Abstract
Traumatic brain injury (TBI) is associated with a host of psychiatric and neurobehavioral problems. As mortality rates have declined for severe TBI, attention has turned to the cognitive, affective, and behavioral sequelae of injuries across the severity spectrum, which are often more disabling than residual physical effects. Moderate and severe TBI can cause personality changes including impulsivity, severe irritability, affective instability, and apathy. Mild TBI, once considered a largely benign phenomenon, is now known to be associated with a range of affective symptoms, with suicidality, and with worsening or new onset of several psychiatric disorders including posttraumatic stress disorder (PTSD) and major depressive disorder. Repetitive head impacts, often in athletic contexts, are now believed to be associated with a number of emotional and behavioral sequelae. The nature and etiology of mental health manifestations of TBI (including a combination of brain dysfunction and psychological trauma and interrelationships between cognitive, affective, and physical symptoms) are complex and have been a focus of recent epidemiologic and mechanistic studies. This paper will review the epidemiology of psychiatric and neurobehavioral problems after TBI in military, civilian, and athletic contexts.
Keywords: Traumatic Brain Injury, Posttraumatic Stress Disorder, Major Depressive Disorder, Generalized Anxiety Disorder, Suicidality, Cognition
Introduction
The past two decades have witnessed tremendous growth in understanding of the complex relationship between traumatic brain injury (TBI) and mental health. As survival rates have improved in moderate-to-severe TBI, attention has turned to the neurobehavioral consequences of these injuries (1, 2). Mild TBI, once considered a largely benign phenomenon, has also been increasingly recognized as a diverse injury spectrum (3) and a major cause of morbidity (4–7). These developments have been spurred in part by the recognition of TBI as one of the signature injuries of the conflicts in Iraq and Afghanistan (8), as well as by increased concern over adverse outcomes in athletes who sustain TBIs in contact sports (9, 10).
In this review, we summarize the epidemiology of mental health problems after TBI in military, civilian, and athletic contexts. We define “mental health” broadly to encompass traditional psychiatric diagnoses (e.g., affective, substance use, and cognitive disorders) as well as symptoms that are either below diagnostic thresholds or that do not fit traditional psychiatric constructs. While our goal is to convey the breadth and frequency of mental health issues after diverse TBIs, we focus on topics that best represent the available literature and highlight ongoing areas of controversy. In particular, this review primarily focuses on affective symptoms and disorders along with a brief overview of other manifestations such as personality changes, substance misuse, and externalizing psychopathology. See other papers in this issue for deeper discussion of affiliated topics, such sleep/wake disturbance (11), neurodegeneration (12), substance use disorders (13), and neurochemical/neuroimaging correlates of post-TBI psychiatric problems (14, 15). Cognitive deficits, while a highly important manifestation of TBI, are also outside of the scope of this review and have been reviewed in detail elsewhere (16–18).
Epidemiology and Classification of Traumatic Brain Injury
In the United States in 2014, 2.53 million emergency department visits, 288,000 hospitalizations, and 56,800 deaths were associated with documented TBI (19). Additionally, there are millions of additional TBIs estimated annually, including injuries not formally diagnosed in hospital settings (56% of TBI in the emergency department (20)) and TBI that either goes untreated or is managed outside the hospital setting (e.g., most of the estimated 3.8 million sport- and recreation-related concussions that occur annually in the U.S.) (21, 22). Furthermore, military service members, not included in hospital-based epidemiologic studies, are at elevated risk of TBI both during combat deployments (e.g., 19.2% of soldiers deployed to Afghanistan) (23) and in garrison (especially post-deployment; (24)).
Although there is no universally agreed upon method for diagnosing and classifying TBI, TBI is generally accepted to reflect altered brain structure or function caused by an external force (25). Clinical signs considered sufficient to warrant a diagnosis typically include one or more of the following: acute intracranial injury on neuroimaging, neurologic deficits, unconsciousness, amnesia for peritraumatic events, and confusion or similar evidence of altered mental status. Historically, TBIs have been classified into injury severity strata (e.g., mild, moderate, severe) according to acute injury characteristics such as the patient’s level of consciousness (quantified with the Glasgow Coma Scale [GCS]) and the duration of unconsciousness and posttraumatic amnesia (if present) (4). Severity classifications are somewhat useful for outcome prediction but do not adequately reflect the vast differences between patients within and across severity strata. For example, the vast majority (>80%) of TBIs are classified as “mild” (mTBI), with diverse injury severity characteristics and outcomes within the mTBI population.
Different subpopulations of TBI (athletes, military service members, and the civilian general population) experience, on average, somewhat different injuries in terms of injury context and severity, and these subfields have developed different norms for TBI diagnosis and classification. Civilian TBI researchers often define mTBI by GCS score (13–15), with additional restrictions sometimes on the duration of unconsciousness (0–30 minutes) and posttraumatic amnesia (0–24 hours) (26). In contrast, the U.S. Department of Veteran Affairs (VA) further restricts the diagnosis of mTBI to injuries with no signs of brain injury on clinical neuroimaging. The vast majority of sport-related TBI meets the more restrictive VA definition of mTBI (sometimes used synonymously with concussion), although acute injury characteristics tend to be milder in athletes as compared to other TBI subpopulations (4).
Conceptualization and Epidemiology of Persistent Post-Concussive Symptoms
Diverse symptoms occur commonly after TBI and may include somatic symptoms (e.g., nausea, dizziness, headache, blurred vision, hearing changes, fatigue), cognitive complaints (including deficits in memory and executive functions), and emotional and behavioral problems (such as emotional lability, irritability, depression, and anxiety) (27). For mTBI especially, these diverse sequelae historically have been viewed through a dualistic lens in which psychological mechanisms (labeled “functional” or “psychogenic”) have been viewed as separate from biological (“organic”) mechanisms. For example, emotional and behavioral manifestations of concussion were sometimes viewed as part of an “accident neurosis” linked to desire for financial compensation (28). However, subsequent research indicated that these complaints did not resolve after compensation was received and also occurred when no compensation claim could be made (1, 29). While examining diverse predictors of persistent post-concussive symptoms is useful, modern psychiatric research recognizes psychological, motivational, and injury factors as important levels of analysis that are intertwined with, rather than distinct from, neurobiology.
