Abstract
Background
The intensive care unit (ICU) is a stressful and complex environment in due to its dynamic nature and severity of admitted patients. EHR interface design can be cumbersome and lead to prolonged times to complete tasks.
Objectives
This paper investigated the relationship between a prominent EHR interface design and interruptions with physician’s efficiency during patient chart review at ICU Pre-Rounds.
Methods
We conducted a live observation of ICU physicians in a 30-bed MICU at a tertiary, southeastern medical center. Directly after the observation sessions, the physicians completed a modified System Usability Scale (SUS) survey.
Results
A total of 52 EHR patient chart reviews were observed at the MICU Pre-rounds. There was statistically significant positive correlation between time spent to review patient EHR with both number of scrolling(p-value<0.0001) across EHR interface; and with number of visited EHR screens (p-value=0.0444). There was positive correlation between number of interruptions with time spent to review patient EHR during ICU prerounds.
Conclusions
EHR design and the occurrence of interruptions lead to reduced physician-EHR efficiency levels. We report that the number of scrolling and visited screens executed by physicians to gather the required information was associated with increased screen time and consequently decreased physician efficiency.
Keywords: EHR, Use, Efficiency, Interface, Design, Critical Care
Introduction
The intensive care unit (ICU) is a stressful and complex environment because of its dynamic nature and severity of admitted patients (1, 2). Physicians value lies in the expert and specialized skills they bring to the care provided in ICUs, including high-level clinical decision making, managing the inter-professional team, coordinating consultant recommendations, performing advanced bedside procedures, and supervising trainees. Physicians’ most valuable resource in the ICU is time. Professional communication, documentation, and reviewing patient data occupy significant amounts of time, the latter two accomplished primarily on the computer. Developing efficient communication and computer systems is necessary to facilitate maximum allocation of time to delivery of high-quality care (3, 4).
The use of Electronic Health Records (EHR) has become a central component in clinical settings. EHRs centralize patient data while reducing medical errors, controlling cost, and providing an efficient communication between the interdisciplinary healthcare team (5). The interface of EHR is designed to eliminate duplicate testing and facilitate easier workflow for providers when inputting and examining patient’s information, however, substantial gaps exist on the efficiency of usage of EHR (6). Due to the large volume of data and unfriendly interface of EHR, providers are often left with information overload and disruption of workflow. This can lead to medical error and waste of valuable time (7, 8).
EHRs designed for stressful work environment is expected to facilitate the workflow, maximize efficiency, effectiveness and satisfaction of its workers. In ICU setting, design with usability in mind can be translated into enhanced performance of providers, better decision making with subsequent improved patient outcome (9). EHRs has the potential to facilitate patient-centered care by improving care coordination and enhancing patient–provider communication (10).
Visions for transforming physician-EHR interaction in the future include design modifications that: provide rapid access to new information, organize by systems or problems as well as by current versus historical patient data, and apply intelligence toward detecting and representing change and urgency (11). This study aims to characterize the specific barriers to efficient EHR interaction during ICU pre-rounds.
Objective
The objective of this paper was to study the association between ICU Interruptions EHR efficiency and satisfaction among physician trainees’.
Methods
To evaluate EHR experience during pre-rounds, we conducted live observations. Prior to data collection, the study team conducted two testing observation sessions to obtain training on the data collection instrument and to become familiar with the MICU environment. Using a Flowsheet chart, two team members would observe a second- or third-year resident while they were pre-rounding on their patients. The team members recorded on paper the EHR screens they viewed, the sequence in which they viewed them, and the time spent collecting data per patient. This was performed on three occasions with two independent pairs of observers. Directly after the observation sessions, the physicians were given a modified System Usability Scale (SUS) to complete. The inter-rated reliability and agreement between the two observers was 79.3%.
