Abstract
Objective:
To estimate the prevalence of pregnancy-associated deaths due to drugs, suicide, and homicide nationwide from 2010 to 2019.
Methods:
Using U.S. death certificate records from 2010 to 2019 for 33 states plus the District of Columbia, we identified pregnancy-associated deaths using the pregnancy checkbox and ICD-10 codes, calculated pregnancy-associated death ratios, and categorized deaths by cause, timing relative to pregnancy, race or ethnicity, and age.
Results:
Of 11,782 pregnancy-associated deaths identified between 2010–2019, 11.4% were due to drugs, 5.4% were due to suicide, and 5.4% were due to homicide, whereas 59.3% were due to obstetric causes and the remaining 18.5% were due to other causes. Drug-related deaths, suicide, and homicide accounted for 22.2% of pregnancy-associated deaths. All three causes of death increased over the study period, with drug-related pregnancy-associated deaths increasing 190%. Homicide during pregnancy and drug-related deaths, suicides, and homicide in the late postpartum period (43 to 365 days) accounted for a larger proportion of all deaths in these time periods than the contribution of these causes to all deaths among women of reproductive age. Pregnant and postpartum people identified as non-Hispanic American Indian or Alaska Native were at highest risk of drug-related and suicide death, whereas people identified as non-Hispanic Black were at highest risk of homicide.
Conclusions:
Deaths due to drug use, suicide, and homicide constitute over one-fifth of all deaths during pregnancy and the first year postpartum. Drug-related deaths and homicides have increased over the past decade. Substantial racial and ethnic inequities in these deaths exist.
Precis
Drug-related deaths, suicide, and homicide accounted for 22% of pregnancy-associated deaths in the United States from 2010 through 2019, with drug-related deaths increasing almost two-fold over that period.
Introduction
In the United States, pregnant and birthing persons die at a higher rate (>20 per 100,000 live births) than in other high-income countries (1), and this rate has increased by an estimated 27% from 2000 to 2014 (2). Reducing these deaths has thus become a public health and clinical priority, and substantial research, public health, and quality improvement efforts now focus on reducing the primary causes of pregnancy-related mortality, including hemorrhage, hypertension, and venous thromboembolism (Box 1) (3–5). However, recent evidence from several states suggests that drug use (illicit or prescription), suicide, and homicide, which are not typically included in estimates of maternal or pregnancy-related mortality (6)—but which fall under the broader definition of pregnancy-associated (Box 1) mortality—are prevalent and increasing causes of death during pregnancy and the first year postpartum (7–12).
Box 1. Definitions of Key Terms.
Maternal death (1): Female death from any cause related to or aggravated by pregnancy or its management (excluding accidental or incidental causes) during pregnancy and childbirth or within 42 days of termination of pregnancy, irrespective of the duration and site of the pregnancy.
Pregnancy-related death (31): Death of a woman while pregnant or within one year of the end of a pregnancy from any cause related to or aggravated by the pregnancy or its management.
Pregnancy-associated death (31): Death of a woman while pregnant or within one year of the end of a pregnancy from any cause.
To date, few national estimates of the burden of pregnancy-associated deaths due to drugs, suicide, or homicide exist. Wallace and colleagues have provided some of the only national estimates of mortality during pregnancy and postpartum due to homicide, suicide, and injury using death certificates from 2005 to 2010, including a range of estimates adjusted for underreporting (9). Our objective was to estimate pregnancy-associated mortality ratios (i.e., deaths per 100,000 live births) in the United States overall and those attributable to drug use, suicide, and homicide from 2010 to 2019 and compare this to mortality among non-pregnant or postpartum women of reproductive age.
Methods
We used U.S. death certificate records from 2010 to 2019, with state identifiers obtained from the National Center for Health Statistics. We obtained the count of live births in each state for each year overall and by race and ethnicity from the Centers for Disease Control and Prevention WONDER database. Race was included in our study because prior research indicates substantial disparities in pregnancy-associated death by race and ethnicity (9,10). We emphasize that race is not a biological variable, but a social construct. To create a comparison group of women of reproductive age, we restricted our study population to deaths identified as female and between the ages of 15–44 years old, acknowledging that we have excluded birthing persons identified as male on the death certificate. We only included data from states (and the District of Columbia [DC]) that had adopted the 2003 Revised Death Certificate by January 1, 2010 (AR, AZ, CT, DC, DE, FL, GA, ID, IL, IN, KS, MI, MO, MT, ND, NE, NH, NJ, NM, NV, NY, OH, OK, OR, RI, SC, SD, TX, UT, VT, WA, WY) because the revised death certificate includes the standard pregnancy check-box (see the next paragraph). To include as much of the U.S. birthing population as possible, we also included data from Maryland, where the unrevised death certificate was used throughout the study period and includes a pregnancy checkbox that identifies timing of death relative to pregnancy in the same way as the standard pregnancy check-box, and California, where the unrevised death certificate asks only if the decedent was pregnant in the last year. Thus, we included data from 33 states plus DC for a total of 28,856,437 live births.
