Abstract
Eating foods high in added sugar has recently increased among people of all ages. This is expected to negatively affect health and life quality. This study was conducted to investigate the relationship between added sugar intake and sleep quality among university students. A total of 100 randomly selected female students (19-25 years old) from Imam Abdulrahman Bin Faisal University, Dammam, Saudi Arabia, participated in the study after applying exclusion criteria. Sample size was calculated with expected correlation of −0.4 between sugar intake and sleep quality, a power of 90%, and a type 1 error of 5%. Participants completed the Food Frequency Questionnaire (FFQ), sleep quality questionnaire, and 24-hour dietary recall. Data were analyzed using IBM SPSS Statistics 25, and the χ2 test was used for measuring the association between added sugar intake and sleep quality, where P <.05 was considered statistically significant. Results showed that only 17% of participants had good sleep. Data of the 24-hour dietary recall showed a significant association (P = .014) between consumption of added sugars and sleep quality. This is the first study to directly report on the effect of higher intake of added sugars on sleep quality. The study concluded that poor sleep quality was significantly related to higher added sugar intake.
Keywords: added sugars, sleep quality, university students, food frequency questionnaire, 24-hour dietary recall
‘Consuming high amounts of added sugar increases heart disease, diabetes, and cancer risk factors such as obesity, high blood pressure, insulin resistance, and inflammation.’
Introduction
The lifestyle and eating habits of Saudis have radically changed over the past few decades; the calorie intake has progressively increased, resulting in high obesity rates and other health consequences. 1 Foods containing added sugar are getting popular, widespread, and heavily consumed, especially with the vast change in the nutrition pattern and the entire lifestyle and the prevalence of fast or junk foods. Added sugar is the type of sugar that is not naturally found in food but is introduced as an ingredient of processed food products such as candy, cookies, desserts, cakes, sweets, junk foods, and sugar-sweetened beverages (SSBs). 2 Per the World Health Organization (WHO) report, 3 added sugar consumption was associated with various health concerns, and the recommended daily intake is less than 10% of the total energy intake in both adults and children. Consuming high amounts of added sugar increases heart disease, diabetes, and cancer risk factors such as obesity, high blood pressure, insulin resistance, and inflammation.4-10 It may further increase depression11,12 and skin and cellular aging13-15 and augment fat build up in the liver. 16 Other venomous effects include worsening cognitive abilities, 17 increasing gout risk, 18 harming kidneys, 19 causing dental cavities, 20 and raising the risk of developing acne. 21
Effects of diet on sleep quality have been explored.22,23 It is evident that high-carbohydrate intake is associated with reduced sleep quality.24,25 Inadequate or poor sleeping has adverse effects on human health, including body weight and insulin resistance.26-28 A prospective cohort study was conducted to examine the effect of sleep duration on weight gain and obesity among 3576 (1411 male and 1824 female) older Spanish adults aged ≥60 years. The results showed a negative impact of sleep duration on obesity and weight gain. Female participants sleeping 5 hours or less had more weight gain and obesity rates. 29
In the current study, the researchers thought that university female students might suffer from lack of sleep, irregular sleep onset, or inadequate sleep duration. This may be attributed to the vast change in the nutrition pattern and lifestyle as well as the challenges and circumstances faced by university students. 30 Up to 60% of university students were reported to suffer from poor sleep quality according to the Pittsburgh Sleep Quality Index. 31 In an intervention study to investigate sleep problems among university students, Schlarb et al 32 stated that 74% of the participants reported symptoms of an insomnia disorder, and 51.9% fulfilled all criteria of an insomnia disorder according to the Diagnostic and Statistical Manual of Mental Disorders.
Despite the evident negative effect of high-carbohydrate intake on sleep quality,22-25 studies that specifically relate the excessive intake of added sugar to sleep quality are scarce. Sampasa-Kanyinga et al 33 studied the relationship between the duration of sleep and the consumption of SSBs among 9473 male and female adolescents aged between 11 and 20 years. Short sleep duration was associated with consumption of SSBs in middle school students. The association between self-reported sleep duration and the consumption of SSBs by US adults (≥18 years old) was also investigated by Prather et al. 34 Among 18 779 participants, those who slept 5 hours or less were found to have 21% higher SSB consumption. This excessive consumption was attributed mainly to caffeinated sugary beverages. It was not clear whether the impaired sleep was a cause or a result of the high consumption of caffeinated sugary drinks.
