | ORIF | No infection | L and R | — a | 4 | 90 | 0.912 |
| 17 | F | 78 | 60 | Left | Weber C | Bimalleolar | ORIF | No infection | L and R | T | — | |||
| 18 | M | 32 | 331 | Right | Weber C | Bimalleolar | ORIF | No infection | L | O | — | |||
| 19 | F | 27 | 311 | Left | Weber C | Bimalleolar | ORIF | POWI after initial surgery | L and R | T | — | |||
| 20 | M | 57 | 3 | 50 | Left | Weber C | Trimalleolar | ORIF | No infection | L | O | — | 100 | 1 |
| 21 | M | 33 | 599 | Right | Weber C | Unimalleolar | ORIF | No infection | L | Z | 5 | |||
| 22 | F | 36 | 2 | 490 | Left | Weber B | Bimalleolar | N-O | No infection | L | 3 | 70 | 1 | |
| 23 | M | 57 | 1 | 127 | Right | Weber C | Unimalleolar | ORIF | POWI after revision | L and R | O | 3 | ||
| 24 | M | 38 | 445 | Left | Weber C | Unimalleolar | ORIF | No infection | L | |||||
| 25 | M | 41 | 243 | Left | Weber C | Unimalleolar | ORIF | No infection | L | O | 2 | |||
| Median | 41 | 82 Days | 67.5 | 0.84 |
Abbreviations: L, lengthening; R, rotation; O, oblique (Weber-B fracture type) osteotomy; Z, Z-shaped osteotomy; T, transverse (original Weber) osteotomy; OMAS, Olerud and Molander Ankle Score; ORIF, open reduction and internal fixation; N-O, non-operative; POWI, Post-Operative Wound Infection.
Osteotomy of the fracture.
Table 2.
Radiological Measurements to Assess Anatomical Alignment Prerevision and Postrevision. a
| Patient | Days Between | OMAS b | TCA Before | TCA After | TT Before | TT After | MCS Before | MCS After |
|---|---|---|---|---|---|---|---|---|
| 1 | 82 | 74.8 | 78.5 | 3.1 | 0.1 | 6.3 | 1.87 | |
| 2 | 12 | 60 | 81 | 78.5 | 3.4 | 2.1 | 4.8 | 1.59 |
| 3 | 73 | 79.8 | 76 | 2.9 | 2 | 5.81 | 2.6 | |
| 4 | 51 | 76.1 | 79.6 | 0.8 | 0.4 | 4.25 | 2.99 | |
| 5 | 21 | 25 | 76 | 74.4 | 3.5 | 1.3 | 3.67 | 3.75 |
| 6 | 36 | 60 | 86.1 | 76.4 | 0.4 | 1.2 | 0.4 | 3.37 |
| 7 | 16 | 78.3 | 84.7 | 4.1 | 2 | 4.56 | 1.91 | |
| 8 | 157 | 90 | 77.2 | 79.4 | 3 | 1 | 7.31 | 3.66 |
| 9 | 193 | 40 | 78.7 | 83.9 | 8.5 | 0.5 | 9.06 | 3.76 |
| 10 | 342 | 80 | 72.2 | 76.6 | 1.2 | 1.5 | 4.9 | 3.63 |
| 11 | 5 | NA | 78.8 | NA | 0.4 | NA | 3.09 | |
| 12 | 273 | 80 | 75.2 | 79 | 3.3 | 0.7 | 5.57 | 3.34 |
| 13 | 3 | 65 | 80.2 | 78.5 | 2.8 | 0.1 | 4.55 | 2.74 |
| 14 | 64 | 76.5 | 80.2 | 0 | 0 | 5.36 | 4.29 | |
| 15 | 82 | 25 | 87.4 | 82.6 | 9.5 | 0.1 | 5.98 | 3.81 |
| 16 | 78 | 90 | 75.8 | 79 | 3.5 | 1.3 | 12.27 | 2.25 |
| 17 | 60 | 89.5 | 85.4 | 6.4 | 4.2 | 3.82 | 3.14 | |
| 18 | 331 | 78.5 | 80.1 | 2.2 | 0.7 | 5.91 | 3.23 | |
| 19 | 311 | 81.6 | 82.8 | 0.3 | 0.4 | 1.88 | 3.68 | |
| 20 | 50 | 100 | 80.9 | 79.7 | 0.1 | 0.5 | 4.76 | 3 |
| 21 | 599 | 79.3 | 79.1 | 5.6 | 1 | 5.68 | 1.6 | |
| 22 | 490 | 70 | 76.2 | 79.5 | 0.2 | 0.4 | 5.88 | 3.19 |
| 23 | 127 | 73.3 | 76.6 | 3.6 | 1.5 | 5.04 | 3.2 | |
| 24 | 445 | 81.3 | 79.4 | 2.2 | 0.1 | 4.58 | 3.15 | |
| 25 | 243 | 76.3 | 78.1 | 0.3 | 0.2 | 5.53 | 2.77 |
