A pervasive theme in this summary is that women are not equally represented across a myriad of organizations, from promotion and tenure, to editorial boards of prestigious journals. [1–2] Despite 60% of the profession identifying as female, women are recognized less often, with 90% of awards between 1981–2014 given to male recipients. [3] Women experience significantly higher rates of workplace harassment. [4] Within the era of social media expansion, rates of harassment online range from 20–40%. [5–6] While a vast number of publications are available surrounding harassment in the workplace within medicine, little data exist on the pharmacy profession. Such holds true for pharmacy trainees as well. Surveys in medical trainees reveal women perceive a high rate of gender discrimination and sexual harassment. [7–9] However, no such granular detail is available for postgraduate pharmacy education.
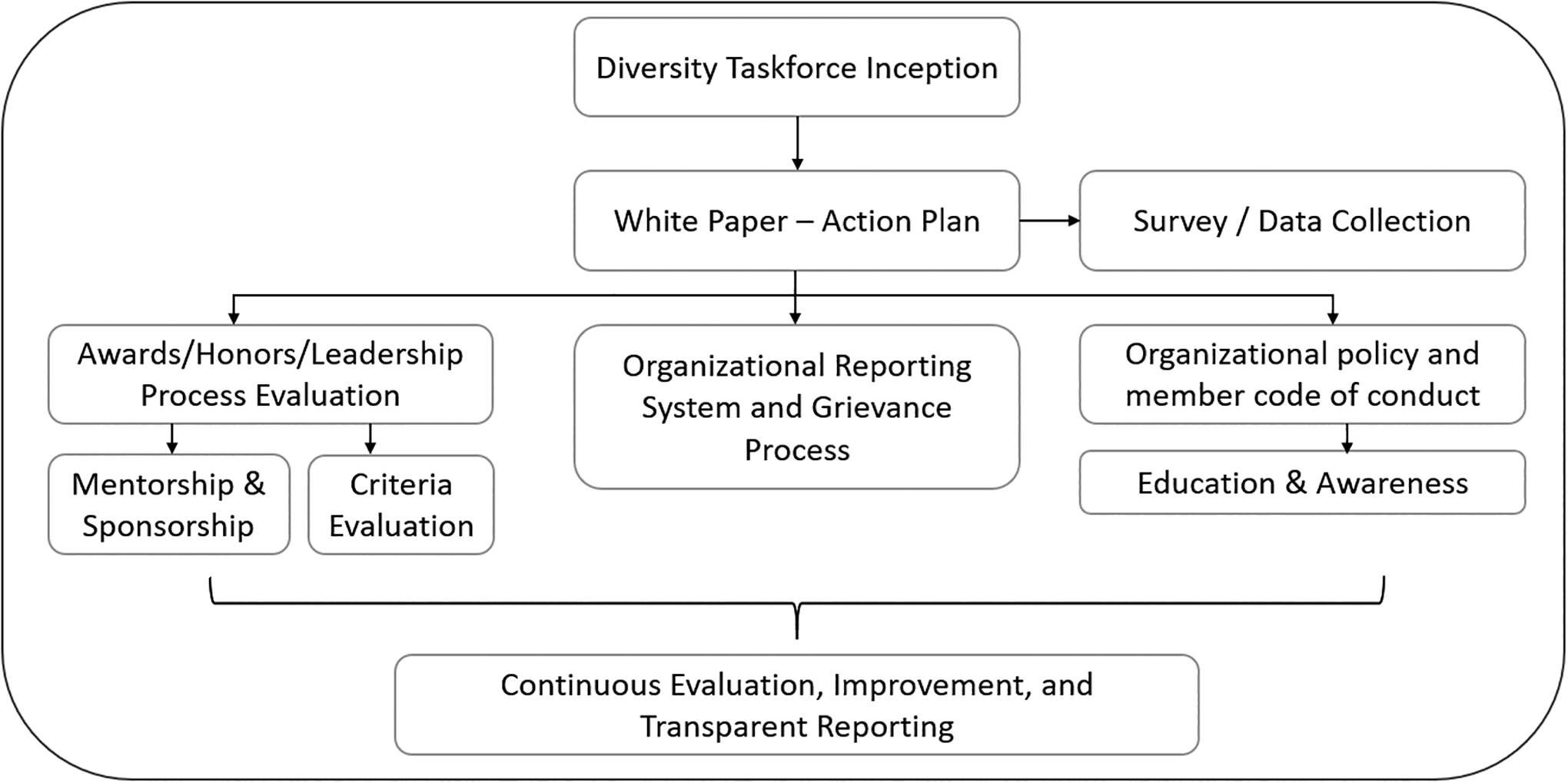
Recommendations are developed around three core areas: (1) building national infrastructure that promotes diversity and gender equity, (2) scoping the problem and establishing a baseline with plans for improvement, (3) developing organizational initiatives to promote diversity in leadership and recognition [Figure 1]. Further, supporting education initiatives and ongoing process improvement will be instrumental to affect change].