In another cross-sectional study, Park et al 35 investigated the relationship between the consumption of energy drinks and sleep dissatisfaction, stress, and depression among 68 043 Korean adolescents aged between 12 and 18 years. It was concluded that the consumption of energy drinks had adverse effects on sleep quality, stress, and mood. An immediate effect of a high-sugar diet on sleep quality in prepubescent girls (10-12 years old) was also reported. 36
The negative effects of consuming high-sugar-containing foods on sleep duration and quality will consequently cause adverse effects on general health, weight gain, and obesity rates. The aim of this research was, therefore, to investigate the effect of excessive consumption of added sugar-containing foods on the quality of sleep among university female students.
Methods
A cross-sectional study design was used in this work, and samples were selected using the convenience sampling method. The sample size was calculated for testing the correlation between sugar intake and sleep quality, with expected correlation as −0.4, power as 90%, and type 1 error as 5%; the minimum number required for the study was 54. Hence, 138 randomly selected female participants (19 to 25 years old) from the College of Applied Studies and Community Service at Imam Abdulrahman Bin Faisal University (IAU), Dammam, Saudi Arabia, were included in the study after giving written consent. The data were collected from December 2018 to March 2019. Weight and height of the participants were taken using Aurora Blue TANITA inner scan 50 (BC-310-BL, Tanita Corporation of America Inc, IL) and ADE M318800 mechanical physician Scale (ADE, Hamburg, Germany), respectively, to calculate the body mass index (BMI; kg/m2).
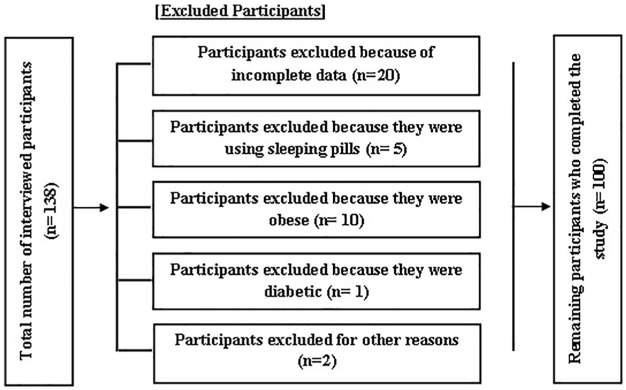
According to the WHO classification 37 the BMI of normal, overweight, and obese adults is 18.5 to 24.9, 25.0 to 29.9, and ≥30.0, respectively. Obese (BMI ≥ 30 kg/m2) participants and those with diabetes were excluded to eliminate the confounding effect of obesity and diabetes on sleep. Obesity and diabetes have been associated with poor sleep quality and sleep disturbances that are mainly attributed to the concomitant sleep disordered breathing, including obstructive sleep apnea, restless leg syndrome, insomnia, nocturia, and nocturnal hypoglycemia.38,39 The degree of obesity was reported to predict sleep disturbances among obese adolescents. 40 Pregnant and lactating individuals were excluded to rule out the possible effects of hormonal, physiological, psychological, and anatomical changes during pregnancy and lactation. These changes may affect the sleeping patterns of participants.37,41 Those taking sleeping pills were also excluded. After applying all the exclusion criteria, the total number of participants was 100 (Figure 1).
Figure 1.
Screening of participants for potential inclusion in the present study.
Two questionnaires were given to the included participants: Food Frequency Questionnaire (FFQ), containing 57 items with quantities and number of grams of sugar in each item, and Sleep Quality Questionnaire to measure sleep duration and other problems that affect its quality. Reliability analysis of the FFQ was obtained using the split half method. Split-;half correlation of the data was 0.86, and the Cronbach’s α value of the covariance matrix was .91, which means high reliability. The validity of the FFQ data was obtained using the Pearson product moment method. There was a good correlation between the item score and total score, and the average correlation of the data was higher than the table value (5% level of significance), which proves the validity of the FFQ for the study. The collected scores from the FFQ were classified into 3 groups: <100, low sugar intake; 100 to 199, moderate sugar intake; 200 to 299, high sugar intake. The participants were further contacted to fill in a 24-hour dietary recall for 2 days (1 weekday and 1 weekend). Data collected from 24-hour dietary recall were analyzed using ESHA’s Food Processor Nutrition Analysis software (Version 11.5). Based on the collected data, the participants were classified into 4 groups based on the contribution of added sugars and total carbohydrates to their total energy intake; group A: carbohydrates >60%, added sugars >10%; group B: carbohydrates <60%, added sugars >10%; group C: carbohydrates >60%, added sugars <10%; or group D: carbohydrates <60%, added sugars <10%. Caffeine consumption was found to be very common among participants. Therefore, participants were divided into 2 groups caffeine consumers and non–caffeine consumers, to study the association between sleep quality and the different levels of added sugars in each group separately and, thus, eliminate the effect of caffeine consumption as a possible confounding factor. Sleeping period from 7 to 8½ hours continuously at night without suffering from insomnia or inability to sleep, taking less than 15 minutes to fall asleep, and not using sleeping pills were considered as determinants of good quality sleep in this study. The experimental protocol and informed consent were approved by the Institutional Review Board of IAU (IRB-UGS014-03-2019).