Clinical nomenclature can further contribute to etiologic confusion. For example, while the terms “post-concussive symptoms” and “posttraumatic stress disorder” might lead to the assumption that the former is caused by direct physical injury to the brain such as axonal damage, while the latter is caused by psychological trauma related to the injury, research has shown that this simple etiologic distinction is untenable. Post-concussive symptoms themselves overlap heavily with symptoms of psychiatric disorders such as PTSD, major depressive disorder, and anxiety disorders (30), and can also occur after non-brain injuries (31–33). At the same time, PTSD is more common after TBI compared to other injuries, and physical damage to the brain such as axonal injury is thought to contribute directly to its development (30). Adding to the complexity, psychiatric disorders are both risk factors as well as outcomes of TBI (34). Contemporary research continues to recognize the multiple biopsychosocial factors that can contribute to individuals’ post-injury emotional functioning while using increasingly advanced neuroscientific methods to improve understanding of the neurobiology of post-concussion symptoms (35–37).
Despite uncertainty about the definition and etiology of persistent post-concussive symptoms, it remains a clinically useful concept to refer to diverse concussion/mTBI symptoms that persist for an unusually long time (e.g., about 1 month in athletes and 3 months in civilians). Prognosis after a single concussion is generally good, especially in athlete samples (e.g., only 1.5% of 127 prospectively-enrolled high school and collegiate athletes still reported symptoms at the 45-day study endpoint (38)). The prevalence of persistent post-concussive symptoms is higher in general community trauma samples with mTBI, although estimates vary a great deal by the definition used (e.g., 11.4–38.7% of a hospital-treated mTBI sample (39)). Despite progress in identifying biomarkers of damage in TBI, the causes of persistent post-concussive symptoms are poorly understood and may reflect the influence of psychosocial mechanisms including changes in self-image, close relationships, social networks, and vocational capacity (10, 34) and emerging pathophysiological mechanisms as discussed in several reviews in this issue (35–37). The higher prevalence of persisting mTBI symptoms in civilian populations is thought to be multifactorial, potentially including demographic/pre-injury risk factors for slower brain injury recovery, greater mTBI severity, and higher prevalence of impairing concurrent peripheral injuries. Further research is therefore needed to clarify the mechanisms of occult brain dysfunction in persistent post-concussive symptoms (40).
Chronic Traumatic Encephalopathy and Traumatic Encephalopathy Syndrome
Highly public case reports have drawn attention to concerns that exposure to repetitive head impacts may cause a neurodegenerative illness—chronic traumatic encephalopathy (CTE)—which has been proposed to cause myriad cognitive, psychiatric, and behavioral problems (traumatic encephalopathy syndrome [TES]) (41, 42). CTE has been recognized as a possible consequence of boxing since the early 20th century, yet only since the early 2000s have conceptions of TES expanded beyond motor and cognitive symptoms to include mood (e.g., depression) and behavioral concerns (e.g., substance abuse, disinhibition, aggression, paranoia) (43). Recently published consensus criteria for TES from the National Institute of Neurological Disorders and Stroke include substantial exposure to repetitive head impacts, cognitive impairment and/or neurobehavioral dysregulation, a progressive course, and lack of explanation for the clinical features based on another condition (44). This expanded conceptualization stems from case series of deceased individuals (especially former professional American football players) who were found to have brain pathology of CTE and for whom loved ones reported, postmortem, that they manifested various psychological and behavioral problems (41, 42).
While these case reports are concerning, prospective longitudinal studies are needed to corroborate or refute the proposal that repetitive head impacts causes CTE, and that CTE causes particular clinical signs and symptoms. Fortunately, with large-scale studies underway to follow athletes for 10 or more years post-sport participation, this area of research is likely to evolve rapidly. Recent reviews concluded relatively robust, replicable associations between retrospectively recalled concussion history and depression in former professional American football players (45, 46). On the other hand, having played professional football appears to either not predict, or predict lower risk of, suicide (47). Some studies also suggest high rates of opioid and alcohol misuse in former professional football players (48). Proposed phenotypes of TES are preliminary and intended to fuel further research. Recent findings that a high percentage of the general population meets the proposed clinical criteria for TES highlights the need to refine and validate TES phenotypes (43).
TBI and Affective Symptoms and Disorders
Affective sequelae of TBI were initially recognized in patients with severe TBI, starting with the famous penetrating brain injury sustained by Phineas Gage (49). Yet only in recent years has research focused on measuring affective changes in diverse TBI samples in lieu of prior emphasis on survival and functional impairment (1). Affective sequelae of TBI are increasingly recognized as highly prevalent and closely tied to TBI-related disability and quality of life (50, 51). This literature is imperfect, with wide variability in methodology and the scope of emotional changes that can make it difficult to draw comparisons across TBI subpopulations and studies.
Notwithstanding these limitations, a wealth of literature has concluded that patients with all severities of TBI are at elevated risk of affective symptoms, and in some cases clinically significant affective disorders, after injury (7, 52). In prospective athlete samples this risk appears time-limited—athletes tend to have on average better emotional functioning (lower symptom severity) than the general population pre-injury (38, 53) and to experience only brief, subtle increases in affective symptoms after concussion (53). In contrast, civilian trauma and military samples demonstrate higher rates of affective disorders and for longer after injury. For example, in a prospectively followed sample of 161 Australians with moderate-severe TBI, 62% met criteria for a least 1 DSM-IV Axis I disorder diagnosed via structured clinical interview in the first year post-injury, most commonly a depressive or anxiety disorder (54). The prevalence of these disorders diminished gradually over 5 years, with rates of returning to near the population base rate at year 2 for anxiety and year 5 for depressive disorder (see Figure 1). The most common diagnosis within each disorder class was Major Depressive Disorder and Anxiety Disorder NOS (usually subthreshold PTSD or generalized anxiety disorder). Although having a pre-injury psychiatric illness was a strong predictor of experiencing a post-TBI psychiatric disorder, a large proportion of mood and anxiety disorders were experienced de novo (Figure 2), consistent with other research suggesting that TBI can cause affective disorders to develop (54); see also (55, 56). A prospective study of civilian trauma patients found that mTBI was associated with elevated odds of developing panic disorder (odds ratio=2.01), social phobia (odds ratio=2.07), and agoraphobia (odds ratio=1.94) (57). In the prospective TRACK-TBI study, civilians with mTBI had a significantly higher rate of probable major depressive disorder than orthopedic trauma controls at 3 months (8.8% compared to 3%) but not at 6 months (58). Reviews have also concluded that the prevalence of affective disorders is higher than population base rates in mild or mostly mild civilian TBI samples (with major depressive disorder best established (59)).