We defined pregnancy-associated deaths as deaths during or within 1 year of pregnancy using two sources of information to capture as many pregnancy-associated deaths as possible. The 2003 Revised Death Certificate contains a standardized pregnancy checkbox that asks whether the decedent fell into one of the following categories: 1) not pregnant within last year, 2) not pregnant but pregnant within 42 days of death, 3) not pregnant but pregnant 43 days to 1 year before death, 4) pregnant at time of death, 5) unknown if pregnant within past year. We considered any death as ‘pregnancy-associated’ if categories 2, 3, or 4 were checked. We also coded deaths with ICD-10 codes associated with death from obstetric causes (A34 [obstetrical tetanus] and 000–099 [pregnancy, childbirth, and the puerperium]), including late maternal deaths, as pregnancy-associated death. We further classified pregnancy-associated death into causes of death based on ICD-10 codes indicating obstetric causes, drug-related causes (unintentional or of undetermined intent), suicide, homicide, and other causes. (See Appendix 1, available online at http://links.lww.com/xxx, for ICD-10 codes.) All remaining deaths to females 15–44 were considered not pregnant or postpartum.
We categorized the race or ethnicity of the decedent as indicated on the death certificate into 5 groups, following the Office of Management and Budget classifications: non-Hispanic American Indian or Alaska Native, non-Hispanic Asian or Pacific Islander, non-Hispanic Black, Hispanic, non-Hispanic White. If the certificate indicated Hispanic ethnicity, the death was categorized as Hispanic, regardless of race or ethnicity (15). We also categorized age (<20, 20–24, 25–29, 30–34, ≥35), educational attainment (<high school, high school diploma, some college, ≥Bachelor’s degree, or unknown), and marital status (married or not married) of the decedent. Timing of pregnancy-associated death is reported using the pregnancy checkbox and was classified as: pregnant at the time of death, pregnant 1–42 days before death, or pregnant 43–365 days before death; the specific timing of pregnancy-associated death is not available for deaths in California. For obstetric deaths identified by ICD-10 code alone (i.e., no pregnancy checkbox), we followed Wallace et al. (8) in classifying timing of these deaths using ICD-10 code when possible (Appendix 2, available online at http://links.lww.com/xxx).
To compare pregnancy-associated death to death among women of reproductive age, we examined the number and proportion of all deaths stratified by whether the decedent was not pregnant or postpartum at the time of death, pregnant at the time of death, not pregnant at the time of death but pregnant within 42 days of death, pregnant within 43–365 days prior to death, or pregnant within a year of death but with unknown timing, overall and by age, race or ethnicity, educational attainment, marital status, and cause of death. These calculations excluded deaths in California, for which we did not have data on specific timing of death relative to pregnancy information.
We calculated the pregnancy-associated death ratio by year for each cause and generated 95% confidence intervals for pregnancy-associated death ratios assuming a chi-squared distribution: To compare pregnancy-associated death ratios at the start of the study period (2010) to the end (2019), we used the incidence rate (ir) command in stata to calculate rate ratios (RRs) and 95% confidence intervals (CIs).
We also calculated the proportion of deaths due to drug-related causes, suicide, homicides, and obstetric causes occurring during pregnancy, in the first 42 days postpartum, and within 43–365 days postpartum. We then calculated the number of pregnancy-associated deaths and pregnancy-associated death ratios by age category and race or ethnicity, as prior research indicates substantial disparities in pregnancy-associated death by these factors (9,10). We calculated RRs and 95% CIs using the incidence rate command in stata. We chose the referent group as the group with the largest number of births (ages 25–29 and non-Hispanic White).
To account for under-reporting of pregnancy-associated death on the death certificate, we relied on one of the few published studies that quantifies the magnitude of under-reporting by cause of death. Specifically, Horon and Cheng (16) used Maryland death certificate data from 2001 to 2008 to combined with a comprehensive review of medical records and a linkage to birth and fetal death certificate to identify pregnancy-associated deaths due to a variety of causes. The authors then calculated the proportion of these pregnancy-associated deaths (overall and by cause) that were identified on the death certificate. The authors found that 35.1%, 42.9%, and 42.5% of pregnancy-associated deaths due to substance use, suicide, and homicide, respectively, were reported as such on the death certificate. We used these proportions (p) and built on the procedure developed by Wallace and colleagues (9) to calculate the expected pregnancy-associated death ratio for drug-related deaths, suicide, and homicide, assuming that these proportions were applied to our data. We used the following equation, where p is the proportion of deaths due to cause c identified from the death certificate alone and yields the expected number of ‘true’ deaths due to cause c if only p of those deaths are marked as such on the death certificate.
We conducted robustness checks excluding the two states that did not adopt the 2003 Revised Death Certificate by January 1, 2010, i.e., California and Maryland. We also conducted an analysis excluding women over the age of 40 because prior research finds plausible overreporting of maternal deaths among this age group (17). Finally, we considered a definition of suicide where we assigned ICD-10 codes Y10-Y19 (poisoning deaths of undetermined intent) as suicide instead of drug-related.
This research was approved by the Institutional Review Board at Michigan State University. Analyses were conducted using Stata MP.
Results
We identified 11,782 pregnancy-associated deaths from 2010 to 2019 using U.S. death certificate data for all 33 states plus DC. Of these deaths, 11,354 (96.4%) were identified using the pregnancy checkbox, and an additional 428 (3.6%) were identified using ICD-10 codes. The majority of deaths (6,561 or 55.7%) had both the pregnancy checkbox and an obstetric ICD-10 code.
Of people who died during pregnancy, 54.6% died due to maternal or obstetric causes, 10.5% due to drug-related causes, 4.9% due to suicide, and 8.0% due to homicide (Table 1 and Appendix 3, available online at http://links.lww.com/xxx). In comparison, over three-quarters of deaths within 42 days postpartum were due to maternal or obstetric causes. During the late postpartum period (43–365 days postpartum), drug-related deaths and suicide made up 17.0% and 8.3%, respectively, of all deaths, compared to 16.5% and 8.1% of all deaths to women of reproductive age. Moreover, homicide accounted for 8.0% of all deaths during pregnancy and 5.9% of deaths in the late postpartum period, compared to 3.4% of deaths to women of reproductive age. The number and proportion of all deaths to females 15–44 stratified by timing relative to pregnancy and by age, race or ethnicity, educational attainment, and marital status is presented in Appendix 2, http://links.lww.com/xxx.
