Abstract
Objective:
This study aimed to determine the frequency of typical and atypical computed tomography (CT) findings of COVID-19 and their effect on hospitalization.
Methods:
We retrospectively assessed 414 patients who were diagnosed with COVID-19 by real-time reverse transcription-polymerase chain reaction and who had lung involvement in their admission chest CT. We evaluated the frequency of typical and atypical chest CT findings and analyzed the relationship between typical and atypical findings of COVID-19 in patients treated in ambulatory versus inpatient settings.
Results:
Ground-glass opacities were the most common typical finding of COVID-19 chest CT scans. The frequencies of other typical findings, including consolidation, air bronchogram, pulmonary vascular enlargement (PVE), airway changes, crazy paving pattern, and reticular pattern, were similar to those reported in the literature. Atypical findings were less common and found at varying frequencies. Crazy paving pattern, air bronchogram, reticular pattern, and PVE were significantly more common in hospitalized patients (p<0.001). The frequencies of other typical and atypical findings were not significantly different between ambulatory and hospitalized patients.
Conclusion:
Increased recognition of typical and atypical findings of COVID-19 and their frequencies, as well as knowledge of admission chest CT findings that are associated with hospitalization, will facilitate medical care during the pandemic.
Keywords: Atypical findings, computed tomography, COVID-19, ground-glass opacity
In December 2019, an outbreak of pneumonia of unknown origin was reported in Wuhan, China. Subsequent studies identified a novel coronavirus, SARS-CoV-2, as the etiological agent of this viral infection. Through person-to-person transmission, the disease rapidly spread around the world. In March 2020, the World Health Organization declared the coronavirus outbreak as a pandemic [1, 2].
Real-time reverse transcription-polymerase chain reaction (RT-PCR) is a commonly used method for detecting SARS-CoV-2 infections due to being fast, easy to use, and practical. In addition, computed tomography (CT) of the chest is easily applied for patients with suspected COVID-19, especially in regions affected by the pandemic, and is very valuable in supporting the diagnosis. According to recent studies, chest CT is more sensitive than RT-PCR in determining COVID-19 and its prognosis [3, 4].
Typical chest CT findings in COVID-19 include bilateral, mostly peripheral multiple ground-glass opacities (GGOs). Despite being common in COVID-19 pneumonia, chest CT findings may vary between individuals [5–7]. Besides GGOs, other typical findings of COVID-19 include consolidations, air bronchogram, pulmonary vascular enlargement (PVE), airway changes, crazy paving pattern, and reticular pattern (Fig. 1) [8]. Atypical chest CT findings of COVID-19 include pleural thickening and/or effusion, nodules, reversed halo signs, lymphadenopathy (LAP), pericardial effusion, subpleural lines, subpleural sparing, spider web signs, air bubble signs, tree-in-bud signs, central and/or peribronchovascular involvement, isolated upper lobe involvement, and isolated lobar consolidation (Fig. 2, 3) [2, 8–10]. Having a comprehensive knowledge of the typical and atypical chest CT findings of COVID-19 will help to reduce false negatives and improve the management of the outbreak [11]. In this study, we aimed to establish the frequency of typical and atypical CT findings in our hospital and their effect on hospitalization.
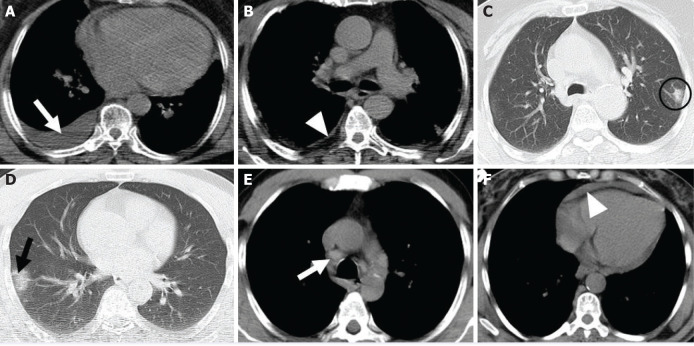
Figure 1.