One interaction is defined as one physician reviewing one patient’s chart in the EHR during morning pre-rounds, i.e. standard work. Each interaction is observed in tandem by two graduate research assistants, who utilize a checklist to record duration, key EHR screens visited, navigation pathway, scrolling burden, toggle burden, interruptions, and use of external resources. A modified version of the validated User Experience Questionnaire is administered to gauge participants’ satisfaction with the EHR in real-time (12).
Setting and Participants
We observed six physicians in a 30-bed medical ICU (MICU) at a tertiary, southeastern medical center. A sample size of six physicians exceed the recommended sample size for usability studies that indicate that 75% of usability problems can be exposed from a sample of five participants (13). Participants were recruited through convenience sampling using verbal communication. The inclusion criteria was a physician or physician trainee whose was, at the time of the study, serving at the MICU. Physicians who agreed to be shadowed had to sign a consent form. This study was approved by the institutional review board (IRB).
Materials
We designed and built an observation tool based on our previous observational studies in the ICU (14, 15). The observational tool included information about the observational session such as date, time, observation number, start/end time, and the initials of the observers. The tool was divided into two section (1) filters, (2) screen activity. Under filters, the observers recorded the frequency and the type of EHR filters used by the participant. Under screen activity, observers recorded the frequency and type of distractions, the frequency and direction of scrolling, the screens visited.
Interruptions were characterized as either directly related to patient care (paging and others related to professional care collaboration) or indirectly related to patient care (social and cell phone interruptions). Interruptions were defined as a question from staff member of colleague, code, or rapid response team. Cell phone was defined as received call, text, or checking of time. Social interactions were defined as non-clinical communications that disrupted the on-going EHR interaction.
Outcomes
The primary outcomes of this study were number of EHR screens visited, duration per patient chart, and interruptions. Secondary outcomes were scrolling per EHR screens and provider satisfaction.
The studied barriers of EHR interaction were: (1) EHR interface design: evaluated by efforts physicians exert to gather required information through number of scrolling across the screen and number of viewed screens. (2) Interruptions: number and type of interruptions occurred in the work place environment. The impact of studied barriers on physician - EHR interaction was evaluated through: (1) Physician efficiency: time required to complete revision of patient condition through Epic interface. (2) Physician satisfaction: system usability score.
We used descriptive statistics to analyze EHR interaction data. Pearson correlation was used to investigate any associations between the study outcomes. We conducted multivariate analysis (MVA) to examine the correlation between measures of EHR interface design with physician efficiency independent of interruptions effect.
Results
A total of 52 distinct EHR patient chart reviews were observed during the MICU Pre-rounds. Six physicians were observed during pre-rounds as end users of EHR interface. Among participating physicians, ICU rotation average was 3.3 range (IQR: 2-5) rotations, while years of training after graduation average was 2.8, range (IQR: 2-6) years. Our sample included two female physicians out of total 6 physicians who were observed through unique 52 EHR interaction with average number of 8.6, range (IQR: 5-12) interactions per resident, Table 1.
Table 1.
Participant Characteristics.
| Physician Participant |
Age | Gender | Level of Training |
Number of Charts Reviewed |
Total Screen Visits |
|---|---|---|---|---|---|
| 1 | 29 | M | PGY-3 | 6 | 42 |
| 2 | 28 | F | PGY-2 | 12 | 63 |
| 3 | 29 | F | PGY-2 | 11 | 71 |
| 4 | 36 | M | PGY-2 | 9 | 62 |
| 5 | 28 | M | PGY-2 | 5 | 56 |
| 6 | N/A | M | PGY-6 | 9 | 36 |
| CUMULATIVE | 52 | 330 |
EHR interaction barriers related to EHR interface design
Most of the physicians had to scroll across EHR interface (screen) to review the required information. Average of scrolling across the screen was 4.8, range (IQR: 0 – 16) scrolling per interaction across physicians with a cumulative total of 251 scrolling across 52 EHR interactions.
All of the physicians had to navigate through more than one screen to review the required information. The average number of patient charts viewed were 4, range (2-6) screens per interaction across physicians. The total number of discrete screens viewed was 20, where results review, summary, flow sheets and chart review (20% of visited screens) constitute more than 50% of total viewed screens.
