Abstract
Asthma remains a significant health problem in the United States. Adults with poorly controlled asthma can affect their community in a number of ways, from lost productivity in the workplace to health care costs to premature death. Asthma self-management education helps individuals achieve better control of their asthma and is critical for the overall health and well-being of individuals with asthma. While there are numerous programs and initiatives targeting children with asthma, there is a lack of comparable focus on the needs of adults with asthma. The American Lung Association developed Breathe Well, Live Well, an adult asthma self-management education program, and launched it nationwide in 2007. The program for adults has a flexible delivery format for community-based implementation. This article describes the development, dissemination, and transformation of the program. Each stage of implementation showed positive changes in asthma self-management practices that contribute to better asthma control, and one local implementation additionally showed decreased reports of missed work and unscheduled health care visits among participants. The findings from the three evaluations support the use of Breathe Well, Live Well for broad community-based implementation to improve asthma self-management efficacy and behaviors.
Keywords: asthma self-management, community-based asthma education, adults, patient education, self-efficacy
Half of the 19 million adults with asthma in the United States have poorly controlled asthma, and experience frequent and sometimes severe symptoms (U.S. Centers for Disease Control and Prevention [CDC] National Center for Environmental Health, Asthma and Community Health Branch [NCEH], 2018b; Zahran et al., 2015). The mortality rate for asthma in the United States is higher in adults than in children (Akinbami et al., 2012). Asthma has a disparate impact, with minority populations suffering higher morbidity and mortality compared with Whites (Press et al., 2012). The burden of the disease is substantial, accounting for nearly 7.3 million physician office visits, 1.2 million asthma-related emergency department (ED) visits, and more than 100,000 asthma-related hospitalizations per year (CDC NCEH, 2019). Asthma incurs around $82 billion in direct and indirect costs to society annually, including $3 billion in lost work productivity (Nurmagambetov et al., 2018).
Asthma control can be more easily achieved when patients take an active role in self-management and engage effectively with their care providers (O’Conor et al., 2017; National Institutes of Health, National Heart, Lung, & Blood Institute, National Asthma Education and Prevention Program, 2007). Self-management of asthma involves self-monitoring, avoiding asthma triggers, recognizing and responding to asthma symptoms, and adhering to prescribed controller medication (Jones, 2008). However, many adults with asthma are not adherent to treatment; they may not recognize that frequent symptoms and health care use indicate poor asthma control, or that better quality of life can be achieved (O’Conor et al., 2017; Schmier & Leidy, 1998).
Asthma self-management education programs for adults are effective in decreasing asthma symptoms and reducing health care utilization, as well as in producing a positive return on investment and cost savings (CDC NCEH, 2018a; Gibson et al., 2002; Hsu et al., 2016). Such self-management initiatives may cost less when programs are offered through community organizations or by nonphysician staff, such as respiratory therapists, health educators, or community health workers (CHWs; Bryant-Stephens et al., 2009; Clark & Partridge, 2002; Newman et al., 2004). Unfortunately, much of the literature on asthma self-management programs is focused on children: For example, two systematic reviews of asthma education interventions included more studies conducted with children than with adults (Clark et al., 2010; Pinnock et al., 2017). Furthermore, these systematic analyses included randomized controlled trials of interventions developed primarily by single institutions, like university hospitals and health systems; the programs are generally not available for implementation in multiple communities. A nonsystematic compilation of nationally available asthma self-management resources prepared by the CDC’s National Asthma Control Program identified eight ready-to-implement programs for children but only two for adults (CDC NCEH, National Asthma Control Program, 2016). The American Lung Association’s Breathe Well, Live Well (BWLW) was developed to address the need for a flexible, standardized adult asthma education program.
In 2002, the American Lung Association adapted and disseminated a standardized, adult asthma self-management education program for nationwide implementation. This article will present the key elements of that program, along with a history of its implementation at community sites across the United States. We will review both unpublished and published evaluations of the Breathe Well, Live Well program conducted by consultants affiliated with the American Lung Association and by a local health department using it as part of its in-home asthma education program for adults.
APPROACH
Each stage of BWLW’s implementation will be considered in turn, as shown in the timeline in Figure 1. We will first summarize the adaptation from the University of Alabama at Birmingham’s (UAB) Asthma Self-Management Program in 2003, followed by the original BWLW pilot evaluation in 2005 (Kohler, 2006). The Lung Association carried out an iterative process in which the evaluation results and feedback guided updates to the program in the next stage. This led to the changes in the 2007 BWLW dissemination (Hagen, 2008). We will highlight the City of Long Beach Department of Health’s local implementation in 2008, which used BWLW as part of an in-home asthma intervention (Lyde et al., 2013). For each of these iterations, we will share the processes and selected results of the evaluations, with a focus on behavioral outcomes related to the self-management of asthma. Finally, we will describe the transformation into the current picture of BWLW, as well as plans for sustained implementation.
FIGURE 1. BWLW Adaptation and Implementation Timeline.