The axial section of the chest computed tomography scan shows typical findings (A) ground glass opacity, crazy paving pattern (black arrows); (B) consolidation, air bronchogram (white arrow); (C) reticular pattern (black arrow-heads); (D) pulmonary vascular enlargement (black circle).
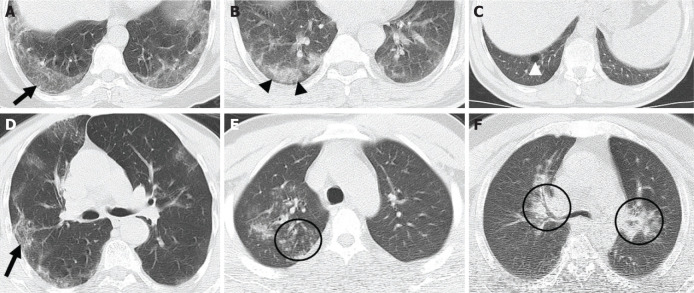
Figure 2.
The axial section of the chest computed tomography scan shows atypical findings (A) pleural effusion (white arrow), (B) pleural thickening (white arrow-head), (C) nodule (black circle), (D) reversed halo sign (black arrow), (E) mediastinal lymph nodes (white arrow), (F) pericardial effusion (white arrow-head).
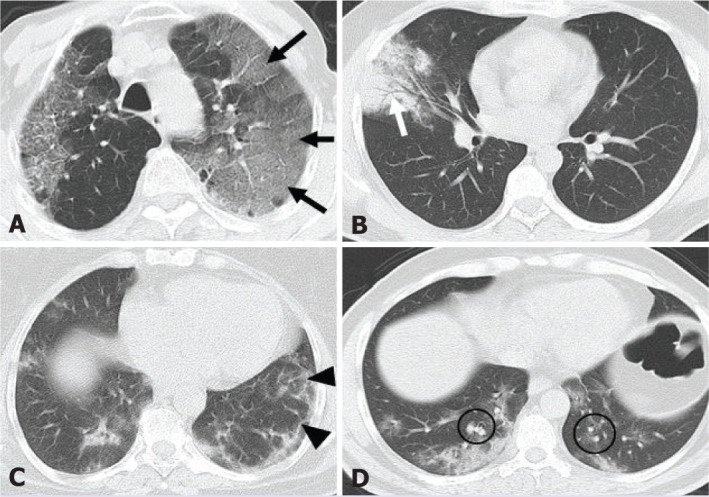
Figure 3.
The axial section of the chest computed tomography scan shows atypical findings (A) subpleural line (black arrow), (B) subpleural sparing (black arrow-heads), (C) air-bubble sign (white arrow-head), (D) spider web sign (black arrow), (E) tree-in-bud (black circle), (F) central-peribronchovascular involvement (black circle).
Materials and Methods
This study was approved by Adiyaman University Non-Interventional Clinical Research Ethics Board (approval code: 2021/01-19) and the Ministry of Health of the Republic of Turkey (approval date: 25.12.2020).
Study Population
We retrospectively assessed records of the patients who were diagnosed with COVID-19 by nasopharyngeal and oropharyngeal RT-PCR between September 2020 and January 2021.
The inclusion criteria included:
-
1.
Being diagnosed with COVID-19 by clinical examination and RT-PCR
-
2.
Unenhanced chest CT obtained at the time of admission
-
3.
Exclusion of other causes of pneumonia.
The exclusion criteria included:
-
1.
COVID-19 diagnosis not being confirmed by RT-PCR
-
2.
Having received treatment before CT imaging
-
3.
Lack of unenhanced admission chest CT images
-
4.
Having a known lung disease
-
5.
Having a non-diagnostic chest CT image with artifacts
-
6.
Patients with non-COVID-19 pneumonia and/or findings suggestive of co-infection.