EHR interaction barriers related to interruption
During ICU preround, social interruptions were the most common type constituting (>60%) 28 interruptions out of total 42 interruptions observed. Other types of interruption related to professional collaboration and paging follow in frequency, while cell phone interruption occurred once only across all 52 EHR interactions.
Physician efficiency
The time spent to revise patient EHR during ICU preround varies across physicians with average 2 minutes and 20 seconds, range (35 -397) per patient across physicians. The total number of minutes spent per resident for the pre-rounding session ranged from 14 minutes to 34 minutes with a cumulative total of 2 hours 40 minutes and 10 seconds for the all pre-rounding sessions.
Physician satisfaction
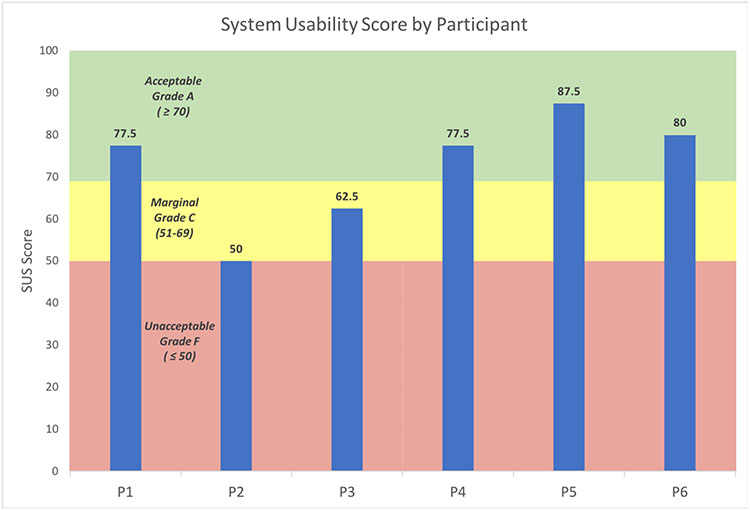
The average total System Usability Score was an acceptable usability grade A of 72 (IQR: 50-87) among all participants. The lowest satisfaction score (SUS) was observed among the two female physicians with unacceptable 50 grade F (SUS) and marginal 62.5 grade C (SUS), after interaction with Epic interface. All male physicians (4 out of 6) had acceptable (SUS), Figure (1).
Figure 1.
System Usability Scale (SUS) scores across ICU physicians.
Correlation between EHR interface design with physician efficiency
There was statistically significant positive correlation between time spent to review patient EHR with both number of scrolling (p value < 0.0001) across EHR interface and with number of reviewed screens (p value = 0.0444). In other words, EHR interface design that require scrolling and navigation across multiple screens was associated with increased time to find the required information, Table 1.
Correlation between interruption with physician efficiency
There was positive correlation (although not statistically significant) between number of interruptions with time spent to review patient EHR during ICU preround. So, increased number of interruptions was associated with decreased physician efficiency, Table 2.
Table 2.
Correlation between different variables of EHR interaction
| Variable | Variable | Correlation | p-value |
|---|---|---|---|
| Time | Interruption | 0.26827 | 0.1456 |
| Time | Scrolling | 0.47498 | < 0.0001* |
| Time | Screens | 0.30715 | 0.0444 * |
| Interruption | Scrolling | −0.09111 | 0.4277 |
| Interruption | Screens | −0.30061 | 0.1191 |
| Scrolling | Screens | 0.07851 | 0.6355 |
statistically significant value (p<.05)
Multivariate analysis
We conducted multivariate analysis (MVA) to examine the correlation between measures of EHR interface design with physician efficiency independent of interruptions effect. EHR interface design measured by scrolling (p value < 0.0001) and number of screens (p value= 0.0216) show significant correlation with resident efficiency independent of interruption. Our study findings emphasized the role of EHR interface design as a barrier to physician EHR interaction independent of other variables like interruption occurred during ICU pre-rounds, Table 3.