Abbreviations: OMAS, Olerud Molander Score; TCA, talocrural angle; TT, talar tilt; MCS, medial clear space; NA, not applicable.
For TCA, TT, and MCS, bold refers to values outside the normal range. Those within the normal range are not bolded.
0-30, Poor; 31-60, fair; 61-90; good; 91-100, excellent.
The median TCA was 78.4° (IQR = 76.0-80.0) before revision and 79.25° after revision (IQR = 78.2-80.2). This difference was not statistically significant (P = .297). The median TT was 2.95° (IQR = 0.50-3.58) before revision and 0.7° (IQR = 0.25-1.45) after revision. This improvement was statistically significant, with P <.001. The MCS before revision was 5.2 mm (IQR = 4.55-5.9) and differed significantly from the MCS after revision, which was 3.17 mm (IQR = 2.64-3.65; P < .000).
After the initial treatment, all radiological measurements (TCA, TT, and MCS) were outside of the normal range in 10 of 25 patients (Table 2). Only 2 patients had a normal score on all measurements. There was a clear improvement after revision; 14 of 25 patients had a normal score for all measurements, and the other 11 patients had just 1 abnormal measurement.
Of the 25 included patients, 12 patients returned the questionnaires. For these patients, median long-term follow-up was calculated to be 81 months (IQR = 54.5-166.5 months) after revision surgery (Table 1). The functional outcome measured by the OMAS had a median of 67.5 points (IQR = 45-87.5). When divided into 4 groups (Poor: 0-30; Fair: 31-60; Good: 61-90; Excellent: 91-100), 1 patient scored excellent, 6 patients, good, 3 patients, fair, and 2 patients, poor (Table 2).
Of the 5 patients who had a poor or fair OMAS, 3 patients (60%) still had an abnormal TCA after revision surgery (Table 2). In the patient group with a good or excellent score, 2 of 7 patients (29%) had an abnormal TCA after revision.
There was no significant difference in the radiological measurements after revision between patients with an excellent or good OMAS and patients with a poor or fair score. We used a χ2 test; P =.276 for the TCA and P =.217 for the TT. The MCS was good in all the 12 measurements, so no statistical analysis could be performed.
There was no relationship found between age and the OMAS, and neither did we find a relationship between time to revision and functional outcome. Analysis of the QoL questionnaires yielded a score of 0.84 points.
Discussion
Anatomical alignment improved significantly after revision surgery of malunited ankles. Changes in TT and the MCS are measured after revision ankle surgery. Measurements of the TCA appear less reliable to use for determining the anatomical alignment possibly because of a natural variation that is larger to begin with. Comparing the TCA with the uninjured side, as described by Sarkisian and Cody, 17 may be more useful in the assessment of alignment than to solely measure the injured side. 18 Unfortunately, contralateral radiographs were not available for analysis in this study.
