Abstract
Chronic stress is a ubiquitous problem shouldered by many people worldwide. Although the stressors are myriad (eg, loneliness, finances, health, discrimination), the corporal response to them either causes or exacerbates mental and physical illness, including depression, anxiety, and cardiovascular disease. Identifying efficient ways to help people buffer their response and promote resilience and wellness is critical to improving overall health. Positive interpersonal connection is a proven way to promote resilience and happiness. It is associated with decreased mortality and markers of better health. Kindness and caring are prosocial behaviors that build positive interpersonal connections and can uplift both the giver and receiver. Simply seeing kindness and caring activates the neuropsychology of kindness, elevating the viewer and promoting generosity, interpersonal connection, and inclusion. That augmenting positive emotions, enhancing interpersonal connection, and inducing prosocial behavior change are possible through seeing kindness opens the opportunity to bolster resilience in higher stress settings like health care. In a recent study, watching kindness media in a health care setting rapidly increased self-reported feelings of happiness, calm, gratitude, and being inspired. Viewers were significantly more generous. Providing staff and patients with a nonjudgmental lift to enhance caring interactions through kindnesses media can be an important, low-cost adjunct to improving the healthcare environment.
Keywords: stress, kindness, altruism, wellness, health, imagery, prosocial, media psychology
K.H. was 19 years of age when he attempted suicide by jumping off of the Golden Gate bridge. On reflection of what might stop him from jumping, he said, “All I wanted is for someone to see my pain and say something kind.” 1 Reflections from others also suffering from suicidal ideation affirmed how kindness was important in deterring suicide, a finding supported in a study of the impact of caring letters on suicides. In that study from Motto and Bostrom, 2 the simple act of sending caring letters to people who previously attempted suicide was enough to substantially reduce new suicide attempts compared to those who received informational letters.
The insight that showing concern can change the outcome in an extreme setting like suicidal ideation is the starting point to a broader understanding as to how kindness and compassion—really connection—can help people buffer the response to stressors and promote resilience and wellness. Epidemiologic and clinical observations reveal the potential impact of kindness and connection on health and longevity, which are mechanistically underpinned by specific biomarkers suggesting that they effect changes opposite to those of stress.
Practically, the promotion of kindness on a wide scale is achievable through the use of kindness imagery, which can trigger positive emotional changes, perceived connection to others, and behavioral change. When streamed into higher stress settings like health care, kindness imagery offers a simple, low-cost, and passive intervention that has the potential to promote quality of life and good health while strengthening the social fabric. In health care, the projected impact of long-term use of kindness media is an uplifted environment in which both the staff and patients are happier, calmer, and less stressed, which, in turn, can lead to improved staff and patient satisfaction and patient engagement. Beyond health care, kindness media has implications for other stressful settings as well as help attenuate self-other differences that are at the core of social and political division.
Understanding the Impact of Stress on Health
A large proportion of people have been shouldering an intolerably high level of stress. This level is partly reflected in the rising suicide rate as well as deaths of despair from alcohol or drugs to quench the pain of existence. 3 Even before the COVID-19 pandemic and the nationwide protests, Americans were among the most stressed citizens in the world. 4
The annual American Psychological Association survey reveals that stress is driven by a myriad factors, including personal health, the cost of health care, mass shootings, financial health, and climate change 5 as well as loneliness. 6 Especially relevant to the present time, discrimination is a potent stressor, affecting the majority of people of color and those from LGBTQ (lesbian, gay, bisexual, transgender, queer/questioning) communities. 5 The physical and mental health as well as financial consequences of COVID-19 and the polarized and anger-fueled political and social climate are exacerbating the experienced stress loads. Beyond the United States, it needs to be emphasized that stress is a worldwide problem, observed in both developing as well as developed countries such as the United Kingdom, Australia, and many others.4,7
Acknowledging the impact of chronic stress on health is important to motivating efforts to address it on a public health scale.8,9 When compared to people with lower stress, high levels of chronic stress are associated with markedly increased risk of mortality, particularly from cerebrovascular and ischemic heart disease, with evidence of a dose response.10,11
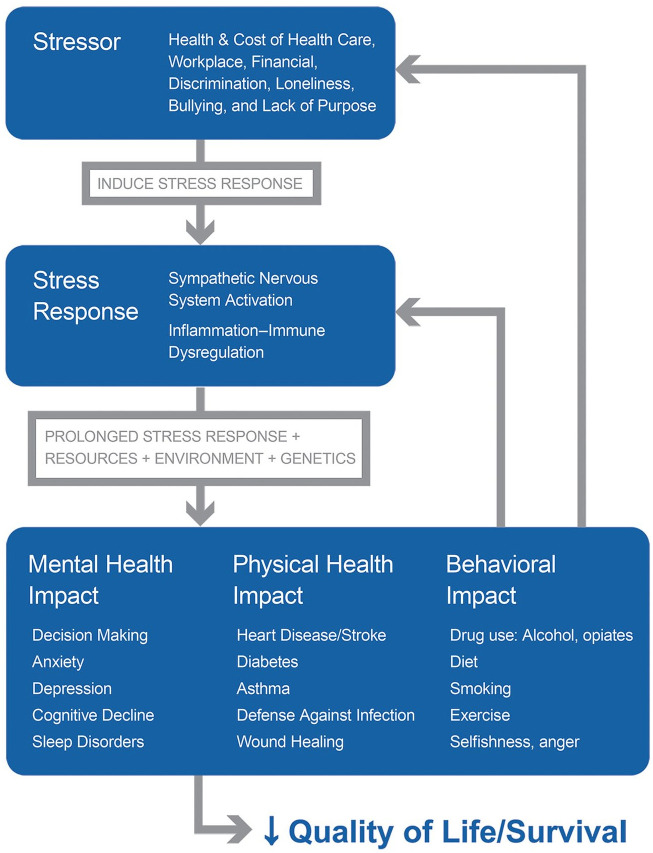
The paths to excess disease and mortality from stress are summarized in Figure 1. For both mental and physical health, stress contributes to the excess risk of diseases through both direct and indirect mechanisms. Directly, the stress response induces inflammation, immune dysregulation, and hypothalamic-pituitary-adrenal (HPA) and sympathetic nervous system activation, pathophysiologic mechanisms common to most of the listed disorders.12-15 Indirectly, stress drives the afflicted toward unhealthy behaviors, including overeating, alcohol and other drugs, decreased exercise, smoking, and so on.
Figure 1.
A graphic depiction of how stress can affect people. Multiple different stressors, alone or in combination, are perceived or experienced by the individual. Depending on that person’s reaction, a stress response is evoked, resulting in sympathetic nervous system activation and accompanied by immune dysregulation and inflammation. When sustained for a long time, and influenced by other factors such as personal resources (eg, health literacy, access to care), environment (eg, allergens), and genetics, the stress response elicits varying forms of mental and physical disease. A partial list of some of the sequelae is shown. Behavioral changes are also affected by stress. This is a vicious cycle, in which the aspects of ill health, disability, isolation, and behavior change, in turn, can create more stress, as indicated by gray arrows. Depending on severity, the quality of life can be impaired and mortality can rise.