Highlight key points
-
•
CT of the chest is easily applied for patients with suspected COVID-19.
-
•
The most common typical finding is bilateral patchy peripheral ground-glass opacity on COVID-19 pneumonia.
-
•
In addition to ground-glass opacity, less frequent other typical findings are common, while atypical findings are seen at varying rates.
-
•
Among the typical chest CT findings, crazy paving pattern, air bronchogram, reticular pattern, and PVE were significantly more common in hospitalized patients.
-
•
The recognition of uncommon atypical findings together with the more common typical findings will facilitate clinical practice during the pandemic.
CT Protocol
All examinations were performed with a 16-slice multidetector CT scanner (MX16, Philips Medical System, Koninklijke, Netherlands). CT images were obtained in the supine position during deep inspiration. The examinations were carried out with a single CT device reserved for the patients with suspected COVID-19 in our hospital within the scope of the precautions taken with the arrival of the pandemic to our country. And according to these precautions, the CT scanner was disinfected after each exam. Scanning and reconstruction parameters were as follows: beam collimation, 16×0.75 mm; rotation time, 0.75 s; slice thickness, 1 mm; slice reconstruction, 1 mm; tube voltage, 90–120 kV; effective tube current-time product, 50–110 mAs. CT images were acquired from lung apex to lung base. The field of view was 250–300 mm.
Image Interpretation
The images were interpreted using the hospital database (Oracle Database V1.10.43.134). All CT images were independently evaluated by two radiologists, one with 6 years (M.Ç.) and one with 3 years (C.O.) of experience in radiology. In the event of a discrepancy between these two observers, a third observer with 16 years of experience in radiology (H.T.B.) reviewed the images to reach an agreement.
Clinical Examination
The indication for hospitalization was made according to the criteria defined by the COVID-19 diagnosis and treatment guidelines of the Ministry of Health of the Republic of Turkey. According to this guideline, a patient who meets at least one of the following criteria was hospitalized [12]:
-
1.
Mild-to-moderate pneumonia (bilateral <50% radiological involvement) AND respiratory rate ≥24/min and SpO2 ≤93%
-
2.
Mild-to-moderate pneumonia AND poor prognosis criteria in admission blood tests (lymphocyte count <800/μL or serum CRP values >10 times upper limit of normal or ferritin >500 ng/mL or D-dimer >1000 ng/mL)
-
3.
Severe pneumonia (altered state of consciousness, respiratory distress, respiratory rate ≥30/min, SpO2 ≤90% in room air, widespread (>50%) bilateral lung involvement)
-
4.
Hypotension (<65 mmHg)
-
5.
Tachycardia (>100 bpm)
-
6.
Sepsis
-
7.
Septic shock
-
8.
Myocarditis
-
9.
Acute coronary syndrome
-
10.
Arrhythmia
-
11.
Acute kidney injury.
Statistical Analysis
Statistical analyses were carried out using Statistical Package for Social Sciences program version 23.0 Inc. Chicago, IL, USA. All variables were categorical and descriptive statistics for categorical variables were given as numbers (n) and percentages. Statistical analysis was performed to compare typical and atypical tomography findings in ambulatory and inpatient patients. Categorical variables were compared using Pearson’s Chi-squared test or Fisher’s exact test. Significance level was considered p<0.05.
Results
About 2405 patients with RT-PCR positivity were evaluated and among them, 414 patients who met the inclusion and exclusion criteria were enrolled for this study. Of the patients, 182 (44%) were female, 232 (56%) were male, and the average age was 52.2±15.1 years (range: 18–88 years).
The frequencies of typical chest CT findings were as follows: GGOs, 388 (93.7%); consolidation, 218 (52.6%); GGOs+consolidation, 194 (46.8%); crazy paving, 213 (51.4%); air bronchogram, 153 (36.9%); airway changes, 26 (6%); reticular pattern, 176 (42.5%); and PVE, 141 (34%) (Table 1).
Table 1.