Patients in this study scored a median OMAS of 67.5 points. This is low compared with the normative value for patients who underwent surgery fixation of an (unstable) ankle fracture without indication for revision surgery. In the available literature, scores are found to be between 66 and 85 points.19-22 Eberl et al 23 found an average OMAS of 82.7 points in 16 patients who underwent a lengthening of the fibula.
The functional outcome after a fibular osteotomy has been described as successful by van Wensen et al 7 in a literature review describing good or excellent results in 75% of patients. In our series, 60% of patients reported excellent or good results, which compares reasonably to the previous literature. The QoL scores of our patient were comparable to those of the healthy population in the Netherlands: 0.83 vs 0.87, respectively. 15 Despite at least 2 surgical procedures, and in some cases a reduced functional outcome, QoL does not seem to be affected in the long-term follow-up.
There are more factors that determine the success of a revision; one of them is the condition of the articular cartilage. 24 Biomechanical studies previously demonstrated that substantial displacement (≥2mm) of the fibula and a decrease in contact area, because of lateral shift, led to subsequent degenerative change in the ankle.4-6 If these degenerative changes are already present before the corrective osteotomy, they will not disappear after revision surgery. The progression of arthritis may be slowed down by a fibula osteotomy at revision, thereby delaying the symptoms of arthritis.9,25
Therefore, we expected to find a worse functional outcome in patients with a longer time to revision. However, in this study, time to revision did not affect the functional outcome. 7 So probably, there were no significant degenerative changes in our patients, which led to a considerable improvement. 26 Another determinant that could affect the functional outcome and QoL is age. It is well known that functional outcome decreases with the years. However, in this study, no relationship between age and functional outcome was found.
This study has a few limitations. First, because of the low incidence of fibula malunion, the sample size of this study was small. This makes our hypothesis that there would be a correlation between the radiological alignment and functional outcome difficult to prove. Measurements were performed with conventional radiographs because CT imaging was not available for all patients. Although measurements might be more reliable when using CT imaging, conventional radiograph measurements increase the external validity and applicability of results because it is always available.
Second, the retrospective nature of this study resulted in a wide range of follow-up times and limited availability of functional and QoL outcomes. In a prospective cohort, OMAS before the corrective osteotomy could have been obtained. However, considering the low incidence of fibula malunions, a prospective study would not have been feasible, even in our institute specializing in foot-ankle injury.
In this study, the focus was on radiological alignment of the ankle joint and the effect this has on the satisfaction of the patient. However, more determinants may have an effect on the functional outcome, such as the level of (preexistent) arthritis.
In conclusion, there is a clear improvement of alignment using radiological measurements, although the TCA seems to be less reliable in the prediction of functional outcome. Functional outcome scores are lower than in patients who underwent surgical fixation for an ankle fracture, but the median score is still a good score. QoL was not lower than that in the general population in the Netherlands.
For future studies trying to establish a relationship between functional outcome and anatomical alignment, we recommend measuring functional outcome also before the corrective osteotomy and having a fixed time point for follow-up measurements. In case of suspicion of a fibula malunion, a radiograph of the uninjured side will help determine the TCA of the injured side. In addition, a preoperative CT scan to determine rotation of the fibula should be part of the workup. If possible, it would be useful to have a larger sample size, making a linear regression analysis possible to allow correction for confounders, such as the grade of arthritis. A larger sample size could be arranged if more specialized hospitals combine their data.
Despite limitations, this study was able to show that radiological measurements are advantageous in detecting a malunion of the fibula. However, the most important part of treating ankle fractures is to prevent malunion. 27 During the initial treatment anatomical alignment and stability should be pursued to improve functional outcome and to prevent arthritis in the first place.
In conclusion, articular reconstruction with malleolar osteotomies is indicated for the treatment of ankle posttraumatic malalignment; it offers reduction in pain, improvement in ankle function, delay in the development of posttraumatic arthritis, and minimization of the need for radical surgery, such as ankle fusion or prosthetic replacement. In the assessment of malunion, especially, the TT and MCS are advantageous, whereas the TCA is less so.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval: Not applicable, because this article does not contain any studies with human or animal subjects.