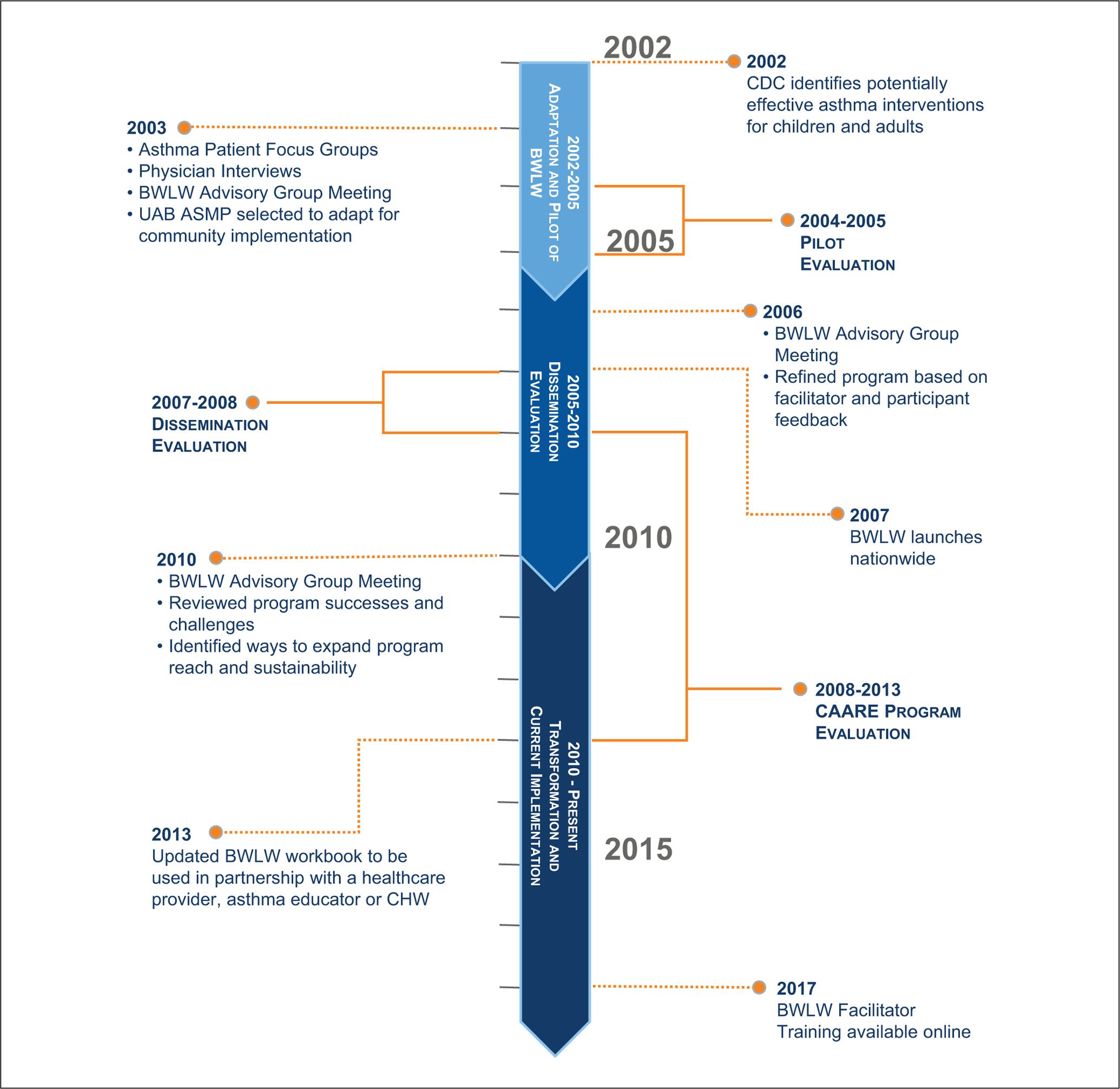
NOTE: ASMP = Asthma Self-management Program; BWLW = Breathe Well, Live Well; CAARE = Community Asthma and Air Quality Resource Education; CDC = Centers for Disease Control and Prevention; CHW = Community Health Worker; UAB = University of Alabama at Birmingham.
DEVELOPMENT OF BREATHE WELL, LIVE WELL: 2002–2005
The CDC NCEH funded the American Lung Association under a 3-year cooperative agreement (U558/CCU222370, 2002–2005). The Lung Association proposed to identify a validated adult asthma management education program from the published literature, adapt it, and pilot it. The project focused on educating adults with asthma in order to reduce morbidity, mortality, and lost productivity, as well as on reducing disparities among populations affected by asthma.
The Lung Association conducted a series of interviews with physicians and a series of asthma patient focus groups from across the United States in July and August 2003 to explore perceived benefits and barriers and the asthma education needs of adults with asthma. In September 2003, the Lung Association convened an Asthma in Adults Advisory Group, selecting 11 members—medical professionals, public health professionals, asthma researchers, and local and national Lung Association staff. The group reviewed the findings of the physician interviews and patient focus groups. They reviewed and ranked 17 validated adult asthma education programs identified as potentially effective by the CDC (CDC NCEH, 2002). They also considered effective adult behavior change and learning strategies needed for the program to be successful. The advisory group selected the UAB Asthma Self-Management Program (ASMP) for adaptation based on its effectiveness in improving asthma management (Bailey et al., 1990).
The UAB ASMP was developed by Dr. William Bailey and colleagues, founded in elements of social cognitive theory and the PRECEDE (Predisposing, Reinforcing, Enabling Causes in Education, Diagnosis, and Evaluation) patient education model (Bailey et al., 1999). UAB researchers conducted systematic in-depth interviews and focus groups with asthma patients, physicians, and community members to understand their needs, priorities, predisposing factors, and barriers to better asthma control (Bailey et al., 1990; Kohler et al., 1993). The program design focused on increasing cognitive skills, creating positive attitudes, providing opportunities to model behaviors and experience success, and helping participants develop effective social support for their asthma. The ASMP consisted of a skill-oriented workbook and asthma self-management education group sessions with a health educator, plus two follow-up reinforcement calls and letters. Two randomized controlled trials demonstrated that the ASMP significantly improved asthma medication adherence and decreased reports of asthma symptoms (Bailey et al., 1987; Bailey et al., 1990; Bailey et al., 1999; Windsor et al., 1990).
The Lung Association worked with the UAB Lung Health Center and the UAB Center for Health Promotion to adapt the ASMP for broad community-based implementation. Lung Association staff and UAB researchers collaborated to update the program content in alignment with the National Institutes of Health’s Expert Panel Report guidelines for asthma care, the key components of asthma self-management education programs identified by a 2002 Cochrane Review, the educational needs of adults with asthma identified from the patient focus groups, and the latest findings on asthma education from the scientific literature (National Institutes of Health, National Heart, Lung, & Blood Institute, National Asthma Education and Prevention Program, 2002; Gibson et al., 2002). The workbook and instructional materials were adapted to be suitable for low-literacy and culturally diverse adult populations. For example, the workbook was rewritten using plain language at a fifth-grade reading level, the visual design was simplified for ease of reading, and images were selected to portray racial, cultural, and age diversity. They developed a training to prepare facilitators to deliver the program, including preparation on teaching about asthma in different cultural populations. The staff and researchers also developed an evaluation plan and questionnaires for testing the efficacy and acceptability of the program. The revised materials included a participant workbook and facilitator guide, Breathe Well, Live Well: An Asthma Management Program for Adults, released in the fall of 2004. The program consisted of three components:
an orientation session;
a 4- to 5-hour intensive workshop with flexible delivery time formats of 1, 2, or 3 days led by a trained facilitator; and
a reinforcement call 2 weeks after the workshop.