The reported frequency of the typical chest computed tomography findings
| Current study | Zarifian et al. (metaanalysis) [16] | Zhao et al. [17] | Bai et al. [18] | Zhang et al. [19] | Li et al. [20] | Wu et al. [21] | Bernheim et al. [2] | |
|---|---|---|---|---|---|---|---|---|
| Number of patients | (n=414) % | (n=9907) % | (n=101) % | (n=219) % | (n=120) % | (n=56) % | (n=80) % | (n=121) % |
| GGO | 93.7 | 6224–4799 (77.1%) | 86.1 | 91 | 89 | 80.4 | 91 | 75.2 |
| Consolidation | 52.6 | 4397–1560 (35.5%) | 43.6 | 69 | 52 | 21.4 | 63 | 42.9 |
| GGO+Consolidation | 46.8 | 385–146 (38%) | 64.4 | 64 | – | 76.8 | – | 41 |
| Crazy paving | 51.4 | – | – | 5 | 25 | 44.6 | 29 | 5 |
| Air bronchogram | 36.9 | 1953–800 (41%) | – | 14 | 20 | 73.2 | – | – |
| Airway changes | 6 | 994–136 (13.6%) | – | 9 | 12 | – | 11 | 13 |
| Reticular pattern | 42.5 | 2667–1232 (46.2%) | 48.5 | 56 | 18 | 53.6 | 20 | 7 |
| PVE | 34 | – | 71.3 | 59 | – | – | – | – |
GGO: Ground glass opacity; PVE: Pulmonary vascular enlargement.
The frequencies of atypical chest CT findings were as follows: pleural thickening and/or effusion, 70 (16.9%); nodules, 24 (5.7%); reversed halo signs, 5 (1.2%); LAP, 9 (2.1%); pericardial effusion, 7 (1.6%); subpleural lines, 4 (0.9%); subpleural sparing, 14 (3.3%); spider web signs, 12 (2.8%); air bubble signs, 13 (3.1%); tree-in-bud signs, 4 (0.9%); central and/or peribronchovascular involvement, 8 (1.9%); and isolated upper lobe involvement, 16 (3.8%) (Table 2).
Table 2.
The reported frequency of the atypical chest computed tomography findings
| Current study | Zarifian et al. (metaanalysis) [16] | Li et al. [20] | Wu et al. [21] | Pakdemirli et al. [22] | Wang et al. [23] | Tabatabaei et al. [24] | Werberich et al. [25] | |
|---|---|---|---|---|---|---|---|---|
| Number of patients | (n=414) | (n=9907) | (n=83) | (n=80) | (n=18) | (n=93) | (n=120) | (n=48) |
| Pleural thickening and/or effusion | 16.9 | 5345–741 (13.8%) | 8.4 | 6 | 88 | 31.1 | 16.6 | 4.2 |
| Nodule | 5.7 | 2582–338 (13.1%) | 7.2 | – | 61 | 18.3 | 25 | 4.2 |
| Reversed halo sign | 1.2 | – | – | – | 0 | 15.1 | 11.6 | 4.2 |
| LAP | 2.1 | 3197–165 (5.1%) | 8.4 | 4 | 17 | 6.5 | 0 | 4.2 |
| Pericardial effusion | 1.6 | – | 4.8 | 5 | – | – | – | 6.2 |
| Subpleural line | 0.9 | – | 20.5 | 20 | 61 | – | – | 14.6 |
| Subpleural sparing | 3.3 | – | – | – | 33 | – | 23.3 | 6.2 |
| Spider web sign | 2.8 | – | 25.3 | 25 | – | – | – | – |
| Air bubble sign | 13 (3.1%) | – | – | – | – | 12.9 | – | 37.5 |
| Tree-in-bud | 4 (0.9%) | – | – | – | 6 | 3.2 | 0 | – |
| Central and/or | 1.9 | 2160–131 (6.1%) | – | 4 | 11 | – | 2.1 | |
| peribronchovascular involvement | ||||||||
| Isolated upper lobe involvement | 3.8 | – | – | – | 0 | – | – | 10.4 |
LAP: Lymphadenopathy.
