Abstract
Introduction
The Coronavirus Disease 2019 (COVID-19) pandemic has impacted breast, colon, prostate, and lung cancer screenings in the U.S. by decreasing screening numbers.We believe multiple types of cancer screenings may have been impacted during the pandemic as a result of cancellations of elective procedures and patient fear of seeking cancer screenings during a pandemic and that Google Trends may be a marker to estimate screening usage.
Methods
Google Trends (trends.google.com) was utilized to assess public interest in multiple cancer types. We then constructed a forecasting model to determine the expected search interest had the pandemic not occurred. We then compared our models to actual screening usage during the pandemic.
Results
Public interest in cancer screenings decreased precipitously at the onset of the COVID-19 pandemic. We found that the Google Trends estimated the decrease in mammogram usage 25.8% below the actual value. Similarly, Google Trends estimated the decrease in colon cancer screening usage 9.7% below the true value.
Discussion
We found the decrease in public interest in breast and colon cancer screenings slightly underestimated the actual screening usage numbers, suggesting Google Trends may be utilized as an indicator for human behavior regarding cancer screening, particularly with colon and breast cancer screenings. If the negative trend in cancer screening continues and missed screenings are not appropriately corrected for, socioeconomic and racial disparities in cancer diagnoses, morbidity, and mortality will widen.
Keywords: Public interest, Cancer screenings, Google Trends, Screening usage
Introduction
Cancer was the second leading cause of mortality in the United States in 2019 leading to approximately 606,000 deaths.1 With 1.7 million new diagnoses annually,1 the overall cancer burden continues to represent a public health crisis1; however, screening is effective for detecting and decreasing cancer morbidity and mortality.
Several studies have found that the Coronavirus Disease 2019 (COVID-19) pandemic has impacted breast, colon, prostate, and lung cancer screenings in the U.S. by decreasing screening numbers.2 , 3 We believe multiple types of cancer screenings may have been impacted during the pandemic as a result of cancellations of elective procedures and patient fear of seeking cancer screenings during a pandemic and that Google Trends may be a marker to estimate screening usage. Our primary objective was to assess how COVID-19 affected public interest in mammography, colonoscopy, human papillomavirus (HPV), and papanicolaou tests. We used Google Trends to analyze public interest in cancer screenings as Schootman et al found weak to moderate associations with public interest in cancer screenings and actual screening usage, suggesting it may be an indicator of screening although not a true surrogate for screening usage.4 Our secondary objective was to assess the efficacy of using public interest in cancer screenings, determined by Google Trends, as an indicator of actual screening usage.
Methods
Google Trends (trends.google.com) was utilized to assess public interest in the following search queries between September 6, 2015 and August 30, 2020: “colonoscopy,” “mammogram,” “HPV,” and “pap smear.” This timeline was chosen to best approximate weekly fluctuations in search interest. Google Trends calculates relative search interest (RSI) on a scale of 0-100 with 100 representing peak interest. To analyze expected search interest had COVID-19 not occurred, we forecasted predictive models using autoregressive interactive moving average algorithms in R (version 4.0.2). To assess our secondary objective, we computed the difference in screening usage predicted by our study to that of Patt et al which calculated actual screening usage.
Results
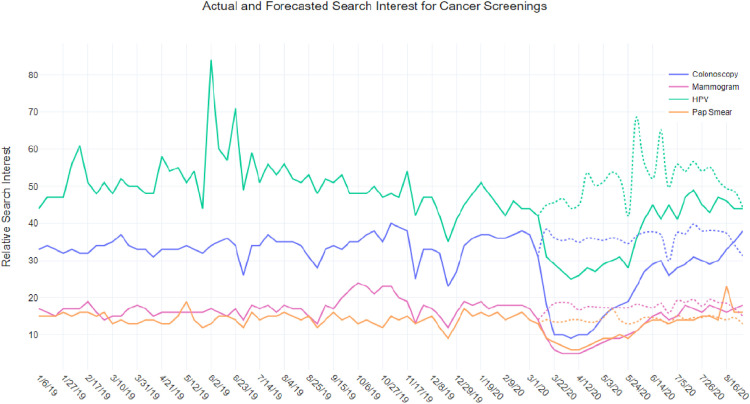
Following the onset of the COVID-19 pandemic within the U.S. (March), RSI for “colonoscopy”, “mammogram”, “HPV”, and “pap smear” sharply declined followed by a slow uptrend to baseline near the end of May. Between March 14 and May 17 of 2020, RSI for “HPV” had a mean difference of -19.96; an average percent change of -40.47% below the forecasted value. “Colonoscopy” RSI showed a mean difference of -57.17; -64.33% below expected. “Mammogram” RSI had a mean difference of -40.46; -59.2% below expected. Finally, RSI for “pap smear” showed a mean difference of -26.83; -43.66% below the forecasted value. Fig. 1 shows all trendlines of cancer screenings and their forecasted values from January 2019 through August 2020.
Fig. 1.
Actual search interest for "colonoscopy," "mammogram," "HPV," and "Pap Smear" is shown as the solid line. Forecasted (expected) search interest for the cancer screenings is shown as the dotted line. (Color version of figure is available online.)