The statistical analysis was done using Microsoft Excel Worksheet and IBM SPSS Statistics 25 software. Frequency tables and descriptive statistics were used for the data description. The association between added sugar and sleep quality was tested using a χ2 test. Logistic regression analysis was performed to estimate the risk for poor sleep among participants with high sugar consumption, and odds ratios with its 95% CIs were presented. The bar-plot is used for the graphical representations, and a P value <.05 was considered as statistically significant.
Results
Distribution of the Participants Based on Their Sleep Quality
This study involved 100 participants from the college of Applied Studies and Community Service at IAU. All of them were women from 19 to 23 years of age, with a mean age of 20 years and SD of 1 year. Good-quality sleep involves many variables that may affect the sleeping pattern. According to the sleep quality criteria used in this study, the participants were classified into 2 groups: those with either good or bad quality sleep. In our study, 17% of the participants reported good quality sleep, whereas 83% of participants had bad quality sleep.
The Association Between Added Sugar Intake and Sleep Quality Based on 24-Hour Dietary Recall
Based on the collected data from 24-hour dietary recall, 13%, 59%, 5%, and 23% of the participants were from groups A, B, C, and D, respectively. We observed an inverse significant relation between added sugar intake and sleep quality based on 24-hour dietary recall data (P = .017; Table 1). This is explained by the fact that the group with the high sugar consumption (group A) showed a higher percentage of participants with poor quality sleep compared with the low-sugar-intake group (group D); that is, with high sugar intake, 100% of the participants had poor quality sleep, whereas with low sugar intake, only 65.2% of the participants had poor quality sleep (Table 1). Furthermore, the odds ratio of the association between sleep quality and sugar intake showed that the participants with high sugar intake (groups A and B) had 3.5 times the probability for having poor sleep (or were 3.5 times more likely to have poor sleep quality) compared with those with low sugar intake (groups C and D; P = .021; Table 2).
Table 1.
Relationship Between Sleep Quality and Intake of Added Sugars Based on 24-Hour Dietary Recall. a
| Sleep Quality | P Value | ||
|---|---|---|---|
| Good, n (%) | Poor, n (%) | ||
| Group A | 0 (0%) | 13 (100%) | .039 |
| Group B | 8 (13.6%) | 51(86.4%) | |
| Group C | 1 (20%) | 4 (80%) | |
| Group D | 8 (34.8%) | 15 (65.2%) | |
Group A: carbohydrates >60%, added sugars >10%; group B: carbohydrates <60%, added sugars >10%; group C: carbohydrates >60%, added sugars <10%; group D: carbohydrates <60%, added sugars <10%.
Table 2.
The Odds of the Association Between Sleep Quality and Sugar Intake. a
| Energy Intake From Added Sugars | Sleep Quality | Odds Ratio (95% CI) | P Value | |
|---|---|---|---|---|
| Good, n (%) | Poor, n (%) | |||
| High sugar (≥10%; groups A + B) | 20 (69%) | 9 (31%) | 3.5 (1.2, 10.4) | .021 |
| Low sugar (<10%; groups C + D) | 63 (89%) | 8 (11%) | 1.0* | |
Group A: carbohydrates >60%, added sugars >10%; group B: carbohydrates <60%, added sugars >10%; group C: carbohydrates >60%, added sugars <10%; group D: carbohydrates <60% added sugars <10%. *1.0 is the notation for the reference category (low sugar group). We are investigating the risk of poor sleep if the person is taking high sugar with reference to the low sugar subjects.
