Summary
Positive airway pressure (PAP) therapy is a commonly prescribed treatment for pediatric obstructive sleep apnea (OSA). Negative health consequences associated with untreated OSA make understanding the utilization of PAP therapy imperative. The aim of this review was to describe PAP use in children and adolescents with OSA, explore factors that influence use, and describe published scientific or clinical approaches to improve use. Among 20 studies, average PAP adherence was 56.9% (range, 24–87%). PAP use averaged 4.0 hours (SD= 3.1) to 5.2 hours (SD= 3.4) per night. Cautious consideration of summary estimates of PAP use is necessary as studies were heterogeneous and adherence definitions widely varied across studies. Age, sex, and developmental delay were the only factors associated with PAP use in more than one study. The majority of approaches to improve use were program evaluations rather than scientifically tested interventions. This review identified critical gaps in the existing literature and sets forth a research agenda for the future.
Keywords: Pediatric, adherence, compliance, obstructive sleep apnea, positive airway pressure
Introduction
Obstructive sleep apnea (OSA) is defined as repeated episodes of complete or partial airway obstruction [1] and is estimated to affect approximately 1–4% of children [2]. Pathophysiological presentations that contribute to the development of pediatric OSA typically include: hypertrophy of pharyngeal soft tissue structures, craniofacial anomalies, neuromuscular disorders, and/or obesity [3, 4]. Nighttime symptoms can include snoring and labored/paradoxical breathing; daytime symptoms frequently present as hyperactivity in younger children and daytime sleepiness in older children, accompanied by issues with attention, mood, school performance and other cognitive and neurobehavioral complications [4]. Further, a multitude of co-morbidities are associated with untreated OSA such as cardiovascular and metabolic complications, delays in growth, and alterations in biomarkers of hormonal and inflammatory processes [5, 6].
While adenotonsillectomy is the primary treatment for pediatric OSA, OSA may still persist, with residual rates ranging from 13–29% in low-risk populations and > 70% in obese and other at-risk populations (e.g. Down syndrome) [6, 7]. Positive airway pressure (PAP) is therefore second-line treatment for pediatric OSA. PAP therapy provides the potential for individuals with OSA to improve or avoid serious complications of untreated OSA [6]. Early measures of pediatric PAP use relied on parental-report. PAP devices now contain an internal microprocessor that records the duration of time the device is powered on and at effective pressure. PAP use, or adherence can be accurately measured and rapidly assessed as nightly use data is automatically uploaded to a Health Insurance Portability and Accountability Act (HIPAA)-compliant, manufacturer-specific, online server when devices are equipped with a modem. The same data is also accessible by secure digital (SD) card, which can be periodically downloaded to the same server source.
In the adult literature, PAP adherence is clinically defined as use ≥ 4 hours per night on 70% of nights for 30 consecutive days within the first 90 days of treatment [8]. Various adherence definitions in the research literature stem from this clinical definition. In pediatrics, the definition of PAP adherence is similarly heterogeneous. For clinical purposes, the adult definition is used for insurance providers to cover PAP machine costs [8]. However, it is unknown what threshold of PAP use is associated with positive outcomes in children and adolescents and therefore, a consensus on an optimal threshold for adherence is yet to be defined [9]. For the purposes of this review, the term “PAP use” is used to define the utilization of PAP; the term “adherence” is used when referring to results wherein the authors define a usage threshold, or definition of adherence, to report results.
While PAP is commonly prescribed, to our knowledge there is no comprehensive, systematic evaluation of PAP use in children and adolescents with OSA. The objectives of this review were: 1) to describe pediatric PAP use, 2) provide an overview of factors that influence PAP use, 3) describe interventions or approaches to promote adherence, and 4) set forth a research agenda to address gaps and opportunities for pediatric PAP adherence.
Methods
This systematic scoping review was conducted in accordance with the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for scoping reviews guidelines [10].
Eligibility criteria
Inclusion criteria were: 1) age 0–21 years; 2) participants with OSA treated with PAP (including continuous positive airway pressure [CPAP], bi-level positive airway pressure, auto-titrating positive airway pressure); 3) studies reporting outcome measures of hours of PAP use or frequency of adherence; and 4) study reported in English. Studies that met any of the following criteria were excluded: 1) age >21 years; 2) PAP treatment for diagnoses other than OSA; 3) PAP treatment employed short-term (i.e., pre-surgical/not used for OSA management); and 4) gray literature, abstracts, reviews and case studies.
Search Strategy
Database searches were conducted by two medical librarians in June 2019. Search strategies were developed in seven databases, PubMed/Medline, PsycINFO, CINAHL, Scopus, Web of Science, and Cochrane Library, and EMBASE. In each database, the controlled vocabularies and keywords associated with the concepts of positive airway pressure, obstructive sleep apnea, and pediatric were identified and combined with Boolean operators in a logic way to construct the search syntax. Search results were limited to English language. Ancestry search of reference lists of eligible articles and review papers was conducted to identify any articles missed by the database searches. Complete search strategies by database are available in the supplementary materials (Tables S1 A–G).
Study selection
Study titles and abstracts were retrieved by (KF and MQ). All retrieved articles were screened by one reviewer (AW). Full texts of potentially eligible articles were obtained and assessed for eligibility by two reviewers (AW and AS). Where multiple publications described the same sample, only the article with the primary objective of reported PAP use was included.
Data collection and quality assessment
Data was extracted and double entered in an investigator-designed database at two different time points by one reviewer (AW). Data extracted included: study and subject characteristics, OSA and PAP characteristics, and PAP use data (see Tables 1–4 for specific variables). The outcome assessment period was defined as the duration of PAP use data collected. Factors influencing PAP use (e.g., patient characteristics, PAP device factors), and descriptions of approaches to improve PAP use were extracted. The methodological quality of evidence was assessed at the study level by two reviewers (AW and BS) using the Johns Hopkins Nursing Evidence-Based Practice evidence appraisal system [11]. Any disagreements regarding evidence ratings were discussed and if consensus was not reached, a third reviewer (AS) was consulted.
Analysis
Frequencies are reported for study, participant, and OSA/PAP characteristics. Pooled means and standard deviations, or medians and ranges are reported for age, frequency of adherence, and hours of PAP use. PAP use data were analyzed in four categories: PAP naïve/new PAP users (1-month), PAP naïve/new PAP users (> 1-month), non-naïve/existing users (1-month), and non-naïve/existing users (>1-month). In instances where average age was reported separately for sample sub-groups (e.g., CPAP group and bi-level PAP group), means/medians were combined if there were no significant group differences (n=7); means/medians were not combined for three studies (p < 0.05) [12–14]. Where studies reported both a mean and median for age, medians are reported [15, 16]. Where PAP use was reported for “all days” and separately for “days used,” “all days” PAP use means/median are reported [17–20]. When hours of PAP use were reported separately by PAP mode (i.e., CPAP, bi-level PAP) and there were no significant differences between groups, means were pooled for the PAP use analysis [14, 21]. Data from four studies were included in both naïve 1-month and naïve >1-month summary statistics, as these studies reported PAP use data at both 1-month and 3-months [21–24].