Table 3.
Correlation between EHR interface design with physician efficiency after controlling for interruption effect using MVA.
statistically significant value (p<.05)
Correlation based on data analysis per resident level
There was no statistically significant correlation between resident characteristics (age, gender, number of rotations, post graduate years) with any of the following: (1) Barriers to EHR interaction; interface design (number of scrolling, number of screens) and interruptions; (2) Physician efficiency using time spent to review patient EHR; (3) Physician satisfaction using SUS.
Discussion
Our study emphasized the important role of EHR user interface design in shaping EHR interaction. We found that the number of scrolling and visited screens executed by physicians to gather the required information was associated with increased screen time and consequently decreased physician efficiency independent of interruptions occurred in ICU work environment. Interruptions were still associated with increased screen time and decreased efficiency of physician during ICU prerounds. In a research by Stanford Medicine, conducted by The Harris Poll on 2018, showed that improving EHR user interface design was the top priority of short-term changes that physicians need when interacting with EHR followed by shifting the load of data entry to other support staff. In fact, six out of 10 (59%) believe EHRs need a complete overhaul (16).
All physicians in the present study had to navigate through more than one screen during EHR interaction. For categories and frequency of visited screens, results review, summary and flow sheets were the most frequently visited screens while demography and vital sheets were the least visited. In a systematic review by Tiago et al, note-entry studies revealed that what clinicians document is affected by EHR interfaces. Similar to our findings, they demonstrated that "assessment and plan" is the most read note section and what clinicians read is affected by external stimuli, care/information goals, and what they know about the patient (17).
Two studies by Nolan et al demonstrated that certain report subtypes likely represent highly important components to medical ICU decision making (18, 19). They found that nearly half of all chart review sessions began by viewing notes (outpatient notes, progress notes, discharge summary), which were overall the most likely data category to which clinicians return after viewing other data. While about one-third of chart review sessions never referenced like historical vital sign data which presumably obtained only at the bedside. Another interesting finding from the same study is that clinicians spent nearly 10% of their time searching or scrolling through screens of meta- data, representing the fourth most common workflow activity by time. While it is possible that useful information can be gleaned during this activity, it may suggest ineffective data presentation.
Carayon et al compared time spent by ICU resident and attending physicians on various tasks before and after EHR implementation. They observed some evidence of efficiency gains, such as less time spent on administrative review and documentation and in-between tasks, for resident physicians but not for attendings, while both physicians and attendings in the ICU spent more time on review and documentation of clinical information (20).
Interruption and EHR efficiency
In the this study, we observed type and number of interruptions occurred to physicians during ICU preround workflow. Four types of interruptions were tracked; paging, other interruptions related to direct patient care, social and cellular phone calls interruptions. We found that interruptions were associated (although not statistically significant) with increased screen time and decreased physician efficiency.
Physicians’ EHR Satisfaction
For resident satisfaction, female physicians (two out of 6) reported the lowest score after interaction with Epic interface in comparison with their male peers. However, female physicians in our sample had the lowest number of ICU rotations and years of training after graduation. The matter that marginalize the impact of gender on resident satisfaction after interaction with Epic interface in ICU preround settings. There was no statistically significant correlation between resident characteristics (age, number of rotations, post graduate years) with; number of interruptions happened in clinical environment; EHR interface design; efficiency using Epic interface. Absence of statistically significant correlation can be attributed to small sample size of our study.
In a previous study Khairat et al EHR usability impact was examined in emergency department with equal distribution of gender and experience among participating physicians(21). They identified some factors that cause high EHR frustrations like; remembering menu and button names; performing tasks that are not straightforward; system speed; and system reliability. In comparison between attending and resident physicians, frustration levels linked to the EHR were significantly higher for attending physicians compared with physicians who were faster in completing half of the assigned tasks and in their overall reaction to the EHR (21).