To further investigate the relation between added sugar intakes and sleep quality, we studied whether the subsequent increase in energy intake from added sugars would be associated with poor quality sleep. We divided the participants into 4 groups depending on their percentage of daily energy intake from the added sugars based on the 24-hour dietary recall (Table 3): <10% (n = 29), 10% to 20% (n = 47), 20% to 30% (n = 20), >30% (n = 4). Despite the insignificant association (P = .099), sleep enjoyment tended to decrease as the energy intake from added sugar increased. This was mostly evident with the group of the highest energy intake from added sugars (>30%): 100% of the participants who consumed >30 % of their energy intake from added sugar had poor quality sleep (ie, none of the participants reported good quality sleep), whereas only 69% of the participants who consumed <10 % of their energy intake from added sugar had poor quality sleep. This again suggests an inverse relation between added sugar intake and sleep quality.
Table 3.
Effect of Increased Energy Intake From Added Sugars on the Quality of Sleep, Based on 24-Hour Dietary Recall.
| Energy Intake From Added Sugars | Sleep Quality | Test Statistic a | P Value | |
|---|---|---|---|---|
| Good, n (%) | Poor, n (%) | |||
| <10% | 9 (31%) | 20 (69%) | 6.272 | .099 |
| 10%-20% | 5 (10.6%) | 42 (89.4%) | ||
| 20%-30% | 3 (15%) | 17 (85%) | ||
| >30% | 0 (0%) | 4 (100%) | ||
Pearson χ2 statistic.
The Association Between Added Sugar Intake and Sleep Quality Based on FFQ
Based on the data from the FFQ, there was a tendency toward an inverse association between the intake of added sugar and sleep quality that did not reach significance. Based on the collected scores from the FFQ, participants were classified into 3 groups: <100, low sugar intake; 100 to 199, moderate sugar intake; 200 to 299, high sugar intake (Table 4). Despite the insignificant association (P = .15), the percentage of participants from the bad quality sleep group tended to be lower in the low-sugar-intake group compared with the moderate- and high-sugar-intake groups.
Table 4.
Relationship Between Sleep Quality and Intake of Added Sugars Based on the FFQ. a
| Collected Scores | Sleep Quality | P Value | |
|---|---|---|---|
| Good, n (%) | Poor, n (%) | ||
| <100 | 13 (23.2%) | 43 (76.8%) | .15 |
| 100-199 | 3 (7.9%) | 35 (92.1%) | |
| 200-299 | 1 (16.7%) | 5 (83.3%) | |
Abbreviation: FFQ, Food Frequency Questionnaire.
<100, Low sugar intake; 100-199, moderate sugar intake; 200-299, high sugar intake.
The Effect of Caffeine Intake as a Confounding Factor
Our results showed that caffeine intake was very common among the study group (66% of participants). Therefore, we thought of the caffeine intake as a possible confounding factor in our experiment. To overcome this limitation, we divided the participants into 2 groups based on their caffeine intake—caffeine consuming and non–caffeine consuming—and then looked at the association between the sleep quality and the different levels of added sugars in each group.
The results of the 24-hour dietary recall revealed a clear association between high added sugar intake and the quality of sleep in the caffeine-consuming group. Data showed that 100% of group A participants suffered from poor sleep, whereas only 40% of group D reported poor-quality sleep (P = .034; Table 5). On the other hand, in the non–caffeine-consuming group, there was no association between sugar intake and sleep quality. The percentages of the participants with poor or good quality sleep did not significantly differ among all the levels of sugar intake (Table 5).
Table 5.
The Association Between Sleep Quality and Added Sugar Intake Based on 24-Hour Dietary Recall in Both Caffeine and Non–Caffeine Consumers. a
| Caffeine Consuming | P Value | Non–Caffeine Consuming | P Value | |||
|---|---|---|---|---|---|---|
| Sleep Quality | Sleep Quality | |||||
| Good, n (%) | Poor, n (%) | Good, n (%) | Poor, n (%) | |||
| Group A | 0 (0%) | 9 (100%) | .572 | 0 (0%) | 4 (100%) | .034 |
| Group B | 3 (15%) | 35 (87%) | 3 (16%) | 16 (84%) | ||
| Group C | 1 (25%) | 3 (75%) | 0 (0%) | 1 (100%) | ||
| Group D | 2 (15%) | 11 (85%) | 6 (60%) | 4 (40%) | ||
Group A: carbohydrates >60%, added sugars >10%; group B: carbohydrates <60%, added sugars >10%; group C: carbohydrates >60%, added sugars <10%; group D: carbohydrates <60%, added sugars <10%.