Results
Study selection
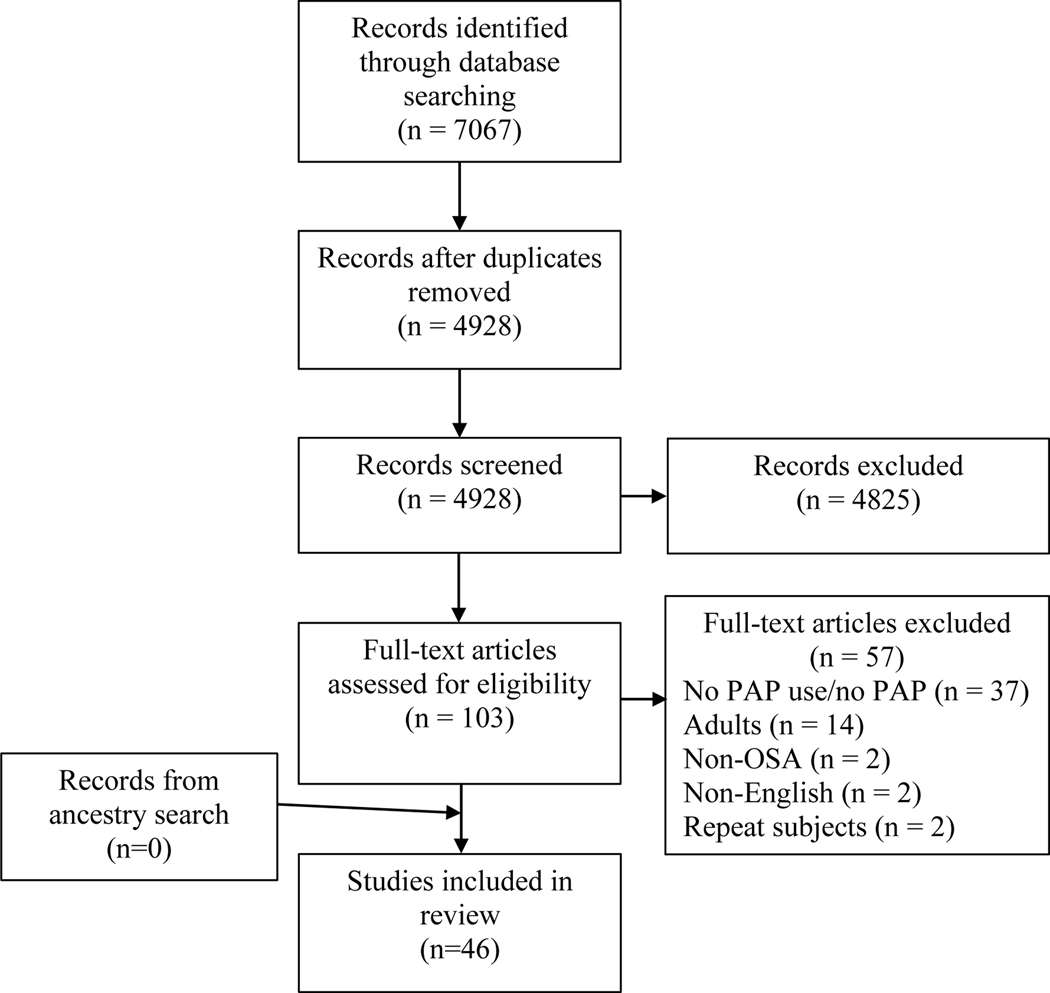
A total of 46 studies were identified for inclusion. The literature search yielded a total of 7,067 citations. After removing duplicates, 4,928 records were screened; 4,825 did not meet inclusion criteria and 103 full-text articles were assessed for eligibility. Fifty-seven were excluded and 46 studies were eligible for inclusion (Figure 1).
Figure 1.
PRISMA flow diagram.
Study characteristics
The identified studies included a total of 3,208 participants (median sample size 50 with range 9–413); 2,216 had complete PAP use/adherence data (median sample size was 27 with range 6 – 275; Table 1). The majority of studies were conducted in the US (54.3%, 25/46), Australia (13%, 6/46) and France (15.2%, 7/46) with 60.9% (28/46) conducted in sleep center settings, 19.6% (9/46) in non-sleep center settings, and 13% (6/46) mixed (sleep and non-sleep centers). Studies were predominantly retrospective (56.5%, 26/46), longitudinal (67.4%, 31/46), and observational (73.9%, 34/46). PAP use or adherence was the primary outcome of interest in 39.1% (18/46) of studies.
Table 1.
Descriptions of studies included in the review
| Author, year | Country/Setting | Study Design | N (n) | Age Mean (SD) Median (IQR or range) | Developmental Delay Y/N | PAP Use Primary Outcome Y/N |
|---|---|---|---|---|---|---|
|
| ||||||
| Adeleye A et al 2016 (15) | Canada SC |
R C O | 92 (20) | 186 d (130.2, 277) | Y | N |
| Alebraheem Z et al 2018 (32) | Canada NR |
P C O | 21 | 16 y (range, 11–17) | N | N |
| Amaddeo A et al 2015 (33) | France SC |
R C O | 26 (20) | 7.8 y (6.2) | Y | N |
| Amaddeo A et al 2018 (38) | France SC |
P L O | 31 | 8.9 y (range, 0.8–17.5) | Y | Y |
| Avis K et al 2019 (53) | US SC |
P L E | 29 (20) | 11.9 y (2.7) | N | N |
| Beebe DW & Byars KC 2011 (54) | US SC & Non-SC |
P L E | 28 (13) | 14.6 y (1.6)§ | N | N |
| Bergeron M et al 2019 (39) | US SC & Non-SC |
P L E | 50 (19) | 8.8 y (95% CI, 6.9–10.6) | Y | N |
| Caldarelli V et al 2013(36) | France Non-SC |
P C O | 39 (15) | 9.7 y (4.7)* | NR | N |
| DiFeo N et al 2012 (22) | US SC |
P L O | 56 | 12 y (4) | Y | Y |
| Dudoignon B et al 2017 (35) | France SC |
R C O | 57 (11) | 6.2 y (5.9) | Y | N |
| Girbal IC et al 2014 (55) | Portugal Non-SC |
R C O | 68 | 6.6 y (1.3, 14.3) | Y | N |
| Harford KL et al 2013 (47) | US SC |
R C O | 19 | 12.1 y (4.4) § | Y | Y |
| Hawkins SM et al 2016 (40) | US SC |
R C O | 140 | 12.4 y (5.2) § | Y | Y |
| Jambhekar SK et al 2013 (16) | US SC |
R L O | 46 | 15.5 y (12,18) | Y | Y |
| Kang EK et al 2019 (12) | US SC |
R L O | 240 (177) | 7.9 (3.2, 13.1) (DD) 11 (5.5, 16) (TD) |
Y | Y |
| Katz SL et al 2017 (26) | Canada Non-SC |
P L O | 27 (22) | 14.5 y (12.6, 16.5) | N | N |
| Konstantinopoulou S et al 2016 (41) | US Non-SC |
P L E | 20* (11) | 10 y (9, 14.3)* | Y | N |
| Koontz KL et al 2003 (48) | US Non-SC |
R L E | 20 | 6 y (2, 10.5) ¶ | Y | Y |
| Kushida CA et al 2014 (34) | US SC &Non-SC |
P L E | 16 (14) | 6 y (1.6) | NR | N |
| Lynch MK et al 2017 (13) | US SC |
P L O | 42 (25) | 10.5 y (2.2) (Ad) 15.5 y (2.3) (Non-Ad) |
N | N |
| Machaalani R et al 2016 (14) | Australia SC |
R L O | 99 | 6.9 y (5.5) (CPAP) 9.8 y (5.9) (BPAP) |
Y | Y |
| Marcus CL et al 1995 (25) | US SC |
R C O | 94 (70) | <1–19 y † | Y | N |
| Marcus CL et al 2006 (29) | US SC |
P L E | 29 (18) | 10.4 y (4) § | N | Y |
| Marcus CL et al 2012 (21) | US SC |
P L E | 56 | 12 y (4) | Y | Y |
| Massa F et al 2002 (56) | UK SC |
R L O | 66 (42) | 5 y (5.4) § | Y | N |
| McNamara F & Sullivan CE 1999 (27) | Australia SC |
R L O | 24 | 37.6 wk (0.7) | Y | N |
| Mendoza-Ruiz et al 2019 (43) | France NR |
P L E | 15 | 5 y (3.8) § | Y | Y |
| Mihai R et al 2017 (44) | Australia SC |
R L O | 52 (26) | 11.9 y (3.4) | Y | N |
| Nakra N et al 2008 (57) | US SC &Non-SC |
P L E | 34 (25) | 13.1 y (3) | NR | N |
| Nathan AM et al 2013 (58) | Singapore Non-SC |
R C O | 51 | 11 y (8, 13) | Y | Y |
| Nixon GM et al 2011 (59) | Australia SC |
R C O | 30 | 9.1 y (5.3) | Y | Y |
| O’Donnell AR et al 2006 (18) | Canada SC |
R L O | 79 (50) | 10 y (5.1) | Y | Y |
| Prashad PS et al 2013 (42) | US SC |
P C O | 21 | 16 y (13, 17) ¶ | N | N |
| Perriol MP et al 2019 (23) | France SC & Non-SC |
P L O | 78 | 10.4 (3.2) | Y | N |
| Puri P et al 2016 (24) | US SC |
R L O | 56 | 13.2 y (3.7) | Y | Y |
| Ramirez A et al 2013 (45) | France Non-SC |
R C O | 51# | 10 y (5) | NR | Y |
| Riley EB et al 2017 (46) | US SC |
R L O | 275 | 9.8 y (5.6) | Y | N |
| Roberts SD et al 2016 (60) | US SC & Non-SC |
R L O | 217 (100) | 9.6 y (4.4) § | NR | N |
| Simon SL et al 2012 (19) | US SC |
P‡ L O | 51 (48) | 13.3 y (2.5) | Y | Y |
| Sundaram SS et al 2018(30) | US Non-SC |
P L E | 9 | 11.5 (1.2) | NR | N |
| Trucco F et al 2018 (28) | UK Non-SC |
R L O | 60 (25) | 5.7 y (3.1, 9.4) | Y | N |
| Uong EC et al 2007 (31) | US SC |
R L O | 46 (27) | 13.6 y (3.1) | Y | N |
| Waters KA et al 1995 (61) | Australia SC |
R C O | 413 (73) | 5.7 y (0.5) # | Y | N |
| Widger JA et al 2014 (37) | Australia SC |
R L O | 42 (27) | 11 y (6) | Y | N |
| Xanthopoulos MS et al 2017 (20) | US SC |
R C O | 161 (141) | 11.9 y (7.9, 15.5) | Y | Y |
| Yuan HC et al 2012 (62) | US NR |
P L E | 21 (6) | 12.3 y (2.5) | N | N |
Notes. N= total sample; (n)= sample with evaluable PAP data;
= only reporting on OSA group;
= no mean/median age provided;
= PAP data retrospective;
= combined means/medians;
= ages reported per participant in study, authors of this review calculated median and IQR;
= only reporting for PAP or OSA group.
