Abstract
Rationale
Determining who is particularly vulnerable to mental health deterioration during the COVID-19 pandemic is essential when designing and targeting interventions to mitigate the adverse psychological impacts of the outbreak. Older people have appeared to be less exposed to mental health deterioration compared with younger individuals, but most exposed to the risk of severe illness and death from the virus, as well as less equipped to use technologies for coping with lockdown measures.
Objective
Amongst the old population, we aim at determining how depressive symptoms have changed during the first wave of the COVID-19 pandemic and identifying individual risk factors associated with changes in reporting depression. We are particularly interested in exploring the role of pre-existing mental health problems and evaluating gender differences.
Method
Data come from the Survey of Health, Ageing and Retirement in Europe, in particular from the first COVID-19 survey administered in summer 2020. Logistic models are estimated and Average Marginal Effects computed to take the degree of individual unobserved heterogeneity into account comparing point estimates across samples. Multiple Imputation (implemented through Multivariate Imputation by Chained Equations) is used to replace missing data. Statistical power of the effect sizes is estimated by a simulation approach.
Results
Pre-existing mental health problems, a diagnosis of affective/emotional disorders, a recent diagnosis of a major illness, and (only for men) job loss during the first wave of the outbreak are the most important risk factors. Statistical differences between genders emerge, with women experiencing higher levels of depression and greater worsening of mental health than men.
Conclusions
To identify people at greater risk of depression deterioration during an outbreak it is very important to consider their pre-existing mental and general health, distinguishing severity level. On population level, it is also crucial to evaluate depression disorders separately by gender.
Keywords: Ageing, COVID-19, Depression, Gender difference, Mental health, Older adults, Sadness, SHARE
1. Introduction
The ongoing coronavirus disease (COVID-19) pandemic has been a disruptive and destructive global event characterised by the spread of a life-threatening infectious disease. It has caused enormous psychological, social and economic harm, and the measures taken to contain its spread have profoundly affected every aspect of the day-to-day lives of people around the world.
The new stressors introduced by COVID-19 have affected the lives of both individuals who contracted the disease and those who did not. Infected people have been found to experience delirium, depression, anxiety and insomnia (Rogers et al., 2020). For example, a few studies conducted in Italy identified a high prevalence of emergent psychiatric sequelae amongst a sample of COVID-19 survivors, half of whom suffered from at least one pathological disorder (Mazza et al., 2020); another study reported that a large proportion of patients with COVID-19 continued to experience psychological distress and physical symptoms even after hospital discharge (Tomasoni et al., 2021). At the same time, the mental health of the general population, mostly studied using representative samples (Bann et al., 2021; Di Gessa and Price, 2021; Pierce et al., 2020), has been found to deteriorate, with increased levels of stress and worries (Salari et al., 2020). These results appear to be consistent around the world. In the US, the prevalence of depressive symptoms was more than three times higher during COVID-19 than before the pandemic (Ettman et al., 2020). A large proportion of individuals in Hong Kong reported a deterioration in their mental health since the onset of the pandemic (Choi et al., 2020). In China, Huang and Zhao (2020) found a high prevalence of generalised anxiety disorder, depressive symptoms and sleep quality deterioration. Even in countries such as Sweden, where the population did not experience lockdown measures during the first wave of the outbreak, significant levels of depression, anxiety and insomnia were reported (McCracken et al., 2020). In England, high levels of depression and anxiety were found during the early stages of the lockdown, followed by a rapid decline as individuals adapted to new circumstances Fancourt et al. (2021). A review by Rajkumar (2020) found consistent evidence that symptoms of anxiety, depression and self-reported stress are common psychological reactions to the pandemic and may also be associated with disturbed sleep.
Existing empirical evidence has often focused on and compared specific sub-groups of the population. The COVID-19 pandemic and lockdown seem particularly stressful for younger adults (Huang and Zhao, 2020; Pieh et al., 2020), females (Wang et al., 2021), individuals with poor self-rated health (Wang et al., 2020) and economically vulnerable people, such as not-working, part-time and contract workers (Ueda et al., 2020). The presence of COVID-19 symptoms and specific health and financial concerns related to the pandemic also appear to be important predictors of psychological distress (McCracken et al., 2020). Exploring the psychological and social effects of COVID-19, Holmes et al. (2020, page 551) claimed that ‘older adults and those with multi-morbidities might be particularly affected by issues including isolation, loneliness, end of life care, and bereavement, which may be exacerbated by the so-called digital divide’. Similarly, the study by Di Gessa and Price (2021) found that clinically vulnerable people (those with specific health profiles and diseases) were more likely to report worse health and social well-being outcomes during the pandemic, even taking pre-pandemic differences into account. Another common and important finding in the current literature is that individuals with pre-existing mental disorders are at a higher risk of relapse or new episodes caused by their disorder (Holmes et al., 2020; McCracken et al., 2020; Yang et al., 2020; Yao et al., 2020).
Determining who is particularly vulnerable to mental health deterioration during the COVID-19 pandemic is essential when designing and targeting interventions with the aim of mitigating the adverse psychological impacts of the outbreak. Although older people have been suggested to have experienced mental health deterioration to a lesser extent compared with younger individuals, they are the population most exposed to the risk of severe illness and death. They are also less equipped to use technologies for coping with lockdown measures and staying connected with family members and friends (Sala et al., 2020; Yu et al., 2016). For such reasons, studying changes in the mental health of the elderly deserves particular attention. The older population includes a very heterogeneous group of people, and disentangling and identifying the characteristics of the most vulnerable individuals is fundamental.
In the current study, we intend to contribute to this topic by shedding light on the mental health of older Europeans during the first wave of the COVID-19 outbreak. In particular, we intend (i) to determine how the depressive symptoms of the population aged 50+ have changed during the first wave of the COVID-19 pandemic and (ii) to identify the individual risk factors associated with changes in depression disorders amongst this population. In answering these research questions, we are interested in (a) exploring whether individuals with pre-existing mental health problems are at a higher risk of depression deterioration and in (b) assessing gender differences.
To achieve the aims of our research, we exploit the richness of the data collected using a special COVID-19 questionnaire administered by the Survey of Health, Ageing and Retirement in Europe (SHARE). SHARE is the first cross-country harmonised ageing survey that collects detailed information to study the health-related and socio-economic impacts of the COVID-19 outbreak. Furthermore, to investigate the role of past mental health problems, we take advantage of SHARE datasets that include multiple items to measure depression; we utilise the depression classification developed by Gennaro et al. (2021) based on the same SHARE respondents interviewed in 2015 and that attributed each individual to a depressive group. We use this refined classification of mental problems amongst older individuals to explore the relationship between belonging to a certain pre-pandemic depressive group and reporting depression-related disorders five years later at the time of COVID-19.
2. Theoretical framework
To study changes in mental health before and during the first wave of the COVID-19 pandemic amongst the older population, we consider and combine two simultaneous processes and phenomena. The first involves understanding the trajectories of mental health and their determinants in normal time. The second consists of the study of the generative mechanisms responsible for depression and sadness during the COVID-19 outbreak. Hence, we try to assess whether mental health patterns may (have) change(d) because of the exogenous shock represented by the pandemic and whether the effects of COVID-19 on depression are different between individuals with and without pre-existing mental health problems.
The incidence of common mental disorders (including depression and anxiety) has increased over the last three decades across high-income countries (Gondek et al., 2021b; Vos et al., 2016). There is a growing amount of evidence showing that mental health problems tend to have a worsening trend from early adulthood (starting from early-30s to mid-40s or mid-50s) as people age, and then reverse and exhibit improvement in late middle age before declining again in the later stages of life (Bell, 2014; Blanchflower and Oswald, 2008; Gondek et al., 2021a; Prior et al., 2020). Likewise, a drop in well-being has been observed in midlife, suggesting that this is a particularly vulnerable phase of life (Blanchflower and Graham, 2020). Such particularly strong vulnerability to psychological distress in midlife has been referred to as ‘midlife mental health crisis’ (Gondek et al., 2021b) and represents the predominant model of the life-course trajectory of mental health in high-income countries. The mechanisms explaining the shape of these trajectories are unclear, and limited theory exists (Gondek et al., 2021b).
Longitudinal studies have been used in the literature to explore the relationships between the course of depression symptoms over old age and various socio-demographic and health-related factors. Trends in mental ill-health have been highly variable and individualised: the ageing and cohort dimensions have explained little variation in these trends (Prior et al., 2020). A longitudinal relationship between changes in mental health, changes in socio-economic factors (including moving from employment to inactivity), and changes in levels of individual deprivation has been identified (Mckenzie et al., 2014), as well as the relationship between depression disorders and health-related behaviours, such as smoking, whose cessation did not result in a worsening of depressive symptoms (Shahab et al., 2015). Depressive trajectories were also found to be associated with a lower education level, a history of poor health and multimorbidity (de la Torre-Luque et al., 2019). The impacts that this pandemic has and will have on mental health trajectories and their dynamic association with various risk factors remain unknown, and whether the midlife mental health crisis will remain as the prevailing trajectory is yet to be studied.