These direct and indirect effects are occurring on the backdrop of (and are influenced by) other genetic, social, and environmental circumstances. One important circumstance is poverty; in addition to more stressors, poor people have less health literacy, less access to healthier food, and greater exposure to physical stressors at work or in the home environment (eg, allergens), compounding risk.
Finally, this process is not linear—it is a vicious cycle. As people become ill, stressors such as concern for health, finances, or disability, loneliness, sleep disturbances, and so on, can be exacerbated, fueling the cycle. The illnesses themselves are added stressors. Thus interruption of the stress-disease cycle at its source is key to prevention (Figure 1).
Although it is recognized that stress is a major contributor to diseases like asthma or cardiovascular disease,14,16 or that stress may accelerate disease progression (eg, from HIV infection to frank AIDS 17 ) and aging (as measured by telomere shortening), current health care practice largely focuses on the manifestations of the disorder, per se, and much less often on the stressor itself (if at all, due to time and resource limitations). As much stress (and disease) have origins in social issues, 18 problems such as loneliness, workplace stress, marital issues, and financial strain (especially poverty), have to be managed by social services or counseling, which are often limited in availability and/or resources and not easily addressed in a 15-minute health care provider visit.
By affecting health and quality of life, stress also has economic consequences that businesses and governments, as well as individuals, must bear the cost of. Workplace stress alone is estimated to cost upward of US$300 billion in the United States and €600 billion in the European Union.19,20 Much of that is due to health care costs. Goh et al 21 estimated that, in the United States, workplace stress accounted for 5% to 8% of total US health care costs (and for 120,000 deaths each year). 21 As health care represents a growing and enormous portion of GDP, reducing costs by interrupting the stress-disease cycle can be both medically and fiscally salutary.
Although directly relieving stressors like financial or health care concerns is the preferred approach, solutions to these are challenges are complex and require a lot of time, money, and compromise. An intermediate step is to help people in how they perceive and respond to these stressors, that is, enhance resilience. The thrust of this article is the pursuit of resilience and wellness by bolstering social support and connection.
Why Kindness?
The central idea is that kindness creates positive (supportive and meaningful) social connections, which, in turn, reduce the response to stressors as well as fulfill basic, innate needs that are critical to health and longevity. Under the umbrella term of “kindness” are included related prosocial emotions and behaviors such as caring, generosity, altruism, empathy, gratitude, and compassion.
It has been long known that positive social connection is associated with longevity and decreased mortality. 22 Along the spectrum from loneliness to social connection is a decreasing risk of mortality observed in multiple studies. 23 Loneliness, a major and highly prevalent stressor of perceived social isolation, has attracted much attention, 24 including from governments, insurers, as well as health professionals. 25 In addition to markedly affecting quality of life, loneliness affects mortality more than obesity and about the same as smoking 15 cigarettes per day. 22
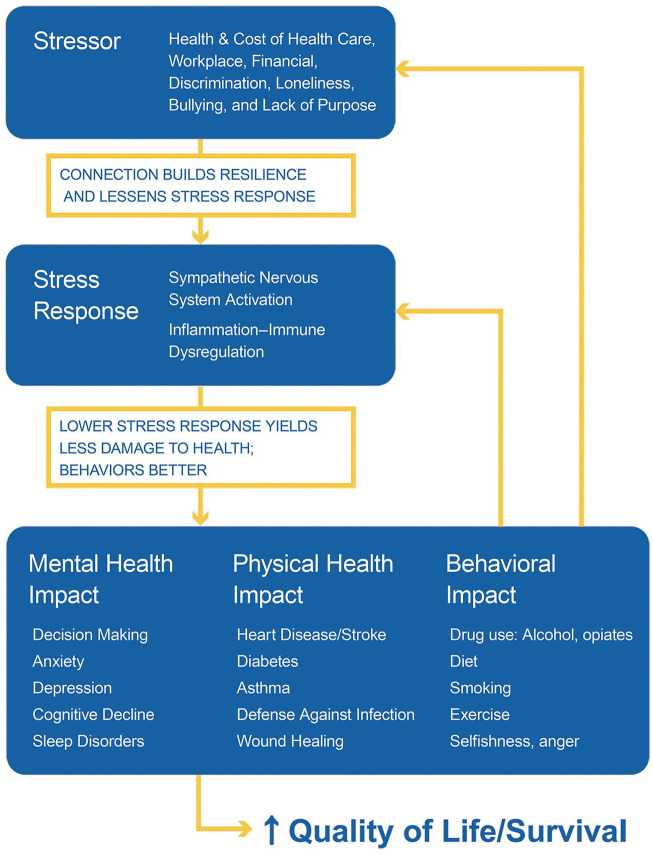
Conversely, positive social connection (social support) is associated with a 50% reduced risk of early mortality, 21 an observation that has been explained (at least partly) through its effect on buffering stress. 26 Buffering stress refers to the diminished response of the person experiencing the stressor, including sympathetic nervous system and HPA axis activation. Multiple studies have documented the relationship between degree of support and cardiovascular reactivity (including blood pressure), immune function, inflammation, and neuroendocrine changes.27-32 Social support (ie, positive prosocial connections), is associated with salutary changes in these parameters as well as in cardiovascular outcomes.29,30 Some of these effects are direct through decreasing the reaction to a stressor, or indirect, in which health-related behaviors (medication adherence, diet, exercise, etc) are improved (Figure 2).
Figure 2.
A graphic summary of how promoting positive social connection can affect the cascading response to stress. By improving resilience and thereby buffering the response to stressors, positive social connection diminishes the subsequent pathophysiology (in yellow). Positive interpersonal connection is also associated with greater engagement of the patient, such that behaviors, including medication adherence, can improve. At a minimum, the vicious cycle is attenuated and potentially allows for the induction of a (more) virtuous cycle, as indicated in yellow.
