Abstract
Airborne transmission of SARS-CoV-2 has been increasingly recognized in the outbreak of COVID-19, especially with the Omicron variant. We investigated an outbreak due to Omicron variant in a restaurant. Besides epidemiological and phylogenetic analyses, the secondary attack rates of customers of restaurant-related COVID-19 outbreak before (Outbreak R1) and after enhancement of indoor air dilution (Outbreak R2) were compared. On 27th December 2021, an index case stayed in restaurant R2 for 98 min. Except for 1 sitting in the same table, six other secondary cases sat in 3 corners at 3 different zones, which were served by different staff. The median exposure time was 34 min (range: 19–98 min). All 7 secondary cases were phylogenetically related to the index. Smoke test demonstrated that the airflow direction may explain the distribution of secondary cases. Compared with an earlier COVID-19 outbreak in another restaurant R1 (19th February 2021), which occurred prior to the mandatory enhancement of indoor air dilution, the secondary attack rate among customers in R2 was significantly lower than that in R1 (3.4%, 7/207 vs 28.9%, 22/76, p<0.001). Enhancement of indoor air dilution through ventilation and installation of air purifier could minimize the risk of SARS-CoV-2 transmission in the restaurants.
Keywords: Outbreak investigation, Airborne transmission, Omicron, Restaurant, Indoor air dilution, Ventilation
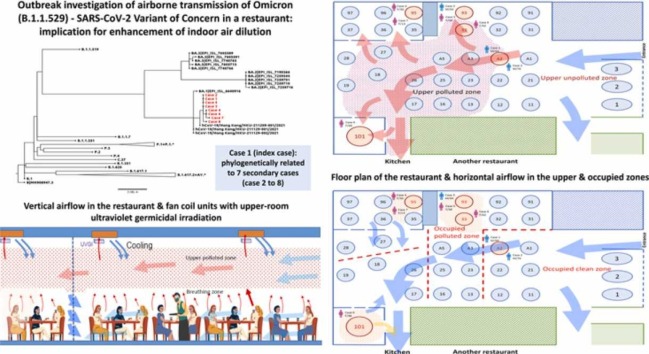
Graphical Abstract
1. Introduction
The Coronavirus Disease 2019 (COVID-19) pandemic caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is the most devastating emerging infectious disease in the 21st century. The cumulative number of infected cases had already exceeded 278 million with almost 5.4 million deaths as of 26th December 2021 (Weekly epidemiological 2021). There has been a steep increase in case number since the emergence of the Omicron (B.1.1.529) - SARS-CoV-2 variant of concern (VOC) (Classification of Omicron 2021). The Omicron variant appeared to be less likely to cause severe disease compared with previously reported VOCs (Abdullah et al., 2021), probably due to less efficient replication and virus-cell fusion as shown in transmembrane serine protease 2-overexpressing VeroE6 cells (Zhao et al., 2021). However, the effective reproduction number of the Omicron variant is 3 times greater than that of Delta under the same epidemiological conditons (Ito et al., 2021), which may be related to the potential for better airborne transmissibility (X. Li et al., 2021), epidemic fatigue of the public and decreased compliance to control measures, and reduced neutralizing antibody activity against the Omicron variant in vaccine recipients (Lu et al., 2021).
In Hong Kong, we adopted stringent measures on border control and required all inbound travelers arriving at the Hong Kong International Airport (HKIA) to undergo compulsory quarantine in designated quarantine hotels for up to 21 days, except for the air crew who were allowed to be quarantined at home if the first SARS-CoV-2 by reverse transcription polymerase chain reaction (RT-PCR) test at the HKIA was negative. With these measures in place, community outbreak was put under control when the fourth wave of COVID-19 came to an end in April 2021. Despite sporadic episodes of SARS-CoV-2 transmission in designated quarantine hotels between persons under compulsory quarantine (Wong et al., 2021, Wong et al., 2021), they did not result in a new wave of COVID-19 in the community (Cheng et al., 2021a).
However, there remains substantial risk of COVID-19 outbreak in Hong Kong due to quarantine exemption of air crew, especially with the global spread of Omicron variant. The risk of SARS-CoV-2 transmission is highest in the indoor areas, such as eateries and bars, where air crew carrying Omicron variant may visit and where people take off their masks during drinking and dining.
In March 2021, the Hong Kong Special Administrative Region Government passed a new legislation mandating the enhancement of air change or addition of air purifier in seating areas of dine-in catering premises to reduce the risk of indoor transmission of SARS-CoV-2 (Air change 2022). In brief, catering businesses are required to attain an air change per hour (ACH) of 6 or above in seating areas. If not feasible, air purifiers can be installed as an alternative measure to reduce the risk of airborne transmission of SARS-CoV-2 (Final Report 2022). Here, we report an incident of COVID-19 outbreak due to the Omicron variant in a restaurant with a relatively lower secondary attack rate, likely as a result of indoor air dilution enhancement by ultraviolet-C air purifying system.
2. Methods
2.1. Epidemiology of COVID-19 in Hong Kong
Since the official announcement of the outbreak of community acquired pneumonia in Wuhan, Hubei Province on 31st December 2019 (The Centre for Health Protection, 2022), rapid and dynamic public health and infection control measures were implemented in the community and hospitals in response to the evolving epidemic to minimize the number of COVID-19 infection (Cheng et al., 2020a, Cheng et al., 2020c, Cheng et al., 2021c; Wong et al., 2020, Wong et al., 2021). Each COVID-19 case, regardless of symptoms, was investigated for the potential source of acquisition. The epidemiological information was uploaded onto the website of the Centre for Health Protection, Department of Health, the Government of Hong Kong Special Administrative Region, China (COVID-19 2022).
2.2. Restaurant-related COVID-19 outbreaks before and after enhancement of air dilution in catering premises
We performed detailed analysis of the epidemiology of COVID-19 cases in Hong Kong, especially for cases who had acquired the infection from restaurants. Outbreak investigation was conducted in a restaurant with COVID-19 outbreak due to the Omicron variant (Outbreak R2) to understand the risk of SARS-CoV-2 transmission among customers. The secondary attack rate of the current episode was compared with a prior COVID-19 outbreak in another restaurant (Outbreak R1) on 19th February 2021, which was before the mandatory implementation of enhancement of air dilution in catering premises.
2.3. Estimation of quanta generation
Estimation of quanta generation in outbreaks R2 and R1 was carried out by using a steady-state mathematical model to describe the transmission of airborne infectious diseases, which is known as the Wells-Riley equation (Riley et al., 1978). The volume of air and the air change rate were measured to calculate the virus-free air. An aerosol deposition rate of 0.30 h−1 and virus deactivation rate of 0.63 h−1 were adopted as described previously (Miller et al., 2021). A pulmonary flow rate per susceptible person of 0.15 L/s was used for the estimation. The median duration of exposure to the infectious case among the susceptible person was recorded.