The workshop contained six modules: Asthma and Breathing; Getting Help from the Professionals; Learning about Asthma Medicines; Asthma, Medicine Use, and other Health Conditions; Daily Self-Management; and Good Health Practices (American Lung Association, 2005). Participants were given the educational workbook and were encouraged to share it with their support network. The program was presented in both English and Spanish and was targeted to adults ages 25 to 64 with either a recent asthma diagnosis or persistent asthma, in historically underserved populations.
PILOT EVALUATION: 2004–2005
Process
The national office of the American Lung Association invited proposals from local Lung Association offices to pilot BWLW at sites around the United States. Six local offices, representing a cross-section of geographic locations and populations, were selected based on a community needs assessment, support from local health care providers, and access to culturally diverse populations of adults with asthma. The locations were
Tucson, AZ;
Washington, DC;
Jacksonville, FL;
Chicago, IL;
San Diego and Imperial counties, CA; and
San Francisco and San Mateo counties, CA.
Pilot site facilitators were trained in February 2005 and then held the adult asthma education sessions through June 2005. The pilot reached 104 adults with asthma across the six sites. Sites recruited adult participants in a variety of ways, most commonly by placing flyers at health care provider sites and community groups but also through newspaper and television advertisements. The evaluation plan measured program efficacy through questionnaires that assessed asthma knowledge, attitudes, and self-management practices among program participants immediately after the workshop and at a 3-month follow-up call. Participants and facilitators also completed evaluation questionnaires on their satisfaction with the program, ratings of the quality of the workshop components, and any recommended changes. A paired Student’s t test was used to compare baseline scores with immediate and follow-up test scores.
Results
Immediate posttest knowledge scores increased significantly, from 19.28 to 21.53 (out of a possible score of 42), with a mean difference of 2.25 (p < .001). Forty-one participants responded at the 3-month follow-up call; their mean knowledge scores increased to 27.17 (p < .001). Attitude scores remained generally the same between the pre- and posttest assessments (Kohler, 2006). Questionnaire items about asthma self-management practices at the 3-month follow-up test showed statistically significant changes in most responses from the 41 follow-up participants (Table 1). Self-reported practices such as, “I keep track of my peak flow readings by writing them down” (p < .001) and “I take my quick relief medication before I exercise” (p = .002) saw improvements at 3 months postworkshop.
TABLE 1.
Pilot Evaluation Participants’ Self-Reported Asthma Self-Management Practices at Pre- and Posttest
| How often do you do the following? | N | Pretest mean score | 3-Month posttest mean score | p |
|---|---|---|---|---|
| I take my long-term control medicines like my health care provider says I should | 39 | 2.95 | 3.41 | .068 |
| I take my quick relief medicines like my health care provider has told me to | 39 | 3.23 | 3.77 | .026 |
| I keep a schedule of when I am supposed to take each of my medicines | 39 | 2.08 | 2.64 | .013 |
| I follow an asthma action plan according to my symptoms or peak flow reading | 38 | 1.95 | 2.89 | .004 |
| I check my peak flow reading at the same time of day each time I check | 38 | 1.34 | 2.16 | .001 |
| I check my peak flow reading when I am not having symptoms | 36 | 1.50 | 2.17 | .013 |
| I keep track of my peak flow readings by writing them down | 37 | 1.14 | 2.08 | <.001 |
| I keep track of how often I have asthma symptoms and how bad they are | 39 | 1.64 | 2.23 | .003 |
| I avoid going places where I know people will be smoking | 39 | 2.64 | 2.97 | .051 |
| I keep my house free of asthma triggers | 38 | 2.55 | 3.00 | .015 |
| I take my quick relief medicine before I exercise | 37 | 2.00 | 3.11 | .002 |
| I try not to let my emotions get out of control | 39 | 2.28 | 3.03 | .003 |
| I see one health care provider regularly | 39 | 3.03 | 3.59 | .002 |
| I see my asthma health care provider even when I am well | 39 | 2.79 | 3.41 | .009 |
| I ask my health care provider questions if I don’t understand something about my asthma | 39 | 2.92 | 3.64 | .003 |
| I know which of my symptoms mean I should get help right away | 39 | 3.00 | 3.67 | .002 |
| 3-month scale mean | 39 | 2.29 | 2.98 | <.001 |
Note. Boldface values are significant at p < .05. Adapted with permission from the American Lung Association (Kohler, 2006).
Participants evaluated the workshops positively at the immediate posttest: 99% of respondents said they would recommend the program to other people with asthma. Participants expressed satisfaction, with 76.5% indicating the program completely met their goals and 23.5% indicating that it partially met their goals. At the 3-month follow-up telephone call, 73% of respondents said they had been referring to the workbook; 72% reported having talked with their provider about their medications and their asthma action plan (Kohler, 2006).
Facilitators of the BWLW pilot noted that partnering with health care providers and organizations was an effective recruitment strategy. They also reported that more time was often needed in workshops and recommended changes to the evaluation questionnaires (Kohler, 2006).
DISSEMINATION EVALUATION: 2005–2010
Process
CDC NCEH awarded the Lung Association another cooperative agreement in 2005 (5U58EH224950, 2005–2010). The Lung Association proposed refining and adapting BWLW in light of the findings from the pilot evaluation, disseminating the program nationally, developing marketing materials to increase program adoption by organizations, and crafting a nationwide training protocol for BWLW facilitators.