On the other hand, we know from the strand of research focused on disaster mental health that emotional distress is ubiquitous in affected populations (Pfefferbaum and North, 2020). The COVID-19 pandemic, compared with other recent disasters, including epidemics and medical emergencies, is much larger in scale; its consequences are unprecedented and therefore more difficult to predict. From former epidemics, such as the 2003 epidemic of Severe Acute Respiratory Syndrome or the 2014 outbreak of Ebola, we know that restrictive measures, such as quarantine, isolation and social distancing, are related to anxiety, depression, sleep disorders and other problems (Knolle et al., 2021). Similarly and on a larger scale, during the COVID-19 outbreak, uncertain prognoses, shortages of resources for testing and treatment, lack of protective devices and health care providers, imposition of unfamiliar public health measures that limit personal freedoms, large and growing financial losses and conflicting messages from the authorities are amongst the major stressors that undoubtedly may contribute to widespread emotional distress and increase the risk for psychiatric illness associated with COVID-19 in the general population (Pfefferbaum and North, 2020). The economic downturn resulting from the COVID-19 pandemic will have significant consequences for people's health outcomes in the short and longer term (Banks et al., 2020), with the negative effects of economic recessions on people's mental health already being evident (Wahlbeck et al., 2011).
While this applies to the general population, extensive research on health inequalities highlights that the risk of experiencing mental health issues is not equally distributed across society. Those who face the greatest disadvantages in life also face the greatest risk to their mental health worsening (Kousoulis et al., 2020). One of these disadvantages is pre-existing mental health conditions. However, limited attention has been given to the consequences for people with pre-existing mental health problems and the mental health services they use (Rains et al., 2021). Possible short-term impacts on people with pre-existing mental health conditions have been suggested in a recent framework synthesis of international experiences and responses (Rains et al., 2021) and include, amongst others, ‘an amplified effect of being infected with COVID-19 among some groups of people with mental health conditions and concerns regarding equitable provision of physical health care; effects on people with mental health problems resulting from infection control measures, including potential impacts of social isolation, and lack of access to usual supports, activities and community resources’ (Rains et al., 2021, page 14).
These processes of generating depressive symptoms can be understood within the Stress Process Model (Pearlin et al., 1981). This influential model has served as a framework for understanding the mechanisms by which stressors lead to health outcomes. This model distinguishes between three elements of stress: sources (e.g., life events and chronic stressors), outcomes (e.g. mental and physical health problems) and mediators (e.g. self-concepts, social support and coping skills). In our research, this translates into the study of the association between the COVID-19 pandemic and depression deterioration, acting through several measurable (and unmeasurable, hence we talk about association) channels, including social interactions and isolation, as well as coping skills that are likely to be different between individuals with and without pre-existing mental health conditions. Such a model reconciles the theoretical frameworks for our work, although caution must be exercised in the interpretation of the model pillars and statistical jargon (e.g., the mediators were not tested using the corresponding causal model).
3. Data and methods
3.1. Data
The data used in this study came from SHARE, a panel survey on ageing that collects a broad range of information on the health, socio-economic status and social interactions of people aged 50 and over (including their partners, irrespective of age) amongst the European population by means of a Computer-Assisted Personal Interviewing (CAPI) instrument. See Börsch-Supan et al. (2013) for methodological details. As a continuation of SHARE wave 8, a special SHARE COVID-19 survey was administered between June 2020 and August 2020; this involved a sub-sample of SHARE panel respondents being interviewed through a Computer-Assisted Telephone Interview (CATI). The survey collected data on the same topics covered in the standard SHARE questionnaire, but it was shortened and targeted to the COVID-19 living situation of the elderly (Scherpenzeel et al., 2020). In our work, we used SHARE data from the sixth (Malter and Börsch-Supan, 2017) and the eighth waves, collected in 2015 and 2019/2020, respectively (Börsch-Supan, 2020, 2021a), and from the SHARE COVID-19 dataset (Börsch-Supan, 2021b). The longitudinal response rates in wave 6 varied from 52.5% in France to 82.5% in Portugal (Malter and Börsch-Supan, 2017), whereas in the COVID-19 survey they ranged from 58% in Luxembourg to 92% in Croatia (Sand, 2021).
3.2. Size of the final sample
The final sample was composed of 37,475 individuals living in 17 European countries (Austria, Belgium, Croatia, Czech Republic, Denmark, Estonia, France, Germany, Greece, Israel, Italy, Luxembourg, Poland, Slovenia, Spain, Sweden and Switzerland). It comprised all respondents identified in any category of the depression classification carried out by Gennaro et al. (2021) on the SHARE wave 6 data (see Section 3.3.2) who completed the COVID-19 survey.
Panel attrition might be a potential problem in longitudinal surveys, such as SHARE, when old populations are investigated. Even if we did not run a panel analysis, we exploited the longitudinal dimension of SHARE to retrieve useful information across waves. After the wave 6 survey, two other rounds of CAPI data collection were carried out before the first (CATI) SHARE COVID-19 survey. The final sample represented nearly 60% of our wave 6 sample (about 18% of the lost respondents, N = 4,445, deceased over time), and no refreshment sample in any wave after the sixth was included in our analysis. Some reassurance came from the fact that the distribution of several variables (gender, age, education and depression classification) was very similar between the two samples (Table 1 ). The main difference concerned the proportion of the oldest respondents (i.e. older than 84 years), which was lower in the final sample than in wave 6 (as a consequence, the percentage of low educated people decreased from the 2015 sample to the 2020 sample).
Table 1.
Basic characteristics of the final sample.
| Wave 6 sample |
Final sample, reduced by attrition due to: |
|||||
|---|---|---|---|---|---|---|
| mortality |
all reasons |
|||||
| (63,178 units) |
(58,733 units) |
(37,475 units) |
||||
| n | % | n | % | N | % | |
| Gender | ||||||
| Females | 35,828 | 56.7 | 33,832 | 57.6 | 21,937 | 58.5 |
| Age class at 2020 | ||||||
| <60 | 6074 | 9.6 | 6023 | 10.3 | 3716 | 9.9 |
| 60–64 | 9440 | 14.9 | 9292 | 15.8 | 5945 | 15.9 |
| 65–69 | 11,337 | 18.0 | 10,994 | 18.7 | 7308 | 19.5 |
| 70–74 | 11,349 | 18.0 | 10,887 | 18.6 | 7376 | 19.7 |
| 75–79 | 8985 | 14.2 | 8419 | 14.3 | 5541 | 14.8 |
| 80–84 | 7452 | 11.8 | 6650 | 11.3 | 4239 | 11.3 |
| >84 | 8541 | 13.5 | 6468 | 11.0 | 3350 | 8.9 |
| Education | ||||||
| Low (ISCED values lower than 3) | 24,744 | 39.2 | 22,372 | 38.1 | 13,344 | 35.6 |
| Middle (ISCED values equal to 3) | 21,249 | 33.6 | 19,969 | 34.0 | 13,095 | 34.9 |
| High (ISCED values larger than 3) | 17,185 | 27.2 | 16,392 | 27.9 | 11,036 | 29.5 |
| Depression categories at 2015 | ||||||
| Very low risk of depression | 25,706 | 40.7 | 24,387 | 41.5 | 15,523 | 41.4 |
| Low risk of depression | 1526 | 2.4 | 1378 | 2.4 | 786 | 2.1 |
| Middle risk of depression | 11,285 | 17.9 | 10,674 | 18.2 | 7097 | 18.9 |
| High risk of depression | 20,230 | 32.0 | 18,628 | 31.7 | 11,935 | 31.9 |
| Depressed | 1887 | 3.0 | 1484 | 2.5 | 865 | 2.3 |
| Severely depressed | 2057 | 3.3 | 1811 | 3.1 | 1073 | 2.9 |
| Extremely depressed | 487 | 0.7 | 371 | 0.6 | 196 | 0.5 |
Note: ISCED = International Standard Classification of Education.
3.3. Measures
3.3.1. Dependent variable
The standard SHARE questionnaire collects the data required to construct the EURO-D mental scale (Prince et al., 1999), which is a validated depression scale comprising 12 items (depression, pessimism, wishing death, guilt, sleep, interest, irritability, appetite, fatigue, concentration, enjoyment and tearfulness). It is a symptom-oriented, self-assessed scale that determines the presence of various depressive or emotional manifestations on a scale from 0 (the lowest level of depression) to 12 (the highest). The COVID-19 questionnaire utilised only a subset of these items; in particular, we considered the question: In the last month, have you been sad or depressed? In the event of a positive answer, the respondents were asked to assess whether the problem was more, less or about the same as before the outbreak.