Figure 1. Steps toward gender equity.
Reprinted with permission from American Society of Health-System Pharmacists
The first step is the creation of a national pharmacy diversity taskforce with a focus on gender equity to oversee the realization of these initiatives, responsible for the publication and subsequent enactment of an action plan to address equity within the profession. This plan should include recommendations for colleges, training programs, and organizations. To support this action plan, complete characterization of the scope of gender inequity and sexual harassment in the profession is recommended. Within this published action plan, the creation of a national resource center specific to gender bias and sexual harassment is recommended. The resource center would serve as the central repository of tools and resources.
At its core, this action plan will be aimed at the development of a diverse membership, fostering diversity in leadership positions and national recognitions. The first step will be an inventory of the organization’s current membership to create plans for improving representation and proactive strategies to identify and cultivate potential female leaders starting early in their careers [Table 1]. These processes would support female membership through diverse mentorship and sponsorship to create avenues for advancement. Notably, processes dedicated to thoroughly reviewing candidates nominated for national awards can ensure that character evaluations are involved in the nomination and selection processes. The review and recall of awards granted to those individuals who have engaged in reproachful behavior. Organizations are encouraged to develop their own transparent reporting system and grievance processes to type transcend institutional barriers and foster professional accountability [Table 2].
Table 1. Recommended Actionable Organizational Changes to Increase Gender Equity in Pharmacy.
Reprinted with permission from American Society of Health-System Pharmacists
| Action | Steps for Completion |
|---|---|
| Acknowledge and rectify the lack of gender equity in leadership and create processes to support female membership through diverse mentorship, with the inclusion of senior male and female mentors, and sponsorship | a. Inventory the current membership of professional organizations and ensure that the leadership roles held by women are proportionate to the number of women that are members. Furthermore, these data should be made publicly available to the organization’s membership in the context of annual yearly reports or published in the organization’s respective journal. b. Enable content sharing among organizations that have developed successful mentorship programs; with an emphasis on the development of transparent criteria for the selection of mentors and the extensive character vetting of interested mentors. c. Advocate for female leadership advancement opportunities for faculty, practitioners, residents, etc. d. Provide specific training for women that addresses barriers commonly encountered in leadership opportunities. |
| Develop equitable, transparent, and just criteria to increase the number of women pharmacists that receive national honors, invitations for national conference speaking engagements, are awarded grants | a. Review current organizational nomination criteria and ensure that the requirements are clearly stated and provide women with both a viable and equal opportunity to attain the pursued honor. b. Perform a gap analysis of current presenter nominations, grantsmanship, and promotion processes as it pertains to equity matters. c. Enact formal and transparent action to rectify identified inequities |
| Form specific task forces dedicated to extensively reviewing those individuals that are nominated for national honors/awards | a. Select and appoint awards committee leaders to make sure they represent equity; ensuring that character evaluations and character attestation is provided in the nomination and selection processes of awardees. b. Implement formal policy and procedure development with competency training and processes for executive committee, awards committee, board committee appointments. c. Create protocols, such as those supported by ASHP and ACCP, that call for the review and/or recall of awards to those individuals that have engaged in reproachful behavior (e.g., sexual harassment). |
| Provide best practice statements for pharmacy schools to address gender inequalities | a. Review recruitment, promotion criteria, and compensation scales periodically, with monitoring to ensure fairness. b. Require training courses in explicit and implicit gender bias. c. Provide symposiums and workshops to: (1) Include special interest groups and sections dedicated to women’s issues within the pharmacy profession; (2) Offer mentorship, sponsorship and other career development programs; (3) Promote policies supporting work-life balance |
Table 2. Recommendations for Developing an Organizational Reporting System and Grievance Process Related to Gender Bias and Sexual Harassment.