Figure 1:
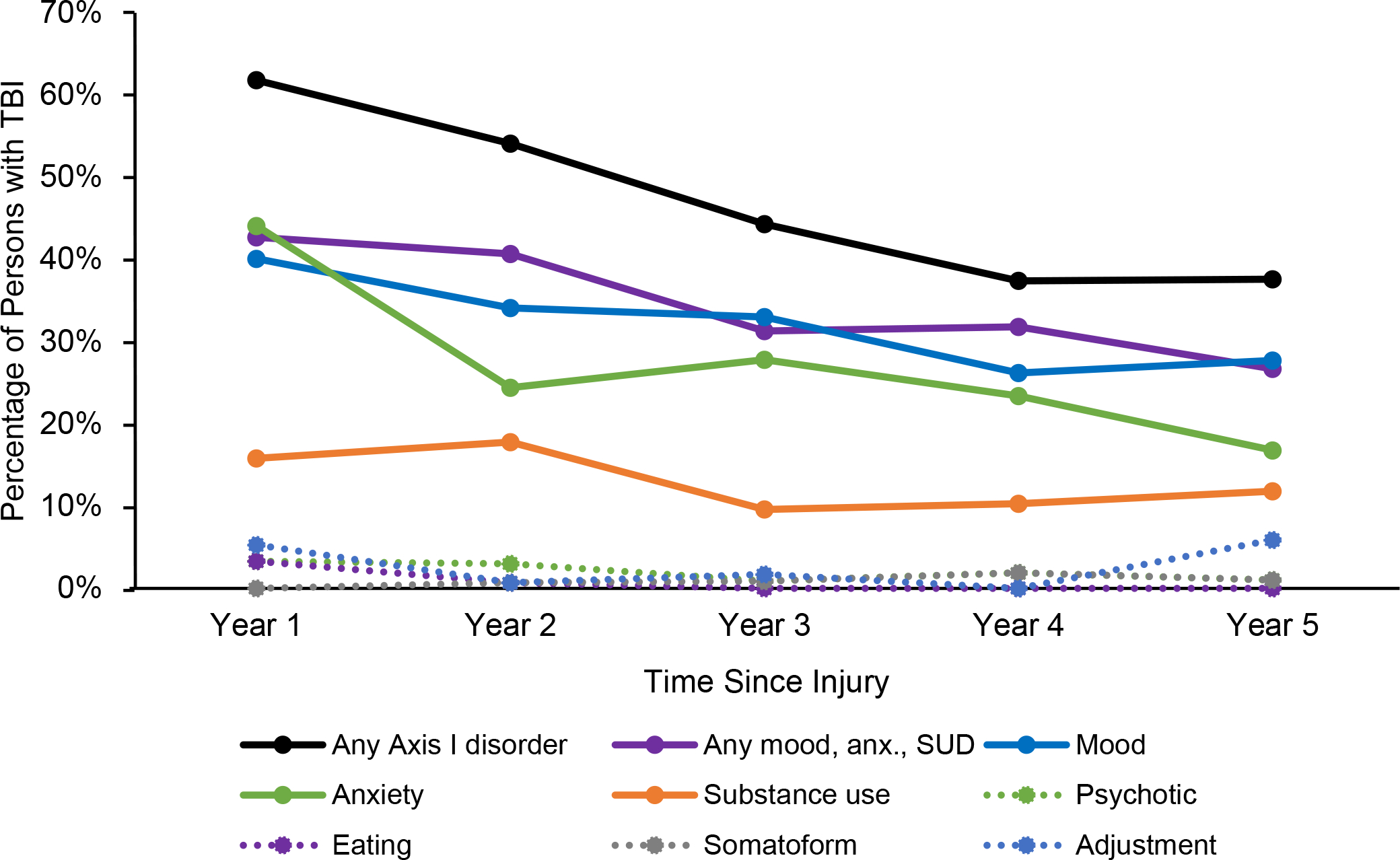
Annual prevalence of different classes of psychiatric disorder in the prospective study of moderate-severe TBI from Alway et al. (54). Diagnostic and Statistical Manual of Mental Disorders—Fourth Edition (DSM-IV) Axis I diagnoses were determined via structured clinical interview. Mood, anxiety, and substance use disorders were most prevalent DSM-IV Axis I disorders across five years of follow-up post-injury, with a steady decline in prevalence over time.
Figure 2:
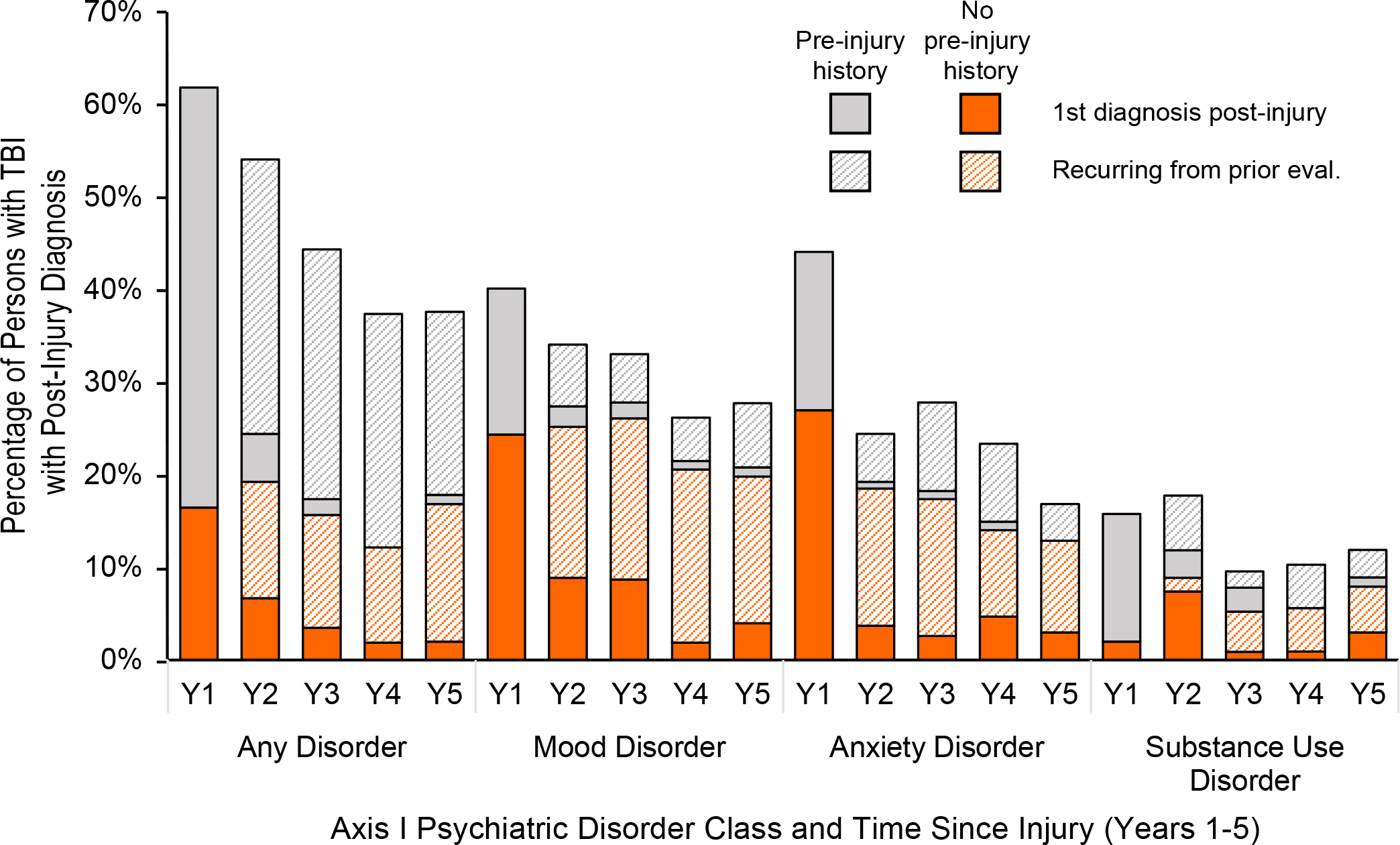
Percentage of individuals with moderate-severe TBI from Alway et al. (54) who met criteria for each psychiatric disorder class in each year of follow-up post-injury, stratified by whether it was the first time being diagnosed post-injury (solid color) or recurring from prior post-injury study visits, and whether or not participants had a pre-injury history of a disorder in that diagnostic class (grey = pre-injury history; orange = no pre-injury history). The first year post-injury was the primary period of vulnerability for the appearance of psychiatric disorders post-TBI (solid colors). Although having a pre-injury psychiatric disorder (grey) was a strong predictor of having disorders post-injury, mood and anxiety disorders in particular often presented in individuals with no pre-injury history (orange) of these types of disorders.