Our dependent variable was a dummy equal to 1 if the individual reported being sadder or more depressed at the time of the SHARE COVID-19 interview compared with the months before the global pandemic and 0 otherwise. Hence, we captured whether respondents’ mental health deteriorated following the onset of the pandemic; this means that the dependent variable was set to 0 also if a respondent reported being depressed both before and during the first wave of the pandemic in equally the same way.
3.3.2. Depression before the COVID-19 outbreak
Using SHARE wave 6 data on the EURO-D scale, Gennaro et al. (2021) investigated the heterogeneity of depressive symptoms amongst older people and identified meaningful sub-groups of depressive symptom profiles. They introduced a model-based approach (consisting of a Latent Class Analysis followed by a Factor Analysis based on the individual probabilities of belonging to each class) for classifying individuals in a more accurate way than the simple dichotomisation of ‘depressed/non-depressed’. Seven homogeneous groups of people with different levels of depressive or emotional symptoms were created, indicating those at a lower/higher risk of developing depression. More specifically, the respondents were classified into the following categories: ‘very low risk of depression’, ‘low risk of depression’, ‘middle risk of depression’, ‘high risk of depression’, ‘depressed’, ‘severely depressed’ and ‘extremely depressed’.
We used such classification to identify the pre-existing mental disorders of individuals at our baseline (i.e., wave 6); therefore, we considered a time span of five years from this baseline to the onset of COVID-19 diffusion. We did not use data from the subsequent wave (the seventh) because in SHARE wave 7 information on the EURO-D scale was collected only for a limited sub-sample of respondents. Likewise, we did not use data from wave 8 because it was almost contemporary to the first COVID-19 survey.
3.3.3. Basic individual characteristics
For all respondents, information on gender, year of birth and education was available without any missing values. Age was calculated with reference to 2020. Education was collected as country-specific values and then translated into the International Standard Classification of Education for comparison.
3.3.4. Individual characteristics at the beginning of the COVID-19 outbreak
The eighth wave of SHARE was carried out a few months before the pandemic started. Based on the data collected in this wave, we constructed two groups of respondent characteristics. The first one included health (several chronic diseases, limitations in activities of daily living, instrumental activities of daily living, body mass index), cognitive function (fluency test score), social characteristics (household size, living with a partner, number of living children) and economic conditions (job status, home ownership). The second group measured important and potentially stressful changes in life that occurred just before the COVID-19 outbreak. Specifically, we captured whether within the two years before the COVID-19 pandemic, the respondent i) had become a widow/er, ii) had retired, iii) had a heart attack or stroke or iv) had been diagnosed with cancer. We selected these specific chronic conditions, as they were the only ones tracked over the last two interviews. Most of these variables displayed some missing values, particularly health status (about one third of the sample), while many economic information can be retrieved from the data collected in previous waves. Item non-responses were imputed according to the Multiple Imputation (MI) procedure described in Section 3.4.1.
3.3.5. Individual characteristics during the first wave of the COVID-19 outbreak
The special SHARE COVID-19 survey collected other important information on the socio-economic and health status of the respondents during the first wave of the COVID-19 outbreak: whether anyone in the household tested either positive or negative for COVID-19; whether anyone in the household either died or was hospitalised because of COVID-19; whether the respondent had no or rare (less than once a week) contact with children, parents or friends, either personally or electronically; whether the respondent received any help to get essential supplies or provided help to others; whether the respondent received additional financial support or became unemployed/was laid off because of the health crisis; whether the respondent had left their home since the beginning of the outbreak; and whether the respondent had been diagnosed with a major illness or health condition since the eighth wave SHARE interview.
3.4. Analytical strategy
According to the nature of the dependent variable and the hierarchical structure of the data (individuals nested in countries), random intercept models (Snijders and Bosker, 2012) were tested initially. A multilevel logistic model was estimated, controlling for age and education, using countries as level-2 units (no missing values were present in this dataset). The estimated intra-class correlation coefficients were 3.61% for men and 4.31% for women. These values were very low and provided evidence of little heterogeneity across countries. Therefore, we decided to use standard (uni-level) logistic models with robust standard errors, introducing country dummies to control for the modest between-country variability.
Given that men and women are known to have different profiles of mental health problems (Nolen-Hoeksema, 1990), the analysis was stratified by gender. Models were estimated over the final sample, in which missing values were replaced (Sidi and Harel, 2018) according to the procedure described in Section 3.4.1. Models were sequentially adjusted for basic socio-demographic individual characteristics (age and education) and depression categories in 2015 (Model I), individual characteristics at the beginning of the global pandemic (Model II) and individual characteristics measured during the first wave of the COVID-19 outbreak (Model III), always controlling for country dummies. Average Marginal Effects (AMEs) are calculated to consider the degree of unobserved heterogeneity in the estimated models when point estimates are compared across models and samples (Mood, 2010). Differently from odds ratios, marginal effects are measured in the probability scale, providing absolute measures of health inequality in our analysis.
Inverse-probability weights for each unit were constructed to assess the possible bias resulting from panel attrition; these are based on individual inclusion probabilities obtained through a logistic model, where the dependent variable was equal to 1 if the individual completed the COVID-19 survey, and explanatory variables comprised demographic, health and socio-economic characteristics collected at wave 6. Weighted logistic model estimations, both excluding any item non-responses and including the first round of missing value imputations (as described in Section 3.4.1), were then performed.
To test gender differences, we first estimated the full model on the pooled sample, introducing gender as an explanatory variable (Model IV). As the variable of interest is investigated through a nonlinear model, we cannot estimate the AMEs for the interaction of gender with any variable because the values of interaction terms cannot change independently of the values of all other covariates in the model, even when no interaction term is specified in the model. Therefore, gender differences were evaluated with Marginal Effects at Representative values (MERs), performed over the final model in which the interaction terms with the gender dummy were specified (Williams, 2012).
3.4.1. Missing data treatment
The set of individual characteristics at the beginning of the outbreak suffers from the presence of missing data. MI is widely accepted as the preferable approach to deal with item non-response in surveys (Rubin, 1987). It is a flexible approach for handling missing data, taking the uncertainty derived from the imputation procedure into account. In our analysis, MI was implemented using the Fully Conditional Specification, also known as the Multivariate Imputation by Chained Equations approach (van Buuren, 2007), in which missing data were replaced by iteratively drawing from the fitted conditional distributions of partially observed variables, given the observed and imputed values of the remaining variables in the imputation model. Five imputed datasets were then created.
Marginal effects in multiple imputed datasets are obtained with the STATA module mimrgns (Klein, 2014); it treats the STATA margins itself as an estimation command and combines its results according to Rubin's rules. Applying Rubin's rules to the margins' results assumes asymptotic normality, which is appropriate for AMEs (White et al., 2011); mimrgns cannot obtain correct confidence intervals because its computation is based on inappropriate degrees of freedom, but the differences are usually small (Klein, 2014).
3.4.2. Statistical power and effect size
The effect sizes of the findings are considered to highlight the substantive significance of the model estimates (Bernardi et al., 2016). To this aim, AMEs were reported together with their confidence intervals at the 95% level (Rainey, 2014).
As our work was focused on the increase in sadness/depression compared with one's condition before the beginning of the COVID-19 pandemic rather than on just reporting people's state of being sad/depressed during the interview period (see Section 3.3.1), it was difficult to find previous studies in this research area working with AMEs that might suggest the evaluation of meaningful effect sizes (Schafer and Schwarz, 2019). We therefore applied global conventional benchmarks. According to the scale of our dependent variable and the nature of the phenomenon under investigation, we hypothesised only one effect size, which was equal to 3.9 percentage points for men and 5.4 percentage points for women. Online Appendix B explains how we calculated these benchmarks and why we did not consider small, medium and large effects, as in Cohen (1988) recommendations.
The statistical power of our effect sizes (AMEs in multiple imputed datasets) cannot be exactly computed, so we provided a rough estimate of their power using a simulation approach. Separately by gender, 10,000 samples with replacement were extracted from the first imputed dataset; AMEs were estimated, and their power was computed as the number of times the null hypothesis that each AME be equal to 0 was rejected at the 5% level. The power estimates of the AMEs were reported in Table A6 in the online supplementary materials.
4. Results
4.1. Descriptive evidence
At the time of the first wave of the outbreak, about 59% of the respondents were females and the average age was 71.2 years. The distribution of depression categories was mostly populated in the ‘very low risk of depression’ group (about 41% of the sample) followed by ‘high risk of depression’ (nearly 32%), while around 6% of the respondents belonged to the highest classes of depression, from ‘depressed’ to ‘extremely depressed’ (Table 1). All other socio-demographic and economic characteristics of the sample are reported and described in Tables A1, A2 and A3 of the online supplementary materials.