Of the subjects, 196 (47.3%) and 218 (52.7%) were treated and followed in ambulatory and inpatient settings, respectively. Seven (3.2%) patients died during inpatient treatment. Among the typical chest CT findings, crazy paving pattern, air bronchogram, reticular pattern, and PVE were significantly more common in hospitalized patients (p<0.001). The frequencies of other typical and atypical findings were not significantly different between ambulatory and hospitalized patients (Table 3).
Table 3.
The frequency of typical and atypical chest computed tomography findings in outpatients and inpatients
| Outpatients (n=196) (%) | Inpatients (n=218) (%) | p | |
|---|---|---|---|
| Typical Findings | |||
| GGO | 92.3 | 95 | 0.314 |
| Consolidation | 50.5 | 54.6 | 0.431 |
| GGO+Consolidation | 43.4 | 50 | 0.200 |
| Crazy paving | 41.8 | 60.1 | <0.001 |
| Air bronchogram | 27.6 | 45.4 | <0.001 |
| Airway changes | 6.1 | 12 (5.5 | 0.788 |
| Reticular pattern | 30.1 | 53.7 | <0.001 |
| PVE | 25 | 42.2 | <0.001 |
| Atypical findings | |||
| Pleural thickening | 13.3 | 14.7 | 0.777 |
| and/or effusion | |||
| Nodule | 5.1 | 6.4 | 0.675 |
| Reversed halo sign | 2 | 0.5 | 0.194 |
| LAP | 3.1 | 1.4 | 0.318 |
| Pericardial effusion | 1 | 2.3 | 0.454 |
| Subpleural line | 1 | 0.9 | 0.647 |
| Subpleural sparing | 5.1 | 1.8 | 0.058 |
| Spider web sign | 3.1 | 2.8 | 0.540 |
| Air bubble sign | 3.6 | 2.8 | 0.78 |
| Tree-in-bud | 1 | 0.9 | 0.647 |
| Central and/or peribronchovascular involvement | 2 | 1.8 | 0.578 |
| Isolated upper lobe involvement | 5.6 | 2.3 | 0.080 |
GGO: Ground glass opacity; PVE: Pulmonary vascular enlargement; LAP: Lymphadenopathy.
Discussion
Chest CT plays an important role in the diagnosis of the patients with suspected COVID-19, particularly when the RT-PCR test is negative. This test may show a false negative result, especially in the initial phase of symptoms [13, 14]. And as stated in the COVID-19 diagnosis and treatment guidelines of the Ministry of Health of the Republic of Turkey, showing lung involvement makes a significant contribution to the determination of the treatment process [12]. Together with typical findings, the presence and increased recognition of atypical findings will facilitate both the diagnosis of COVID-19 with chest CT and the disease management [3, 15]. In this study, we identified the frequency of typical and atypical CT findings and their effect on hospitalization.
In our study, the most common typical finding was GGO (93.7%). This finding is consistent with the literature, where GGOs are reported in 75%–91% of COVID-19 patients. In a meta-analysis by Zarifian et al. [16] that included data from 103 studies, 4799 of 6224 patients (77.1%) had GGOs. The frequencies of consolidation, GGOs+consolidation, air bronchogram, airway changes, and reticular pattern reported in the same study are consistent with our results. In our study, we also evaluated the frequencies of crazy paving pattern and PVE. The literature reports that the prevalence of crazy paving pattern ranges between 5% and 44% in COVID-19 patients. In our study, this rate was 51.4%. PVE was found in 59%–71% of the patients in the literature and in 34% of our patients [2, 16–21]. In the literature, the prevalence of typical findings is mostly similar, with small differences that may be ascribed to variances in study populations.