Table 1.
Number and percent of deaths by cause to females of reproductive age (15–44 years) overall and by timing relative to pregnancy in 32 US states and the District of Columbia, 2010–2019.
| All female deaths ages 15–44 | Timing relative to pregnancy | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Not pregnant or postpartum | Pregnant at time of death | Pregnant within 42 days of death | Pregnant 43–365 days before death | Pregnant within a year, but exact timing unknown* | ||||||||
| Cause of death | n | % | n | % | n | % | n | % | n | % | n | % |
| Drug-Related | 52047 | 16.5 | 50789 | 16.7 | 432 | 10.5 | 242 | 8.5 | 584 | 17.0 | 0 | 0.0 |
| Suicide | 25,492 | 8.1 | 24,934 | 8.2 | 202 | 4.9 | 72 | 2.5 | 284 | 8.3 | 0 | 0.0 |
| Homicide | 10,824 | 3.4 | 10,248 | 3.4 | 327 | 8.0 | 48 | 1.7 | 201 | 5.9 | 0 | 0.0 |
| Obstetric | 6,244 | 2.0 | -- | 0.0 | 2,241 | 54.6 | 2,161 | 76.0 | 1,628 | 47.5 | 214 | 100.0 |
| Other causes | 220932 | 70.0 | 218977 | 71.8 | 903 | 22.0 | 322 | 11.3 | 730 | 21.3 | 0 | 0.0 |
| Total | 315,539 | 100 | 304,948 | 100 | 4,105 | 100 | 2,845 | 100 | 3,427 | 100 | 214 | 100 |
Deaths identified by ICD-10 codes associated with death from obstetric causes, but without substantial information to assign timing
Of the 11,782 pregnancy-associated deaths from 2010 to 2019, 11.4% were due to drugs, 5.4% were due to suicide, and 5.4% were due to homicide, whereas 59.3% were due to obstetric causes and 18.5% were due to other causes (Table 2). For the entire period of 2010–2019, the pregnancy-associated death ratio due to drug-related causes was 4.7/100,000 live births (95% confidence interval [CI]: 4.4–4.9). For both suicide and homicide, the pregnancy-associated death ratio was 2.2/100,000 live births (Table 1) (95% CI: 2.2–2.4 for both).
Table 2.
Number of pregnancy-associated deaths by cause and year, pregnancy-associated death ratios by cause, and percent of all deaths by cause in 33 US states and the District of Columbia, 2010–2019.
| Pregnancy-associated deaths | ||||||||
|---|---|---|---|---|---|---|---|---|
| Measure | Drug-Related | Suicide | Homicide | Obstetric | Other | Total | Number of births | |
| Number of deaths | ||||||||
| Year | ||||||||
| 2010 | 80 | 56 | 54 | 618 | 263 | 1071 | 2,954,034 | |
| 2011 | 108 | 65 | 56 | 679 | 269 | 1177 | 2,914,824 | |
| 2012 | 83 | 53 | 44 | 660 | 182 | 1022 | 2,915,408 | |
| 2013 | 97 | 57 | 65 | 728 | 213 | 1160 | 2,898,700 | |
| 2014 | 99 | 71 | 54 | 716 | 227 | 1167 | 2,943,675 | |
| 2015 | 121 | 63 | 45 | 686 | 242 | 1157 | 2,936,361 | |
| 2016 | 155 | 66 | 77 | 718 | 189 | 1205 | 2,911,965 | |
| 2017 | 184 | 49 | 81 | 711 | 203 | 1228 | 2,838,136 | |
| 2018 | 206 | 85 | 78 | 703 | 224 | 1296 | 2,789,355 | |
| 2019 | 216 | 69 | 82 | 770 | 162 | 1299 | 2,753,979 | |
| All years | 1349 | 634 | 636 | 6989 | 2174 | 11782 | 28,856,437 | |
| Pregnancy-associated death ratio* | 4.7 | 2.2 | 2.2 | 24.2 | 7.5 | -- | -- | |
| Percent of all deaths | 11.4% | 5.4% | 5.4% | 59.3% | 18.5% | -- | -- | |
Pregnancy-associated death ratio =
The pregnancy-associated death ratio due to drug-related causes rose 190% from 2.7/100,000 in 2010 to 7.8/100,000 in 2019 (Figure 1) (RR: 2.9, 95% CI: 2.2–3.8). The pregnancy-associated death ratio due to suicide increased approximately 30% from 2010 to 2019 from 1.9/100,000 to 2.5/100,000, but this increase was not statistically significant (RR: 1.3, 95% CI: 0.9–1.9). The homicide pregnancy-associated death ratio increased 63% (RR: 1.6, 95% CI: 1.1–2.3) from 1.8/100,000 to 3.0/100,000 in 2019.
Figure 1.