About a quarter of the respondents reported problems with sadness/depression after the first wave of the pandemic, with 16.3% being sadder or more depressed at the time of the interview than in the months before the outbreak (Table 2 ). As expected, gender differences were quite evident, with twice as many women experiencing higher levels of depression/sadness than men. Surprisingly, the proportion of respondents who were sad or depressed in the last month was much lower than those observed in previous SHARE waves (both for men and women) and this applied to all countries, except Italy, Spain and Greece. This could be attributed to the change in the mode of data collection (from CAPI to CATI) of the COVID-19 survey. However, more than half of the respondents who reported to be depressed in the first months of 2020 (SHARE wave 8) did not report the same answer in the COVID-19 survey: the time span between these two interviews was less than six months. Nevertheless, evaluating how much this affected our dependent variable was difficult because we may think that those respondents who evaluated themselves to be more depressed because of the outbreak can be likelier to report problems with sadness/depression in the first addressed question.
Table 2.
Depression reporting during the first wave of the COVID-19 outbreak of the final sample (37,475 units) - No missing data.
| n | % | |
|---|---|---|
| Sad/depressed at the time of interview (summer 2020) | 9446 | 25.2 |
| Males | 2764 | 17.8a |
| Females | 6682 | 30.5a |
| Sadder/more depressed at the time of interview (summer 2020) than before the COVID-19 outbreak | 6094 | 16.3 |
| Males | 1708 | 11.0a |
| Females | 4386 | 20.0a |
Computed with respect to the size of the specific gender group.
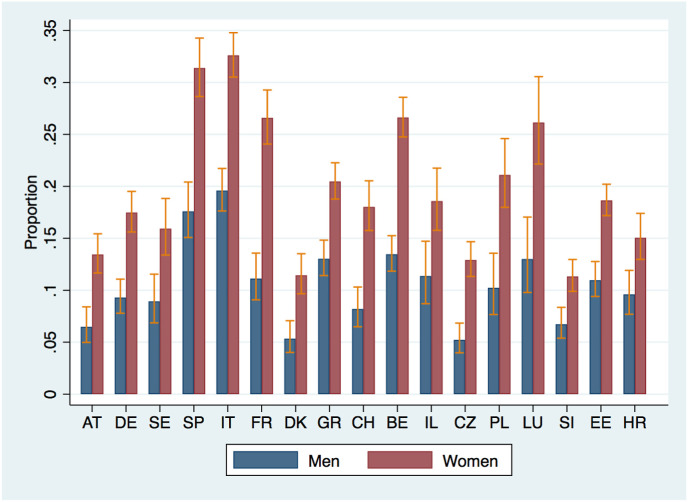
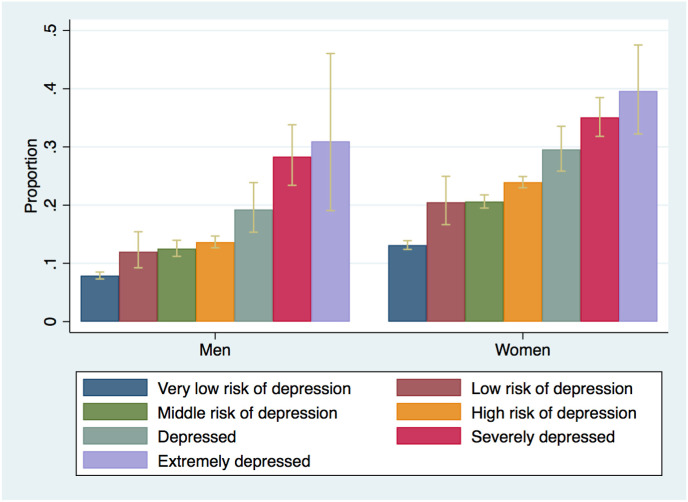
Fig. 1 reports the country-specific distributions of the dependent variable by gender: in all countries, women presented higher proportions than men. Fig. 2 shows the proportion of participants who reported higher depression levels during the COVID-19 outbreak by depression category measured five years earlier. This proportion increased with the severity of the pre-existing depression: about 40% of women and 31% of men classified as extremely depressed in 2015 had more depressive problems five years later, whereas around 10% of the individuals belonging to the very low risk of depression category reported increased depressive problems during the pandemic (7.9% men and 13.1% women).
Fig. 1.
Distribution of reporting to be sadder/more depressed than before the first wave of the COVID-19 outbreak, by country and gender.
Fig. 2.
Distribution of reporting to be sadder/more depressed than before the first wave of the COVID-19 outbreak, by depression categories identified in 2015 (SHARE wave 6).
4.2. Multivariable analyses
Table 3 presents the results from the estimation of Model III, whereas the results from Models I and II are reported in the online materials (Table A4). Country dummy estimates are not reported, but are available upon request. In Model I, all categories of baseline depression were statistically significant, with a higher likelihood of reporting an increase in sadness/depression during the first wave of the pandemic for the most severe categories compared with the least ones, consistent with the findings shown in Fig. 2. As we introduced the other groups of variables into the model (Models II and III), the effect size of the core variables was reduced, but each estimate of the depression categories remained statistically significant. Accounting for all selected risk factors (Model III), individuals with a ‘high risk of depression’ compared with the reference category presented a slightly lower risk than those in Model I (male AME 0.039, 95% CI 0.028:0.051 vs AME 0.054, 95% CI 0.041:0.065 in Model I; female AME 0.085, 95% CI 0.072:0.097 vs 0.102, 95% CI 0.090:0.115 in Model I) and very similar estimates to those obtained in Model II (male AME 0.043, 95% CI 0.032:0.055; female AME 0.089, 95% CI 0.077:0.102).
Table 3.
Estimates of Models III and IV on the probability of reporting to be sadder/more depressed during the first wave of the COVID-19 pandemic than before the outbreak: Average Marginal Effects (AMEs) and their confidence intervals (CI) at the 95% level in multiple imputed dataset.
| Variable | Model III |
Model IV |
||||
|---|---|---|---|---|---|---|
| Males (15,538 units) |
Females (21,937 units) |
All respondents (37,475 units) |
||||
| AME | CI 95% | AME | CI 95% | AME | CI 95% | |
| Age (at 2020) | ||||||
| <60 | ref. | ref. | ref. | |||
| 60–64 | −0.006 | [-0.030 0.017] | −0.005 | [-0.027 0.017] | −0.005 | [-0.021 0.010] |
| 65–69 | −0.016 | [-0.043 0.011] | −0.014 | [-0.039 0.011] | −0.015 | [-0.034 0.003] |
| 70–74 | −0.013 | [-0.040 0.015] | −0.010 | [-0.037 0.017] | −0.012 | [-0.032 0.008] |
| 75–79 | −0.022 | [-0.050 0.007] | −0.020 | [-0.048 0.009] | −0.021 | [-0.042–0.001] |
| 80–84 | 0.010 | [-0.020 0.041] | −0.012 | [-0.042 0.018] | −0.003 | [-0.025 0.019] |
| >84 | −0.014 | [-0.046 0.018] | −0.041 | [-0.072–0.009] | −0.030 | [-0.053–0.008] |
| Education | ||||||
| Low | ref. | ref. | ref. | |||
| Middle | −0.015 | [-0.028–0.002] | −0.010 | [-0.024 0.004] | −0.012 | [-0.022–0.002] |
| High | −0.015 | [-0.028–0.001] | −0.011 | [-0.026 0.005] | −0.013 | [-0.023–0.002] |
| Depression categories (at 2015) | ||||||
| Very low risk of depression | ref. | ref. | ref. | |||
| Low risk of depression | 0.029 | [-0.001 0.059] | 0.054 | [ 0.013 0.095] | 0.043 | [ 0.016 0.069] |
| Middle risk of depression | 0.046 | [ 0.030 0.061] | 0.070 | [ 0.056 0.084] | 0.060 | [ 0.050 0.070] |
| High risk of depression | 0.039 | [ 0.028 0.051] | 0.085 | [ 0.072 0.097] | 0.067 | [ 0.058 0.075] |
| Depressed | 0.064 | [ 0.029 0.100] | 0.108 | [ 0.073 0.143] | 0.091 | [ 0.065 0.116] |
| Severely depressed | 0.142 | [ 0.096 0.188] | 0.161 | [ 0.127 0.194] | 0.147 | [ 0.121 0.173] |
| Extremely depressed | 0.086 | [ 0.000 0.171] | 0.161 | [ 0.091 0.232] | 0.129 | [ 0.075 0.183] |
| Become widow/er (within 2 years before the outbreak) | 0.012 | [-0.030 0.054] | 0.012 | [-0.021 0.044] | 0.013 | [-0.013 0.039] |
| Retired (within 2 years before the outbreak) | 0.003 | [-0.032 0.038] | 0.011 | [-0.023 0.044] | 0.007 | [-0.019 0.033] |
| Had heart attack/stroke (within 2 years before the outbreak) | 0.015 | [-0.010 0.041] | −0.008 | [-0.054 0.038] | 0.007 | [-0.020 0.035] |
| Diagnosed a cancer (within 2 years before the outbreak) | 0.004 | [-0.029 0.038] | 0.025 | [-0.017 0.067] | 0.016 | [-0.011 0.042] |
| Ever diagnosed chronic lung disease | 0.005 | [-0.014 0.025] | 0.006 | [-0.014 0.027] | 0.007 | [-0.008 0.022] |