Prosocial behaviors (eg, volunteering) are very effective ways to create positive connections, 33 including in children 34 and adolescents. 35 Prosocial behaviors, including compassion and gratitude, can increase self-other similarity or overlap, emphasizing shared common qualities,36-38 an effect that involves increased vagal nerve activity. 39 As a consequence of increasing connection (or self-other similarity), prosocial behavior also increases cooperation.33,40 Analogously, social exclusion decreases prosocial behavior and cooperation 41 and increases aggression and hostility. 42
Prosocial behavior also induces happiness and well-being, which, in turn, would promote more prosocial behavior in a mutually reinforcing, virtuous cycle.43,44 This type of happiness (eudaimonia) can be driven by “elevation,” a positive emotion elicited when witnessing other people engage in virtuous acts such as generosity, kindness, or selflessness. The uplifted feeling of elevation can manifest physical sensations such as warmth in the chest 45 and is associated with feeling optimistic and connected to others, that is, a self-transcendent state of being.46,47 Readers have likely experienced elevation (or a similar feeling called “kama muta” 48 ) after helping someone or seeing someone being helped. There is evidence that this uplifted feeling associated with social support is partly mediated through the opioid system. 49
Identifying paths to eudaimonic happiness can enable flourishing and well-being, especially for primary or secondary prevention of disease, particularly cardiovascular disease.9,50-52 As a result of its impact on disease, positive psychologists have advocated for interventions to promote eudaimonia as part of health care that can also increase the use of prevention services and improve wound healing, among other effects.9,51
Data supporting the effects of kindness on health can be found in epidemiologic surveys that included measures of volunteerism. Although these are complicated surveillance studies, multiple reports have yielded similar results. Taken together, meta-analyses have shown that volunteering is associated with a decrease in mortality of approximately 20%. 53 Similarly, longitudinal studies of caregivers of the elderly (a subtype of volunteer) have significantly lower mortality than non-caregivers, 54 a result that may be influenced by level of perceived stress. 55
Aligned with the stress-social connection hypothesis, marker studies of kindness and connection show salutary shifts in inflammation and autonomic nervous system responses. For example, volunteers have lower markers of inflammation, such as C-reactive protein. 56 Similarly, a 4-week kindness exercise decreased leukocyte transcripts of a set of proinflammatory genes that are upregulated in response to stress. 57 Along with neuroimaging markers of empathy and altruism,58,59 these studies provide more biological insight into how kindness and connection could explain clinical outcomes. Positive social connection as attained through volunteerism would yield the opposite effect of stress, per se, increasing parasympathetic (vagal) activity along with reducing inflammation and promoting immune competence, 28 providing a consistent explanation for the decrease in mortality.
Figure 2 illustrates how kindness and connection can affect the stress-disease cycle, including building resilience and lessening the psychological and corporal reaction to stressors.
Another important aspect of kindness is how caring displayed by the health care provider affects patient response and behavior. As recently compiled by Trzeciak and Mazzarelli, 60 there are multiple reasons why the patient’s perception of provider compassion is critical to outcomes. From a high-level view, patient-perceived caring (compassion and empathy) from the provider is critical to creating connection and trust. 61 That trust lowers stress (fear) and affects patient engagement or activation in their own care, including adherence to a regimen, 62 resulting in lower cost of care. 63 Perceived caring will also lead to higher patient satisfaction. It is expectable, therefore, that adherence to diet, exercise, or long-term medication use requires caring to instill and help maintain those behavioral changes. For example, more empathic caregivers of patients with diabetes have lower HbA1c (glycated hemoglobin),64,65 suggesting that patient engagement in their own care was greater due to the connection with the physician. Thus, identifying ways to bring kindness and compassion into healthcare has the potential to affect the quality of the interaction between patient and provider, improve patient engagement, as well as reduce stress.
Promoting Kindness on a Population Basis
The challenge is how to promote kindness and connection on a population (and low cost) basis, especially at a time in which people are overloaded with distractions, such as the large volume of “information” or input received from a variety of sources. We are also living in an age of increasing narcissism, in which the focus on the self, individual success, and materialism would make encouraging kindness and altruism much more challenging and understandably generate skepticism that it can be achieved.66,67 Some might imagine that promoting kindness would be based on negative pressures such as shame, guilt, or moral persuasion. This approach, however, is not desirable and runs counter to promoting that uplifted, connected feeling described above. Although encouraging moral rectitude has value, it is more desirable to directly activate the neuropsychology of kindness through positive (uplifting) means.
The promotion of kindness through positive methods is made possible, however, by the observation that simply seeing acts of kindness and caring can evoke elevation, promote altruism, as well as promote a sense of being connected to others.46,47,68-71 In laboratory-based studies, viewers watching short, uplifting films, report significant increases in elevation and happiness as well as changing behavior as measured in increased generosity, donating either time or money.69,70 The same effect has been observed in a field study in which participants were asked to observe kind actions of others. 71 Finally, viewing kindness media can also affect the acceptance of people of other races46,68,70 and affect the dehumanization of others, 48 supporting the timely idea that mutual respect can be promoted by elevating people through kindness. This latter point has much relevance to diversity and inclusion as well as to health equity.
The impact of kindness media on emotions and behavior was recently tested in a health care setting. The health care environment represents an important microcosm to test this concept in, given that it is stressful for patients and particularly for providers who demonstrate burnout, depression, and suicide rates twice that of the general public. 72 It is also a busy and time-constrained setting in which there are multiple, competing events for both patients and staff (completing forms, being called, people entering and leaving, interruptions by phone, problem-solving, etc) in addition to the personal stressors all parties are otherwise experiencing (anxiety about the visit, issues in their own home life, etc).
In a pilot study of the effects of kindness media in a pediatric health care office, parents and staff were recruited to participate and randomized to watch either commercial children’s television or kindness media streamed onto a television in the waiting room. All participants completed questionnaires before and after 8 minutes of exposure to either media type. In comparison with commercial children’s television, kindness media inspired and uplifted viewers, including staff and parents. People were happier, calmer, more grateful, and more generous than after watching children’s programming. 73 Figure 3 shows a still image example of kindness media. A video example of kindness media used in this study can be seen here: https://vimeo.com/manage/392331523/general. Other kindness-related media used in the study (not shown) includes concepts in kindness, quotes, and humor.
Figure 3.
Sample kindness media. This image is of a park ranger and a baby rhinoceros at the Lewa Wildlife Conservancy in Kenya. After viewing the image, readers should reflect on how they feel, allowing personal insight into the effect of kindness media. Photo © Martin Buzora.
Operationalizing the promotion of kindness entails sharing kindness media with people in health care settings on a regular basis using digital signage technology. That could be streaming kindness media directly into waiting rooms, workrooms, cafeterias, patient rooms, and so forth, as applicable and able. Current technology can easily enable streaming as well as mix kindness media with other messaging such as health instruction, messages from training programs, etc.