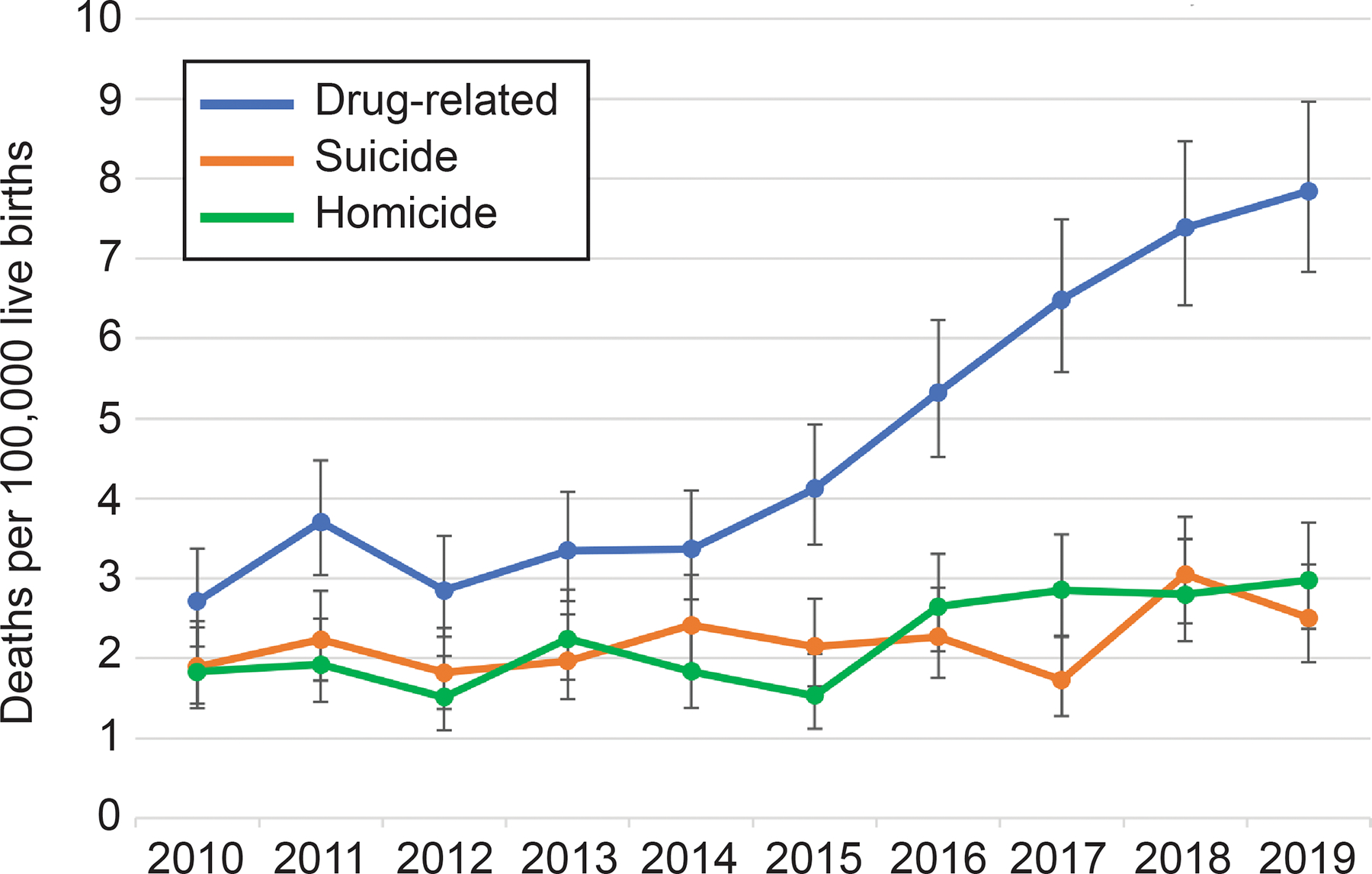
Pregnancy-associated death ratios and 95% CIs for drug-related deaths, suicide, and homicide in 33 U.S. states and the District of Columbia, 2010 to 2019. The pregnancy-associated death ratio due to drug-related causes rose 190% from 2.7/100,000 in 2010 to 7.8/100,000 in 2019 (RR: 2.9, 95% CI: 2.2–3.8). The pregnancy-associated death ratio due to suicide increased approximately 30% from 2010–2019 from 1.9/100,000 to 2.5/100,000, but this increase was not statistically significant (RR: 1.3, 95% CI: 0.9–1.9). The homicide pregnancy-associated death ratio increased 63% (RR: 1.6, 95% CI: 1.1–2.3) from 1.8/100,000 to 3.0/100,000 in 2019.
For deaths due to drug-related causes, 34.3% occurred during pregnancy, 19.2% occurred in the first 42 days postpartum, and 46.4% occurred between 43–365 days postpartum. For deaths due to suicide, these percentages were 36.2, 12.9, and 50.9, respectively, and for homicides, the percentages were 56.8, 8.3, and 34.9. For obstetric causes of deaths, the percentages were 35.9, 35.0, and 26.1, with 3.4% having unknown timing. (Figure 2)
Figure 2.