Reprinted with permission from American Society of Health-System Pharmacists
| Action | Questions to Ask and Items to Consider |
|---|---|
| Define the intent and scope of the grievance process |
|
| Structure the grievance process |
|
| Develop a statement of rights as part of the grievance process |
|
| Commit to continuous quality improvement |
|
| Explore and evaluate future considerations |
|
At local levels, mitigation strategies should be developed to identify both conscious and unconscious biases within the workplace and education. It should prevent preclusion of females from future opportunities or promotion. Understanding the scope of the problem will require critical observation and self-reflection of the institutional norms and culture it has created.
Much work is needed to promote gender equity more effectively within pharmacy, but this work is essential to ensuring future sustained infrastructure. Gender inequity and sexual harassment are persistent in pharmacy profession. Women in pharmacy have started the discussion, but the drivers of continued change will be through organizational leadership and awareness and advocacy by individual pharmacists.
Disclosures:
A.B. B.B., B.D.B., M.H., J.C., L.K., T.H.K., T.J.M, J.A.M, J. J., K.B., M.A.R., R.R.S., C.M., A.N.: No disclosures
A.S.N.: Dr. Newsome has received research funding through the National Center for Advancing Translational Sciences (NCATS) of the National Institutes of Health (NIH) under Award Numbers UL1TR002378 and KL2TR002381.
J.J.: Dr. Jacobi is a consultant for Pfizer Hospital Products Division and La Jolla Pharmaceuticals.
S.E.K.: Speaker’s Bureau – Servier Pharmaceuticals LLC; Consulting fees – Accord Healthcare and Servier Pharmaceuticals LLC
Footnotes
This is an Executive Summary of a Review published in AJHP: American Journal of Health-System Pharmacy https://doi.org/10.1093/ajhp/zxab275
Contributor Information
Brittany D. Bissell, University of Kentucky, 1000 S. Limestone, Room H110, Lexington, KY 40536, USA.
Jackie P. Johnston, Ernest Mario School of Pharmacy, Rutgers, The State University of New Jersey, 160 Frelinghuysen Road, Piscataway, NJ 08854, USA.
Rebecca R. Smith, University of Arkansas for Medical Sciences, Department of Pharmacy, 4301 West Markham Street, Slot 522, Little Rock, AR 72205.
Andrea Sikora Newsome, University of Georgia College of Pharmacy, Department of Clinical and Administrative Pharmacy, 120 15th Street, HM-118, Augusta, GA 30912.
Melissa L. Thompson Bastin, University of Kentucky, 800 Rose Street, Room H110, Lexington, KY 40536, USA.
Jacinda Abdul-Mutakabbir, Loma Linda University School of Pharmacy, Department of Pharmacy Practice, 24745 Stewart Street, Shryock Hall Room 212, Loma Linda, CA 92350, USA.
Ashley Barlow, The University of Texas MD Anderson Cancer Center, 1515 Holcombe Boulevard, Houston Texas 77030.
Brooke Barlow, University of Kentucky, 1000 S. Limestone, Room H110, Lexington, KY 40536, USA
Karen Berger, Neurocritical Care, New York-Presbyterian Hospital/Weill Cornell Medical Center, 525 East 68th St, New York, NY 10065.
Jessica R. Crow, The Johns Hopkins Hospital, Department of Pharmacy, 600 N. Wolfe Street, Carnegie 180, Baltimore, MD 21287.
Deepali Dixit, Ernest Mario School of Pharmacy, Rutgers, The State University of New Jersey, 160 Frelinghuysen Road, Piscataway, NJ 08854, USA.