In our study, pleural thickening and/or effusion and nodules were the most common atypical chest CT findings, with prevalence of 16.9% and 5.7%, respectively. Our results are generally consistent with those reported in the literature, with the exception of a study by Pakdemirli et al. [22] reporting the incidence of pleural thickening and/or effusion and nodules to be 88% and 61%, respectively. This discrepancy may be due to the small sample size (n=18) in the study by Pakdemirli et al.
Compared to typical findings, the prevalence of atypical findings reported in the literature is highly variable. In our study, the prevalences of reversed halo signs, LAP, pericardial effusion, subpleural lines, subpleural sparing, spider web signs, air bubble signs, tree-in-bud signs, central and/or peribronchovascular involvement, and isolated upper lobe involvement were 1.2%, 2.1%, 1.6%, 0.9%, 3.3%, 2.8%, 3.1%, 0.9%, 1.9%, and 3.8%, respectively. Atypical findings evaluated in the literature vary. These differences may stem from a lack of a clear definition. Another reason may be the differences in study populations and working conditions during the pandemic. For patients with COVID-19, the literature reports reversed halo signs in 0–15%, LAP in 0–17%, pericardial effusion in 4–6%, subpleural lines in 14–61%, subpleural sparing in 6–33%, spider web signs in 25%, air bubble signs in 12–37%, tree-in-bud signs in 0–6%, central and/or peribronchovascular involvement in 2–11%, and isolated upper lobe involvement in 0–10% of individuals [15, 16, 21–25].
The literature on the effect of typical and atypical chest CT findings of the COVID-19 on hospitalization is highly limited. Emara et al. [26] investigated the impact of findings on intensive care unit (ICU) admission and mortality. They found that pleural effusion and GGOs were significantly associated with ICU admission and mechanical ventilation, but they did not report the impact of typical and atypical findings on mortality. In our study, we found that crazy paving pattern, air bronchogram, reticular pattern, and PVE were significantly associated with hospitalization. Other typical and atypical findings were not significantly associated with hospitalization. In our study, we were unable to assess ICU admission and mechanical ventilation since our primary objective was to investigate the impact of admission chest CT findings on hospitalization and to establish whether chest CT findings, as well as other clinical criteria [12], contribute to the decision of hospitalization.
The high percentage of hospitalized patients in our study is due to including patients with pulmonary involvement in their admission chest CT images. We excluded patients without pulmonary involvement regardless of a positive RT-PCR test. Our mortality rate (1.6%) is similar to those reported by the Ministry of Health of the Republic of Turkey [27]. The limitations of our study include not being able to investigate the association between chest CT findings and mortality due to the small number of deaths, the retrospective and single-center design, and having a small number of the patients with atypical findings. Further studies with larger samples are needed to clarify the impact of atypical findings on COVID-19 prognosis. Furthermore, we did not include CT images from during and after treatment; therefore, we did not evaluate atypical findings that may occur during or after treatment. Finally, exclusion of bacterial infections accompanying COVID-19 infection with only RT-PCR test and initial thoracic CT findings may be insufficient to exclude all co-infections. However, it is known that the bacterial co-infection rate is low in COVID-19 pneumonia [28, 29]. However, it should be kept in mind that this may affect the frequency of atypical findings, while evaluating the results of the study.
Conclusion
The recognition of uncommon atypical findings together with the more common typical findings will help to prevent false negatives in radiology reports and the diagnosis of COVID 19. When evaluating admission chest CT findings, knowing the clinical criteria and chest CT findings that will affect hospitalization will facilitate clinical practice during the pandemic.
Footnotes
Cite this article as: Corapli M, Cil E, Oktay C, Bulut HT, Corapli G. Frequency of typical and atypical computed tomography findings of COVID-19 and their effect on hospitalization. North Clin Istanb 2021;8(6):554–561.
Ethics Committee Approval: The Adiyaman University Non-Interventional Research Ethics Committee granted approval for this study (date: 19.01.2021, number: 2021/01-19).