Adherent (Ad), bilevel positive airway pressure (BPAP), cross sectional (C), continuous positive airway pressure (CPAP), days (d), developmental delay (DD), experimental (E), longitudinal (L), months (m), non-adherent (Non-Ad), non-sleep center (Non-SC), not reported (NR), observational (O), positive airway pressure (PAP), prospective (P), retrospective (R), sleep center (SC), typically developing (TD), unspecified/undetermined (U), years (y).
Subject characteristics
Pooled mean was calculated for studies that reported a mean and standard deviation for age (63%, 29/46), resulting in an average of 9.4 years (SD= 5.0) with a range of 0.7 years – 14.6 years; the range in studies reporting median age (26%, 12/46) is 0.5 years – 16 years. Four studies could not be included in this summary due to reporting mean ages independently for two sub-groups (e.g. CPAP and bi-level PAP, adherent and non-adherent, typically developing and developmental delay) [12–14], or reporting only a range of ages [25]. Seventy-four percent (34/46) of studies included children and adolescents with developmental delays. OSA was severe in the majority of studies based on apnea hypopnea index (AHI) or obstructive apnea hypopnea index (oAHI) ≥ 10 (n=18, n=9, respectively; Table 2). Seven studies reported both AHI and oAHI; three were categorically congruent as severe for both AHI and oAHI [12, 26, 27].
Table 2.
Obstructive sleep apnea, polysomnography and positive airway pressure characteristics
| Author (year) | Metric of Use | OSA (AHI or oAHI [o]) Criteria events/h | AHI or oAHI (o) (events/h) Mean (SD) Median (IQR or range) | Mask Type | PAP Type* | PAP Naïve Only Y/N |
|---|---|---|---|---|---|---|
|
| ||||||
| Adeleye A et al 2016 (15) | PR O C |
> 1.5 | 33.2 (36.6) 22.5 (11.3, 37.0) |
NR | U | NR |
| Alebraheem Z et al 2018 (32) | O | ≥ 1.5 | 14.1 (13.6)
(o)† 9.2 (5.9, 17.8) (o)† |
NR | U | N |
| Amaddeo A et al 2015 (33) | O | > 10 | NR | NR | CPAP (n=20) | N |
| Amaddeo A et al 2018 (38) | O | > 5 (o) | 12.5 (range, 5–100) (o) | Nasal FF Prongs |
CPAP (n=15) APAP (n=12) |
Y |
| Avis K et al 2019 (53) | O | ≥ 1.5 | 10.7 (15) | NR | CPAP (n=20) | Y |
| Beebe DW & Byars KC 2011 (54) | PR | > 1 (o) | 10.0 (6.8) (o) (Ad) 9.3 (5.7) (o) (Non-Ad) |
NR | U | NR |
| Bergeron M et al 2019 (39) | O | ≥ 1 | 9.8 (1.4–76.2) 10 (0.9–76.2) (o) |
NR | CPAP (n=19) | Y/N |
| Caldarelli V et al 2013 (36) | O | NR | NR | Nasal FF |
BPAP (n=14) PS-VP (n=1) |
N |
| DiFeo N et al 2012 (22) | O | NR | 19 (16) | NR | CPAP (n=13) BPAP (n=43) |
Y |
| Dudoignon B et al 2017 (35) | O | > 1 | 14 (16) 8 (11) (o) |
Nasal Nasobuccal | CPAP (n=15)§ NIV (n=4)§ |
N |
| Girbal IC et al 2014 (55) | PR | ≥ 1 | 9.7 (5.8,18.8) | Nasal Prongs |
CPAP (n=52) BPAP (n=16) |
N |
| Harford KL et al 2013 (47) | O | NR | 23.6 (22.1) (New Pt) 29 (23.7) (Prior Pt) |
NR | U | Y/N |
| Hawkins SM et al 2016 (40) | O | ≥ 1 | 20.3 (26.8) (Ad) 16.5 (21.2) (Non-Ad) |
NR | CPAP‡ BPAP‡ |
NR |
| Jambhekar SK et al 2013 (16) | O | NR | 26.7 (30) 16.1 (8.4–35.5) |
NR | U | N |
| Kang EK et al 2019 (12) | O | NR | 15.8 (9.8, 30.5) 14.7 (9.5, 29) (o) |
NR | CPAP‡ BPAP‡ APAP‡ |
Y |
| Katz SL et al 2017 (26) | MDR O |
> 1 (o) | 15.5 (7.4, 25.2) 16.8 (7.1, 23.9) (o) |
NR | CPAP (n=14)§ BPAP (n=13)§ |
Y |
| Konstantinopoulou S et al 2016 (41) | O | ≥ 1.5 | 13.9 (6.8, 21.5) (o) | NR | CPAP (n=11) | Y |
| Koontz KL et al 2003 (48) | O | NR | NR | NR | BPAP (n=20) | NR |
| Kushida CA et al 2014 (34) | O | NR | 17.3 (17) | Nasal FF Pillows |
CPAP (n=8) BPAP (n=6) | N |
| Lynch MK et al 2017 (13) | O | > 1.5 | 13.2 (19.6) (Ad) 10.5 (7.6) (Non-Ad) |
NR | CPAP (n=25) | Y |
| Machaalani R et al 2016 (14) | O | NR | 24.9 (22.8) (CPAP) 21.2 (21.5) (BPAP) 19 (18.4) (o) (CPAP) 9 (8.7) (o) (BPAP) |
Nasal FF Pillows |
CPAP (n=55) BPAP (n=44) |
Y |
| Marcus CL et al 1995 (25) | O PR |
NR | NR | Nasal | CPAP (n=70) | N |
| Marcus CL et al 2006 (29) | O | ≥ 5 | 27 (32) (o) | NR | CPAP (n=13) BPAP (n=16)†† | Y |
| Marcus CL et al 2012 (21) | O | NR | 22 (21) (CPAP) 18 (15) (BPAP) |
NR | CPAP (n=13) BPAP (n=43) | Y |
| Massa F et al 2002 (56) | PR | ≥ 5 | NR | Nasal | CPAP (n=42) | N |
| McNamara F & Sullivan CE 1999 (27) | NR | > 5 | 44.4 (9.3) (NREM) 68.6 (8.9) (REM) 14.6 (3.9) (o) (NREM) 43.6 (8.3) (o) (REM) |
Nasal | CPAP (n=24) | N |
| Mendoza-Ruiz et al 2019 (43) | O | > 5 | 25 (16) (Ad) 20 (15) (Non-Ad) |
NR | CPAP (n=15) | Y |
| Mihai R et al 2017 (44) | O | > 1 | 16.6 (11, 35) (o) | Nasal FF |
APAP (n=26) | Y |
| Nakra N et al 2008 (57) | O | ≥ 1.5/h | 8.7 (9.6) | NR | CPAP (n=25) | Y |
| Nathan AM et al 2013 (58) | C | ≥ 1 | 26.7 (12, 79.9) (o) | NR | CPAP (n=47) BPAP (n=4) |
N |
| Nixon GM et al 2011 (59) | O | NR | 22.6 (16) (o) (consistent users) 22.9 (22.6) (o) (intermittent) |
NR | CPAP (n=30) | Y |
| O’Donnell AR et al 2006 (18) | O | > 1 | 11.3 (5.4, 25.9) | Nasal FF |
CPAP (n=50) | Y |
| Prashad PS et al 2013 (42) | O | NR | 14 (4–78.3)# | NR | CPAP (n=21) | N |
| Perriol MP et al 2019 (23) | O | NR | 12.2 (10.6) | NR | CPAP (n=78) | Y |
| Puri P et al 2016 (24) | O | ≥ 1 | 25.2 (28.7) (o) 12.8 (7.9, 24) (o) |
NR | U | Y |
| Ramirez A et al 2013 (45) | O | NR | NR | Nasal FF Cannula |
CPAP or BPAP (n=51) | N |
| Riley EB et al 2017 (46) | O | NR | NR | NR | CPAP (n=275) | Y |
| Roberts SD et al 2016 (60) | O | ≥ 1 | 17.6 (19.8) (Ad) 12.0 (19.1) (Non-Ad) |
NR | CPAP (n=100) | NR |
| Simon SL et al 2012 (19) | O | NR | 17.7 (21.7) | Nasal FF |
CPAP (n=23) BPAP (n=4) APAP (n=24) |
N |
| Sundaram SS et al 2018 (30) | O | > 2 | NR | Nasal | CPAP (n=9) | Y |
| Trucco F et al 2018 (28) | O | > 1 | 11.1 (4.4,
24.9)¶ 2.7 (0.5, 18.8) (o)¶ |
NR | CPAP (n=18) BPAP (n=7) |
Y |
| Uong EC et al 2007 (31) | O PR |
≥ 5 | 28.4 (31.8) | NR | CPAP (n=20) BPAP (n=7) |
Y |
| Waters KA et al 1995 (61) | NR | NR | NR | Nasal Prongs | CPAP (n=73) | Y |
| Widger JA et al 2014 (37) | O | NR | NR | NR | CPAP (n=22) BPAP (n=5) | N |
| Xanthopoulos MS et al 2017 (20) | O | NR | 13.8 (7.1, 29.7) | NR | CPAP (n=141) | NR |
| Yuan HC et al 2012 (62) | PR | ≥ 5 | 19.5 (15.8) | NR | U | N |
Notes.