A number of studies examining affective symptoms from symptom inventories have yielded similar conclusions—that affective symptoms are common after civilian and military TBI. For example, recent large-scale prospective studies have reported a high prevalence of affective symptoms in level 1 trauma center mTBI samples (43–57% at 3–12 months) (60), with mTBI patients reporting significantly more psychological distress than orthopedic controls at 1 year (d = 0.20) (5). Similarly, another sample showed high rates of persisting affective and other mTBI-related symptoms at 1 year post-mTBI, despite relatively complete recovery of cognitive performance and functional abilities (33). Findings are equivocal regarding the relevance of TBI severity to affective symptoms. Numerous studies have found either a minimal relationship, while others have found an inverse relationship between TBI severity and symptoms severity (61). Numerous explanations have been offered for why individuals with severe TBI may have less severe emotional distress, including impaired insight and apathy that can result from severe TBI (2) as well as a potentially lower likelihood of developing PTSD for severe injuries (which tend not to be remembered by patients; see TBI and PTSD subsection for more discussion of this topic).
Like other community members, military service members are at increased risk of MDD, PTSD, and suicidality. The relationship between TBI and these outcomes in military service members is discussed in topic-specific subsections below. Additionally, a cohort study of 1567 US Army soldiers recruited shortly after return from deployment to Iraq or Afghanistan found an increased rate of reported “severe” or “very severe” irritability (adjusted relative risk = 2.73) among soldiers who sustained mTBI on deployment, which was consistent over the follow-up interval (3, 6, and 12 months) (62). In the prospective Army STARRS study, deployment-acquired TBI (mostly mTBI in this sample) was associated with increased risk of major depressive disorder (adjusted odds ratio=1.45) and generalized anxiety disorder adjusted (adjusted odds ratio=1.81) at 3 months post-deployment (23). At 9 months post-deployment, the association between TBI and generalized anxiety disorder persisted (adjusted odds ratio=1.81), but the association with major depressive disorder was no longer significant. Number of TBIs was positively associated with depressive symptoms in a different sample of military personnel referred for TBI evaluation (63).
TBI and PTSD
PTSD is of particular interest in relation to TBI, as the events that cause TBI can be emotionally traumatic. PTSD is characterized by re-experiencing symptoms, avoidance, and alterations in arousal, cognition, and mood, resulting from exposure to severe traumatic events. Events resulting in TBI often meet criteria as Criterion A traumas according to DSM-5 (American Psychiatric Association, 2013). While it was once argued that comorbid TBI and PTSD was uncommon, and that loss of consciousness and amnesia due to TBI may actually be protective against PTSD (64), a number of studies initiated after the conflicts in Iraq and Afghanistan have clearly demonstrated that TBI is actually an important risk factor for PTSD. However, given evidence that mTBI carries a higher risk of PTSD than more severe TBI (65), it remains possible that extended loss of consciousness and amnesia in severe TBI (as opposed to mTBI) do exert a protective effect.
Much of the research documenting a relationship between TBI and PTSD has occurred in military populations. Importantly, there are several factors that distinguish this population from civilians experiencing TBI, including the frequency of repeated blast injuries and the frequency of repeated deployments. Military personnel also often experience repeated psychological trauma through combat exposures, and these effects are difficult to fully disentangle from the physical trauma of TBI in epidemiologic studies. Cross-sectional studies in military personnel provided early evidence for a link between TBI and PTSD, with one survey of U.S. Army soldiers after return from deployment to Iraq finding PTSD rates of 43.9% of those reporting TBI with loss of consciousness, 27.3% of those reporting mTBI with altered mental status, 16.2% of those with other injuries, and 9.1% of those with no injury (66). A different cross-sectional study of military personnel after deployment to Iraq or Afghanistan found an association between mTBI sustained in combat and PTSD, with a prevalence ratio of 2.37 (67). Evidence also emerged for a dose-response relationship between TBI and PTSD, with number of lifetime TBIs being associated with PTSD symptom severity in a sample of military personnel referred for TBI evaluation while on deployment in Iraq (63).
Subsequent prospective studies in military personnel have confirmed that TBI is an important risk factor for PTSD. In the Marine Resiliency Study, which assessed Marine and Navy service members before and after deployment to Iraq or Afghanistan, deployment-related mTBI increased predicted PTSD symptoms by a factor of 1.23, while moderate or severe TBI increased predicted symptoms by a factor of 1.71 (68). In the same study, TBI doubled or nearly doubled risk of PTSD in individuals with less severe pre-deployment PTSD symptoms. Army STARRS assessed U.S. Army soldiers before and after deployment to Afghanistan (23). After controlling for other risk factors, deployment-acquired TBI (mostly mTBI in this sample) was associated with risk of PTSD at 3 months (adjusted odds ratio 1.81) and 9 months (adjusted odds ratio 1.48) post-deployment. There was also evidence for a dose-response relationship between severity of TBI (very mild, mild, and more-than-mild) and risk of PTSD.