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
Authorship Contributions: Concept – MC, EC; Design – MC, CO; Supervision – EC, HTB; Materials – EC, GC; Data collection and/or processing – GC, HTB; Analysis and/or interpretation – HTB, MC; Literature review – MC, GC; Writing – MC, CO; Critical review – MC, CO.
References
- 1.Song F, Shi N, Shan F, Zhang Z, Shen J, Lu H, et al. Emerging 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology. 2020;295:210–7. doi: 10.1148/radiol.2020200274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bernheim A, Mei X, Huang M, Yang Y, Fayad ZA, Zhang N, et al. Chest CT findings in coronavirus disease-19 (COVID-19): relationship to duration of infection. Radiology. 2020;295:200463. doi: 10.1148/radiol.2020200463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, et al. Correlation of chest CT and RT-PCR testing for coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology. 2020;296:E32–40. doi: 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jin YH, Cai L, Cheng ZS, Cheng H, Deng T, Fan YP, et al. for the Zhongnan Hospital of Wuhan University Novel Coronavirus Management and Research Team, Evidence-Based Medicine Chapter of China International Exchange and Promotive Association for Medical and Health Care (CPAM) A rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (standard version). Mil Med Res. 2020;7:4. doi: 10.1186/s40779-020-0233-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kong W, Agarwal PP. Chest imaging appearance of COVID-19 infection. Radiol Cardiothorac Imaging. 2020;2:e200028. doi: 10.1148/ryct.2020200028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li X, Zeng X, Liu B, Yu Y. COVID-19 infection presenting with CT halo sign. Radiol Cardiothorac Imaging. 2020;2:e200026. doi: 10.1148/ryct.2020200026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ng MY, Lee EYP, Yang J, Yang F, Li X, Wang H, et al. Imaging profile of the COVID-19 infection: radiologic findings and literature review. Radiol Cardiothorac Imaging. 2020;2:e200034. doi: 10.1148/ryct.2020200034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ufuk F, Savaş R. Chest CT features of the novel coronavirus disease (COVID-19). Turk J Med Sci. 2020;50:664–78. doi: 10.3906/sag-2004-331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chung M, Bernheim A, Mei X, Zhang N, Huang M, Zeng X, et al. CT imaging features of 2019 novel coronavirus (2019-nCoV). Radiology. 2020;295:202–7. doi: 10.1148/radiol.2020200230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A. Coronavirus disease 2019 (COVID-19): a systematic review of imaging findings in 919 patients. AJR Am J Roentgenol. 2020;215:87–93. doi: 10.2214/AJR.20.23034. [DOI] [PubMed] [Google Scholar]
- 11.Kim D, Quinn J, Pinsky B, Shah NH, Brown I. Rates of co-infection between SARS-CoV-2 and other respiratory pathogens. JAMA. 2020;323:2085–6. doi: 10.1001/jama.2020.6266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Republic of Turkey Ministry of Healhty. Hospitalization indications on COVID-19, 2020. Available at: https://covid19.saglik.gov.tr/Eklenti/39061/0/COVID19rehberieriskinhastatedavisipdf.pdf. Accessed Oct 9,2020. [Google Scholar]
- 13.Xie X, Zhong Z, Zhao W, Zheng C, Wang F, Liu J. Chest CT for typical coronavirus disease 2019 (COVID-19) pneumonia: relationship to negative RT-PCR testing. Radiology. 2020;296:E41–5. doi: 10.1148/radiol.2020200343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Miao C, Jin M, Miao L, Yang X, Huang P, Xiong H, et al. Early chest computed tomography to diagnose COVID-19 from suspected patients: A multicenter retrospective study. Am J Emerg Med. 2021;44:346–51. doi: 10.1016/j.ajem.2020.04.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li K, Wu J, Wu F, Guo D, Chen L, Fang Z, Li C. The clinical and chest CT features associated with severe and critical COVID-19 pneumonia. Invest Radiol. 