| Ever diagnosed diabetes | −0.004 | [-0.015 0.008] | −0.002 | [-0.016 0.013] | −0.003 | [-0.013 0.007] |
| Ever diagnosed hypertension |
−0.002 |
[-0.013 0.009] |
0.009 |
[-0.003 0.021] |
0.004 |
[-0.004 0.012] |
| Variable | Model III | Model IV | ||||
| Males (15,538 units) | Females (21,937 units) | All respondents (37,475 units) | ||||
| AME |
CI 95% |
AME |
CI 95% |
AME |
CI 95% |
|
| Ever diagnosed cholesterol | −0.007 | [-0.019 0.006] | −0.001 | [-0.018 0.015] | −0.003 | [-0.013 0.006] |
| Ever diagnosed Alzheimer's disease | −0.018 | [-0.056 0.019] | −0.029 | [-0.064 0.005] | −0.026 | [-0.044–0.007] |
| Ever diagnosed other affective diseases | 0.039 | [ 0.016 0.061] | 0.049 | [ 0.031 0.067] | 0.045 | [ 0.031 0.059] |
| Ever diagnosed rheumatoid arthritis | −0.005 | [-0.021 0.011] | 0.008 | [-0.008 0.024] | 0.002 | [-0.009 0.013] |
| Ever diagnosed osteoarthritis | 0.020 | [ 0.005 0.035] | 0.013 | [ 0.000 0.026] | 0.014 | [ 0.005 0.024] |
| At least one ADL limitation | −0.003 | [-0.024 0.018] | 0.003 | [-0.016 0.022] | 0.001 | [-0.015 0.016] |
| At least one IADL limitation | 0.025 | [ 0.007 0.043] | 0.015 | [-0.013 0.043] | 0.018 | [-0.001 0.037] |
| Body Mass Index | ||||||
| Normal weight/underweighted | ref. | ref. | ref. | |||
| Being overweighted | −0.005 | [-0.017 0.007] | −0.003 | [-0.018 0.011] | −0.005 | [-0.015 0.005] |
| Being obese | 0.002 | [-0.013 0.016] | −0.016 | [-0.031–0.002] | −0.011 | [-0.021–0.001] |
| Fluency test score (cognitive abilities) | −0.001 | [-0.001 0.001] | −0.001 | [-0.002 0.000] | −0.001 | [-0.002 0.000] |
| Household size | −0.005 | [-0.011 0.002] | −0.013 | [-0.021–0.006] | −0.010 | [-0.015–0.005] |
| Living with a partner | −0.009 | [-0.024 0.007] | 0.008 | [-0.006 0.022] | 0.004 | [-0.005 0.014] |
| Number of living children | ||||||
| None | ref. | ref. | ref. | |||
| One | 0.017 | [-0.006 0.039] | 0.020 | [-0.001 0.042] | 0.018 | [ 0.003 0.034] |
| More than one | 0.012 | [-0.007 0.031] | 0.011 | [-0.007 0.030] | 0.011 | [-0.003 0.024] |
| Job status | ||||||
| Employee | ref. | ref. | ref. | |||
| Self-employed | 0.012 | [-0.022 0.046] | −0.038 | [-0.095 0.019] | −0.012 | [-0.046 0.022] |
| Retired | 0.017 | [-0.008 0.042] | 0.003 | [-0.025 0.031] | 0.009 | [-0.012 0.031] |
| Other (unemployed, permanently sick, …) | 0.025 | [-0.006 0.057] | 0.004 | [-0.027 0.035] | 0.011 | [-0.011 0.033] |
| Homemaker | 0.026 | [-0.086 0.137] | 0.007 | [-0.027 0.040] | 0.010 | [-0.016 0.035] |
| House ownership | ||||||
| Owner/Member of a cooperative | ref. | ref. | ref. | |||
| Tenant/Subtenant | 0.020 | [-0.002 0.041] | 0.025 | [ 0.007 0.044] | 0.023 | [ 0.008 0.039] |
| Rent free |
0.006 |
[-0.017 0.029] |
0.013 |
[-0.012 0.037] |
0.010 |
[-0.007 0.027] |
| Variable | Model V | Model IV | ||||
| Males (15,538 units) | Females (21,937 units) | All respondents (37,475 units) | ||||
| AME |
CI 95% |
AME |
CI 95% |
AME |
CI 95% |
|
| Anyone in the hh tested positive for COVID-19 | 0.004 | [-0.016 0.023] | 0.004 | [-0.017 0.025] | 0.004 | [-0.010 0.019] |
| Anyone in the hhtested negative for COVID-19 | 0.030 | [ 0.016 0.044] | 0.044 | [ 0.030 0.058] | 0.038 | [ 0.028 0.048] |
| Anyone in the hh hospitalised due to infection | 0.026 | [-0.003 0.054] | 0.009 | [-0.021 0.040] | 0.016 | [-0.005 0.037] |
| Anyone in the hh died because infection | 0.028 | [-0.001 0.057] | 0.035 | [ 0.001 0.069] | 0.033 | [ 0.010 0.056] |
| Never/rarely personal contacts | 0.022 | [ 0.011 0.033] | 0.028 | [ 0.016 0.040] | 0.026 | [ 0.017 0.035] |
| Never/rarely electronic contacts | −0.006 | [-0.024 0.012] | −0.077 | [-0.100–0.054] | −0.039 | [-0.054–0.023] |
| Helped others outside home | 0.004 | [-0.011 0.019] | 0.016 | [ 0.001 0.032] | 0.011 | [ 0.000 0.022] |
| Were helped by others outside home | 0.047 | [ 0.033 0.060] | 0.070 | [ 0.057 0.083] | 0.060 | [ 0.051 0.070] |
| Received additional financial support | 0.013 | [-0.009 0.034] | 0.025 | [ 0.001 0.048] | 0.019 | [ 0.002 0.035] |
| Become unemployed/were laid off | 0.062 | [ 0.030 0.095] | 0.022 | [-0.008 0.052] | 0.038 | [ 0.016 0.060] |
| Never left home since outbreak | 0.002 | [-0.011 0.016] | −0.003 | [-0.017 0.011] | −0.001 | [-0.011 0.009] |
| Diagnosed major illness since wave8 | 0.085 | [ 0.066 0.104] | 0.084 | [ 0.065 0.103] | 0.085 | [ 0.071 0.098] |
| Being female | – | – | 0.064 | [ 0.056 0.072] | ||
Notes: Model III includes all individual characteristics and is estimated separately by gender.
Model IV runs for the whole sample (men and women) and includes all individual characteristics plus a gender dummy.
ADL = Activity of Daily Living; IADL = Instrumental Activity of Daily Living; hh = household.
Previous diagnoses of certain conditions were also associated with having a higher risk of becoming more depressed/sadder during the pandemic, particularly affective/emotional disorders (male AME 0.039, 95% CI 0.016:0.061; female AME 0.049, 95% CI 0.031:0.067). Other risk factors with positive marginal effects were the presence of someone in the household who tested negative for COVID-19, not having (or rarely having) personal contacts, receiving help outside the home, becoming unemployed only for men (0.062, 95% CI 0.030:0.095) and being diagnosed with a major illness since wave 8, which was the strongest predictor amongst these factors (male AME 0.085, 95% CI 0.066:0.104, female AME 0.084, 95% CI 0.065:0.103). Interestingly, not having electronic contacts with family and friends was negatively associated with the outcome, but it was statistically significant only amongst women (AME -0.077, 95% CI -0.100: −0.054).
A note of attention was devoted to gender differences. Considering the pooled dataset (Table 3, Model IV), we found a statistically significant association between gender and the probability of becoming sadder/more depressed (being female was associated with a 6.4 percentage point increase compared with being male). According to MER evaluations, there were limited gender differences instead in most of the observed characteristics of the sample; the confidence intervals at the 95% level for both genders overlapped for almost all individual variables, except for the category of ‘high risk of depression’ at baseline (male AME 0.040 vs. female AME 0.094) and the lack of electronic contacts during the first wave of the outbreak (male AME -0.010 vs. female AME -0.085), see Figures C1 and C3 in the online Appendix. Gennaro et al. (2021, p. 357) claimed that individuals falling into the high risk of depression category ‘are not yet classified as depressed but should be monitored to prevent future development of depression’, and this applied particularly to women, whose effect size was much larger than that of men.