In parallel with emerging evidence of the role of TBI as a risk factor for PTSD in military populations, several prospective studies have documented a similar relationship in civilian populations. Importantly, injury profiles differ in this population as they typically experienced a single impact injury as opposed to repetitive blast injuries often seen in military populations. A prospective cohort study of civilians who were traumatically injured found that individuals who sustained mTBI were more likely to develop PTSD (odds ratio=1.92) (57). In the TRACK-TBI study comparing 1155 civilians with mTBI with 230 patients with orthopedic injuries, the rate of probable PTSD at 6 months was 19.2% in the mTBI group and 9.8 % in the orthopedic control group (58). Risk factors for probable PTSD after mTBI included less education, being black, self-reported psychiatric history, and injury resulting from assault or other violence.
While epidemiologic studies have demonstrated that TBI is a risk factor for PTSD, the causal mechanism of this association remains unclear. TBI may damage neural circuits involved in regulating fear responses (30). Alternatively, cognitive impairment after TBI could reduce coping capacity and use of adaptive cognitive strategies (69). Finally, inflammatory responses after TBI could also contribute to worsened mental health outcomes (70). The possible contributions of direct physical damage to the brain, in addition to psychological trauma related to the context of an injury, to PTSD symptoms is highlighted by preclinical work demonstrating the emergence of PTSD-like behavior in rodent models of TBI (71).
TBI and Suicidality
Suicidality (including suicidal ideation and suicidal behaviors) is a particularly important sequela of TBI in military and civilian community samples. Several cross-sectional studies have found associations between TBI and suicidal ideation and behaviors, including studies controlling for other risk factors including depression, PTSD, and TBI symptom severity (63, 72–74). A study of 108,930 male Marines assessed at basic training and followed during active duty found that TBI was associated with risk of completed suicide after controlling for other risk factors such as depression (HR = 4.09) (75). An analysis of data from 7677 deployed US Army soldiers as part of the Army STARRS study found that, of all lifetime TBI characteristics evaluated pre-deployment, only past-month post-TBI symptoms were prospectively associated with risk of suicide attempt after deployment (76). Similarly, an analysis of 1158 civilian patients as part of the prospective TRACK-TBI study found that post-TBI symptoms were strongly associated with suicidal ideation after controlling for pre-injury factors (77). Importantly, a retrospective cohort study of 7,418,391 civilians in Denmark found that individuals with medical contacts for TBI had a higher risk of completed suicide than the general population without TBI (adjusted incidence rate ratio = 1.90) after adjusting for covariates such as psychiatric diagnoses, with severe TBI carrying the highest risk (adjusted incidence rate ratio = 2.38 for severe TBI vs. adjusted incidence rate ratio = 1.81 for mTBI) (74). A recent review concluded that individuals with TBI are at higher risk for suicide death than the general population and that comorbid depression and PTSD are significant post-TBI risk factors for suicide (78). An exception to these findings from military and civilian community samples, retired professional American football players have a lower risk of suicide than the general population, implying that exposure to sport-related concussion and repetitive head impacts may not increase risk of suicide (47).
Other Manifestations of TBI
Early psychological studies of the effects of severe TBI were largely focused on cognitive functions, but extensive behavioral consequences received increasing attention in the 1970s. Interviews with patients’ relatives revealed that these sequelae caused much greater distress than physical disabilities due to TBI and often had major life consequences in the form of relationship problems, social isolation, and unemployment (1). Major alterations in behavioral responses after moderate or severe TBI are often described by survivors and caregivers as “personality changes,” which are typically characterized by impulsivity, severe irritability, affective instability, apathy, and a frequent lack of awareness of these changes on the part of the affected individual (2). This pattern of behavioral changes is thought to reflect impaired functioning of specific frontal-subcortical circuits that are particularly vulnerable to damage in TBI (2). The emergence of affective lability, impulsivity, aggressive behavior, apathy, suspiciousness, or a combination of these after a TBI is included in DSM-5 under the diagnosis Personality Change Due to Another Medical Condition (79). Apathy experienced by a subset of severe TBI participants is clinically distinct from depression (by concomitant levels of negative affect) but may be difficult to discern from depression in studies that rely on self-reported mood.
Although the bulk of the literature has emphasized internalizing and somatic symptoms in individuals with TBI, externalizing psychopathology can also present after TBI. Substance misuse, in particular, is common both pre- and post-TBI. In the aforementioned sample of persons with moderate-severe TBI assessed through structured diagnostic interviews, substance use disorders were the 3rd most common class of DSM-IV Axis I disorders (after depression and anxiety) experienced by the sample and commonly reflected pre-injury pathology (Figure 1; (54)). See Olsen & Corrigan (13) in this issue for a detailed discussion of the evidence around the impact of TBI on substance use.
Conclusions
TBI is a common form of neurological injury and is associated with substantial morbidity. Mental health problems are increasingly recognized as important consequences of TBI that adversely affect quality of life and day-to-day functioning. Just as the TBI population is diverse, the mental health sequelae that can be experienced post-TBI are broad and comprise myriad concerns about emotional, cognitive, physical, and behavioral functioning. Concussion commonly presents with a host of physical, somatic, and cognitive symptoms (often below the threshold to warrant a psychiatric diagnosis) that are time-limited. However, differences the base rate of clinically significant mental health problems varies by mTBI subpopulation (low in contact sport athletes, higher in civilian and military trauma patients), for reasons that should continue to be explored. While it is possible that repeated mTBI exposure causes cumulative problems later in life, the quality of evidence for this remains poor due to a lack of prospective cohort studies. Mental health problems after moderate-severe TBI are common and span a variety of phenotypes, including apathy and impulsivity as well as affective symptoms and disorders common to all severities of TBI (especially major depression and generalized anxiety). Given the complex etiology of mental health manifestations of TBI (including a combination of brain dysfunction and psychological trauma and interrelationships between cognitive, affective, and physical symptoms), conceptual schemes should be continually updated in response to new evidence from epidemiologic, mechanistic, and treatment studies. Improved understanding of mental health sequelae of TBI will require ongoing collaboration between specialists in different disciplines.
Acknowledgments and Disclosures
Jonathon Howlett is supported by a grant from the Veterans Health Administration Clinical Sciences Research and Development Service (Career Development Award # IK2 CX001887). Lindsay Nelson is supported by National Institute of Neurological Disorders and Stroke (NINDS) grant #R01 NS110856.
Dr. Howlett previously received funds through his institution to participate in a clinical trial for a Janssen medication.