2.4. Study design and participants
This is a descriptive epidemiological study to evaluate the effect of air dilution enhancement in restaurants on the secondary attack rate of COVID-19 outbreak. For the air crew who were required to undergo compulsory testing for COVID-19, symptomatic patients, and asymptomatic persons who were tested for contact tracing purpose, combined nasal and throat swabs were collected by staff with training in community testing centers, or in hospitals including the newly built temporary hospital adjacent to the community treatment facility at AsiaWorld-Expo in Hong Kong. Respiratory specimens such as nasopharyngeal swabs, throat swabs, and sputa were collected for serial monitoring of viral load by RT-PCR upon hospitalization. Deep throat saliva was accepted as an alternative specimen (To et al., 2020). Whole genome sequencing was performed on respiratory specimens or deep throat saliva from laboratory-confirmed COVID-19 cases. This study was approved by the Institutional Review Board of The University of Hong Kong/Hospital Authority Hong Kong West Hospital Cluster.
2.5. Whole genome sequencing
Whole genome sequencing of SARS-CoV-2 was performed using Nanopore sequencing technology (Oxford Nanopore Technologies, Oxford, UK) as we previously described (Chan et al., 2021). Briefly, RNA extracted from respiratory specimens by QIAamp Viral RNA Kit (Qiagen, Hilden, Germany) was reverse transcribed into cDNA using SuperScriptTM IV reverse transcriptase (ThermoFisher Scientific, Waltham, MA, USA). PCR was then performed using the ARTIC nCov-2019 V3 Panel (IDT, USA) and Q5® Hot Start High-Fidelity 2X Master Mix (New England Biolabs, Ipswich, Massachusetts, United States). PCR products clean-up was done by 1x Agencourt AMPure XP (Beckman Coulter, California, USA). End-prep, barcode ligation and sequencing adaptor ligation were performed according to the PCR tiling of SARS-CoV-2 virus with Native Barcoding Expansion 96 protocol (Version: PTCN_9103_v109_revH_13Jul2020). The library was loaded and sequenced on MinION with R9.4.1 flow cells for 48 h. Nanopore sequencing data were analyzed using Artic Network nCoV-2019 novel coronavirus bioinformatics protocol (Loman and Rambaut 2020).
2.6. Phylogenetic analysis
The sequences were first aligned using MAFFT (Katoh and Standley 2013). The maximum-likelihood whole genome phylogenetic tree was constructed using IQTREE (Nguyen et al., 2015). The best fit substitution model was chosen automatically according to the Bayesian information criterion score (BIC). Then 1000 ultrafast bootstraps were applied to calculate the final tree. The unrelated substructures of the tree with branch length representing mutation count of less than 1 were removed using the -czb option. Finally, the SARS-CoV-2 reference genome (accession no.: MN908947.3) is chosen as the outgroup representative.
2.7. Statistical analysis
Differences in the secondary attack rates of SARS-CoV-2 acquisition in restaurants were evaluated using Chi-square test or Fisher exact test for categorical variables. Statistical analyses were performed using IBM SPSS Statistics (version 26). A two-sided p-value of <0.05 was considered statistically significant.
2.8. Role of the funding source
The funding sources had no role in the study design, data collection, analysis, interpretation, or writing of the report. The corresponding author had full access to all data in the study and had the final responsibility for the decision to submit for publication.
3. Results
3.1. Epidemiology of COVID-19 in Hong Kong
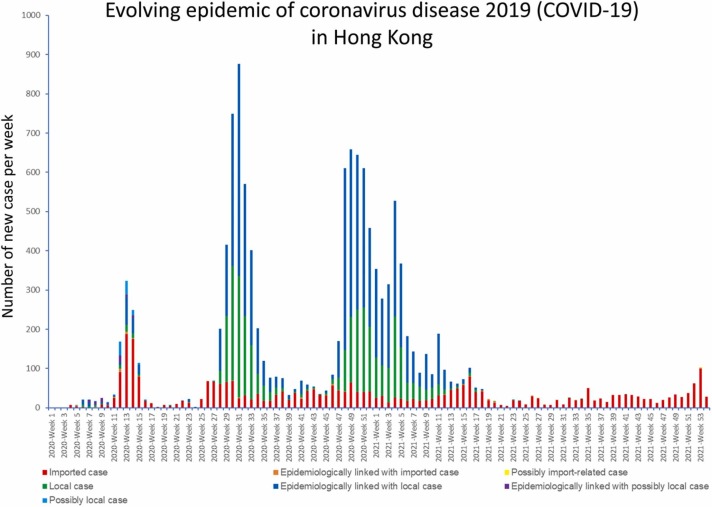
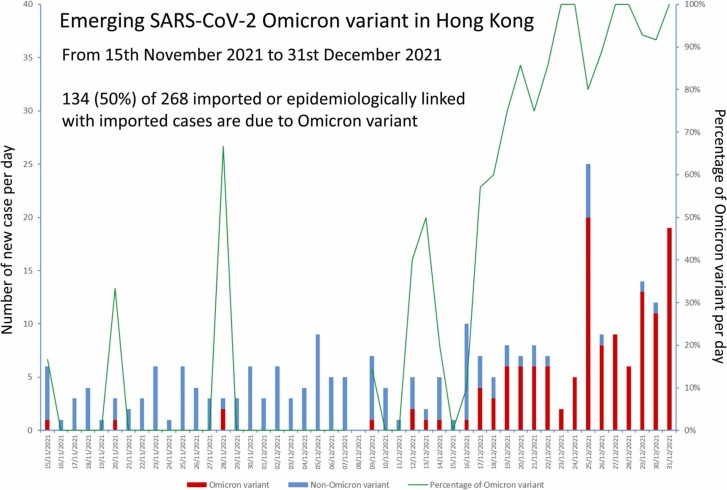
By 31st December 2021, there were 12,655 laboratory-confirmed COVID-19 cases in Hong Kong of whom 6113 (48.3%) were male. The median age was 43 years (range, 1 month to 100 years). The overall case-fatality ratio was 1.7% (213/12,655). The weekly number of COVID-19 cases was shown in Fig. 1. Imported cases and their secondary cases constituted 26.1% (3306/12,655) of all COVID-19 patients. The proportion of imported cases and their secondary cases significantly increased to 99.3% (807/813) between 1st June 2021 and 31st December 2021 (p<0.001). The first case of the Omicron variant was retrospectively recognized in an imported case on 15th November 2021. Among 268 imported or epidemiologically linked with imported cases between 15th November 2021 and 31st December 2021, 134 (50.5%) were infected by the Omicron variant ( Fig. 2).
Fig. 1.
Evolving epidemic of coronavirus disease 2019 (COVID-19) in Hong Kong.
Note: The number of newly diagnosed COVID-19 case was illustrated in weekly interval.
Fig. 2.
Emerging SARS-CoV-2 Omicron variant in Hong Kong.