5. Discussion
Identifying the individuals amongst the older population exposed to a higher risk of mental health deterioration during the COVID-19 outbreak is essential to tailor effective interventions aimed at alleviating the burden of the pandemic on people who are particularly vulnerable. In this study, we intended to determine whether the depressive symptoms of the European population aged 50+ changed during the first wave of the COVID-19 pandemic and to identify the individual risk factors associated with changes in this mental health condition. The most striking finding was the positive relationship between pre-existing depression and the risk of reporting higher levels of sadness or depression during the pandemic. The existence of a gradient in the severity of pre-existing depression persisted even after controlling for a large set of individual characteristics and attitudes measured before and during the outbreak. The association was particularly strong for women, for which we observed a clear gradient (the more severe the depression category, the higher the risk), with effect sizes that are much larger than the meaningful one (the three most severe depression categories had AMEs larger than 10 percentage points). The high statistical power of these tests strengthened the results. For men, the results were similar, but smaller in magnitude: all categories of baseline depression showed a significant association with the outcome, although the two extreme categories, compared with the reference one (‘very low risk of depression’), had a statistically significant difference only at the 10% level, and the power of their test was not large. This could be due to the size of these two classes: half of the men belonged to the ‘very low risk of depression’ category, whereas only about 0.3% of them belonged to the ‘extremely depressed’ category.
Another important finding that corroborates the importance of pre-existing conditions is that being diagnosed with other affective/emotional disorders before the pandemic increased the risk of having higher depressive/sadness problems during the pandemic by about four and five percentage points for men and women, respectively. These effects were highly powered and statistically significant at the 1% level.
As expected, for both genders, not having or having rare personal contacts with family and friends was a risk factor for becoming sad/depressed, although the magnitude was modest (2.2% for men and 2.8% for women, the effects were not meaningful), while only for women the lack of electronic contacts was associated with a reduced risk of higher depression in a meaningful way, ceteris paribus. This finding could be related to the (reasonably low) proportion of old people who have familiarity with technological tools and is inversely correlated with in-person contact such that less electronic contact implies more in-person contact and hence lower depression or sadness levels (Atzendorf and Gruber, 2021).
The risk of being sadder/more depressed was found to increase in the presence of household financial fragility (i.e., tenants/subtenants had higher risk than owners, individuals helped by people external to the household and those who received additional financial support had higher risk compared to respondents who were/did not), probably because of the lack of internal resources or support. For both genders, becoming a widow/er or retiring close to the pandemic did not show statistically significant AMEs.
Current physical health status was weakly related to reporting increased levels of depression. In particular, for both genders, no meaningful effect was observed with a diagnosis of chronic lung disease and this finding was somewhat unexpected because COVID-19 is a respiratory viral disease, and suffering from related conditions may be thought of as a source of fear or stress. Instead, what seems to matter were changes in health conditions during the outbreak. The respondents were at a higher risk of suffering from deteriorating depressive disorders if they were diagnosed with a major illness or health condition during the outbreak, and this was very similar between men and women (the effect size was larger than 8 percentage points) and statistically significant at the 1% level. Being obese was statistically significant at the 5% level only for women, showing a protective role in the risk of increased sadness/depression (this effect was also highly powered). The ‘Jolly Fat’ hypothesis may explain such lower risk, particularly for post-menopausal women (Jasienska et al., 2005).
Having anyone in the household testing negative for COVID-19 showed a positive, meaningful and highly powered association, and similar findings in terms of effect size were observed for the death of anyone in the household resulting from the infection (significant at 1% only for women) and being hospitalised because of COVID-19. No association was found with the presence of a household member positive to COVID-19 test. These results suggest that, during the first COVID-19 wave, when the mode of virus transmission was not completely clear, people were worried about the chance of being infected by the virus more than the fact of being infected (Makhashvili et al., 2020).
The AMEs of current job status were never statistically significant and low powered for both genders, even if meaningful benchmarks belonged to the confidence intervals of these effects for men. For women, meaningful protective effects may be found in the confidence interval of the self-employed condition. Another important and interesting result was that job loss during the first wave of the pandemic (becoming unemployed, being laid off or closing down own's business) was a strong predictor of becoming sadder/more depressed for men (the effect size was larger than six percentage points, statistically significant at the 1% level and highly powered), but not for women (the relationship was not statistically significant, although its confidence interval covered a meaningful effect), even if the proportion of males and females who lost their jobs during the outbreak was substantially the same. Regardless of gender differences, this finding was in line with previous evidence of the association between changes in socio-economic inequalities and mental health (in normal times), such that moving from employment to inactivity is important for short-term mental health outcomes (Mckenzie et al., 2014). Given that we controlled for various measures of economic insecurity, losing one's job could be related to the worsening of mental health not only because of its immediate economic implications, but also through social pressure or loss of individual identity, and men may suffer from these much more than women.
The relationship between age and reporting depression deserved particular attention. Models I (adjusted for a smaller set of confounders) showed some positive, statistically significant and meaningful effects of the oldest age classes, particularly for men. When we introduced socio-economic and health characteristics of the respondents, the estimates were no longer statistically significant for men (but their confidence intervals still included meaningful effects), whereas for women, the 84 years and over group presented a negative and significant association (AME -0.03, power of its test 0.72). This finding should be interpreted considering that in the final sample, the 84 years and above group may suffer the most from attrition, so the survived respondents may be a selected group of the strongest and most resilient individuals. Overall, age was found to be weakly related to an increase in depression status, and this was in line with the results of previous studies showing that the pandemic is particularly stressful for younger adults.
5.1. Strengths and limitations
An important strength of this study comes from the data source used, which provides a timely picture of the population at the time of the pandemic; it covers a wide spectrum of individual characteristics measured during the first wave of the COVID-19 pandemic and the possibility of merging this information with a broader set of indicators collected in previous (regular) waves. Second, we could categorise pre-existing individual depression disorders with a refined classification, accounting for intermediate levels of depression, which proved to be particularly important in predicting mental health deterioration, more than a binary classification, as increasingly recognised in the literature (Pongiglione et al., 2017).
Amongst the limitations of this study, an important one is that the final sample was obtained after different selection steps. Attrition may be a potential problem in our study, even if the comparison of the distribution of some variables included in the analysis suggested that selection bias would affect mostly the oldest old group. To account for this limitation, we estimated weighted logistic models by gender (the results are reported in Table A5 in the online supplementary materials), and very limited differences emerged with the results from Model III. To strengthen the findings of this study, future studies could integrate our analysis with a Heckman sample selection approach (Heckman, 1979), exploiting the longitudinal information available in SHARE. Item non-response is another source of potential bias. We addressed this limitation using MI, which, however, requires the assumption that the mechanism of missingness is at random, and this may not always be the case. The proportion of respondents who reported being sad or depressed in the COVID-19 survey was lower than that in previous SHARE waves; in summer 2021, a second wave of this COVID-19 survey was administered (data not available at the time of writing this paper), and this longitudinal information may be used to further investigate this issue. Second, the depression categories used in the analysis were created from the validated EURO-D depression scale, while the variable of interest was related to just one of the 12 items of this scale. Therefore, this study is not a typical state dependence analysis because later-life depression is characterised by great heterogeneity in terms of symptoms and emotional disorders. However, the outcome may be correlated with unobserved individual heterogeneity, and misspecification of the heterogeneity process could lead to erroneous estimates of the true relationship between pre-existing mental disorders and current depression/sadness reporting (Heckman, 2007). While our final estimated model included a large set of explanatory variables covering several aspects of the socio-economic and health status of the respondents, as soon as data from SHARE COVID-19 survey wave 2 will be available, dynamic models that explicitly investigate state dependence processes might be constructed. Information from all standard waves of SHARE could also be used to consider the correlation between the initial observation and the relevant unobserved factors, which is another potential source of problem in the analysis of longitudinal data (Skrondal and Rabe-Hesketh, 2014). In the end, even if a limited between-country variability was found in the analysis, the introduction of country dummies might not be enough to completely control for such heterogeneity. There are differences across countries in terms of the time and way they experienced the first wave of the outbreak, as well as the contrasting measures used to fight the virus. Likewise, there could be country differences in retirement ages and educational levels. Cross-country comparisons need to be further studied, also taking response and attrition rates into account.
6. Conclusions
Determining who is vulnerable to the mental health disorders caused by and associated with COVID-19 is essential when designing and implementing evidence-based interventions to mitigate the adverse psychological impacts of the outbreak. Our analysis clearly shows that pre-existing mental health problems are strongly associated with depression deterioration during COVID-19, and using a refined classification of the risk of depression can be very helpful in identifying a wider spectrum of older adults who might report depressive symptoms during an outbreak, such as the COVID-19 pandemic. Indeed, a multi-categorical classification of depression, that goes beyond a dichotomisation, is important because people in intermediate levels who may not be classified as depressed (e.g., those in the ‘high risk of depression’ group) show important disadvantages compared with individuals with the lowest level of depression at baseline. Not just pre-existing mental health problems, but also the diagnosis of some affective/emotional disorders before lockdown and being diagnosed with a major illness before the onset of the first wave of COVID-19 result in a higher risk of reporting to be sadder or more depressed during the pandemic. This suggests a general concern and feeling of vulnerability for having health problems during a health emergency. Stressful events that occurred during the first wave of the outbreak also represent a risk factor, especially losing a job, but only for men. Gender differences emerge as well: women not only have higher levels of depression than men in ‘normal times’, but they also report higher levels of increasing depression than men in the first wave of the outbreak; women with pre-existing mental health problems, at each severity level, are exposed to a much higher risk of worsening mental health.