Dr. Stein in the past 3 years has received consulting income from Actelion, Acadia Pharmaceuticals, Aptinyx, Boehringer Ingelheim, Bionomics, BioXcel Therapeutics, Clexio, EmpowerPharm, GW Pharmaceuticals, Janssen, Jazz Pharmaceuticals, and Roche/Genentech. Dr. Stein has stock options in Oxeia Biopharmaceuticals and Epivario. He is paid for his editorial work on Depression and Anxiety (Editor-in-Chief), Biological Psychiatry (Deputy Editor), and UpToDate (Co-Editor-in-Chief for Psychiatry). He has also received research support from NIH, Department of Veterans Affairs, and the Department of Defense. He is on the scientific advisory board for the Brain and Behavior Research Foundation and the Anxiety and Depression Association of America.
Dr. Nelson in the past 3 years has received consulting income from the Department of Energy and research support from the National Institutes of Health, Department of Defense, National Football League, and the Medical College of Wisconsin Advancing a Healthier Wisconsin endowment.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ponsford JL (1990): Psychological sequelae of closed head injury: time to redress the imbalance. Brain Inj. 4:111–114. [DOI] [PubMed] [Google Scholar]
- 2.McAllister TW (2008): Neurobehavioral sequelae of traumatic brain injury: evaluation and management. World Psychiatry. 7:3–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mayer AR, Quinn DK, Master CL (2017): The spectrum of mild traumatic brain injury: A review. Neurology. 89:623–632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peskind ER, Brody D, Cernak I, McKee A, Ruff RL (2013): Military- and sports-related mild traumatic brain injury: clinical presentation, management, and long-term consequences. J Clin Psychiatry. 74:180–188; quiz 188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nelson LD, Temkin NR, Dikmen S, Barber J, Giacino JT, Yuh E, et al. (2019): Recovery After Mild Traumatic Brain Injury in Patients Presenting to US Level I Trauma Centers: A Transforming Research and Clinical Knowledge in Traumatic Brain Injury (TRACK-TBI) Study. JAMA Neurol. 76:1049–1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Silverberg ND, Duhaime AC, Iaccarino MA (2020): Mild Traumatic Brain Injury in 2019–2020. Jama. 323:177–178. [DOI] [PubMed] [Google Scholar]
- 7.Albrecht JS, Abariga SA, Rao V, Wickwire EM (2020): Incidence of New Neuropsychiatric Disorder Diagnoses Following Traumatic Brain Injury. The Journal of Head Trauma Rehabilitation. 35:E352–E360. [DOI] [PubMed] [Google Scholar]
- 8.Tanielian TL, Jaycox L (2008): Invisible Wounds of War: Psychological and Cognitive Injuries, Their Consequences, and Services to Assist Recovery. Santa Monica, CA: Rand Corporation. [Google Scholar]
- 9.Omalu BI, DeKosky ST, Minster RL, Kamboh MI, Hamilton RL, Wecht CH (2005): Chronic Traumatic Encephalopathy in a National Football League Player. Neurosurgery. 57:128–134. [DOI] [PubMed] [Google Scholar]
- 10.Blennow K, Brody DL, Kochanek PM, Levin H, McKee A, Ribbers GM, et al. (2016): Traumatic brain injuries. Nature Reviews Disease Primers. 2:16084. [DOI] [PubMed] [Google Scholar]
- 11.Piantino JA, Iliff JJ, Lim MM (2021): The bidirectional link between sleep disturbances and traumatic brain injury symptoms: A role for glymphatic dysfunction? Biological Psychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brett BL, Gardner RC, Godbout J, Dams-O’Connor K, Keene CD (2021): Traumatic Brain Injury and Risk of Neurodegenerative Disorder. Biological Psychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Olsen CM, Corrigan JD (2021): Does TBI Cause Risky Substance Use or Substance Use Disorder? Biological Psychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mayer AR, Quinn DK (2021): Neuroimaging Biomarkers of New-Onset Psychiatric Disorders Following Traumatic Brain Injury. Biological Psychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Meier TB, Savitz J (2021): The Kynurenine Pathway in Traumatic Brain Injury: Implications for Psychiatric Outcomes. Biological Psychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Karr JE, Areshenkoff CN, Garcia-Barrera MA (2014): The neuropsychological outcomes of concussion: a systematic review of meta-analyses on the cognitive sequelae of mild traumatic brain injury. Neuropsychology. 28:321–336. [DOI] [PubMed] [Google Scholar]
- 17.Schretlen DJ, Shapiro AM (2003): A quantitative review of the effects of traumatic brain injury on cognitive functioning. Int Rev Psychiatry. 15:341–349. [DOI] [PubMed] [Google Scholar]
- 18.Dikmen SS, Corrigan JD, Levin HS, Machamer J, Stiers W, Weisskopf MG (2009): Cognitive outcome following traumatic brain injury. J Head Trauma Rehabil. 24:430–438. [DOI] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention (2019): Surveillance Report of Traumatic Brain Injury-related Emergency Department Visits, Hospitalizations, and Deaths—United States, 2014. In: Centers for Disease Control and Prevention USDoHaHS, editor. [Google Scholar]
- 20.Powell JM, Ferraro JV, Dikmen SS, Temkin NR, Bell KR (2008): Accuracy of mild traumatic brain injury diagnosis. Arch Phys Med Rehabil. 89:1550–1555. [DOI] [PubMed] [Google Scholar]
- 21.Langlois JA, Rutland-Brown W, Wald MM (2006): The epidemiology and impact of traumatic brain injury: a brief overview. J Head Trauma Rehabil. 21:375–378. [DOI] [PubMed] [Google Scholar]
- 22.Coronado VG, McGuire LC, Sarmiento K, Bell J, Lionbarger MR, Jones CD, et al. (2012): Trends in Traumatic Brain Injury in the U.S. and the public health response: 1995–2009. J Safety Res. 43:299–307. [DOI] [PubMed] [Google Scholar]
- 23.Stein MB, Kessler RC, Heeringa SG, Jain S, Campbell-Sills L, Colpe LJ, et al. (2015): Prospective longitudinal evaluation of the effect of deployment-acquired traumatic brain injury on posttraumatic stress and related disorders: results from the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS). Am J Psychiatry. 172:1101–1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Helmick KM, Spells CA, Malik SZ, Davies CA, Marion DW, Hinds SR (2015): Traumatic brain injury in the US military: epidemiology and key clinical and research programs. Brain Imaging Behav. 9:358–366. [DOI] [PubMed] [Google Scholar]