3.2. Restaurant-related COVID-19 outbreaks before and after enhancement of air dilution in catering premises
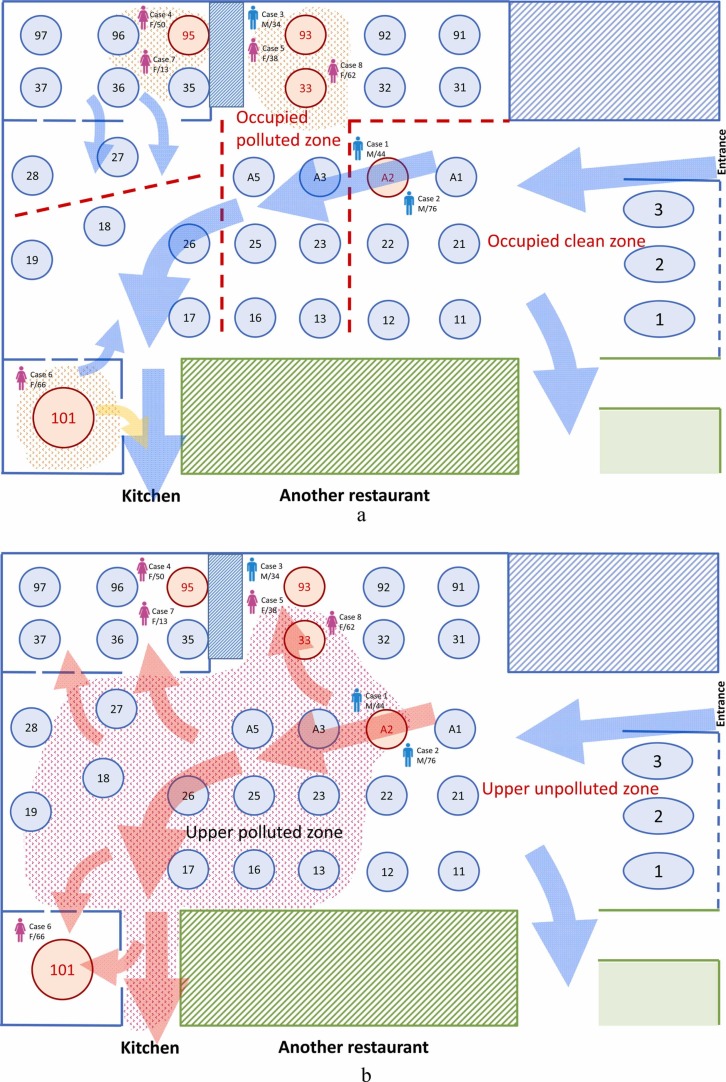
A 44-year-old male air crew was suspected to have breached the home quarantine requirement after returning from the United States on 25th December 2021. He had lunch at a restaurant R2 with his family on 27th December 2021 (13:16–14:54), despite having developed headahce since 26th December 2021. He was subsequently confirmed to have SARS-CoV-2 Omicron variant infection by regular compulsory testing at community testing center per protocol in the evening of 27th December 2021 with a cycle threshold (Ct) value of 21 (case 1, index case). Based on the dining table reservation book, credit card payment record, and closed-circuit television (CCTV) of R2, a total of 207 persons who had lunch at the restaurant were exposed to the index case between 13:00–15:00, 27th December 2021. They, together with 22 staff serving at R2, were sent to quarantine camp for observation. Review of CCTV footage showed that the index case did not leave his seat during the entire duration of lunch.
This restaurant-related outbreak, designated Outbreak R2, involved 7 secondary cases of Omicron variant, who were diagnosed during the quarantine period ( Table 1). The median age was 50 years (range: 13–76 years). Five of them (71.4%) had symptomatic infection with the median onset 5 days after exposure (range: 3–7 days after exposure). All of them had completed 2 doses of COVID-19 vaccine at a median of 164 days prior to exposure (range: 129–238 days). All secondary cases involved customers who did not wear masks while staying in the dining area of R2, resulting in a secondary attack rate of 3.4% (7/207) among the customers ( Table 2).
Table 1.
Epidemiological information of cases of SARS-CoV-2 Omicron variant transmission in restaurant R2.a
| Case | Date of report [symptom onset] | Sex/age | Exposure with index | Incubation periodb | COVID-19 vaccination | Date of 1st [2nd dose] of vaccine | Remark |
|---|---|---|---|---|---|---|---|
| 1 (index)c | 27th Dec 2021 [26th Dec 2021] | M/44 | NA | NA | Comirnaty | 29th May 2021 [19th Jun 2021] | Air crew member; attended R2 (Table A2) on 27th Dec 2021 (13:16–14:54) |
| 2c | 31st Dec 2021 [asymptomatic] | M/76 | 98 min | NA | Comirnaty | 7th Jul 2021 [28th Jul 2021] | Father of case 1; only exposed in R2 (Table A2) on 27th Dec 2021 (13:16–14:54) |
| 3c | 31st Dec 2021 [asymptomatic] | M/34 | 32 min | NA | Comirnaty | 13th Jun 2021 [4th Jul 2021] | Construction site worker; attended R2 (Table 93) on 27th Dec 2021 (14:22–15:50) |
| 4d | 2nd Jan 2022 [30th Dec 2021] | F/50 | 98 min | 3 days | Comirnaty | 24th May 2021 [14th Jun 2021] | Housewife; attended R2 (Table 95) on 27th Dec 2021 (12:42–15:00) |
| 5c | 3rd Jan 2022 [1st Jan 2022] | F/38 | 32 min | 5 days | Comirnaty | 19th Jun 2021 [16th Jul 2021] | Wife of case 3; attended R2 (Table 93) on 27th Dec 2021 (14:22–15:50) |
| 6d | 4th Jan 2022 [2nd Jan 2022] | F/66 | 19 min | 6 days | CoronaVac | 16th Jul 2021 [13th Aug 2021] | Housewife; attended R2 (Table 101) on 27th Dec 2021 (12:25–13:35) |
| 7e | 5th Jan 2022 [3rd Jan 2022] | F/13 | 98 min | 7 daysf | Comirnaty | 29th Jul 2021 [20th Aug 2021] | Daughter of case 4; attended R2 (Table 95) on 27th Dec 2021 (12:42–15:00) |
| 8g | 6th Jan 2022 [30th Dec 2021] | F/62 | 34 min | 3 days | Comirnaty | 12th Apr 2021 [3rd May 2021] | Housewife; attended R2 (Table 33) on 27th Dec 2022 (12:29–13:50) |
Note. COVID-19, coronavirus disease 2019; NA, not applicable; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; US, the United States.
Index case and all secondary cases were Hong Kong resident.
Counting from the date of contact with the index case in R2 for symptomatic cases.
Whole genome sequencing showed the identical sequence.
Whole genome sequencing showed that there was one additional mutation (A19950G) to the index case.
Whole genome sequencing showed that there were two additional mutations (C12459T and A19950G) to the index case.
Given the long incubation period and two additional mutations in nucleotide sequence, case 7 likely acquired COVID-19 from case 4, instead of acquiring the infection from the index case.
Whole genome sequencing showed that there was one additional mutation (G3947A) to the index case.
Table 2.
Comparison of secondary attack rate during COVID-19 outbreaks in two Chinese restaurants before and after enhancement of indoor air dilution.
| Outbreak R1 | Outbreak R2 | P value | |
|---|---|---|---|
| Customers | |||
| Number of exposed | 76 | 207 | |
| Number of secondary infected | 22 | 7a | |
| Secondary attack rate | 28.9% | 3.4% | P<0.001 |
| Restaurant staff | |||
| Number of exposed | 19 | 22 | |
| Number of secondary infected | 10 | 0 | |
| Secondary attack rate | 52.6% | 0% | P<0.001 |
| Secondary attack rate (overall) | 33.7% | 2.6% | P<0.001 |
Note. Outbreak R1 occurred on 19th February 2021 (before enhancement of indoor air dilution). Outbreak R2 occurred on 27th December 2021 (after enhancement of indoor air dilution).