In February 2006, the Lung Association convened the BWLW Advisory Group again to review the findings of the pilot evaluation and to revise the BWLW program materials, the workshop delivery format, and the evaluation questionnaires. The advisory group reviewed the results and evaluation feedback from participants and made recommendations on changes to the program and evaluation materials (e.g., updating medication information, adding more group discussion time, and streamlining questionnaires to remove repetitive questions). Facilitator feedback and training materials were examined to make recommendations to the Lung Association on improving facilitator training in several areas: instruction in asthma medications and device techniques, cultural competency, and knowledge of local resources. Members of the advisory group analyzed the perspectives of the primary audiences for BWLW—patient and provider groups, employers, community organizations, and health systems—and developed strategies and messages to promote the chances of program adoption by each group (e.g., clinic presentations, worksite communications, and promotions by managed care and other health plans). A revised version of the BWLW workbook and facilitator materials were produced in August 2006.
National staff and twelve local Lung Association offices collaborated in November 2006 to build their capacity to disseminate BWLW and contribute to its improvement and sustainability in their communities. The Lung Association funded five local Lung Associations with support from CDC NCEH. An additional seven offices were funded through an educational sponsorship from the pharmaceutical company, AstraZeneca. Dissemination areas were
Phoenix/Maricopa County, AZ;
Kern, Tulare, Kings, Fresno, Madera, Merced/Mariposa, and Stanislaus counties, CA;
Wilmington, DE;
Cities of Atlanta, Augusta, and Albany, GA;
Sangamon County, Springfield, and Menard, IL;
Cook County, Englewood, Evanston, and metropolitan Chicago, IL area;
Cities of Fort Wayne, Gary, and Indianapolis, IN;
Minneapolis and St. Paul, MN;
Douglas and Sarpy Counties, NE;
Union, NJ;
Newport/Lincoln County and metropolitan Portland, OR area;
Tulsa and Oklahoma City, OK;
Wake, Cleveland, Craven, Gaston, and Buncombe Counties, NC;
Cities of Bethlehem, Scranton, Camp Hill, and Philadelphia, PA; and
Cities of Milwaukee, Madison, Green Bay, and Fox Valley, WI.
Results
An evaluation of the first 6 months of the BWLW dissemination—January 1 through June 30, 2007—indicated that most sites found success in recruiting and training facilitators, with over 200 facilitators trained. However, only eight of the sites were able to implement BWLW during the evaluation period, with 167 adults participating. The dissemination sites reported participant recruitment as the greatest challenge (Hagen, 2008).
Of the 167 enrolled participants, 143 (86%) completed the intake questionnaire and 128 (77%) completed a posttest questionnaire immediately after the workshop. However, only 36 adults (22% of enrollees) completed a mailed 6-week follow-up questionnaire. Questionnaires covered asthma-related knowledge, attitudes, self-management practices, and evaluation of the acceptability and utility of the program.
Evaluation results showed significant increases in participant asthma-related knowledge scores. Significance was calculated with a paired Student’s t test. The mean score of the 128 participants who completed the posttest knowledge questionnaire improved from 3.86 at the pretest to 4.69 (out of a possible score of 9), with a mean difference of 0.83 (p < .001; data not shown). The limited number of 6-week follow-up responses showed no significant change (paired pretest sample mean 3.78, follow-up mean 4.42, p = .100). Attitude scores showed improvement at both the immediate posttest and 6-week follow-up, with nonsignificant declines for some items (Hagen, 2008).
As in the pilot evaluation, the asthma self-management practices questionnaire indicated significant improvements at the 6-week posttest (Table 2). Self-reported practices like writing down all peak flow readings (p < .001) and taking quick-relief medications before exercise (p < .001) showed improvements at 6 weeks postworkshop. Participants in the dissemination evaluation also reported satisfaction with the program, with 82% reporting that the program met their goals completely at the immediate posttest. Nearly all the respondents said they would recommend the program to other people with asthma (Hagen, 2008).
TABLE 2.
Dissemination Evaluation Participants’ Self-Reported Asthma Self-Management Practices at Pretest and Immediate and 6-Week Follow-Up Posttest
| How often do you do the following? |
Pretest N |
Pretest mean score | Immediate posttest mean score | p |
Follow-up N |
Follow-up posttest mean score |
Follow-up p |
|---|---|---|---|---|---|---|---|
| Keep a schedule of when to take medications | 91 | 3.51 | 3.67 | .350 | 29 | 3.79 | .085 |
| Check peak flow reading same time every day | 74 | 1.68 | 2.41 | <.001 | 26 | 2.81 | <.001 |
| Write down all peak flow readings | 71 | 1.54 | 2.31 | <.001 | 23 | 2.65 | <.001 |
| Keep track of frequency of asthma symptoms | 86 | 2.24 | 2.76 | .001 | 25 | 3.00 | .004 |
| Keep house free of asthma triggers | 84 | 3.21 | 3.36 | .280 | 28 | 3.71 | .069 |
| Take quick-relief medications before exercise | 82 | 2.71 | 3.01 | .066 | 27 | 3.26 | .001 |
| Avoid activities because of asthma (reversed) | 84 | 2.21 | 2.40 | .202 | 29 | 2.10 | .077 |
| Try not to let emotions get out of control | 84 | 3.60 | 3.81 | .075 | 29 | 3.90 | .009 |
| Know which symptoms mean to get help right away | 85 | 3.81 | 4.06 | .040 | 29 | 4.31 | .001 |
| Overall Practice Scale Mean Score | 93 | 2.77 | 3.13 | <.001 | 31 | 3.26 | <.001 |
Note. Boldface values are significant at p < .05. Adapted with permission from the American Lung Association (Hagen, 2008).
LOCAL IMPLEMENTATION: LONG BEACH DEPARTMENT OF HEALTH AND HUMAN SERVICES’ COMMUNITY ASTHMA AND AIR QUALITY RESOURCE EDUCATION (CAARE) PROGRAM: 2008–2013
Process
The Long Beach Department of Health and Human Services carried out a large implementation of BWLW with support from the local and national Lung Associations, as well as funds from the BP/South Coast Air Quality Management District Community Benefit programs and the Port of Long Beach Community Grant Program. The Community Asthma and Air Quality Resource Education (CAARE) program was designed to improve the respiratory health and well-being of adults with asthma in an area with poor air quality due to nearby shipping ports, highways, and oil refineries. Lung Association staff in California trained CHWs employed by the health department to deliver BWLW, using the curriculum with adults and seniors as part of an in-home, one-on-one intensive asthma self-management education program. The evaluation period ran from August 2008 to September 2013 in the cities of Long Beach, Carson, and Wilmington, CA (Lyde et al., 2013).