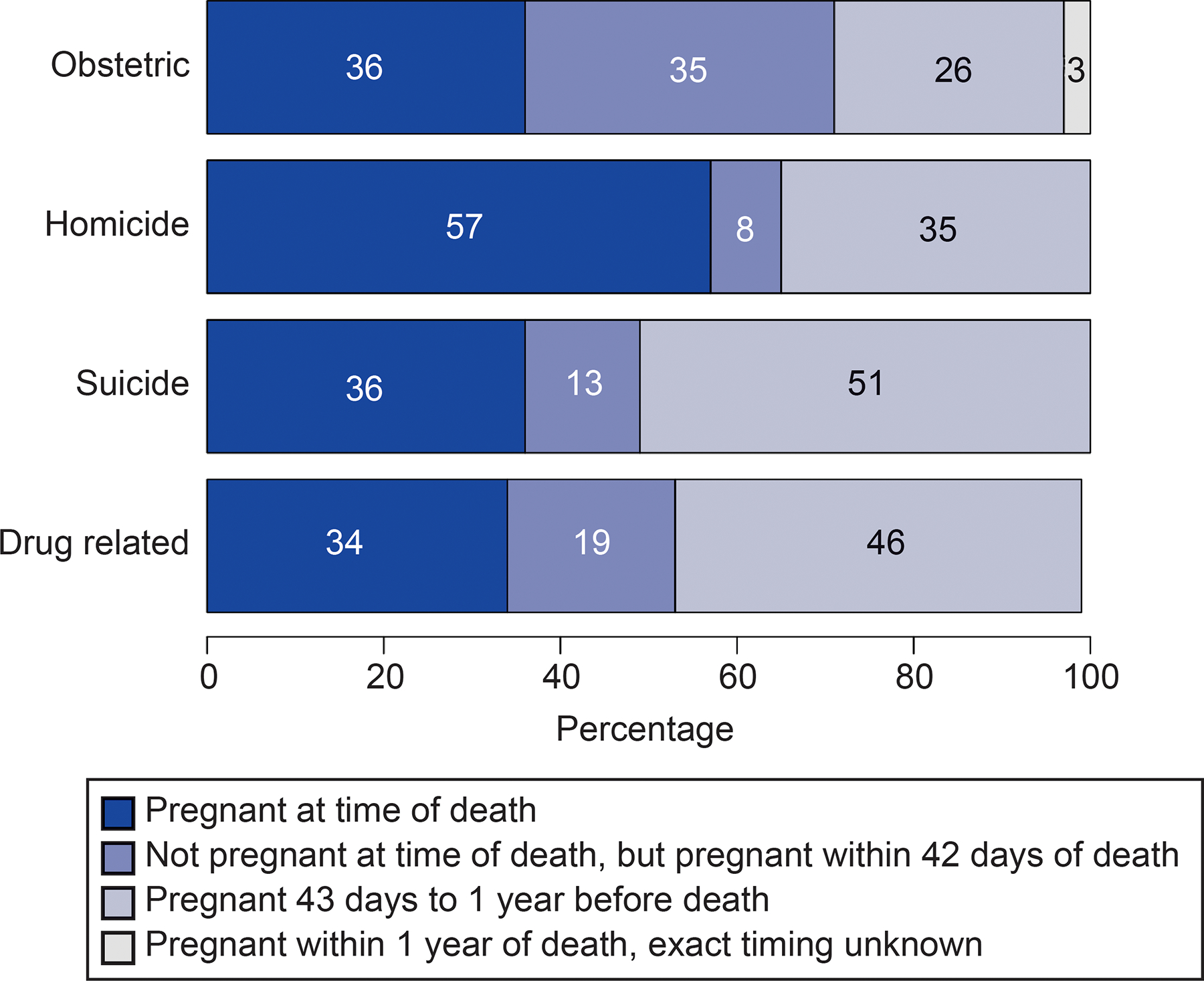
Percentage of cause-specific pregnancy-associated deaths by timing relative to pregnancy in 32 U.S. states* and the District of Columbia, 2010 to 2019. *California data not included in this figure due to lack of specificity of timing relative to pregnancy.
The pregnancy-associated death ratio for drug-related causes was highest among decedents identified as Non-Hispanic American Indian or Alaska Native (10.1/100,000), followed by Non-Hispanic White (7.2/100,000), and Non-Hispanic Black (3.4/100,000) (Table 3). The pregnancy-associated death ratio for suicide was also highest among decedents identified as non-Hispanic American Indian or Alaska Native (7.7/100,000), followed by Non-Hispanic White (2.8/100,000), and Non-Hispanic Asian and Pacific Islander (2.0/100,000). Homicide was most prevalent among Non-Hispanic Black decedents (7.0/100,000), followed by Non-Hispanic American Indian or Alaska Native (2.1/100,000).
Table 3.
Pregnancy-associated deaths due to drugs, homicide, and suicide by race and ethnicity and age: counts, pregnancy-associated mortality rate, and rate ratios in 33 US states and the District of Columbia, 2010 to 2019.