To further investigate the relation between added sugar intake and sleep quality with and without caffeine consumption, based on the FFQ data, the participants were again divided into 2 groups: caffeine- and non–caffeine-consuming groups (Table 6). In the caffeine-consuming group, whereas the relationship between sleep quality and added sugar intake was inverse and consistent (reflected by the percentage of participants from both the good- and poor-quality sleep groups), it did not reach significance (P = .43). In the non–caffeine-consuming group, comparison of the percentage of participants in the poor- or good-quality sleep group among the 3 groups of sugar intake (high, moderate, and low) showed an inconsistent and nonsignificant association between sleep quality and sugar intake as well (P = .28; Table 6).
Table 6.
Effect of High Intake of Added Sugars on Sleep Quality Based on the FFQ Assessment in Both Caffeine and Non–Caffeine Consumers.
| Count (Percentage Within FFQ) | Caffeine Consuming | P Value | Non–Caffeine Consuming | P Value | ||
|---|---|---|---|---|---|---|
| Sleep Quality | Sleep Quality | |||||
| Good, n (%) | Poor, n (%) | Good, n (%) | Poor, n (%) | |||
| >100 | 6 (16.7%) | 30 (83.3%) | .43 | 7 (35%) | 13 (65%) | .28 |
| 100-199 | 2 (7.4%) | 25 (92.6%) | 1 (9.1%) | 10 (90.9%) | ||
| 199-299 | 0 (0%) | 3 (100%) | 1 (33.3%) | 2 (66.7%) | ||
Abbreviation: FFQ, Food Frequency Questionnaire.
Discussion
To the best of our knowledge, this is the first study to address several aspects of assessing the quality of sleep and report on its association with the high intake of added sugars among Saudi University students. The reason for choosing to study the sleep quality in university students is that there are various factors that affect sleep quality at this developmental stage of life. Adolescents’ inadequate sleep duration has been an increasing concern.28,42 Over the past 20 years, a sharper decrease in sleep time was reported for adolescents compared with adults and children.28,42 The use of technological devices and the excessive exposure to artificial light, the stress faced by university students caused by prolonged and intensive homework, afterschool activities or work, the high consumption of caffeinated beverages or energy drinks, or simply the perception that sleep is a wasted time are among the factors that promote inadequate sleep duration in this population group. 28
Our study found that 83% of the participants had poor sleep quality. This percentage is comparable to that in the Buboltz et al 30 study, which estimated the prevalence of occasional sleep difficulties to be 73% among US university students. Most of the assessed sleep problems were more common in female than in male students. 30 Buboltz et al determined sleep quality using a Sleep Quality Index with 8 items, which was very similar to the sleep questionnaire we used in our study. We assessed sleep quality depending on the average number of actual sleep hours, from 7 to 8.5 hours, which complies with the recommendation of the National Sleep Foundation of between 7 and 9 hours of sleep per night in young adults and adults. 43 The other assessment criteria were taking less than 15 minutes to fall asleep at night, which was also according to the recommendation of the National Sleep Foundation 44 ; not taking sleeping pills; and not suffering from insomnia or inability to sleep or having any medical condition that hinders sleep.
In our study, 72% of the participants reported that their added sugars intake actually contributed to more than 10% of their total energy intake. This finding reflects the relatively high intake of added sugars in this population group. The higher added sugar intake was shown to be significantly associated with young age as well as unhealthy eating style in general (ie, low intake of fibers, fruits, and vegetables and high intake of fat). 45 In an exploratory study among US college students, the reasons for adopting an unhealthy eating style, including consuming high added sugar containing diets, were stress, insufficient time and knowledge to prepare healthy food, the lack of and high cost of healthy food and beverage options in the college, the availability and convenience of having junk foods, and pressures from peers and media. 46
We observed a positive association between high added sugar intake and poor quality of sleep, based on 24-hour dietary recall. This finding is in agreement with other studies that reported an inverse association between the consumption of SSBs, energy drinks, and high sugar diet and sleep duration and satisfaction in adolescents.33,35,36 Unlike the studies by Sampasa-Kanyinga et al 33 and Prather et al, 34 our study not only examined the sleep duration-SSB relationship, but also expanded the scope to include dietary added sugars and a more comprehensive perspective of sleep variables (ie, sleep quality). Park et al 35 reported a positive association between energy drink consumption and sleep dissatisfaction. However, sleep satisfaction was only determined by answering 1 question inquiring about “the degree of the sleep satisfaction in terms of fatigue relief.” Interestingly, sleep deprivation is linked to impaired glucose metabolism and high blood sugar levels that are partially a result of the associated pattern of unhealthy eating choices and increased appetite. 47 Therefore, it seems that there is a vicious cycle between sleep and sugar. Further studies are, however, needed to elucidate the underlying mechanisms of the unfavorable impact of added sugar intake on sleep quality.