The educational program included a home environment assessment and education on reducing asthma triggers in the home. Participants were recruited via partner referrals from health care providers and community organizations, as well as door-to-door visits in local neighborhoods. Participation was incentivized with “green” cleaning supplies, spacers or peak flow meters, and gift cards offered at different time points in the program. The CHWs delivering the in-home asthma education collected intake forms and questionnaires at the initial orientation visit, then delivered the six BWLW lessons in 1.5-hour segments spaced over 2 weeks. The asthma questionnaire covered asthma symptoms, self-management practices, missed days of work or school, and health care utilization. Participants completed the asthma questionnaire at baseline, at the end of the second home visit, and at a 3-month follow-up visit.
The evaluation compared health status and practices at enrollment and at a follow-up assessment 3 months after enrollment. A total of 1,050 participants completed the 3-month follow-up assessment. The participant population was primarily Hispanic and mostly women, with an average age of 42. Many were nonworking adults, but others reported working or attending an educational institution (Lyde et al., 2013).
Results
Over the evaluation period, participants who completed the full series of questionnaires reported improvements in various asthma self-management practices and outcomes. The significance of changes in continuous outcomes between baseline and follow-up scores was measured with a Student’s t test, while McNemar’s test was used to test the significance of changes in dichotomous answers between matched responses.
Several self-reported practices promoting better asthma control improved between the baseline assessment and the 3-month follow-up, while others did not change significantly (Table 3). For example, a significantly higher proportion of participants reported having a written asthma action plan from a physician (3.8% to 27.1%, McNemar’s p < .001) and using a peak flow meter (8.7% to 59.8%, McNemar’s p < .001) at the 3-month follow-up visit. Other practices, like taking controller medication daily, did not show a significant increase at follow-up (31.9% to 32.3%, McNemar’s p = .839).
TABLE 3.
CAARE Program Self-Reported Asthma Self-Management Practices at Baseline and Three-Month Follow-Up
| Asthma self-management practice | N | Baseline “Yes” response | Follow-up “Yes” response |
McNemar’s p |
|---|---|---|---|---|
| Has a written action plan | 953 | 3.8% | 27.1% | <.001 |
| Has controller medications | 756 | 32% | 38.8% | <.001 |
| Takes controller medications daily | 953 | 31.9% | 32.3% | .839 |
| Has quick-relief medications | 953 | 75.4% | 72.4% | .085 |
| Takes quick-relief medications fewer than two times weekly | 953 | 37.9% | 37.3% | .831 |
| Uses a spacer all or most of the time | 735 | 7.2% | 53.3% | <.001 |
| Uses a peak flow meter | 747 | 8.7% | 59.8% | <.001 |
Note. Boldface values are significant at p < .05. CAARE = Community Asthma and Air Quality Resource Education.
The CAARE questionnaire also asked about missed days of school and work and about health care utilization (Table 4). Among the small numbers of participants who reported missing days of school or work in the previous month due to asthma, days of work missed decreased from a mean of 3.7 days of work missed at baseline to a mean of 2 days of work missed at follow-up (p = .015; Table 4). The number of school days missed in the previous month did not change significantly at follow-up (4.2 to 2.6, p = .306). The proportion of participants missing any days of work or school decreased, from 40.19% to 16.26% (McNemar’s p < .001) and 20.44% to 10.67% (McNemar’s p < .001), respectively; the proportion of caregivers for adult participants with asthma missing any days of work due to providing care also decreased significantly (11.23% to 3.99%, McNemar’s p < .001; data not shown).
TABLE 4.
CAARE Program Participants’ Missed Days of School and Work and Health Care Utilization at Baseline and 3-Month Follow-Up
| In the past 1 month, how many days did you … | N (matched) |
Baseline mean days (SD) | Follow-up mean days (SD) | Mean difference (SD) | 95% Confidence interval | p | |
|---|---|---|---|---|---|---|---|
| Lower bound | Upper bound | ||||||
| Miss work due to asthma (self) | 49 | 3.694 (5.683) | 2.0 (2.327) | 1.694 (4.722) | 0.337 | 3.050 | .015 |
| Miss school due to asthma (self) | 19 | 4.158 (6.492) | 2.632 (1.342) | 1.526 (6.319) | −1.519 | 4.572 | .306 |
| Caregiver missed work due to participant’s asthma | 12 | 3.0 (2.374) | 2.083 (1.73) | 0.917 (0.996) | 0.284 | 1.55 | .009 |
| In the past 6 months, how many … | N (matched) |
Baseline mean visits (SD) | Follow-up mean visits (SD) | Mean difference (SD) | 95% Confidence interval | p | |
| Lower bound | Upper bound | ||||||
| Times hospitalized due to asthma | 77 | 2.429 (1.867) | 1.857 (1.189) | 0.571 (1.824) | 0.157 | 0.985 | .007 |
| Visits to emergency department due to asthma | 40 | 2.025 (1.31) | 1.825 (1.196) | 0.2 (1.344) | −0.23 | 0.63 | .352 |
| Unscheduled visits to doctor’s office for asthma attack | 133 | 2.549 (2.19) | 1.985 (1.497) | 0.564 (1.676) | 0.276 | 0.851 | <.001 |
Note. Boldface values are significant at p < .05. CAARE = Community Asthma and Air Quality Resource Education.
Mean self-reported emergency department visits due to asthma decreased from 2.43 visits over the previous 6 months at baseline to 1.86 visits at the 3-month follow-up (p = .007; Table 4). Participants also reported a significant decrease in unscheduled health care visits due to asthma in the past 6 months, from a mean of 2.55 visits to 1.99 (p < .001). Using estimates of asthma care costs in California from Milet et al. (2013) and Aetna health maintenance organization, these decreases in health care utilization saved an estimated $5 million over the evaluation period.