- 25.Department of Veterans Affairs, Department of Defense (2016): Clinical Practice Guideline: Management of Concussion-mild Traumatic Brain Injury. Version 2.0 ed. [Google Scholar]
- 26.Silverberg ND, Iverson GL (2021): Expert Panel Survey to Update the American Congress of Rehabilitation Medicine Definition of Mild Traumatic Brain Injury. Arch Phys Med Rehabil. 102:76–86. [DOI] [PubMed] [Google Scholar]
- 27.Polinder S, Cnossen MC, Real RGL, Covic A, Gorbunova A, Voormolen DC, et al. (2018): A Multidimensional Approach to Post-concussion Symptoms in Mild Traumatic Brain Injury. Frontiers in Neurology. 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Miller H (1966): Mental after-effects of head injury. Proc R Soc Med. 59:257–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Merskey H, Woodforde JM (1972): Psychiatric sequelae of minor head injury. Brain. 95:521–528. [DOI] [PubMed] [Google Scholar]
- 30.Stein MB, McAllister TW (2009): Exploring the convergence of posttraumatic stress disorder and mild traumatic brain injury. American Journal of Psychiatry. 166:768–776. [DOI] [PubMed] [Google Scholar]
- 31.Meares S, Shores EA, Taylor AJ, Batchelor J, Bryant RA, Baguley IJ, et al. (2011): The prospective course of post-concussion syndrome: the role of mild traumatic brain injury. Neuropsychology. 25:454. [DOI] [PubMed] [Google Scholar]
- 32.Ponsford J, Cameron P, Fitzgerald M, Grant M, Mikocka-Walus A (2011): Long-term outcomes after uncomplicated mild traumatic brain injury: a comparison with trauma controls. J Neurotrauma. 28:937–946. [DOI] [PubMed] [Google Scholar]
- 33.Dikmen S, Machamer J, Temkin N (2017): Mild traumatic brain injury: longitudinal study of cognition, functional status, and post-traumatic symptoms. J Neurotrauma. 34:1524–1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McAllister TW (2021): Chicken or Egg? Mental Illness as a Risk Factor and Outcome of Traumatic Brain Injury. Biological Psychiatry. [DOI] [PubMed] [Google Scholar]
- 35.Mayer A (This Issue): Neuroimaging biomarkers of psychiatric disturbance after TBI. Biol Psych. [Google Scholar]
- 36.Meier T, Savitz J (This Issue): The kynurenine pathway in traumatic brain injury. [DOI] [PMC free article] [PubMed]
- 37.Risbrough VB (This Issue): Immune mechanisms of post-TBI psychiatric changes. Biol Psych. [Google Scholar]
- 38.Nelson LD, Tarima S, LaRoche AA, Hammeke TA, Barr WB, Guskiewicz K, et al. (2016): Preinjury somatization symptoms contribute to clinical recovery after sport-related concussion. Neurology. 86:1856–1863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Voormolen DC, Cnossen MC, Polinder S, von Steinbuechel N, Vos PE, Haagsma JA (2018): Divergent Classification Methods of Post-Concussion Syndrome after Mild Traumatic Brain Injury: Prevalence Rates, Risk Factors, and Functional Outcome. J Neurotrauma. 35:1233–1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Biagianti B, Stocchetti N, Brambilla P, Van Vleet T (2020): Brain dysfunction underlying prolonged post-concussive syndrome: A systematic review. J Affect Disord. 262:71–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Montenigro PH, Baugh CM, Daneshvar DH, Mez J, Budson AE, Au R, et al. (2014): Clinical subtypes of chronic traumatic encephalopathy: literature review and proposed research diagnostic criteria for traumatic encephalopathy syndrome. Alzheimers Res Ther. 6:68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Omalu B, Bailes J, Hamilton RL, Kamboh MI, Hammers J, Case M, et al. (2011): Emerging histomorphologic phenotypes of chronic traumatic encephalopathy in American athletes. Neurosurg. 69:173–183; discussion 183. [DOI] [PubMed] [Google Scholar]
- 43.Iverson GL, Gardner AJ (2021): Symptoms of traumatic encephalopathy syndrome are common in the US general population. Brain Commun. 3:fcab001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Katz DI, Bernick C, Dodick DW, Mez J, Mariani ML, Adler CH, et al. (2021): National Institute of Neurological Disorders and Stroke Consensus Diagnostic Criteria for Traumatic Encephalopathy Syndrome. Neurology. 96:848–863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kerr ZY, Marshall SW, Harding HP Jr., Guskiewicz KM (2012): Nine-year risk of depression diagnosis increases with increasing self-reported concussions in retired professional football players. Am J Sports Med. 40:2206–2212. [DOI] [PubMed] [Google Scholar]
- 46.Rice SM, Parker AG, Rosenbaum S, Bailey A, Mawren D, Purcell R (2018): Sport-Related Concussion and Mental Health Outcomes in Elite Athletes: A Systematic Review. Sports Med. 48:447–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Manley G, Gardner AJ, Schneider KJ, Guskiewicz KM, Bailes J, Cantu RC, et al. (2017): A systematic review of potential long-term effects of sport-related concussion. British Journal of Sports Medicine. 51:969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cottler LB, Ben Abdallah A, Cummings SM, Barr J, Banks R, Forchheimer R (2011): Injury, pain, and prescription opioid use among former National Football League (NFL) players. Drug Alcohol Depend. 116:188–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Damasio H, Grabowski T, Frank R, Galaburda A, Damasio A (1994): The return of Phineas Gage: clues about the brain from the skull of a famous patient. Science. 264:1102–1105. [DOI] [PubMed] [Google Scholar]
- 50.Agtarap SD, Campbell-Sills L, Jain S, Sun X, Dikmen S, Levin H, et al. (2021): Satisfaction with Life after Mild Traumatic Brain Injury: A TRACK-TBI Study. J Neurotrauma. 38:546–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zahniser E, Nelson LD, Dikmen SS, Machamer JE, Stein MB, Yuh E, et al. (2019): The Temporal Relationship of Mental Health Problems and Functional Limitations following mTBI: A TRACK-TBI and TED Study. J Neurotrauma. 36:1786–1793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Albrecht JS, Barbour L, Abariga SA, Rao V, Perfetto EM (2019): Risk of Depression after Traumatic Brain Injury in a Large National Sample. J Neurotrauma. 36:300–307. [DOI] [PubMed] [Google Scholar]