The aforementioned study compared children’s television programming to kindness media. It is noted that many adult health care facilities show either emotionally neutral (eg, home and garden) or negative (eg, mainstream news) programming in the waiting rooms. As mainstream news is well known to rapidly induce stress and anxiety, 74 healthcare settings (especially emergency rooms, surgical waiting rooms, etc) should carefully consider what is being shown in the waiting rooms and work areas. Beyond a well-intentioned effort to simply distract the viewer, it could be more beneficial for practices to show inspirational media that can help facilitate positive emotions and interactions for patients and staff. This has implications for areas such as emergency rooms, in which waiting is often associated with aggression and violence. 75
A very desirable quality of this approach is that it is passive and does not require active engagement or training in a time-constrained environment where any added requirement could be considered onerous. Health care staff are already significantly burdened (and time-constrained) by requirements such as completing electronic health records as well as other required training and certifications. These training programs often include instruction on effective and compassionate communication to address the perceived need to increase compassion and empathy. These programs can be very effective, yielding evidence of increased compassion and better communication.76,77
Yet training programs have their own limitations. First, the training requires dedicated time from providers who are already stressed in part because of time limitations. Adding more time requirements can be viewed negatively, imposing additional burdens and further increasing stress. Second, memory from training fades over time, as it does for instruction in general. Third, human behavior is dynamic; as people are exposed to new events and experiences over time, particularly stressful experiences, the more recent (proximal) experiences can be a greater determinant of emotions and behaviors.Finally, some clinicians may react adversely to the unintended notion of needing to train to be more compassionate and communicative, perhaps inferring that they are not compassionate people and therefore be reluctant to attend.
Training is not necessary for kindness media—the ability to interpret and respond to body language (including facial expression) is inborn and transcends culture. Similarly to the effect of training, exposure to kindness media cannot simply be for a limited timeframe and expect emotions and behaviors to continue to improve while other experiences are also taking place. Kindness media is intended to be delivered to the environment regularly, preferably daily, in order to provide viewers recurrent and quick reminders of their innate humanity and activate the neuropsychology of caring. Finally, as kindness media is a relatively unbiased way of rapidly reminding all viewers of the human capacity to be kind and caring, it is much less likely to be met with dissatisfaction. A potential (and untested) approach is to combine kindness media with key messages from training.
On a cognitive level, displaying imagery and text on kindness and compassion can be a simple conscious reminder that may evoke positive or pleasant associations. Yet seeing kindness and compassion, like many other subjects (eg, hostility), can subconsciously influence thoughts and behaviors through priming, enabling more positive attitudes and emotions on a subconscious basis.78,79
Based on the aforementioned media studies, kindness imagery is likely another type of sensory prime. Although there are no formal kindness priming studies with imagery that the author has identified (versus semantic kindness primes), that watching kindness media for a few minutes affects the participants’ willingness to make a donation in several studies supports this idea. Moreover, the rapid induction of the effect suggests that it is evaluated by automatic (system 1) processing, consistent with priming. This idea is supported by an electroencephalographic study of images of gentle human touch. While the aforementioned kindness imagery studies used exposures of ~2 to 8 minutes, in an EEG study of images of gentle human touch, viewing a series of images for ~1 second each elicited significant mu-wave decreases compared with other image types (mu-wave decreases are associated with heightened empathy and social skills). 80 These observations collectively suggest that kindness media taps into intuitive and subconscious automatic processing (implicit memory) rather than (or in addition to) reflective or conscious (cognitive) processing.
This rapid effect also makes the approach attractive in a fast-paced, busy environment. Health care settings are important environments to be sure that kindness and compassion are front-and-center. After all, patients are seeking it while providers—physicians, nurses, as well as other staff—came to the profession to offer kindness and compassion in the context of administering the science of medicine. Yet given the brisk pace and multiple distractions, the intervention needs to be delivered regularly and received very quickly. Having that quick reminder can help reset perspectives, emotional state, and subsequent behaviors.
Other stressful and busy settings, of course, could also benefit from kindness primes, including schools, corporate workplaces, government offices, and so on. There is much relevance to the prevention of the negative (eg, bullying), and the promotion of the positive behaviors (teamwork and cooperation) in these and other environments. Bullying in schools or in workplaces is a large source of stress and disconnection. Teamwork and cooperation flow from the knowledge that we are all connected to each other. Adapted for situation-specific circumstances, kindness media can likely prime helping and cooperation behaviors, something greatly needed in a hyperpolarized and very competitive society.
Kindness Media Promotes What Nature Wants Us to Do: Help Each Other
Beyond the ability to uplift people and promote connection and generosity through priming, is there more of a teleology as to why people respond to kindness media? Does the preservation of kindness and connection have evolutionary salience to survival and health? Why would responses like these, along with salutary shifts in biology, be retained by humans and other living beings?
If viewed from an evolutionary perspective, we (and many other species) evolved with multiple mechanisms that would promote cooperation and mutual aid to better ensure the survival of the species. 81 Darwin recognized this, writing in The Descent of Man that communities with the greatest number of sympathetic (or altruistic) members would flourish the best, that is, members must help one another (and sacrifice) to better assure survival of the community. 82
Multiple examples support this idea of an evolutionary requirement to aid each other rather than be solely driven by self-interest. A more obvious one is the oxytocin-mediated drive a mother has to take care of her offspring and not abandon kin. That is, without the willingness to sacrifice food and incur other risks, many offspring would likely be neglected as the mother promotes her own survival. 83
More and diverse examples in support of nature’s mechanisms to promote connection and cooperation are summarized in Table 1. An important reinforcement mechanism that living beings have is the pleasurable feeling that comes from doing and seeing kindness. Studies have demonstrated that internal reward systems are activated by seeing or experiencing kindness, yielding a pleasurable experience (eg, ventral striatum; 84 ), whereas loneliness (social isolation) is a painful and distressing experience. As organisms, particularly humans, seek pleasure and avoid pain, the activation of reward systems reinforces the behavior to connect and help one another. It is resonant with this observation that naltrexone partially attenuates the good feeling accompanying social connection. 49 Other examples included in the table provide additional points of emphasis that being kind and positively connecting to others is well-conserved in our psychobiology. Many of the same features are seen in animals.
Table 1.
Examples Supporting the Biological and Psychological Aspects of Altruism. a
| Examples | Comment |
|---|---|
| Basic science | |
| Dedicated neurophysiology | Neuroanatomy responsible for empathy, compassion, and connection, along with neurohormonal effects (eg, oxytocin, serotonin) suggest an intricate system designed to encourage and sustain kindness and altruism.58,59 |
| Altruism has genetic basis | The population genetics of altruism and cooperation have been defined showing overall advantage to a species 88 |
| Social connection and kindness feel good | Powerful internal mechanisms exist to reinforce being kind and connecting positively with others. Being kind to someone else, or seeing kindness, makes people feel good, affecting reward/pleasure centers. Conversely, loneliness is a painful state, providing motivation to connect with others.28,31 |
| Psychosocial and biomedical observations | |
| Toddlers demonstrate helping behaviors | Observed in multiple studies, including with infants. Empathy allows for helping behaviors. Supports notion that altruism appears before moral development 89 |
| Partner selection | Selection of long-term partners is significantly influenced by kindness of the potential partner. Being described as kind increases physical attractiveness of potential partner. 90 |
| Effect of caring touch | Humans, and many other species, respond positively to caring touch with relaxation response and decrease in blood pressure. 91 Caring touch decreases pain and promotes social connection. 92 Hugs are very effective at relieving stress and can affect response to viral infection. 91 Simply seeing caring touch elicits effects on viewers. 80 |
| Volunteers have lower mortality | People who volunteer regularly have decreased death rates, likely through the promotion of positive connection when giving to another. Volunteers have decreases in markers of inflammation compared with non-volunteers. 53 |
| Altruism is present in many species | Multiple species will sacrifice for its own members—including ants, bats, rodents, and primates 81 |
This table illustrates the multiple facets supporting the thesis that altruism (kindness and caring) is an intrinsic part of behavior and biology. The number and diversity of facets exemplify the evolutionary drive to conserve altruism and related aspects (empathy, compassion, etc). Although the list is not exhaustive, taken together, these and other observations support the contention that the need for positive interpersonal connection through kindness and caring is an innate characteristic that has important implication for health. It also suggests that promoting kindness and cooperation does not necessarily depend on moral persuasion or guilt.