The CAARE home visitors observed that it was difficult to motivate adults to access medical care and resources for their asthma. They recommended longer intervention times and more CHW contacts to help participants commit to sustainable behavior changes that would help control their asthma. In addition, social and economic barriers (e.g., renting) often prevented these adults with asthma from being able to control some of the environmental triggers in their homes (Lyde et al., 2013).
TRANSFORMATION AND CURRENT IMPLEMENTATION: 2010–PRESENT
The American Lung Association reconvened the BWLW Advisory Group in May 2010 to review the program’s successes and challenges in implementation and to identify ways to expand and sustain the program. Staff and facilitators from dissemination sites presented their results from implementing BWLW in their communities and shared a variety of experiences with recruitment and program delivery. For example, one highly effective strategy in California involved reaching out directly to adults with asthma from health plans’ patient databases. Many other sites reported significant difficulties recruiting adults to group education classes. Adaptations were recommended to the program and facilitator training based on the successes and barriers reported by the dissemination sites, including adding a one-on-one format to accommodate usage in nongroup settings and developing an online module to prepare BWLW facilitators at their own pace and convenience.
The Lung Association updated the program design and delivery formats to help overcome implementation barriers and meet the needs of BWLW facilitators and participants. In October 2012, the Lung Association updated the workbook, adding more information about asthma triggers at home and work, with links to online educational videos. Designed to be used in partnership with a health care provider, CHW, or asthma educator, the print and e-reader workbook, Breathe Well, Live Well: The Guide for Managing Asthma at Home and Work, was launched in June 2013 (American Lung Association, 2013).
The increasing focus on having CHWs provide in-home asthma interventions, reflecting the strong recommendation for services by the Community Preventive Services Task Force (along with the evidence from the Long Beach CAARE program), led the Lung Association to include CHWs as a major audience for training as BWLW facilitators (Task Force on Community Services, 2011). In 2017, the Lung Association developed and released an online facilitator training that targets CHWs, health care practitioners in hospital and clinic settings, certified asthma educators (AE-Cs), and community health educators (American Lung Association, 2017). The training provides a foundation in asthma knowledge and skills, as well as motivational interviewing and shared decision-making techniques.
Breathe Well, Live Well is currently available across the United States. The program is primarily disseminated through local Lung Association offices and includes the online training and BWLW workbooks. The Lung Association recruits BWLW facilitators through nationwide promotion of the program and via community-based partnerships. Sites adopting and implementing the BWLW program include public and private hospitals, community health centers, health departments, and local Lung Associations. Many current BWLW facilitators are CHWs, nurses, or health educators working as part of a care team at clinics and community health centers.
In focus groups and interviews conducted as part of regular program review by the Lung Association after the release of the online training in 2017, current BWLW facilitators report that they find the evidence base and flexible implementation design of the program attractive. Bringing the training online to prepare qualified facilitators to deliver the program has expanded its reach and made implementation more accessible. Program uptake has been successful when the facilitator is adopting the program as part of their role within their organization and can act as the “institutional champion” for asthma education. Facilitators report feeling confidence in the training and success when providing the program in both small group and one-on-one formats: The flexibility allows facilitators to customize the frequency and timing of lessons to meet the needs of their community or institution. This accessibility and flexibility help drive program adoption and sustainability in their diverse settings.
Similar to the experiences of the implementation sites during the pilot and dissemination studies, many current BWLW facilitators report struggling with participant recruitment. They report difficulty getting health care providers to complete referrals during asthma clinic visits and little success with promotions on the radio or through community announcements. Some facilitators have achieved successful recruitment by offering the program through senior centers, a chronic disease center at a local hospital, and by collaborating with a social worker providing other services. Many facilitators are working to educate the health care providers at their clinics to provide referrals to the program and are building partnerships with local asthma coalitions to improve future recruitment.
The Lung Association actively collaborates with the BWLW facilitators to learn about best practices and effective strategies, such as referral mechanisms, to share with others. The organization provides technical assistance, networking, and support opportunities for facilitators, and evaluates the programs. The Lung Association reviews facilitator feedback on an annual basis and makes updates to the curriculum, training, and technical assistance opportunities for continuous improvement.
DISCUSSION
Successes
Breathe Well, Live Well is an asthma self-management intervention for adults with a flexible delivery format that can improve asthma knowledge, attitudes, and self-management practices. A review of three stages of implementation of BWLW reveals progress in its development and success. The 2005 pilot evaluation showed improved asthma knowledge scores and responses to asthma self-management behavior questions between baseline and follow-up questionnaires. The 2007 dissemination evaluation reflected similar improvements in participants who completed the program at a variety of sites and locations across the United States. The 2008 CAARE evaluation in Long Beach, CA, showed improvements in asthma self-management practices, plus decreased missed work, hospitalizations, and unscheduled doctor visits due to asthma. If these behavior changes are sustainable, these populations could see reduced health care utilization, improved quality of life, and other positive health outcomes resulting from better asthma control.
Implications for Practice
Self-management programs can encounter difficulties with recruiting and engaging adult participants, often due to lack of awareness, transportation problems, and cost barriers (Jerant et al., 2005; Murphy et al., 2017). BWLW facilitators have tested strategies to overcome recruitment and participation barriers when implementing BWLW in community settings. Some sites found success with direct methods like door-to-door recruitment by CHWs, while others found that the reach and capacity of health plans worked well to get participants involved in the program. Current successful implementation strategies include partnerships with community centers (e.g., senior centers) and collaborations with local asthma coalitions.
Collaborations among groups and agencies that deliver information and services into the community offer significant promise in reaching populations with a higher asthma burden and helping them control their asthma. Local delivery of programs and services can encourage community ownership and promote sustainability (Chin et al., 2012; Jordan & Osborne, 2007). Promising strategies in the implementation of BWLW reflect this effort toward collaboration with local organizations with the reach and focus needed to integrate asthma self-management education with other services. The Lung Association supports ongoing implementation of BWLW by developing community partnerships with hospitals, health systems, federally qualified health centers, and physician offices. The active dissemination and technical assistance provided by the national and local Lung Associations promotes adoption by new organizations and sustainable implementation by current facilitators.