Usability study design
Assessment of end-user EHR behavior has often been conducted via self-reports and surveys, direct observation, and meaningful use measure reporting. An observational time motion study found that ICU physicians spent only 17% of their time on direct patient care. In contrast, ICU physicians spent the majority of their time (62%) on professional communication, followed by 38% of their time on data review and documentation, and 9% on educational activities. Interruptions were common, occurring an average of 2.5 times per hour, and participants were found to be multitasking 67% of the time (8).
A systematic review and meta-analysis conducted by Khairat et al demonstrated that currently no conclusion can be made regarding the effect of health information technology on inpatient and ICU outcomes such as mortality, length of stay, and cost. They concluded that more research is needed with standardized interventions and endpoints to evaluate EHR use and implementation (22).
Epic vendor among others
A recent study by Holmgren et al, showed that vendor choice accounts for a meaningful proportion of variation in hospital meaningful use performance. Epic was associated with significantly higher performance on 5 of the 6 criteria; relationships for other vendors were mixed, with some associated with significantly worse performance on multiple criteria (23).
Recently, research efforts have been focusing on improving EHR interaction to enhance efficiency and effectiveness of healthcare providers. In a literature review, visualization dashboard solutions showed decrease time spent on data gathering, difficulty of data gathering process, cognitive load, time to task completion, errors, and improve situation awareness, compliance with evidence-based safety guidelines, usability, and navigation (22). Pickering et al, observed the impact of an ICU-specific patient viewer and monitoring system called The Ambient Warning and Response Evaluation (AWARE) system. They found that compared to the existing EMR, information management (data presentation format, efficiency of data access) and cognitive mental load was reported to be better after AWARE implementation (24). In a study conducted by Asan et al, the importance of training and orientation affects the adoption and use patterns of a new EHR interface technology Large Customizable Interactive Monitor (LCIM) (25). Another study by Robinson et al demonstrated that EHR training programs may have impact on the safety, quality, accuracy, and timeliness of care and may also help reduce physician burnout by improving critical skills and reducing time interfacing with all aspects of a patient’s health record (26).
Recommendations
EHR implementation is a major additions to the clinical workflow however, developing EHR interface with a user centered design is a challenging task for many developers because of the multifaceted nature of healthcare practices. Many studies concluded that transformative changes in EHR interaction need multidisciplinary approach including but not limited to; user centered design, visualization dashboard solutions, ongoing training for healthcare providers to build up skills for effective use of advances in HIT. Such approach should flip the coin of current EHR interaction barriers into facilitators and achieve better HCP performance and overall patient outcome.
Study Limitation
Our purposive sample size for participating physicians was relatively small, which was homogenous purposive sample based on participants’ age, clinical experience, and EHR experience. However, the current study can be considered as a pilot for future larger studies to further examine and explore physician EHR interaction especially with expected ongoing changes in EHR interface design.
Participating physicians were not controlled for number of ICU rotation and years of training after graduation. These factors may affect physician EHR interaction regarding efficiency and satisfaction. Also, we only looked at Medicine physicians in one setting, so findings may not apply to trainees in Surgery or Anesthesia or Pediatrics, etc.
Observation in this study was based on subjective evaluation of barriers to EHR interactions like scrolling number across the screen, screens viewed and time. We tried to enhance accuracy and reliability of our study results by taking the average of two observers for each EHR interaction measurable.
Conclusion
We investigated the association between the EHR interface design and interruptions with physician’s efficiency and satisfaction during patient chart review at ICU Pre-Rounds. We report that the number of scrolling and visited screens executed by physicians to gather the required information was associated with increased screen time and consequently decreased physician efficiency independent of interruptions occurred in ICU work environment. Also, EHR design and the occurrence of interruptions can lead to reduced physician-EHR efficiency levels. In conclusion, more user-centered design is required to deliver an EHR interface that is useful by the users.
Key Messages.
The amount of scrolling and visited screens executed by physicians to gather the required information was associated with increased screen time and consequently decreased physician efficiency independent of interruptions occurred in ICU work environment.