Although a positive relationship between high added sugars and poor quality of sleep was also observed based on the FFQ, it did not reach significance. The observed discrepancy between the findings of FFQ and 24-hour dietary recall may be a result of the fact that the FFQ uses a fixed list of items that may be less accurate in determining the absolute intake of nutrients. For instance, some of the items used in our FFQ had very high added sugar content but did not have high consumption frequency (eg, candy bars). Other items that may not be in the list may have low sugar content but were more frequently consumed (eg, white bread). This may have confounded the actual intake of the participants’ added sugars. The use of FFQ in studying the association between the diet and another variable is sometimes questionable because the correlation of nutrient intake between the FFQ and 24-hour dietary recall is often poor. 48 In our study, 24-hour dietary recall showed the credibility of the real consumption of added sugars in some participants. Even though their answers to some items were “rarely or poorly consumed,” there was a reported consumption of these items based on the 24-hour dietary recall. So overall, we think that the 24-hour dietary recall data are more accurate and reflective of the actual added sugar consumption.
Caffeine intake may have been a possible confounding factor in our study and was associated with shorter sleep duration and poorer sleep quality. 49 A disruptive effect of 400 mg caffeine on sleep was reported, even when taken 6 hours before bed. 50 So we decided to divide our participants into 2 groups based on their caffeine intake and then study the association of our research question in each group separately. Even after eliminating the caffeine effect, we were still able to see an inverse significant association between sleep quality and added sugar intake in the non–caffeine-consuming group. The lack of the association in the caffeine-consuming group may have been a result of the confounding effect of caffeine.
The main limitation of our study is that we have not excluded caffeine consumers. Future studies are needed to explore the association between sleep quality and added sugar intake after excluding the participants who consume caffeine ≤6 hours before bed time. Future studies may also investigate whether the timing of the added sugar intake (before bed time or during the day) would have a differential effect on the sleep quality. Future studies should also include a larger sample size, including both male and female participants, and should further include participants with sleep disorders.
In conclusion, this study confirms the negative effects of high added sugar on sleep quality and duration and recommends reducing its intake to less than 10% of the total energy for better health and life quality. It is worth confirming that the findings reported herein are in line with other dietary recommendations for health in the general population, including those of the WHO. 3
Acknowledgments
We would like to thank all the study participants for giving their time and efforts. Without their great cooperation, the completion of this study would not have been possible. We further thank Dr Sahar Fallatah, the Vice Dean of the College of Applied Studies and Community Service at Imam Abulrahman Bin Faisal University, Dammam, Saudi Arabia, for providing support to facilitate this work.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval: Not applicable, because this article does not contain any studies with human or animal subjects.
Informed Consent: The experimental protocol and informed consent were approved by the Institutional Review Board of Imam Abdulrahman Bin Faisal University, Dammam, Saudi Arabia (IRB-UGS014-03-2019).
Trial Registration: Not applicable, because this article does not contain any clinical trials.
ORCID iDs: Tunny S. Purayidathil  https://orcid.org/0000-0003-3363-9778
https://orcid.org/0000-0003-3363-9778
Rabie Y. Khattab  https://orcid.org/0000-0002-1715-970X
https://orcid.org/0000-0002-1715-970X
References
- 1.Al-Shahri MZ. Health and lifestyle: a Saudi profile. J Fam Community Med. 1996;3:13-21. [PMC free article] [PubMed] [Google Scholar]
- 2.United States Department of Agriculture. What are added sugars? https://www.choosemyplate.gov/what-are-added-sugars. Accessed July 7, 2019.