= n provided for those with adherence data;
= review authors calculated mean and median based on provided values per individual participant;
= n not provided;
= adherence data only available for a subsample but not specified how many per group;
= not exclusively OSA;
= AHI reported per participant in study, authors of this review calculated median and range
= n’s reflects full sample (n=29), not just those with adherence data (n=18).
Adherent (Ad), apnea hypopnea index (AHI), Automatic Positive Airway Pressure (APAP), bilevel positive airway pressure (BPAP), chart (C), continuous positive airway pressure (CPAP), full-face (FF), Medical Doctor report (MDR), non-adherent (Non-Ad), non-invasive ventilation (NIV), not reported (NR), objective (O), obstructive apnea hypopnea index (oAHI; o), obstructive sleep apnea (OSA), positive airway pressure (PAP), parent report (PR), pressure-support volume targeted ventilation (PS-VP), patient (Pt), unspecified/undetermined- article states “PAP” (U).
PAP characteristics and equipment
PAP use was most frequently measured using only an objective measure (76%, 35/46; Table 2). There was variability in the definition of OSA and/or OSA criteria for study inclusion; 41.3% (19/46) reported AHI or oAHI ≥ 1 < 5, 17.4% (8/46) ≥ 5, and 41.3% (19/46) did not state AHI criteria for inclusion. The type of PAP mask was frequently not reported (67.4%, 31/46); of studies that did report mask type (n=15), 26.7% (4/15) reported nasal mask only or a combination of nasal, full-face, pillows, or prongs (73.3%, 11/15). Studies with participants on CPAP made up 41.3% of studies (19/46), 39.1% (18/46) reported data on a combination of CPAP, bi-level PAP, or auto-PAP, 4.3% (2/46) reported only all auto-PAP or all bi-level PAP, and 15.2% (7/46) did not specify beyond “PAP.” Fifty-percent (23/46) enrolled participants that were new to PAP (i.e., PAP naïve), 37.2% (16/46) included existing PAP users, 10.9% (5/46) did not specify, and 4.3% (2/46) included a combination of new and existing PAP users.
PAP Use/Adherence
Varied definitions of PAP adherence were used, providing 24 unique definitions (see Table S2). Twenty-three studies (54.8%; 23/42) reported frequency of adherence and/or reported hours of PAP use (71.4%, 30/42; Table 3). Four studies included in the review did not report adherence as frequency or hours per night and were therefore excluded from Table 3 and PAP use analyses (see Table S3). In instances where authors provided a median and range, the minimum range value was selected for reporting in Table 3. Across 20 studies, inclusive of 1079 participants, average adherence across study samples was 56.9% (range, 24–87). Three studies [14, 26, 28] that reported percentage of adherence were excluded from the analysis as only sub-sample adherence data was reported.
Table 3.
Reported PAP use and adherence across 42 studies.
| Author (year) | n* | Definition of Adherence | Met Adherence n (%) | Average hours/night M (SD) or Median (IQR or range) | Outcome Assessment Period† |
|---|---|---|---|---|---|
|
| |||||
| Alebraheem Z et al 2018 (32) | 21 | > 4 h/night for >50% nights | 6 (29%) | 3.1 (3)c | 1 mo |
| Amaddeo A et al 2015 (33) | 20 | NR | NR | 7.4 (2.1)c | 1 mo |
| Amaddeo A et al 2018 (38) | 27 | ≥ 4 h/night after 2 mo | 27/31 (87%) | 8.2 (range, 5.5–12.2) | ≥ 2 mo |
| Avis K et al 2019 (53) | 20 | ≥ 4 h/night | 11 (55%) | NR | 3 mo |
| Beebe DW & Byars KC 2011 (54) | 13 | > 21% of sleep time | 7 (54%) | NR | 2 mo |
| Bergeron M et al 2019 (39) | 19 | > 4h/night | 8 (42%) | 4.0 (0.5–5.6) | ≥ 3 mo |
| Caldarelli V et al 2013 (36) | 15 | NR | NR | 7.3 (1.8) | NR |
| DiFeo N et al 2012 (22) | 56 | NR | NR | 3 (3)a 2.8 (2.7)b |
1 mo 3 mo |
| Dudoignon B et al 2017 (35) | 11 | > 4 h/night | 9 (82%) | 8.8 (4)d | 24 mo |
| Girbal IC et al 2014 (55) | 68 | > 3h/night | 53 (78%) | NR | NR |
| Harford KL et al 2013 (47) | 19 | > 4h/night for >70% nights | 5 (42%) (new pt) 3 (43%) (prior pt) |
NR | ≥ 6 wks |
| Hawkins SM et al 2016 (40) | 140 | ≥ 4 h/night for >70% nights | 69 (49%) | 7.4 (5.5–9.3)‡ (Ad,
n=69) 1.7 (0.3–3.1)‡ (Non-ad, n=71) |
NR |
| Jambhekar SK et al 2013 (16) | 46 | > 4 h/night for > 50% nights | 22 (48%) | NR | NR |
| Kang EK et al 2019 (12) | 177 | h use on nights used | NR | 5.72 (no IQR or range)# | 6 mo |
| Katz SL et al 2017 (26) | 22 | ≥ 4 h/night for > 50% nights | 14 (64%) (6 mo, n=22) 11 (69%) (12 mo, n=16) |
NR | 6 mo 12 mo |
| Konstantinopoulou S et al 2016 (41) | 11 | NR | NR | 1.9 (1.2, 2.3) | 3 mo |
| Koontz KL et al 2003 (48) | 20 | NR | NR | BT (n=11): 0.8 (no SD) (baseline) 5.9 (no SD) (post) CR+ (n=6): 1.7 (no SD) (baseline) 8.5 (no SD) (post) CR- (n=3): 3.3 (no SD) (baseline) 0.7 (no SD) (post) |
Baseline: NR Post: 25.7 mo (average) |
| Kushida CA et al 2014 (34) | 14 | NR | NR | 7.4 (2.6)§ d | ≥ 21 d |
| Lynch MK et al 2014 (13) | 25 | > 4 h/night for ≥ 50% nights | 15 (60%) | NR | 3 mo |
| Machaalani R et al 2016 (14) | 99 | ≥ 4 h/night for ≥ 70% nights | ≥ 4 wk: 41 (75%) (CPAP,
n=55) 40 (91%) (BPAP n=44) 12 mo: 13 (76%) (CPAP, n=17) 15 (80%) (BPAP, n=19) |
≥ 4 wk: 6.8 (2.8) (CPAP) 9.3 (3.6) (BPAP) 12 mo: 8 (4.1) (CPAP)b 9.3 (3.8) (BPAP)b |
≥ 4 wks 12 mo |
| Marcus CL et al 2006 (29) | 18 | Poor adherence < 3 h/night | NR | 5.3 (2.5) (PP; n=18)b 3.8 (3.3) (ITT; n=29) |
6 mo |
| Marcus CL et al 2012 (21) | 56 | NR | NR | CPAP (n=13) 3.4 (2.3) (1 mo)a 2.1 (2.5) (3 mo)b BPAP (n=43) 3.1 (2.8) (1 mo)a 3.1 (2.8) (3 mo)b |
1 mo 3 mo |
| Massa F et al 2002 (56) | 42 | Use every night, all night long | 28 (68%) | NR | NR |
| Mendoza-Ruiz et al 2019 (43) | 15 | >3 h/night | NR | 1 wk: 7.3 (1.9) (Ad; n=9) 1 (0.6) (Non-Ad; n=6 1 mo: 7.5 (2) (Ad; n=9) 4.5 (1.2) (Non-Ad; n=6 | 1 wk 1 mo |
| Mihai R et al 2017 (44) | 26 | NR | NR | 6.3 (2) (APAP)# 6.3 (2.7) (CPAP)# |
1 mo |
| Nathan AM et al 2013 (58) | 51 | ≥ 4 d/wk | 21 (41%) | NR | NR |
| Nixon GM et al 2011 (59) | 30 | > 1 h/night > 6 nights/wk | 10 (33%) | 4.7 (2.7)b | 2–3 mo |
| O’Donnell AR et al 2006 (18) | 51 | NR | NR | 4.7 (1.4–7) | ≥ 1.3 mo |
| Prashad PS et al 2013 (42) | 21 | NR | NR | 6.4 (1.3) (high use; n=7) ¶ 0.5 (0.4) (low use; n=7) ¶ 0 (0) (no use; n=7) ¶ | 1 mo |
| Perriol MP et al 2019 (23) | 78–34 | NR | NR | 6.1 (2.8) (1 mo;
n=78)a 6.2 (2.6) (3 mo; n=72)b 6.2 (2.8) (6 mo; n=63) 6.3 (2.8) (12 mo; n=55) 7.0 (2.7) (24 mo; n=34) |
1 mo 3 mo 6 mo 12 mo 24 mo |
| Puri P et al 2016 (24) | 56 | NR | NR | 3.5 (2.7) 2.9 (2.4)a 2.8 (2.4)b |
1 wk 1 mo 3 mo |
| Ramirez A et al 2013 (45) | 62 | > 8 h/night | 45 (72%) | 8.3 (2.5)# | 1 mo |
| Riley EB et al 2017 (46) | 275 | > 6 h/night for > 80% nights | 59 (24%) | 4.3 (2.9)# | 1 mo |
| Roberts SD et al 2016 (60) | 100 | ≥ 4h/night for 70% of nights for ≥ 6 mo | 50 (50%) | NR | ≥ 6 mo |
| Simon SL et al 2012 (19) | 48 | NR | NR | 3.4 (2.8)d | 3 mo |
| Sundaram SS et al 2018 (30) | 9 | NR | NR | 4.9 (2.1)b | ≥ 1 mo |
| Trucco F et al 2018 (28) | 25 | >4 h/night for >50% nights | Mo 4: 9 (50%) (CPAP, n=18) 4 (57%) (BPAP,
n=7) 1.9 y (IQR 0.8–3.7): 7 (39%) (CPAP, n=18) 4 (67%) (BPAP, n=6) |
Mo 4: 5 (2–8) (CPAP) 8 (2–8)