Informed Consent: Not applicable, because this article does not contain any studies with human or animal subjects.
Trial Registration: Not applicable, because this article does not contain any clinical trials.
ORCID iD: Merel F. N. Birnie  https://orcid.org/0000-0001-7899-8323
https://orcid.org/0000-0001-7899-8323
References
- 1. De Boer AS, Schepers T, Panneman MJ, Van Beeck EF, Van Lieshout EM. Health care consumption and costs due to foot and ankle injuries in the Netherlands, 1986-2010. BMC Musculoskelet Disord. 2014;15:128. doi: 10.1186/1471-2474-15-128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Thur CK, Edgren G, Jansson KÅ, Wretenberg P. Epidemiology of adult ankle fractures in Sweden between 1987 and 2004: a population-based study of 91,410 Swedish inpatients. Acta Orthop. 2012;83:276-281. doi: 10.3109/17453674.2012.672091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mont MA, Sedlin ED, Weiner LS, Miller AR. Postoperative radiographs as predictors of clinical outcome in unstable ankle fractures. J Orthop Trauma. 1992;6:352-357. [DOI] [PubMed] [Google Scholar]
- 4. Ramsey PL, Hamilton W. Changes in tibiotalar area of contact caused by lateral talar shift. J Bone Joint Surg Am. 1976;58:356-357. [PubMed] [Google Scholar]
- 5. Curtis MJ, Michelson JD, Urquhart MW, Byank RP, Jinnah RH. Tibiotalar contact and fibular malunion in ankle fractures: a cadaver study. Acta Orthop Scand. 1992;63:326-329. doi: 10.3109/17453679209154793 [DOI] [PubMed] [Google Scholar]
- 6. Thordarson DB, Motamed S, Hedman T, Ebramzadeh E, Bakshian S. The effect of fibular malreduction on contact pressures in an ankle fracture malunion model. J Bone Joint Surg Am. 1997;79:1809-1815. [DOI] [PubMed] [Google Scholar]
- 7. van Wensen RJ, van den Bekerom MP, Marti RK, van Heerwaarden RJ. Reconstructive osteotomy of fibular malunion: review of the literature. Strategies Trauma Limb Reconstr. 2011;6:51-57. doi: 10.1007/s11751-011-0107-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Chao KH, Wu CC, Lee CH, Chu CM, Wu SS. Corrective-elongation osteotomy without bone graft for old ankle fracture with residual diastasis. Foot Ankle Int. 2004;25:123-127. doi: 10.1177/107110070402500302 [DOI] [PubMed] [Google Scholar]
- 9. Henderson WB, Lau JT. Reconstruction of failed ankle fractures. Foot Ankle Clin. 2006;11:51-60. doi: 10.1016/j.fcl.2005.12.006 [DOI] [PubMed] [Google Scholar]
- 10. Hohmann E, Foottit F, Tetsworth K. Relationships between radiographic pre- and postoperative alignment and patient perceived outcomes following Weber B and C ankle fractures. Foot Ankle Int. 2017;38:270-276. doi: 10.1177/1071100716674703 [DOI] [PubMed] [Google Scholar]
- 11. Weber B. Die verletzungen des oberen sprunggelenkes. 2nd ed. Berne, Switzerland: Verlag Hans Huber; 1972. [Google Scholar]
- 12. Pott P. Some few general remarks on fractures and dislocations. 1758. Clin Orthop Relat Res. 2007;458:40-41. doi: 10.1097/BLO.0b013e31803dd063 [DOI] [PubMed] [Google Scholar]
- 13. Olerud C, Molander H. A scoring scale for symptom evaluation after ankle fracture. Arch Orthop Trauma Surg. 1984;103:190-194. doi: 10.1007/BF00435553 [DOI] [PubMed] [Google Scholar]