Credit author statement
Paccagnella Omar: Conceptualization, Methodology, Software, Formal analysis, Writing – original draft, Writing – review & editing Pongiglione Benedetta: Conceptualization, Writing – original draft, Writing – review & editing
Acknowledgments
The authors are grateful to the Associate Editor and two anonymous referees for their helpful comments and suggestions. This paper uses data from SHARE Wave 6 (DOI: 10.6103/SHARE.w6.710, Wave 8 (DOI: 10.6103/SHARE.w8.100) and Wave 8.COVID-19 Survey 1 (DOI: 10.6103/SHARE.w8ca.100). The SHARE data collection has been funded by the European Commission, DG RTD through FP5 (QLK6-CT-2001-00360), FP6 (SHARE-I3: RII-CT-2006-062193, COMPARE: CIT5-CT-2005-028857, SHARELIFE: CIT4-CT-2006-028812), FP7 (SHARE-PREP: GA N°211909, SHARE-LEAP: GA N°227822, SHARE M4: GA N°261982, DASISH: GA N°283646) and Horizon 2020 (SHARE-DEV3: GA N°676536, SHARE-COHESION: GA N°870628, SERISS: GA N°654221, SSHOC: GA N°823782, SHARE-COVID19: GA N°101015924) and by DG Employment, Social Affairs & Inclusion through VS 2015/0195, VS 2016/0135, VS 2018/0285, VS 2019/0332, and VS 2020/0313. Additional funding from the German Ministry of Education and Research, the Max Planck Society for the Advancement of Science, the U.S. National Institute on Aging (U01_AG09740-13S2, P01_AG005842, P01_AG08291, P30_AG12815, R21_AG025169, Y1-AG-4553-01, IAG_BSR06-11, OGHA_04-064, HHSN271201300071C, RAG052527A) and from various national funding sources is gratefully acknowledged (see www.share-project.org).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.socscimed.2022.114828.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Atzendorf J., Gruber S. Depression and loneliness of older adults in Europe and Israel after the first wave of covid-19. Eur. J. Ageing. 2021 doi: 10.1007/s10433-021-00640-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banks J., Karjalainen H., Propper C. Recessions and health: the long-term health consequences of responses to the coronavirus. Fisc. Stud. 2020;41(2):337–344. doi: 10.1111/1475-5890.12230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bann D., Villadsen A., Maddock J., Hughes A., Ploubidis G., Silverwood R., Patalay P. Changes in the behavioural determinants of health during the COVID-19 pandemic: gender, socioeconomic and ethnic inequalities in five British cohort studies. J. Epidemiol. Community Health. 2021;75:1136–1142. doi: 10.1136/jech-2020-215664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell A. Life-course and cohort trajectories of mental health in the UK, 1991-2008-a multilevel age-period-cohort analysis. Soc. Sci. Med. 2014;120:21–30. doi: 10.1016/j.socscimed.2014.09.008. [DOI] [PubMed] [Google Scholar]
- Bernardi F., Chakhaia L., Leopold L. Sing me a song with social significance‘: the (mis)use of statistical significance testing in European sociological research. Eur. Socio Rev. 2016;33:1–15. [Google Scholar]
- Blanchflower D., Graham C. 2020. The Mid-life Dip in Well-Being: Economists (Who Find it) versus Psychologists (Who Don't)! NBER Working. Paper No. w26888. [Google Scholar]
- Blanchflower D., Oswald A. Is well-being U-shaped over the life cycle? Soc. Sci. Med. 2008;66(8):1733–1749. doi: 10.1016/j.socscimed.2008.01.030. [DOI] [PubMed] [Google Scholar]
- Börsch-Supan A. SHARE-ERIC. Data set; 2020. Survey of Health, Ageing and Retirement in Europe (SHARE) Wave 6. Release Version: 7.1.0. [DOI] [Google Scholar]
- Börsch-Supan A. SHARE-ERIC. Data set; 2021. Survey of Health, Ageing and Retirement in Europe (SHARE) Wave 8. Release Version: 1.0.0. [DOI] [Google Scholar]
- Börsch-Supan A. SHARE-ERIC. Data set; 2021. Survey of Health, Ageing and Retirement in Europe (SHARE) Wave 8. COVID-19 Survey 1. Release Version: 1.0.0. [DOI] [Google Scholar]
- Börsch-Supan A., Brandt M., Hunkler C., Kneip T., Korbmacher J., Malter F., Schaan B., Stuck S., Zuber S. Data resource profile: the survey of health, ageing and retirement in Europe (SHARE) Int. J. Epidemiol. 2013;42(4):992–1001. doi: 10.1093/ije/dyt088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi E., Hui B., Wan E. Depression and anxiety in Hong Kong during COVID-19. Int. J. Environ. Res. Publ. Health. 2020;17(10):3740. doi: 10.3390/ijerph17103740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. 2 ed. Academic Press; New York, NY: 1988. Statistical Power Analysis for the Behavioral Sciences. [Google Scholar]
- de la Torre-Luque A., de la Fuente J., Prina M., Sanchez-Niubo A., Haro J., Ayuso-Mateos J. Long-term trajectories of depressive symptoms in old age: relationships with sociodemographic and health-related factors. J. Affect. Disord. 2019;246:329–337. doi: 10.1016/j.jad.2018.12.122. [DOI] [PubMed] [Google Scholar]
- Di Gessa G., Price D. Changes in health and social well-being in the COVID-19 clinically vulnerable older English population during the pandemic. J. Epidemiol. Community Health. 2021;75:1070–1077. doi: 10.1136/jech-2021-216405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ettman C., Abdalla S., Cohen G., Sampson L., Vivier P., G S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw. Open. 2020;3(9) doi: 10.1001/jamanetworkopen.2020.19686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fancourt D., Steptoe A., Bu F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: a longitudinal observational study. Lancet Psychiatr. 2021;8(2):141–149. doi: 10.1016/S2215-0366(20)30482-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gennaro C., Paccagnella O., Zaninotto P. A model-driven approach to better identify older people at risk of depression. Ageing Soc. 2021;41:339–361. [Google Scholar]
- Gondek D., Bann D., Patalay P., Goodman A., McElroy E., Richards M., Ploubidis G. Psychological distress from early adulthood to early old age: evidence from the 1946, 1958 and 1970 British birth cohorts. Psychol. Med. 2021:1–10. doi: 10.1017/S003329172000327X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gondek D., Moltrecht B., Ploubidis G. Mental health crisis in midlife - a proposed research agenda. Research Ideas and Outcomes. 2021;7 [Google Scholar]
- Heckman J. Sample selection bias as a specification error. Econometrica. 1979;47(1):153–162. [Google Scholar]
- Heckman J. In: Studies in Labor Markets. Rosen S., editor. University of Chicago Press; Chicago: 2007. 3. Heterogeneity and state dependence; pp. 91–140. [Google Scholar]
- Holmes E., O'Connor R., Perry H., Tracey I., Wessely S., Arseneault L., Ballard C., Christensen C., et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatr. 2020;7(6):547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Y., Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatr. Res. 2020;288:112954. doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jasienska G., Ziomkiewicz A., Górkiewicz M., Pajak A. Body mass, depressive symptoms and menopausal status: an examination of the ”Jolly Fat” hypothesis. Wom. Health Issues. 2005;15(3):145–151. doi: 10.1016/j.whi.2005.02.002. [DOI] [PubMed] [Google Scholar]
- Klein D. Boston College Department of Economics; 2014. MIMRGNS: Stata Module to Run Margins after MI Estimate. Statistical Software Components S457795. revised 28 Feb 2021. [Google Scholar]
- Knolle F., Ronan L., Murray G. The impact of the COVID-19 pandemic on mental health in the general population: a comparison between Germany and the UK. BMC psychology. 2021;9:1–17. doi: 10.1186/s40359-021-00565-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kousoulis A., McDaid S., Crepaz-Keay D., Solomon S., Lombardo C., Yap J., Weeks L., O'Sullivan C., Baird R., Grange R. Mental Health Foundation; Glasgow: 2020. The COVID-19 Pandemic, Financial Inequality and Mental Health. [Google Scholar]
- Makhashvili N., Javakhishvili J., Sturua L., Pilauri K., Fuhr D., Roberts B. The influence of concern about COVID-19 on mental health in the republic of Georgia: a cross-sectional study. Glob. Health. 2020;16:111. doi: 10.1186/s12992-020-00641-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malter F., Börsch-Supan A. Munich Center for the Economics of Aging; Munich, Germany: 2017. SHARE Wave 6: Panel Innovations and Collecting Dried Blood Spots. (MEA) [Google Scholar]