Excluding the index case (case 1), there were 7 secondary infected cases in this outbreak.
Restaurant R2 (245 m2, 0.84 customer per m2) was connected to an adjoining restaurant R3 (70 m2) through a doorway in the middle, but had separate entrance and kitchen. The primary air handling unit (PAU) was located at R3, and fresh air is distributed through the doorway to R2. The PAU rate capacity was 5400 m3/hour, and the designated ACH for the whole premises was equivalent to 5.7. An ACH of 2.0 was recorded in the seating area of R2 during on-site measurement of the outdoor air supply in air ducts on 30th December 2021.
To comply with the legal requirement stipulated above, ultraviolet-C air purifier system had been installed in R2 (Guide on Compliance 2022). A total of 14 ultraviolet-C air purifiers were installed at the ceiling level of the restaurant (ranging from 3.4 to 4.1 m above ground level), all near the return air grille of the fan coil unit. All air purifiers were under normal operation on 27th December 2021, when the index case visited the restaurant. During on-site visit, specific advice was given to improve air balancing and augment distribution of fresh air supply to R2. The post-adjustment ACH was 4.6 in the seating area. Smoke test was conducted on 4th January 2022, which demonstrated dominant flow from entrance to kitchen across the seating area. Smoke test also showed inward flow and leakage of smoke through crevices into VIP rooms ( Fig. 3a & 3b). The position of the table of index case and the tables of the secondary cases was also shown in Fig. 3a & 3b. The vertical airflow in R2 was illustrated in Fig. 4.
Fig. 3.
a & b. Floor plan of the restaurant R2 with outbreak of SARS-CoV-2 Omicron variant. Note of Fig. 3a. Tables where customers who are infected sat in are marked in red. The red dotted line indicated that the restaurant was divided into 4 different zones and a designated team of staff was assigned to serve each zone. Table 35, 36, 37, 95, 96, 97 were located in a VIP room, while Table 101 was located in another VIP room. The arrow in blue indicated the direction of airflow from the entrance to the kitchen as demonstrated by smoke test in the air layer occupied by the customers. The blue dotted line indicates the crevices present in the partitions between the VIP rooms and the main area of the restaurant. The same crevices exist in the partitions separating the main area and the exterior of the restaurant. Note of Fig. 3b. The direction of airflow in the upper air layer is illustrated. The arrow in blue indicates the direction of clean air (upper unpolluted zone) from the entrance. The arrow in red indicated the direction of contaminated air at the upper polluted zone after passing through the index case in Table A2.
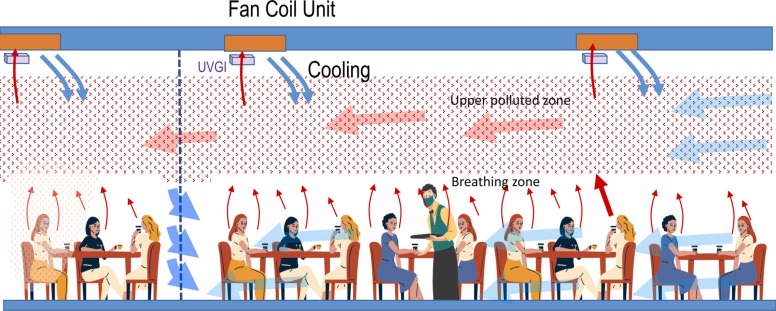
Fig. 4.
Schematic representation of vertical airflow in the restaurant R2 with outbreak of Omicron variant. Note. The upper partial layer which was polluted by the rising exhaled air stream assisted by rising plumes of body and even warm food. The cool clean air generated from the fan coil units with upper-room ultraviolet-C germicidal irradiation (UVGI), and also mainly from entrance. For the corner or the two VIP rooms (illustrated by the blue dotted line), if their temperature was lower than the main area, there would be a bi-directional flow with upper inflow and lower outflow. This would explain why the air polluted by the index case would “jump” to the “distant” corner or VIP rooms, and somehow bypass the tables in the main area.
Outbreak R1 occurred on 19th February 2021 involving a different restaurant R1. The outbreak was located at the ground level of R1 (138 m2, 0.55 customer per m2). All the affected cases, with the median age of 54 years (range: 33–74 years), dinned on the ground floor where the ACH measured onsite was 1.2. There was no air purifier installed in R1. All customers and restaurant staff were not vaccinated and were subsequently quarantined according to the prevailing public health measures. The secondary attack rates among customers and restaurant staff were 28.9% (22/76) and 52.6% (10/19), respectively, during the quarantine period.
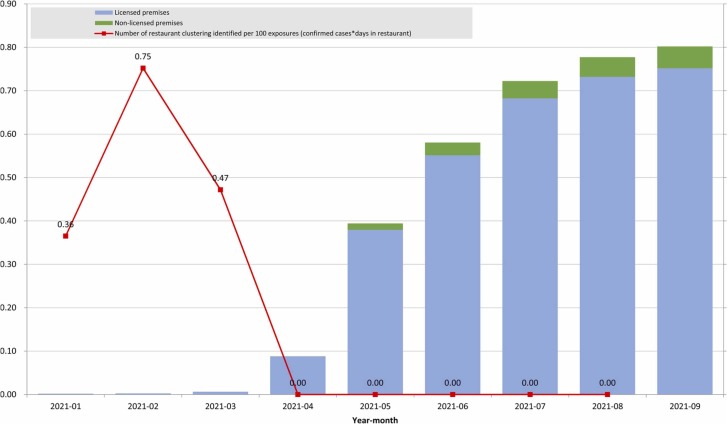
The improvement in indoor air dilution with installation of air purifiers and upper-room ultraviolet-C germicidal irradiation significantly decreased the secondary attack rate during COVID-19 outbreak among customers in these two Chinese restaurants (Table 2). The number of restaurant clustering per 100 episodes of exposure by COVID-19 patients was inversely related to the number of air purifiers being installed in the restaurants ( Fig. 5).
Fig. 5.
The relationship between COVID-19 outbreaks and installation of air purifiers in the restaurants.
3.3. Estimation of quanta generation
Given the aerosol deposition rate (0.30 h−1), virus deactivation rate (0.63 h− 1), and the pulmonary flow rate per susceptible person (0.15 L/s), the quanta generation rate was estimated in R2 and R1. In R2, the virus-free air was 2530.2 L/s. Among 207 customers, 7 infected secondary cases were exposed with a median duration of 0.57 h. The estimated quanta generation rate was 1023.4 quanta per h in R2. In R1, the virus-free air was 232.5 L/s. Among 76 customers, 22 infected secondary cases were exposed with a median duration of 0.95 h. The estimated quanta generation rate was 557.7 quanta per h in R1.