Judith Jacobi, Visante, Inc., 604 N East St., Lebanon, IN 46052.
Lamis R. Karaoui, Director of Experiential Education/Acting Assistant Dean for Student Affairs, Department of Pharmacy Practice School of Pharmacy, Lebanese American University, P.O.Box: 36 (S23), Byblos, Lebanon.
Tyree H. Kiser, Department of Clinical Pharmacy, University of Colorado Skaggs School of Pharmacy and Pharmaceutical Sciences, 12850 E Montview Blvd, C238, Aurora, CO 80045.
Jill Kolesar, College of Pharmacy, University of Kentucky, 789 S. Limestone, Lexington KY 40536.
Susannah E. Koontz, Koontz Oncology Consulting LLC, 2617C W. Holcombe Blvd. #365, Houston, TX 77025-1601, USA.
T. Joseph Mattingly, II, Department of Pharmaceutical Health Services Research, University of Maryland School of Pharmacy, 220 Arch Street, Baltimore, Maryland 21201.
Chelsea Mitchell, Methodist University Hospital, 1265 Union Ave, Memphis TN 38104.
Alexsandra Nilges, University of Kentucky College of Pharmacy, 789 S. Limestone, Lexington, KY 40506 USA.
Megan A. Rech, Adjunct Assistant Professor - Department of Emergency Medicine, Research Coordinator - Department of Emergency Medicine, Stritch School of Medicine, Loyola University Chicago, Loyola University Medical Center, 2160 S 1st Ave, Maywood IL 60153.
Mojdeh S. Heavner, Department of Pharmacy Practice and Sciences, University of Maryland School of Pharmacy, 20 N. Pine Street, N427, Baltimore, MD 21201.
References
- 1.Andreoli L, Ovseiko PV, Hassan N, et al. Gender equity in clinical practice, research and training: Where do we stand in rheumatology? Joint Bone Spine. 2019;86(6):669–672. 10.1016/j.jbspin.2019.05.005 [DOI] [PubMed] [Google Scholar]
- 2.Boxer R, Norman M, Abadir P, et al. When women rise, we all rise: American Geriatrics Society position statement on achieving gender equity in geriatrics. J Am Geriatr Soc. 2019;67(12):2447–2454. 10.1111/jgs.16195\ [DOI] [PubMed] [Google Scholar]
- 3.Draugalis JR, Plaza CM, Taylor DA, Meyer SM. The status of women in US academic pharmacy. Am J Pharm Educ. 2014;78(10):178. doi: 10.5688/ajpe7810178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Choo EK, van Dis J, Kass D. Time’s Up for Medicine? Only Time Will Tell. N Engl J Med. 2018;379(17):1592–1593. doi: 10.1056/NEJMp1809351. [DOI] [PubMed] [Google Scholar]
- 5.Barry AR, Pearson GJ. Professional use of social media by pharmacists. Can J Hosp Pharm. 2015;68(1):22–27. doi: 10.4212/cjhp.v68i1.1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vogels EA. The State of Online Harassment [Internet]. Pew Research Center. 2021. [cited 2021Jan25]. Available from: https://www.pewresearch.org/internet/2021/01/13/the-state-of-online-harassment/
- 7.Hu Y-Y, Ellis RJ, Hewitt DB, et al. Discrimination, Abuse, Harassment, and Burnout in Surgical Residency Training. N Engl J Med. 2019;381(18):1741–1752. doi: 10.1056/nejmsa1903759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nora LM, McLaughlin MA, Fosson SE, et al. Gender discrimination and sexual harassment in medical education: Perspective gained by a 14-school study. Acad Med. 2002;77(12):1226–1234. doi: 10.1097/00001888-200212000-00018 [DOI] [PubMed] [Google Scholar]
- 9.Jendretzky K, Boll L, Steffens S, Paulmann V. Medical students’ experiences with sexual discrimination and perceptions of equal opportunity: A pilot study in Germany. BMC Med Educ. 2020;20(56). doi: 10.1186/s12909-020-1952-9 [DOI] [PMC free article] [PubMed] [Google Scholar]