Interruptions were still associated with increased screen time and decreased efficiency of physician during ICU prerounds.
Interruptions were associated with increased screen time and decreased physician efficiency.
Funding sources:
This work was supported by the National Library of Medicine (NLM) under grant number 1T15LM012500-01.
Footnotes
Conflict of Interest: The authors declare no conflicts of interest.
All authors had access to the data and a role in writing the manuscript.
Contributor Information
Saif Khairat, Carolina Health Informatics Program, University of North Carolina at Chapel Hill, NC, USA.
Eman Metwally, Carolina Health Informatics Program, University of North Carolina at Chapel Hill, NC, USA.
Cam Coleman, Carolina Health Informatics Program, University of North Carolina at Chapel Hill, NC, USA.
Elaine James, School of Nursing, University of North Carolina at Chapel Hill, NC, USA.
Samantha Russomagno, School of Nursing, University of North Carolina at Chapel Hill, NC, USA.
Thomas Bice, Pulmonary Diseases and Critical Care Medicine, University of North Carolina at Chapel Hill, NC, USA.
References
- 1.Ellsworth MA, Lang TR, Pickering BW, Herasevich V. Clinical data needs in the neonatal intensive care unit electronic medical record. BMC Medical Informatics and Decision Making. 2014;14(1):92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carayon P, Cartmill R, Blosky MA, Brown R, Hackenberg M, Hoonakker P, et al. ICU nurses' acceptance of electronic health records. Journal of the American Medical Informatics Association : JAMIA. 2011;18(6):812–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Halpern SD. ICU capacity strain and the quality and allocation of critical care. Current opinion in critical care. 2011;17(6):648–57. [DOI] [PubMed] [Google Scholar]
- 4.Vranas KC, Kerlin MP. ICU Physician Workflow: Inside the Balloon. Crit Care Med. 2016;44(8):1607–8. [DOI] [PubMed] [Google Scholar]
- 5.Middleton B, Bloomrosen M, Dente MA, Hashmat B, Koppel R, Overhage JM, et al. Enhancing patient safety and quality of care by improving the usability of electronic health record systems: recommendations from AMIA. Journal of the American Medical Informatics Association : JAMIA. 2013;20(e1):e2–e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coleman C, Gotz D, Eaker S, James E, Bice T, Carson S, et al. Analysing EHR navigation patterns and digital workflows among physicians during ICU pre-rounds. Health Inf Manag. 2020:1833358320920589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.March CA, Steiger D, Scholl G, Mohan V, Hersh WR, Gold JA. Use of simulation to assess electronic health record safety in the intensive care unit: a pilot study. BMJ open. 2013;3(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Doberne JW, He Z, Mohan V, Gold JA, Marquard J, Chiang MF. Using High-Fidelity Simulation and Eye Tracking to Characterize EHR Workflow Patterns among Hospital Physicians. AMIA Annual Symposium proceedings AMIA Symposium. 2015;2015:1881–9. [PMC free article] [PubMed] [Google Scholar]
- 9.Nielsen J Usability Engineering: Morgan Kaufmann Publishers Inc.; 1993. 358 p. [Google Scholar]
- 10.Meyerhoefer CD, Sherer SA, Deily ME, Chou SY, Guo X, Chen J, et al. Provider and patient satisfaction with the integration of ambulatory and hospital EHR systems. Journal of the American Medical Informatics Association : JAMIA. 2018;25(8):1054–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wright MC, Dunbar S, Macpherson BC, Moretti EW, Del Fiol G, Bolte J, et al. Toward Designing Information Display to Support Critical Care. A Qualitative Contextual Evaluation and Visioning Effort. Appl Clin Inform. 2016;7(4):912–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schrepp M, Hinderks A, Thomaschewski J. Applying the User Experience Questionnaire (UEQ) in Different Evaluation Scenarios. In: Marcus A, editor. Design, User Experience, and Usability Theories, Methods, and Tools for Designing the User Experience: Third International Conference, DUXU 2014, Held as Part of HCI International 2014, Heraklion, Crete, Greece, June 22-27, 2014, Proceedings, Part I. Cham: Springer International Publishing; 2014. p. 383–92. [Google Scholar]