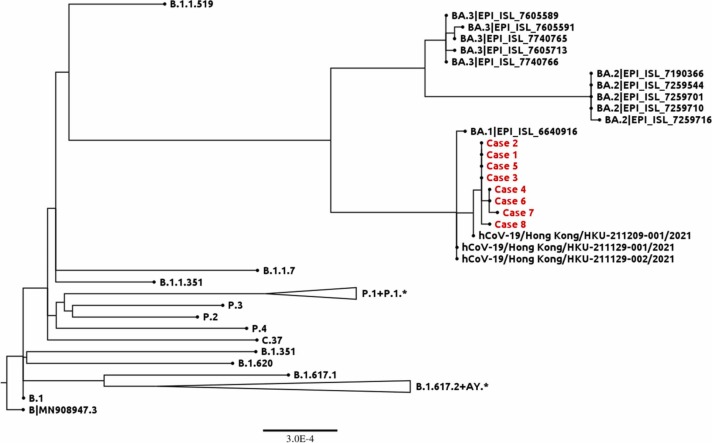
3.4. Whole genome sequencing and phylogenetic analysis
Whole genome sequencing was performed for the 8 cases in Outbreak R2 ( Fig. 6). Phylogenetic tree showed that they clustered together. Four cases had identical sequence (case 1 - index case, case 2, case 3, and case 5). For cases 4 and 6, one additional mutation (A19950G) was found. Another mutation (G3947A) was found in case 8. And two additional mutations (C12459T and A19950G) were found in case 7. Phylogenetic analysis of the infected cases in Outbreak R1 also showed clustering suggestive of transmission in R1 (Supplementary Figure).
Fig. 6.
Phylogenetic analysis of the SARS-CoV-2 Omicron variant strains in the COVID-19 outbreak in a Chinese restaurant R2 in Hong Kong. The tree was rooted on the reference genome NCBI accession number MN_908947.3. The R2 outbreak cases are highlighted in red.
4. Discussion
With the evolution of COVID-19 pandemic, there has been increasing evidence of airborne transmission of SARS-CoV-2 (Dinoi et al., 2022), especially in poorly ventilated indoor areas (Tang et al., 2021; Morawska et al., 2020; Conte et al., 2021). Dining places and bars are considered as the high-risk area for COVID-19 outbreaks as people may interact closely without wearing masks (Li et al., 2021a; Zhang et al., 2021; Chau et al., 2021). In fact, social gathering with mask-off activities has been shown to increase the risk of SARS-CoV-2 transmission during the early phase of COVID-19 pandemic (Cheng et al., 2020a). In Hong Kong, the first community outbreak of COVID-19 with superspreading event was attributed to the family gathering and dining in a commercial party room (Lam et al., 2020). During the subsequent waves of COVID-19, there had been at least 12 restaurant-related COVID-19 outbreaks, involving an average of 23 infected cases per each outbreak (unpublished data) before the report of outbreak R1 in February 2021.
Poor ventilation and insufficient dilution of indoor air increase the risk of short-range and even long-range airborne transmission of respiratory viruses including SARS-CoV-2. Based on the analysis using a macroscopic aerosol balance model, a ventilation rate of 10 L/s per person provided a similar concentration and distance decay profile to that in outdoor settings (Li et al., 2021b). In the restaurant-related COVID-19 outbreak with probable long-range airborne transmission, the measured ventilation rate was only 0.9 L/s per person (Li et al., 2021a). Similarly, insufficient ventilation has been associated with long-range airborne transmission of SARS-CoV-2 on two buses where the time-averaged ventilation rates were approximately 1.7 and 3.2 L/s per person, respectively (Ou et al., 2022). Given these findings, the Hong Kong Government stipulated on infection control grounds a requirement on the standard of air change or the use of air purifiers in indoor seating areas of dine-in catering premises in March 2021 (Air change 2022). It provides an opportunity for us to investigate the effect of enhancement of indoor air dilution on the extent of COVID-19 transmission by measuring the secondary attack rate before and after its implementation.
Before the implementation of enhanced indoor air dilution, the overall secondary attack rate of COVID-19 in Outbreak R1 (33.4%) was two times higher than that among household contacts (Fung et al., 2021). The postulation of airborne transmission of SARS-CoV-2 inside restaurant R1 may not fully explain the unusually high secondary attack rate among the staff members as they were supposed to wear masks all the time at work, which has already been shown to minimize the transmission of respiratory viruses in hospital settings (Cheng et al., 2010; Wong et al., 2021b). The possibility of SARS-CoV-2 acquisition during off-work social gatherings may not be completely excluded. Therefore, we analyzed and compared the secondary attack rate of COVID-19 among the customers, where there were fewer confounding factors.
After the enhancement of indoor air dilution in the restaurants, the secondary attack rate of COVID-19 was significantly lower in Outbreak R2 than that in Outbreak R1. On-site investigation demonstrated a strong air current from entrance to kitchen that may carry the virus-laden aerosol exhaled from the index case to other parts of the restaurant. In addition, increased indoor air dilution can theorectically reduce air stagnation and minimize the risk of short-range airborne transmission of SARS-CoV-2. Therefore, except for the secondary case who sat at the same table with the index case within a distance of less than 1 m, those sitting at the adjoining table were not infected. However, it appears unusual to have 6 more secondary cases who sat in the corners of the restaurant some distance away from the table of index case. In fact, three of 6 secondary cases stayed in 2 different VIP rooms, where air can pass through the crevices into VIP rooms. It is postulated that local stagnation of air in the corners, inadequate fresh air intake, and insufficient air mixing may result in recirculation of contaminated air without adequate air exchange in corner areas. Since the ultraviolet-C air purifiers were located at a relatively high level, their efficacy may be compromised at locations with poor air mixing, such as in the corners of the restaurant. Moreover, ultraviolet-C air purifier can only reduce, but not completely eliminate the risk of COVID-19 transmission by virus-laden aerosols.
Transmission of SARS-CoV-2 by indirect contact with fomites or by droplet route may also be possible in R2. During our on-site investigation, the practice of infection control and other preventive measures in R2 were found to be satisfactory upon interviewing their staff and reviewing the CCTV footage. To reduce the risk of contamination, the restaurant was divided into 4 zones and a designated team of staff was assigned to serve each zone. Except for case 2 who sat at the same table with index case, the remaining secondary cases were located outside the zone of index case and distributed in 3 different zones. The likelihood of contact or droplet transmission of SARS-CoV-2 was low in this setting.
Whole genome sequencing of the SARS-CoV-2 strains revealed identical nucleotide sequence in 4 patients, including the index case, and one additional nucleotide difference in 3 patients. Presumably, these cases were phylogenetically related. Despite harboring two nucleotide differences compared with the index case, the strain from case 7 shared one nucleotide mutation with case 4, who sat at the same table (Table 95) inside one of the VIP rooms. Based on the phylogenetic analysis, case 7 likely acquired COVID-19 from case 4, instead of acquiring the infection from the index case during the stay in R2. This was corroborated by the fact that the symptom onset of case 7 was 4 days later than the symptom onset of case 4. Here, genomic analysis provided additional information to enrich the epidemiological investigation. Nevertheless, we included case 7 in the calculation of secondary attack rate in Outbreak R2, where whole genome sequencing demonstrated phylogenetic clustering suggestive of a point source outbreak.