For some, this proposition might stand in contrast to “survival of the fittest,” a self-oriented, self-preservation concept bolstered by our individualistic culture. The notion that humans are innately altruistic, however, does not exclude that self-interest and perceived threat to survival are powerful motivators of behavior, as are fear, ego, and hedonic satisfaction. The key point is that the behavior of living beings is not just self-oriented; it is a malleable balance of self-interest and altruism. By promoting kindness using an automatic/mimicry approach (without scolding or moral persuasion), we can help people intuitively reconnect with their innate desire to help others, shifting that balance.
A challenge to thinking about promoting kindness as a public health intervention is that kindness can manifest in a myriad of ways and may at first glance appear ill-defined. Kindness can include major acts of sacrifice and compassion to smiling and saying hello or simply not criticizing someone else. Yet similarly to the many types of exercise that yield salutary effects, the multiple manifestations of kindness can likely be beneficial, particularly those that are meaningful to participants. Like exercise, the most important part is having people experience kindness regularly.
It is hypothesized that the initial viewing of kindness media will start a ripple. Like many emotions and behaviors, kindness is contagious.85,86 Envisioning what this could look like begins with kindness media deployed in stressful settings, like health care. As people are primed with kindness media, their moods can shift positively and caring behaviors enhanced. Those experiencing or witnessing kindness, in turn, can mimic these actions and propagate them further, simultaneously strengthening interpersonal connection and communication.85,87 Both patient and provider (staff) can share in this experience, bolstering trust and engagement. Thus, the media starts the ripple, but people spread it and become change agents.
It is important to acknowledge several valuable and effective methods to help individuals manage stress, including meditation, exercise, counseling, as well as pharmacotherapy in more intractable cases or situations. The promotion of kindness on a population scale can add to these important, individual methods as well as strengthen social cohesion and mutual respect. There are reasons to believe that by priming kindness, including kindness to oneself, we can encourage people to participate more in these self-help efforts.
The promotion of kindness alone will not directly solve societal problems like poverty, discrimination, and climate change. However, by enabling people to feel less stressed and more connected to each other, the opportunities to find compromises and solutions can flow from that culture change. As health professionals, that’s what we can do for K.H. and so many others.
Acknowledgments
The author thanks the many scientists, volunteers, and other contributors and supporters who over the years helped create this integrated view of how the promotion of kindness may affect personal connection and quality of life and the use of imagery to accomplish it. Envision Kindness is a 501(c)(3) with a mission to reduce stress and promote positive interpersonal connection through inspiring kindness, compassion, joy, and love through imagery of the same. Envision Kindness creates, produces, and distributes kindness media (EnSpireTM).
Footnotes
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: The author is the co-founder and President of Envision Kindness, a 501(c)(3) not-for-profit organization. He serves in these roles as a volunteer. As a not-for-profit, no ownership stake is available to anyone. Thus, there is no financial conflict of interest to report.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The author gratefully acknowledges the funding of Envision Kindness’s work by our generous donors and granting organizations including The Good People Fund, The Kitchings Family Foundation, The Petit Family Foundation, and the Southeastern Connecticut Cultural Coalition.
ORCID iD: David A. Fryburg  https://orcid.org/0000-0002-5348-2707
https://orcid.org/0000-0002-5348-2707
References
- 1.Hines K. How caring letters prevent suicide. Accessed December 30, 2020. https://www.youtube.com/watch?v=36bk3V__hZ8&t=5s
- 2.Motto JA, Bostrom AG. A randomized controlled trial of postcrisis suicide prevention. Psychiatr Serv. 2001;52:828-833. doi: 10.1176/appi.ps.52.6.828 [DOI] [PubMed] [Google Scholar]
- 3.Rehm J, Shield KD. Global burden of disease and the impact of mental and addictive disorders. Curr Psychiatry Rep. 2019;21:10. [DOI] [PubMed] [Google Scholar]
- 4.Ray J. Americans’ stress, worry and anger intensified in 2018. Gallup. Published April 25, 2019. Accessed December 30, 2020. https://news.gallup.com/poll/249098/americans-stress-worry-anger-intensified-2018.aspx
- 5.American Psychological Association. Stress in America™ press room. Stress in America 2020. A national mental health crisis. Accessed December 30, 2020. https://www.apa.org/news/press/releases/stress [Google Scholar]
- 6.Holt-Lunstad J. Why social relationships are important for physical health: a systems approach to understanding and modifying risk and protection. Annu Rev Psychol. 2018;69:437-458. doi: 10.1146/annurev-psych-122216-011902 [DOI] [PubMed] [Google Scholar]
- 7.Australian Psychological Society. Stress and wellbeing: how Australians are coping with life. Published November 2015. Accessed December 30, 2020. https://www.headsup.org.au/docs/default-source/default-document-library/stress-and-wellbeing-in-australia-report.pdf?sfvrsn=7f08274d_4
- 8.Cohen S, Janicki-Deverts D, Miller GE. Psychological stress and disease. JAMA. 2007;298:1685-1687. [DOI] [PubMed] [Google Scholar]
- 9.Lianov LS, Fredrickson BL, Barron C, Krishnaswami J, Wallace A. Positive psychology in lifestyle medicine and health care: strategies for implementation. Am J Lifestyle Med. 2019;13):480-486. doi: 10.1177/1559827619838992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Russ TC, Stamatakis E, Hamer M, Starr JM, Kivimäki M, Batty GD. Association between psychological distress and mortality: individual participant pooled analysis of 10 prospective cohort studies. BMJ. 2012;345:e4933. doi: 10.1136/bmj.e4933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brotman DJ, Golden SH, Wittstein IS. The cardiovascular toll of stress. Lancet. ]2007;370:1089-100. doi: 10.1016/s0140-6736(07)61305-1 [DOI] [PubMed] [Google Scholar]