(BPAP) 1.9y: 4 (2–8) (CPAP) 8 (5–8) (BPAP) |
4 mo (average) 1.9 y (average) |
| Uong EC et al 2007 (31) | 27 | >4 h/night ≥5 nights/wk | 19 (70%) | 7.7 (1.5)b | ≥ 3 mo |
| Waters KA et al 1995 (61) | 73 | Regular use >6mo | 63 (86%) | NR | NR |
| Widger JA et al 2014 (37) | 27 | NR | NR | 5.2 (2.5) (CPAP, n=22) 9.3 (1.4) (BPAP, n=5) | NR |
| Xanthopoulos MS et al 2017 (20) | 141 | NR | NR | 2.9 (0.6– 5.8) | 1 mo |
| Yuan HC et al 2012 (62) | 6 | “Yes” for PAP use at evening and following morning ≥5 nights/wk | 4 (67%) | NR | 5–6 mo |
Notes.
= sample with adherence data;
= does not indicate short-term versus long term-use (i.e., 1 month may refer to 1 month of data at any given time point, not necessarily data from first month of PAP use);
= mean (mean − 1 SD–mean + 1 SD);
= from baseline mask and flow generator (i.e., pre-intervention);
= based on tertiles, participants purposefully recruited for each group;
= hours PAP use/night on nights used.
Included in the PAP use pooled mean (SD):
= PAP naïve (1 mo);
= PAP naïve (>1 mo);
= non-naïve (1 mo);
= non-naïve (>1 mo). Machaalani et al (14), 12 mo data used for analysis as outcome assessment period was more direct than ≥ 4 wks. Perriol et al (23), 3 mo data used since timepoint had the least attrition.
Adherent (Ad), Automatic Positive Airway Pressure (APAP), bilevel positive airway pressure (BPAP), continuous positive airway pressure (CPAP), hours (h), intention to treat (ITT), month (mo), non-adherent (Non-Ad), not reported (NR), patient (pt), per protocol (PP), positive airway pressure (PAP), week (wk).
At one month (i.e., first month of PAP use), PAP naïve participants used PAP for a pooled mean of 4.0 hours (SD= 3.1) per night; this statistic was derived from a total of 246 participants across four studies [21–24]. PAP naïve participants with > 1 month of data averaged 4.8 hours (SD= 3.4) per night across 9 studies with a total sample size of 360 [14, 17, 21–24, 29–31]. Two studies, consisting of 41 total participants, evaluated one month PAP use in non-naïve/existing PAP users; average PAP use was 5.2 hours (SD= 3.4) per night [32, 33]. Three studies, consisting of 73 total participants, evaluated > 1-month PAP use in non-naïve/existing PAP users; across the two studies participants averaged 5.0 hours (SD=3.7) hours per night [19, 34, 35]. Studies that reported mean hours of use but did not report an outcome assessment period (i.e., 1-month or > 1-month) [36, 37], reported use as median/range or interquartile range [12, 18, 20, 28, 38–41]; samples that were purposefully recruited as no-PAP, low-PAP, or high-PAP users [42, 43], or mean use reported for nights used rather than all nights [44–46] were excluded from pooled analysis but included in Table 3.
Based on 1079 cumulative participants from 20 studies, PAP is adhered to by less than 60% of participants, though varying definitions of adherence per study contribute risk to the reliability of this estimate of average pediatric PAP adherence. Further, PAP was used, on average, 4.0 hours (SD= 3.1) to 5.2 hours (SD= 3.4) per night. Though this closely mirrors the clinical definition of adherence by third party payers, it is not known if this amount of PAP use is therapeutically beneficial in pediatrics.
Factors influencing PAP use
Sixteen studies examined various factors associations with PAP use (Table 4). Across 16 studies, 43 individual factors were examined; 18 of which are not included in Table 4 as they were not significant and did not align with common categories of factors used across the PAP adherence literature (i.e., patient characteristics, device, OSA, or family/socioeconomic factors). Of 43 factors examined, 19 were statistically significantly associated with PAP use or adherence, though these individual factors were not consistently significant across multiple studies. Age was the most frequently examined patient characteristic and was significantly associated with PAP use in 38% (5/13) of studies examining age (Table 4) with younger children using PAP more than adolescents. Sex was found to be a significant predictor in 18.2% (2/11) of studies with females using PAP more than males and developmental delay was found to be a significant predictor in 40% (2/5) of studies, with those with developmental delay being more adherent. All other tested factors were not significant in two or more studies.
Table 4.
Factors influencing PAP use
| Avis et al. (2019) [53] | DiFeo et al. (2012) [22] | Hawkins et al. (2016) [40] | Kang et al. (2019) [12] | Lynch et al. (2019) [13] | Machaalani et al. (2017) [14] | Marcus et al. (2006) [29] | Macrcus et al. (2012) [21] | Nathan et al. (2013) [58] | Nixon et al. (2011) [59] | O’Donnell et al. (2006) [18] | Puri et al. (2016) [24] | Ramirez et al. (2013) [45] | Simon et al. (2012) [19] | Uong et al. (2007) [31] | Xanthopoulos et al. (2017) [20] | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient Characteristics | ||||||||||||||||
|
| ||||||||||||||||
| Age | * | * | NS | * | NS | NS | NS | NS | NS | * | * | NS | NS | |||
|
| ||||||||||||||||
| Sex | NS | NS | * | NS | NS | NS | * | NS | NS | NS | NS | |||||
|
| ||||||||||||||||
| Race/Ethnicity | NS | * | NS | NS | NS | NS | ||||||||||
|
| ||||||||||||||||
| BMI | NS | NS | * | NS | NS | NS | ||||||||||
|
| ||||||||||||||||
| Developmental delay | NS | * | * | NS | NS | |||||||||||
|
| ||||||||||||||||
| Comorbidities | * | NS | NS | |||||||||||||
|
| ||||||||||||||||
| Technological Device Factors | ||||||||||||||||
|
| ||||||||||||||||
| Device pressure | NS | NS | NS | NS | ||||||||||||
|
| ||||||||||||||||
| Mask type | * | NS | NS | |||||||||||||
|
| ||||||||||||||||
| Device type | NS | * | NS | NS | NS | |||||||||||
|
| ||||||||||||||||
| Unintentional leaks | NS | |||||||||||||||
|
| ||||||||||||||||
| Device brand | NS | |||||||||||||||
|
| ||||||||||||||||
| Disease | ||||||||||||||||
|
| ||||||||||||||||
| Severity | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS | * | |||||
|
| ||||||||||||||||
| Side effects/ symptoms |
NS | NS | NS | NS | NS | |||||||||||
|
| ||||||||||||||||
| Duration of PAP use |
NS | NS | NS | * | ||||||||||||
|
| ||||||||||||||||
| Family/Socioeconomic Status | ||||||||||||||||
|
| ||||||||||||||||
| Parent on PAP | * | |||||||||||||||
|
| ||||||||||||||||
| Insurance status | NS | |||||||||||||||
|
| ||||||||||||||||
| Household income | NS | * | NS | |||||||||||||
|
| ||||||||||||||||
| SES | NS | |||||||||||||||
|
| ||||||||||||||||
| Maternal education | * | NS | ||||||||||||||
|
| ||||||||||||||||
| Other | ||||||||||||||||
|
| ||||||||||||||||
| Titration prior to 6 mo | * | |||||||||||||||
|
| ||||||||||||||||
| Self-efficacy CG Self | ||||||||||||||||
| CG | * | |||||||||||||||
| Self | NS | |||||||||||||||
|
| ||||||||||||||||
| Caregiver concern** | * | |||||||||||||||
|
| ||||||||||||||||
| Greater barriers to treatment | * | |||||||||||||||
|
| ||||||||||||||||
| Change in PAP pressure | * | |||||||||||||||
|
| ||||||||||||||||
| Monetary assistance from social work dept in purchasing machine | * | |||||||||||||||
Notes.