Limitations
The findings of the pilot and dissemination evaluations were limited by low rates of enrollment and participation in the follow-up tests. Respondent bias in the follow-up results is likely due to the reduced number of respondents; those participants who felt most positively about the experience would have been more likely to respond after 3 months. The results may overestimate the changes participants made in their asthma self-management practices. However, the CAARE evaluation had high rates of participation at follow-up and showed similar, statistically significant improvements in self-management practices as the pilot and dissemination evaluations.
CONCLUSION
This is the first published evaluation to bring together the results of multiple stages of implementation of Breathe Well, Live Well. The findings of the three evaluations of BWLW, implemented in different geographic areas and settings, support the use of this adult asthma self-management education curriculum in improving adults’ self-efficacy and effective self-management behaviors.
Authors’ Note:
The authors would like to recognize as contributors Dr. Connie Kohler of the UAB School of Public Health, John Hagen of Health Strategies, Inc., Dr. Michael Lyde of Lyde Enterprises, and Judeth Luong of the Long Beach Department of Health and Human Services, Bureau of Environmental Health. This work would not have been possible without their previous evaluations. We would also like to thank the participants, Breathe Well, Live Well (BWLW) facilitators, and other partners whose involvement made the development and improvement of BWLW possible. The American Lung Association supported the development of this article in collaboration with the Centers for Disease Control and Prevention (CDC). Emily A. Gardner received support as a fellow from the Research Participation Program at the CDC administered by the Oak Ridge Institute for Science and Education (ORISE) through an interagency agreement between the U.S. Department of Energy and the CDC, and after the fellowship, for completion of the article through Karna, LLC. The content of this article is solely the responsibility of the authors and does not necessarily represent the official position of the Centers for Disease Control and Prevention.
REFERENCES
- Akinbami LJ, Bailey CM, Johnson CA, King ME, Liu X, Moorman JE, & Zahran HS (2012). Trends in asthma prevalence, health care use, and mortality in the United States, 2001–2010 (NCHS Data Brief, No 94). National Center for Health Statistics. [PubMed] [Google Scholar]
- American Lung Association. (2005). Breathe Well, Live Well®: Participant workbook.
- American Lung Association. (2013). Breathe Well, Live Well®: The guide to controlling asthma at work. https://www.lung.org/lung-health-diseases/lung-disease-lookup/asthma/living-with-asthma/creating-asthma-friendly-environments/guide-to-controlling-asthma-at-work
- American Lung Association. (2017). Breathe Well, Live Well® educator training. https://lung.training/courses/breathe-well-live-well.html
- Bailey WC, Kohler CL, Richards JM, Windsor RA, Brooks CM, Gerald LB, Martin B, Higgins DM, & Liu T (1999). Asthma self-management: Do patient education programs always have an impact? Archives of Internal Medicine, 159(20), 2422–2428. 10.1001/archinte.159.20.2422 [DOI] [PubMed] [Google Scholar]
- Bailey WC, Richards JM Jr., Brooks CM, Soong SJ, Windsor RA, & Manzella BA (1990). A randomized trial to improve self-management practices of adults with asthma. Archives of Internal Medicine, 150(8), 1664–1668. 10.1001/archinte.150.8.1664 [DOI] [PubMed] [Google Scholar]
- Bailey WC, Richards JM Jr., Manzella BA, Windsor RA, Brooks CM, & Soong SJ (1987). Promoting self-management in adults with asthma: an overview of the UAB program. Health Education Quarterly, 14(3), 345–355. 10.1177/109019818701400308 [DOI] [PubMed] [Google Scholar]
- Bryant-Stephens T, Kurian C, Guo R, & Zhao H (2009). Impact of a household environmental intervention delivered by lay health workers on asthma symptom control in urban, disadvantaged children with asthma. American Journal of Public Health, 99(Suppl. 3), S657–S665. 10.2105/AJPH.2009.165423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chin MH, Clarke AR, Nocon RS, Casey AA, Goddu AP, Keesecker NM, & Cook SC (2012). A roadmap and best practices for organizations to reduce racial and ethnic disparities in health care. Journal of General Internal Medicine, 27(8), 992–1000. 10.1007/s11606-012-2082-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark NM, Griffiths C, Keteyian SR, & Partridge MR (2010). Educational and behavioral interventions for asthma: Who achieves which outcomes? A systematic review. Journal of Asthma and Allergy, 3, 187. 10.2147/JAA.S14772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark NM, & Partridge MR (2002). Strengthening asthma education to enhance disease control. Chest, 121(5), 1661–1669. 10.1378/chest.121.5.1661 [DOI] [PubMed] [Google Scholar]
- Gibson PG, Powell H, Wilson A, Abramson MJ, Haywood P, Bauman A, Hensley MJ, & Roberts JJ (2002). Self-management education and regular practitioner review for adults with asthma. Cochrane Database of Systematic Reviews. 10.1002/14651858.CD001117 [DOI] [PubMed] [Google Scholar]
- Hagen J (2008). Evaluation of Breathe Well, Live Well: For activities conducted January 1–June 30, 2007 [Unpublished internal report]. American Lung Association. [Google Scholar]
- Hsu J, Wilhelm N, Lewis L, & Herman E (2016). Economic evidence for US asthma self-management education and home-based interventions. Journal of Allergy and Clinical Immunology: in Practice, 4(6), 1123–1134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jerant AF, von Friederichs-Fitzwater MM, & Moore M (2005). Patients’ perceived barriers to active self-management of chronic conditions. Patient education and counseling, 57(3), 300–307. 10.1016/j.pec.2004.08.004 [DOI] [PubMed] [Google Scholar]
- Jones MA (2008). Asthma self-management patient education. Respiratory Care, 53(6), 778–786. [PubMed] [Google Scholar]