| Drug-related | Suicide | Homicide | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Count | Pregnancy-associated death ratio* | Rate ratio† | 95% CI | Count | Pregnancy-associated death ratio* | Rate ratio† | 95% CI | Count | Pregnancy-associated death ratio* | Rate ratio† | 95% CI | |
| Race or ethnicity | ||||||||||||
| Hispanic | 129 | 1.6 | 0.2 | 0.2–0.3 | 105 | 1.3 | 0.5 | 0.4–0.6 | 127 | 1.6 | 1.1 | 0.9–1.4 |
| Non Hispanic American Indian or Alaska Native | 29 | 10.1 | 1.4 | 0.9–2.0 | 22 | 7.7 | 2.8 | 1.7–4.2 | <10 | 2.1 | 1.4 | 0.5–3.1 |
| Non Hispanic Asian or Pacific Islander | 12 | 0.6 | 0.1 | 0.0–0.1 | 42 | 2.0 | 0.7 | 0.5–1.0 | <10 | 0.2 | 0.2 | 0.1–0.4 |
| Non Hispanic Black | 140 | 3.4 | 0.5 | 0.4–0.6 | 64 | 1.6 | 0.6 | 0.4–0.7 | 285 | 7.0 | 4.8 | 4.0–5.7 |
| Non Hispanic White | 1039 | 7.2 | Referent | 401 | 2.8 | Referent | 213 | 1.5 | Referent | |||
| Age (years) | ||||||||||||
| 15–19 | 34 | 1.8 | 0.4 | 0.2–0.5 | 64 | 3.5 | 1.9 | 1.4–2.5 | 90 | 4.9 | 2.5 | 1.9–3.3 |
| 20–24 | 261 | 4.3 | 0.8 | 0.7–1.0 | 146 | 2.4 | 1.3 | 1.0–1.6 | 226 | 3.7 | 1.9 | 1.5–2.3 |
| 25–29 | 427 | 5.2 | Referent | 152 | 1.8 | Referent | 160 | 1.9 | Referent | |||
| 30–34 | 334 | 4.3 | 0.8 | 0.7–1.0 | 136 | 1.7 | 0.9 | 0.7–1.2 | 97 | 1.2 | 0.6 | 0.5–0.8 |
| ≥ 35 | 293 | 6.1 | 1.2 | 1.0–1.4 | 136 | 2.9 | 1.5 | 1.2–2.0 | 63 | 1.3 | 0.7 | 0.5–0.9 |
Count per 100,000 live births in that racial and ethnic group from 2010 to2019.
Rate ratio = Pregnancy-associated death ratio in group divided by pregnancy-associated death ratio in reference group
CI: Confidence interval
Drug-related deaths were most common among people ages ≥35 (6.1/100,000), followed by those 25–29 (5.2/100,000) and those 20–24 and 30–34 (4.3/100,000 (Table 3)). Suicide was most common among people in the youngest age category (15–19, pregnancy-associated death ratio: 3.5/100,000), followed by ≥35 (2.9/100,000) and 20–24 (2.4/100,000). The pregnancy-associated death ratio for homicide was highest among people aged 15–19 (4.9/100,000), followed by those aged 20–24 (3.7/100,000).
When applying the Horon and Cheng (16) estimated proportion of ‘true’ pregnancy-associated deaths identified by the death certificate to our data, we found that the pregnancy-associated death ratio per 100,000 for drug-related causes would be 13.0 (vs. 4.7 in the observed data); for suicide, the pregnancy-associated death ratio would be 5.1 (vs. 2.2); and for homicide, the pregnancy-associated death ratio would be 5.2 (vs. 2.2) (Appendix 4, available online at http://links.lww.com/xxx). If we add the misclassified deaths due to these causes to the total 11,782 deaths found based on the death certificate, there would be a total of 15,895 pregnancy-associated deaths. Of these, drug-related deaths would account for 23.6%, suicide for 9.3%, and homicide for 9.4%, compared to the percentages calculated from the observed data of 11.4, 5.4, and 5.4 (Table 2).
Compared to our main analyses, when we excluded California and Maryland, we found slightly higher pregnancy-associated death ratios due to drugs, suicide, and homicide, and when excluding women over 40 years, we found slightly smaller pregnancy-associated death ratios for drug-related deaths, suicides, and homicides (Appendixes 5 and 6, available online at http://links.lww.com/xxx). When we assigned ICD-10 codes Y10-Y19 (poisoning deaths of undetermined intent) as suicide instead of drug-related, the pregnancy-associated mortality ratio due to suicide changed from 2.2 to 2.5 per 100,000 live births, and the ratio due to drug-related causes changed from 4.7 to 4.4 per 100,000 live births (Appendix 7, available online at http://links.lww.com/xxx).
Discussion
Using U.S. death certificate records from 2010 to 2019 from 33 states and the District of Columbia, we found that drug-related deaths, suicide, and homicide accounted for 22.2% of all deaths during pregnancy and the first year after pregnancy (i.e., pregnancy-associated death). All three causes of death increased over the study period, with drug-related pregnancy-associated death increasing 190%.
Approximately half of all drug-related and suicide deaths occurred between 6 weeks and one year postpartum and another 20% of drug-related deaths occurred during the first 6 weeks postpartum, consistent with reports from Utah (8) and Massachusetts (12). Indeed, drug-related and suicide deaths account for a larger proportion of deaths between 43 and 365 days postpartum than among all deaths to women of reproductive age. The high risk of drug-related and suicide death in the late postpartum period may be due to lack of continuous postpartum care, lack of specialized mental health and substance use services, increasing stress of caring for a newborn, lack of structural supports (e.g., stable housing), stigma or fear of punitive consequences, hormonal changes, and decreased tolerance after abstinence during pregnancy (18,19). Pregnancy-associated homicides, on the other hand, occurred disproportionately during pregnancy (56.8%), and homicide made up a substantially larger share of deaths during pregnancy (8.0%) than among all women of reproductive age (3.4%).
These data also demonstrate unacceptable racial and ethnic inequities in pregnancy-associated deaths. Pregnant and birthing people identified as American Indian or Alaska Native had much higher rates of drug-related death and suicide compared to all other racial or ethnic groups. Non-Hispanic White people had the second highest rates of pregnancy-associated drug and suicide death. Non-Hispanic Asian and Pacific Islander people, who had the lowest pregnancy-associated death ratio for both drug-related deaths and homicide, had the third highest ratio for suicide. Non-Hispanic Black people had disproportionately high pregnancy-associated death ratios due to homicide, consistent with data from 2005 to2010 (9). Pregnancy-associated drug-related deaths were most common among those ≥35 years, while suicide and homicide were most common among youngest birthing people.