- 3.World Health Organization. Sugars Intake for Adults and Children. Geneva, Switzerland: World Health Organization; 2015. [Google Scholar]
- 4.Seneff S, Wainwright G, Mascitelli L. Is the metabolic syndrome caused by a high fructose, and relatively low fat, low cholesterol diet? Arch Med Sci. 2011;7:8-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.De Pergola G, Silvestris F. Obesity as a major risk factor for cancer. J Obes. 2013;2013:291546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Orgel E, Mittelman SD. The links between insulin resistance, diabetes, and cancer. Curr Diab Rep. 2013;13:213-222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pagidipati NJ, Gaziano TA. Estimating deaths from cardiovascular disease: a review of global methodologies of mortality measurement. Circulation. 2013;127:749-756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yang Q, Zhang Z, Gregg EW, Flanders EW, Merritt R, Hu FB. Added sugar intake and cardiovascular diseases mortality among US adults. JAMA Intern Med. 2014;174:516-524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wu Y, Ding Y, Tanaka Y, Zhang W. Risk factors contributing to type 2 diabetes and recent advances in the treatment and prevention. Int J Med Sci. 2014;11:1185-1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.DiNicolantonio JJ, Lucan SC, O’Keefe JH. The evidence for saturated fat and for sugar related to coronary heart disease. Prog Cardiovasc Dis. 2016;58:464-472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Akbaraly TN, Brunner EJ, Ferrie JE, Marmot MG, Kivimaki M, Singh-Manoux A. Dietary pattern and depressive symptoms in middle age. Br J Psychiatry. 2009;195:408-413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Guo X, Park Y, Freedman NDet al. Sweetened beverages, coffee, and tea and depression risk among older US adults. PLoS One. 2014;9:e94715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gkogkolou P, Böhm M. Advanced glycation end products: key players in skin aging? Dermatoendocrinol. 2012;4:259-270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee D, Hwang W, Artan M, Jeong DE, Lee SJ. Effects of nutritional components on aging. Aging Cell. 2015;14:8-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aragno M, Mastrocola R. Dietary sugars and endogenous formation of advanced glycation endproducts: emerging mechanisms of disease. Nutrients. 2017;9:E385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ma J, Fox CS, Jacques PFet al. Sugar-sweetened beverage, diet soda, and fatty liver disease in the Framingham Heart Study cohorts. J Hepatol. 2015;63:462-469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Crane PK, Walker R, Hubbard RAet al. Glucose levels and risk of dementia. N Engl J Med. 2013;369:540-548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Merriman TR, Dalbeth N, Johnson RJ. Sugar-sweetened beverages, urate, gout and genetic interaction. Pac Health Dialog. 2014;20:31-38. [PubMed] [Google Scholar]
- 19.Karalius VP, Shoham DA. Dietary sugar and artificial sweetener intake and chronic kidney disease: a review. Adv Chronic Kidney Dis. 2013;20:157-164. [DOI] [PubMed] [Google Scholar]
- 20.Gupta P, Gupta N, Pawar AP, Birajdar SS, Natt AS, Singh HP. Role of sugar and sugar substitutes in dental caries: a review. ISRN Dent. 2013;2013:519421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kucharska A, Szmurło A, Sińska B. Significance of diet in treated and untreated acne vulgaris. Postepy Dermatol Alergol. 2016;33:81-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.St-Onge MP, Mikic A, Pietrolungo CE. Effects of diet on sleep quality. Adv Nutr. 2016;7:938-949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kim H, Jeong G, Park KY, Kang SW. Sleep quality and nutritional intake in subjects with sleep issues according to perceived stress levels. J Lifestyle Med. 2018;8:42-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Afaghi A, O’Connor H, Chow CM. High-glycemic-index carbohydrate meals shorten sleep onset. Am J Clin Nutr. 2007;85:426-430. [DOI] [PubMed] [Google Scholar]
- 25.Perricone NV, Bagchi D, Echard B, Preuss HG. Blood pressure lowering effects of niacin-bound chromium (III) (NBC) in sucrose-fed rats: renin-angiotensin system. J Inorg Biochem. 2008;102:1541-1548. [DOI] [PubMed] [Google Scholar]
- 26.Vgontzas AN, Lin HM, Papaliag Met al. Short sleep duration and obesity: the role of emotional stress and sleep disturbances. Int J Obes (Lond). 2008;32:801-809. [DOI] [PubMed] [Google Scholar]
- 27.Kaneita Y. Sleep and health promotion. Sleep Biol Rhythms. 2014;12:73. [Google Scholar]