- 53.Hammer E, Hetzel S, Pfaller A, McGuine T (2021): Longitudinal Assessment of Depressive Symptoms After Sport-Related Concussion in a Cohort of High School Athletes. Sports Health. 13:31–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Alway Y, Gould KR, Johnston L, McKenzie D, Ponsford J (2016): A prospective examination of Axis I psychiatric disorders in the first 5 years following moderate to severe traumatic brain injury. Psychol Med. 46:1331–1341. [DOI] [PubMed] [Google Scholar]
- 55.Ashman TA, Spielman LA, Hibbard MR, Silver JM, Chandna T, Gordon WA (2004): Psychiatric challenges in the first 6 years after traumatic brain injury: cross-sequential analyses of Axis I disorders. Arch Phys Med Rehabil. 85:S36–42. [DOI] [PubMed] [Google Scholar]
- 56.Gould KR, Ponsford JL, Johnston L, Schönberger M (2011): The nature, frequency and course of psychiatric disorders in the first year after traumatic brain injury: a prospective study. Psychol Med. 41:2099–2109. [DOI] [PubMed] [Google Scholar]
- 57.Bryant RA, O’donnell ML, Creamer M, McFarlane AC, Clark CR, Silove D (2010): The psychiatric sequelae of traumatic injury. American Journal of Psychiatry. 167:312–320. [DOI] [PubMed] [Google Scholar]
- 58.Stein MB, Jain S, Giacino JT, Levin H, Dikmen S, Nelson LD, et al. (2019): Risk of Posttraumatic Stress Disorder and Major Depression in Civilian Patients After Mild Traumatic Brain Injury: A TRACK-TBI Study. JAMA Psychiatry. 76:249–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ponsford J, Alway Y, Gould KR (2018): Epidemiology and Natural History of Psychiatric Disorders After TBI. J Neuropsychiatry Clin Neurosci. 30:262–270. [DOI] [PubMed] [Google Scholar]
- 60.McMahon P, Hricik A, Yue JK, Puccio AM, Inoue T, Lingsma HF, et al. (2014): Symptomatology and functional outcome in mild traumatic brain injury: results from the prospective TRACK-TBI study. J Neurotrauma. 31:26–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Nelson LD, Kramer MD, Joyner KJ, Patrick CJ, Stein MB, Temkin N, et al. (2021): Relationship between transdiagnostic dimensions of psychopathology and traumatic brain injury (TBI): A TRACK-TBI study. J Abnorm Psychol. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ferdosi H, Schwab KA, Metti A, Brenner LA, Terrio H, Pazdan RM, et al. (2018): Trajectory of Post-concussive Symptoms 12 Months After Deployment in Soldiers With and Without Mild Traumatic Brain Injury: Warrior Strong Study. American Journal of Epidemiology. 188:77–86. [DOI] [PubMed] [Google Scholar]
- 63.Bryan CJ, Clemans TA (2013): Repetitive traumatic brain injury, psychological symptoms, and suicide risk in a clinical sample of deployed military personnel. JAMA Psychiatry. 70:686–691. [DOI] [PubMed] [Google Scholar]
- 64.Sbordone RJ, Liter JC (1995): Mild traumatic brain injury does not produce post-traumatic stress disorder. Brain Injury. 9:405–412. [DOI] [PubMed] [Google Scholar]
- 65.Jamora CW, Young A, Ruff RM (2012): Comparison of subjective cognitive complaints with neuropsychological tests in individuals with mild vs more severe traumatic brain injuries. Brain Inj. 26:36–47. [DOI] [PubMed] [Google Scholar]
- 66.Hoge CW, McGurk D, Thomas JL, Cox AL, Engel CC, Castro CA (2008): Mild traumatic brain injury in U.S. Soldiers returning from Iraq. N Engl J Med. 358:453–463. [DOI] [PubMed] [Google Scholar]
- 67.Schneiderman AI, Braver ER, Kang HK (2008): Understanding sequelae of injury mechanisms and mild traumatic brain injury incurred during the conflicts in Iraq and Afghanistan: persistent post-concussive symptoms and posttraumatic stress disorder. American Journal of Epidemiology. 167:1446–1452. [DOI] [PubMed] [Google Scholar]
- 68.Yurgil KA, Barkauskas DA, Vasterling JJ, Nievergelt CM, Larson GE, Schork NJ, et al. (2014): Association between traumatic brain injury and risk of posttraumatic stress disorder in active-duty Marines. JAMA Psychiatry. 71:149–157. [DOI] [PubMed] [Google Scholar]
- 69.Bryant RA (2008): Disentangling mild traumatic brain injury and stress reactions. N Engl J Med. 358:525–527. [DOI] [PubMed] [Google Scholar]
- 70.Tanev KS, Pentel KZ, Kredlow MA, Charney ME (2014): PTSD and TBI comorbidity: scope, clinical presentation and treatment options. Brain Inj. 28:261–270. [DOI] [PubMed] [Google Scholar]
- 71.Elder GA, Dorr NP, De Gasperi R, Gama Sosa MA, Shaughness MC, Maudlin-Jeronimo E, et al. (2012): Blast exposure induces post-traumatic stress disorder-related traits in a rat model of mild traumatic brain injury. J Neurotrauma. 29:2564–2575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wisco BE, Marx BP, Holowka DW, Vasterling JJ, Han SC, Chen MS, et al. (2014): Traumatic brain injury, PTSD, and current suicidal ideation among Iraq and Afghanistan U.S. veterans. J Trauma Stress. 27:244–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Fonda JR, Fredman L, Brogly SB, McGlinchey RE, Milberg WP, Gradus JL (2017): Traumatic Brain Injury and Attempted Suicide Among Veterans of the Wars in Iraq and Afghanistan. Am J Epidemiol. 186:220–226. [DOI] [PubMed] [Google Scholar]
- 74.Madsen T, Erlangsen A, Orlovska S, Mofaddy R, Nordentoft M, Benros ME (2018): Association Between Traumatic Brain Injury and Risk of Suicide. JAMA. 320:580–588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Phillips CJ, LeardMann CA, Vyas KJ, Crum-Cianflone NF, White MR (2017): Risk Factors Associated With Suicide Completions Among US Enlisted Marines. American Journal of Epidemiology. 186:668–678. [DOI] [PubMed] [Google Scholar]
- 76.Campbell-Sills L, Stein MB, Liu H, Agtarap S, Heeringa SG, Nock MK, et al. (2020): Associations of Lifetime Traumatic Brain Injury Characteristics With Prospective Suicide Attempt Among Deployed US Army Soldiers. J Head Trauma Rehabil. 35:14–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Campbell-Sills L, Jain S, Sun X, Fisher LB, Agtarap SD, Dikmen S, et al. (2021): Risk Factors for Suicidal Ideation Following Mild Traumatic Brain Injury: A TRACK-TBI Study. J Head Trauma Rehabil. 36:E30–e39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.McIntire KL, Crawford KM, Perrin PB, Sestak JL, Aman K, Walter LA, et al. (2021): Factors Increasing Risk of Suicide after Traumatic Brain Injury: A State-of-the-Science Review of Military and Civilian Studies. Brain Inj. 35:151–163. [DOI] [PubMed] [Google Scholar]
- 79.American Psychiatric Association (2013): Diagnostic and Statistical Manual of Mental Disorders: DSM-5. Washington, DC: American Psychiatric Association. [Google Scholar]