Our findings are consistent with those of Wallace and colleagues, who used death certificate data from 2005 to 2010 and reported a pregnancy-associated suicide mortality ratio of 1.6/100,000 live births and a homicide ratio of 2.2/100,000 live births (9). Our study indicates that these pregnancy-associated death ratios have increased over time, and in 2019, were 2.5 and 3.0, respectively. Our findings also comport with those of Gemmill and colleagues, who identified increases in opioid-related deaths during pregnancy and postpartum using national death certificate data from 2010 to 2016, with particularly steep increases from 2014 to 2016 (20). Our study builds on this previous research by using the most recent 10 years of national data available, by estimating mortality due to all drug types, and by examining disparities among multiple racial or ethnic and age groups and trends over time from 2010 to 2019, a key time period during which the U.S. experienced the Great Recession, declines in fertility rates (14), and an escalating opioid epidemic (13). Our findings are also congruent with those from in-depth maternal mortality reviews of pregnancy-related deaths conducted in 14 states (21), which found that pregnancy-related deaths due to mental health conditions were particularly common among non-Hispanic white people and during the late postpartum period. This study also found that 100% of these mental-health related deaths were considered preventable (21).
We also demonstrate that the contribution of drug-related deaths, suicide, and homicide to overall pregnancy and postpartum mortality is likely much higher than our unadjusted estimates due to under-use of the pregnancy checkbox for these causes of death. After adjustment for under-reporting, these deaths may account for over 40% of all pregnancy-associated deaths (compard to 22.2%). We note that the data used in this study were not collected explicitly for this purpose. Because only one study—using Maryland data from 2001 to 2008—has validated the death certificate against an in-depth review of pregnancy-associated deaths, estimates of underreporting are uncertain and underreporting remains a major barrier to producing valid estimates of the burden of these deaths nationwide. Another potential limitation is that some suicides may be misclassified as unintentional drug-related deaths. Indeed, the California Pregnancy Associated Mortality Review report found that about half of accidental deaths during pregnancy or postpartum were identified as suicides upon review (22). Prior research also suggests potential underestimation and misclassification of overdose mortality, especially for deaths involving opioids (23,24). Thus, our analyses may underestimate the relative contribution of suicides and drug use to pregnancy-associated death. Overall, our findings are limited by inconsistent uptake of the 2003 Revised Death Certificate by states in the United States, resulting in our inclusion of only 33 states and D.C.
Our findings indicate that deaths due to drug-use, suicide, and homicide are a substantial and increasing contributor to pregnancy-associated mortality. Preventing these deaths could have saved the lives of over 2,600 pregnant and birthing people from 2010 to2019. Loss of these lives is particularly devastating to infants and families and has long-term repercussions on infants who lose their parent (25,26). Our findings point to the need to generate scientific evidence on risk factors and prevention approaches for pregnancy-associated death due to drugs, suicide, and homicide. Potential avenues include 1) screening for substance use, suicidality, psychological distress, and intimate partner violence, which has been linked to both pregnancy-associated homicide and suicide (27), combined with the ability for health care professionals to connect people with resources (28,29); 2) coordination of obstetric care with other areas such as addiction medicine, behavioral health, and social services (30); and, perhaps most importantly, 3) attention to structural barriers to accessing care and support including housing, transportation, child care, domestic abuse, stigma, and fear of legal ramifications or social service interventions (31).
Supplementary Material
Funding:
This research was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R01HD095951-02S1, PI Margerison and R01HD102319, MPIs Margerison and Goldman-Mellor).
Footnotes
Financial Disclosure
Alison Gemmill reports money was paid to her from the World Health Organization and Avenir Health. The other authors did not report any potential conflicts of interest.
Each author has confirmed compliance with the journal’s requirements for authorship.
References
- 1.World Health Organization. Trends in maternal mortality 2000 to 2017: estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. Geneva: World Health Organization; 2019. Accessed July 6, 2021. https://www.who.int/reproductivehealth/publications/maternal-mortality-2000-2017/en/ [Google Scholar]
- 2.MacDorman MF, Declercq E, Cabral H, Morton C. Recent Increases in the U.S. Maternal Mortality Rate: Disentangling Trends From Measurement Issues. Obstet Gynecol 2016;128:447–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Main EK, Menard MK. Maternal mortality: time for national action. Obstet Gynecol 2013;122:735–6. [DOI] [PubMed] [Google Scholar]
- 4.Main EK. Reducing Maternal Mortality and Severe Maternal Morbidity Through State-based Quality Improvement Initiatives. Clin Obstet Gynecol 2018;61:319–31. [DOI] [PubMed] [Google Scholar]
- 5.D’Alton ME, Main EK, Menard MK, Levy BS. The National Partnership for Maternal Safety. Obstet Gynecol 2014;123:973–7. [DOI] [PubMed] [Google Scholar]