=significant (p < 0.05); NS= non-significant;
= based on OSA-18 questionnaire.
Body mass index (BMI), caregiver (CG), department (dept), positive airway pressure (PAP), socioeconomic status (SES).
Two studies not included in Table 4 used qualitative methods to identify factors related to PAP use. These studies [32, 42] identified home and family structure, style of communication, social reactions and attitudes, adolescent perception of PAP benefits, and design of the machine (e.g., mask and tubing) to be influential. Other factors reported were; importance of an adjustment period to adapt and address unique issues, perceived barriers and challenges being more apparent than experiencing symptom relief, and amount of family support desired being individual and based on the unique needs of adolescents. Age, sex, and developmental delay were the only factors found to be significant across two or more studies, however, these are not consistently identified (significant in 18.2% - 40% of studies). Factors identified by qualitative studies should be further explored in prospective, quantitative studies to further substantiate their influence on PAP non-adherence in the general pediatric PAP population.
Approaches to improve PAP use and adherence
A small number of studies included in this review described approaches to improve PAP use in the form of programmatic changes [16, 46, 47] or systematic testing of interventions [43, 48]. Descriptions of the approaches are detailed in Table S4. Reported programmatic changes were reported as effective at improving adherence with 33–43% of the samples improving PAP use [16, 47], or increasing rates of follow-up visits and completed PAP titrations with 24% reporting “excellent” adherence [46].
Two small pilot studies with modest sample sizes systematically tested PAP interventions [43, 48]. When three groups were compared, 1) formal behavioral therapy 6-week session, 2) one 1.5 hour consultation session and parent-reported implementation of changes at home, and 3) one 1.5 hour consultation and parent reported no implementation at home, the only significant difference for PAP adherence post-treatment (average of 25.7 months) was identified between home implementation groups, with those that implemented changes being more adherent (p<0.05) [48]. Another study identified that by having non-adherent children log days they did and did not use their PAP on a calendar resulted in a significant improvement in hours of PAP used from 1-week to 1-month (1 hour ± 33 minutes, 4 hours ± 31 minutes, respectively; p < 0.001).
Evidence appraisal
Using the Johns Hopkins appraisal system [11], studies were: Level 1 study (n = 4), Level 2 (n = 7), Level 3 (n = 33), Level 4 (n = 0), and Level 5 (n = 2). Study quality ratings were of high quality (n = 3), good quality (n = 27), or low quality (n = 16; Table S5).
Discussion
The scoping review addressed the state of the science for pediatric PAP use in the management of OSA, factors influencing PAP use, and described approaches that promote PAP use. This review is the first to cumulatively evaluate PAP use in pediatrics. The pediatric PAP literature lacks both high level and quality evidence and is heterogeneous for design, measurement, and reported analyses which contribute to challenges for summarizing and comparing studies. Study heterogeneity was also noted for sample size, sampling criteria and thereby reported characteristics (e.g., age, developmental delays, OSA severity, new or established PAP users), and PAP modes (e.g., CPAP, bi-level PAP, auto-PAP). Perhaps one of the largest barriers identified by the review is the absence of an evidence-based PAP use threshold that equates to adherence, or at least a consistently applied definition of PAP adherence. In the absence of a study-provided definition of PAP adherence and consistency with employing such a definition across studies, a systematic review with or without a meta-analysis to more precisely estimate PAP use in pediatrics is not feasible. Additionally, varied measurement intervals of the primary outcome of PAP use contributes to low feasibility for systematically summarizing the state of the science of PAP adherence in pediatrics. Furthermore, included studies reported one-month PAP use, but “one month” may be reflective of the first month of PAP use in naïve users, or, reflective of one month use data at any given time point as samples included both established users and new users. Cautious consideration of these caveats with the provided summary estimates of this scoping review are therefore necessary.
In attempt to mitigate inconsistent reporting of results, we propose that dose-response studies are needed in order to form a consensus on the most efficacious threshold of PAP use and that any such thresholds should be separately established for infants, children and adolescents. Doing so would allow the field to identify a consistent definition of pediatric PAP adherence that is not only clinically beneficial, but would also support accurate comparisons between and across studies. Until such evidence is available, an initial suggestion is that investigators uniformly present PAP use data as mean (SD) and median (IQR) hours or minutes for “all days” and separately for “days used”. This will necessarily be reported for the entire sample and as indicated by study methods and objectives, for sub-groups that are a priori precisely defined.
The heterogeneous outcome assessment intervals for both PAP naïve and existing PAP users highlights the need for longitudinal studies that follow new PAP users; this approach will permit discovery of PAP patterns of use, or adherence, over time. Mean PAP use was reported for both naïve and existing PAP users at 1-month and > 1-month, however, mean use does not account for attrition where PAP use may have been discontinued in a portion of the sample. Longitudinal studies are needed to determine if a behavioral pattern of PAP use exists in pediatrics. Clinically, reimbursements by insurance mandate adequate adherence by 90 days; research aimed to investigate patterns of adherence in pediatrics, across the age spectrum, would be beneficial to determine if meeting this threshold is actually appropriate or feasible for this population. Furthermore, such studies would be insightful for determining potential critical intervention points in the course of starting and maintaining PAP treatment in pediatrics.
In order to better understand factors that influence PAP use, future study samples should include similar aged participants, or be large enough to statistically examine factors separately for children and adolescents. This is important as age is one of the consistently identified predictors of PAP adherence. This would support more precise estimates of association while also taking into consideration clinically relevant developmental differences between children and adolescents. For example, a younger child is likely to have different adherence-related barriers and facilitators as well as a longer sleep opportunity than an adolescent. Similarly, studies in this review included a sub-set of children, or adolescents, with developmental delays. Early evidence suggests that adherence rates may be different for children who are developmentally delayed versus those that are typically developing [12, 40]. Multi-center trials are required to yield sufficient numbers to evaluate age-specific sub-group analyses of influential factors on PAP use and such studies should prioritize factors of influences as the primary aim. By doing so, the development and testing of targeted interventions to improve PAP use is likely to emerge.
Because the state of science on PAP adherence in pediatrics is currently underdeveloped, including PAP adherence interventions, the field may benefit from developing and adapting theory-guided adherence and self-management interventions from other pediatric chronic conditions. Another opportunity may be the adaptation of efficacious PAP adherence interventions derived from the adult literature for specific testing in older children and adolescents. This, however, can only be considered if familial/caregiver units are addressed with the adaptation as this is a unique and important contextual factor in pediatrics.
The field currently lacks evidence-based recommendations and direction for initiating and managing PAP use in pediatric populations. Though prior review papers addressing PAP in pediatrics exist [6, 49–52], the current review is the first to focus specifically on PAP adherence in the general pediatric OSA population while employing rigorous review methods. The present review provides a focused description of the state of the science addressing PAP treatment of OSA in pediatrics and sets forth recommendations and a research agenda. Though the heterogeneity of studies currently prohibits a rigorous analysis using a systematic review or meta-analysis approach, this review is the first to summarize PAP use in pediatric OSA.
Limitations
Limitations of the current review were related to the inability to make strong, direct comparisons across studies due to low level and quality of included studies, heterogeneity of included studies, and the limited number of systematically tested interventions for PAP adherence to inform recommendations for improving adherence. Because the literature is heterogeneous across multiple factors (e.g., study characteristics, subject characteristics, adherence parameters, outcome assessment periods), an estimate of PAP use in pediatric OSA is provided with acknowledged methodological caveats.
Conclusion
Though PAP has been used to treat pediatric OSA for a few decades, rates and determinants of PAP use are not well understood. To address this limitation for the field, higher level and quality studies are needed which include: 1) prospective, longitudinal studies that are a priori adequately powered; 2) replication studies; and 3) rigorous trials, beginning with pilot studies that appropriately progress to randomized control trials. These studies are needed to: 1) identify the optimal duration of nightly PAP use to inform appropriate adherence parameters, 2) gain a comprehensive understanding of PAP use and adherence, 3) determine influential factors on PAP use that may be putative for intervention development, and 4) design and test the efficacy of PAP adherence interventions.