- 28.Chaput JP, Dutil C. Lack of sleep as a contributor to obesity in adolescents: impacts on eating and activity behaviors. Int J Behav Nutr Phys Act. 2016;13:103-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.López-García E, Faubel R, León-Muñoz L, Zuluaga MC, Banegas JR, Rodríguez-Artalejo F. Sleep duration, general and abdominal obesity, and weight change among the older adult population of Spain. Am J Clin Nutr. 2008;87:310-316. [DOI] [PubMed] [Google Scholar]
- 30.Buboltz WC, Jr, Brown F, Soper B. Sleep habits and patterns of college students: a preliminary study. J Am Coll Health. 2001;50:131-135. [DOI] [PubMed] [Google Scholar]
- 31.Lund HG, Reider BD, Whiting AB, Prichard JR. Sleep patterns and predictors of disturbed sleep in a large population of college students. J Adolesc Health. 2010;46:124-132. [DOI] [PubMed] [Google Scholar]
- 32.Schlarb AA, Friedrich A, Claßen M. Sleep problems in university students—an intervention. Neuropsychiatr Dis Treat. 2017;13:1989-2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sampasa-Kanyinga H, Hamilton HA, Chaput JP. Sleep duration and consumption of sugar-sweetened beverages and energy drinks among adolescents. Nutrition. 2018;48:77-81. [DOI] [PubMed] [Google Scholar]
- 34.Prather AA, Leung CW, Adler NE, Ritchie L, Laraia B, Epel ES. Short and sweet: associations between self-reported sleep duration and sugar-sweetened beverage consumption among adults in the United States. Sleep Health. 2016;2:272-276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Park S, Lee Y, Lee JH. Association between energy drink intake, sleep, stress, and suicidality in Korean adolescents: energy drink use in isolation or in combination with junk food consumption. Nutr J. 2016;15:87-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Blunden S, Watson E, Rigney Get al. T-O-136 The effects of a high sugar diet on sleep quality and attention capacity in prepubescent girls: a preliminary study. Sleep Med. 2011;12:S94. [Google Scholar]
- 37.World Health Organization. Physical Status: the Use and Interpretation of Anthropometry: Report of a WHO Expert Committee. Geneva, Switzerland: World Health Organization; 1995. [PubMed] [Google Scholar]
- 38.Hargens TA, Kaleth AS, Edwards ES, Butner KL. Association between sleep disorders, obesity, and exercise: a review. Nat Sci Sleep. 2013;5:27-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Surani S, Brito V, Surani A, Ghamande S. Effect of diabetes mellitus on sleep quality. World J Diabetes. 2015;6:868-873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Whitaker BN, Fisher PL, Jambhekar Set al. Impact of degree of obesity on sleep, quality of life, and depression in youth. J Pediatr Health Care. 2018;32:e37-e44. [DOI] [PubMed] [Google Scholar]
- 41.Facco FL, Kramer J, Ho KH, Zee PC, Grobman WA. Sleep disturbances in pregnancy. Obstet Gynecol. 2010;115:77-83. [DOI] [PubMed] [Google Scholar]
- 42.Herring SJ, Foster GD, Pien GWet al. Do pregnant women accurately report sleep time? A comparison between self-reported and objective measures of sleep duration in pregnancy among a sample of urban mothers. Sleep Breath. 2013;17:1323-1327. doi: 10.1007/s11325-013-0835-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Keyes KM, Maslowsky J, Hamilton A, Schulenberg J. The great sleep recession: changes in sleep duration among US adolescents, 1991-2012. Pediatrics. 2015;135:460-468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hirshkowitz M, Whiton K, Albert SMet al. National Sleep Foundation’s updated sleep duration recommendations. Sleep Health. 2015;1:233-243. [DOI] [PubMed] [Google Scholar]
- 45.Ohayon M, Wickwire EM, Hirshkowitz Met al. National Sleep Foundation’s sleep quality recommendations: first report. Sleep Health. 2017;3:6-19. [DOI] [PubMed] [Google Scholar]
- 46.Kaartinen NE, Similä ME, Kanerva N, Valsta LM, Harald K, Männistö S. Naturally occurring and added sugar in relation to macronutrient intake and food consumption: results from a population-based study in adults. J Nutr Sci. 2017;6:e7. doi: 10.1017/jns.2017.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Knutson KL. Impact of sleep and sleep loss on glucose homeostasis and appetite regulation. Sleep Med Clin. 2007;2:187-197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kristal AR, Peters U, Potter JD. Is it time to abandon the Food Frequency Questionnaire? Cancer Epidemiol Biomarkers Prev. 2005;14:2826-2828. [DOI] [PubMed] [Google Scholar]
- 49.Watson EJ, Coates AM, Kohler M, Banks S. Caffeine consumption and sleep quality in Australian adults. Nutrients. 2016;8:E479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Drake C, Roehrs T, Shambroom J, Roth T. Caffeine effects on sleep taken 0, 3, or 6 hours before going to bed. J Clin Sleep Med. 2013;9:1195-1200. [DOI] [PMC free article] [PubMed] [Google Scholar]