- 13.Nielsen J, Landauer TK. A mathematical model of the finding of usability problems. Proceedings of the INTERACT '93 and CHI '93 Conference on Human Factors in Computing Systems; Amsterdam, The Netherlands. 169166: ACM; 1993. p. 206–13. [Google Scholar]
- 14.Khairat S, Gong Y. Understanding effective clinical communication in medical errors. Studies in Health Technology & Informatics. 2010;160(Pt 1):704–8. [PubMed] [Google Scholar]
- 15.Khairat S, Gong Y. Knowledge representation in ICU communication. Proceedings of the 1st ACM International Health Informatics Symposium; Arlington, Virginia, USA. 1883102: ACM; 2010. p. 718–23. [Google Scholar]
- 16.Poll H How Doctors Feel About Electronic Health Records 2018. [Available from: https://med.stanford.edu/content/dam/sm/ehr/documents/EHR-Poll-Presentation.pdf. [Google Scholar]
- 17.Colicchio TK, Cimino JJ. Clinicians' reasoning as reflected in electronic clinical note-entry and reading/retrieval: a systematic review and qualitative synthesis. Journal of the American Medical Informatics Association : JAMIA. 2019;26(2):172–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nolan ME, Siwani R, Helmi H, Pickering BW, Moreno-Franco P, Herasevich V. Health IT Usability Focus Section: Data Use and Navigation Patterns among Medical ICU Clinicians during Electronic Chart Review. Appl Clin Inform. 2017;8(4):1117–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nolan ME, Cartin-Ceba R, Moreno-Franco P, Pickering B, Herasevich V. A Multisite Survey Study of EMR Review Habits, Information Needs, and Display Preferences among Medical ICU Clinicians Evaluating New Patients. Appl Clin Inform. 2017;8(4):1197–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Carayon P, Wetterneck TB, Alyousef B, Brown RL, Cartmill RS, McGuire K, et al. Impact of electronic health record technology on the work and workflow of physicians in the intensive care unit. Int J Med Inform. 2015;84(8):578–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Khairat S, Burke G, Archambault H, Schwartz T, Larson J, Ratwani RM. Perceived Burden of EHRs on Physicians at Different Stages of Their Career. Appl Clin Inform. 2018;9(2):336–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Khairat SS, Dukkipati A, Lauria HA, Bice T, Travers D, Carson SS. The Impact of Visualization Dashboards on Quality of Care and Clinician Satisfaction: Integrative Literature Review. JMIR human factors. 2018;5(2):e22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Holmgren AJ, Adler-Milstein J, McCullough J. Are all certified EHRs created equal? Assessing the relationship between EHR vendor and hospital meaningful use performance. Journal of the American Medical Informatics Association : JAMIA. 2018;25(6):654–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pickering BW, Dong Y, Ahmed A, Giri J, Kilickaya O, Gupta A, et al. The implementation of clinician designed, human-centered electronic medical record viewer in the intensive care unit: a pilot step-wedge cluster randomized trial. Int J Med Inform. 2015;84(5):299–307. [DOI] [PubMed] [Google Scholar]
- 25.Asan O, Holden RJ, Flynn KE, Yang Y, Azam L, Scanlon MC. Provider Use of a Novel EHR display in the Pediatric Intensive Care Unit. Large Customizable Interactive Monitor (LCIM). Applied clinical informatics. 2016;7(3):682–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Robinson KE, Kersey JA. Novel electronic health record (EHR) education intervention in large healthcare organization improves quality, efficiency, time, and impact on burnout. Medicine (Baltimore). 2018;97(38):e12319. [DOI] [PMC free article] [PubMed] [Google Scholar]