- Mazza M., De Lorenzo R., Conte C., Poletti S., Vai B., Bollettini I., Melloni E., Furlan R., Ciceri F., Rovere-Querini P., Benedetti F. Anxiety and depression in COVID-19 survivors: role of inflammatory and clinical predictors. Brain Behav. Immun. 2020;89:594–600. doi: 10.1016/j.bbi.2020.07.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCracken L., Badinlou F., Buhrman M., Brocki K. Psychological impact of COVID-19 in the Swedish population: depression, anxiety, and insomnia and their associations to risk and vulnerability factors. Eur. Psychiatr. 2020;63(1):1–9. doi: 10.1192/j.eurpsy.2020.81. e81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKenzie S., Gunasekara F., Richardson K., Carter K. Do changes in socioeconomic factors lead to changes in mental health? Findings from three waves of a population based panel study. J. Epidemiol. Community Health. 2014;68(3):253–260. doi: 10.1136/jech-2013-203013. [DOI] [PubMed] [Google Scholar]
- Mood C. Logistic regression: why we cannot do what we think we can do, and what we can do about it. Eur. Socio Rev. 2010;26(1):67–82. [Google Scholar]
- Nolen-Hoeksema S. Stanford University Press; Stanford, CA: 1990. Sex Differences in Depression. [Google Scholar]
- Pearlin L., Menaghan E., Lieberman M., Mullan J. The stress process. J. Health Soc. Behav. 1981;22(4):337–356. [PubMed] [Google Scholar]
- Pfefferbaum B., North C. Mental health and the COVID-19 pandemic. N. Engl. J. Med. 2020;383(6):510–512. doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- Pieh C., Budimir S., Probst T. The effect of age, gender, income, work, and physical activity on mental health during coronavirus disease (COVID-19) lockdown in Austria. J. Psychosom. Res. 2020;136:110186. doi: 10.1016/j.jpsychores.2020.110186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce M., Hope H., Ford T., Hatch S., Hotopf M., John A., Kontopantelis E., Webb R., Wessely S., McManus S. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatr. 2020;7(10):883–892. doi: 10.1016/S2215-0366(20)30308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pongiglione B., Ploubidis G., De Stavola B. Levels of disability in the older population of England: comparing binary and ordinal classifications. Disability and Health Journal. 2017;10(4):509–517. doi: 10.1016/j.dhjo.2017.01.005. [DOI] [PubMed] [Google Scholar]
- Prince M., Reischies F., Beekman A., Fuhrer R., Jonker S., Kivelä C., Lawlor B., Lobo A., Magnusson H., Fichter I., van Oyen H., Roelands M., Skoog I., Turrina C., Copeland J. Development of the EURO-D scale - a European Union initiative to compare symptoms of depression in 14 European centres. Br. J. Psychiatry. 1999;174(4):330–338. doi: 10.1192/bjp.174.4.330. [DOI] [PubMed] [Google Scholar]
- Prior L., Jones K., Manley D. Ageing and cohort trajectories in mental ill-health: an exploration using multilevel models. PLoS One. 2020;15(7) doi: 10.1371/journal.pone.0235594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rainey C. Arguing for a negligible effect. Am. J. Polit. Sci. 2014;58:1083–1091. [Google Scholar]
- Rains L., Johnson S., Barnett P., Steare T., Needle J., Carr S., Taylor B., Bentivegna F., Edbrooke-Childs J., Scott H. Early impacts of the COVID-19 pandemic on mental health care and on people with mental health conditions: framework synthesis of international experiences and responses. Soc. Psychiatr. Psychiatr. Epidemiol. 2021;56(1):13–24. doi: 10.1007/s00127-020-01924-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajkumar R. COVID-19 and mental health: a review of the existing literature. Asian Journal of Psychiatry. 2020;52:102066. doi: 10.1016/j.ajp.2020.102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers J., Chesney E., Oliver D., Pollak T., McGuire P., Fusar-Poli P., Zandi M., Lewis G., David A. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatr. 2020;7(7):611–627. doi: 10.1016/S2215-0366(20)30203-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin D. John Wiley & Sons; 1987. Multiple Imputation for Nonresponse in Surveys. [Google Scholar]
- Sala E., Gaia A., Cerati G. 2020. The Gray Digital Divide in Social Networking Site Use in Europe: Results from a Quantitative Study. Social Science Computer Review. First Published. [Google Scholar]
- Salari N., Hosseinian-Far A., Jalali R., Vaisi-Raygani A., Rasoulpoor S., Mohammadi M., Rasoulpoor S., Khaledi-Paveh B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Glob. Health. 2020;16:57. doi: 10.1186/s12992-020-00589-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sand G. In: SHARE Wave 8 Methodology: Collecting Cross-National Survey Data in Times of COVID-19. Bergmann M., Börsch-Supan A., editors. MEA; Munich: 2021. Fieldwork monitoring and survey participation in the first telephone-based SHARE Corona Survey. (forthcoming) [Google Scholar]
- Schafer T., Schwarz M. The meaningfulness of effect sizes in psychological research: differences between sub-disciplines and the impact of potential biases. Front. Psychol. 2019;10:813. doi: 10.3389/fpsyg.2019.00813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scherpenzeel A., Axt K., Bergmann M., Douhou S., Oepen A., Sand G., Schuller K., Stuck S., Wagner M., Börsch-Supan A. Collecting survey data among the 50+ population during the COVID-19 outbreak: the survey of health, ageing and retirement in Europe (SHARE) Survey Research Methods. 2020;14(2):217–221. [Google Scholar]
- Shahab L., Gilchrist G., Hagger-Johnson G., Shankar A., West E., West R. Reciprocal associations between smoking cessation and depression in older smokers: findings from the English longitudinal study of ageing. Br. J. Psychiatry. 2015;207(3):243–249. doi: 10.1192/bjp.bp.114.153494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sidi Y., Harel O. The treatment of incomplete data: reporting, analysis, reproducibility, and replicability. Soc. Sci. Med. 2018;209:169–173. doi: 10.1016/j.socscimed.2018.05.037. [DOI] [PubMed] [Google Scholar]
- Skrondal A., Rabe-Hesketh S. Handling initial conditions and endogenous covariates in dynamic/transition models for binary data with unobserved heterogeneity. Journal of the Royal Statistical Society - Series C (Applied Statistics) 2014;63:211–237. [Google Scholar]
- Snijders T., Bosker R. 2 ed. Sage Publishers; London: 2012. Multilevel Analysis: an Introduction to Basic and Advanced Multilevel Modeling. [Google Scholar]
- Tomasoni D., Bai F., Castoldi R., Barbanotti D., Falcinella C., Mulé G., Mondatore D., Tavelli A., Vegni E., Marchetti G., d'Arminio Monforte A. Anxiety and depression symptoms after virological clearance of COVID-19: a cross-sectional study in Milan, Italy. J. Med. Virol. 2021;93(2):1175–1179. doi: 10.1002/jmv.26459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ueda M., Stickley A., Sueki H., Matsubayashi T. 2020. Mental Health Status of the General Population during the COVID-19 Pandemic: A Cross-Sectional National Survey in Japan. medRxiv 2020.04.28.20082453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Buuren S. Multiple Imputation of discrete and continuous data by fully conditional specification. Stat. Methods Med. Res. 2007;16:219–242. doi: 10.1177/0962280206074463. [DOI] [PubMed] [Google Scholar]
- Vos T., Allen C., Arora M., Barber R., Bhutta Z., Brown A., Carter A., Casey D., Charlson F., Chen A. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the global burden of disease study 2015. Lancet. 2016;388(10053):1545–1602. doi: 10.1016/S0140-6736(16)31678-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wahlbeck K., Anderson P., Basu S., McDaid D., Stuckler D. World Health Organization; 2011. Impact of Economic Crises on Mental Health. [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C., Ho R. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Publ. Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Di Y., Ye J., Wei W. Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID-19) in some regions of China. Psychol. Health Med. 2021;26(1):13–22. doi: 10.1080/13548506.2020.1746817. [DOI] [PubMed] [Google Scholar]
- White I., Royston P., Wood M. Multiple Imputation using chained equations: issues and guidance for practice. Stat. Med. 2011;30:377–399. doi: 10.1002/sim.4067. [DOI] [PubMed] [Google Scholar]
- Williams R. Using the margins command to estimate and interpret adjusted predictions and marginal effects. STATA J. 2012;12(2):308–331. [Google Scholar]
- Yang Y., Li W., Zhang Q., Zhang L., Cheung T., Xiang Y.-T. Mental health services for older adults in China during the COVID-19 outbreak. Lancet Psychiatr. 2020;7(4):e19. doi: 10.1016/S2215-0366(20)30079-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao H., Chen J., Xu Y. Rethinking online mental health services in China during the COVID-19 epidemic. Asian Journal of Psychiatry. 2020;50:102015. doi: 10.1016/j.ajp.2020.102015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu R., Ellison N., McCammon R., Langa K. Mapping the two levels of digital divide: internet access and social network site adoption among older adults in the USA. Inf. Commun. Soc. 2016;19(10):1445–1464. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.