Supplementary Material
Practice points:
There are unique developmental considerations for PAP use and adherence across age groups and developmental abilities.
Certain youth may be at higher risk for PAP non-adherence, including older children/adolescents and males, though factors are not well-established at this time and other factors are yet to be identified.
-
Guidelines from the American Academy of Pediatrics suggest that if PAP adherence is suboptimal, clinicians can institute measures such as behavioral modifications and treating of side effects and clinicians should institute alternative treatments if these measures are ineffective. These recommendations are also supported by the American Academy of Sleep Medicine Task Force for promoting high quality patient-centered care. We recommend readers to these resources until additional evidence is available.
Research agenda:
Conduct high quality studies to determine an ideal threshold of PAP at various stages of childhood.
Determine appropriate age-related adherence parameters and reach a consensus for a definition of “adherent”.
Recruit more homogeneous samples (e.g., all new PAP users; limit age criteria or larger sample sizes to permit sub-group analyses).
Identify factors that may influence PAP adherence to guide tailored intervention opportunities.
Develop interventions that address both parent/caregiver and child/adolescent to maximize potential of success.
Utilize technology and telehealth as a viable and innovative approach for intervention development, as PAP use can be objectively measured and rapidly assessed and children/adolescents are high technology consumers.
Acknowledgements:
Support from NIH/NHLBI Award T32 HL07953 (AJW). The ideas and opinions expressed in this article are those of the authors and endorsement of those opinions by the funding agency, or Veterans Affairs, is not intended nor inferred.
Abbreviations:
- AHI
apnea hypopnea index
- CPAP
continuous positive airway pressure
- OSA
obstructive sleep apnea
- PAP
positive airway pressure
Footnotes
Conflicts of Interest: The authors do not have any conflicts of interest to disclose.
References
- 1.American Thoracic Society. Standards and indications for cardiopulmonary sleep studies in children.Am J Respir Crit Care Med. 1996;153(2):866–78. [DOI] [PubMed] [Google Scholar]
- 2.Lumeng JC, Chervin RD. Epidemiology of pediatric obstructive sleep apnea. Proc Am Thorac Soc. 2008;5(2):242–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Katz ES, D’Ambrosio CM. Pathophysiology of pediatric obstructive sleep apnea. Proc Am Thorac Soc. 2008;5(2):253–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.American Academy of Sleep Medicine. International Classification of Sleep Disorders. 3 ed. Darien IL: American Academy of Sleep Medicine; 2014. [Google Scholar]
- 5.Capdevila OS, Kheirandish-Gozal L, Dayyat E, Gozal D. Pediatric obstructive sleep apnea: complications, management, and long-term outcomes. Proc Am Thorac Soc. 2008;5(2):274–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *6.Marcus CL, Brooks LJ, Draper KA, Gozal D, Halbower AC, Jones J, et al. Diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics. 130. United States 2012. p. e714–55. [DOI] [PubMed] [Google Scholar]
- 7.Lee CF, Lee CH, Hsueh WY, Lin MT, Kang KT. Prevalence of obstructive sleep apnea in children with down syndrome: A meta-analysis. J Clin Sleep Med. 2018;14(5):867–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Medicare & Medicaid Services. Positive Airway Pressure (PAP) Devices: Complying with Documentation & Coverage Requirements. In: Services DoHaH, editor. 2016. [Google Scholar]
- 9.King MS, Xanthopoulos MS, Marcus CL. Improving positive airway pressure adherence in children. Sleep Med Clin. 2014;9(2):219–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann Intern Med. 2018;169(7):467–73. [DOI] [PubMed] [Google Scholar]
- 11.Newhouse R, Dearholt S, Poe S, Pugh LC, White K. The Johns Hopkins Nursing Evidence-based Practice Rating Scale. Baltimore, MD: The Johns Hopkins Hospital; Johns Hopkins University School of Nursing; 2005. [Google Scholar]
- *12.Kang EK, Xanthopoulos MS, Kim JY, Arevalo C, Shults J, Beck SE, et al. Adherence to positive airway pressure for the treatment of obstructive sleep apnea in children with developmental disabilities. J Clin Sleep Med. 2019;16(6):915–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lynch MK, Elliott LC, Avis KT, Schwebel DC, Goodin BR. Quality of life in youth with obstructive sleep apnea syndrome (OSAS) treated with continuous positive airway pressure (CPAP) therapy. Behav Sleep Med. 2019;17(3):238–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *14.Machaalani R, Evans CA, Waters KA. Objective adherence to positive airway pressure therapy in an Australian paediatric cohort. Sleep Breath. 2016;20(4):1327–36. [DOI] [PubMed] [Google Scholar]
- 15.Adeleye A, Ho A, Nettel-Aguirre A, Buchhalter J, Kirk V. Noninvasive positive airway pressure treatment in children less than 12 months of age. Can Respir J. 2016;2016:7654631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jambhekar SK, Com G, Tang X, Pruss KK, Jackson R, Bower C, et al. Role of a respiratory therapist in improving adherence to positive airway pressure treatment in a pediatric sleep apnea clinic. Respir Care. 2013;58(12):2038–44. [DOI] [PubMed] [Google Scholar]
- 17.Nixon GM, Mihai R, Verginis N, Davey MJ. Patterns of continuous positive airway pressure adherence during the first 3 months of treatment in children. J Pediatr. 2011;159(5):802–7. [DOI] [PubMed] [Google Scholar]
- 18.O’Donnell AR, Bjornson CL, Bohn SG, Kirk VG. Compliance rates in children using noninvasive continuous positive airway pressure. Sleep. 2006;29(5):651–8. [PubMed] [Google Scholar]
- 19.Simon SL, Duncan CL, Janicke DM, Wagner MH. Barriers to treatment of paediatric obstructive sleep apnoea: Development of the adherence barriers to continuous positive airway pressure (CPAP) questionnaire. Sleep Med. 2012;13(2):172–7. [DOI] [PubMed] [Google Scholar]
- 20.Xanthopoulos MS, Kim JY, Blechner M, Chang MY, Menello MK, Brown C, et al. Self-efficacy and short-term adherence to continuous positive airway pressure treatment in children. Sleep. 2017;40(7). [DOI] [PubMed] [Google Scholar]
- *21.Marcus CL, Beck SE, Traylor J, Cornaglia MA, Meltzer LJ, DiFeo N, et al. Randomized, double-blind clinical trial of two different modes of positive airway pressure therapy on adherence and efficacy in children. J Clin Sleep Med. 2012;8(1):37–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *22.DiFeo N, Meltzer LJ, Beck SE, Karamessinis LR, Cornaglia MA, Traylor J, et al. Predictors of positive airway pressure therapy adherence in children: a prospective study. J Clin Sleep Med. 2012;8(3):279–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *23.Perriol MP, Jullian-Desayes I, Joyeux-Faure M, Bailly S, Andrieux A, Ellaffi M, et al. Long-term adherence to ambulatory initiated continuous positive airway pressure in non-syndromic OSA children. Sleep Breath. 2019;23(2):575–8. [DOI] [PubMed] [Google Scholar]
- 24.Puri P, Ross KR, Mehra R, Spilsbury JC, Li H, Levers-Landis CE, et al. Pediatric positive airway pressure adherence in obstructive sleep apnea enhanced by family member positive airway pressure usage. J Clin Sleep Med. 2016;12(7):959–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Marcus CL, Ward SL, Mallory GB, Rosen CL, Beckerman RC, Weese-Mayer DE, et al. Use of nasal continuous positive airway pressure as treatment of childhood obstructive sleep apnea. J Pediatr. 1995;127(1):88–94. [DOI] [PubMed] [Google Scholar]
- 26.Katz SL, MacLean JE, Hoey L, Horwood L, Barrowman N, Foster B, et al. Insulin resistance and hypertension in obese youth with sleep-disordered breathing treated with positive airway pressure: A prospective multicenter study. J Clin Sleep Med. 2017;13(9):1039–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McNamara F, Sullivan CE. Obstructive sleep apnea in infants and its management with nasal continuous positive airway pressure. Chest. 1999;116(1):10–6. [DOI] [PubMed] [Google Scholar]
- 28.Trucco F, Chatwin M, Semple T, Rosenthal M, Bush A, Tan HL. Sleep disordered breathing and ventilatory support in children with Down syndrome. Pediatr Pulmonol. 2018;53(10):1414–21. [DOI] [PubMed] [Google Scholar]