Comparing our results to Patt et al, a nationally representative sample of the U.S. Medicare population, found that the Google Trends estimated the decrease in mammogram usage 25.8% below the actual value. Similarly, Google Trends estimated the decrease in colon cancer screening usage 9.7% below the true value. The comparator study did not assess cervical cancer screening usage.
Discussion
Our study identified a sharp decline in public interest related to colonoscopies, mammography, HPV, and pap smears corresponding with the onset of COVID-19 followed by a slow uptrend to baseline near the end of May. The decrease in public interest was greatest for colonoscopies and mammography. Second, we found the decrease in public interest in breast and colon cancer screenings slightly underestimated the actual screening usage numbers, suggesting Google Trends may be utilized as an indicator for human behavior regarding cancer screening, particularly with colon and breast cancer screenings. Our findings suggest that there is a large population in need of cancer screenings to reduce the fallout of delayed or missed cancer diagnoses.
Cancer screening is known to reduce morbidity and mortality; between 1970 and 2016, colorectal cancer screening and improved treatments reduced mortality by 53%.1 Comparably in pap smears and the use of HPV testing, mortality rates from cervical cancers have declined in the United States from 3.5 to 2.2 per 100,000 between 1992 and 2017.5 Unfortunately, the projected incidence and mortality rates due to cancer will likely rise due to reduced cancer screening access and public fear during and following the pandemic. It is possible that public interest in cancer screenings returned to baseline at the end of May 2020 as patients became accustomed to utilizing telehealth visits to discuss screening options which were not previously widely used. Another possible reason is that individuals were spending time searching for COVID-19 rather than cancer screening information when the pandemic began due to it being a new and previously unheard of topic that caught readers’ attention. Alternatively, the decrease in interest may have been related to the lack of ability to schedule screening services even for patients who were motivated to get screened at the beginning of the pandemic.
This study had several strengths and limitations. First, although Google is the most widely used search engine for patients seeking online health information,6 it is possible that our use of Google Trends did not accurately assess true interest in cancer screenings. Second, this was a cross-sectional study; therefore, causation for the decrease in public interest cannot be attributed solely to the COVID-19 pandemic. Alternatively, the study strengths included the robust data extracted through Google Trends as well as the use of 5 years of previous data in calculating accurate forecasting models.
Although Google Trends underestimated the decrease in actual cancer screenings, it may be a viable and cheap option to use in the future when assessing cancer screening usage. If the negative trend in cancer screening continues and missed screenings are not appropriately corrected for, socioeconomic and racial disparities in cancer diagnoses, morbidity, and mortality will widen. Therefore, we recommend physicians in both primary care and oncology settings seek out high cancer risk patients and aggressively make efforts to attenuate this disparity. Solutions for improving cancer screening compliance during the pandemic include fecal immunochemical testing, telemammography, and preferentially performing pap smears with HPV cotesting in high-risk patients.7 , 8 Furthermore, public health initiatives and community efforts should be implemented to increase screening compliance during this pandemic.
Credit author statement
Benjamin Greiner: Conceptualization, methodology, data curation, writing original draft, reviewing final draft, and supervision. Shelby Tipton: Conceptualization, writing original draft, reviewing/editing final draft. Blessie Nelson: Conceptualization, writing original draft, reviewing/editing final draft. Micah Hartwell: Supervision, visualization, methodology, formal analysis, writing, and reviewing/editing of final draft.
Footnotes
Role of Funding Source: This study was not funded.
Conflict of Interest: We declare no conflicts of interest.
References
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69:7–34. doi: 10.3322/caac.21551. [DOI] [PubMed] [Google Scholar]
- 2.Parikh KD, Ramaiya NH, Kikano EG, et al. COVID-19 pandemic impact on decreased imaging utilization: a single institutional experience. Acad Radiol. 2020;27:1204–1213. doi: 10.1016/j.acra.2020.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Patt D, Gordan L, Diaz M, et al. Impact of COVID-19 on cancer care: how the pandemic is delaying cancer diagnosis and treatment for American seniors. JCO Clin Cancer Inform. 2020;4:1059–1071. doi: 10.1200/CCI.20.00134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schootman M, Toor A, Cavazos-Rehg P, et al. The utility of Google Trends data to examine interest in cancer screening. BMJ Open. 2015;5 doi: 10.1136/bmjopen-2014-006678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cancer of the Cervix Uteri - Cancer Stat Facts. Accessed September 12, 2020. https://seer.cancer.gov/statfacts/html/cervix.html.
- 6.Cocco AM, Zordan R, Taylor DM, et al. Dr Google in the ED: searching for online health information by adult emergency department patients. Med J Aust. 2018;209:342–347. doi: 10.5694/mja17.00889. https://www.ncbi.nlm.nih.gov/pubmed/30107763 [DOI] [PubMed] [Google Scholar]
- 7.Dockter AG, Angelos GC. Molecular-based alternatives for colorectal cancer screening during the COVID-19 pandemic. Surg Technol Int. 2020;36:143–147. https://www.ncbi.nlm.nih.gov/pubmed/32347964 [PubMed] [Google Scholar]
- 8.Seely JM, Scaranelo AM, Yong-Hing C, et al. COVID-19: safe guidelines for breast imaging during the pandemic. Can Assoc Radiol J. 2020;71(4):459–469. doi: 10.1177/0846537120928864. Published online May 26846537120928864. [DOI] [PubMed] [Google Scholar]