- Jordan JE, & Osborne RH (2007). Chronic disease self-management education programs: Challenges ahead. Medical Journal of Australia, 186(2), 84. 10.5694/j.1326-5377.2007.tb00807.x [DOI] [PubMed] [Google Scholar]
- Kohler C (2006). Pilot evaluation: American Lung Association, “Breathe Well, Live Well”: Final report [Unpublished internal report]. American Lung Association. [Google Scholar]
- Kohler CL, Dolce JJ, Manzella BA, Higgins D, Brooks CM, Richards JM, & Bailey WC (1993). Use of focus group methodology to develop an asthma self-management program useful for community-based medical practices. Health Education Quarterly, 20(3), 421–429. 10.1177/109019819302000311 [DOI] [PubMed] [Google Scholar]
- Lyde M, Willis K, & Luong J (2013). Community Asthma and Air Quality Resource Education (CAARE) Program: In-home asthma case management for adults and seniors in Long Beach, Carson and Wilmington, CA. http://www.longbeach.gov/globalas-sets/health/media-library/documents/healthy-living/individual/asthma/caare-program-y1-y5-cumulative-report-120413
- Milet M, Lutzker L, & Flattery J (2013). Asthma in California: A surveillance report. California Department of Public Health, Environmental Health Investigations Branch. [Google Scholar]
- Murphy LB, Brady TJ, Boring MA, Theis KA, Barbour KE, Qin J, & Helmick CG (2017). Self-management education participation among US adults with arthritis: Who’s attending? Arthritis Care & Research, 69(9), 1322–1330. 10.1002/acr.23129 [DOI] [PubMed] [Google Scholar]
- National Institutes of Health, National Heart, Lung, & Blood Institute, National Asthma Education and Prevention Program. (2002). Expert Panel Report 2 (EPR-2): Guidelines for the diagnosis and management of asthma: Update on selected topics (NIH Publication 02–5074). https://www.nhlbi.nih.gov/files/docs/guidelines/asthmafullrpt_archive.pdf [PubMed]
- National Institutes of Health, National Heart, Lung, & Blood Institute, National Asthma Education and Prevention Program. (2007). Expert Panel Report 3 (EPR 3): Guidelines for the diagnosis and management of asthma (NIH Publication 08–4051). https://www.nhlbi.nih.gov/health-topics/guidelines-for-diagnosis-management-of-asthma
- Newman S, Steed L, & Mulligan K (2004). Self-management interventions for chronic illness. Lancet, 364(9444), 1523–1537. 10.1016/S0140-6736(04)17277-2 [DOI] [PubMed] [Google Scholar]
- Nurmagambetov T, Kuwahara R, & Garbe P (2018). The economic burden of asthma in the United States, 2008–2013. Annals of the American Thoracic Society, 15(3), 348–356. 10.1513/AnnalsATS.201703-259OC [DOI] [PubMed] [Google Scholar]
- O’Conor R, Martynenko M, Gagnon M, Hauser D, Young E, Lurio J, Wisnivesky JP, Wolf MS, & Federman AD, & Supporting Asthma Self-Management Behaviors Among Aging Adults (SAMBA) Investigators. (2017). A qualitative investigation of the impact of asthma and self-management strategies among older adults. Journal of Asthma, 54(1), 39–45. 10.1080/02770903.2016.1193602 [DOI] [PubMed] [Google Scholar]
- Pinnock H, Parke HL, Panagioti M, Daines L, Pearce G, Epiphaniou E, Bower P, Sheikh A, Griffiths CJ, & Taylor SJ (2017). Systematic meta-review of supported self-management for asthma: A healthcare perspective. BMC Medicine, 15(1), 64. 10.1186/s12916-017-0823-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Press VG, Pappalardo AA, Conwell WD, Pincavage AT, Prochaska MH, & Arora VM (2012). Interventions to improve outcomes for minority adults with asthma: A systematic review. Journal of General Internal Medicine, 27(8), 1001–1015. 10.1007/s11606-012-2058-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmier JK, & Leidy NK (1998). The complexity of treatment adherence in adults with asthma: challenges and opportunities. Journal of Asthma, 35(6), 455–472. 10.3109/02770909809070999 [DOI] [PubMed] [Google Scholar]
- Task Force on Community Services. (2011). Recommendations from the Task Force on Community Preventive Services to decrease asthma morbidity through home-based, multi-trigger, multicomponent interventions. American Journal of Preventive Medicine, 41(2 Suppl. 1), S1–S4. 10.1016/j.amepre.2011.04.011 [DOI] [PubMed] [Google Scholar]
- U.S. Centers for Disease Control and Prevention, National Center for Environmental Health, Asthma and Community Health Branch. (2002). Potentially effective interventions for asthma. https://www.cdc.gov/asthma/interventions/potentially-effective-interventions.htm
- U.S. Centers for Disease Control and Prevention, National Center for Environmental Health, Asthma and Community Health Branch. (2018a). EXHALE: A technical package to control asthma. https://www.cdc.gov/asthma/pdfs/EXHALE_technical_package-508.pdf
- U.S. Centers for Disease Control and Prevention, National Center for Environmental Health, Asthma and Community Health Branch. (2018b). Most recent asthma data. https://www.cdc.gov/asthma/most_recent_data.htm
- U.S. Centers for Disease Control and Prevention, National Center for Environmental Health, Asthma and Community Health Branch. (2019). Asthma surveillance data: Healthcare use data, 2016. https://www.cdc.gov/asthma/healthcare-use/healthcare-use-2016.htm
- U.S. Centers for Disease Control and Prevention, National Center for Environmental Health, National Asthma Control Program. (2016). Asthma self-management education: A compilation of selected resources [Unpublished internal document]. https://floridaasthmacoalition.com/flasthma/assets/File/2016%20Sept%20Asthma%20Self-Management%20Education%20Resource.pdf
- Windsor RA, Bailey WC, Richards JM Jr., Manzella B, Soong SJ, & Brooks M (1990). Evaluation of the efficacy and cost effectiveness of health education methods to increase medication adherence among adults with asthma. American Journal of Public Health, 80(12), 1519–1521. 10.2105/AJPH.80.12.1519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zahran HS, Bailey CM, Qin X, & Moorman JE (2015). Assessing asthma control and associated risk factors among persons with current asthma: Findings from the child and adult Asthma Call-back Survey. Journal of Asthma, 52(3), 318–326. 10.3109/02770903.2014.956894 [DOI] [PMC free article] [PubMed] [Google Scholar]