Airborne transmission of SARS-CoV-2 becomes a great concern, especially with the spread of the Omicron variant which demonstrated a higher basic reproduction number (Ito et al., 2021). Our serial air sampling conducted in airborne infection isolation facilitates designated for COVID-19 patients have eventually demonstrated the presence of viral RNA in the air samples (Cheng et al. 2020c, 2020b; Wong et al., 2021a). Airborne transmission with superspreading phenomenon has also been observed in a medical ward with 6 ACH (Cheng et al., 2021b), posing a new challenge to our infection control and prevention strategies in the hospitals (Cheng et al., 2021c). Therefore, it is virtually impossible to completely eliminate SARS-CoV-2 transmission in restaurants. The enhancement of indoor air dilution is aimed at reducing the risk of transmission, as evidenced by our comparison of secondary attack rates between two restaurant-related COVID-19 outbreaks. However, restaurants, especially those with high sitting density and poor ventilation, remain a high-risk area for SARS-CoV-2, including but not limit to the Omicron variant. In outbreaks R2 and R1, the estimated quanta generation rate was 1023.4 h−1 and 557.7 h−1, respectively, which were much higher than the estimated quanta generation rate of 79.3 h−1 in a restaurant outbreak reported in the literature, and the rates of 35.0 h−1 and 58.3 h−1 in two bus-related outbreaks in early 2020 (Li et al., 2021a; Ou et al., 2022). Although the quanta generation rate for the Omicron variant in R2 was 83.5% higher than that for the non-Omicron variant in R1, the secondary attack rate was much lower in R2 (3.4%) than in R1 (28.9%), suggesting that enhancement of indoor air dilution can reduce SARS-CoV-2 transmission.
While the catering premises are complying with the requirement on indoor air dilution enhancement, it is more important to educate the public not to visit restaurants if they have respiratory symptoms suggestive of COVID-19. It has been shown that completion of two or three doses COVID-19 vaccination does not offer complete protection against infection by the Omicron variant. Further upgrade of heating and ventilation systems to reduce infection risk requires extra costs, especially regarding the materials and energy consumption (Risbeck et al., 2021). In the modern heating, ventilation, and air conditioning systems, increasing ventilation can be overly costly with limited benefit since indoor air must be maintained at a given temperature and humidity, while improving filtration may deliver more benefit with less cost.
There are several limitations in this study. First, we are not able to compare the secondary attack rates of all restaurant-related COVID-19 outbreaks in Hong Kong. Due to the evolving contact tracing practice through the COVID-19 pandemic, not all exposed persons in the restaurants were quarantined in the initial phase making a comprehensive assessment of their epidemiological features and secondary attack rates impossible. Second, the epidemiological background of the two outbreaks in R1 and R2 may be heterogeneous in terms of the area occupied per customer, vaccination rate among the secondary cases, and more importantly, the difference in SARS-CoV-2 variants. All the secondary cases in Outbreak R1 were not vaccinated because the COVID-19 vaccination program was launched on 26th February 2021 (7 days after the onset of Outbreak R1). On the other hand, all the secondary cases in Outbreak R2 were fully vaccinated, despite a lower neutralizing antibody response against the Omicron variant among the vaccine recipients (Lu et al., 2021). Third, it was not possible for us to perform an aerodynamic study in detail because the fresh air supply was augmented soon after the outbreak. However, the direction of airflow demonstrated by smoke test provided valuable information to support our epidemiological investigation. Although a definite causal effect of the improvement in indoor air dilution on reducing COVID-19 transmission was not established, the relationship between indoor air dilution and risk of SARS-CoV-2 transmission warrants further investigation (Bazant and Bush 2021).
Funding
This study was partially supported by the Health and Medical Research Fund (HMRF) Commissioned Research on Control of Infectious Disease (Phase IV), CID-HKU1–2 and CID-HKU1–16, Food and Health Bureau, Hong Kong SAR Government.
CRediT authorship contribution statement
VC-CC, DCL, S-CW, and K-YY had roles in study design, data analysis, literature search, and writing up of the manuscript. VC-CC, DCL, S-CW, AK-WA, CH, SKC, and K-YY had roles in outbreak investigation. DCL, HT, KH-LN and KK-WT had roles in whole genome sequencing and phylogenetic analysis. AW-HC, JDI, WMC, HWT had roles in laboratory work. QW and YL had roles in the analysis of ventilation from the perspective of mechanical engineering. AK-WA, LX, and MY-WK had roles in collection of patient specimens. All authors reviewed and approved the final version of the manuscript.
Environmental implication
In view of the increased airborne transmissibility of Omicron variant, it would be difficult to prevent the SARS-CoV-2 transmission in the indoor areas, especially in the restaurants, which should be regarded as the high-risk area where people take off the masks during dining. Our study demonstrated that the risk of SARS-CoV-2 transmission could be significantly reduced in the restaurant, even for Omicron variant, after the enhancement of indoor air dilution through ventilation and installation of air purifiers.
Declaration of Competing Interest
All authors declare no conflict of interest.
Acknowledgement
We thank our frontline staff and management team of Centre for Health Protection, Department of Health, and Hospital Authority to facilitate this study. We thank staff and management team of Food and Environmental Hygiene Department, and Electrical and Mechanical Services Department of Hong Kong Special Administrative Region, China, for the participation in the outbreak investigations. We also thank the members of the Working Group on Implementing the Requirement on Air Change or Air Purifier in Dine-in Restaurants.
Editor: Danmeng Shuai
Footnotes
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.jhazmat.2022.128504.
Appendix A. Supplementary material
Supplementary material
.
Data sharing
Data are available upon reasonable request. The genome sequences of the eight cases have been deposited into GISAID. The accession number and GISAID virus name are EPI_ISL_8744063 and hCoV-19/Hong Kong/HKU-220114–001/2021, respectively, for the case 1 (index case). The corresponding accession numbers and GISAID virus names for case 2 to 8 are as follows: EPI_ISL_8744064 and hCoV-19/Hong Kong/HKU-220114–002/2022 (case 2); EPI_ISL_8744065 and hCoV-19/Hong Kong/HKU-220114–003/2021 (case 3); EPI_ISL_8744066 and hCoV-19/Hong Kong/HKU-220114–004/2022 (case 4); EPI_ISL_8744067 and hCoV-19/Hong Kong/HKU-220114–005/2022 (case 5); EPI_ISL_8744068 and hCoV-19/Hong Kong/HKU-220114–006/2022 (case 6); EPI_ISL_8744069 and hCoV-19/Hong Kong/HKU-220114–007/2022 (case 7); and EPI_ISL_8744070 and hCoV-19/Hong Kong/HKU-220114–008/2022 (case 8).
References
- Abdullah F., Myers J., Basu D., Tintinger G., Ueckermann V., Mathebula M., et al. Decreased severity of disease during the first global omicron variant covid-19 outbreak in a large hospital in tshwane, south africa. Int. J. Infect. Dis. 2021 doi: 10.1016/j.ijid.2021.12.357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Air change / Installation of Air Purifier in Catering Premises. Food and Environmental Hygiene Department. The Government of Hong Kong Special Administrative Region. 〈https://www.fehd.gov.hk/english/licensing/guide_general_reference/report_air-changes_purification.html〉. Accessed on 8th January 2022.