2020;55:327–31. doi: 10.1097/RLI.0000000000000672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zarifian A, Ghasemi Nour M, Akhavan Rezayat A, Rahimzadeh Oskooei R, Abbasi B, Sadeghi R. Chest CT findings of coronavirus disease 2019 (COVID-19): A comprehensive meta-analysis of 9907 confirmed patients. Clin Imaging. 2021;70:101–10. doi: 10.1016/j.clinimag.2020.10.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhao W, Zhong Z, Xie X, Yu Q, Liu J. Relation between chest CT findings and clinical conditions of coronavirus disease (COVID-19) pneumonia: a multicenter study. AJR Am J Roentgenol. 2020;214:1072–7. doi: 10.2214/AJR.20.22976. [DOI] [PubMed] [Google Scholar]
- 18.Bai HX, Hsieh B, Xiong Z, Halsey K, Choi JW, Tran TML, et al. Performance of radiologists in differentiating COVID-19 from non-COVID-19 viral pneumonia at chest CT. Radiology. 2020;296:E46–54. doi: 10.1148/radiol.2020200823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang R, Ouyang H, Fu L, Wang S, Han J, Huang K, et al. CT features of SARS-CoV-2 pneumonia according to clinical presentation: a retrospective analysis of 120 consecutive patients from Wuhan city. Eur Radiol. 2020;30:4417–26. doi: 10.1007/s00330-020-06854-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li K, Fang Y, Li W, Pan C, Qin P, Zhong Y, et al. CT image visual quantitative evaluation and clinical classification of coronavirus disease (COVID-19). Eur Radiol. 2020;30:4407–16. doi: 10.1007/s00330-020-06817-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wu J, Wu X, Zeng W, Guo D, Fang Z, Chen L, et al. Chest CT findings in patients with coronavirus disease 2019 and its relationship with clinical features. Invest Radiol. 2020;55:257–61. doi: 10.1097/RLI.0000000000000670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pakdemirli E, Mandalia U, Monib S. Characteristics of chest CT images in patients with COVID-19 pneumonia in London, UK. Cureus. 2020;12:e10289. doi: 10.7759/cureus.10289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang J, Xu Z, Wang J, Feng R, An Y, Ao W, et al. CT characteristics of patients infected with 2019 novel coronavirus: association with clinical type. Clin Radiol. 2020;75:408–14. doi: 10.1016/j.crad.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tabatabaei SMH, Talari H, Moghaddas F, Rajebi H. CT features and short-term prognosis of COVID-19 pneumonia: a single-center study from Kashan, Iran. Radiol Cardiothorac Imaging. 2020;2:e200130. doi: 10.1148/ryct.2020200130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Werberich GM, Marchiori E, Barreto MM, Rodrigues RS. Computed tomography findings in a Brazilian cohort of 48 patients with pneumonia due to coronavirus disease. Rev Soc Bras Med Trop. 2020;53:e20200405. doi: 10.1590/0037-8682-0405-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Emara DM, Naguib NN, Moustafa MA, Ali SM, El Abd AM. Typical and atypical CT chest imaging findings of novel coronavirus 19 (COVID-19) in correlation with clinical data: impact on the need to ICU admission, ventilation and mortality. Egyptian Journal of Radiology and Nuclear Medicine. 2020;51:1–9. [Google Scholar]
- 27.Republic of Turkey Ministry of Healhty. COVID-19 information page, 2020. Available at: https://covid19.saglik.gov.tr/EN-69532/general-coronavirus-table.html. Accessed Feb 23, 2020. [Google Scholar]
- 28.Lansbury L, Lim B, Baskaran V, Lim WS. Co-infections in people with COVID-19: a systematic review and meta-analysis. J Infect. 2020;81:266–75. doi: 10.1016/j.jinf.2020.05.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Langford BJ, So M, Raybardhan S, Leung V, Westwood D, MacFadden DR, et al. Bacterial co-infection and secondary infection in patients with COVID-19: a living rapid review and meta-analysis. Clin Microbiol Infect. 2020;26:1622–9. doi: 10.1016/j.cmi.2020.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]