- 12.Furman D, Campisi J, Verdin E, et al. Chronic inflammation in the etiology of disease across the life span. Nat Med. 2019;25:1822-1832. doi: 10.1038/s41591-019-0675-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cohen S, Gianaros PJ, Manuck SB. A stage model of stress and disease. Perspect Psychol Sci. 2016;11:456-63. doi: 10.1177/1745691616646305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gianaros PJ, Jennings JR. Host in the machine: a neurobiological perspective on psychological stress and cardiovascular disease. Am Psychol. Nov 2018;73:1031-1044. doi: 10.1037/amp0000232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kiecolt-Glaser JK, Gouin JP, Hantsoo L. Close relationships, inflammation, and health. Neurosci Biobehav Rev. 2010;35:33-38. doi: 10.1016/j.neubiorev.2009.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Slavich GM, Irwin MR. From stress to inflammation and major depressive disorder: a social signal transduction theory of depression. Psychol Bull. 2014;140:774-815. doi: 10.1037/a0035302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ironson G, O’Cleirigh C, Fletcher MA, et al. Psychosocial factors predict CD4 and viral load change in men and women with human immunodeficiency virus in the era of highly active antiretroviral treatment. Psychosom Med. 2005;67:1013-1021. doi: 10.1097/01.psy.0000188569.58998.c8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Link BG, Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav. 1995;spec no:80-94. [PubMed] [Google Scholar]
- 19.Matrix, Share Our Insight. Economic analysis of workplace mental health promotion and mental disorder prevention programmes and of their potential contribution to EU health, social and economic policy objectives. Published May 2013. Accessed December 30, 2020. https://ec.europa.eu/health/sites/health/files/mental_health/docs/matrix_economic_analysis_mh_promotion_en.pdf
- 20.Hassard J, Teoh KRH, Visockaite G, Dewe P, Cox T. The cost of work-related stress to society: a systematic review. J Occup Health Psychol. 2018;23:1-17. doi: 10.1037/ocp0000069 [DOI] [PubMed] [Google Scholar]
- 21.Goh J, Pfeffer J, Zenios SA. The relationship between workplace stressors and mortality and health costs in the United States. Manag Sci. 2016/02/01 2015;62:608-628. doi: 10.1287/mnsc.2014.2115 [DOI] [Google Scholar]
- 22.Holt-Lunstad J. The potential public health relevance of social isolation and loneliness: prevalence, epidemiology, and risk factors. Public Policy Aging Rep. 2018;27:127-130. doi: 10.1093/ppar/prx030 [DOI] [Google Scholar]
- 23.Holt-Lunstad J, Smith TB, Baker M, Harris T, Stephenson D. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect Psychol Sci. 2015;10:227-237. doi: 10.1177/1745691614568352 [DOI] [PubMed] [Google Scholar]
- 24.Cacioppo JT, Cacioppo S. The growing problem of loneliness. Lancet. 2018;391:426. doi: 10.1016/s0140-6736(18)30142-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Graham J. Understanding loneliness in older adults—and tailoring a solution. Published March 14, 2019. Accessed December 30, 2020. https://khn.org/news/understanding-loneliness-in-older-adults-and-tailoring-a-solution/
- 26.Cohen S. Social relationships and health. Am Psychol. 2004;59:676-684. doi: 10.1037/0003-066x.59.8.676 [DOI] [PubMed] [Google Scholar]
- 27.Eisenberger NI, Taylor SE, Gable SL, Hilmert CJ, Lieberman MD. Neural pathways link social support to attenuated neuroendocrine stress responses. Neuroimage. 2007;35:1601-1612. doi: 10.1016/j.neuroimage.2007.01.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Eisenberger NI, Moieni M, Inagaki TK, Muscatell KA, Irwin MR. In sickness and in health: the co-regulation of inflammation and social behavior. Neuropsychopharmacology. 2017;42:242-253. doi: 10.1038/npp.2016.141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Uchino BN, Holt-Lunstad J, Bloor LE, Campo RA. Aging and cardiovascular reactivity to stress: longitudinal evidence for changes in stress reactivity. Psychol Aging. 2005;20:134-143. doi: 10.1037/0882-7974.20.1.134 [DOI] [PubMed] [Google Scholar]
- 30.Uchino BN, Cacioppo JT, Kiecolt-Glaser JK. The relationship between social support and physiological processes: a review with emphasis on underlying mechanisms and implications for health. Psychol Bull. 1996;119:488-531. doi: 10.1037/0033-2909.119.3.488 [DOI] [PubMed] [Google Scholar]
- 31.Inagaki TK, Haltom KEB, Suzuki S, et al. The neurobiology of giving versus receiving support: the role of stress-related and social reward-related neural activity. Psychosom Med. 2016;78:443-453. doi: 10.1097/psy.0000000000000302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cacioppo JT, Cacioppo S. Social relationships and health: the toxic effects of perceived social isolation. Soc Personal Psychol Compass. 2014;8:58-72. doi: 10.1111/spc3.12087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Keltner D, Kogan A, Piff PK, Saturn SR. The sociocultural appraisals, values, and emotions (SAVE) framework of prosociality: core processes from gene to meme. Annu Rev Psychol. 2014;65:425-460. doi: 10.1146/annurev-psych-010213-115054 [DOI] [PubMed] [Google Scholar]
- 34.Layous K, Nelson SK, Oberle E, Schonert-Reichl KA, Lyubomirsky S. Kindness counts: prompting prosocial behavior in preadolescents boosts peer acceptance and well-being. PLoS One. 2012;7:e51380. doi: 10.1371/journal.pone.0051380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Son D, Padilla-Walker LM. Happy helpers: a multidimensional and mixed-method approach to prosocial behavior and its effects on friendship quality, mental health, and well-being during adolescence. J Happ Stud. 2020;21:1705-1723. doi: 10.1007/s10902-019-00154-2 [DOI] [Google Scholar]
- 36.Oveis C, Horberg EJ, Keltner D. Compassion, pride, and social intuitions of self-other similarity. J Pers Soc Psychol. 2010;98:618-630. doi: 10.1037/a0017628 [DOI] [PubMed] [Google Scholar]