- 6.Building U.S. Capacity to Review and Prevent Maternal Deaths. Report from Nine Maternal Mortality Review Committees. 2018. Accessed December 7, 2020. https://reviewtoaction.org/national-resource/report-nine-mmrcs [Google Scholar]
- 7.Metz TD, Rovner P, Hoffman MC, Allshouse AA, Beckwith KM, Binswanger IA. Maternal Deaths From Suicide and Overdose in Colorado, 2004–2012. Obstet Gynecol 2016;128:1233–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Smid MC, Stone NM, Baksh L, Debbink MP, Einerson BD, Varner MW, et al. Pregnancy-Associated Death in Utah: Contribution of Drug-Induced Deaths. Obstet Gynecol 2019;133:1131–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wallace ME, Hoyert D, Williams C, Mendola P. Pregnancy-associated homicide and suicide in 37 US states with enhanced pregnancy surveillance. American journal of obstetrics and gynecology 2016;215:364.e1–364.e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goldman-Mellor S, Margerison CE. Maternal drug-related death and suicide are leading causes of postpartum death in California. Am J Obstet Gynecol 2019;221:489.e1–489.e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mangla K, Hoffman MC, Trumpff C, O’Grady S, Monk C. Maternal self-harm deaths: an unrecognized and preventable outcome. American journal of obstetrics and gynecology 2019;221:295–303. [DOI] [PubMed] [Google Scholar]
- 12.Schiff DM, Nielsen T, Terplan M, Hood M, Bernson D, Diop H, et al. Fatal and Nonfatal Overdose Among Pregnant and Postpartum Women in Massachusetts. Obstet Gynecol 2018;132:466–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Scholl L, Seth P, Kariisa M, Wilson N, Baldwin G. Drug and Opioid-Involved Overdose Deaths - United States, 2013–2017. MMWR Morb Mortal Wkly Rep 2018;67:1419–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Martin JA, Hamilton BE, Osterman MJK, Driscoll AK. Births: Final Data for 2019. Natl Vital Stat Rep 2021;70:1–51. [PubMed] [Google Scholar]
- 15.Hoyert DL, Miniño AM. Maternal Mortality in the United States: Changes in Coding, Publication, and Data Release, 2018. Natl Vital Stat Rep 2020;69:1–18. [PubMed] [Google Scholar]
- 16.Horon IL, Cheng D. Effectiveness of pregnancy check boxes on death certificates in identifying pregnancy-associated mortality. Public health reports 2011;126:195–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.MacDorman MF, Declercq E, Thoma ME. Trends in Maternal Mortality by Sociodemographic Characteristics and Cause of Death in 27 States and the District of Columbia. Obstet Gynecol 2017;129:811–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wilder C, Lewis D, Winhusen T. Medication assisted treatment discontinuation in pregnant and postpartum women with opioid use disorder. Drug Alcohol Depend 2015;149:225–31. [DOI] [PubMed] [Google Scholar]
- 19.Sanmartin MX, Ali MM, Chen J, Dwyer DS. Mental Health Treatment and Unmet Mental Health Care Need Among Pregnant Women With Major Depressive Episode in the United States. Psychiatr Serv 2019;70:503–6. [DOI] [PubMed] [Google Scholar]
- 20.Gemmill A, Kiang MV, Alexander MJ. Trends in pregnancy-associated mortality involving opioids in the United States, 2007–2016. American journal of obstetrics and gynecology 2019;220:115–6. [DOI] [PubMed] [Google Scholar]
- 21.Trost SL, Beauregard JL, Smoots AN, Ko JY, Haight SC, Moore Simas TA, et al. Preventing Pregnancy-Related Mental Health Deaths: Insights From 14 US Maternal Mortality Review Committees, 2008–17. Health Aff (Millwood). 2021. Oct;40(10):1551–1559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.The California Pregnancy-Associated Mortality Review. CA-PAMR Report: Pregnancy-associated suicide 2002–2012. 2019. Accessed July 6, 2021. https://www.cmqcc.org/sites/default/files/PAMR%202.0%20Report_FINAL_8.8%20%281%29.pdf [Google Scholar]
- 23.Ruhm CJ. Geographic Variation in Opioid and Heroin Involved Drug Poisoning Mortality Rates. Am J Prev Med 2017;53:745–53. [DOI] [PubMed] [Google Scholar]
- 24.Mertz KJ, Janssen JK, Williams KE. Underrepresentation of heroin involvement in unintentional drug overdose deaths in Allegheny County, PA. J Forensic Sci 2014;59:1583–5. [DOI] [PubMed] [Google Scholar]
- 25.Zanardi DM, Santos JP, Pacagnella RC, Parpinelli MA, Silveira C, Andreucci CB, et al. Long-Term Consequences of Severe Maternal Morbidity on Infant Growth and Development. Matern Child Health J 2021;25:487–96. [DOI] [PubMed] [Google Scholar]
- 26.Chikhungu LC, Newell M-L, Rollins N. Under-five mortality according to maternal survival: a systematic review and meta-analysis. Bull World Health Organ 2017;95:281–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Campbell J, Matoff-Stepp S, Velez ML, Cox HH, Laughon K. Pregnancy-Associated Deaths from Homicide, Suicide, and Drug Overdose: Review of Research and the Intersection with Intimate Partner Violence. J Womens Health 2021;30:236–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Krans EE, Bobby S, England M, Gedekoh RH, Chang JC, Maguire B, et al. The Pregnancy Recovery Center: A women-centered treatment program for pregnant and postpartum women with opioid use disorder. Addict Behav 2018;86:124–9. [DOI] [PubMed] [Google Scholar]
- 29.Krans EE, Cochran G, Bogen DL. Caring for Opioid-dependent Pregnant Women: Prenatal and Postpartum Care Considerations. Clin Obstet Gynecol 2015;58:370–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McKenney KM, Martinez NG, Yee LM. Patient navigation across the spectrum of women’s health care in the United States. Am J Obstet Gynecol 2018;218:280–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ruderman RS, Dahl EC, Williams BR, Davis K, Feinglass JM, Grobman WA, et al. Provider Perspectives on Barriers and Facilitators to Postpartum Care for Low-Income Individuals. Womens Health Rep 2021;2:254–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