- Bazant M.Z., Bush J.W.M. A guideline to limit indoor airborne transmission of COVID-19. Proc. Natl. Acad. Sci. USA. 2021;118(17) doi: 10.1073/pnas.2018995118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan W.M., Ip J.D., Chu A.W., Tse H., Tam A.R., Li X., et al. Phylogenomic analysis of COVID-19 summer and winter outbreaks in Hong Kong: an observational study. Lancet Reg. Health West. Pac. 2021;10 doi: 10.1016/j.lanwpc.2021.100130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chau N.V.V., Hong N.T.T., Ngoc N.M., Thanh T.T., Khanh P.N.Q., Nguyet L.A. OUCRU COVID-19 research group1. Superspreading event of SARS-CoV-2 Infection at a bar, ho chi minh city, Vietnam. Emerg. Infect. Dis. 2021;27(1):310–314. doi: 10.3201/eid2701.203480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng V.C., Tai J.W., Wong L.M., Chan J.F., Li I.W., To K.K. Prevention of nosocomial transmission of swine-origin pandemic influenza virus A/H1N1 by infection control bundle. J. Hosp. Infect. 2010;74(3):271–277. doi: 10.1016/j.jhin.2009.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng V.C., Wong S.C., Chuang V.W., So S.Y., Chen J.H., Sridhar S. The role of community-wide wearing of face mask for control of coronavirus disease 2019 (COVID-19) epidemic due to SARS-CoV-2. J. Infect. 2020;81(1):107–114. doi: 10.1016/j.jinf.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng V.C., Wong S.C., Chan V.W., So S.Y., Chen J.H., Yip C.C. Air and environmental sampling for SARS-CoV-2 around hospitalized patients with coronavirus disease 2019 (COVID-19) Infect. Control Hosp. Epidemiol. 2020;41(11):1258–1265. doi: 10.1017/ice.2020.282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng V.C.C., Wong S.C., Chen J.H.K., Yip C.C.Y., Chuang V.W.M., Tsang O.T.Y., et al. Escalating infection control response to the rapidly evolving epidemiology of the coronavirus disease 2019 (COVID-19) due to SARS-CoV-2 in Hong Kong. Infect. Control Hosp. Epidemiol. 2020;41(5):493–498. doi: 10.1017/ice.2020.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng V.C., Siu G.K., Wong S.C., Au A.K., Ng C.S., Chen H., et al. Complementation of contact tracing by mass testing for successful containment of beta COVID-19 variant (SARS-CoV-2 VOC B.1.351) epidemic in Hong Kong. Lancet Reg. Health West. Pac. 2021;17 doi: 10.1016/j.lanwpc.2021.100281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng V.C., Fung K.S., Siu G.K., Wong S.C., Cheng L.S., Wong M.S., et al. Nosocomial outbreak of coronavirus disease 2019 by possible airborne transmission leading to a superspreading event. Clin. Infect. Dis. 2021;73(6):e1356–e1364. doi: 10.1093/cid/ciab313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng V.C., Wong S.C., Tong D.W., Chuang V.W., Chen J.H., Lee L.L., et al. Multipronged infection control strategy to achieve zero nosocomial coronavirus disease 2019 (COVID-19) cases among Hong Kong healthcare workers in the first 300 days of the pandemic. Infect. Control Hosp. Epidemiol. 2021;19:1–10. doi: 10.1017/ice.2021.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Classification of Omicron (B.1.1.529): SARS-CoV-2 Variant of Concern. World Health Organization (published 26th November 2021). Available at 〈https://www.who.int/news/item/26-11-2021-classification-of-omicron-(b.1.1.529)-sars-cov-2-variant-of-concern〉. Accessed on 5th January 2022.
- Conte M., Feltracco M., Chirizzi D., Trabucco S., Dinoi A., Gregoris E., et al. Airborne concentrations of SARS-CoV-2 in indoor community environments in Italy. Environ. Sci. Pollut. Res. Int. 2021:1–12. doi: 10.1007/s11356-021-16737-7. Oct 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- COVID-19 Thematic Website. Centre for Health Protection. Department of Health. The Government of the Hong Kong Special Administrative Region. Available at 〈https://www.coronavirus.gov.hk/eng/index.html〉. Accessed on 5th January 2022.
- Dinoi A., Feltracco M., Chirizzi D., Trabucco S., Conte M., Gregoris E., et al. A review on measurements of SARS-CoV-2 genetic material in air in outdoor and indoor environments: implication for airborne transmission. Sci. Total Environ. 2022;809 doi: 10.1016/j.scitotenv.2021.151137. Feb 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Final Report on Compliance with the Requirement on Air Change or Air Purifiers in Seating Areas of Dine-in Catering Premises under Cap. 599F. Food and Environmental Hygiene Department. The Government of Hong Kong Special Administrative Region. 〈https://www.fehd.gov.hk/english/licensing/guide_general_reference/air-changes_report2021.pdf〉. Accessed on 8th January 2022.
- Fung H.F., Martinez L., Alarid-Escudero F., Salomon J.A., Studdert D.M., Andrews J.R., et al. Stanford-CIDE coronavirus simulation model (SC-COSMO) modeling group. the household secondary attack rate of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): a rapid review. Clin. Infect. Dis. 2021;73(Suppl 2):S138–S145. doi: 10.1093/cid/ciaa1558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guide on Compliance with Requirement on Air Change / Air Purifiers in Seating Areas of Dine-in Catering Premises. Food and Environmental Hygiene Department. The Government of Hong Kong Special Administrative Region. https://www.fehd.gov.hk/english/licensing/guide_general_reference/guide_on_compliance_with_requirement_on_air_change.html. Accessed on 8th January 2022.
- Ito K., Piantham C., Nishiura H. Relative instantaneous reproduction number of Omicron SARS-CoV-2 variant with respect to the Delta variant in Denmark. J. Med. Virol. 2021 doi: 10.1002/jmv.27560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katoh K., Standley D.M. MAFFT multiple sequence alignment software version 7: improvements in performance and usability. Mol. Biol. Evol. 2013;30(4):772–780. doi: 10.1093/molbev/mst010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lam H.Y., Lam T.S., Wong C.H., Lam W.H., Mei E.L.C., Kuen Y.L.C. A superspreading event involving a cluster of 14 coronavirus disease 2019 (COVID-19) infections from a family gathering in Hong Kong Special Administrative Region SAR (China) West. Pac. Surveill. Response J. 2020;11(4):36–40. doi: 10.5365/wpsar.2020.11.1.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X., Lester D., Rosengarten G., Aboltins C., Patel M., Cole I. A spatiotemporally resolved infection risk model for airborne transmission of COVID-19 variants in indoor spaces. Sci. Total Environ. 2021;812 doi: 10.1016/j.scitotenv.2021.152592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y., Qian H., Hang J., Chen X., Cheng P., Ling H. Probable airborne transmission of SARS-CoV-2 in a poorly ventilated restaurant. Build. Environ. 2021;196 doi: 10.1016/j.buildenv.2021.107788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y., Cheng P., Jia W. Poor ventilation worsens short-range airborne transmission of respiratory infection. Indoor Air. 2021:12946. doi: 10.1111/ina.12946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loman N., Rambaut A. nCoV-2019 novel coronavirus bioinformatics protocol. 2020. Available at 〈https://artic.network/ncov-2019/ncov2019-bioinformatics-sop.html〉. Accessed 5th January 2022.