- 37.Stellar JE, Gordon AM, Piff PK, et al. Self-transcendent emotions and their social functions: compassion, gratitude, and awe bind us to others through prosociality. Emotion Rev. 2017;9:200-207. doi: 10.1177/1754073916684557 [DOI] [Google Scholar]
- 38.Cialdini RB, Brown SL, Lewis BP, Luce C, Neuberg SL. Reinterpreting the empathy-altruism relationship: when one into one equals oneness. J Pers Soc Psychol. 1997;73:481-494. [PubMed] [Google Scholar]
- 39.Fredrickson BL, Kok BE. Evidence for the upward spiral stands steady: a response to Nickerson (2018). Psychol Sci. 2018;29:467-470. doi: 10.1177/0956797617707319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Drouvelis M, Grosskopf B. The effects of induced emotions on pro-social behaviour. J Public Econ. 2016;134:1-8. doi: 10.1016/j.jpubeco.2015.12.012 [DOI] [Google Scholar]
- 41.Twenge JM, Baumeister RF, DeWall CN, Ciarocco NJ, Bartels JM. Social exclusion decreases prosocial behavior. J Pers Soc Psychol. 2007;92:56-66. doi: 10.1037/0022-3514.92.1.56 [DOI] [PubMed] [Google Scholar]
- 42.Twenge JM, Baumeister RF, Tice DM, Stucke TS. If you can’t join them, beat them: effects of social exclusion on aggressive behavior. J Pers Soc Psychol. 2001;81:1058-1069. doi: 10.1037/0022-3514.81.6.1058 [DOI] [PubMed] [Google Scholar]
- 43.Aknin LB, Dunn EW, Norton MI. Happiness runs in a circular motion: evidence for a positive feedback loop between prosocial spending and happiness. J Happ Stud. 2012;13:347-355. doi: 10.1007/s10902-011-9267-5 [DOI] [Google Scholar]
- 44.Layous K, Nelson SK, Kurtz JL, Lyubomirsky S. What triggers prosocial effort? A positive feedback loop between positive activities, kindness, and well-being. J Posit Psychol. 2017;12:385-398. doi: 10.1080/17439760.2016.1198924 [DOI] [Google Scholar]
- 45.Algoe SB, Haidt J. Witnessing excellence in action: the 'other-praising' emotions of elevation, gratitude, and admiration. J Posit Psychol. 2009;4:105-127. doi: 10.1080/17439760802650519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Oliver MB, Kim K, Hoewe J, et al. Media-induced elevation as a means of enhancing feelings of intergroup connectedness. J Soc Issues. 2015;71:106-122. doi: 10.1111/josi.12099 [DOI] [Google Scholar]
- 47.Oliver MB, Raney AA, Slater MD, et al. Self-transcendent media experiences: taking meaningful media to a higher level. J Commun. 2018;68:380-389. doi: 10.1093/joc/jqx020 [DOI] [Google Scholar]
- 48.Blomster Lyshol JK, Thomsen L, Seibt B. Moved by observing the love of others: kama muta evoked through media fosters humanization of out-groups. Front Psychol. 2020;11:1240. doi: 10.3389/fpsyg.2020.01240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Inagaki TK, Irwin MR, Eisenberger NI. Blocking opioids attenuates physical warmth-induced feelings of social connection. Emotion. 2015;15:494-500. doi: 10.1037/emo0000088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Howell RT, Kern ML, Lyubomirsky S. Health benefits: meta-analytically determining the impact of well-being on objective health outcomes. Health Psychol Rev. 20072007;1:83-136. doi: 10.1080/17437190701492486 [DOI] [Google Scholar]
- 51.Trudel-Fitzgerald C, Millstein RA, von Hippel C, et al. Psychological well-being as part of the public health debate? Insight into dimensions, interventions, and policy. BMC Public Health. 2019;19:1712. doi: 10.1186/s12889-019-8029-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kubzansky LD, Huffman JC, Boehm JK, et al. Positive psychological well-being and cardiovascular disease: JACC health promotion series. J Am Coll Cardiol. 2018;72:1382-1396. doi: 10.1016/j.jacc.2018.07.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Jenkinson CE, Dickens AP, Jones K, et al. Is volunteering a public health intervention? A systematic review and meta-analysis of the health and survival of volunteers. BMC Public Health. 2013;13:773. doi: 10.1186/1471-2458-13-773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Brown SL, Smith DM, Schulz R, et al. Caregiving behavior is associated with decreased mortality risk. Psychol Sci. 2009;20:488-494. doi: 10.1111/j.1467-9280.2009.02323.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Fredman L, Cauley JA, Hochberg M, Ensrud KE, Doros G. Mortality associated with caregiving, general stress, and caregiving-related stress in elderly women: results of caregiver-study of osteoporotic fractures. J Am Geriatr Soc. 2010;58:937-943. doi: 10.1111/j.1532-5415.2010.02808.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kim S, Ferraro KF. Do productive activities reduce inflammation in later life? Multiple roles, frequency of activities, and C-reactive protein. Gerontologist. 2014;54:830-839. doi: 10.1093/geront/gnt090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Nelson-Coffey SK, Fritz MM, Lyubomirsky S, Cole SW. Kindness in the blood: a randomized controlled trial of the gene regulatory impact of prosocial behavior. Psychoneuroendocrinology. 2017;81:8-13. doi: 10.1016/j.psyneuen.2017.03.025 [DOI] [PubMed] [Google Scholar]
- 58.Marsh AA. Neural, cognitive, and evolutionary foundations of human altruism. Wiley Interdiscip Rev Cogn Sci. 2016;7:59-71. doi: 10.1002/wcs.1377 [DOI] [PubMed] [Google Scholar]
- 59.Bernhardt BC, Singer T. The neural basis of empathy. Annu Rev Neurosci. 2012;35:1-23. doi: 10.1146/annurev-neuro-062111-150536 [DOI] [PubMed] [Google Scholar]
- 60.Trzeciak S, Mazzarelli A, Booker C. Compassionomics: The Revolutionary Scientific Evidence That Caring Makes a Difference. Studer Group; 2019. [Google Scholar]
- 61.Greene J, Ramos C. A mixed methods examination of health care provider behaviors that build patients’ trust. Patient Educ Couns. Published online September 12, 2020. doi: 10.1016/j.pec.2020.09.003 [DOI] [PubMed] [Google Scholar]
- 62.Greene J, Hibbard JH. Why does patient activation matter? An examination of the relationships between patient activation and health-related outcomes. J Gen Intern Med. 2012;27:520-526. doi: 10.1007/s11606-011-1931-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Greene J, Hibbard JH, Sacks R, Overton V, Parrotta CD. When patient activation levels change, health outcomes and costs change, too. Health Aff (Millwood). 2015;34:431-437. doi: 10.1377/hlthaff.2014.0452 [DOI] [PubMed] [Google Scholar]