- 14. Herdman M, Gudex C, Lloyd A, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res. 2011;20:1727-1736. doi: 10.1007/s11136-011-9903-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Versteegh M, Vermeulen KM, Evers SM, de Wit GA, Prenger R, Stolk EA. Dutch tariff for the five-level version of EQ-5D. Value Health. 2016;19:343-352. doi: 10.1016/j.jval.2016.01.003 [DOI] [PubMed] [Google Scholar]
- 16. Nilsson GM, Eneroth M, Ekdahl CS. The Swedish version of OMAS is a reliable and valid outcome measure for patients with ankle fractures. BMC Musculoskelet Disord. 2013;14:109. doi: 10.1186/1471-2474-14-109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Sarkisian JS, Cody GW. Closed treatment of ankle fractures: a new criterion for evaluation—a review of 250 cases. J Trauma. 1976;16:323-326. doi: 10.1097/00005373-197604000-00014 [DOI] [PubMed] [Google Scholar]
- 18. Rolfe B, Nordt W, Sallis JG, Distefano M. Assessing fibular length using bimalleolar angular measurements. Foot Ankle Int. 1989;10:104-109. doi: 10.1177/107110078901000210 [DOI] [PubMed] [Google Scholar]
- 19. Willett K, Keene DJ, Mistry D, et al. Close contact casting vs surgery for initial treatment of unstable ankle fractures in older adults. JAMA. 2016;316:1455-1463. doi: 10.1001/jama.2016.14719 [DOI] [PubMed] [Google Scholar]
- 20. Garratt AM, Naumann MG, Sigurdsen U, Utvåg SE, Stavem K. Evaluation of three patient reported outcome measures following operative fixation of closed ankle fractures. BMC Musculoskelet Disord. 2018;19:134. doi: 10.1186/s12891-018-2051-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Sanders DW, Tieszer C, Corbett B; Canadian Orthopedic Trauma Society. Operative versus nonoperative treatment of unstable lateral malleolar fractures: a randomized multicenter trial. J Orthop Trauma. 2012;26:129-134. [DOI] [PubMed] [Google Scholar]
- 22. Schepers T, van der Linden H, van Lieshout EM, Niesten DD, van der Elst M. Technical aspects of the syndesmotic screw and their effect on functional outcome following acute distal tibiofibular syndesmosis injury. Injury. 2014;45:775-779. doi: 10.1016/J.INJURY.2013.09.035 [DOI] [PubMed] [Google Scholar]
- 23. Eberl R, Kaminski A, Hauser J, Arens S, Nicolas V, Muhr G. Oblique osteotomy for post-traumatic fibula incongruity [in German]. Chirurg. 2006;77:439-446. doi: 10.1007/s00104-005-1150-7 [DOI] [PubMed] [Google Scholar]
- 24. Offierski CM, Graham JD, Hall JH, Harris WR, Schatzker JL. Late revision of fibular malunion in ankle fractures. Clin Orthop Relat Res. 1982;(171):145-149. [PubMed] [Google Scholar]
- 25. Weber BG, Simpson LA. Corrective lengthening osteotomy of the fibula. Clin Orthop Relat Res. 1985;(199):61-67. [PubMed] [Google Scholar]
- 26. El-Rosasy M, Ali T. Realignment-lengthening osteotomy for malunited distal fibular fracture. Int Orthop. 2013;37:1285-1290. doi: 10.1007/s00264-013-1876-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Rammelt S, Obruba P. An update on the evaluation and treatment of syndesmotic injuries. Eur J Trauma Emerg Surg. 2015;41:601-614. doi: 10.1007/s00068-014-0466-8 [DOI] [PubMed] [Google Scholar]
- 28. Walling A, Sanders RW, Behboudi A, Anderson JG, Bohat DR. Ankle fractures. In: Coughlin M, Saltzman C, Anderson RB, eds. Mann’s Surgery of the Foot and Ankle. Philadelpia, PA: Saunders Elsevier; 2013:2003-2040. [Google Scholar]