- Lu L., Mok B.W., Chen L.L., Chan J.M., Tsang O.T., Lam B.H. Neutralization of SARS-CoV-2 Omicron variant by sera from BNT162b2 or Coronavac vaccine recipients. Clin. Infect. Dis. 2021 doi: 10.1093/cid/ciab1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller S.L., Nazaroff W.W., Jimenez J.L., Boerstra A., Buonanno G., Dancer S.J., et al. Transmission of SARS-CoV-2 by inhalation of respiratory aerosol in the skagit valley chorale superspreading event. Indoor Air. 2021;31(2):314–323. doi: 10.1111/ina.12751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morawska L., Tang J.W., Bahnfleth W., Bluyssen P.M., Boerstra A., Buonanno G. How can airborne transmission of COVID-19 indoors be minimised? Environ. Int. 2020;142 doi: 10.1016/j.envint.2020.105832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen L.T., Schmidt H.A., von Haeseler A., Minh B.Q. IQ-TREE: a fast and effective stochastic algorithm for estimating maximum-likelihood phylogenies. Mol. Biol. Evol. 2015;32(1):268–274. doi: 10.1093/molbev/msu300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ou C., Hu S., Luo K., Yang H., Hang J., Cheng P. Insufficient ventilation led to a probable long-range airborne transmission of SARS-CoV-2 on two buses. Build. Environ. 2022;207 doi: 10.1016/j.buildenv.2021.108414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riley E.C., Murphy G., Riley R.L. Airborne spread of measles in a suburban elementary school. Am. J. Epidemiol. 1978;107(5):421–432. doi: 10.1093/oxfordjournals.aje.a112560. [DOI] [PubMed] [Google Scholar]
- Risbeck M.J., Bazant M.Z., Jiang Z., Lee Y.M., Drees K.H., Douglas J.D. Modeling and multiobjective optimization of indoor airborne disease transmission risk and associated energy consumption for building HVAC systems. Energy Build. 2021;253 doi: 10.1016/j.enbuild.2021.111497. Dec 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang J.W., Bahnfleth W.P., Bluyssen P.M., Buonanno G., Jimenez J.L., Kurnitski J. Dismantling myths on the airborne transmission of severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) J. Hosp. Infect. 2021;110:89–96. doi: 10.1016/j.jhin.2020.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Centre for Health Protection closely monitors cluster of pneumonia cases on Mainland. Press release of the Department of Health, Hong Kong Special Administrative Region. Available at 〈https://www.info.gov.hk/gia/general/201912/31/P2019123100667.htm〉. Accessed on 5th January 2022.
- To K.K., Tsang O.T., Leung W.S., Tam A.R., Wu T.C., Lung D.C. Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS-CoV-2: an observational cohort study. Lancet Infect. Dis. 2020;20(5):565–574. doi: 10.1016/S1473-3099(20)30196-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weekly epidemiological update on COVID-19 - 28 December 2021. World Health Organization. Available at https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---28-december-2021. Accessed on 5th January 2022.
- Wong S.C., Leung M., Lee L.L., Chung K.L., Cheng V.C. Infection control challenge in setting up a temporary test centre at Hong Kong international airport for rapid diagnosis of COVID-19 due to SARS-CoV-2. J. Hosp. Infect. 2020;105(3):571–573. doi: 10.1016/j.jhin.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong S.C., Yuen L.L., Chan V.W., Chen J.H., To K.K., Yuen K.Y., et al. Airborne transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): what is the implication of hospital infection control? Infect. Control Hosp. Epidemiol. 2021:1–2. doi: 10.1017/ice.2021.318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong S.C., Lam G.K., AuYeung C.H., Chan V.W., Wong N.L., So S.Y. Absence of nosocomial influenza and respiratory syncytial virus infection in the coronavirus disease 2019 (COVID-19) era: implication of universal masking in hospitals. Infect. Control Hosp. Epidemiol. 2021;42(2):218–221. doi: 10.1017/ice.2020.425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong S.C., Au A.K., Chen H., Yuen L.L., Li X., Lung D.C., et al. Transmission of Omicron (B.1.1.529) - SARS-CoV-2 Variant of Concern in a designated quarantine hotel for travelers: a challenge of elimination strategy of COVID-19. Lancet Reg. Health West. Pac. 2021 doi: 10.1016/j.lanwpc.2021.100360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong S.C., Leung M., Tong D.W., Lee L.L., Leung W.L., Chan F.W. Infection control challenges in setting up community isolation and treatment facilities for patients with coronavirus disease 2019 (COVID-19): implementation of directly observed environmental disinfection. Infect. Control Hosp. Epidemiol. 2021;42(9):1037–1045. doi: 10.1017/ice.2020.1355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong S.C., Chen H., Lung D.C., Ho P.L., Yuen K.Y., Cheng V.C. To prevent SARS-CoV-2 transmission in designated quarantine hotel for travelers: is the ventilation system a concern? Indoor Air. 2021;31(5):1295–1297. doi: 10.1111/ina.12870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang N., Chen X., Jia W., Jin T., Xiao S., Chen W., et al. Evidence for lack of transmission by close contact and surface touch in a restaurant outbreak of COVID-19. J. Infect. 2021;83(2):207–216. doi: 10.1016/j.jinf.2021.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao H., Lu L., Peng Z., Chen L.L., Meng X., Zhang C., et al. SARS-CoV-2 Omicron variant shows less efficient replication and fusion activity when compared with delta variant in TMPRSS2-expressed cells. Emerg. Microbes Infect. 2021:1–18. doi: 10.1080/22221751.2021.2023329. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material
Data Availability Statement
Data are available upon reasonable request. The genome sequences of the eight cases have been deposited into GISAID. The accession number and GISAID virus name are EPI_ISL_8744063 and hCoV-19/Hong Kong/HKU-220114–001/2021, respectively, for the case 1 (index case). The corresponding accession numbers and GISAID virus names for case 2 to 8 are as follows: EPI_ISL_8744064 and hCoV-19/Hong Kong/HKU-220114–002/2022 (case 2); EPI_ISL_8744065 and hCoV-19/Hong Kong/HKU-220114–003/2021 (case 3); EPI_ISL_8744066 and hCoV-19/Hong Kong/HKU-220114–004/2022 (case 4); EPI_ISL_8744067 and hCoV-19/Hong Kong/HKU-220114–005/2022 (case 5); EPI_ISL_8744068 and hCoV-19/Hong Kong/HKU-220114–006/2022 (case 6); EPI_ISL_8744069 and hCoV-19/Hong Kong/HKU-220114–007/2022 (case 7); and EPI_ISL_8744070 and hCoV-19/Hong Kong/HKU-220114–008/2022 (case 8).