- 29.Marcus CL, Rosen G, Ward SL, Halbower AC, Sterni L, Lutz J, et al. Adherence to and effectiveness of positive airway pressure therapy in children with obstructive sleep apnea. Pediatrics. 2006;117(3):e442–51. [DOI] [PubMed] [Google Scholar]
- 30.Sundaram SS, Halbower AC, Klawitter J, Pan Z, Robbins K, Capocelli KE, et al. Treating obstructive sleep apnea and chronic intermittent hypoxia improves the severity of nonalcoholic fatty liver disease in children. J Pediatr. 2018;198:67–75.e1. [DOI] [PubMed] [Google Scholar]
- 31.Uong EC, Epperson M, Bathon SA, Jeffe DB. Adherence to nasal positive airway pressure therapy among school-aged children and adolescents with obstructive sleep apnea syndrome. Pediatrics. 2007;120(5):e1203–11. [DOI] [PubMed] [Google Scholar]
- 32.Alebraheem Z, Toulany A, Baker A, Christian J, Narang I. Facilitators and barriers to positive airway pressure adherence for adolescents. A qualitative study. Ann Am Thorac Soc. 2018;15(1):83–8. [DOI] [PubMed] [Google Scholar]
- 33.Amaddeo A, Caldarelli V, Fernandez-Bolanos M, Moreau J, Ramirez A, Khirani S, et al. Polygraphic respiratory events during sleep in children treated with home continuous positive airway pressure: description and clinical consequences. Sleep Med. 2015;16(1):107–12. [DOI] [PubMed] [Google Scholar]
- 34.Kushida CA, Halbower AC, Kryger MH, Pelayo R, Assalone V, Cardell CY, et al. Evaluation of a new pediatric positive airway pressure mask. J Clin Sleep Med. 2014;10(9):979–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dudoignon B, Amaddeo A, Frapin A, Thierry B, de Sanctis L, Arroyo JO, et al. Obstructive sleep apnea in Down syndrome: Benefits of surgery and noninvasive respiratory support. Am J Med Genet A. 2017;173(8):2074–80. [DOI] [PubMed] [Google Scholar]
- 36.Caldarelli V, Borel JC, Khirani S, Ramirez A, Cutrera R, Pepin JL, et al. Polygraphic respiratory events during sleep with noninvasive ventilation in children: description, prevalence, and clinical consequences. Intensive Care Med. 2013;39(4):739–46. [DOI] [PubMed] [Google Scholar]
- 37.Widger JA, Davey MJ, Nixon GM. Sleep studies in children on long-term non-invasive respiratory support. Sleep Breath. 2014;18(4):885–9. [DOI] [PubMed] [Google Scholar]
- *38.Amaddeo A, Frapin A, Touil S, Khirani S, Griffon L, Fauroux B. Outpatient initiation of long-term continuous positive airway pressure in children. Pediatr Pulmonol. 2018;53(10):1422–8. [DOI] [PubMed] [Google Scholar]
- 39.Bergeron M, Duggins A, Chini B, Ishman SL. Clinical outcomes after shared decision-making tools with families of children with obstructive sleep apnea without tonsillar hypertrophy. Laryngoscope. 2019. [DOI] [PubMed] [Google Scholar]
- *40.Hawkins SM, Jensen EL, Simon SL, Friedman NR. Correlates of pediatric CPAP adherence. J Clin Sleep Med. 2016;12(6):879–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Konstantinopoulou S, Tapia IE, Kim JY, Xanthopoulos MS, Radcliffe J, Cohen MS, et al. Relationship between obstructive sleep apnea cardiac complications and sleepiness in children with Down syndrome. Sleep Med. 2016;17:18–24. [DOI] [PubMed] [Google Scholar]
- 42.Prashad PS, Marcus CL, Maggs J, Stettler N, Cornaglia MA, Costa P, et al. Investigating reasons for CPAP adherence in adolescents: a qualitative approach. J Clin Sleep Med. 2013;9(12):1303–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mendoza-Ruiz A, Dylgjeri S, Bour F, Damagnez F, Leroux K, Khirani S. Evaluation of the efficacy of a dedicated table to improve CPAP adherence in children: a pilot study. Sleep Medicine. 2019;53:60–4. [DOI] [PubMed] [Google Scholar]
- 44.Mihai R, Vandeleur M, Pecoraro S, Davey MJ, Nixon GM. Autotitrating CPAP as a tool for CPAPinitiation for children. J Clin Sleep Med. 2017;13(5):713–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ramirez A, Khirani S, Aloui S, Delord V, Borel JC, Pepin JL, et al. Continuous positive airway pressure and noninvasive ventilation adherence in children. Sleep Med. 2013;14(12):1290–4. [DOI] [PubMed] [Google Scholar]
- 46.Riley EB, Fieldston ES, Xanthopoulos MS, Beck SE, Menello MK, Matthews E, et al. Financial analysis of an intensive pediatric continuous positive airway pressure program. Sleep. 2017;40(2). [DOI] [PubMed] [Google Scholar]
- 47.Harford KL, Jambhekar S, Com G, Pruss K, Kabour M, Jones K, et al. Behaviorally based adherence program for pediatric patients treated with positive airway pressure. Clin Child Psychol Psychiatry. 2013;18(1):151–63. [DOI] [PubMed] [Google Scholar]
- 48.Koontz KL, Slifer KJ, Cataldo MD, Marcus CL. Improving pediatric compliance with positive airway pressure therapy: the impact of behavioral intervention. Sleep. 2003;26(8):1010–5. [DOI] [PubMed] [Google Scholar]
- 49.Castro-Codesal ML, Dehaan K, Featherstone R, Bedi PK, Martinez Carrasco C, Katz SL, et al. Long-term non-invasive ventilation therapies in children: A scoping review. Sleep Med Rev. 2018;37:148–58. [DOI] [PubMed] [Google Scholar]
- 50.Sawyer AM, Gooneratne NS, Marcus CL, Ofer D, Richards KC, Weaver TE. A systematic review of CPAP adherence across age groups: clinical and empiric insights for developing CPAP adherence interventions. Sleep Med Rev. 15. England: 2011 Elsevier Ltd; 2011. p. 343–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Andersen IG, Holm JC, Homoe P. Obstructive sleep apnea in obese children and adolescents, treatment methods and outcome of treatment - A systematic review. Int J Pediatr Otorhinolaryngol. 2016;87:190–7. [DOI] [PubMed] [Google Scholar]
- 52.Kirk VG, O’Donnell AR. Continuous positive airway pressure for children: a discussion on how to maximize compliance. Sleep Med Rev. 2006;10(2):119–27. [DOI] [PubMed] [Google Scholar]
- 53.Avis KT, Gamble KL, Schwebel DC. Effect of positive airway pressure therapy in children with obstructive sleep apnea syndrome: does positive airway pressure use reduce pedestrian injury risk? Sleep Health. 2019;5(2):161–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Beebe DW, Byars KC. Adolescents with obstructive sleep apnea adhere poorly to positive airway pressure (PAP), but PAP users show improved attention and school performance. PLoS One. 2011;6(3):e16924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Girbal IC, Goncalves C, Nunes T, Ferreira R, Pereira L, Saianda A, et al. Non-invasive ventilation in complex obstructive sleep apnea--a 15-year experience of a pediatric tertiary center. Rev Port Pneumol. 2014;20(3):146–51. [DOI] [PubMed] [Google Scholar]
- 56.Massa F, Gonsalez S, Laverty A, Wallis C, Lane R. The use of nasal continuous positive airway pressure to treat obstructive sleep apnoea. Arch Dis Child. 2002;87(5):438–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Nakra N, Bhargava S, Dzuira J, Caprio S, Bazzy-Asaad A. Sleep-disordered breathing in children with metabolic syndrome: the role of leptin and sympathetic nervous system activity and the effect of continuous positive airway pressure. Pediatrics. 2008;122(3):e634–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Nathan AM, Tang JP, Goh A, Teoh OH, Chay OM. Compliance with noninvasive home ventilation in children with obstructive sleep apnoea. Singapore Med J. 2013;54(12):678–82. [DOI] [PubMed] [Google Scholar]
- 59.Nixon GM, Mihai R, Verginis N, Davey MJ. Patterns of continuous positive airway pressure adherence during the first 3 months of treatment in children. J Pediatr. 2011;159(5):802–7. [DOI] [PubMed] [Google Scholar]
- 60.Roberts SD, Kapadia H, Greenlee G, Chen ML. Midfacial and dental changes associated with nasal positive airway pressure in children with obstructive sleep apnea and craniofacial conditions. J Clin Sleep Med. 2016;12(4):469–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Waters KA, Everett FM, Bruderer JW, Sullivan CE. Obstructive sleep apnea: the use of nasal CPAP in 80 children. Am J Respir Crit Care Med. 1995;152(2):780–5. [DOI] [PubMed] [Google Scholar]
- 62.Yuan HC, Sohn EY, Abouezzeddine T, Mahrer NE, Barber BA, Keens TG, et al. Neurocognitive functioning in children with obstructive sleep apnea syndrome: a pilot study of positive airway pressure therapy. J Pediatr Nurs. 2012;27(6):607–13. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.