- 64.Hojat M, Louis DZ, Markham FW, Wender R, Rabinowitz C, Gonnella JS. Physicians’ empathy and clinical outcomes for diabetic patients. Acad Med. 2011;86:359-364. doi: 10.1097/ACM.0b013e3182086fe1 [DOI] [PubMed] [Google Scholar]
- 65.Hojat M, Maio V, Markham FW, Louis DZ, Gonnella JS. Physician empathy and diabetes outcomes. J Gen Intern Med. 2019;34:1966. doi: 10.1007/s11606-019-05187-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Twenge JM, Miller JD, Campbell WK. The narcissism epidemic: commentary on modernity and narcissistic personality disorder. Personal Disord. 2014;5:227-229. doi: 10.1037/per0000008 [DOI] [PubMed] [Google Scholar]
- 67.Paris J. Modernity and narcissistic personality disorder. Personal Disord. 2014;5:220-226. doi: 10.1037/a0028580 [DOI] [PubMed] [Google Scholar]
- 68.Krämer N, Eimler SC, Neubaum G, Winter S, Rösner L, Oliver MB. Broadcasting one world: how watching online videos can elicit elevation and reduce stereotypes. New Media Soc. 2017;19:1349-1368. doi: 10.1177/1461444816639963 [DOI] [Google Scholar]
- 69.Schnall S, Roper J, Fessler DM. Elevation leads to altruistic behavior. Psychol Sci. 2010;21:315-320. doi: 10.1177/0956797609359882 [DOI] [PubMed] [Google Scholar]
- 70.Freeman D, Aquino K, McFerran B. Overcoming beneficiary race as an impediment to charitable donations: social dominance orientation, the experience of moral elevation, and donation behavior. Pers Soc Psychol Bull. 2009;35:72-84. doi: 10.1177/0146167208325415 [DOI] [PubMed] [Google Scholar]
- 71.Rowland L, Curry OS. A range of kindness activities boost happiness. J Soc Psychol. 2019;159:340-343. doi: 10.1080/00224545.2018.1469461 [DOI] [PubMed] [Google Scholar]
- 72.National Academy of Medicine Action Collaborative on Clinician Well-Being and Resinlience. Clinician well-being is essential for safe, high-quality patient care. Accessed December 30, 2020. https://nam.edu/initiatives/clinician-resilience-and-well-being/
- 73.Fryburg DA, Ureles S, Myrick JG, Dillman-Carpentier F, Oliver MB. Kindness media rapidly inspires viewers and increases happiness, calm, gratitude, and generosity in a health care setting. Front Psychol. In press. 10.3389/fpsyg.2020.591942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Johnston WM, Davey GCL. The psychological impact of negative TV news bulletins: the catastrophizing of personal worries. Br J Psychol. 1997;88:85-91. doi: 10.1111/j.2044-8295.1997.tb02622.x [DOI] [PubMed] [Google Scholar]
- 75.Efrat-Treister D, Cheshin A, Harari D, et al. How psychology might alleviate violence in queues: perceived future wait and perceived load moderate violence against service providers. PLoS One. 2019;14:e0218184. doi: 10.1371/journal.pone.0218184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Patel S, Pelletier-Bui A, Smith S, et al. Curricula for empathy and compassion training in medical education: A systematic review. PLoS One. 2019;14(8):e0221412. Published 2019. Aug 22. doi: 10.1371/journal.pone.0221412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Lown BA. A social neuroscience-informed model for teaching and practicing compassion in health care. Med Educ. 2016;50:332-42. doi: 10.1111/medu.12926.PMID:26896018. [DOI] [PubMed] [Google Scholar]
- 78.Srull TK, Wyer RS. The role of category accessibility in the interpretation of information about persons: some determinants and implications. J Pers Soc Psychol. 1979;37:1660-1672. doi: 10.1037/0022-3514.37.10.1660 [DOI] [Google Scholar]
- 79.Sheeran P, Gollwitzer PM, Bargh JA. Nonconscious processes and health. Health Psychol. 2013;32:460-473. doi: 10.1037/a0029203 [DOI] [PubMed] [Google Scholar]
- 80.Peled-Avron L, Goldstein P, Yellinek S, Weissman-Fogel I, Shamay-Tsoory SG. Empathy during consoling touch is modulated by mu-rhythm: an EEG study. Neuropsychologia. 2018;116(pt A):68-74. doi: 10.1016/j.neuropsychologia.2017.04.026 [DOI] [PubMed] [Google Scholar]
- 81.de Waal FB. Putting the altruism back into altruism: the evolution of empathy. Annu Rev Psychol. 2008;59:279-300. doi: 10.1146/annurev.psych.59.103006.093625 [DOI] [PubMed] [Google Scholar]
- 82.Ekman P. Darwin’s compassionate view of human nature. JAMA. 2010;303:557-558. doi: 10.1001/jama.2010.101 [DOI] [PubMed] [Google Scholar]
- 83.Hostinar CE, Sullivan RM, Gunnar MR. Psychobiological mechanisms underlying the social buffering of the hypothalamic-pituitary-adrenocortical axis: a review of animal models and human studies across development. Psychol Bull. 2014;140:256-282. doi: 10.1037/a0032671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Inagaki TK. Neural mechanisms of the link between giving social support and health. Ann N Y Acad Sci. 2018;1428:33-50. doi: 10.1111/nyas.13703 [DOI] [PubMed] [Google Scholar]
- 85.Christakis NA, Fowler JH. Social contagion theory: examining dynamic social networks and human behavior. Stat Med. 2013;32:556-577. doi: 10.1002/sim.5408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Barsade SG. The ripple effect: emotional contagion and its influence on group behavior. Admin Sci Q. 2002;47:644-675. doi: 10.2307/3094912 [DOI] [Google Scholar]
- 87.Chartrand TL, Lakin JL. The antecedents and consequences of human behavioral mimicry. Annu Rev Psychol. 2013;64:285-308. doi: 10.1146/annurev-psych-113011-143754 [DOI] [PubMed] [Google Scholar]
- 88.Lehmann L, Keller L. The evolution of cooperation and altruism–a general framework and a classification of models. J Evol Biol. 2006;19:1365-1376. doi: 10.1111/j.1420-9101.2006.01119.x [DOI] [PubMed] [Google Scholar]
- 89.Warneken F. Insights into the biological foundation of human altruistic sentiments. Curr Opin Psychol. 2016;7:51-56. doi: 10.1016/j.copsyc.2015.07.013 [DOI] [Google Scholar]
- 90.Ehlebracht D, Stavrova O, Fetchenhauer D, Farrelly D. The synergistic effect of prosociality and physical attractiveness on mate desirability. Br J Psychol. 2018;109:517-537. doi: 10.1111/bjop.12285 [DOI] [PubMed] [Google Scholar]
- 91.Light KC, Grewen KM, Amico JA. More frequent partner hugs and higher oxytocin levels are linked to lower blood pressure and heart rate in premenopausal women. Biol Psychol. 2005;69:5-21. doi: 10.1016/j.biopsycho.2004.11.002 [DOI] [PubMed] [Google Scholar]
- 92.Field T. Touch for socioemotional and physical well-being: a review. Dev Rev. 2010;30:367-383. doi: 10.1016/j.dr.2011.01.001 [DOI] [Google Scholar]